Introduction
Patients with cancer are subjected to numerous
stressors, caused not only by the cancer itself but also by the
subsequent treatment. These stressors include physical, mental and
social factors that can collectively affect the patient's quality
of life (QOL). The World Health Organization has included QOL as a
fundamental concept in the definition of ‘health’, which is a state
of complete physical, mental, and social well-being, and not merely
the absence of disease or infirmity (1).
Currently, the impact on QOL is an important factor
to consider, in addition to treatment efficacy, when determining
treatment regimens. Previous studies in various types of cancer,
such as colorectal and non-small cell lung cancer, have reported
that QOL affects the prognosis of patients (2–5). Most of
these studies included patients with cancer and distant metastases,
who had received chemotherapy, and reported that
chemotherapy-associated side effects caused deterioration in QOL.
However, in hormone receptor-positive breast cancer with distant
metastases, unless death is imminent, a common first-line treatment
is endocrine therapy (6). Even
though this treatment is not curative, it is chosen because of its
positive impact on QOL (fewer treatment-associated side effects),
as well as patient prognosis.
As the average life expectancy and the number of
elderly breast cancer cases have increased, the evaluation of QOL
in the elderly patients has become more important. In the present
study, the differences in QOL were evaluated based on the age and
prognostic indicators of patients with breast cancer and distant
metastases (stage IV), who received first-line endocrine
therapy.
Patients and methods
Study design
In this retrospective cohort study, patients treated
with first-line endocrine therapy, after being diagnosed with
hormone receptor-positive breast cancer with distant metastases at
the Osaka City University Hospital between November 2007 and
November 2016, were selected. The study was conducted at Osaka City
University Graduate School of Medicine, according to the Reporting
Recommendations for Tumor Marker Prognostic Studies (REMARK)
guidelines and following a retrospectively written research,
pathological evaluation, and statistical plan (7). The study protocol was approved by the
Ethics Committee of Osaka City University (approval no. 926) and
written informed consent was obtained from all patients.
Patient background
Forty-six patients were treated with first-line
endocrine therapy after being diagnosed with hormone
receptor-positive breast cancer [estrogen receptor (ER) and/or
progesterone receptor (PgR)-positive] with distant metastases. All
patients were pathologically diagnosed with breast cancer, and the
expression levels of ER, PgR, human epidermal growth factor
receptor 2 (HER2), and Ki67 were confirmed by immunostaining.
Staging was evaluated by ultrasonography (US), computed tomography
(CT), and bone scintigraphy. Patients with dementia were excluded.
All patients were prescribed hormonal therapy drugs as outpatients.
Patients were required to visit the hospital 3 months after
treatment initiation for physical examinations, US and CT to
determine the therapeutic effects, which were evaluated according
to the Response Evaluation Criteria in Solid Tumors (8).
Study outcomes
To determine the objective response rate (ORR),
‘responder’ was defined as a patient showing a clinical partial
response (cPR) or a clinical complete response (cCR); and
‘non-responder’ was defined as a patient with a clinical stable
disease (cSD) or a clinical progressive disease (cPD).
Progression-free survival (PFS) rate was defined as the period from
the treatment initiation to the time when cPD was detected or to
the date of death. Overall survival (OS) rate was defined as the
period from the treatment initiation to the date of death or the
censor date at the end of the study period, if still alive. All
patients underwent follow-up physical examinations every 3 months,
and US and CT every 6 months.
QOL evaluation
The widely accepted general QOL scale for cancer in
Japan is based on the Quality of Life Questionnaire for Cancer
Patients Treated with Anti-Cancer Drugs (QOL-ACD), developed by
Kurihara et al (9) and
supported by the Japanese Ministry of Health and Welfare (Tokyo,
Japan). Specialized QOL scales for different cancer types have been
developed. In the present study, the scale developed for breast
cancer was used, known as QOL-ACD-B (10).
Briefly, QOL-ACD-B consists of 18 criteria, each of
which is evaluated on a scale from 1 to 5 (1 being the worst and 5
being the best). The 18 criteria are grouped into 4 subcategories:
‘Physical symptoms and pain’ (6 criteria), ‘Satisfaction with
treatment and coping with disease’ (4 criteria), ‘Side effects of
treatment’ (4 criteria), and ‘Dress, sexual aspect, other’ (4
criteria) (Table SI). The scores of
the entire QOL-ACD-B and each subcategory are calculated by
subtracting 1 from the average of the criteria evaluated and
multiplied by 25; thus, the minimum value is 0 and the maximum
value is 100.
QOL at the time of diagnosis and 3 months after
treatment was retrospectively evaluated. Changes in the overall QOL
and per subcategory 3 months after treatment initiation were also
calculated based on age. In addition, the association of QOL scores
with patient clinicopathological factors and effect on prognosis
were analyzed.
Statistical analysis
Statistical analyses were performed using the JMP
software package version 10 (SAS Institute, Inc.). Student's t-test
was used for the comparison of the score distributions. The
associations between variables were examined using the
χ2 test. Regarding age, the patients were categorized
into the elderly and the younger age group using the median age (65
years) as the cut-off value for stratification. The Kaplan-Meier
method was used to determine PFS rate and OS rate, and the log-rank
test was used to compare the survival curves. Hazard ratios (HRs)
and 95% confidence intervals (CIs) were calculated using the Cox
proportional-hazards model. Univariate and multivariate analyses
were performed using the Cox regression model. P<0.05 was
considered to indicate a statistically significant difference.
Results
Clinicopathological features
The clinicopathological features of 46 patients who
were diagnosed with hormone receptor-positive breast cancer with
distant metastases and treated with first-line endocrine therapy
are detailed in Table I. The median
age at treatment initiation was 65 years (range, 40–89 years), and
tumor diameter was 39.4 mm (range, 11.8–146.3 mm). The median
overall follow-up time since treatment initiation was 1,272 days
(range, 120–3,271 days).
 | Table I.Clinicopathological characteristics of
46 patients with stage IV breast cancer receiving first-line
endocrine therapy. |
Table I.
Clinicopathological characteristics of
46 patients with stage IV breast cancer receiving first-line
endocrine therapy.
| Parameters | Data |
|---|
| Age, years
(range) | 65 (40–89) |
| Tumor size, mm
(range) | 39.4
(11.8–146.3) |
| Skin infiltration, n
(%) |
|
|
Negative | 13 (28.3) |
|
Positive | 33 (71.7) |
| Lymph node
metastasis, n (%) |
|
| N0 | 7 (15.2) |
| N1 | 9 (19.6) |
| N2 | 13 (28.3) |
| N3 | 17 (37.0) |
| No. of metastatic
organs, n (%) |
|
| 1 | 23 (50.0) |
| 2 | 15 (32.6) |
| 3 | 7 (15.2) |
| 4 | 1 (2.2) |
| Site of metastasis, n
(%) |
|
| Lung | 25 (54.3) |
| Bone | 31 (67.4) |
|
Liver | 7 (15.2) |
|
Brain | 1 (2.2) |
| Skin | 1 (2.2) |
| Distant
lymph node | 13 (28.3) |
| HER2, n (%) |
|
|
Negative | 44 (95.7) |
|
Positive | 2 (4.3) |
| Ki67, n (%) |
|
|
Negative | 28 (60.9) |
|
Positive | 18 (39.1) |
| Endocrine therapy,
n (%) |
|
| LH-RH
agonist + TAM | 6 (13.0) |
|
TAM | 1 (2.2) |
|
LET | 28 (60.9) |
|
ANA | 10 (21.7) |
|
EXE | 1 (2.2) |
| Combined radiation
therapy, n (%) |
|
| No | 43 (93.5) |
|
Yes | 3 (6.5) |
| ORR 3 months after
starting treatment, n (%) |
|
|
Non-responders | 18 (39.1) |
|
Responders | 28 (60.9) |
| ORR, n (%) |
|
|
Non-responders | 12 (26.1) |
|
Responders | 34 (73.9) |
| QOL-ACD-B before
treatment (range) | 90.63
(71.88–98.44) |
| Change in QOL
(First 3 months after treatment initiation) (range) | 3.13
(−21.88–14.06) |
| QOL-ACD-B (3 months
after treatment initiation) (range) | 93.75
(62.50–98.44) |
Thirty-three patients (71.7%) had skin infiltration
and 39 patients (84.8%) were diagnosed with lymph node metastases.
Overall, 23 patients (50.0%) had distant metastasis to a single
organ, whereas the remaining 23 patients (50.0%) had distant
metastases to multiple organs. The sites of metastasis included the
lungs (25 patients; 54.3%), bones (31 patients; 67.4%), liver (7
patients; 15.2%), brain (1 patient; 2.2%), skin (1 patient; 2.2%),
and distant lymph nodes (13 patients; 28.3%). While tamoxifen in
conjunction with luteinizing hormone-releasing hormone (LH-RH)
agonist was offered to 6 patients (13.0%), single-agent treatment
was prescribed with the following drugs: Tamoxifen (1 patient;
2.2%), letrozole (28 patients; 60.9%), anastrozole (10 patients;
21.7%), and exemestane (1 patient; 2.2%). In all cases with bone
metastases, zoledronic acid or denosumab was used in combination
with endocrine therapy; 3 of these patients received the drugs in
combination with radiation therapy. Two cases (4.3%) that were
HER2-positive received no anti-HER2 therapy. None of the cases
developed cCR; however, 28 patients (60.9%) showed cPR 3 months
after treatment initiation, and by the end of the study period, a
total of 34 patients (73.9%) showed cPR. The median QOL score prior
to treatment was 90.63 (range, 71.88–98.44), and 3 months after
treatment initiation was 93.75 (range, 62.50–98.44). Overall, 13
cases of mortality were attributed to breast cancer, and no deaths
due to other causes were noted.
Differences in clinicopathological
features and QOL based on age
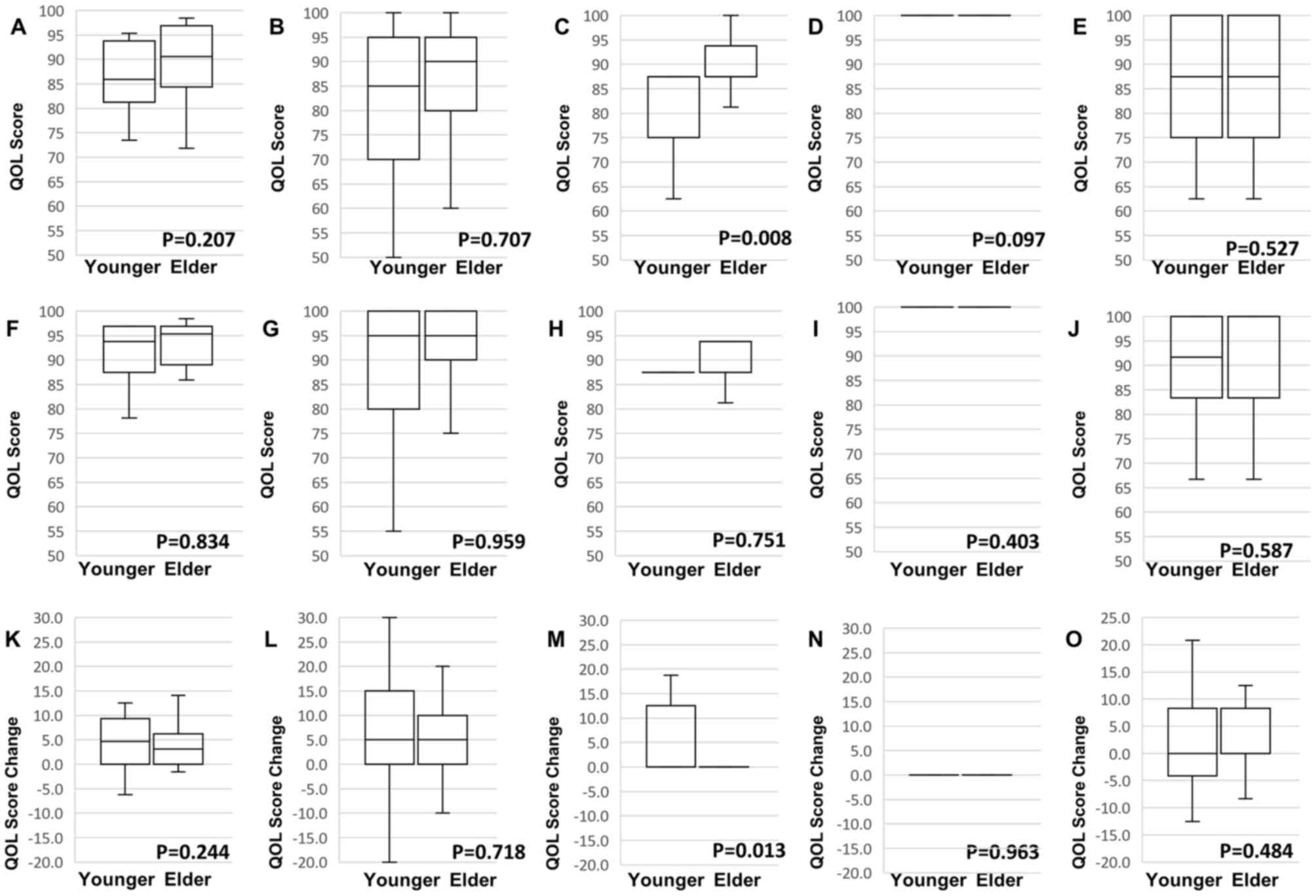
There was no significant association between age and
any of the clinicopathological features investigated (Table II). Additionally, there was no
significant difference in overall QOL prior to treatment based on
age (Fig. 1A). However, QOL score
was significantly higher among the elderly in the ‘Satisfaction
with treatment and coping with disease’ subcategory (P=0.008;
Fig. 1C). After 3 months of
treatment, no association was found between age and overall QOL or
any of the subcategories (Fig.
1F-J). However, QOL score in the ‘Satisfaction with treatment
and coping with disease’ subcategory was significantly improved by
treatment in the younger age group (P=0.013; Fig. 1M).
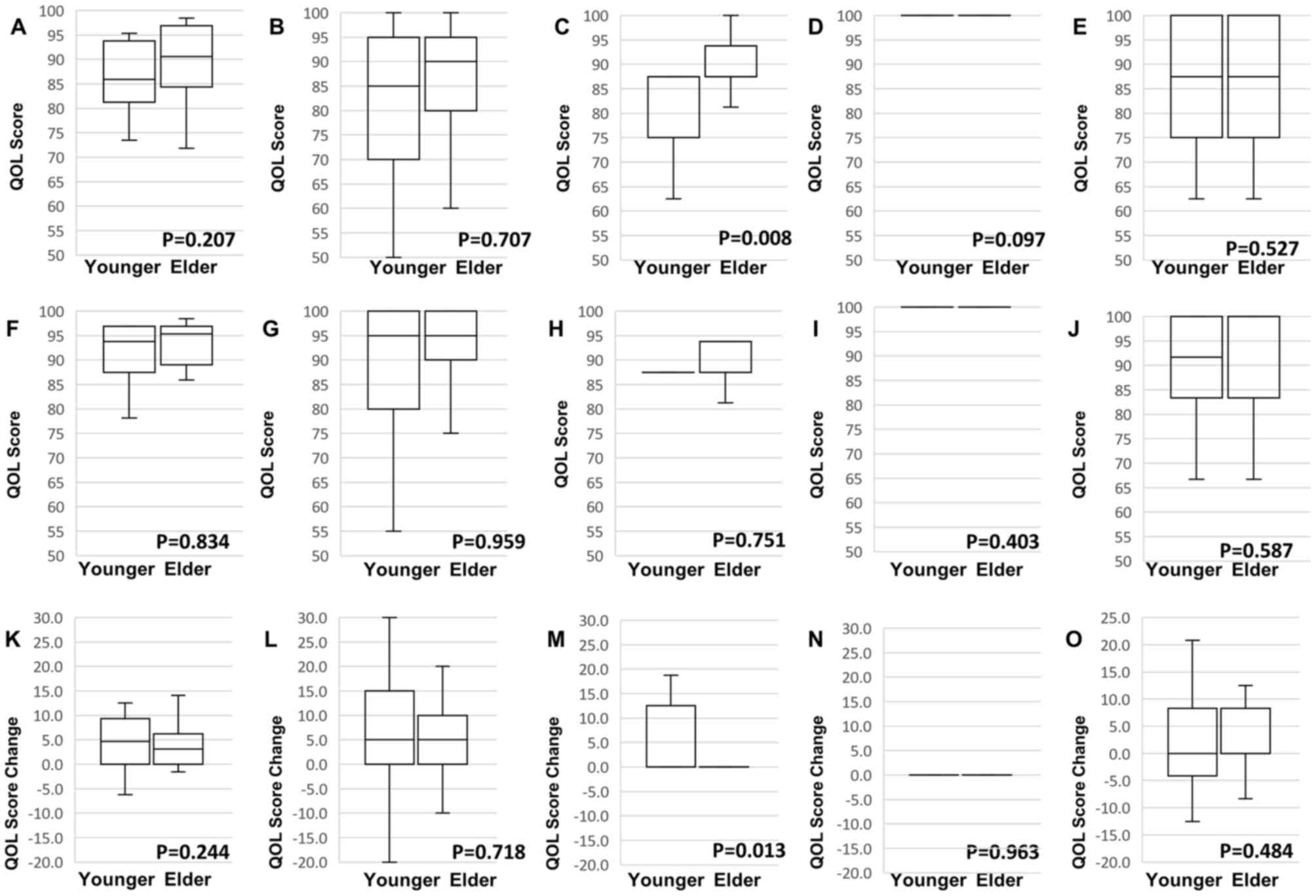 | Figure 1.Comparison of overall QOL score and
subscales before treatment between the younger and the elder
patients using box-plot diagrams: (A) Whole QOL, (B) ‘Physical
symptoms and pain’, (C) ‘Satisfaction to treatment and coping with
disease’, (D) ‘Side effects of treatment’, (E) ‘Dress, sexual
aspect, other’. Comparison of overall QOL score and subscales at 3
months after treatment initiation between the younger and the elder
using box-plot diagrams: (F) Whole QOL, (G) ‘Physical symptoms and
pain’, (H) ‘Satisfaction with treatment and coping with disease’,
(I) ‘Side effects of treatment’, (J) ‘Dress, sexual aspect, other’.
Comparison of change in overall QOL score and subscales during 3
months of treatment between the younger and the elder using
box-plot diagrams: (K) Whole QOL, (L) ‘Physical symptoms and pain’,
(M) ‘Satisfaction with treatment and coping with disease’, (N)
‘Side effects of treatment’, (O) ‘Dress, sexual aspect, other’.
QOL, quality of life. |
 | Table II.Association of clinicopathological
features with age. |
Table II.
Association of clinicopathological
features with age.
|
| Age, n (%) |
|
|---|
|
|
|
|
|---|
| Parameters | Younger (≤65 years)
(n=23) | Elder (>65
years) (n=23) | P-value |
|---|
| Tumor size, mm |
|
|
|
|
≤39.4 | 12 (52.2) | 11 (47.8) |
|
|
>39.4 | 11 (47.8) | 12 (52.2) | 0.774 |
| Skin
infiltration |
|
|
|
|
Negative | 5 (21.7) | 8 (34.8) |
|
|
Positive | 18 (78.3) | 15 (65.2) | 0.337 |
| Lymph node
metastasis |
|
|
|
|
Negative | 4 (17.4) | 3 (13.0) |
|
|
Positive | 19 (82.6) | 20 (87.0) | 0.690 |
| No. of metastatic
organs |
|
|
|
| ≤2 | 19 (82.6) | 19 (82.6) |
|
| ≥3 | 4 (17.4) | 4 (17.4) | 1.000 |
| Lung
metastasis |
|
|
|
|
Negative | 8 (34.8) | 13 (56.5) |
|
|
Positive | 15 (65.2) | 10 (43.5) | 0.145 |
| Bone
metastasis |
|
|
|
|
Negative | 10 (43.5) | 5 (21.7) |
|
|
Positive | 13 (56.5) | 18 (78.3) | 0.121 |
| Liver
metastasis |
|
|
|
|
Negative | 19 (82.6) | 20 (87.0) |
|
|
Positive | 4 (17.4) | 3 (13.0) | 0.690 |
| Distant lymph node
metastasis |
|
|
|
|
Negative | 19 (82.6) | 14 (60.9) |
|
|
Positive | 4 (17.4) | 9 (39.1) | 0.106 |
| Ki67 |
|
|
|
|
Negative | 13 (56.5) | 15 (65.2) |
|
|
Positive | 10 (43.5) | 8 (34.8) | 0.556 |
| Combined radiation
therapy |
|
|
|
| No | 20 (87.0) | 23 (100.0) |
|
|
Yes | 3 (13.0) | 0 (0.0) | 0.076 |
| ORR (3 months after
treatment initiation) |
|
|
|
|
Non-responders | 8 (34.8) | 10 (43.5) |
|
|
Responders | 15 (65.2) | 13 (56.5) | 0.556 |
| ORR |
|
|
|
|
Non-responders | 6 (26.1) | 6 (26.1) |
|
|
Responders | 17 (73.9) | 17 (73.9) | 1.000 |
Association of QOL with survival
outcomes
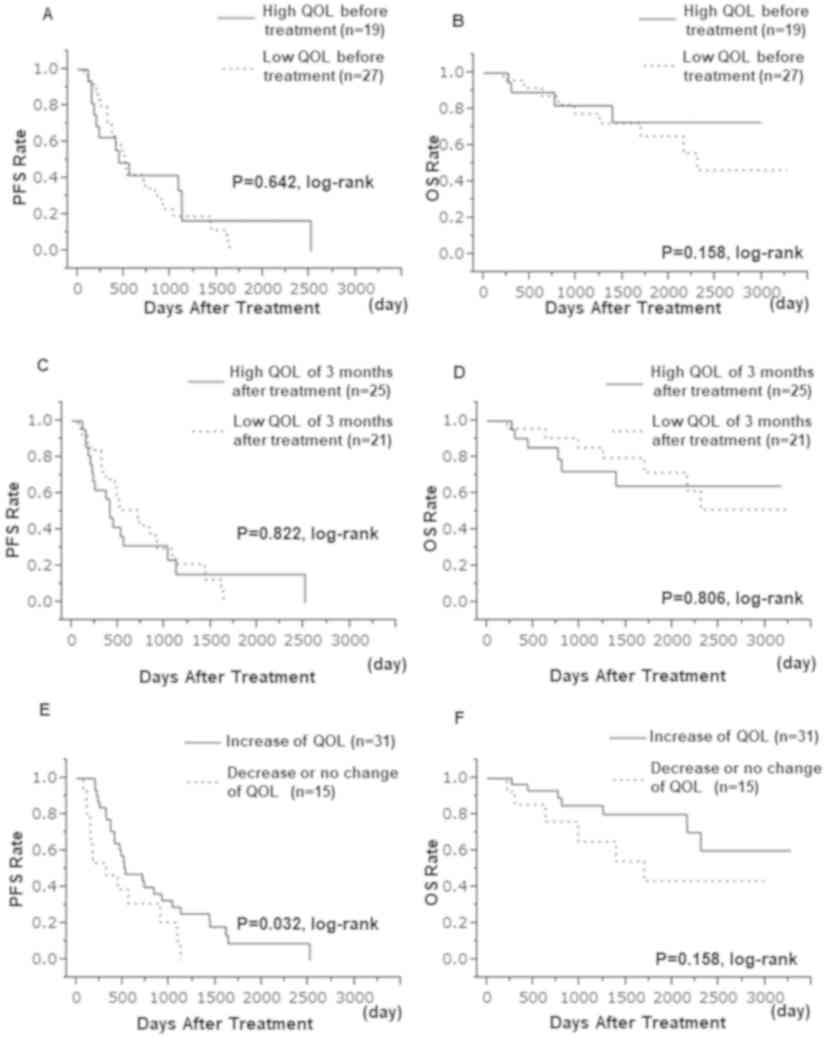
Patients were divided into high and low QOL groups,
before and at 3 months after treatment initiation; the median QOL
score at each time point was used as the cut-off value. Nineteen
patients (41.3%) had high QOL score before treatment, whereas 27
patients (58.7%) had low QOL score. The pre-treatment QOL score had
no significant impact on PFS rate (P=0.642) and OS rate (P=0.158;
Fig. 2A and B). Three months after
treatment initiation, 21 patients (45.7%) and 25 patients (54.3%)
had low and high QOL score, respectively. Again, no significant
impact of QOL was observed on PFS rate (P=0.822) and OS rate
(P=0.806; Fig. 2C and D).
The QOL score increased for 31 patients (67.4%)
during the 3 months following treatment initiation; these patients
were referred to as the ‘increased QOL group’. Conversely, the QOL
score decreased or did not change for 15 patients (32.6%); these
patients were referred to as the ‘decreased QOL group.’ Tumor size
was significantly larger and lymph node metastases were more
frequently observed in the ‘increased QOL group’ when compared with
the ‘decreased QOL group’ (P=0.004 and P=0.017, respectively).
Furthermore, in the ‘increased QOL group’ the ORR was higher 3
months after treatment initiation (P=0.007), as well as during the
treatment period (P=0.003). The ‘increased QOL group’ had a
significantly lower pre-treatment QOL-ACD-B score than the
‘decreased QOL group’ (P=0.015; Table
III).
 | Table III.Association of clinicopathological
features with change in QOL during treatment. |
Table III.
Association of clinicopathological
features with change in QOL during treatment.
|
| Change in QOL
during treatment, n (%) |
|
|---|
|
|
|
|
|---|
| Parameters | Decrease/no change
(n=15) | Increase
(n=31) | P-value |
|---|
| Age |
|
|
|
| ≤65
years | 6 (40.0) | 17 (54.8) |
|
| >65
years | 9 (60.0) | 14 (45.2) | 0.344 |
| Tumor size, mm |
|
|
|
|
≤39.4 | 12 (80.0) | 11 (35.5) |
|
|
>39.4 | 3 (20.0) | 20 (64.5) | 0.004 |
| Skin
infiltration |
|
|
|
|
Negative | 6 (40.0) | 7 (22.6) |
|
|
Positive | 9 (60.0) | 24 (77.4) | 0.228 |
| Lymph node
metastasis |
|
|
|
|
Negative | 5 (33.3) | 2 (6.5) |
|
|
Positive | 10 (66.7) | 29 (93.5) | 0.017 |
| No. of metastatic
organs |
|
|
|
| ≤2 | 12 (80.0) | 26 (83.9) |
|
| ≥3 | 3 (20.0) | 5 (16.1) | 0.752 |
| Lung
metastasis |
|
|
|
|
Negative | 8 (53.3) | 13 (41.9) |
|
|
Positive | 7 (46.7) | 18 (58.1) | 0.478 |
| Bone
metastasis |
|
|
|
|
Negative | 2 (13.3) | 13 (41.9) |
|
|
Positive | 13 (86.7) | 18 (58.1) | 0.054 |
| Liver
metastasis |
|
|
|
|
Negative | 12 (80.0) | 27 (87.1) |
|
|
Positive | 3 (20.0) | 4 (12.9) | 0.540 |
| Distant lymph node
metastasis |
|
|
|
|
Negative | 11 (73.3) | 22 (71.0) |
|
|
Positive | 4 (26.7) | 9 (29.0) | 0.871 |
| Ki67 |
|
|
|
|
Negative | 7 (46.7) | 21 (67.7) |
|
|
Positive | 8 (53.3) | 10 (32.3) | 0.177 |
| Combined radiation
therapy |
|
|
|
| No | 14 (93.3) | 29 (93.5) |
|
|
Yes | 1 (6.7) | 2 (6.5) | 0.979 |
| ORR (3 months after
treatment initiation) |
|
|
|
|
Non-responders | 10 (66.7) | 8 (25.8) |
|
|
Responders | 5 (33.3) | 23 (74.2) | 0.007 |
| ORR |
|
|
|
|
Non-responders | 8 (53.3) | 4 (12.9) |
|
|
Responders | 7 (46.7) | 27 (87.1) | 0.003 |
| QOL-ACD-B before
treatment |
|
|
|
|
Low | 5 (33.3) | 22 (71.0) |
|
|
High | 10 (66.7) | 9 (29.0) | 0.015 |
| QOL-ACD-B (3 months
after treatment initiation) |
|
|
|
|
Low | 7 (46.7) | 18 (58.1) |
|
|
High | 8 (53.3) | 13 (41.9) | 0.478 |
The ‘increased QOL group’ had a significant PFS rate
extension when compared with the ‘decreased QOL group’ (P=0.032;
Fig. 2E). However, there was no
significant difference in OS rate between the two groups (P=0.158;
Fig. 2F). In the univariate analysis
of PFS rate, the ‘increased QOL group’ was found to have a
significantly longer PFS rate (HR=0.476; 95% CI, 0.240–0.979;
P=0.044). However, this association was not found to be
statistically significant in multivariate analysis (HR=0.686; 95%
CI, 0.303–1.577; P=0.369). In univariate and multivariate analyses
of OS rate, neither QOL nor change in QOL was significantly
associated with longer OS rate (Table
IV).
 | Table IV.Univariate and multivariate analysis
of PFS rate and OS rate of 46 patients with stage IV breast cancer
under endocrine therapy. |
Table IV.
Univariate and multivariate analysis
of PFS rate and OS rate of 46 patients with stage IV breast cancer
under endocrine therapy.
|
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|---|
| Parameter | Items | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| PFS rate |
|
|
|
|
|
|
|
| Age at
treatment | ≤65/>65
years | 1.021 | 0.540–1.926 | 0.948 |
|
|
|
| Tumor
size | ≤39.4/>39.4
mm | 0.911 | 0.478–1.748 | 0.776 |
|
|
|
| Skin
infiltration |
Negative/positive | 0.618 | 0.314–1.294 | 0.194 |
|
|
|
|
HER2 |
Negative/positive | 3.335 | 0.526–11.787 | 0.169 |
|
|
|
|
Ki67 |
Negative/positive | 1.832 | 0.923–3.537 | 0.082 | 1.220 | 0.524–2.652 | 0.631 |
| Lymph
node metastasis |
Negative/positive | 0.781 | 0.347–2.088 | 0.592 |
|
|
|
| Νο. of
metastatic organs | ≤2/≥3 | 1.496 | 0.634–3.126 | 0.334 |
|
|
|
| Lung
metastasis |
Negative/positive | 0.533 | 0.277–1.024 | 0.059 | 0.523 | 0.263–1.042 | 0.065 |
| Bone
metastasis |
Negative/positive | 1.722 | 0.878–3.582 | 0.116 |
|
|
|
| Liver
metastasis |
Negative/positive | 3.624 | 1.421–8.156 | 0.009 | 2.636 | 0.882–7.552 | 0.081 |
| Distant
lymph node metastasis |
Negative/positive | 1.445 | 0.718–2.768 | 0.291 |
|
|
|
|
Combined radiation
therapy | No/yes | 1.852 | 0.295–6.400 | 0.446 |
|
|
|
|
QOL-ACD-B before
treatment | Low/high | 0.855 | 0.431–1.631 | 0.640 |
|
|
|
|
QOL-ACD-B (3 months after
treatment initiation) | Low/high | 1.077 | 0.555–2.040 | 0.823 |
|
|
|
| Change
in QOL during treatment | Decrease or no
change/increase | 0.476 | 0.240–0.979 | 0.044 | 0.686 | 0.303–1.577 | 0.369 |
|
ORR |
Non-responders/responders | 0.261 | 0.128–0.555 | 0.001 | 0.328 | 0.141–0.789 | 0.014 |
| OS rate |
|
|
|
|
|
|
|
| Age at
treatment | ≤65/>65
years | 1.027 | 0.329–3.112 | 0.962 |
|
|
|
| Tumor
size | ≤39.4/>39.4
mm | 1.133 | 0.376–3.527 | 0.822 |
|
|
|
| Skin
infiltration |
Negative/positive | 1.202 | 0.367–5.369 | 0.776 |
|
|
|
|
HER2 |
Negative/positive | – | – | 0.124 |
|
|
|
|
Ki67 |
Negative/positive | 0.832 | 0.225–2.557 | 0.757 |
|
|
|
| Lymph
node metastasis |
Negative/positive | 2.729 | 0.532–49.780 | 0.269 |
|
|
|
| No. of
metastatic organs | ≤2/≥3 | 3.206 | 0.959–9.745 | 0.058 | 3.038 | 0.747–11.841 | 0.116 |
| Lung
metastasis |
Negative/positive | 0.646 | 0.210–2.045 | 0.445 |
|
|
|
| Bone
metastasis |
Negative/positive | 1.965 | 0.621–7.440 | 0.257 |
|
|
|
| Liver
metastasis |
Negative/positive | 4.115 | 0.889–14.540 | 0.067 | 1.247 | 0.178–6.601 | 0.811 |
| Distant
lymph node metastasis |
Negative/positive | 1.239 | 0.373–3.724 | 0.711 |
|
|
|
|
Combined radiation
therapy | No/yes | 2.008 | 0.108–11.022 | 0.549 |
|
|
|
|
QOL-ACD-B before
treatment | Low/high | 0.650 | 0.176–1.997 | 0.462 |
|
|
|
|
QOL-ACD-B (3 months after
treatment initiation) | Low/high | 1.146 | 0.368–3.459 | 0.872 |
|
|
|
| Change
in QOL during treatment | Decrease or no
change/increase | 0.464 | 0.154–1.443 | 0.177 |
|
|
|
|
ORR |
Non-responders/responders | 0.257 | 0.084–0.808 | 0.022 | 0.273 | 0.071–1.079 | 0.063 |
Discussion
With the aging of society in recent years the number
of elderly patients diagnosed with breast cancer has increased. In
addition, the clinical features of breast cancer in the elderly
differ from those in younger patients. For example, some studies
have reported higher incidence of hormone-positive breast cancer,
larger tumor size, fewer cases of lymph node metastases, and more
frequent skin infiltrations in the elderly rather than the younger
patients with breast cancer (11–14). As
previously reported by our group, large tumors, lymph node
metastases, and skin infiltrations resulted in deterioration of QOL
in patients with breast cancer. In the present study, the QOL was
analyzed in patients with advanced breast cancer undergoing
hormonal therapy, and the results revealed no significant
difference, based on any clinical features, including age.
Various studies have been conducted on the changes
in the QOL during chemotherapy, with the majority reporting that
QOL decreased within a few months following treatment (15–18). In
the present study, it was shown that adverse reactions greatly
decreased QOL scores in patients undergoing preoperative
chemotherapy for breast cancer. There are also reports that the
magnitude of the side effects varies depending on age (19–21).
However, since this study included patients who underwent endocrine
therapy, only a few patients had treatment-associated side effects.
Therefore, a statistically significant improvement in QOL, due to
the treatment, could be observed in most patients.
Although some studies have reported that
chemotherapy led to mild deterioration of QOL in the elderly
patients, the results of the present study are in accordance with
numerous reports (including a meta-analysis of 10 studies) that
have shown that age was not a predictor of QOL (17,18,22–24).
However, there was a significant age-based difference in the QOL
score in the subcategory of ‘Satisfaction with treatment and coping
with disease’. Young subjects were more significantly affected by
mental stress following diagnosis; however, their recovery
thereafter was good, and they had the same QOL score as the elderly
patients at 3 months after treatment initiation. These findings are
similar to a previous study, in which little change was noted in
the emotional status of elderly patients (17).
While QOL improved for a number of patients, it
worsened for some others, and differences in clinical
characteristics between these patient groups were observed.
Patients with improved QOL had significantly larger tumor size and
higher incidence of lymph node metastases, whereas no significant
differences were observed in distant metastatic sites or the number
of metastatic organs between the two groups. Additionally, those
with improved QOL had significantly lower QOL prior to treatment
initiation. Presumably, this is because the symptoms arising from a
progressive primary breast cancer that decrease patient QOL score
are alleviated by the endocrine treatment, leading to an improved
QOL.
Similar to previous reports, the patients of the
present study with liver metastases or multiple organ metastases
did not have a significantly worse prognosis, whereas patients who
responded to endocrine therapy had a significantly better prognosis
(25–27). Additionally, this study showed that
the change in QOL during the 3 months after treatment initiation
affected PFS rate. This is important since, according to other
studies, the survival is prolonged by further improvements in QOL
as a result of treatment (15,28).
One of the limitations of the present study is the
small sample size. Therefore, the median age of the cohort was used
as the cut-off to create patient subgroups suitable for age-based
comparisons. A small cohort is likely to be affected by various
confounding factors. As shown in Table
III, changes in QOL were significantly associated with tumor
size, axillary lymph node metastasis and ORR. In particular, ORR
had strong effects on both PFS rate and OS rate. In breast cancer
with distant metastasis, it is clear that the response to treatment
and the status of distant metastasis affect prognosis, and similar
results are shown in this study. Changes in QOL score were found to
have no significant effect on PFS rate in multivariate analysis,
probably due to its association with ORR. However, ORR and QOL
changes are not completely consistent. Furthermore, the QOL score
may not be accurate, since it is a subjective evaluation. It is
obvious that the QOL during treatment is influenced by the social
position, family environment, and financial aspect. An examination
of these parameters would facilitate comparisons with patients from
other countries. Furthermore, QOL has been shown to change with
treatment and to be affected by clinical factors. In the future, it
would be important to consider factors, other than
clinicopathological variables, and perform high-quality analysis
based on them.
Taken together, psychological stress was more
prominent in young patients with hormone receptor-positive breast
cancer and distant metastases, who were treated with first-line
endocrine therapy compared with elderly patients. Moreover,
improving QOL within 3 months following treatment initiation could
lead to longer PFS rate. Breast cancer with distant metastases is
considered difficult to cure; hence the patient's QOL becomes more
important when deciding upon a treatment plan. Young patients
experience more psychological trauma during the diagnosis, and
thus, the improvement of the patient's QOL should be an important
consideration, since it may also have an impact on prognosis.
Interestingly, some studies, albeit their small sample size, have
reported that psychological support improved patient prognosis
(29–31). The present study supports the
importance of psychological care of patients, not only for the
improvement of their QOL, but also for the improvement in
prognosis.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to thank Miss Yayoi Matsukiyo
and Miss Tomomi Okawa (Data Manager, Department of Breast and
Endocrine Surgery, Osaka City University Graduate School of
Medicine) for the helpful advice regarding data management.
Funding
The study was supported by grants from the Japan
Society for the Promotion of Science (KAKENHI) (grant nos.
19K18067, 26461957 and 17K10559) to SK. The funding agency had no
role in the design, collection, analysis, interpretation of data or
writing of this manuscript.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
KoT participated in the design of the study and
drafted the manuscript. SK participated in the design of the study
and editing of the manuscript. YA, WG, TM, MS, RA and TT helped
with study data collection and manuscript preparation. KaT and ST
created T1-4 by aggregating the date, produced the figures and
participated in the design of the study. KH and MO conceived the
study, participated in the study design and coordination, and
assisted with the drafting of the manuscript. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
This study was conducted at Osaka City University
Graduate School of Medicine in Osaka, Japan, according to the
REMARK guidelines, following a retrospectively written research,
pathological evaluation, and statistical plan (10). The study protocol was approved by the
Ethics Committee of Osaka City University (approval no. 926). The
research conformed to the provisions of the Declaration of
Helsinki, 2013. All patients were informed of the investigational
nature of the study and provided written, informed consent.
Patient consent for publication
Not applicable.
Competing interest
The authors declare that they have no competing
interests.
References
|
1
|
Saracci R: The World Health Organisation
needs to reconsider its definition of health. BMJ. 314:1409–1410.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Maisey NR, Norman A, Watson M, Allen MJ,
Hill ME and Cunningham D: Baseline quality of life predicts
survival in patients with advanced colorectal cancer. Eur J Cancer.
38:1351–1357. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kaasa S, Mastekaasa A and Lund E:
Prognostic factors for patients with inoperable non-small cell lung
cancer, limited disease. The importance of patients' subjective
experience of disease and psychosocial well-being. Radiother Oncol.
15:235–242. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gotay CC, Kawamoto CT, Bottomley A and
Efficace F: The prognostic significance of patient-reported
outcomes in cancer clinical trials. J Clin Oncol. 26:1355–1363.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dancey J, Zee B, Osoba D, Whitehead M, Lu
F, Kaizer L, Latreille J and Pater JL: Quality of life scores: An
independent prognostic variable in a general population of cancer
patients receiving chemotherapy. The National Cancer Institute of
Canada Clinical Trials Group. Qual Life Res. 6:151–158. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hortobagyi GN: Treatment of breast cancer.
N Engl J Med. 339:974–984. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
McShane LM, Altman DG, Sauerbrei W, Taube
SE, Gion M and Clark GM; Statistics Subcommittee of the NCI-EORTC
Working Group on Cancer Diagnostics, : Reporting recommendations
for tumor marker prognostic studies (REMARK). J Natl Cancer Inst.
97:1180–1184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kurihara M, Shimizu H, Tsuboi K, Kobayashi
K, Murakami M, Eguchi K and Shimozuma K: Development of quality of
life questionnaire in Japan: Quality of life assessment of cancer
patients receiving chemotherapy. Psychooncology. 8:355–363. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Otsuka S, Watanabe N, Sasaki Y and
Shimojima R: Postoperative courses of breast reconstruction using
inferior adipofascial tissue repair. Breast Cancer. 22:570–577.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Crivellari D, Aapro M, Leonard R, von
Minckwitz G, Brain E, Goldhirsch A, Veronesi A and Muss H: Breast
cancer in the elderly. J Clin Oncol. 25:1882–1890. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Louwman WJ, Vulto JC, Verhoeven RH,
Nieuwenhuijzen GA, Coebergh JW and Voogd AC: Clinical epidemiology
of breast cancer in the elderly. Eur J Cancer. 43:2242–2252. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gennari R, Curigliano G, Rotmensz N,
Robertson C, Colleoni M, Zurrida S, Nolè F, de Braud F, Orlando L,
Leonardi MC, et al: Breast carcinoma in elderly women: Features of
disease presentation, choice of local and systemic treatments
compared with younger postmenopasual patients. Cancer.
101:1302–1310. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wildiers H, Kunkler I, Biganzoli L,
Fracheboud J, Vlastos G, Bernard-Marty C, Hurria A, Extermann M,
Girre V, Brain E, et al: Management of breast cancer in elderly
individuals: Recommendations of the International Society of
Geriatric Oncology. Lancet Oncol. 8:1101–1115. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shimozuma K, Sonoo H, Ichihara K and
Tanaka K: The prognostic value of quality-of-life scores:
Preliminary results of an analysis of patients with breast cancer.
Surg Today. 30:255–261. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schou I, Ekeberg O, Sandvik L, Hjermstad
MJ and Ruland CM: Multiple predictors of health-related quality of
life in early stage breast cancer. Data from a year follow-up study
compared with the general population. Qual Life Res. 14:1813–1823.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Watters JM, Yau JC, O'Rourke K, Tomiak E
and Gertler SZ: Functional status is well maintained in older women
during adjuvant chemotherapy for breast cancer. Ann Oncol.
14:1744–1750. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Akin S, Can G, Durna Z and Aydiner A: The
quality of life and self-efficacy of Turkish breast cancer patients
undergoing chemotherapy. Eur J Oncol Nurs. 12:449–456. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hurwitz N: Predisposing factors in adverse
reactions to drugs. Br Med J. 1:536–539. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cassidy J, Twelves C, Van Cutsem E, Hoff
P, Bajetta E, Boyer M, Bugat R, Burger U, Garin A, Graeven U, et
al: First-line oral capecitabine therapy in metastatic colorectal
cancer: A favorable safety profile compared with intravenous
5-fluorouracil/leucovorin. Ann Oncol. 13:566–575. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Levy M, Kewitz H, Altwein W, Hillebrand J
and Eliakim M: Hospital admissions due to adverse drug reactions: A
comparative study from Jerusalem and Berlin. Eur J Clin Pharmacol.
17:25–31. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hurria A, Hurria A, Zuckerman E, Panageas
KS, Fornier M, D'Andrea G, Dang C, Moasser M, Robson M, Seidman A,
et al: A prospective, longitudinal study of the functional status
and quality of life of older patients with breast cancer receiving
adjuvant chemotherapy. J Am Geriatr Soc. 54:1119–1124. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mols F, Vingerhoets AJ, Coebergh JW and
van de Poll-Franse LV: Quality of life among long-term breast
cancer survivors: A systematic review. Eur J Cancer. 41:2613–2619.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chee Chean D, Kuo Zang W, Lim M and
Zulkefle N: Health Related Quality of Life (HRQoL) among breast
cancer patients receiving chemotherapy in Hospital Melaka: Single
Centre Experience. Asian Pac J Cancer Prev. 17:5121–5126.
2016.PubMed/NCBI
|
|
25
|
Llombart-Cussac A, Pivot X, Biganzoli L,
Cortes-Funes H, Pritchard KI, Pierga JY, Smith I, Thomssen C, Srock
S, Sampayo M and Cortes J: A prognostic factor index for overall
survival in patients receiving first-line chemotherapy for
HER2-negative advanced breast cancer: An analysis of the ATHENA
trial. Breast. 23:656–662. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dunphy FR, Spitzer G, Fornoff JE, Yau JC,
Huan SD, Dicke KA, Buzdar AU and Hortobagyi GN: Factors predicting
long-term survival for metastatic breast cancer patients treated
with high-dose chemotherapy and bone marrow support. Cancer.
73:2157–2167. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tsuji W, Teramukai S, Ueno M, Toi M and
Inamoto T: Prognostic factors for survival after first recurrence
in breast cancer: A retrospective analysis of 252 recurrent cases
at a single institution. Breast Cancer. 21:86–95. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Coates A, Gebski V, Signorini D, Murray P,
McNeil D, Byrne M and Forbes JF: Prognostic value of
quality-of-life scores during chemotherapy for advanced breast
cancer. Australian New Zealand Breast Cancer Trials Group. J Clin
Oncol. 10:1833–1838. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Spiegel D, Bloom JR, Kraemer HC and
Gottheil E: Effect of psychosocial treatment on survival of
patients with metastatic breast cancer. Lancet. 2:888–891. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Spiegel D, Sephton SE, Terr AI and Stites
DP: Effects of psychosocial treatment in prolonging cancer survival
may be mediated by neuroimmune pathways. Ann N Y Acad Sci.
840:674–683. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kuchler T, Bestmann B, Rappat S,
Henne-Bruns D and Wood-Dauphinee S: Impact of psychotherapeutic
support for patients with gastrointestinal cancer undergoing
surgery: 10-year survival results of a randomized trial. J Clin
Oncol. 25:2702–2708. 2007. View Article : Google Scholar : PubMed/NCBI
|