Introduction
Surgery is the most commonly used treatment for the
majority of solid tumours. However, there is a growing recognition
that surgery could potentially influence tumour recurrence and
spread because of its effect on the immune system, the
microenvironment or as a direct effect on cancer cells (1). Some retrospective studies have
demonstrated that anaesthetic drugs have an impact, probably as one
of multiple factors, on tumour proliferation and metastasis
(1,2). Some studies have shown that
anaesthetics played a role in promoting cancer metastasis, whilst
others demonstrate that anaesthetics could induce apoptosis and
reduce cancer recurrence and metastasis (1,3,4). However, a comprehensive understanding
of the underlying mechanisms is still unclear.
The tumour microenvironment (TME), containing blood
vessels, stroma cells and the extracellular matrix (ECM), plays a
key role in cancer progression and metastasis (5). Fibroblasts, as one of the important
components in the TME, play a vital role in tumour progression and
metastasis (6). Fibroblasts,
considered to be indolent in ECM in normal tissues become activated
in response to wound healing, inflammation, or tissue damage caused
by cancer cells (5). After that,
stimuli including chemokines, cytokines, growth factors and
exosomes released by fibroblasts can affect the TME by mediating
immune cells, self-sustained activation and regulating cancer cells
(5,7). Stromal cell-derived factor-1 (SDF-1)
and hepatocyte growth factor (HGF) are key chemokines and cytokines
derived from fibroblasts. They are known to promote tumourigenesis,
metastasis and drug resistance (7,8). Whether
anaesthetics are involved in tumour progression through the
regulation of factors derived from fibroblasts remains to be
clearly understood.
Rocuronium bromide (RB), vecuronium bromide (VB) and
suxamethonium chloride CRS (SCC) are general intravenous
anaesthetics (9). Studies have
demonstrated that RB and SCC could enhance gastric cancer and
breast cancer cell proliferation, invasion and migration and VB has
been shown to promote the adhesiveness of gastric cancer cells
(9,10). Additionally, dexmedetomidine
hydrochloride (DH) was demonstrated to promote cancer cell
proliferation and progression (11)
whereas lidocaine, widely used as a local anaesthetic, has been
demonstrated to reduce cancer recurrence and help cancer
sensitivity to cisplatin (12,13).
In order to further explore the role of these
anaesthetics in cancer progression and gain additional insights
into their potential mechanisms, we explored whether different
anaesthetics may play a role in regulating SDF-1 and HGF derived
from fibroblasts.
Materials and methods
Cell culture
MRC-5 cells were obtained from ATCC (LGC Standards).
The cells were cultured in Dulbecco's modified Eagle's medium
(DMEM) (Sigma-Aldrich; Merck KGaA), supplemented with an antibiotic
mixture containing penicillin, streptomycin and amphotericin B
(Sigma-Aldrich; Merck KGaA) and 10% foetal calf serum (FCS)
(Sigma-Aldrich), in an incubator at 37°C, 95% humidification and 5%
CO2.
Anaesthetics
The five anaesthetics RB, VB, SCC, DH and lidocaine
are widely used in clinical practice. They were obtained from Sigma
(Sigma-Aldrich; Merck KGaA). RB, SCC and lidocaine were diluted in
phosphate-buffered saline (PBS), DH and VB were diluted in PBS
containing dimethyl sulphoxide (DMSO) (Sigma-Aldrich; Merck KGaA)
to generate stocks. Final concentrations were based on
extrapolation from anaesthetic doses used in clinical practice and
from previous cell culture experiments where available.
Subsequently, RB was diluted with DMEM to 8 µg/ml, 45 and 80 µg/ml
(10). VB was diluted with DMEM to
1.5 µg/ml, 10 and 15 µg/ml (10).
SCC was diluted with DMEM to 20 µg/ml, 100 and 200 µg/ml (10). DH was diluted with DMEM to 2.5 ng/ml,
5 and 50 ng/ml (11,14–16).
Lidocaine was diluted with DMEM to 0.1 mM, 1 and 10 Mm (12,13,17–19).
Control groups consisted of either media alone or media containing
the respective final concentration of DMSO in accordance with
treatment preparation.
Treatment of MRC-5 cells with
anaesthetics
MRC-5 cells were seeded into 6-well plates and
cultured until 70–90% confluent. Following this, MRC-5 cells were
treated with different concentrations of anaesthetics or control
solutions. Following that the 6-well plates were incubated at 37°C
for 1 h.
Total RNA isolation and RNA
quantification
Following treatment of MRC-5 with the respective
anaesthetics, RNA was extracted using TRI reagent (Sigma-Aldrich;
Merck KGaA) in accordance with the manufacturer's instructions.
Following extraction and resuspension, RNA concentration was
measured using a nanophotometer (Implen, Geneflow).
Reverse Transcription (RT)
RNA from MRC-5 cells treated with different
anaesthetics was standardised to 500 ng and used as a template for
reverse transcription to generate cDNA using a GoScript oligo (dT)
Reverse Transcription kit (Promega Corp.) in accordance with the
manufacturer's instructions. The reaction was undertaken in a
SimpliAmp Thermal Cycler (Thermo Fisher Scientific, Inc.).
Polymerase chain reaction (PCR) and
agarose gel electrophoresis
PCR was performed on sample cDNA to probe for
molecules of interest. The 16 µl reaction consisted of cDNA,
forward primer, reverse primer (Table
I), GoTaq Green Mastermix (Promega Corp.) and PCR grade water
and was conducted in a SimpliAmp Thermal Cycler (Thermo Fisher
Scientific, Inc.). Following this, DNA fragments were separated by
agarose (Melford Laboratories Ltd.) gel electrophoresis.
 | Table I.PCR and quantitative PCR primer
sequences used to detect SDF-1, HGF and GAPDH. |
Table I.
PCR and quantitative PCR primer
sequences used to detect SDF-1, HGF and GAPDH.
| Primer name | Primer sequence
(5′-3′) |
|---|
| SDF-1 F1 |
CAACGTCAAGCATCTCAAAA |
| SDF-1 R1 |
AGGTACTCCTGAATCCACTT |
| SDF-1 Zr1 |
ACTGAACCTGACCGTACAAGGTACTCCTGAATCCACTT |
| HGF F9 | TACGCTACGAAGTG |
| HGF Zr9 |
ACTGAACCTGACCGTACATCTTGCCTGATTCTGTATGA |
| GAPDH F8 |
GGCTGCTTTTAACTCTGGTA |
| GAPDH R8 |
GACTGTGGTCATGAGTCCTT |
| GAPDH F1 |
AAGGTCATCCATGACAACTT |
| GAPDH Zr1 |
ACTGAACCTGACCGTACAGCCATCCACAGTCTTCTG |
Reverse transcription-quantitative PCR
(RT-qPCR)
The Amplifilour™ Uniprimer™ Universal system
(Intergen Company) was used to quantify relative transcript copy
number as previously described (20). In brief, the reaction contained a
forward primer, reverse primer (Table
I), present at 1/10th concentration of the forward primer and
containing an additional sequence named as the Z sequence
(5′-ACTGAACCTGACCGTACA-3′), Uniprimer probe, 2X Precision FAST
mastermix (Primerdesign), cDNA and PCR water. All samples were run
alongside standards of known transcript copy numbers, allowing
generation of a standard curve and determination of relative
transcript expression within each sample.
The reaction was undertaken in a StepOne Plus qPCR
system (Thermo Fisher Scientific, Inc.). Additionally, sample
glyceraldehyde 3-phosphate dehydrogenase (GAPDH) levels were also
quantified and used to normalise transcript expression.
Statistical analysis
Statistical analysis was undertaken using a one-way
analysis of variance (ANOVA), with Holm-Sidak post hoc analysis
used to compare individual groups to the control, and the SigmaPlot
(version 11) statistical software. Every experiment was repeated at
least three times. Differences were considered statistically
significant when P<0.05. Bar charts were prepared using GraphPad
Prism (version 8) software.
Results
Effect of different anaesthetics on
SDF-1 transcript expression in MRC-5 cells
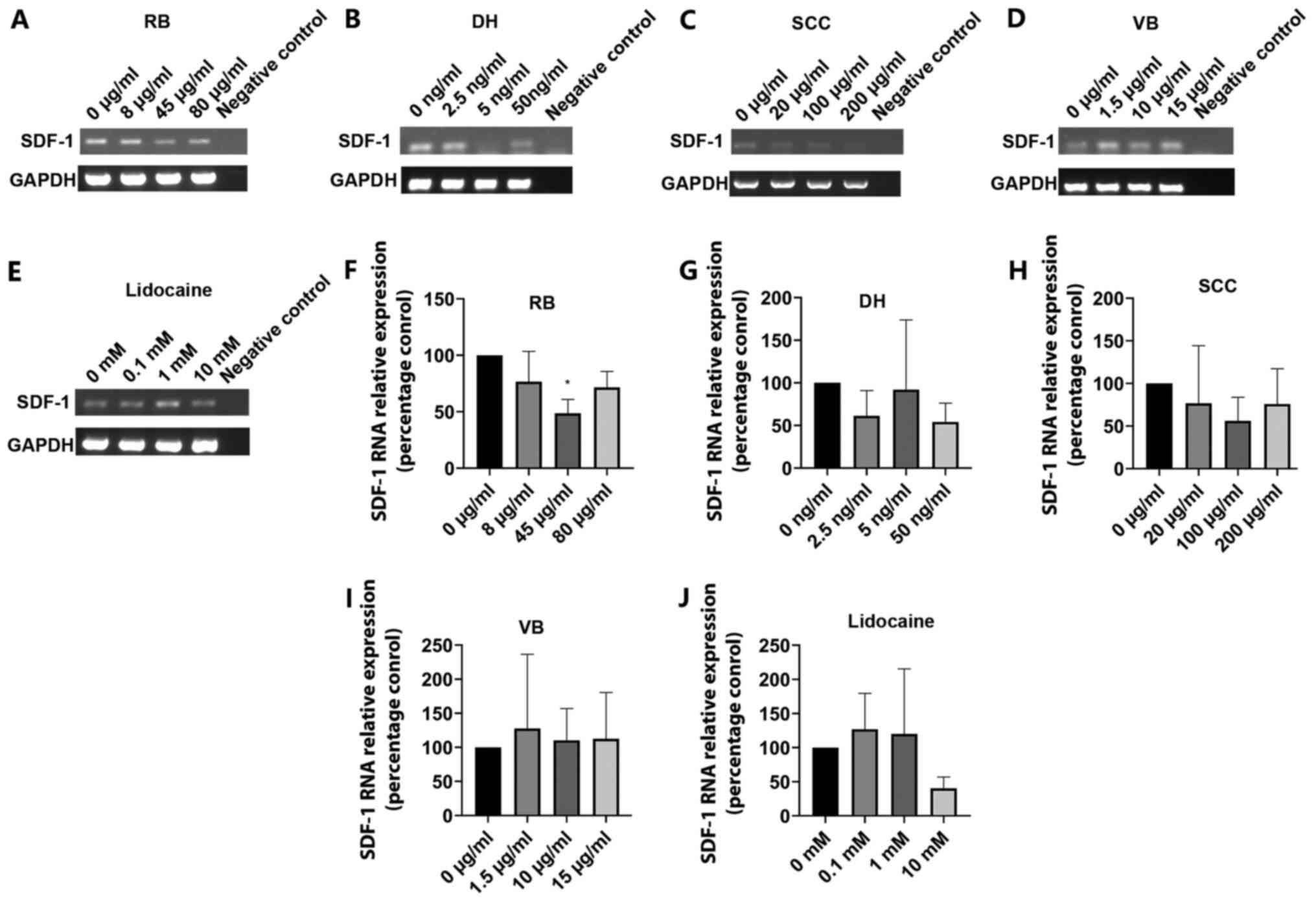
The impact of anaesthetic treatment on MRC-5
transcript expression was examined using PCR. The results showed
that the expression of SDF-1 was generally reduced with increasing
doses of RB (Fig. 1A), DH (Fig. 1B) and SCC (Fig. 1C). A slight increased SDF-1
expression was observed with increasing doses of VB (Fig. 1D). Lidocaine had little effect on
SDF-1 expression in MRC-5 cells (Fig.
1E).
 | Figure 1.Effect of anaesthetics on SDF-1
transcript expression in MRC-5 fibroblasts. SDF-1 transcript
expression was assessed using PCR following treatment with a range
of concentrations of (A) RB, (B) DH, (C) SCC, (D) VB and (E)
lidocaine. Representative images are shown. Additionally, SDF-1
transcript expression was quantified using quantitative PCR
following treatment with varying concentrations of (F) RB, (G) DH,
(H) SCC, (I) VB and (J) lidocaine. Data are presented as the mean
percentage control values +/- standard error of mean. Statistical
comparisons were performed using ANOVA. *P<0.05 vs. 0 µg/ml
control. SDF-1, stromal cell-derived factor-1; RB, rocuronium
bromide; DH, dexmedetomidine hydrochloride; SCC, suxamethonium
chloride CRS; VB, vecuronium bromide. |
SDF-1 expression was further explored using qPCR.
Expression in the treatment groups was calculated as a percentage
of the control group, which itself was taken as having a value of
100%. Similar to the PCR result, the RB treatment group showed a
reduced expression of SDF-1 following treatment and this was found
to be significant, with post hoc analysis indicating a significant
reduction in the 45 µg/ml group compared with 0 µg/ml group
(P<0.05) (Fig. 1F). Lower
expression of SDF-1 was also observed following treatment with DH,
apparent at the 2.5 and 50 ng/ml concentrations, though a large
degree of variability was observed in the 5 ng/ml group which
limited statistical significance (Fig.
1G). Similarly, SCC generally decreased SDF-1 expression over
increasing concentrations, but this was variable and did not reach
statistical significance (P>0.05; Fig. 1H). No significant difference in SDF-1
expression was noted following treatment with VB (Fig. 1I). Lidocaine had variable effects,
increasing SDF-1 expression at the 0.1 and 1 mM concentration but
brining about a large reduction at 10 mM, though ANOVA analysis
indicated no significance within the group (Fig. 1J).
Effect of different anaesthetics on
HGF expression in MRC-5 cells
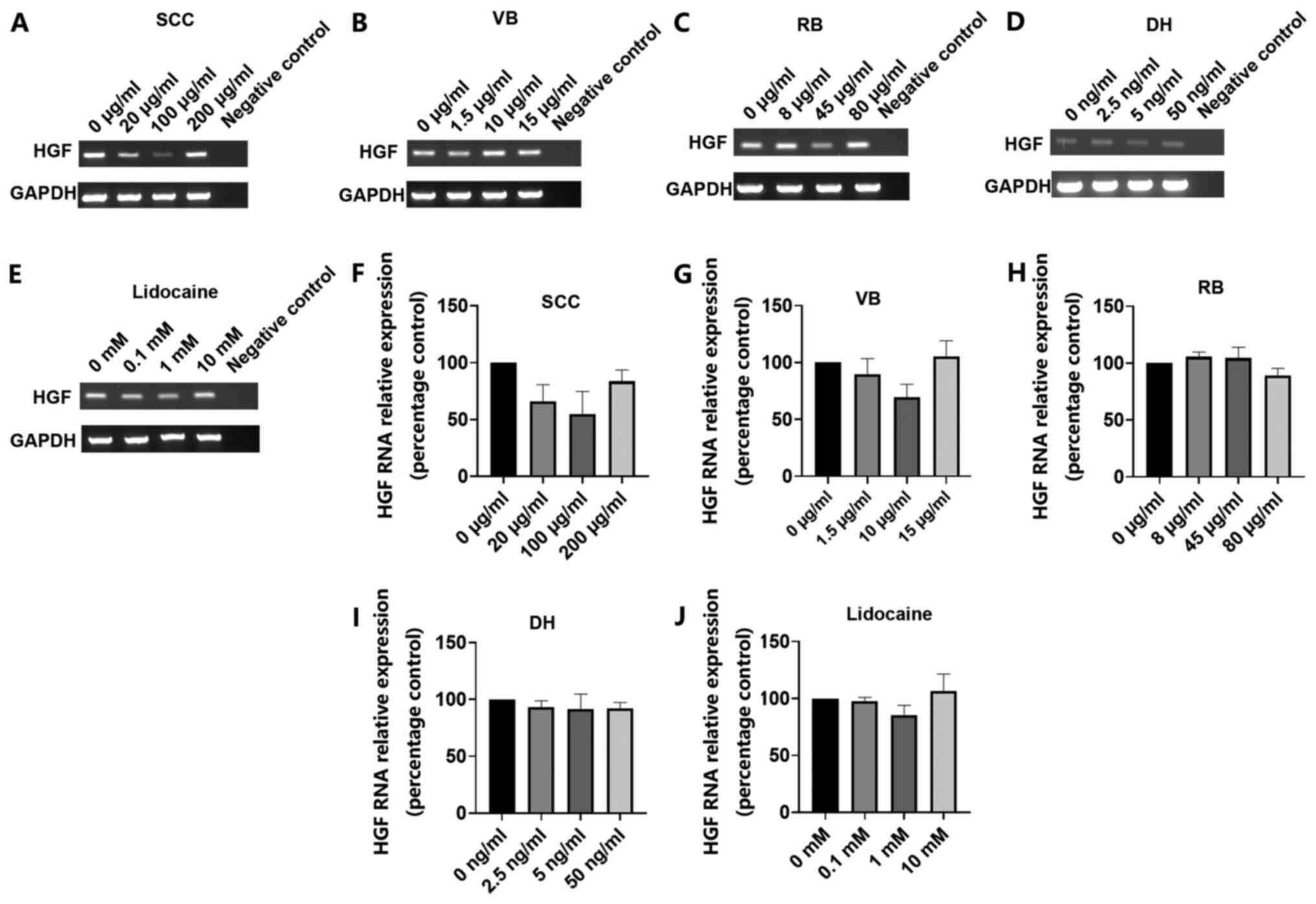
Conventional PCR analysis demonstrated reduced HGF
transcript expression at the lower 20 and 100 µg/ml concentrations
but no difference compared to the control at the 200 µg/ml
treatment concentration of SCC treatment (Fig. 2A). However, VB, RB, DH and lidocaine
treatment generally produced little or no change in HGF transcript
levels in MRC-5 cells (Fig.
2B-E).
 | Figure 2.Effect of Anaesthetics on HGF
transcript expression in MRC-5 fibroblasts. HGF transcript
expression was assessed using PCR following treatment with a range
of concentrations of (A) SCC, (B) VB, (C) RB, (D) DH and (E)
lidocaine. Representative images are shown. HGF transcript
expression was also quantified using quantitative PCR following
treatment with varying concentrations of (F) SCC, (G) VB, (H) RB,
(I) DH and (J) lidocaine. Data are presented as the mean percentage
control values +/- standard error of mean. Statistical comparison
were performed using ANOVA. HGF, hepatocyte growth factor; RB,
rocuronium bromide; DH, dexmedetomidine hydrochloride; SCC,
suxamethonium chloride CRS; VB, vecuronium bromide. |
Similarly, qPCR analysis was also used to explore
HGF transcript expression following treatment with the various
anaesthetics. Expression in the treatment groups was calculated as
a percentage of the control group, which itself was taken as having
a value of 100%. As with the PCR data, SCC treatments tended to
decrease HGF expression at 20 and 100 µg/ml but had no effect at
the higher 200 µg/ml, although no statistical significance was
observed (Fig. 2F). Interestingly, a
slight enhancement of HGF expression was noted following the 15
µg/ml treatment of VB but ANOVA analysis demonstrated no
significance within the group (Fig.
2G). No significant differences in HGF expression were
identified following RB, DH or lidocaine treatment, with little
variation in HGF expression from the controls observed following
treatment of MRC-5 cells with these anaesthetics (Fig. 2H-J).
Discussion
Anaesthetics are unavoidable for patients undergoing
major cancer surgery. In recent years increasing evidence indicates
that anaesthetics may impact patients undergoing surgery for cancer
resection, highlighting the potential effect of anaesthetics on
cancers (21–23). Some research has shown that
anaesthetic drugs contribute to tumour proliferation and
metastasis, whilst others have demonstrated the reverse response
(1,3,10,17). The
mechanisms by which anaesthetics influence tumour growth and
dissemination remain poorly understood. Our study examined five
different widely used anaesthetics and how they may impact the
production of cancer promoting factors from stromal cells.
In order to explore our hypothesis, we focused on
five intravenous and local anaesthetics, namely RB, VB, SCC, DH and
lidocaine. RB, VB and SCC are anaesthetics which act by blocking
nerve impulses to muscles. Previous research has demonstrated that
RB can enhance gastric cancer growth, invasion and migration and
promote MDA-MB-231 breast cancer cell proliferation, migration and
invasion (9,10). Similarly, SCC has also been found to
promote MDA-MB-231 proliferation, migration and invasion (10). VB has been noted to influence the
malignant phenotype of cancer cells at a common concentration,
whilst it has been observed to have an impact at a higher dose in
gastric cancer but had very little impact on MDA-MB-231 breast
cancer cells (9,10). DH is a highly selective α2-adrenergic
receptor agonist (1). α2-adrenergic
receptors have been shown to be expressed by human breast cancer
cells (24) and DH has been shown to
promote tumour growth and metastasis in murine mammary tumours
(25). It was also demonstrated to
increase cell proliferation, migration and survival by activating
α2-adrenoceptors in lung carcinoma (16). Lidocaine acts by blocking
voltage-gated sodium channels (VGSC) on the nerve cell membrane.
Several studies have demonstrated that lidocaine can inhibit
growth, invasion, metastasis and promote apoptosis in lung
adenocarcinoma cells, breast cancer and hepatocellular cancer cells
(19,26,27).
Until now, a number of mechanisms have been
implicated in relation to how other anaesthetic drugs can impact on
the tumour process. For instance, it has been demonstrated that
propofol can inhibit the migratory capacity of cervical cancer
cells by altering their morphology by regulating cytoskeletal
structural stability and affecting the membrane ultrastructure
(28). Additionally, it has also
been indicated to induce apoptosis and inhibit growth and migration
by influencing a number of different pathways. In colorectal cancer
cells propofol was shown to influence the phosphatidylinositol
3-kinase (PI3K)/protein kinase B (AKT) pathway and in pancreatic
cancer cells it was found to regulate miR-21/Slug signals, where
Slug has been implicated as a zinc finger transcriptional repressor
known to promote cancer cell invasion and survival (29). Morphine has been shown to prompt
breast cancer cell migration by inducing overexpression of
neuroepithelial cell transforming 1 (NET1) which is important in
cell migration (30). Local
anaesthetics such as lidocaine and ropivacaine have been suggested
to induce non-small cell lung cancer (NSCLC) cell apoptosis, to be
involved in apoptotic pathways and mitogen activated protein kinase
(MAPK) pathways and to inhibit cell growth by arresting cell cycles
at G0/1 phase through downregulating cyclin D1 which plays a vital
role in G1 to S phase progression (17).
It appears that anaesthetics can influence cancer
activity, not only via cancer cells directly but also via an
indirect impact. It is known that surgical tumour resection can
sometimes induce tumour recurrence and metastasis. One of the
reasons is that surgery can inhibit the immune system and also
affects the inflammatory system (1).
Propofol has been proven to protect the immune system from being
suppressed (31,32). Hence, this may represent one method
through which propofol could inhibit cancer growth and migration.
Cell experiments and retrospective studies have suggested that DH
engages in promoting tumour activity and is associated with reduced
inflammatory cytokine release and regulation of the immune system
(33). For example, DH could promote
tumour metastasis and angiogenesis by expanding monocytic
myeloid-derived suppressor cells (MDSC), and monocytic MDSC have
the capacity to inhibit T cell proliferation and produce the
proangiogenic factor vascular endothelial growth factor (VEGF)
(11). Thereby, cancer progression
is influenced not only by tumour cells themselves but also the
contributions of components in the TME. Taken together, a full
understanding of the mechanism of anaesthetics in cancer is crucial
for selecting an effective treatment.
The TME is key in influencing the development and
dissemination of cancer. It consists of the ECM, cytokines and
stromal cells including fibroblasts, endothelial cells and immune
cells (34). Fibroblasts, as the key
members of the stroma, play a crucial role in tumour-stroma
interaction (7). Cancer associated
fibroblasts (CAF) can release a number of growth factors,
cytokines, chemokines and other stimuli, most of which promote
tumour progression, though some inhibit tumour function (35,36).
SDF-1 known as chemokine (C-X-C motif) ligand 12 (CXCL12) is a
chemokine secreted by fibroblasts and engages in tumourigenesis and
metastatic activity in different types of cancers, such as breast
cancer (37), colorectal cancer
(38) and lung cancer (39). The chemokine (C-X-C motif) receptor 4
(CXCR4), a SDF-1 receptor, has been found to be overexpressed in
over 30 types of tumours (8). Its
role in promoting tumour growth, migration and angiogenesis is
achieved via the CXCL12/CXCR4 axis (8). HGF, released by tumour and fibroblasts,
is a key cytokine that binds its receptor c-MET on different tumour
cells. It modulates tumour processes such as proliferation,
motility, angiogenesis, invasion and metastasis through the
HGF/c-MET signalling pathway (40).
Both are key factors derived from fibroblasts and contribute to
tumour progression in the TME. In the current study we explored how
the expression of these key factors in fibroblasts could be
influenced after treatment with anaesthetic drugs.
Previous in vitro studies showed that RB
promoted breast cancer and gastric cancer cell proliferation,
migration and invasion (9,10). SCC also increased the breast cancer
cells' malignant phenotype but this was not seen in gastric cancer
(10). VB had little impact on
gastric and breast cancer cells activity (9,10). In
vitro experiments have suggested that DH contributed to cell
proliferation and metastasis. Similar results were reported in
vivo, which showed that DH also participated in the promotion
of tumour growth (41,42). Several studies proved that lidocaine
could inhibit tumour cell proliferation, invasion and migration
(19,26,27). In
our research, we explored the effect of RB, VB, SCC, DH and
lidocaine on the production of SDF-1 and HGF in MRC-5 cells. SDF-1
was significantly reduced by RB treatment at a concentration of 45
µg/ml. The DH treatment group also showed lower SDF-1 transcript
levels at concentrations of 2.5 and 50 ng/ml, although there was a
large degree of variability in the 5 ng/ml DH treatment group. SCC
treatment resulted in a similar trend to RB treatment, although it
did not reach statistical significance. SCC and VB treatment appear
to have similar trends on HGF expression. It seemed that HGF
transcript expression was reduced at the lower 20 and 100 µg/ml
concentrations of SCC treatment but little impact on expression was
seen at the 200 µg/ml SCC concentration compared to the control
group. VB treatment also appeared to decrease HGF expression at 1.5
and 10 µg/ml concentrations but no effect at the higher 15 µg/ml
concentration. Our study showed that lidocaine resulted in a large
reduction of SDF-1 expression at 10 mM concentration but had little
impact at the other concentrations and no impact on HGF expression
in MRC-5 fibroblast cells. Previous studies proved that RB, SCC and
DH act in a promotive role for tumour growth, invasion and
migration and lidocaine is an inhibitor of tumour progression.
However, our current work demonstrates that some anaesthetics may
inhibit SDF-1 and HGF expression to some extent in MRC-5 and hence
could subsequently impact tumour proliferation, migration and
angiogenesis in response to such factors. Previous studies explored
the impact of the anaesthetics directly on cancer cells, whereas
here our work has focused on the implications on the stromal
components. It is likely that both aspects are key in the overall
response of the tumour to such anaesthetics. Multiple factors
should be taken into consideration when exploring the impact of
anaesthetics on the tumour process. Therefore, additional complex,
co-culture and in vivo assessment is needed to further
understand the full significance.
There are, however, limitations to our research.
Firstly, we used only one type of fibroblast cell, MRC-5, which may
not be representative of all fibroblasts in vivo. Secondly,
the impact of the various anaesthetics on the expression of SDF-1
and HGF were investigated at the transcript level in this initial
study. Whilst this raises an important relationship of significant
importance, both HGF and SDF-1 are secreted proteins. Therefore,
the findings reported in this manuscript represent preliminary
data. It is now of fundamental importance to further examine this
relationship at the protein level and, importantly, in the context
of the impact on secretion and bioactivity of such factors in the
microenvironment, to validate these initial findings. This warrants
further biochemical investigation to fully establish the impact of
anaesthetics on fibroblast-cancer cell signalling. Thirdly, our
model lacks a combination of tumour cells and TME to more fully
inform the study. Additional research is required to investigate
the impact of conditioned fibroblast derived medium, following
anaesthetic exposure, on cancer cells. Furthermore, the current
study investigated only one chemokine and one cytokine which makes
it harder to represent the TME completely. Ultimately, animal
studies and prospective randomized controlled trials will be
required. It will be important not only to study individual drug
effects on cancer growth and progression markers, but also to look
at drug combinations, dosing schedules and exposure times in order
to elucidate the optimum anaesthetic regimens for patients
undergoing major cancer surgery in the future.
In conclusion, this study has shown that some
anaesthetic drugs have the capacity to inhibit SDF-1 and HGF
expression to some extent in MRC-5 fibroblasts. This alone may not
result in inhibition of tumour proliferation and metastasis but
does provide insights into the impact of anaesthetics on
fibroblasts derived factors which may provide a new direction for
improving cancer treatment. However, in vitro research
cannot truly reflect the complex interaction between drugs and
multiple cell types in vivo. Further studies are required to
confirm the exact role of different anaesthetic agents in promoting
or suppressing cancer cell proliferation and dissemination. This
may open up a novel way in which cancer surgery could be optimised
in future to reduce the likelihood of recurrence and
metastasis.
Acknowledgements
Not applicable.
Funding
Cardiff University China Medical Scholarship, the
Outstanding Young Scholarship from Yantai Yuhuangding Hospital
(grant no. YDH050719).
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WGJ, PS and AJ were involved in the study concept
and study design. WG, AJS and TAM participated in data acquisition,
quality control of data and data analysis. WG, RH, AJS, TAM and WGJ
were involved in data interpretation, preparation, editing and
critical review of the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yang W, Cai J, Zabkiewicz C, Zhang H, Ruge
F and Jiang WG: The effects of anesthetics on recurrence and
metastasis of cancer, and clinical implications. World J Oncol.
8:63–70. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tavare AN, Perry NJ, Benzonana LL, Takata
M and Ma D: Cancer recurrence after surgery: Direct and indirect
effects of anesthetic agents. Int J Cancer. 130:1237–1250. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Le-Wendling L, Nin O and Capdevila X:
Cancer recurrence and regional anesthesia: The theories, the data,
and the future in outcomes. Pain Med. 17:756–775. 2016.PubMed/NCBI
|
|
4
|
Tazawa K, Koutsogiannaki S, Chamberlain M
and Yuki K: The effect of different anesthetics on tumor
cytotoxicity by natural killer cells. Toxicol Lett. 266:23–31.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kalluri R: The biology and function of
fibroblasts in cancer. Nat Rev Cancer. 16:582–598. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ohlund D, Elyada E and Tuveson D:
Fibroblast heterogeneity in the cancer wound. J Exp Med.
211:1503–1523. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huang TX, Guan XY and Fu L: Therapeutic
targeting of the crosstalk between cancer-associated fibroblasts
and cancer stem cells. Am J Cancer Res. 9:1889–1904.
2019.PubMed/NCBI
|
|
8
|
Ahirwar DK, Nasser MW, Ouseph MM, Elbaz M,
Cuitiño MC, Kladney RD, Varikuti S, Kaul K, Satoskar AR, Ramaswamy
B, et al: Fibroblast-derived CXCL12 promotes breast cancer
metastasis by facilitating tumor cell intravasation. Oncogene.
37:4428–4442. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jiang A, Zhao H, Liu X, Yu M, Chen J and
Jiang WG: Comparison of different muscle-relaxant anesthetics on
growth, migration and invasion of gastric cancer cells. Anticancer
Res. 37:4371–4378. 2017.PubMed/NCBI
|
|
10
|
Jiang A, Zhao H, Cai J and Jiang WG:
Possible effect of muscle-relaxant anaesthetics on invasion,
adhesion and migration of breast cancer cells. Anticancer Res.
36:1259–1265. 2016.PubMed/NCBI
|
|
11
|
Su X, Fan Y, Yang L, Huang J, Qiao F, Fang
Y and Wang J: Dexmedetomidine expands monocytic myeloid-derived
suppressor cells and promotes tumour metastasis after lung cancer
surgery. J Transl Med. 16:3472018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sun H and Sun Y: Lidocaine inhibits
proliferation and metastasis of lung cancer cell via regulation of
miR-539/EGFR axis. Artif Cells Nanomed Biotechnol. 47:2866–2874.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang L, Hu R, Cheng Y, Wu X, Xi S, Sun Y
and Jiang H: Lidocaine inhibits the proliferation of lung cancer by
regulating the expression of GOLT1A. Cell Prolif. 50:e123642017.
View Article : Google Scholar
|
|
14
|
Deng F, Ouyang M, Wang X, Yao X, Chen Y,
Tao T, Sun X, Xu L, Tang J and Zhao L: Differential role of
intravenous anesthetics in colorectal cancer progression:
Implications for clinical application. Oncotarget. 7:77087–77095.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bao F, Kang X, Xie Q and Wu J: HIF-α/PKM2
and PI3K-AKT pathways involved in the protection by dexmedetomidine
against isoflurane or bupivacaine-induced apoptosis in hippocampal
neuronal HT22 cells. Exp Ther Med. 17:63–70. 2019.PubMed/NCBI
|
|
16
|
Wang C, Datoo T, Zhao H, Wu L, Date A,
Jiang C, Sanders RD, Wang G, Bevan C and Ma D: Midazolam and
dexmedetomidine affect neuroglioma and lung carcinoma cell biology
in vitro and in vivo. Anesthesiology. 129:1000–1014. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang HW, Wang LY, Jiang L, Tian SM, Zhong
TD and Fang XM: Amide-linked local anesthetics induce apoptosis in
human non-small cell lung cancer. J Thorac Dis. 8:2748–2757. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Piegeler T, Schlapfer M, Dull RO, Schwartz
DE, Borgeat A, Minshall RD and Beck-Schimmer B: Clinically relevant
concentrations of lidocaine and ropivacaine inhibit TNFα-induced
invasion of lung adenocarcinoma cells in vitro by blocking the
activation of Akt and focal adhesion kinase. Br J Anaesth.
115:784–791. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xing W, Chen DT, Pan JH, Chen YH, Yan Y,
Li Q, Xue RF, Yuan YF and Zeng WA: Lidocaine induces apoptosis and
suppresses tumor growth in human hepatocellular carcinoma cells in
vitro and in a xenograft model in vivo. Anesthesiology.
126:868–881. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Owen S, Ye L, Sanders AJ, Mason MD and
Jiang WG: Expression profile of receptor activator of nuclear-κB
(RANK), RANK ligand (RANKL) and osteoprotegerin (OPG) in breast
cancer. Anticancer Res. 33:199–206. 2013.PubMed/NCBI
|
|
21
|
Hooijmans CR, Geessink FJ,
Ritskes-Hoitinga M and Scheffer GJ: A systematic review of the
modifying effect of anaesthetic drugs on metastasis in animal
models for cancer. PLoS One. 11:e01561522016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Niwa H, Rowbotham DJ, Lambert DG and Buggy
DJ: Can anesthetic techniques or drugs affect cancer recurrence in
patients undergoing cancer surgery? J Anesth. 27:731–741. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kim R: Anesthetic technique and cancer
recurrence in oncologic surgery: Unraveling the puzzle. Cancer
Metastasis Rev. 36:159–177. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vazquez SM, Mladovan AG, Perez C, Bruzzone
A, Baldi A and Luthy IA: Human breast cell lines exhibit functional
alpha2-adrenoceptors. Cancer Chemother Pharmacol. 58:50–61. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Szpunar MJ, Burke KA, Dawes RP, Brown EB
and Madden KS: The antidepressant desipramine and α2-adrenergic
receptor activation promote breast tumor progression in association
with altered collagen structure. Cancer Prev Res (Phila).
6:1262–1272. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Piegeler T, Votta-Velis EG, Liu G, Place
AT, Schwartz DE, Beck-Schimmer B, Minshall RD and Borgeat A:
Antimetastatic potential of amide-linked local anesthetics:
Inhibition of lung adenocarcinoma cell migration and inflammatory
Src signaling independent of sodium channel blockade.
Anesthesiology. 117:548–559. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lirk P, Berger R, Hollmann MW and Fiegl H:
Lidocaine time- and dose-dependently demethylates deoxyribonucleic
acid in breast cancer cell lines in vitro. Br J Anaesth.
109:200–207. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang F, Wang C, Cui Y, Li S, Yao Y, Ci Y,
Wang J, Hou W, Wu A and Li E: Effects of propofol on several
membrane characteristics of cervical cancer cell lines. Cell
Physiol Biochem. 40:172–182. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu Z, Zhang J, Hong G, Quan J, Zhang L
and Yu M: Propofol inhibits growth and invasion of pancreatic
cancer cells through regulation of the miR-21/Slug signaling
pathway. Am J Transl Res. 8:4120–4133. 2016.PubMed/NCBI
|
|
30
|
Ecimovic P, Murray D, Doran P, McDonald J,
Lambert DG and Buggy DJ: Direct effect of morphine on breast cancer
cell function in vitro: Role of the NET1 gene. Br J Anaesth.
107:916–923. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen Y, Liang M, Zhu Y and Zhou D: The
effect of propofol and sevoflurane on the perioperative immunity in
patients under laparoscopic radical resection of colorectal cancer.
Zhonghua Yi Xue Za Zhi. 95:3440–3444. 2015.(In Chinese). PubMed/NCBI
|
|
32
|
Jaura AI, Flood G, Gallagher HC and Buggy
DJ: Differential effects of serum from patients administered
distinct anaesthetic techniques on apoptosis in breast cancer cells
in vitro: A pilot study. Br J Anaesth. 113 (Suppl 1):i63–i67. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tsuchiya Y, Sawada S, Yoshioka I, Ohashi
Y, Matsuo M, Harimaya Y, Tsukada K and Saiki I: Increased surgical
stress promotes tumor metastasis. Surgery. 133:547–555. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bissell MJ and Radisky D: Putting tumours
in context. Nat Rev Cancer. 1:46–54. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chen X and Song E: Turning foes to
friends: Targeting cancer-associated fibroblasts. Nat Rev Drug
Discov. 18:99–115. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
LeBleu VS and Kalluri R: A peek into
cancer-associated fibroblasts: Origins, functions and translational
impact. Dis Model Mech. 11:dmm0294472018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Huang M, Li Y, Zhang H and Nan F: Breast
cancer stromal fibroblasts promote the generation of
CD44+CD24− cells through SDF-1/CXCR4
interaction. J Exp Clin Cancer Res. 29:802010. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Todaro M, Gaggianesi M, Catalano V,
Benfante A, Iovino F, Biffoni M, Apuzzo T, Sperduti I, Volpe S,
Cocorullo G, et al: CD44v6 is a marker of constitutive and
reprogrammed cancer stem cells driving colon cancer metastasis.
Cell Stem Cell. 14:342–356. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Li H, Chen Y, Xu N, Yu M, Tu X, Chen Z,
Lin M, Xie B, Fu J and Han L: AMD3100 inhibits brain-specific
metastasis in lung cancer via suppressing the SDF-1/CXCR4 axis and
protecting blood-brain barrier. Am J Transl Res. 9:5259–5274.
2017.PubMed/NCBI
|
|
40
|
Noriega-Guerra H and Freitas VM:
Extracellular matrix influencing HGF/c-MET signaling pathway:
Impact on cancer progression. Int J Mol Sci. 19:33002018.
View Article : Google Scholar
|
|
41
|
Bruzzone A, Piñero CP, Rojas P, Romanato
M, Gass H, Lanari C and Lüthy IA: α(2)-Adrenoceptors enhance cell
proliferation and mammary tumor growth acting through both the
stroma and the tumor cells. Curr Cancer Drug Targets. 11:763–774.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bruzzone A, Piñero CP, Castillo LF,
Sarappa MG, Rojas P, Lanari C and Lüthy IA: Alpha2-adrenoceptor
action on cell proliferation and mammary tumour growth in mice. Br
J Pharmacol. 155:494–504. 2008. View Article : Google Scholar : PubMed/NCBI
|