|
1
|
International Agency for Research on
Cancer (IARC): GLOBOCAN 2012, . Estimated Cancer Incidence.
Mortality and Prevalence Worldwide. 2013.
|
|
2
|
Malvezzi M, Carioli G, Bertuccio P,
Boffetta P, Levi F, La Vecchia C and Negri E: European cancer
mortality predictions for the year 2017, with focus on lung cancer.
Ann Oncol. 28:1117–1123. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jemal A, Ward EM, Johnson CJ, Cronin KA,
Ma J, Ryerson B, Mariotto A, Lake AJ, Wilson R, Sherman RL, et al:
Annual report to the nation on the status of cancer, 1975–2014,
featuring survival. J Natl Cancer Inst. 109:djx0302017. View Article : Google Scholar
|
|
4
|
Herbst RS, Morgensztern D and Boshoff C:
The biology and management of non-small cell lung cancer. Nature.
553:446–454. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Morgensztern D, Ng SH, Gao F and Govindan
R: Trends in stage distribution for patients with non-small cell
lung cancer: A National cancer database survey. J Thorac Oncol.
5:29–33. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2019. CA Cancer J Clin. 69:7–34. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jemal A, Miller KD, Ma J, Siegel RL,
Fedewa SA, Farhad I, Devesa SS and Thun MJ: Higher lung cancer
incidence in young women than young men in the United States. N
Engl J Med. 378:1999–2009. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ragavan MV and Patel MI: Understanding sex
disparities in lung cancer incidence: Ar women more at risk? Lung
Cancer Manag. 9:LMY342020. View Article : Google Scholar
|
|
9
|
Yuan Y, Liu L, Chen H, Wang Y, Xu Y, Mao
H, Li J, Mills GB, Shu Y, Li L and Liang H: Comprehensive
characterization of molecular differences in cancer between male
and female patients. Cancer Cell. 29:711–722. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
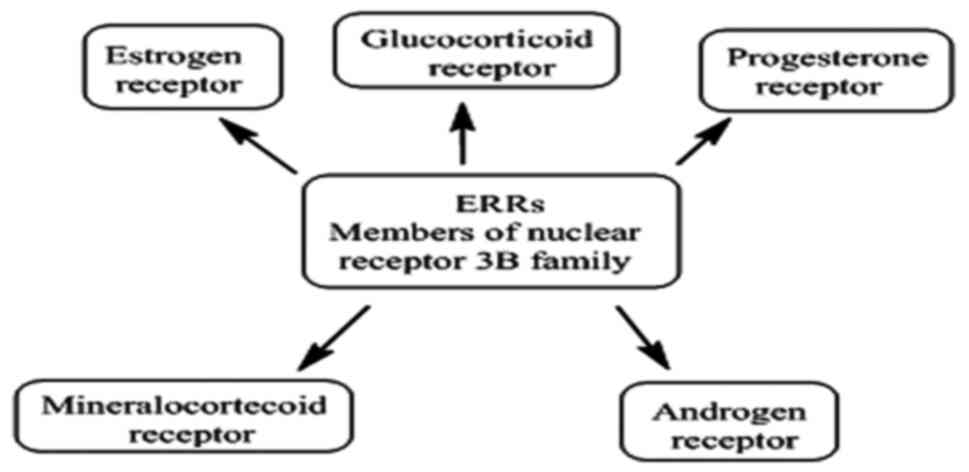
|
Xia B, Feldman R, Cozen W, Kang I, Raez
LE, Borghaei H, Kim C, Nagasaka M, Mamdani H, Vanderwalde AM, et
al: Sex disparities in hormone positive lung cancer. J Clin Oncol.
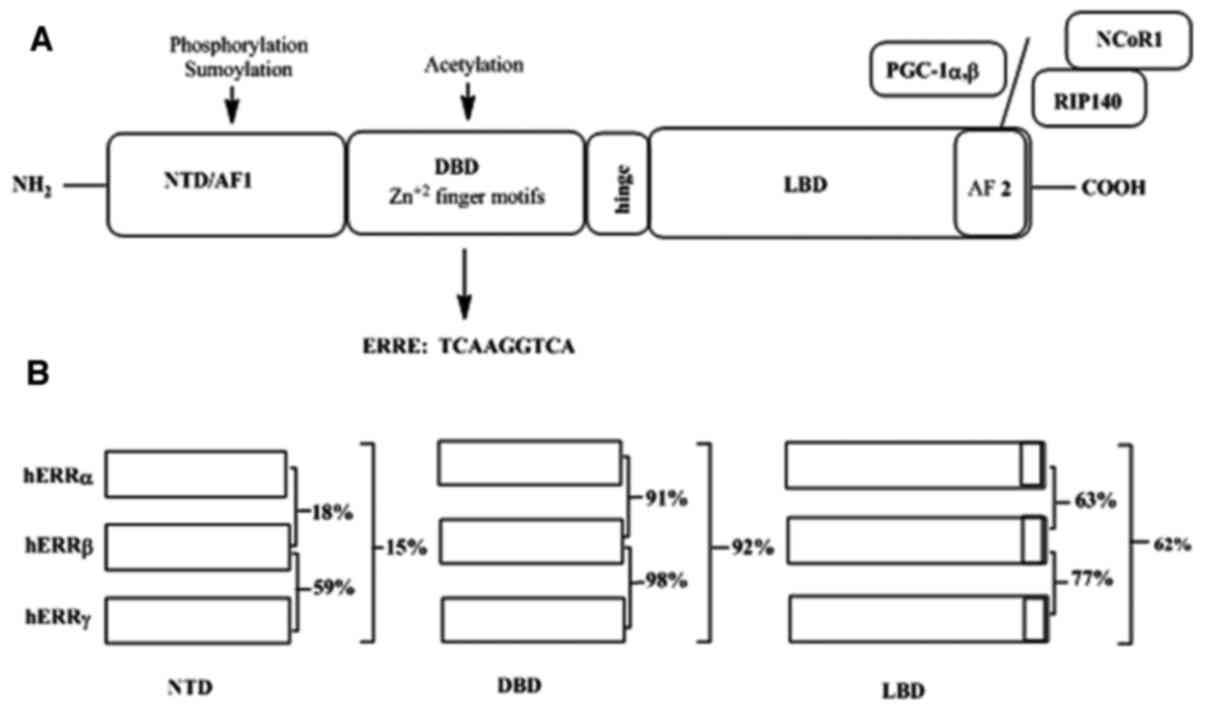
38 (15_suppl):e215522020. View Article : Google Scholar
|
|
11
|
Fidler-Benaoudia MM, Torre LA, Bray F,
Ferlay J and Jemal A: Lung cancer incidence in young women vs.
young men: A systematic analysis in 40 countries. Int J Cancer.
147:811–819. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Skov BG, Fischer BM and Pappot H:
Oestrogen receptor beta over expression in males with non-small
cell lung cancer is associated with better survival. Lung Cancer.
59:88–94. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Greiser CM, Greiser EM and Dören M:
Menopausal hormone therapy and risk of lung cancer: Systematic
review and meta-analysis. Maturitas. 65:198–204. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Adami HO, Persson I, Hoover R, Schairer C
and Bergkvist L: Risk of cancer in women receiving hormone
replacement therapy. Int J Cancer. 44:833–839. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Risch HA, Howe GR, Jain M, Burch JD,
Holowaty EJ and Miller AB: Are female smokers at higher risk for
lung cancer than male smokers? A case-control analysis by
histologic type. Am J Epidemiol. 138:281–293. 1993. View Article : Google Scholar : PubMed/NCBI
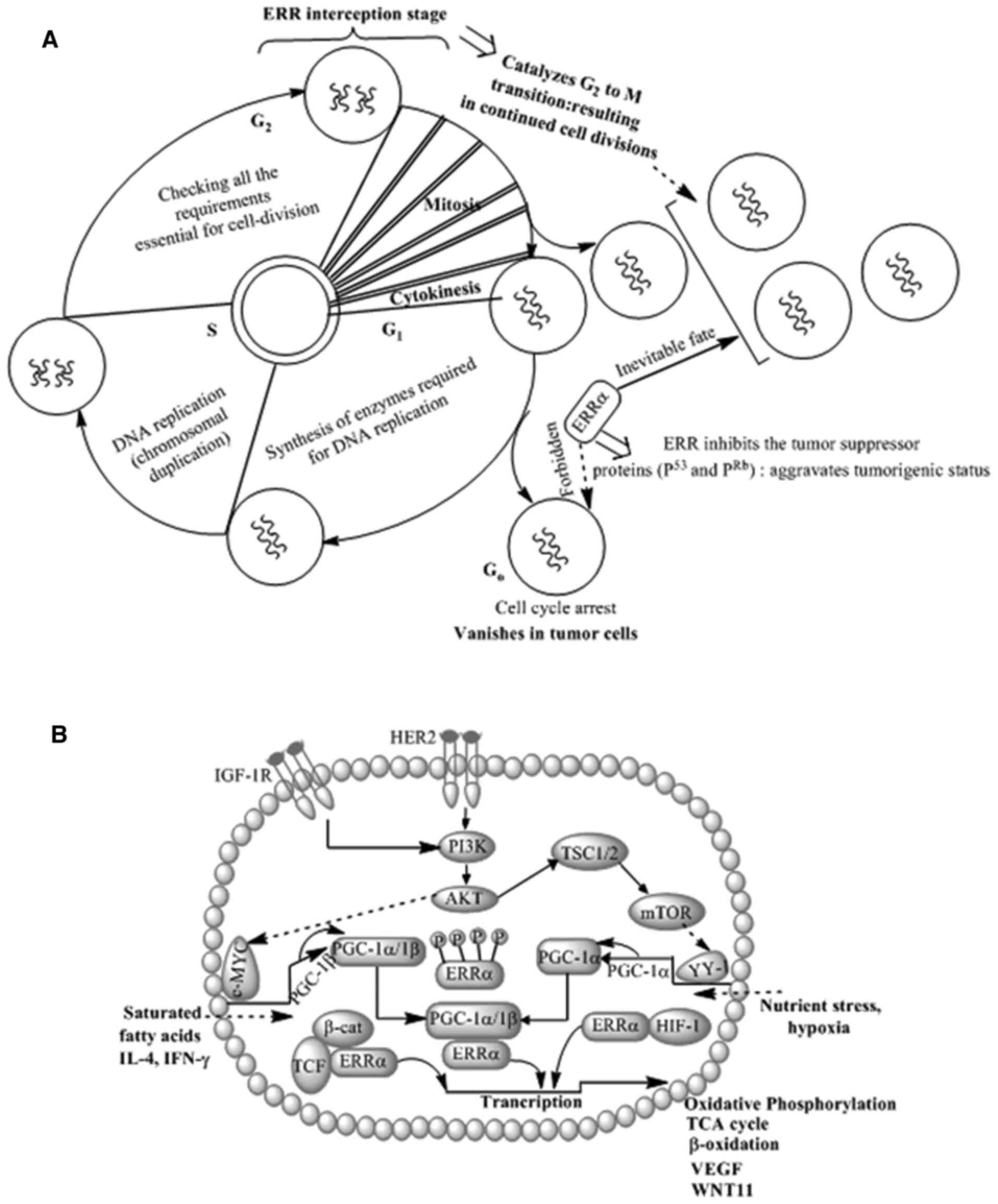
|
|
16
|
Mollerup S, Berge G, Baera R, Skaug V,
Hewer A, Phillips DH, Stangeland L and Haugen A: Sex differences in
risk of lung cancer: Expression of genes in the PAH bioactivation
pathway in relation to smoking and bulky DNA adducts. Int J Cancer.
119:741–744. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
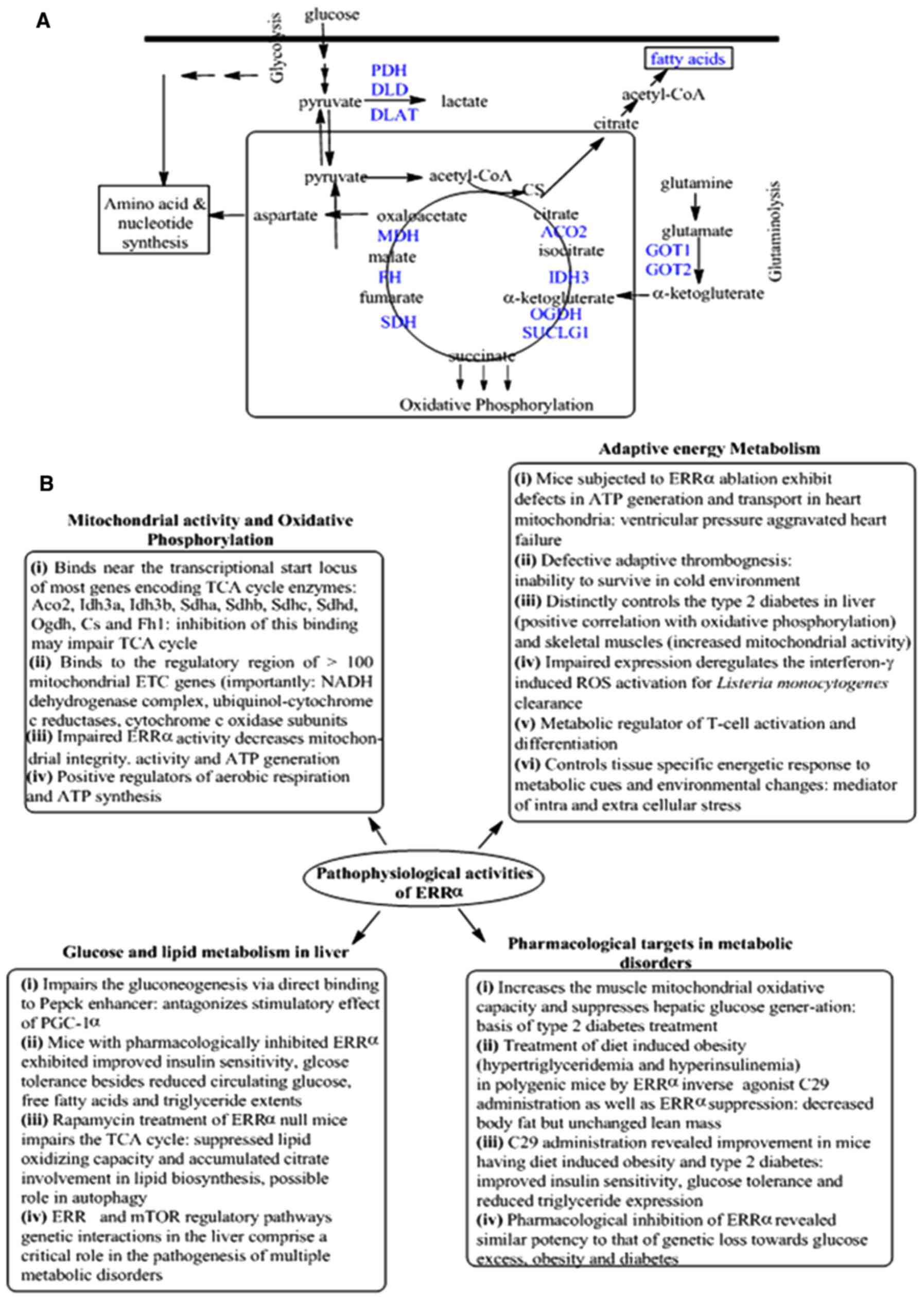
Klugman M, Xue X and Hosgood HD III:
Race/ethnicity and lung cancer survival in the United States: A
meta-analysis. Cancer Causes Control. 30:1231–1241. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schabath MB, Cress D and Muñoz-Antonia T:
Racial and ethnic differences in the epidemiology and genomics of
lung cancer. Cancer Control. 23:338–346. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Izbicka E, Streeper RT, Michalek JE,
Louden CL, Diaz A III and Campos DR: Plasma biomarkers distinguish
non-small cell lung cancer from asthma and differ in men and women.
Cancer Genomics Proteomics. 9:27–35. 2012.PubMed/NCBI
|
|
20
|
Hastings RH, Laux AM, Casillas A, Xu R,
Lukas Z, Ernstrom K and Deftos LJ: Sex-specific survival advantage
with parathyroid hormone-related protein in non-small cell lung
carcinoma patients. Clin Cancer Res. 12:499–506. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang YL, Yuan JQ, Wang KF, Fu XH, Han XR,
Threapleton D, Yang ZY, Mao C and Tang JL: The prevalence of EGFR
mutation in patients with non-small cell lung cancer: A systematic
review and meta-analysis. Oncotarget. 7:78985–78993. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
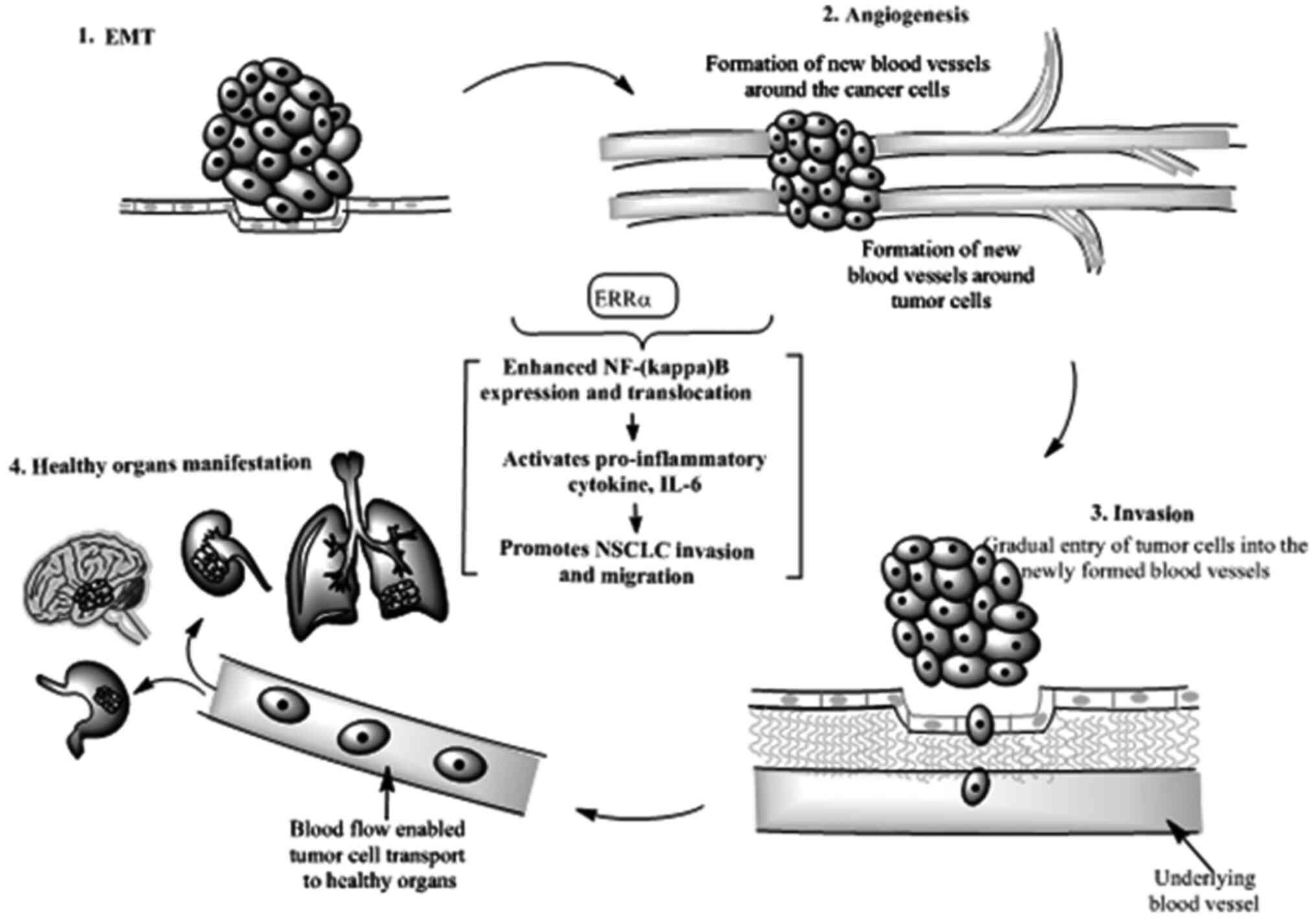
|
Kim HR, Shim HS, Chung JH, Lee YJ, Hong
YK, Rha SY, Kim SH, Ha SJ, Kim SK, Chung KY, et al: Distinct
clinical features and outcomes in never-smokers with nonsmall cell
lung cancer who harbor EGFR or KRAS mutations or ALK rearrangement.
Cancer. 118:729–739. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Patel MI, McKinley M, Cheng I, Haile R,
Wakelee H and Gomez SL: Lung cancer incidence trends in California
by race/ethnicity, histology, sex and neighbourhood socioeconomic
status: An analysis spanning 28 years. Lung Cancer. 108:140–149.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chang CH, Lee CH, Ho CC, Wang JY and Yu
CJ: Sex-based impact of epidermal growth factor receptor mutation
in patients with non-small cell lung cancer and previous
tuberculosis. Medicine (Baltimore). 94:e4442015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang C, Qiao W, Jiang Y, Zhu M, Shao J,
Ren P, Liu D and Li W: Effect of sex on the efficacy of patients
receiving immune checkpoint inhibitors in advanced non-small cell
lung cancer. Cancer Med. 8:4023–4031. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pinto JA, Vallejos CS, Raez LE, Mas LA,
Ruiz R, Torres-Roman JS, Morante Z, Araujo JM, Gomez HL, Aguilar A,
et al: Sex and outcomes in non-small cell lung cancer: An old
prognostic variable comes back for targeted therapy and
immunotherapy? ESMO Open. 3:e0003442018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nelson R: ALK inhibitors: Possible new
treatment for lung cancer. Medscape Medical News AACR-IASLC Joint
Conference on Molecular Origins of Lung Cancer. Jan 15–2010.
|
|
28
|
Wang WC, Shiao HY, Lee CC, Fung KS and
Hsieh HP: Anaplastic lymphnoma kinase (ALK) inhibitors: A review of
deign and discovery. Med Chem Comm. 5:1266–1279. 2014. View Article : Google Scholar
|
|
29
|
Shepherd FA, Rodrigues Pereira J, Ciuleanu
T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S,
Smylie M, Martins R, et al: Erlotinib in previously treated
non-small-cell lung cancer. N Engl J Med. 353:123–132. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yim SH and Chung YJ: Molecular
epidemiology of female lung cancer. Cancers (Basel). 3:1861–1876.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Guinee DG Jr, Travis WD, Trivers GE, De
Benedetti VM, Cawley H, Welsh JA, Bennett WP, Jett J, Colby TV,
Tazelaar H, et al: Sex comparisons in human lung cancer: Analysis
of p53 mutations, anti-p53 serum antibodies and C-erbB-2
expression. Carcinogenesis. 16:993–1002. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kure EH, Ryberg D, Hewer A, Phillips DH,
Skaug V, Baera R and Haugen A: p53 mutations in lung tumours:
Relationship to sex and lung DNA adduct levels. Carcinogenesis.
17:2201–2205. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Rivlin N, Brosh R, Oren M and Rotter V:
Mutations in the p53 tumor suppressor gene. Genes Cancers.
2:466–474. 2011. View Article : Google Scholar
|
|
34
|
Rivera MP: Lung cancer in women:
Differences in epidemiology, biology, histology and treatment
outcomes. Semin Respir. Crit Care Med. 34:792–801. 2013.
|
|
35
|
Stocco C: Tissue physiology and pathology
of aromatase. Steroids. 77:27–35. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Barakat R, Oakley O, Kim H, Jin J and Ko
CJ: Extra-gonadal sites of estrogen biosynthesis and function. BMV
Rep. 49:488–496. 2016.
|
|
37
|
Hammes SR and Levin ER: Impact of
estrogens in males and androgens in females. J Clin Invest.
129:1818–1826. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Reckelhoff JF: Sex differences in the
regulation of blood pressure. Hypertension. 37:1199–1208. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Blenck CL, Harvey PA, Reckelhoff JF and
Leinwand LA: The importance of biological sex and estrogen in
rodent models of cardiovascular health and disease. Circ Res.
118:1294–1312. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Simpson ER, Clyne C, Rubin G, Boon WC,
Robertson K, Britt K, Speed C and Jones M: Aromatase-A brief
Overview. Ann Rev Physiol. 64:93–127. 2002. View Article : Google Scholar
|
|
41
|
Weinberg OK, Marquez-Garban DC, Fishbein
MJ, Goodglick L, Garban HJ, Dubinett SM and Pietras RJ: Aromatase
inhibitors in human lung cancer therapy. Cancer Res.
65:11287–11291. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mollerup S, Jørgensen K, Berge G and
Haugen A: Expression of estrogen receptors alpha and beta in human
lung tissue and cell lines. Lung Cancer. 37:1531592002. View Article : Google Scholar
|
|
43
|
Stabile LP, Davis AL, Gubish CT, Hopkins
TM, Luketich JD, Christie N, Finkelstein S and Siegfried JM: Human
non-small cell lung tumors and cells derived from normal lung
express both estrogen receptor alpha and beta and show biological
responses to estrogen. Cancer Res. 62:2141–2150. 2002.PubMed/NCBI
|
|
44
|
Carey MA, Card JW, Voltz JW, Germolec DR,
Korach KS and Zeldin DC: The impact of sex and sex hormones on lung
physiology and disease: Lessons from animal studies. Am J Physiol
Lung Cell Mol Physiol. 293:L272–L278. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Brandenberger AW, Tee MK, Lee JY, Chao V
and Jaffe RB: Tissue distribution of estrogen receptors alpha
(ER-alpha) and beta (ER-beta) mRNA in the midgestational human
fetus. J Clin Endocrinol Metab. 82:3509–3512. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Márquez-Garbán DC, Chen HW, Fishbein MC,
Goodglick L and Pietras RJ: Estrogen receptor signaling pathways in
human non-small cell lung cancer. Steroids. 72:135–143. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Baik CS and Eaton KD: Estrogensignaling in
lung cancer: An opportunity for novel therapy. Cancers (Basel).
4:969–988. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Hsu LH, Liu KJ, Tsai MF, Wu CR, Feng AC,
Chu NM and Kao SH: Estrogen adversely affects the prognosis of
patients with lung adenocarcinoma. Cancer Sci. 106:51–59. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Heilbroner SP, Xanthopoulos EP, Buono D,
Huang Y, Carrier D, Shah A, Kim J, Corradetti M, Wright JD, Neugut
AI, et al: Impact of estrogen monotherapy on survival in women with
stage III–IV non-small cell lung cancer. Lung Cancer. 129:8–15.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Garon EB, Siegfried JM, Stabile LP, Young
PA, Marquez-Garban DC, Park DJ, Patel R, Hu EH, Sadeghi S, Parikh
RJ, et al: Randomized phase II study of fulvestrant and erlotinib
compared with erlotinib alone in patients with advanced or
metastatic non-small cell lung cancer. Lung Cancer. 123:91–98.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Giguere V, Yang N, Segui P and Evans RM:
Identification of a new class of steroid hormone receptors. Nature.
331:91–94. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Eudy JD, Yao S, Weston MD, Ma-Edmonds M,
Talmadge CB, Cheng JJ, Kimberling WJ and Sumegi J: Isolation of a
gene encoding a novel member of the nuclear receptor superfamily
from the critical region of Usher syndrome type IIa at 1q41.
Genomics. 50:382–384. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Hong H, Yang L and Stallcup MR:
Hormone-independent transcriptional activation and coactivator
binding by novel orphan nuclear receptor ERR3. J Biol Chem.
274:22618–22626. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Lata K and Mukherjee TK: Knockdown of
receptor for advanced glycation end products attenuate
17α-ethinyl-estradiol dependent proliferation and survival of MCF-7
breast cancer cells. Biochim Biophys Acta. 1840:1083–1091. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Riggins RB, Lan JP, Zhu Y, Klimach U,
Zwart A, Cavalli LR, Haddad BR, Chen L, Gong T, Xuan J, et al:
ERRgamma mediates tamoxifen resistance in novel models of invasive
lobular breast cancer. Cancer Res. 68:8908–8917. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Manna S, Bostner J, Sun Y, Miller LD,
Alayev A, Schwartz NS, Lager E, Fornander T, Nordenskjöld B, Yu JJ,
et al: ERRα is a marker of tamoxifen response and survival in
triple-negative breast cancer. Clin Cancer Res. 22:1421–1431. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lam SS, Mak AS, Yam JW, Cheung AN, Ngan HY
and Wong AS: Targeting estrogen-related receptor alpha inhibits
epithelial-to-mesenchymal transition and stem cell properties of
ovarian cancer cells. Mol Ther. 22:743–751. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Yoriki K, Mori T, Kokabu T, Matsushima H,
Umemura S, Tarumi Y and Kitawaki J: Estrogen-related receptor alpha
induces epithelial-mesenchymal transition through cancer-stromal
interactions in endometrial cancer. Sci Rep. 9:66972019. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Fujimura T, Takahashi S, Urano T, Ijichi
N, Ikeda K, Kumagai J, Murata T, Takayama K, Horie-Inoue K, Ouchi
Y, et al: Differential expression of estrogen-related receptors
beta and gamma (ERRbeta and ERRgamma) and their clinical
significance in human prostate cancer. Cancer Sci. 101:646–651.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Liang R, Lin Y, Yuan CL, Liu ZH, Li YQ,
Luo XL, Ye JZ and Ye HH: High expression of estrogen-related
receptor α is significantly associated with poor prognosis in
patients with colorectal cancer. Oncol Lett. 15:5933–5935.
2018.PubMed/NCBI
|
|
61
|
Li P, Wang J, Wu D, Ren X, Wu W, Zuo R,
Zeng Q, Wang B, He X, Yuan J and Xie N: ERRα is an aggressive
factor in lung adenocarcinoma indicating poor prognostic outcomes.
Cancer Manag Res. 11:8111–8123. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ariazi EA and Jordan VC: Estrogen-related
receptors as emerging targets in cancer and metabolic disorders.
Curr Top Med Chem. 6:203–215. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Busch BB, Stevens WC Jr, Martin R,
Ordentlich P, Zhou S, Sapp DW, Horlick RA and Mohan R:
Identification of a selective inverse agonist for the orphan
nuclear receptor estrogen-related receptor alpha. J Med Chem.
47:5593–5596. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Willey PJ, Murray IR, Qian J, Busch BB,
Stevens WC Jr, Martin R, Mohan R, Zhou S, Ordentlich P, Wei P, et
al: Regulation of PPARgamma coactivator 1alpha (PGC-1alpha)
signaling by an estrogen-related receptor alpha (ERRalpha) ligand.
Proc Natl Acad Sci USA. 101:8912–8917. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Chisamore MJ, Cunningham ME, Flores O,
Wilkinson HA and Chen JD: Characterization of a novel small
molecule subtype specific estrogen-related receptor alpha
antagonist in MCF-7 breast cancer cells. PLoS One. 4:e56242009.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Teng CT, Beames B, Merrick BA, Martin N,
Romeo C and Jetten AM: Development of a stable cell line with an
intact PGC-1α/ERRα axis for screening environmental chemicals.
Biochem Biophys Res Commun. 444:177–181. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Teng CT, Hsieh JH, Zhao J, Huang R, Xia M,
Martin N, Gao X, Dixon D, Auerbach SS, Witt KL and Merick BA:
Development of novel cell lines for high-throughput screening to
detect estrogen-related receptor alpha modulators. SLAS Discov.
22:720–731. 2017.PubMed/NCBI
|
|
68
|
Wei W, Schwaid AG, Wang X, Wang X, Chen S,
Chu Q, Saghatelian A and Wan Y: Ligand activation of ERRα by
cholesterol mediates statin and bisphosphonate effects. Cell Metab.
23:479–491. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Nuclear Receptors Nomenclature Committee,
. A unified nomenclature system for the nuclear receptor
superfamily. Cell. 97:161–163. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Tremblay AM and Giguere V: The NR3B
subgroup: An ovERRview. Nucl Recept Signal. 5:e0092007. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Heard DJ, Norby PL, Holloway J and Vissing
H: Human ERRgamma, a third member of the estrogen receptor-related
receptor (ERR) subfamily of orphan nuclear receptors:
Tissue-specific isoforms are expressed during development and in
the adult. Mol Endocrinol. 14:382–392. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Laudet V, Hënni C, Coll J, Catzeflis F and
Stéhelin D: Evolution of the nuclear receptor gene superfamily.
EMBO J. 11:1003–1013. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Huss JM, Garbacz W and Xie W: Constitutive
activities of estrogen related receptors: Transcriptional
regulation of metabolism by the ERR pathways in health and disease.
Biochim Biophys Acta. 1852:1912–1927. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Tremblay AM, Wilson BJ, Yang XJ and
Giguere V: Phosphorylation-dependent sumoylation regulates
estrogen-related receptor-alpha and-gamma transcriptional activity
through a synergy control motif. Mol Endocrinol. 22:570–584. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Vu EH, Kraus RJ and Mertz JE:
Phosphorylation-dependent sumoylation of estrogen-related
receptor-alpha1. Biochemistry. 46:9795–9804. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Gearhart MD, Hombeck SM, Evans RM, Dyson
HJ and Wright PE: Monomeric complex of human orphan estrogen
related receptor-2 with DNA: A pseudo-dimer interface mediates
extended half-site recognition. J Mol Biol. 327:819–832. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Huppunen J and Aarnisalo P: Dimerisation
modulates the activity of the orphan nuclear receptor ERRgamma.
Biochem. Biophys Res Commun. 314:964–970. 2004. View Article : Google Scholar
|
|
78
|
Oka SI, Zhai P, Alcendor R, Park JY and
Sadoshima J: Suppression of ERR targets by a PPARα/Sirt1 complex in
the failing heart. Cell Cycle. 11:856–864. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Onofrio ND, Servillo L and Balestrieri ML:
SIRT1 and SIRt6 signaling pathways in cardiovascular diseases
protection. Antioxid Redox Signal. 28:711–732. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Wang C, Fu M and Pestell RG: Estrogen
receptor acetylation and phosphorylation in hormone responses. Br
Cancer Online. 8:e462005. View Article : Google Scholar
|
|
81
|
Wilson BJ, Tremblay AM, Deblois G,
Sylvain-Drolet G and Giguere V: An acetylation switch modulates the
transcriptional activity of estrogen-related receptor alpha. Mol
Endocrinol. 24:1349–1358. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Chen S, Zhou D, Yang C and Sherman M:
Molecular basis for the constitutive activity of estrogen-related
receptor alpha-1. J Biol Chem. 276:28465–28470. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Xie W, Hong H, Yang NN, Lin RJ, Simon CM,
Stallcup MR and Evans RM: Constitutive activation of transcription
and binding of coactivator by estrogen-related receptors 1 and 2.
Mol Endocrinol. 13:2151–2162. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Kallen J, Schlaeppi JM, Bitsch F,
Filipuzzi I, Schib A, Riou V, Graham A, Strauss A, Geiser M and
Foumier B: Evidence for ligand-independent transcriptional
activation of the human estrogen-related receptor alpha (ERRalpha):
Crystal structure of ERRalpha ligand binding domain in complex with
peroxisome proliferator-activated receptor coactivator-1alpha. J
Biol Chem. 279:49330–49337. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Greschik H, Flaig R, Renaud JP and Moras
D: Structural basis for the deactivation of the estrogen-related
receptor gamma by diethylstilbestrol or 4-hydroxytamoxifen and
determinants of selectivity. J Biol Chem. 279:33639–33646. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Greschik H, Wurtz JM, Sanglier S, Borguet
W, van Dorsselaer A, Moras D and Renaud JP: Structural and
functional evidence for ligand-independent transcriptional
activation by the estrogen-related receptor 3. Mol Cell. 9:303–313.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Kallen J, Lattmann R, Beerli R,
Blechschmidt A, Blommers MJ, Geiser M, Ottl J, Schlaeppi JM,
Strauss A and Fournier B: Crystal structure of human
estrogen-related receptor alpha in complex with a synthetic inverse
agonist reveals its novel molecular mechanism. J Biol Chem.
282:23231–23239. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Wang L, Zuercher WJ, Consler TG, Lambert
MH, Miller AB, Orband-Miller LA, McKee DD, Wilson TM and Nolte RT:
X-ray crystal structures of the estrogen-related receptor gamma
ligand binding domain in three functional states reveal the
molecular basis of small molecule regulation. J Biol Chem.
281:37773–37781. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Jin KS, Park JK, Yoon J, Rho Y, Kim JH,
Kim EE and Ree M: Small-angle X-ray scattering studies on
structures of an estrogen-related receptor α ligand binding domain
and its complexes with ligands and coactivators. J Phys Chem B.
112:9603–9612. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Yaşar P, Ayaz G, User SD, Güpür G and
Muyan M: Molecular mechanism of estrogen-estrogen receptor
signaling. Reprod Med Biol. 16:4–20. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Couse JF and Korach KS: Estrogen receptor
null mice: What have we learned and where will they lead us? Endocr
Rev. 20:358–417. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Klinge CM, Brolly CL, Bambara RA and Hilf
R: Hsp70 is not required for high affinity binding of purified calf
uterine estrogen receptor to estrogen response element DNA in
vitro. J Steroid Biochem Mol Biol. 63:283–301. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Devin-Leclerc J, Meng X, Delahaye F,
Leclerc P, Baulieu EE and Catelli MG: Interaction and dissociation
by ligands of estrogen receptor and Hsp90: The antiestrogen RU
58668 induces a protein synthesis-dependent clustering of the
receptor in the cytoplasm. Mol Endocrinol. 12:842–854. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Kumar S, Lata K, Mukhopadhyay S and
Mukherjee TK: Role of estrogen receptors in pro-oxidative and
anti-oxidative actions of estrogens: A perspective. Biochim Biophys
Acta. 1800:1127–1135. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Klinge CM: Estrogen receptor interaction
with co-activators and co-repressors. Steroids. 65:227–251. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Klein-Hitpass L, Ryffel GU, Heitlinger E
and Cato AC: A 13 bp palindrome is a functional estrogen responsive
element and interacts specifically with estrogen receptor. Nucleic
Acids Res. 16:647–663. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Cheung E and Kraus WL: Genomic analyses of
hormone signaling and gene regulation. Annu Rev Physiol.
72:191–218. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Carroll JS, Meyer CA, Song J, Li W,
Geistlinger TR, Eeckhoute J, Brodsky AS, Keeton EK, Fertuck KC,
Hall GF, et al: Genome-wide analysis of estrogen receptor binding
sites. Nat Genet. 38:1289–1297. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
99
|
Hall JM, Couse JF and Korach KS: The
multifaceted mechanisms of estradiol and estrogen receptor
signaling. J Biol Chem. 276:36869–36872. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Li C, Briggs MR, Ahlborn TE, Kraemer FB
and Liu J: Requirement of Sp1 and estrogen receptor alpha
interaction in 17β-estradiol-mediated transcriptional activation of
the low density lipoprotein receptor gene expression. Endocrinol.
142:1546–1553. 2001. View Article : Google Scholar
|
|
101
|
Safe S: Transcriptional activation of
genes by 17 beta-estradiol through estrogen receptor Sp1
interactions. Vitam Horm. 62:231–252. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Paech K, Webb P, Kuiper GG, Nilsson S,
Gustafsson J, Kushner PJ and Scanlan TS: Differential ligand
activation of estrogen receptors ERalpha and ERbeta at AP1 sites.
Science. 277:1508–1510. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Webb P, Nguyen P, Valentine C, Lopez GN,
Kwok GR, McInerney E, Katzenellenbogen BS, Enmark E, Gustafsson JA,
Nilsson S and Kushner PJ: The estrogen receptor enhances AP-1
activity by two distinct mechanisms with different requirements for
receptor transactivation functions. Mol Endocrinol. 13:1672–1685.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Kushner PJ, Agard DA, Greene GL, Scanlan
TS, Shiau AK, Uht RM and Webb P: Estrogen receptor pathways toAP-1.
J Steroid Biochem Mol Biol. 74:311–317. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Marino M, Galluzzo P and Ascenzi P:
Estrogen signaling multiple pathways to impact gene transcription.
Curr Genomics. 7:497–508. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Klinge CM: Estrogen receptor interaction
with estrogen response elements. Nucleic Acids Res. 29:2905–2919.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Johnston SD, Liu XD, Zuo F, Eisenbraun TL,
Wiley SR, Kraus RJ and Mertz JE: Estrogen-related receptor alpha 1
functionally binds as a monomer to extended half-site sequences
including ones contained within estrogen-response elements. Mol
Endocrinol. 11:342–352. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Zhang Z and Teng CT: Estrogen
receptor-related receptor alpha 1 interacts with coactivator and
constitutively activates the estrogen response elements of the
human lactoferrin gene. J Biol Chem. 275:20837–20846. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Vanacker JM, Petterson K, Gustafsson JA
and Laudet V: Transcriptional targets shared by estrogen
receptor-related receptors (ERRs) and estrogen receptor (ER) alpha,
but not by ER beta. EMBO J. 18:4270–4279. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Mullen EM, Gu P and Cooney AJ: Nuclear
receptors in regulation of mouse ES cell pluripotency and
differentiation. PPAR Res. 2007:615632007. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Deblois G and Giguere V: Oestrogen-related
receptors in breast cancer: Control of cellular metabolism and
beyond. Nat Rev Cancer. 13:27–36. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Gravel SP: Deciphering the dichotomous
effects of PGC-1α on tumorigenesis and metastasis. Front Oncol.
8:752018. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
LeBleu VS, O'Connell JT, Gonzalez Herrera
KN, Wikman H, Pantel K, Haigis MC, de Carvalho FM, Damascena A,
Domingos Chinen LT, Rocha RM, et al: PGC-1α mediates mitochondrial
biogenesis and oxidative phosphorylation in cancer cells to promote
metastasis. Nat Cell Biol. 16:992–1003, 1-15. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Tan Z, Luo X, Xiao L, Tang M, Bode AM,
Dong Z and Cao Y: The role of PGC-1α in cancer metabolism and its
therapeutic implications. Mol Cancer Ther. 15:774–782. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Torrano V, Valcarcel-Jimenez L, Cortazar
AR, Liu X, Urosevic J, Castillo-Martin M, Fernandez-Ruiz S,
Morciano G, Caro-Maldonado A, Guiu M, et al: The metabolic
co-regulator PGC1α suppresses prostate cancer metastasis. Nat Cell
Biol. 18:645–656. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Deblois G, St-Pierre J and Giguere V: The
PGC-1/ERR signaling axis in cancer. Oncogene. 32:3483–3490. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Audet-Walsh É, Yee T, McGuirk S, Vernier
M, Ouellet C, St-Pierre J and Giguère V: Androgen-dependent
repression of ERRγ reprograms metabolism in prostate cancer. Cancer
Res. 77:378–389. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Sun P, Sehouli J, Denkert C, Mustea A,
Kongsen D, Koch I, Wei L and Lichtenegger W: Expression of estrogen
receptor-related receptors, a subfamily of orphan nuclear
receptors, as new tumor biomarkers in ovarian cancer cells. J Mol
Med. 83:457–467. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Kang MH, Choi H, Oshima M, Cheong JH, Kim
S, Lee JH, Park YS, Choi HS, Kweon MN, Pack CG, et al:
Estrogen-related receptor gamma functions as a tumor suppressor in
gastric cancer. Nat Commun. 9:19202018. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Kim JH, Choi YK, Byun JK, Kim MK, Kang YN,
Kim SH, Lee S, Jang BK and Park KG: Estrogen-related receptor γ is
upregulated in liver cancer and its inhibition suppresses liver
cancer cell proliferation via induction of p21 and p27. Exp Mol
Med. 48:e2132016. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Pons F, Varela M and Llovet JM: Sensing
systems in hepatocellular carcinoma. HPB (Oxford). 7:35–41. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Zhou Y, Jia Q, Meng X, Chen D and Zhu B:
ERRα regulates OTUB1 expression to promote colorectal cancer cell
migration. J Cancer. 10:5812–5819. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Luo C, Balsa E, Thomas A, Hatting M,
Jedrychowski M, Gygi SP, Widlung HR and Puigserver P: ERRα
maintains mitochondrial oxidative metabolism and constitutes an
actionable target in PGC1α-elevated melanomas. Mol Cancer Res.
15:1366–1375. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Bookout AL, Jeong Y, Downes M, Yu RT,
Evans RM and Mangelsdorf DJ: Anatomical profiling of nuclear
receptor expression reveals a hierarchical transcriptional network.
Cell. 126:789–799. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Ranhotra HS: The orphan estrogen-related
receptor alpha and metabolic regulation: New frontiers. J Recept
Signal Transduct Res. 35:565–568. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Giguère V: Transcriptional control of
energy homeostasis by the estrogen-related receptors. Endocr Rev.
29:677–696. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Ijichi N, Ikeda K, Horie-Inoue K, Yagi K,
Okazaki Y and Inoue S: Estrogen-related receptor alpha modulates
the expression of adipogenesis-related genes during adipocyte
differentiation. Biochem Biophys Res Commun. 358:813–818. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Kubo M, Ijichi N, Ikeda K, Horie-Inoue K,
Takeda S and Inoue S: Modulation of adipogenesis-related gene
expression by estrogen-related receptor gamma during adipocytic
differentiation. Biochim Biophys Acta. 1789:71–77. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Lorke DE, Susens U, Borgmeyer U and
Hermans-Borgmeyer I: Differential expression of the estrogen
receptor related receptor gamma in the mouse brain. Brain Res Mol
Brain Res. 77:277–280. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Luo J, Sladek R, Bader JA, Matthyssen A,
Rossant J and Giguère V: Placental abnormalities in mouse embryos
lacking the orphan nuclear receptor ERR-beta. Nature. 388:778–782.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Borgmeyer-Hermans I, Süsens U and
Borgmeyer U: Developmental expression of the estrogen
receptor-related receptor gamma in the nervous system during mouse
embryogenesis. Mech Dev. 97:197–199. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Luo J, Sladek R, Carrier J, Bader JA,
Richard D and Giguère V: Reduced fat mass in mice lacking orphan
nuclear receptor estrogen-related receptor alpha. Mol Cell Biol.
23:7947–7956. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Huss JM, Imahashi K, Dufour CR, Weinheimer
CJ, Courtois M, Kovacs A, Giguère V, Murphy E and Kelly DP: The
nuclear receptor ERRalpha is required for the bioenergetic and
functional adaptation to cardiac pressure overload. Cell Metab.
6:25–37. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Villena JA and Kralli A: ERRalpha: A
metabolic function for the oldest orphan. Trends Endocrinol Metab.
19:269–276. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Alaynick WA, Kondo RP, Xie W, He W, Dufour
CR, Downes M, Jonker JW, Giles W, Naviaux RK, Giguere V and Evans
RM: ERRgamma directs and maintains the transition to oxidative
metabolism in the postnatal heart. Cell Metab. 6:13–24. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Zhou W, Liu Z, Wu J, Liu JH, Hyder SM,
Antoniou E and Lubahn DB: Identification and characterization of
two novel splicing isoforms of human estrogen-related receptor
beta. Clin Endocrinol Metab. 91:569–579. 2006. View Article : Google Scholar
|
|
137
|
Xu Z, Wang Y, Xiao ZG, Zou C, Zhang X,
Wang Z, Wu D, Yu S and Chan FL: Nuclear receptor ERRα and
transcription factor ERG form a reciprocal loop in the regulation
of TMPRSS2: ERGfusion gene in prostate cancer. Oncogene.
37:6259–6274. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Bonnelye E, Vanacker JM, Dittmar T, Begue
A, Desbiens X, Denhardt DT, Aubin JE, Laudet V and Fournier B: The
ERR-1 orphan receptor is a transcriptional activator expressed
during bone development. Mol Endocrinol. 11:905–916. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Pettersson K, Svensson K, Mattsson R,
Carlsson B, Ohlsson R and Berkenstam A: Expression of a novel
member of estrogen response element-binding nuclear receptors is
restricted to the early stages of chorion formation during mouse
embryogenesis. Mech Dev. 54:211–223. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Wang J, Wang Y and Wong C:
Oestrogen-related receptor alpha inverse agonist XCT-790 arrests
A549 lung cancer cell population growth by inducing mitochondrial
reactive oxygen species production. Cell Prolif. 43:103–113. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Fouad YF and Aanei C: Revisiting the
hallmarks of cancer. Am. J Cancer Res. 7:1016–1036. 2017.
|
|
142
|
Pardee AB: G1 events and regulation of
cell proliferation. Science. 246:603–608. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Harper JV: Synchronization of cell
populations in G1/S and G2/M phases of the cell cycle. Methods Mol
Biol. 296:157–166. 2005.PubMed/NCBI
|
|
144
|
Makowiecki C, Nolte A, Sutaj B, Keller T,
Avci-Adali M, Stoll H, Schlensak C, Wendel HP and Walker T: New
basic approach to treat non-small cell lung cancer based on
RNA-interference. Thorac Cancer. 5:112–120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Martin TA, Ye L, Sanders AJ, Lane J and
Jiang WG: Cancer invasion and metastasis: Molecular and cellular
perspective. Mad Curie Bioscience Database. Landes Bioscience;
2000-2013
|
|
146
|
Polyak K and Weinberg RA: Transitions
between epithelial and mesenchymal states: Acquisition of malignant
and stem cell traits. Nat Rev Cancer. 9:265–273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Craene BD and Berx G: Regulatory networks
defining EMT during cancer initiation and progression. Nat Rev
Cancer. 13:97–110. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Singh A and Settleman J: EMT, Cancer stem
cells and drug resistance: An emerging axis of evil in the war on
cancer. Oncogene. 29:4741–4751. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Tiwari N, Gheldof A, Tatari M and
Christofori G: EMT as the ultimate survival mechanism of cancer
cells. Semin Cancer Biol. 22:194–207. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Krebs MG, Sloane R, Priest L, Lancashire
L, Hou JM, Greystoke A, Ward TH, Ferraldeschi R, Hughes A, Clack G,
et al: Evaluation and prognostic significance of circulating tumor
cells in patients with non-small cell lung cancer. J Clin Oncol.
29:1556–1563. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Jakobsen KR, Demuth C, Sorensen BS and
Nielsen AL: The role of epithelial to mesenchymal transition in
resistance to epidermal growth factor receptor tyrosine kinase
inhibitors in non-small cell lung cancer. Transl Lung Cancer Res.
5:172–182. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Li L, Gu X, Yue J, Zhao Q, Lv D, Chen H
and Xu L: Acquisition of EGFR TKI resistance and EMT phenotype is
linked with activation of IGF1R/NF-κB pathway in EGFR-mutant NSCLC.
Oncotarget. 8:92240–92253. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Byers LA, Diao L, Wang J, Saintigny P,
Girard L, Peyton M, Shen L, Fan Y, Giri U, Tumula PK, et al: An
epithelial-mesenchymal transition gene signature predicts
resistance to EGFR and PI3K inhibitors and identifies Axl as a
therapeutic target for overcoming EGFR inhibitor resistance. Clin
Can Res. 19:279–290. 2013. View Article : Google Scholar
|
|
154
|
Aguilera TA and Giaccia AJ: Molecular
Pathways: Oncologic pathways and their role in T-cell exclusion and
immune evasion-A new role for the AXL receptor tyrosine kinase.
Clin Cancer Res. 23:2928–2933. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Datar I and Schalper KA:
Epithelial-Mesenchymal transition and immune evasion during lung
cancer progression: The chicken or the egg? Clin Cancer Res.
22:3422–3424. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Lou Y, Diao L, Cuentas ER, Denning WL,
Chen L, Fan YH, Byers LA, Wang J, Papadimitrakopoulou VA, Behrens
C, et al: Epithelial-mesenchymal transition is associated with a
distinct tumor microenvironment including elevation of inflammatory
signals and multiple immune checkpoints in lung adenocarcinoma.
Clin Can Res. 22:3630–3642. 2016. View Article : Google Scholar
|
|
157
|
Chen L, Gibbons DL, Goswami S, Cortez MA,
Ahn YH, Byers LA, Zhang X, Yi X, Dwyer D, Lin W, et al: Metastasis
is regulated via microRNA-200/ZEB1 axis control of tumour cell
PD-L1 expression and intratumoral immunosuppression. Nat Commun.
5:52412014. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Chae YK, Chang S, Ko T, Anker J, Agte S,
Iams W, Choi WM, Lee K and Cruz M: Epithelial-mesenchymal
transition (EMT) signature is inversely associated with T-cell
infiltration in non-small cell lung cancer (NSCLC). Sci Rep.
8:29182018. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Kwaśniak K, Czarnik-Kwaśniak J, Maziarz A,
Aebisher D, Zielińska K, Karczmarek-Borowska B and Tabarkiewicz J:
Scientific reports concerning the impact of interleukin 4,
interleukin 10 and transforming growth factor β on cancer cells.
Cent Eur J Immunol. 44:190–220. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Steen EH, Wang X, Balaji S, Butte MJ,
Bollyky PL and Keswani SG: The role of the anti-inflammatory
cytokine Interleukn-10 in tissue fibrosis. Adv Wound Care (New
Rochelle). 9:184–198. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Tsoukalas N, Aravantinou-Fatorou A, Tolia
M, Giaginis C, Galanapoulos M, Kiakou M, Kostakis ID, Dana E,
Vamvakaris I, Korogiannos A, et al: Epithelial-mesenchymal
transition in non small-cell lung cancer. Anticancer Res.
37:1773–1778. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Mahmood MQ, Ward C, Muller HK, Sohal SS
and Walters EH: Epithelial mesenchymal transition (EMT) and
non-small cell lung cancer (NSCLC): A mutual association with
airway disease. Med Oncol. 34:452017. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Thompson JC, Hwang WT, Davis C, Deshpande
C, Jeffries S, Rajpurohit Y, Krishna V, Smirnov D, Verona R,
Lorenzi MV, et al: Gene signatures of tumor inflammation and
epithelial-to-mesenchymal transition (EMT) predict responses to
immune checkpoint blockade in lung cancer with high accuracy. Lung
Cancer. 139:1–8. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Huang JW, Guan BZ, Yin LH, Liu FN, Hu B,
Zheng QY, Li FL, Zhong YX and Chen Y: Effects of estrogen-related
receptor alpha (ERRα) on proliferation and metastasis of human lung
cancer A549 cells. J Huazhong Univ Sci Technolog Med Sci.
34:875–881. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Zhang J, Guan X, Liang N and Li S:
Estrogen-related receptor alpha triggers the proliferation and
migration of human non-small cell lung cancer via interleukin-6.
Cell Biochem Funct. 36:255–262. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Wang Y, Zhao M, Liu J, Ni J, Jiao Y and
Bai C: Up regulation of IL-6 is involved in di (2-ethylhexyl)
phthalate (DEHP) induced migration and invasion of non-small cell
lung cancer (NSCLC) cells. Biomed. Pharmacother. 89:1037–1044.
2017. View Article : Google Scholar
|
|
167
|
Kim JH: Di(2-ethylhexyl) phthalate
promotes lung cancer cell line A549 progression via Wnt/β-catenin
signaling. J Toxicol Sci. 44:237–244. 2019. View Article : Google Scholar : PubMed/NCBI
|