Introduction
Breast cancer is the most common malignancy and
first cause of cancer-related death among women worldwide (1). In the last years it has become clear
that breast cancer is a heterogeneous disease with distinct
molecular characteristics and clinical behavior. Human epidermal
growth factor receptor 2 (HER2) gene amplification resulting in
overexpression of the HER2 protein can be detected in approximately
15–20% of invasive breast tumors and is, historically, associated
with an aggressive disease course with common distant metastases
and poor prognosis (2–4).
HER2, a member of the epidermal growth factor
family, is a transmembrane protein consisting of an extracellular
ligand-binding domain, a transmembrane domain and an intracellular
domain with tyrosine kinase activity. Homo- and heterodimerization
of the HER family proteins [epidermal growth factor receptor
(EGFR), HER2, HER3, HER4], mostly involving HER2 as the preferred
dimerization partner, leads to activation of various downstream
signaling pathways such as mitogen-activated protein kinase (MAPK)
and phosphatidylinositol-4,5-biphosphate 3-kinase (PI3K) that
promote cell proliferation, migration, survival and invasion
(5,6).
The introduction of therapies inhibiting the HER2
signaling has drastically altered the landscape of treatment with
significantly improved outcomes in this group of patients (7). However, primary or acquired resistance
to anti-HER2 regimens leads almost universally to disease
progression, often with development of difficult to treat central
nervous system (CNS) metastases. In this review, we will summarize
the existing therapeutic options for HER2-positive metastatic
disease as well as novel agents currently under development that
are likely to further improve prognosis.
Established HER2-targeting agents
Trastuzumab
Trastuzumab is a recombinant humanized IgG
monoclonal antibody directed against the extracellular domain of
HER2 with various molecular mechanisms (8). Upon binding to its receptor,
trastuzumab induces internalization and degradation of HER2,
inhibits the HER2-dependent downstream proliferation signaling and
activates natural killer (NK) cells in the tumor microenvironment
through antibody-dependent cellular cytotoxicity (ADCC).
Trastuzumab was the first targeted agent to demonstrate impressive
efficacy as monotherapy as well as in combination with chemotherapy
in the first-line setting and the first monoclonal antibody to be
approved for the treatment of metastatic HER2-positive breast
cancer in 1998 (9,10).
Trastuzumab and chemotherapy in the
first line setting
According to the landmark study of Slamon et
al (10), the addition of
trastuzumab to taxane or anthracycline/cyclophosphamide resulted in
higher objective response rate (ORR) (50 vs. 32%, P<0.001),
longer progression free survival (PFS) (7.4 vs. 4.6 months, HR=0.5,
95% CI: 0.41–0.63, P<0.001) and overall survival (OS) (25.1 vs.
20.3 months, HR=0.8, 95% CI: 0.64–1.00, P=0.046) compared to
chemotherapy alone in patients with HER2-positive metastatic breast
cancer (10). Because of the
cardiotoxicity attributed to the combination of trastuzumab with
anthracycline (cardiac dysfunction in 27 vs. 13% of the patients),
trastuzumab and taxane was since adopted as the preferred
treatment.
It has been suggested that vinorelbine could be an
alternative option for taxanes in this setting, demonstrating
similar PFS (12.4 vs. 15.3 months HR=0.94, 95% CI: 0.71–1.25;
P=0.67) and OS rates (35.7 vs. 38.8 months, HR=1.01, 95% CI:
0.71–1.42; P=0.98) in a phase III trial (11). On the other hand, triple therapy with
the addition of carboplatin (12,13) or
non-pegylated liposomal doxorubicin (14) to trastuzumab and taxane showed no OS
benefit and was associated with excessive toxicity.
Sequential trastuzumab and
chemotherapy
Sequential treatment with initial single-agent
trastuzumab followed by the addition of chemotherapy upon
progression has always been considered an appealing strategy, given
that it delays the initiation of chemotherapy. It has been
evaluated in three randomized trials which, however, failed to
demonstrate non-inferiority.
In the phase II HERTAX trial (15), patients received either trastuzumab
monotherapy and switched to docetaxel at progression or upfront
trastuzumab and docetaxel combination. ORR was better in the
combination group (79 vs. 53%, P=0.016) and, despite similar PFS in
both groups (9.4 vs. 9.9 months, HR=1.33, 95% CI: 0.86–2.06,
P=0.2), OS was longer in the combination arm, with a trend towards
statistical significance (30.5 vs. 19.7 months, HR=1.49, 95% CI:
0.91–2.47, P=0.12).
The phase III JO17360 trial (16) evaluated single-agent trastuzumab
followed by the addition of docetaxel after progression vs. upfront
docetaxel and trastuzumab combination. PFS after both trastuzumab
and docetaxel was comparable (12.4 vs. 14.6 months, HR=1.35, 95%
CI: 0.79–2.30, p=0.27). Nevertheless, patient accrual was
terminated prematurely due to better PFS in the combination arm
compared to trastuzumab monotherapy (14.6 vs. 3.7 months, HR=4.24,
95% CI: 2.48–7.24, P<0.01), which was the primary endpoint of
the study. OS was also significantly better in the upfront
combination arm (median OS not available due to small number of
deaths, HR=2.72, 95% CI: 1.03–7.18, P=0.04).
SAKK 22/99 (17), a
phase III study with similar design to JO17360, randomized patients
to receive either trastuzumab followed by trastuzumab plus
chemotherapy or upfront trastuzumab plus chemotherapy. Time to
progression (TTP) and OS did not differ significantly between the
two groups (12.2 vs. 10.3 months, HR=0.7, 95% CI: 0.5–1.1, P=0.10
and 35.6 vs. 36.3 months, HR=0.9, P=0.55, respectively). In
subgroup analysis of the trastuzumab alone arm, patients without
visceral disease had a significantly longer TTP compared to the
ones with visceral metastases (21.8 vs. 10.1 months, P=0.03). Based
on these findings, the authors suggest that single-agent
trastuzumab could be a sufficient treatment option for individual
patients without visceral involvement.
Pertuzumab
Like trastuzumab, pertuzumab is a recombinant
monoclonal antibody against HER2. It binds to a different
extracellular dimerization domain than trastuzumab and prevents
HER2/HER3 heterodimerization, thereby acting complementarily to
trastuzumab in inhibiting the downstream proliferation pathways
(6).
Pertuzumab, trastuzumab and docetaxel
in the first-line setting
Dual HER2 inhibition with trastuzumab and pertuzumab
in combination with chemotherapy has been introduced as the current
standard-of-care in first-line treatment based on the results of
the phase III CLEOPATRA study (18,19).
Previously untreated patients were randomized to receive
trastuzumab and docetaxel with or without pertuzumab. The addition
of pertuzumab led to significant improvement of ORR (80 vs. 69%,
P=0.001), PFS (18.5 vs. 12.4 months, HR=0.62, 95% CI: 0.51–0.75,
P<0.001) and OS (56.5 vs. 40.8 months, HR=0.68; 95% CI:
0.56–0.84, P<0.001). Recently, the end-of-study analysis further
confirmed the durable superiority of the dual blockade with 8-year
OS rates of 37 and 23%, respectively (20). According to a post-hoc analysis,
continuing the administration of docetaxel after 6 cycles did not
add clinical benefit in terms of PFS or OS (21). Patients who had previously received
trastuzumab in the neoadjuvant or adjuvant setting were also found
to experience similar benefit from the three-agent combination.
Pertuzumab, trastuzumab and other
chemotherapy-regimens in the first-line setting
Chemotherapy regimens other than docetaxel have been
evaluated in combination with trastuzumab and pertuzumab. As shown
in the preliminary results of the PERUSE trial (22), paclitaxel-containing regimens are
valid alternative options to docetaxel. ORR was 79% with docetaxel,
83% with paclitaxel and 77% with nab-paclitaxel, while PFS was
19.6, 23.0 and 18.1 months, respectively. Toxicity was in
accordance with known safety profiles, with docetaxel being
associated more frequently with febrile neutropenia (11 vs. 1%) and
mucositis (25 vs. 14%) and less frequently with peripheral
neuropathy (16 vs. 31%). Smaller single-arm studies have
demonstrated efficacy for vinorelbine (ORR 74,2%, PFS 14.3 months)
(23) and eribulin (ORR 80%)
combined with dual HER2 blockade (24).
Pertuzumab, trastuzumab and
chemotherapy in the second-line setting
Efficacy of dual HER2-blockade with trastuzumab and
pertuzumab in patients previously treated with trastuzumab for
advanced disease was investigated in the phase III PHEREXA trial
(25). Patients who had progressed
on trastuzumab and taxane in the first-line setting were randomized
to receive trastuzumab and capecitabine with or without the
addition of pertuzumab. The primary endpoint of PFS (11.1 vs. 9
months, HR=0.82, 95% CI: 0.65–1.02, P=0.07) was not reached,
although there was a non-significant improvement in the pertuzumab
arm. Similarly, there was a numerical survival benefit in the
pertuzumab group (OS 36.1 vs. 28.1 months, HR=0.76; 95% CI:
0.60–0.98), but statistical significance was not claimed as the
trial was underpowered for OS analysis (26). Although the combination of
trastuzumab and pertuzumab does seem to offer clinical benefit
beyond the first-line setting and the reported median PFS is
comparable to the one demonstrated with ado trastuzumab emtasine
(T-DM1), PHEREXA is a negative trial and T-DM1 remains the current
standard-of-care in the second-line setting.
Ado Trastuzumab emtasine (T-DM1)
T-DM1 is an antibody-drug conjugate composed of
trastuzumab and the potent microtubule-inhibitory agent DM1. In
binding HER2, the cytotoxic component is selectively delivered to
HER2+ cells and leads to apoptosis upon intracellular
release (27).
T-DM1 in the second- and third-line
setting
Efficacy of T-DM1 as third- and second-line
treatment was demonstrated in TH3RESA (28,29) and
EMILIA (30,31) trials, respectively. TH3RESA compared
T-DM1 to treatment of physician's choice after previous exposure to
trastuzumab, lapatinib and taxane and demonstrated a significantly
longer PFS (6.2 vs. 3.3 months, HR=0.53, 95% CI: 0.42–0.66,
P<0.0001) and OS (22.7 vs. 15.8 months, HR=0.68, 95% CI:
0.54–0.85, P=0.0007) in the T-DM1 group, thereby establishing T-DM1
as preferred therapy in the third line. T-DM1 was also associated
with a lower incidence of grade 3 or worse adverse events (32 vs.
43%).
In EMILIA, patients previously treated with
trastuzumab and a taxane were randomized to receive T-DM1 or
lapatinib plus capecitabine-the standard-of-care at the time. T-DM1
was associated with significantly improved PFS (9.6 vs. 6.4 months,
HR=0.65, 95% CI: 0.55–0.77, P<0.001) and OS (30.9 vs. 25.1
months, HR=0.68, 95% CI: 0.55–0.85, P<0.001) and lower toxicity
(grade 3/4 adverse events in 41 vs. 57% of the patients). Based on
these results, T-DM1 was rapidly adopted as the preferred regimen
in the second line.
T-DM1 in the first-line setting
T-DM1 in the first-line was evaluated in the
MARIANNE trial (32,33). In this randomized phase III study,
previously untreated patients were divided in three treatment arms:
T-DM1, T-DM1 plus pertuzumab and trastuzumab plus taxane. The study
demonstrated non-inferiority-but also no superiority - concerning
the primary endpoint of PFS for both the T-DM1 and T-DM1 plus
pertuzumab arms (14.1 and 15.2 months, respectively vs. 13.7 months
in the trastuzumab plus taxane group, P=0.31 and 0.14). OS exceeded
50 months and was also similar across three treatment arms.
T-DM1-containing arms were associated with lower treatment
discontinuation rates due to adverse events and better quality of
life. However, since comparison was not made to a group receiving
dual HER2 blockade, which is the current standard-of-care, T-DM1
remains an alternative first-line option mainly for patients
unsuitable to receive the preferred regimen.
Lapatinib
Lapatinib is a small-molecule dual tyrosine kinase
inhibitor (TKI) reversibly targeting the intracellular domain of
both EGFR and HER2 and blocking activation of downstream
proliferation pathways and was, until recently, the only TKI
approved in the treatment of HER2+ breast cancer
(34).
Historically, lapatinib in combination with
capecitabine was a commonly used treatment upon progression on
trastuzumab plus chemotherapy (35).
However, since superiority of T-DM1 and, more recently, neratinib
was demonstrated, this regimen is reserved for later lines of
therapy.
Lapatinib in the first-line
setting
Lapatinib is inferior to trastuzumab in the
first-line setting, as shown in the MA.31 trial (36), in which previously untreated patients
with metastatic disease received taxane and HER2 blockade with
either trastuzumab or lapatinib. Lapatinib was associated with
shorter intention-to-treat PFS (9.0 vs. 11.3 months, HR=1.37, 95%
CI: 1.13–1.65, P=0.001), which was the primary endpoint of the
study. Toxicity was also higher in the lapatinib arm, with more
incidents of grade 3/4 diarrhea and rash (P<0.001).
Lapatinib +/− trastuzumab in
pretreated patients
According to the findings of the EFG104900 trial
(37), combination of lapatinib and
trastuzumab in trastuzumab-exposed patients is superior to
lapatinib alone in terms of PFS (11.1 vs. 8.1 weeks, HR=0.74, 95%
CI: 0.58–0.94, P=0.011) and OS (14 vs. 9.5 months, HR=0.74, 95% CI:
0.57–0.97, P=0.026), with the exception of hormone receptor
(HR)-positive tumors, which are known to demonstrate higher levels
of HER2 resistance (38). Therefore,
combination of lapatinib plus trastuzumab can be considered a
chemotherapy-free alternative for heavily pretreated patients.
Triple positive breast cancer
Approximately 50% of HER2-positive breast tumors
also express HR (38). There is a
known bidirectional crosstalk between the estrogen receptor (ER)
and HER receptor families, resulting in overexpression of ER in the
presence of acquired HER2 resistance and resistance to hormonal
treatment through HER2 overexpression (39). The obvious therapeutic strategy for
this group of patients includes simultaneous blocking of both
signaling pathways with a combination of HER2-targeted agents and
endocrine therapy. It has been previously shown that addition of
trastuzumab or lapatinib to an aromatase inhibitor prolongs PFS,
although not OS, compared to endocrine therapy alone in the
metastatic setting (40–42). Addition of endocrine therapy to
HER2-targeted treatment is much less studied although widely used -
there is to date no randomized trial.
Historically, clinical trials did not distinguish
the HR status in HER2+ disease. Dual HER blockade plus
chemotherapy has been the standard of care for these patients,
although the idea of chemotherapy-free regimens has always been
appealing. Efficacy of endocrine treatment combined with
single-agent or dual HER2 blockade in the absence of chemotherapy
has been recently investigated in the PERTAIN and ALTERNATIVE
trials (43,44).
In the phase II PERTAIN trial, treatment-naïve
patients (with exception of endocrine therapy) were randomized to
receive trastuzumab and an aromatase inhibitor with or without
Pertuzumab (43). The primary
endpoint of the study was PFS, which was shown to be significantly
better with the dual blockade (18.9 vs. 15.8 months, HR=0.65, 95%
CI: 0.48–0.89, P=0.007). ORR was similar between the two arms (63.3
vs. 55.7%, P=0.254), nevertheless, duration of response was
significantly longer in the pertuzumab group (27.1 vs. 15.1 months,
HR=0.57, 95% CI: 0.36–0.91, P=0.018).
ALTERNATIVE (44), a
randomized, phase III trial, evaluated first-line treatment with an
aromatase inhibitor combined with trastuzumab or lapatinib or both
in postmenopausal women. Patients in the dual blockade arm had a
significantly longer PFS compared to trastuzumab (11.0 vs. 5.7
months, HR=0.62, 95% CI: 0.45–0.88, P=0.0064), which was the
primary endpoint of the study. Median PFS with lapatinib was 8.3
months (HR vs. trastuzumab 0.71, 95% CI: 0.51–0.98, P=0.036).
Adverse events like diarrhea, rash and paronychia were more common
in the lapatinib containing regimens, mostly grade 1 and 2.
Both trials suggest encouraging efficacy of dual
HER2 blockade and endocrine therapy in previously untreated
HER2-positive, HR-positive disease, thereby offering an alternative
chemotherapy-free option for selected patients unfit to receive
chemotherapy.
Novel agents
New generation TKIs
Novel TKIs currently adopted in clinical practice
include neratinib and pyrotinib, two irreversible pan-HER TKIs
targeting EGFR, HER2 and HER4, as well as tucatinib, a highly
selective HER2 inhibitor with minimal inhibition of EGFR, therefore
with decreased potential for EGFR-related toxicities.
Neratinib in later-line setting
The phase III NALA trial (45) compared neratinib plus capecitabine to
lapatinib plus capecitabine after two or more anti-HER2 containing
treatment lines. Treatment with neratinib resulted in significantly
longer PFS (8.8. vs. 6.6 months, P=0.0003) and a trend towards
improved OS (24.0 vs. 22.2 months, HR=0.88, 95% CI: 0.72–1.07,
P=0.2086). Grade 3 diarrhea was more common in the neratinib arm
(24 vs. 13%), although discontinuation of treatment due to adverse
events was lower with neratinib (10.9 vs. 14.5%). Based on these
findings, the combination of neratinib and capecitabine has been
approved from the Food and Drug Administration (FDA) in April 2020
as third-line treatment in metastatic HER2-positive breast
cancer.
Neratinib in the first-line
setting
In the phase II NEfERT-T trial (46), neratinib failed to demonstrate
superiority against trastuzumab as first-line therapy. Patients
with previously untreated advanced disease were randomized to
receive paclitaxel with either trastuzumab or neratinib. There was
no difference in the median PFS (12.9 months in both arms), while
neratinib was associated with higher incidence of grade 3 diarrhea
(30.4 vs. 3.8%). However, a sub-analysis of NEfERT-T showed
neratinib to be more effective than trastuzumab in preventing CNS
disease (relative risk of brain metastases 0.48, P=0.002).
Neratinib in CNS disease
CNS activity of neratinib has also been tested
outside the NEfERT-T trial. In one cohort of the single-arm
multi-cohort TBCRC 022 trial (47),
forty patients with progressive CNS disease after at least one line
of CNS-directed treatment were treated with neratinib monotherapy.
ORR was only 8%, resulting in a median PFS of 1.9 months. However,
combination of neratinib and capecitabine in another cohort of the
same trial (48) resulted in more
promising outcomes. Patients with or without prior exposure to
lapatinib were treated with neratinib and capecitabine, with an ORR
of 33 and 49%, PFS of 3.1 and 5.5 months and OS of 15.1 and 13.3
months, respectively. As noted in the study, these findings support
a synergy between HER2-targeted agents and chemotherapy.
Pyrotinib in second-line setting
Efficacy of pyrotinib has been recently evaluated in
a Chinese open-label, randomized phase II study (49). Patients enrolled in the study had
been previously treated with chemotherapy and trastuzumab and were
randomized to receive either pyrotinib or lapatinib - both drugs in
combination with capecitabine. ORR was the primary endpoint of the
study and was significantly better in the pyrotinib group (78.5 vs.
57.1%, treatment difference 21.3%, 95% CI: 4.0–38.7, P=0.01).
Pyrotinib demonstrated significant superiority in terms of PFS as
well (18.1 vs. 7.0 months, HR=0.36, 95% CI: 0.23–0.58, P<0.001).
As far as toxicity is concerned, grade 3/4 hand-foot syndrome and
diarrhea were more common in the pyrotinib arm (24.6 vs. 20.6% and
15.4 vs. 4.8%, respectively). These findings were confirmed in the
phase III PHOEBE trial (50)
comparing pyrotinib plus capecitabine to lapatinib plus
capecitabine after exposure to trastuzumab and taxane. PFS was
significantly longer with pyrotinib (12.5 vs. 6.8 months, HR=0.39,
95% CI: 0.27–0.56, P<0.0001), while the toxicity profile was in
accordance with the one of the phase II trial.
Another randomized phase≈III trial (51) evaluated capecitabine with pyrotinib
or placebo in Chinese patients after failure of trastuzumab and
taxane. PFS was significantly longer in the pyrotinib arm (11.1 vs.
4.1 months). According to the study design, patients who progressed
on placebo plus capecitabine received pyrotinib monotherapy. In
this subgroup of patients, ORR was 38% and PFS 5.5 months. The most
common adverse event in the pyrotinib arm was grade 3 diarrhea,
which was observed in 30.8% of patients.
The biggest limitation of these trials is that,
among the study population, there was no prior exposure to current
standards of care in earlier lines such as pertuzumab and T-DM1.
However, pyrotinib in combination with capecitabine has already
received approval in China for HER2+ breast cancer after
anthracycline or taxane chemotherapy (52).
Tucatinib in later-line setting
Tucatinib was recently granted Breakthrough Therapy
designation by the FDA in combination with trastuzumab and
capecitabine as second or later line treatment, based on the
positive results of the HER2CLIMB trial (53). In this randomized trial, patients
pretreated with trastuzumab, pertuzumab and T-DM1 received a
combination of trastuzumab and capecitabine with or without
tucatinib. The addition of tucatinib resulted in improved PFS at 1
year (33.1 vs. 12.3%, HR for progression or death 0.54, 95% CI:
0.42–0.71, P<0.001). ORR (40.6 vs. 22.8%) and OS at 2 years
(44.9 vs. 26.6%, HR for death 0.66, 95% CI: 0.50–0.88, P=0.005)
were significantly better in the tucatinib group as well.
Tucatinib in CNS disease
Interestingly, patients with brain metastases were
included in HER2CLIMB, composing almost half of the study
population (47.5%), and seemed to benefit particularly from the
triplet therapy (PFS at 1 year 24.9 vs. 0%, HR=0.48, 95% CI:
0.34–0.69, P<0.001, median CNS-PFS 9.9 vs. 4.2 months, median OS
18.1 vs. 12.0 months, HR=0.58, 95% CI: 0.40–0.85, P=0.005)
(54). Since brain metastases appear
often in the course of the disease, these findings make tucatinib
an extremely promising later-line option.
Antibody-drug conjugate Trastuzumab
deruxtecan (DS-8201)
Trastuzumab deruxtecan is an antibody-drug conjugate
comprised of an anti-HER2 antibody bound to a cytotoxic
topoisomerase I inhibitor (a derivative of irinotecan) (55). It has been recently granted
accelerated approval by the FDA for patients who have received at
least two anti-HER2-based treatment lines. Efficacy was evaluated
in the phase II single-arm DESTINY-Breast01 trial (55) enrolling patients pretreated with
trastuzumab and T-DM1. Patients included in the study had received
a median of six previous treatments, however achieved an impressive
ORR of 60.9% (95% CI: 53.4–68.0), with a median duration of
response of 14.8 months (95% CI: 13.8–16.9). As far as tolerability
is concerned, among myelosuppression and nausea, interstitial lung
disease occurred in 13.6% of the patients, including one death.
Thus, careful monitoring for pulmonary symptoms is considered
mandatory during treatment.
Interestingly, DESTINY-Breast01 included 24 patients
with pretreated asymptomatic brain metastases. ORR was similar to
the whole patient population (58,3%, 95% CI 36,3-77.9), with a
median duration of response of 16.9 months (95% CI: 5.7–16.9)
(56). In fact, one patient
experienced a >50% regression of in-brain disease.
Antibody-drug conjugate trastuzumab
duocarmazine (SYD985)
Trastuzumab duocarmazine is composed of trastuzumab
linked, via a cleavable linker, to a prodrug of the alkylating
agent duocarmycin. Evaluation of the drug in a phase I
dose-escalation and dose-expansion study (57) including patients with different solid
tumors showed an ORR of 33% (16 of 48 patients) in
HER2-overexpressing breast cancer and 29% (9 of 32 patients) in
hormone-receptor positive, HER2-low breast cancer. A phase III
trial comparing trastuzumab duocarmazine to physician's choice
treatment in patients who have progressed after two anti-HER2
therapies is currently recruiting (NCT03262935).
Several other antibody-drug conjugates in earlier
stages of development are being investigated in preclinical and
clinical trials (A166, ALT-P7, ARX788, DHES0815A, MEDI4276, RC48,
XMT-1522) (58).
HER2-targeting monoclonal antibody
Margetuximab (MGAH22)
Fc-receptor (FcR) polymorphism is considered one of
the mechanisms of resistance to trastuzumab by reducing the
trastuzumab-mediated cellular cytotoxicity. Margetuximab is a
chimeric IgG monoclonal antibody with similar antiproliferative
effects as trastuzumab, but greater affinity to variants of the
CD16A receptor (59).
Margetuximab in later-line
setting
Based on the rationale that increased affinity can
enhance antibody-mediated immunity, margetuximab versus trastuzumab
in heavily pretreated patients has been investigated in the phase
III SOPHIA trial (60). Patients
exposed to two or more HER2-targeting regimens were randomized to
margetuximab plus chemotherapy or trastuzumab plus chemotherapy.
PFS was significantly longer in the margetuximab arm in the ITT
population (5.8 vs. 4.9 months, HR=0.76, P=0.033) and,
interestingly, in patients harboring the CD16A-158 F allele (6.9
vs. 5.1 months, HR=0.68, P=0.005), which is associated with poor
clinical response to trastuzumab. Furthermore, OS in the second
interim analysis of patients carrying the CD16A-158F allele favored
margetuximab, although not significantly (23.7 vs. 19.4 months,
P=0.087). Trastuzumab performed better in the homozygous patients,
although clinical characteristics of the population were not
balanced, with more patients with visceral and brain metastasis and
older age being assigned to margetuximab. Final OS analysis is
awaited in order to better define the role of margetuximab in this
setting.
Bispecific antibody ZW25
ZW25 is a bispecific HER2-targeting antibody that
simultaneously binds two non-overlapping HER2 epitopes, resulting
in dual HER2 blockade with increased tumor cell binding and
internalization (61). Effectiveness
and safety of ZW25 in HER2-expressing tumors are being currently
investigated in a 3-part study (NCT02892123). Part 1 has recently
demonstrated clinical benefit in heavily pretreated patients with a
variety of solid tumors, with a median PFS of 5.2 months and ORR
>30% (62), while no
dose-limiting adverse events occurred. Parts 2 and 3 of the study
evaluating ZW25 as monotherapy and combined with chemotherapy in
specific tumor types are still ongoing. Furthermore, a currently
recruiting phase II trial evaluates ZW25 in combination with
palbociclib and fulvestrant in HR+/HER2+
breast cancer (NCT04224272).
Bispecific antibody MCLA-128
MCLA-128 is a bispecific antibody with high
antibody-dependent cellular cytotoxicity binding HER2 and HER3.
Preliminary clinical activity in solid tumors has been confirmed in
a phase I trial (62), where, among
10 patients with heavily pretreated metastatic breast cancer,
clinical benefit rate was 70% and the drug showed a favorable
toxicity profile (only one infusion related reaction grade 4 in a
total of 15 patients). An ongoing phase II trial investigates the
addition of MCLA-128 to trastuzumab and vinorelbine in
HER2+ tumors, as well as to endocrine therapy in
HR+/HER2 low tumors (NCT03321981).
Cyclin dependent kinases (CDK)4/6
inhibitors
CDK4/6 inhibitors target the cell proliferative
activity of CDK4/6 in the estrogen signaling pathway and are
currently, in combination with endocrine therapy, the
standard-of-care in the treatment of hormone receptor positive/HER2
negative breast cancer (63).
Potential for integration of CDK4/6 inhibitors in HER2-positive
disease was first confirmed in the phase II monarchHER trial
(64), in which patients were
randomized to receive either abemaciclib, fulvestrant and
trastuzumab (arm A), or abemaciclib and trastuzumab (arm B) or
trastuzumab plus chemotherapy (arm C). The triple combination
significantly improved PFS (8.3 vs. 5.5 months, HR=0.67, P=0.051)
compared to trastuzumab plus chemotherapy. On the other hand, no
benefit was demonstrated for the abemaciclib/trastuzumab arm.
According to an exploratory analysis, median overall survival is to
date not significantly different between arms A and C (24 vs. 21
months).
CDK4/6 inhibition in ER+/HER2+
disease is being further studied in ongoing clinical trials. The
phase II PATRICIA trial (65)
evaluates the combination of palbociclib and trastuzumab in
postmenopausal patients after 2–4 lines of HER2-directed
treatments. During phase I of the trial, 60 patients were divided
in 3 cohorts: ER-negative (cohort A), ER-positive (cohort B1) and
ER-positive receiving letrozole (cohort B2). Phase I confirmed the
efficacy of the regimen for both the luminal A and luminal B
subtypes (median PFS 12.4 vs. 4.1 months in cohort A, p=0.025).
Recruitment in phase II is ongoing with a target of a total of 232
patients (NCT02448420). In accordance with the known safety profile
of CDK4/6 inhibitors, high grade neutropenia was observed in at
least 80% of the participants. In the phase III PATINA trial
(66), patients receive 6–8 cycles
of chemotherapy with taxane or vinorelbine plus dual HER2-directed
treatment with trastuzumab and pertuzumab and are then randomized
to trastuzumab/pertuzumab and endocrine treatment with or without
palbociclib. Primary endpoint of the study is PFS
(NCT02947685).
PI3K/AKT/mTOR inhibition
A potential mechanism of resistance to HER2-targeted
therapy is the permanent upregulation of the PI3K/AKT/mTOR pathway,
often due to mutations of the PIK3CA gene or loss of function of
the PTEN tumor suppressing phosphatase (67). Various studies have tested the
hypothesis that combined targeting of PIK/AKT/mTOR and HER2 could
overcome HER2 resistance.
Everolimus
Everolimus is an mTOR inhibitor that showed
promising results in combination with trastuzumab and chemotherapy
in early studies (68), nonetheless
failed to demonstrate clinically significant benefit in the phase
III BOLERO-3 (69) and BOLERO-1
(70) trials.
BOLERO-3 assessed the addition of everolimus to
trastuzumab and chemotherapy in patients with disease progression
under HER2-inhibition. Everolimus led to a median PFS of 7.0 vs.
5.8 months (HR=0.78, 95% CI: 0.65–0.95, P=0.0067), a statistically
significant but moderate benefit. In BOLERO-1, a study including
patients in the first-line setting, hazard of progression was
similar in both groups (15.0 vs. 14.5 months, HR=0.89, 95% CI:
0.73–1.08, P=0.1166), while everolimus was associated with
increased toxicity. However, according to a combined exploratory
analysis of both studies, the subpopulation of patients with
hyperactivation of the PI3K pathway seemed to profit from
everolimus in terms of PFS (71).
PI3K inhibitors
Efficacy of PI3K blockage was initially tested using
non-specific anti-PI3K drugs (68).
A phase Ib trial evaluated treatment with the pan-PI3K inhibitor
buparlisib and lapatinib in trastuzumab-pretreated patients
(72). The combination led to a
disease control rate of 79% (95% CI: 57–92) and clinical benefit
rate of 29% (95% CI: 12–51) in a total of 24 patients, although
high toxicity rates were found to be an important limiting
factor.
More recently, newer agents managed to demonstrate
clinical activity in small studies, while offering a better
tolerated toxicity profile. For instance, the combination of
alpelisib, a PI3Kα isoform-specific inhibitor, and T-DM1 in
trastuzumab-refractory disease resulted in an ORR of 43% in the
total population (n=17) and 30% in T-DM1-resistant patients (n=10)
(73). Alpelisib combined with dual
HER2-blockade is currently under evaluation as maintenance
treatment in patients harboring a PIK3CA mutation in a phase III
trial (NCT04208178). Other selective PI3K inhibitors such as
taselisib and MEN1611 are also being tested in combination with
anti-HER2 treatment in early-phase trials (NCT02390427,
NCT03767335) (68).
Immunotherapy
Although breast cancer is historically considered
poorly immunogenic, HER2+ tumors have more often higher
expression of possible predictive biomarkers such as programmed
death-ligand 1 (PD-L1), tumor-infiltrating lymphocytes (TILs) and
tumor mutational burden (TMB) compared to luminal subtypes
(74). Trastuzumab is also believed
to enhance immunogenicity due to ADCC (59). Based on this rationale, immunotherapy
with immune checkpoint-inhibitors has been evaluated in
HER2+ breast cancer with considerable results in certain
subgroups of patients.
Atezolizumab immunotherapy
Atezolizumab is a monoclonal IgG1 antibody directed
against PD-L1. Efficacy in metastatic HER2+ breast
cancer has been tested in the phase II KATE2 trial (75,76),
where patients with progressive disease after trastuzumab and
taxane were randomized to receive T-DM1 with or without
atezolizumab and were stratified in two cohorts based on PD-L1
expression. There was no statistical significance in PFS in the
intention-to-treat population (HR=0.82, P=0.3332), but an
exploratory analysis of the PD-L1-positive subgroup (PD-L1 ≥1%)
revealed a numerical PFS benefit in the atezolizumab arm (HR=0.60,
95% CI: 0.32–1.11). 1-year OS also favored not significantly the
atezolizumab group (HR=0.55, 95% CI: 0.22–1.38). However,
generalizability of the results remains uncertain due to the
limited number of patients (n=19).
Pembrolizumab
Combination of pembrolizumab, a programmed cell
death protein-1 (PD-1) inhibitor, with trastuzumab in patients
pretreated with trastuzumab was evaluated in the phase Ib-II
PANACEA trial (77). In
PD-L1-positive tumors, ORR was 15% (6 of 40 patients) and disease
control rate (DCR) 25%, while there were no objective responders
among PD-L1-negative patients. ORR reached 39% and DCR 47% in a
subgroup of PD-L1-positive patients with TILs >5% in the
metastatic lesion, further underlying the need for reliable
biomarkers allowing efficient patient selection.
Anyhow, more data are necessary to define the role
of immune checkpoint inhibitors in HER2 positive metastatic breast
cancer. Several phase I and II trials evaluating immunotherapy with
PD-1/PD-L1 and CTLA4-blockade in HER2 positive breast cancer are
currently ongoing (78).
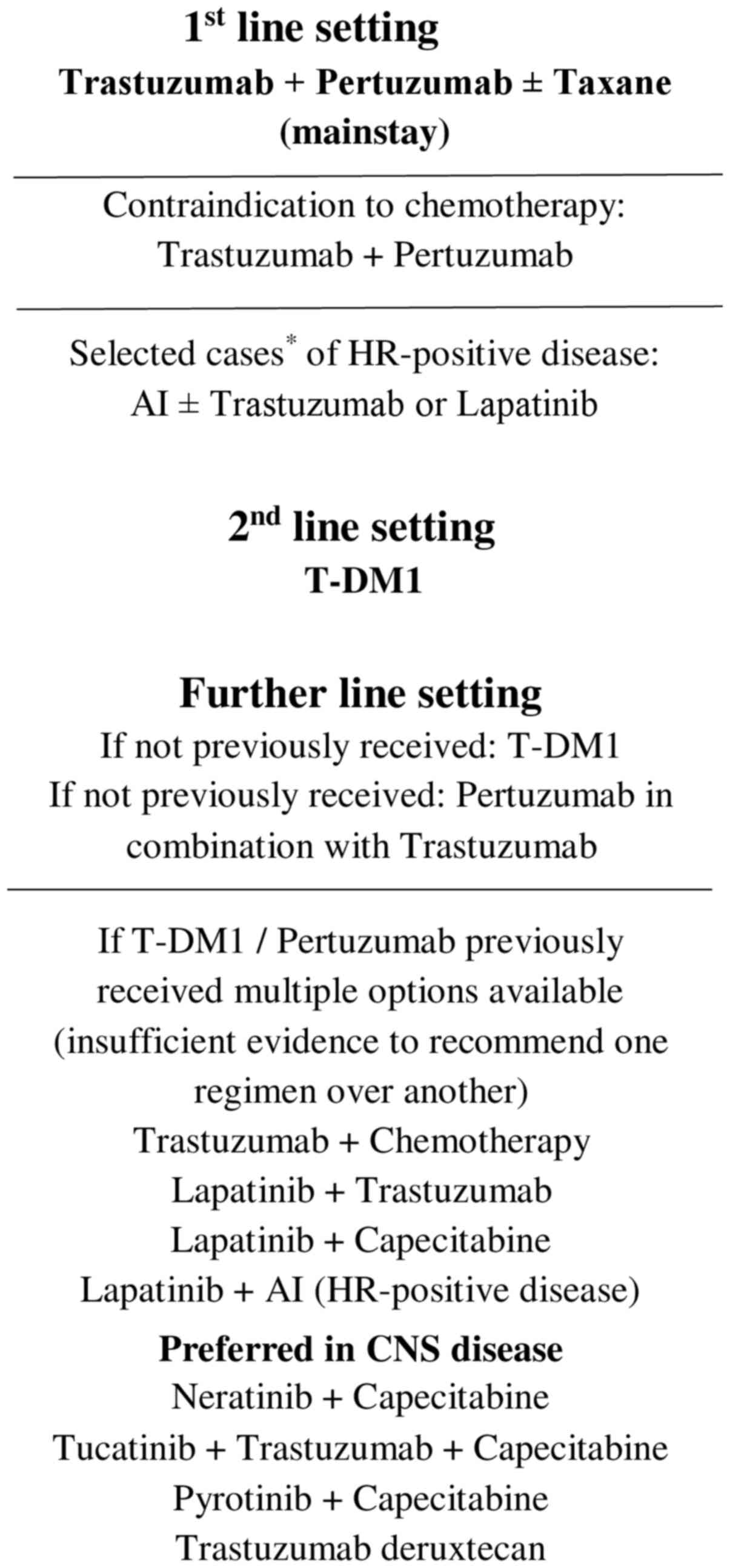
Proposed treatment algorithm
Based on the data presented above, a proposed
treatment algorithm for patients with metastatic HER2-positve
breast cancer is shown in (Fig. 1).
Distinct molecular targets of the different drugs assessed in the
treatment of these patients are presented in (Table I).
 | Table I.Molecular targets of the various
therapeutic agents in metastatic HER2-positive breast cancer |
Table I.
Molecular targets of the various
therapeutic agents in metastatic HER2-positive breast cancer
| Drug Name(s) | Target |
|---|
| Anti-HER2
agents |
|
|
Trastuzumab,
pertuzumaba | HER2 |
|
Margentuximaba | HER2 (greater
affinity to variants of the CD16A receptor) |
|
ZW25b | Two non-overlapping
HER2 epitopes |
|
MCLA-12b | HER2, HER3 |
|
Lapatinibc | EGFR, HER2 |
|
Neratinib,
pyrotinibc | EGFR, HER2, HER3,
HER4 |
|
Tucatinibc | HER2 |
| Antibody-drug
conjugates (trastuzumab + cytotoxic agent) |
|
|
T-DM1 | HER2 +
microtubules |
|
Trastuzumab deruxtecan | HER2 +
topoisomerase 1 |
|
Trastuzumab duocarmazine | HER2 + DNA (alkyl
group binding) |
| CDK4/6 inhibitors
(estrogen signaling pathway) |
|
|
Abemaciclib, palbociclib | CDK 4/6 |
| PI3K/AKT/mTOR
inhibitors |
|
|
Everolimus | mTOR |
|
Buparlisib, alpelisib | PI3K |
| Immunotherapeutic
agents |
|
|
Atezolizumab | PD-L1 |
|
Pembrolizumab | PD-1 |
Conclusion
Prognosis of HER2-positive metastatic breast cancer
has improved drastically since the introduction of HER2-targeted
therapies. However, acquired resistance to treatment is common in
the course of the disease, with the development of brain metastases
remaining a difficult problem in clinical practice. Various novel
agents are currently under investigation either as monotherapy or
in combination with existing regimens with encouraging results in
pretreated patients. Integration of new treatments for specific
subgroups such as patients with HR-positive/HER2-positive tumors or
CNS disease could further improve prognosis. Most importantly,
identification of predictive factors is crucial to better determine
the most appropriate therapeutic approach for different
patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
MM and IPT wrote the manuscript, GG, SI and NKS
critically revised the manuscript and EAK revised the manuscript
and supervised the work. All authors read and approved the final
manuscript. MM and EAK confirm the authenticity of all the
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ADCC
|
antibody-dependent cellular
cytotoxicity
|
|
CDK
|
cyclin dependent kinase
|
|
CNS
|
central nervous system
|
|
CTLA4
|
cytotoxic T-lymphocyte antigen 4
|
|
DCR
|
disease control rate
|
|
EGFR
|
epidermal growth factor receptor
|
|
ER
|
estrogen receptor
|
|
FcR
|
fc-receptor
|
|
FDA
|
Food and Drug Administration
|
|
HER2
|
human epidermal growth factor receptor
2
|
|
HR
|
hormone receptor
|
|
MAPK
|
mitogen-activated protein kinase
|
|
mTOR
|
mechanistic target of rapamycin
|
|
NK
|
natural killer cells
|
|
ORR
|
objective response rate
|
|
OS
|
overall survival
|
|
PD-1
|
programmed cell death protein 1
|
|
PD-L1
|
programmed death-ligand 1
|
|
PFS
|
progression free survival
|
|
PI3K
|
phosphatidylinositol-4,5-biphosphate
3-kinase
|
|
T-DM1
|
ado Trastuzumab emtasine
|
|
TILs
|
tumor-infiltrating lymphocytes
|
|
TKI
|
tyrosine kinase inhibitor
|
|
TMB
|
tumor mutational burden
|
|
TTP
|
time to progression
|
References
|
1
|
Torre LA, Islami F, Siegel RL, Ward EM and
Jemal A: Global cancer in women: Burden and trends. Cancer
Epidemiol Biomarkers Prev. 26:444–457. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Slamon DJ, Clark GM, Wong SG, Levin WJ,
Ullrich A and McGuire WL: Human breast cancer: Correlation of
relapse and survival with amplification of the HER-2/neu oncogene.
Science. 235:177–182. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Burstein HJ: The distinctive nature of
HER2-positive breast cancers. N Engl J Med. 353:1652–1654. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kennecke H, Yerushalmi R, Woods R, Cheang
MC, Voduc D, Speers CH, Nielsen TO and Gelmon K: Metastatic
behavior of breast cancer subtypes. J Clin Oncol. 28:3271–3277.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Harbeck N, Penault-Llorca F, Cortes J,
Gnant M, Houssami N, Poortmans P, Ruddy K, Tsang J and Cardoso F:
Breast cancer. Nat Rev Dis Primers. 5:662019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Iqbal N and Iqbal N: Human epidermal
growth factor receptor 2 (HER2) in cancers: Overexpression and
therapeutic implications. Mol Biol Int. 2014:8527482014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mendes D, Alves C, Afonso N, Cardoso F,
Passos-Coelho JL, Costa L, Andrade S and Batel-Marques F: The
benefit of HER2-targeted therapies on overall survival of patients
with metastatic HER2-positive breast cancer - a systematic review.
Breast Cancer Res. 17:1402015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hudis CA: Trastuzumab - mechanism of
action and use in clinical practice. N Engl J Med. 357:39–51. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vogel CL, Cobleigh MA, Tripathy D, Gutheil
JC, Harris LN, Fehrenbacher L, Slamon DJ, Murphy M, Novotny WF,
Burchmore M, et al: Efficacy and safety of trastuzumab as a single
agent in first-line treatment of HER2-overexpressing metastatic
breast cancer. J Clin Oncol. 20:719–726. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Slamon DJ, Leyland-Jones B, Shak S, Fuchs
H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M,
et al: Use of chemotherapy plus a monoclonal antibody against HER2
for metastatic breast cancer that overexpresses HER2. N Engl J Med.
344:783–792. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Andersson M, Lidbrink E, Bjerre K, Wist E,
Enevoldsen K, Jensen AB, Karlsson P, Tange UB, Sørensen PG, Møller
S, et al: Phase III randomized study comparing docetaxel plus
trastuzumab with vinorelbine plus trastuzumab as first-line therapy
of metastatic or locally advanced human epidermal growth factor
receptor 2-positive breast cancer: The HERNATA study. J Clin Oncol.
29:264–271. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Robert N, Leyland-Jones B, Asmar L, Belt
R, Ilegbodu D, Loesch D, Raju R, Valentine E, Sayre R, Cobleigh M,
et al: Randomized phase III study of trastuzumab, paclitaxel, and
carboplatin compared with trastuzumab and paclitaxel in women with
HER-2-overexpressing metastatic breast cancer. J Clin Oncol.
24:2786–2792. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Valero V, Forbes J, Pegram MD, Pienkowski
T, Eiermann W, von Minckwitz G, Roche H, Martin M, Crown J, Mackey
JR, et al: Multicenter phase III randomized trial comparing
docetaxel and trastuzumab with docetaxel, carboplatin, and
trastuzumab as first-line chemotherapy for patients with
HER2-gene-amplified metastatic breast cancer (BCIRG 007 study): Two
highly active therapeutic regimens. J Clin Oncol. 29:149–156. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Baselga J, Manikhas A, Cortés J, Llombart
A, Roman L, SemiglazovV F, Byakhov M, Lokanatha D, Forenza S,
Goldfarb RH, et al: Phase III trial of nonpegylated liposomal
doxorubicin in combination with trastuzumab and paclitaxel in
HER2-positive metastatic breast cancer. Ann Oncol. 25:592–598.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hamberg P, Bos MM, Braun HJ, Stouthard JM,
van Deijk GA, Erdkamp FL, van der Stelt-Frissen IN, Bontenbal M,
Creemers GJ, Portielje JE, et al Dutch Breast Cancer Trialists'
Group (BOOG), : Randomized phase II study comparing efficacy and
safety of combination-therapy trastuzumab and docetaxel vs.
sequential therapy of trastuzumab followed by docetaxel alone at
progression as first-line chemotherapy in patients with HER2+
metastatic breast cancer: HERTAX trial. Clin Breast Cancer.
11:103–113. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Inoue K, Nakagami K, Mizutani M, Hozumi Y,
Fujiwara Y, Masuda N, Tsukamoto F, Saito M, Miura S, Eguchi K, et
al: Randomized phase III trial of trastuzumab monotherapy followed
by trastuzumab plus docetaxel versus trastuzumab plus docetaxel as
first-line therapy in patients with HER2-positive metastatic breast
cancer: The JO17360 Trial Group. Breast Cancer Res Treat.
119:127–136. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pagani O, Klingbiel D, Ruhstaller T, Nolè
F, Eppenberger S, Oehlschlegel C, Bernhard J, Brauchli P, Hess D,
Mamot C, et al Swiss Group for Clinical Cancer Research (SAKK), :
Do all patients with advanced HER2 positive breast cancer need
upfront-chemo when receiving trastuzumab? Randomized III trial SAKK
22/99. Ann Oncol. 28:305–312. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Baselga J, Cortés J, Kim SB, Im SA, Hegg
R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, et al
CLEOPATRA Study Group, : Pertuzumab plus trastuzumab plus docetaxel
for metastatic breast cancer. N Engl J Med. 366:109–119. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Swain SM, Baselga J, Kim S-B, Ro J,
Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A,
Heeson S, et al CLEOPATRA Study Group, : Pertuzumab, trastuzumab,
and docetaxel in HER2-positive metastatic breast cancer. N Engl J
Med. 372:724–734. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Swain SM, Miles D, Kim SB, Im YH, Im SA,
Semiglazov V, Ciruelos E, Schneeweiss A, Loi S, Monturus E, et al:
Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic
breast cancer (CLEOPATRA): end-of-study results from a
double-blind, randomised, placebo-controlled, phase 3 study. Lancet
Oncol. 21:519–530. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Miles D, Im YH, Fung A, Yoo B, Knott A,
Heeson S, Beattie MS and Swain SM: Effect of docetaxel duration on
clinical outcomes: Exploratory analysis of CLEOPATRA, a phase III
randomized controlled trial. Ann Oncol. 28:2761–2767. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bachelot T, Ciruelos E, Schneeweiss A,
Puglisi F, Peretz-Yablonski T, Bondarenko I, Paluch-Shimon S,
Wardley A, Merot JL, du Toit Y, et al PERUSE investigators, :
Preliminary safety and efficacy of first-line pertuzumab combined
with trastuzumab and taxane therapy for HER2-positive locally
recurrent or metastatic breast cancer (PERUSE). Ann Oncol.
30:766–773. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Perez EA, López-Vega JM, Petit T, Zamagni
C, Easton V, Kamber J, Restuccia E and Andersson M: Safety and
efficacy of vinorelbine in combination with pertuzumab and
trastuzumab for first-line treatment of patients with HER2-positive
locally advanced or metastatic breast cancer: VELVET Cohort 1 final
results. Breast Cancer Res. 18:1262016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Inoue K, Ninomiya J, Saito T, Okubo K,
Nakakuma T, Yamada H, Kimizuka K and Higuchi T; SBCCSG-36
investigators, : Eribulin, trastuzumab, and pertuzumab as
first-line therapy for patients with HER2-positive metastatic
breast cancer: A phase II, multicenter, collaborative, open-label,
single-arm clinical trial. Invest New Drugs. 37:538–547.
2019.Erratum in: Invest New Drugs 37: 592–593, 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Urruticoechea A, Rizwanullah M, Im SA,
Ruiz ACS, Láng I, Tomasello G, Douthwaite H, Badovinac Crnjevic T,
Heeson S, Eng-Wong J, et al: Randomized phase III trial of
trastuzumab plus capecitabine with or without pertuzumab in
patients with human epidermal growth factor receptor 2-positive
metastatic breast cancer who experienced disease progression during
or after trastuzumab-based therapy. J Clin Oncol. 35:3030–3038.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Urruticoechea A, Rizwanullah M, Im SA,
Sánchez Ruiz AC, Lang I, Tomasello G, Douthwaite H, Badovinac
Crnjevic T, Heeson S, Eng-Wong J, et al: Final overall survival
(OS) analysis of PHEREXA: A randomized phase III trial of
trastuzumab (H) + capecitabine (X) ± pertuzumab (P) in patients
with HER2-positive metastatic breast cancer (MBC) who experienced
disease progression during or after H-based therapy. J Clin Oncol.
36 (Suppl 15):10132018. View Article : Google Scholar
|
|
27
|
Lewis Phillips GD, Li G, Dugger DL,
Crocker LM, Parsons KL, Mai E, Blättler WA, Lambert JM, Chari RV,
Lutz RJ, et al: Targeting HER2-positive breast cancer with
trastuzumab-DM1, an antibody-cytotoxic drug conjugate. Cancer Res.
68:9280–9290. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Krop IE, Kim SB, González-Martín A,
LoRusso PM, Ferrero JM, Smitt M, Yu R, Leung AC and Wildiers H;
TH3RESA study collaborators, : Trastuzumab emtansine versus
treatment of physician's choice for pretreated HER2-positive
advanced breast cancer (TH3RESA): A randomised, open-label, phase 3
trial. Lancet Oncol. 15:689–699. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Krop IE, Kim SB, Martin AG, LoRusso PM,
Ferrero JM, Badovinac-Crnjevic T, Hoersch S, Smitt M and Wildiers
H: Trastuzumab emtansine versus treatment of physician's choice in
patients with previously treated HER2-positive metastatic breast
cancer (TH3RESA): Final overall survival results from a randomised
open-label phase 3 trial. Lancet Oncol. 18:743–754. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Verma S, Miles D, Gianni L, Krop IE,
Welslau M, Baselga J, Pegram M, Oh DY, Diéras V, Guardino E, et al
EMILIA Study Group, : Trastuzumab emtansine for HER2-positive
advanced breast cancer. N Engl J Med. 367:1783–1791. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Diéras V, Miles D, Verma S, Pegram M,
Welslau M, Baselga J, Krop IE, Blackwell K, Hoersch S, Xu J, et al:
Trastuzumab emtansine versus capecitabine plus lapatinib in
patients with previously treated HER2-positive advanced breast
cancer (EMILIA): A descriptive analysis of final overall survival
results from a randomised, open-label, phase 3 trial. Lancet Oncol.
18:732–742. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Perez EA, Barrios C, Eiermann W, Toi M, Im
YH, Conte P, Martin M, Pienkowski T, Pivot X, Burris H III, et al:
Trastuzumab emtansine with or without pertuzumab versus trastuzumab
plus taxane for human epidermal growth factor receptor 2-positive,
advanced breast cancer: Primary results From the Phase III MARIANNE
Study. J Clin Oncol. 35:141–148. 2017.Erratum in: J Clin Oncol 35:
2342, 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Perez EA, Barrios C, Eiermann W, Toi M, Im
YH, Conte P, Martin M, Pienkowski T, Pivot XB, Burris HA III, et
al: Trastuzumab emtansine with or without pertuzumab versus
trastuzumab with taxane for human epidermal growth factor receptor
2-positive advanced breast cancer: Final results from MARIANNE.
Cancer. 125:3974–3984. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Roskoski R Jr: Small molecule inhibitors
targeting the EGFR/ErbB family of protein-tyrosine kinases in human
cancers. Pharmacol Res. 139:395–411. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Cameron D, Casey M, Press M, Lindquist D,
Pienkowski T, Romieu CG, Chan S, Jagiello-Gruszfeld A, Kaufman B,
Crown J, et al: A phase III randomized comparison of lapatinib plus
capecitabine versus capecitabine alone in women with advanced
breast cancer that has progressed on trastuzumab: Updated efficacy
and biomarker analyses. Breast Cancer Res Treat. 112:533–543. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gelmon KA, Boyle FM, Kaufman B, Huntsman
DG, Manikhas A, Di Leo A, Martin M, Schwartzberg LS, Lemieux J,
Aparicio S, et al: Lapatinib or trastuzumab plus taxane therapy for
human epidermal growth factor receptor 2-positive advanced breast
cancer: Final results of NCIC CTG MA.31. J Clin Oncol.
33:1574–1583. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Blackwell KL, Burstein HJ, Storniolo AM,
Rugo HS, Sledge G, Aktan G, Ellis C, Florance A, Vukelja S,
Bischoff J, et al: Overall survival benefit with lapatinib in
combination with trastuzumab for patients with human epidermal
growth factor receptor 2-positive metastatic breast cancer: Final
results from the EGF104900 Study. J Clin Oncol. 30:2585–2592. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Prat A and Baselga J: The role of hormonal
therapy in the management of hormonal-receptor-positive breast
cancer with co-expression of HER2. Nat Clin Pract Oncol. 5:531–542.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Montagna E and Colleoni M: Hormonal
treatment combined with targeted therapies in endocrine-responsive
and HER2-positive metastatic breast cancer. Ther Adv Med Oncol.
11:17588359198941052019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kaufman B, Mackey JR, Clemens MR, Bapsy
PP, Vaid A, Wardley A, Tjulandin S, Jahn M, Lehle M, Feyereislova
A, et al: Trastuzumab plus anastrozole versus anastrozole alone for
the treatment of postmenopausal women with human epidermal growth
factor receptor 2-positive, hormone receptor-positive metastatic
breast cancer: Results from the randomized phase III TAnDEM study.
J Clin Oncol. 27:5529–5537. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Johnston S, Pippen J Jr, Pivot X,
Lichinitser M, Sadeghi S, Dieras V, Gomez HL, Romieu G, Manikhas A,
Kennedy MJ, et al: Lapatinib combined with letrozole versus
letrozole and placebo as first-line therapy for postmenopausal
hormone receptor-positive metastatic breast cancer. J Clin Oncol.
27:5538–5546. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Huober J, Fasching PA, Barsoum M,
Petruzelka L, Wallwiener D, Thomssen C, Reimer T, Paepke S, Azim
HA, Ragosch V, et al: Higher efficacy of letrozole in combination
with trastuzumab compared to letrozole monotherapy as first-line
treatment in patients with HER2-positive, hormone-receptor-positive
metastatic breast cancer - results of the eLEcTRA trial. Breast.
21:27–33. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Rimawi M, Ferrero J-M, de la
Haba-Rodriguez J, Poole C, De Placido S, Osborne CK, Hegg R, Easton
V, Wohlfarth C and Arpino G; PERTAIN Study Group, : First-line
trastuzumab plus an aromatase inhibitor, with or without
pertuzumab, in human epidermal growth factor receptor 2-positive
and hormone receptor-positive metastatic or locally advanced breast
cancer (PERTAIN): A randomized, open-label phase II trial. J Clin
Oncol. 36:2826–2835. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Johnston SRD, Hegg R, Im SA, Park IH,
Burdaeva O, Kurteva G, Press MF, Tjulandin S, Iwata H, Simon SD, et
al: Phase III, randomized study of dual human epidermal growth
factor receptor 2 (HER2) blockade with lapatinib plus trastuzumab
in combination with an aromatase inhibitor in postmenopausal women
with HER2-positive, hormone receptor-positive metastatic breast
cancer: ALTERNATIVE. J Clin Oncol. 36:741–748. 2018.Retraction in:
J Clin Oncol 39: 95, 2021. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Saura C, Oliveira M, Feng Y, Dai M-S,
Hurvitz SA, Kim SB, Moy B, Delaloge S, Gradishar WJ, Masuda N, et
al: Neratinib plus capecitabine versus lapatinib plus capecitabine
in HER2-positive metastatic breast cancer previously treated with
≥2 HER2-directed regimens: Phase III NALA trial. J Clin Oncol.
38:3138–3149. 2019. View Article : Google Scholar
|
|
46
|
Awada A, Colomer R, Inoue K, Bondarenko I,
Badwe RA, Demetriou G, Lee SC, Mehta AO, Kim SB, Bachelot T, et al:
Neratinib plus paclitaxel vs trastuzumab plus paclitaxel in
previously untreated metastatic ERBB2-positive breast cancer. The
NEfERT-T randomized clinical trial. JAMA Oncol. 2:1557–1564. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Freedman RA, Gelman RS, Wefel JS, Melisko
ME, Hess KR, Connolly RM, Van Poznak CH, Niravath PA, Puhalla SL,
Ibrahim N, et al: Translational Breast Cancer Research Consortium
(TBCRC) 022: A phase II trial of neratinib for patients with human
epidermal growth factor receptor 2-positive breast cancer and brain
metastases. J Clin Oncol. 34:945–952. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Freedman RA, Gelman RS, Anders CK, Melisko
ME, Parsons HA, Cropp AM, Silvestri K, Cotter CM, Componeschi KP,
Marte JM, et al Translational Breast Cancer Research Consortium, :
TBCRC 022: A phase II trial of neratinib and capecitabine for
patients with human epidermal growth factor receptor 2-positive
breast cancer and brain metastases. J Clin Oncol. 37:1081–1089.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ma F, Ouyang Q, Li W, Jiang Z, Tong Z, Liu
Y, Li H, Yu S, Feng J, Wang S, et al: Pyrotinib or lapatinib
combined with capecitabine in HER2-positive metastatic breast
cancer with prior taxanes, anthracyclines, and/or trastuzumab: A
randomized, phase II study. J Clin Oncol. 37:2610–2619. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Xu B, Yan M, Ma F, Hu XC, Feng FJ, Ouyang
Q, Tong Z, Li H, Zhang Q, Sun T, et al: Pyrotinib or lapatinib plus
capecitabine for HER2+ metastatic breast cancer (PHOEBE): a
randomized phase III trial. J Clin Oncol. 38 (Suppl 15):10032020.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Jiang Z, Yan M, Hu X, Zhang Q, Ouyang Q,
Feng J, Yin Y, Sun T, Tong Z, Wang X, et al: Pyrotinib combined
with capecitabine in women with HER2+ metastatic breast cancer
previously treated with trastuzumab and taxanes: A randomized phase
III study. J Clin Oncol. 37 (Suppl 15):10012019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Blair HA: Pyrotinib: First global
approval. Drugs. 78:1751–1755. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Murthy RK, Loi S, Okines A, Paplomata E,
Hamilton E, Hurvitz SA, Lin NU, Borges V, Abramson V, Anders C, et
al: Tucatinib, trastuzumab and capecitabine for HER2-positive
metastatic breast cancer. N Engl J Med. 382:597–609. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Lin NU, Borges V, Anders C, Murthy RK,
Paplomata E, Hamilton E, Hurvitz S, Loi S, Okines A, Abramson V, et
al: Intracranial efficacy and survival with tucatinib plus
trastuzumab and capecitabine for previously treated HER2-positive
breast cancer with brain metastases in the HER2CLIMB trial. J Clin
Oncol. 38:2610–2619. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Modi S, Saura C, Yamashita T, Park YH, Kim
SB, Tamura K, Andre F, Iwata H, Ito Y, Tsurutani J, et al
DESTINY-Breast01 Investigators, : Trastuzumab Deruxtecan in
previously treated HER2-positive breast cancer. N Engl J Med.
382:610–621. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Jerusalem G, Park YH, Yamashita T, Hurvitz
SA, Chen S, Cathcart J, Lee C and Perrin C: CNS metastases in
HER2-positive metastatic breast cancer treated with trastuzumab
deruxtecan: DESTINY-Breast01 subgroup analyses. Ann Oncol.
31:Abstract nr. 1380. 2020. View Article : Google Scholar
|
|
57
|
Banerji U, van Herpen CML, Saura C,
Thistlethwaite F, Lord S, Moreno V, Macpherson IR, Boni V, Rolfo C,
de Vries EGE, et al: Trastuzumab duocarmazine in locally advanced
and metastatic solid tumours and HER2-expressing breast cancer: A
phase 1 dose-escalation and dose-expansion study. Lancet Oncol.
20:1124–1135. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Rinnerthaler G, Gampenrieder SP and Greil
R: HER2 directed antibody-drug-conjugates beyond T-DM1 in breast
cancer. Int J Mol Sci. 20:1152019. View Article : Google Scholar
|
|
59
|
Dolcetti R: Predictive value of FcR
polymorphisms. A further step on the long and winding road to
application. JAMA Oncol. 3:342–343. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Rugo HS, Im SA, Cardoso F, Cortes J,
Curigliano G, Pegram MD, Musolino A, Bachelot T, Wright GS, De
Laurentiis M, et al: Phase III SOPHIA study of margetuximab +
chemotherapy vs trastuzumab + chemotherapy in patients with HER2+
metastatic breast cancer after prior anti-HER2 therapies: second
interim overall survival analysis. Cancer Res. 80:Abstract Nr.
GS1-02. 2019.
|
|
61
|
Meric-Bernstam F, Hanna D, Beeram M, Lee
K, Kang Y, Chaves J, Lee J, Goodwin R, Vaklavas C, Oh D, et al:
Safety, anti-tumor activity, and biomarker results of the
HER2-targeted bispecific antibody ZW25 in HER2-expressing solid
tumors. Ann Oncol. 30 (Suppl 5):v159–v193. 2019. View Article : Google Scholar
|
|
62
|
Alsina M, Boni V, Schellens J, Moreno V,
Bol K, Westendorp M, Sirulnik LA, Tabernero J and Calvo E:
First-in-human phase 1/2 study of MCLA-128, a full length IgG1
bispecific antibody targeting HER2 and HER3: Final phase 1 data and
preliminary activity in HER2+ metastatic breast cancer (MBC). J
Clin Oncol. 35 (Suppl 15):25222017. View Article : Google Scholar
|
|
63
|
Schettini F, Giudici F, Giuliano M,
Cristofanilli M, Arpino G, Del Mastro L, Puglisi F, De Placido S,
Paris I, De Placido P, et al: Overal survival of
CDK4/6-inhibitors-based treatments in clinically relevant subgroups
of metastatic breast cancer: Systematic review and meta-analysis. J
Natl Cancer Inst. 112:1089–1097. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tolaney SM, Wardley AM, Zambelli S, Hilton
JF, Troso-Sandoval TA, Ricci F, Im SA, Kim SB, Johnston SR, Chan A,
et al: Abemaciclib plus trastuzumab with or without fulvestrant
versus trastuzumab plus standard-of-care chemotherapy in women with
hormone receptor-positive, HER2-positive advanced breast cancer
(monarcHER): A randomised, open-label, phase 2 trial. Lancet Oncol.
21:763–775. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ciruelos E, Villagrasa P, Paré L, Oliveira
M, Pernas S, Cortés J, Soberino J, Adamo B, Vazquez S, Martínez N,
et al: SOLTI-1303 PATRICIA phase II trial (STAGE 1) - Palbociclib
and trastuzumab in postmenopausal patients with HER2-positive
metastatic breast cancer. Cancer Res. 79 (Suppl 4):Abstract nr
PD3-03. 2019.
|
|
66
|
Metzger O, Mandrekar S, Loibl S, Mundhenke
C, Seiler S, Valagussa P, Lim E, Tripathy D, Winer EP, Huang C, et
al: PATINA: A randomized, open label, phase III trial to evaluate
the efficacy and safety of palbociclib + anti-HER2 therapy +
endocrine therapy (ET) vs. anti-HER2 therapy + ET after induction
treatment for hormone receptor positive (HR+)/HER2-positive
metastatic breast cancer (MBC). Cancer Res. 79 (Suppl 4):Abstract
nr OT3-02-07. 2019.
|
|
67
|
Wang Q, Liu P, Spangle JM, Von T, Roberts
TM, Lin NU, Krop IE, Winer EP and Zhao JJ: PI3K-p110α mediates
resistance to HER2-targeted therapy in HER2+, PTEN-deficient breast
cancers. Oncogene. 35:3607–3612. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Mezni E, Vicier C, Guerin M, Sabatier R,
Bertucci F and Gonçalves A: New therapeutics in HER2-positive
advanced breast cancer: Towards a change in clinical practices?
Cancers (Basel). 12:15732020. View Article : Google Scholar
|
|
69
|
André F, O'Regan R, Ozguroglu M, Toi M, Xu
B, Jerusalem G, Masuda N, Wilks S, Arena F, Isaacs C, et al:
Everolimus for women with trastuzumab-resistant, HER2-positive,
advanced breast cancer (BOLERO-3): A randomised, double-blind,
placebo-controlled phase 3 trial. Lancet Oncol. 15:580–591. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Hurvitz SA, André F, Jiang Z, Shao Z, Mano
MS, Neciosup SP, Tseng LM, Zhang Q, Shen K, Liu D, et al:
Combination of everolimus with trastuzumab plus paclitaxel as
first-line treatment for patients with HER2-positive advanced
breast cancer (BOLERO-1): A phase 3, randomised, double-blind,
multicentre trial. Lancet Oncol. 16:816–829. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
André F, Hurvitz S, Fasolo A, Tseng LM,
Jerusalem G, Wilks S, O'Regan R, Isaacs C, Toi M, Burris H, et al:
Molecular alterations and everolimus efficacy in human epidermal
growth factor receptor 2-overexpressing metastatic breast cancers:
Combined exploratory biomarker analysis From BOLERO-1 and BOLERO-3.
J Clin Oncol. 34:2115–2124. 2016.Erratum in: J Clin Oncol 37: 357,
2019. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Guerin M, Rezai K, Isambert N, Campone M,
Autret A, Pakradouni J, Provansal M, Camerlo J, Sabatier R,
Bertucci F, et al: PIKHER2: A phase IB study evaluating buparlisib
in combination with lapatinib in trastuzumab-resistant
HER2-positive advanced breast cancer. Eur J Cancer. 86:28–36. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Jain S, Shah AN, Santa-Maria CA,
Siziopikou K, Rademaker A, Helenowski I, Cristofanilli M and
Gradishar WJ: Phase I study of alpelisib (BYL-719) and trastuzumab
emtansine (T-DM1) in HER2-positive metastatic breast cancer (MBC)
after trastuzumab and taxane therapy. Breast Cancer Res Treat.
171:371–381. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Viale G, Morganti S, Ferraro E, Zagami P,
Marra A and Curigliano G: What therapies are on the horizon for
HER2 positive breast cancer? Expert Rev Anticancer Ther.
19:811–822. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Emens LA, Esteva F, Beresford M, Saura C,
De Laurentiis M, Kim SB, Im SA, Patre M, Wang Y, Mani A, et al:
Results from KATE2, a randomized phase 2 study of atezolizumab
(atezo)+trastuzumab emtasine (T-DM1) vs placebo (pbo)+T-DM1 in
previously treated HER2+ advanced breast cancer (BC). Cancer Res.
79 (Suppl 4):Abstract nr PD3-01. 2019.
|
|
76
|
Emens L, Esteva F, Beresford M, Saura C,
De Laurentiis M, Kim SB, Im SA, Wang Y, Mani A, Shah J, et al:
Overall survival (OS) in KATE2, a phase 2 study of programmed death
ligand 1 (PD-L1) inhibitor atezolizumab (atezo)+trastuzumab
emtasine (T-DM1) vs placebo (pbo)+T-DM1 in previously treated HER2+
advanced breast cancer (BC). Ann Oncol. 30 (Suppl 5):v104–v142.
2019. View Article : Google Scholar
|
|
77
|
Loi S, Giobbie-Hurder A, Gombos A,
Bachelot T, Hui R, Curigliano G, Campone M, Biganzoli L, Bonnefoi
H, Jerusalem G, et al International Breast Cancer Study Group and
the Breast International Group, : Pembrolizumab plus trastuzumab in
trastuzumab-resistant, advanced, HER2-positive breast cancer
(PANACEA): A single-arm, multicentre, phase 1b-2 trial. Lancet
Oncol. 20:371–382. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Ayoub NM, Al-Shami KM and Yaghan RJ:
Immunotherapy for HER2-positive breast cancer: Recent advances and
combination therapeutic approaches. Breast Cancer (Dove Med Press).
11:53–69. 2019.PubMed/NCBI
|