Introduction
Oral squamous cell carcinoma (OSCC) is the most
frequent type of head and neck squamous cell carcinoma (HNSCC),
with >500,000 new cases annually worldwide (1). OSCC is more likely to invade local
tissues and spread to the lymph nodes, and has a mortality rate of
~50% within five years (2). Despite
the increasing knowledge into the etiology of OSCC and the advances
in chemotherapy, radiation and surgery, there has been little
improvement in the relative survival time in patients with OSCC in
recent decades (2). Smoking and
drinking are major risk factors for OSCC (3). In addition, infection with human
papillomavirus (HPV) has been identified as another risk factor for
developing carcinoma in the oral cavity (4).
HPV is a circular double-stranded DNA molecule, ~8
kb and over 100 genotypes have been reported (5). The high-risk types, HPV-16 and 18 have
been associated with 90% of uterine cervical cancers (6–8). The HPV
genome is composed of early and late genes, which encode the early
proteins, E1 to E7, and the late proteins L1 and L2. Among these
genes, E6 and E7 have critical functions in malignant
transformation of squamous cells (9). E6 binds to TP53 and inactivates its
function by ubiquitin-dependent degradation (10). E7 manipulates and degrades the
retinoblastoma tumor suppressor protein (Rb), resulting in the
activation of the transcription factor E2F, which enhances the
expression of the cyclin-dependent kinase inhibitor 2A (CDKN2A;
p16) (11). The expression of the
p16 protein has been used as a surrogate marker for HPV infection
in HNSCC (12).
The relevance of HPV infection in cervical cancer
and HNSCC is well-known. Patients with HNSCC and are HPV-positive
have an improved prognosis compared with those who are HPV-negative
(13). According to a systematic
review on HPV detection among 4,852 HNSCC cases worldwide, the
overall prevalence rate of HPV was 34.5% (14). HPV-16 and 18 are the most common
genotypes in HPV-positive OSCC, with a frequency rate of 32.4%
(204/630) and 11.3% (71/630), respectively (15). Another systematic review on HPV
infection, in patients with OSCC, reported that the prevalence rate
of HPV was 55.5% (76/137) and the most common genotype was HPV-16
(16).
However, the association between HPV infection and
OSCC remains unclear. For example, the prevalence of HPV in
patients with OSCC varies in different regions worldwide (17,18). In
addition, a wide range of HPV prevalence was observed among
patients from Japan (0-78%) (19–23). The
present study aimed to determine the prevalence of HPV and clarify
the association between HPV-16 infection, p16 protein expression
and clinicopathological characteristics of OSCC.
Materials and methods
Patients and samples
Tissue samples were obtained from 100 patients with
OSCC, including basaloid squamous cell carcinoma (BSCC), who
underwent surgical resection at the Department of Oral and
Maxillofacial Surgery at Ehime University Hospital (Ehime, Japan)
between April 2004 and March 2013. Tumor staging was assessed
according to the Union for International Cancer Control TNM
Classification of Malignant Tumors 7th Edition and histological
grading was performed according to the World Health Organization
criteria for OSCC (24). The
Institutional Review Board of Ehime University Hospital (Ehime,
Japan) approved the present study.
Immunohistochemistry
Surgically resected OSCC specimens were fixed in 10%
phosphate-buffered formalin for 24 h at room temperature and
embedded in paraffin. A series of 4-µm thick sections were prepared
from each sample. Immunohistochemical (IHC) staining was performed
using the avidin-biotin-peroxidase complex method. Briefly, the
sections were deparaffinized and heated at 121°C in an autoclave
for 20 min in 10 mM citrate buffer (pH 6.0) to regenerate epitopes.
The sections were incubated with 0.3% hydrogen peroxide in
distilled water for 5 min at room temperature to block endogenous
peroxidase activity. The sections were then incubated overnight at
4°C with a specific mouse monoclonal antibody to anti-human p16
(cat. no. 550834; diluted 1:50; BD Pharmingen; BD Biosciences).
After washing with TBS+Tween-20 (TBS-T; Sigma-Aldrich; Merck KGaA),
the sections were overlaid with biotinylated anti-mouse antibody
(Maravai LifeSciences) at room temperature for 60 min, washed with
TBS-T, then labeled with streptavidin-peroxidase complex (Maravai
LifeSciences). The sections were subsequently counterstained with
hematoxylin for 10 sec at room temperature, dehydrated with a
series of graded ethanols (75, 95, 100 and 100%) for 5 min each at
room temperature, treated with xylene and enclosed in synthetic
resin. IHC staining was observed at ×40 and ×100 magnifications
under a light microscope (Nikon Corporation). Positive expression
of p16 protein was determined as when >70% of tumor cells showed
strong and diffuse nuclear and cytoplasmic staining.
RNA extraction and RT-qPCR
Total RNA was extracted using ISOGEN (Nippon Gene)
from lysing the tissues, after homogenization, with a TissueLyser
(Qiagen), according to the manufacturer's protocol.
The presence of HPV-16E6 mRNA in the tissues was
determined using RT-qPCR and the TaqMan®
RNA-to-CT™ 1-Step kit (Thermo Fisher Scientific, Inc.).
PCR amplification was performed in a 10-µl final reaction mixture
containing 0.25 µl TaqMan® RT Enzyme Mix (40X), 5 µl
TaqMan® RT-PCR Mix (2X), 0.4 µl each forward and reverse
primers (10 µM each), 0.2 µl TaqMan® probe (10 µM) and 1
µl total RNA (100 ng/µl). The following thermocycling conditions
were used: RT at 48°C for 15 min, then initial denaturation at 95°C
for 10 min, followed by 40 cycles at 95°C for 15 min and 60°C for 1
min. Oropharyngeal cancer tissues from biopsy materials obtained
from patients with tonsil cancer treated in the Department of Oral
and Maxillofacial Surgery at Ehime University Hospital were used as
the positive control. Written informed patient consent was
obtained.
The expression of HPV-18E6 mRNA was detected using
RT-qPCR and the SYBR® system. PCR amplification was
performed in a 10-µl final reaction mixture containing 5 µl 2X One
Step SYBR® RT-PCR Buffer 4, 0.4 µl
PrimeScript® One Step Enzyme Mix 2, 0.2 µl ROX reference
Dye II (50X), 2.6 µl RNase-free distilled water (all from Takara
Bio, Inc.), 0.4 µl forward and reverse primers (10 µM each) and 1
µl total RNA (100 ng/µl). The following thermocycling conditions
were used: RT at 45°C for 5 min and 95°C for 10 sec, followed by 40
cycles at 95°C for 5 sec and 55°C for 30 sec.
Amplification and detection were performed using the
ViiA™ 7 real-time PCR system (Thermo Fisher Scientific, Inc.).
Hydroxymethylbilane synthase (HMBS) was used as an internal
control. To confirm the amplicon size, the PCR products were
electrophoresed on 3% agarose gels (Bio-Rad Laboratories), stained
with ethidium bromide for 5 min at room temperature, and visualized
under an ultraviolet transilluminator (FAS-III; Toyobo Life
Science).
The following primers and TaqMan® probe
were used: HPV-16E6 forward, 5′-GAATGTGTGTACAAGCAACAG-3′, reverse,
5′-TGGATTCCCATCTCTATATACTATGCAT-3′ and TaqMan® probe,
5′-CGACGTGAGGTATATGACTTTGCTTTTCGG-3′ (25); HPV-18E6 forward,
5′-CAGAAACCGTTGAATCCAGCA-3′ and reverse,
5′-TTTCTCTGCGTCGTTGGAGTC-3′ (25)
and HMBS forward, 5′-CATGCAGGCTACCATCCATGTC-3′ and reverse,
5′-GTTACGAGCAGTGATGCCTACCAA-3′.
Genomic DNA extraction and exonuclease
V-qPCR
Genomic DNA was extracted from formalin fixed
paraffin embedded (FFPE) OSCC tissues using a GeneRead DNA FFPE kit
(Qiagen GmbH). Exonuclease V (ExoV; New England BioLabs, Inc.)
digestion was performed, as previously described (26). For detecting HPV-16E6 DNA, qPCR
amplification was conducted in a 10-µl final reaction mixture
containing 5 µl 2X PowerTrack™ SYBR™ Green Master Mix (Thermo
Fisher Scientific, Inc.), 0.5 µl each forward and reverse primers
(8 µM each), 3 µl nuclease-free distilled water and 1 µl genomic
DNA (10 ng/µl) with or without ExoV digestion. The following
thermocycling conditions were used: Enzyme activation at 95°C for 2
min, followed by 40 cycles at 95°C for 15 sec and 60°C for 1 min.
Amplification and detection was performed using a ViiA™ 7 real-time
PCR system (Thermo Fisher Scientific, Inc.). Human ribosomal 18S
DNA (rDNA) was used as an internal control. To confirm the amplicon
size, the PCR products were electrophoresed and visualized using an
Agilent 2100 Bioanalyzer with the DNA 1000 kit (Agilent
Technologies). The following primers were used: HPV-16E6 forward,
5′-GAGAACTGCAATGTTTCAGGACC-3′ and reverse,
5′-TGTATAGTTTGCAGCTCTGTGC-3′; rDNA forward, 5′-GCAATTCCCCATGAACG-3′
and reverse, 5′-GGGACTTAATCAACGCAAGC-3′ (26).
Statistical analysis
χ2 or Fisher's exact tests was used to
determine significant differences between 2 groups. The
Kaplan-Meier method was applied for survival analysis after
follow-up for 36 months. Differences in patient survival were
determined using the log-rank test. P<0.05 was considered to
indicate a statistically significant difference. Statistical
analyses were performed using GraphPad Prism software (v5.04;
GraphPad Software, Inc.).
Results
Characteristics of the patients
The 100 OSCC cases included 54 men and 46 women,
ranging in age from 39 to 93 years (median, 70.3 years). The
primary tumor was located in the tongue (n=36), mandibular gingiva
(n=31), maxillary gingiva (n=13), floor of the mouth (n=9), buccal
mucosa (n=9), or lower lip (n=2). All the patients were
histopathologically diagnosed with squamous cell carcinoma,
including BSCC (n=1).
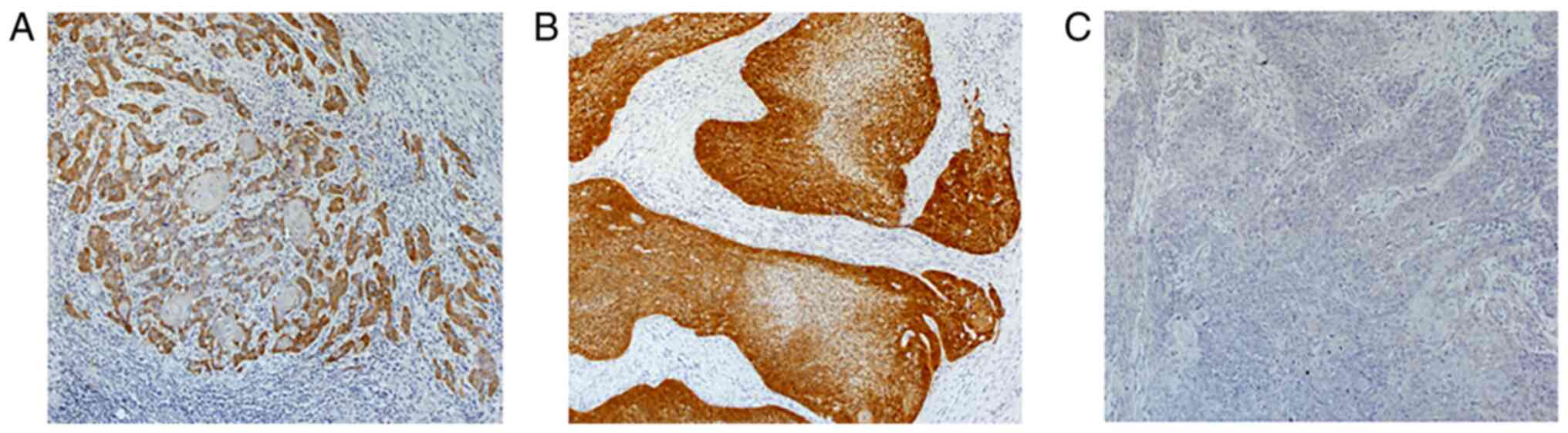
Immunohistochemistry staining of p16
protein
Positive expression of p16 protein was observed in
10 out of 100 OSCC cases (10%). Most p16-positive cases showed
strong and diffuse staining in the nucleus and the cytoplasm of the
tumor cells (Fig. 1A and B). The
association between p16 immunohistochemistry expression in the
tumors from 100 patients with OSCC and their clinicopathological
parameters was investigated; however, the differences were not
significant (Table I). Furthermore,
following the analysis between p16 expression and survival using
the Kaplan-Meier method, no significant association between overall
and disease-free survival times was found (Fig. S1).
 | Table I.Association between p16 status and
the characteristics of patients with oral squamous cell
carcinoma. |
Table I.
Association between p16 status and
the characteristics of patients with oral squamous cell
carcinoma.
| Characteristic | p16-positive
(n=10) | p16-negative
(n=90) | P-value |
|---|
| Median age,
years | 71 | 70 | 0.383 |
| Sex |
|
|
|
|
Male | 7 | 47 | 0.335 |
|
Female | 3 | 43 |
|
| Primary site |
|
| 0.185 |
|
Tongue | 1 | 35 |
|
|
Maxillary gingiva | 2 | 11 |
|
|
Mandibular gingiva | 3 | 28 |
|
| Floor
of mouth | 2 | 7 |
|
| Buccal
mucosa | 1 | 8 |
|
|
Lip | 1 | 1 |
|
| Histological
grading |
|
| 0.465 |
| G1 | 7 | 56 |
|
| G2 | 3 | 22 |
|
| G3 | 0 | 12 |
|
| T-status |
|
| 0.077 |
| ½ | 4 | 63 |
|
| ¾ | 6 | 27 |
|
| N-status |
|
| 0.515 |
| 0 | 5 | 55 |
|
|
1–3 | 5 | 35 |
|
| Clinical stage |
|
| 0.504 |
|
I/II | 3 | 42 |
|
|
III/IV | 7 | 48 |
|
|
Recurrence/metastasis |
|
| >0.999 |
| No | 6 | 56 |
|
|
Yes | 4 | 34 |
|
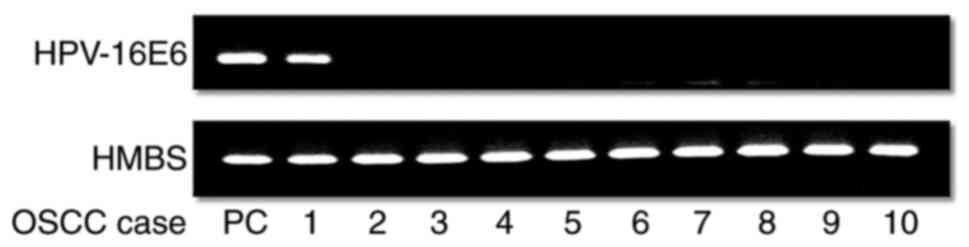
Prevalence of HPV-16 in all patients
with OSCC
To clarify HPV-16 infection, the expression level of
HPV-16E6 mRNA in 100 OSCC cases was determined using RT-qPCR.
HPV-16E6 mRNA expression was only detected in one case (1%), which
was also positive for p16 expression. PCR products of HPV-16E6 and
HMBS were visualized using agarose gel electrophoresis (Fig. 2). HPV-18E6 mRNA expression was
investigated in p16 positive OSCC tissues using RT-qPCR; however,
it was not detected (data not shown). Furthermore, the possibility
of persistent or silent infection with HPV-16 was investigated
using genomic DNA derived from p16 positive OSCC cases using qPCR.
HPV-16E6 DNA was detected in 3 out of 10 cases (Cases 1, 3 and 10;
Fig. S2A). One of these cases
expressed HPV-16E6 mRNA (Case 1), but the other cases did not (Case
3 and 10). Subsequently, genomic DNA was digested by ExoV, which
preserved nicked and supercoiled DNAs but degraded linear DNAs,
followed by qPCR for the detection of HPV-16E6 DNA. HPV-16E6 DNA
was ExoV-resistant, suggesting that the circular episome was
observed only in the HPV-16E6 DNA and mRNA positive case (Case 1;
Fig. S2B). Since neither HPV-16E6
DNA nor RNA was detected in 7 of the 10 cases of p16 overexpression
(Case 2, 4, 5, 6, 7, 8 and 9), the false-positive rate of HPV-16
infection was 70%. Finally, only the HPV-16E6 DNA- and
mRNA-positive case (Case 1) was histopathologically determined as
BSCC, which is a rare variant of OSCC. The other cases (Case 3 and
10) were determined to be keratinized squamous cell carcinomas.
Discussion
HPV has been recognized as a possible pathogen of
oral cancer (27–29). HPV has been associated with cancer of
the uterus and cervix and was found in most cases (6–8).
However, its role in oral carcinogenesis is still unknown (30–33). In
oropharyngeal HNSCC, HPV-positive tumors may have different
clinical and biological functions, with improved overall survival
time and favorable prognosis (34).
It has also been associated with therapeutic response in patients
with HNSCC of the oropharynx (35).
Another study showed that cases positive for HPV-16 had lower
recurrence rates compared with that for their negative
counterparts, indicating an association between HPV-16 infection
and a good prognosis in OSCC (36).
In contrast, HPV-16 infection reportedly enhanced the risk of
distant metastasis and poor survival in patients with advanced OSCC
(37). In the present study, the
prevalence of HPV-16 in patients with OSCC was only 1%. Therefore,
the association between HPV infection and prognosis could not be
evaluated.
Several techniques have been used to detect HPV.
Examples include PCR, an HPV genotyping test, morphology, in
situ hybridization and p16 immunohistochemistry. HPV detection
methods, such as morphology, in situ hybridization and p16
immunohistochemistry lack sensitivity and specificity, as well as
the ability to detect high-risk HPV types. Therefore, PCR was
considered the most sensitive method (38,39). The
prevalence of HPV infection varied from 0% (19,40) to
100% (41), even in oral cavity
cases. In the present study, p16 protein expression, which was used
as a surrogate marker of HPV infection, was detected in 10% of
cases, and the rate of HPV-16 infection with E6 expression was only
1% in 100 OSCC cases. The one case of HPV-16E6 mRNA positive
expression also had expression of the p16 protein. To investigate
the association between HPV-16 infection and p16 expression, the
presence of HPV-16E6 DNA in genomic DNA samples, which were also
p16 positive was determined and HPV-16E6 DNA was found not only in
the E6 mRNA positive case, but also in additional 2 cases without
E6 expression. The expression of p16 was also 70% HPV-16
false-positive, indicating the low reliability of the surrogate
marker of HPV infection in OSCC. A previous study showed 100% HPV
false-positive results in mobile tongue cancer (19). It suggested that although p16 protein
expression was a biomarker for cervical or tonsillar cancer arising
from carcinogenic HPV infection, it was not applicable for tongue
cancer (19). Furthermore, another
study indicated that p16 expression was not a suitable surrogate
marker of HPV infection in oral lesions and HPV-16 infection was
associated with BSCC (42). In fact,
only one HPV-16E6 mRNA-positive case was histopathologically
determined to be BSCC in the present study. However, both HPV-16E6
DNA positive cases, without E6 expression, were keratinized
squamous cell carcinomas.
Most cervical and oropharyngeal cancers show high
expression of E6 and E7; however, OSCC has a lower positive rate of
E6 and E7 mRNA expression compared with that for HPV DNA positive
rate (43). We have hypothesized
that there are two types of HPV DNA positive OSCCs. One is
HPV-related OSCC, which is a silent infection with no expression of
E6 and E7, but is caused by the integration of HPV DNA into the
genome. The other is non-keratinized OSCC with E6 and E7
expression, in which HPV DNA is actively infected as a nuclear
episome and/or genome integration.
In summary, the results from the present study
indicated that there were few OSCC cases due to HPV-16 infection.
The expression of p16 protein was not an appropriate surrogate
marker for HPV-16 infection in OSCC. In addition, HPV-16 DNA may
also be detected in p16 negative OSCC cases. As the number of
HPV-16 DNA positive cases was extremely low in the present study,
further investigation is required to examine the presence of
episomal and integrated HPV DNA and the expression of E6 and E7
mRNA, regardless of p16 expression, using the large number of fresh
frozen OSCC tissues.
Supplementary Material
Supporting Data
Acknowledgements
The authors would like to thank Ms Yumiko Fukuda
(Department of Oral and Maxillofacial Surgery, Ehime University
Graduate School of Medicine, Ehime, Japan) for providing technical
assistance.
Funding
This study was supported by a Grant-in-Aid for
Scientific Research (B) from the Japan Society for the Promotion of
Science (grant no. 16H05543).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NT and KN confirm the authenticity of all the raw
data. KN, NK and DU advised and supervised the study. KN designed
the experiments. NT and ST performed the experiments. NT, HG, NK
and DU analyzed the data. NT and KN wrote the manuscript. All
authors read and approved the final version of manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institute
Research Ethics Committee of the Ehime University Hospital
(approval number, 1607005) and written informed consent was
provided by all the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
HPV
|
human papillomavirus
|
|
OSCC
|
oral squamous cell carcinoma
|
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gupta S, Kong W, Peng Y, Miao Q and
Mackillop WJ: Temporal trends in the incidence and survival of
cancers of the upper aerodigestive tract in Ontario and the United
States. Int J Cancer. 125:2159–2165. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Blot WJ, McLaughlin JK, Winn DM, Austin
DF, Greenberg RS, Preston-Martin S, Bernstein L, Schoenberg JB,
Stemhagen A and Fraumeni JF Jr: Smoking and drinking in relation to
oral and pharyngeal cancer. Cancer Res. 48:3282–3287.
1988.PubMed/NCBI
|
|
4
|
Leemans CR, Braakhuis BJ and Brakenhoff
RH: The molecular biology of head and neck cancer. Nat Rev Cancer.
11:9–22. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dell G and Gaston K: Human
papillomaviruses and their role in cervical cancer. Cell Mol Life
Sci. 58:1923–1942. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
zur Hausen H: Papillomaviruses and cancer:
From basic studies to clinical application. Nat Rev Cancer.
2:342–350. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Clifford GM, Smith JS, Plummer M, Muñoz N
and Franceschi S: Human papillomavirus types in invasive cervical
cancer worldwide: A meta-analysis. Br J Cancer. 88:63–73. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bosch FX and de Sanjosé S: The
epidemiology of human papillomavirus infection and cervical cancer.
Dis Markers. 23:213–227. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Münger K, Baldwin A, Edwards KM, Hayakawa
H, Nguyen CL, Owens M, Grace M and Huh K: Mechanisms of human
papillomavirus-induced oncogenesis. J Virol. 78:11451–11460. 2004.
View Article : Google Scholar
|
|
10
|
Narisawa-Saito M and Kiyono T: Basic
mechanisms of high-risk human papillomavirus-induced
carcinogenesis: Roles of E6 and E7 proteins. Cancer Sci.
98:1505–1511. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
McLaughlin-Drubin ME and Münger K: The
human papillomavirus E7 oncoprotein. Virology. 384:335–344. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
El-Naggar Ak and Westra WH: p16 expression
as a surrogate marker for HPV-related oropharyngeal carcinoma: A
guide for interpretative relevance and consistency. Head Neck.
34:459–461. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Deng Z, Hasegawa M, Yamashita Y, Matayoshi
S, Kiyuna A, Agena S, Uehara T, Maeda H and Suzuki M: Prognostic
value of human papillomavirus and squamous cell carcinoma antigen
in head and neck squamous cell carcinoma. Cancer Sci.
103:2127–2134. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Termine N, Panzarella V, Falaschini S,
Russo A, Matranga D, Lo Muzio L and Campisi G: HPV in oral squamous
cell carcinoma vs. head and neck squamous cell carcinoma biopsies:
A meta-analysis (1988–2007). Ann Oncol. 19:1681–1690. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sritippho T, Chotjumlong P and Iamaroon A:
Roles of Human Papillomaviruses and p16 in Oral Cancer. Asian Pac J
Cancer Prev. 16:6193–6200. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hobbs CG, Sterne JA, Bailey M, Heyderman
RS, Birchall MA and Thomas SJ: Human papillomavirus and head and
neck cancer: A systematic review and meta-analysis. Clin
Otolaryngol. 31:259–266. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Castillo A, Koriyama C, Higashi M, Anwar
M, Bukhari MH, Carrascal E, Mancilla L, Okumura H, Matsumoto M,
Sugihara K, et al: Human papillomavirus in upper digestive tract
tumors from three countries. World J Gastroenterol. 17:5295–5304.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Krüger M, Pabst AM, Walter C, Sagheb K,
Günther C, Blatt S, Weise K, Al-Nawas B and Ziebart T: The
prevalence of human papilloma virus (HPV) infections in oral
squamous cell carcinomas: A retrospective analysis of 88 patients
and literature overview. J Craniomaxillofac Surg. 42:1506–1514.
2014. View Article : Google Scholar
|
|
19
|
Kabeya M, Furuta R, Kawabata K, Takahashi
S and Ishikawa Y: Prevalence of human papillomavirus in mobile
tongue cancer with particular reference to young patients. Cancer
Sci. 103:161–168. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shima K, Kobayashi I, Saito I, Kiyoshima
T, Matsuo K, Ozeki S, Ohishi M and Sakai H: Incidence of human
papillomavirus 16 and 18 infection and p53 mutation in patients
with oral squamous cell carcinoma in Japan. Br J Oral Maxillofac
Surg. 38:445–450. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sugiyama M, Bhawal UK, Kawamura M, Ishioka
Y, Shigeishi H, Higashikawa K and Kamata N: Human papillomavirus-16
in oral squamous cell carcinoma: Clinical correlates and 5-year
survival. Br J Oral Maxillofac Surg. 45:116–122. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rushatamukayanunt P, Morita K, Matsukawa
S, Harada H, Shimamoto H, Tomioka H and Omura K: Lack of
association between high-risk human papillomaviruses and oral
squamous cell carcinoma in young japanese patients. Asian Pac J
Cancer Prev. 15:4135–4141. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ono K, Sugahara K, Nomura T, Takano N,
Shibahara T and Katakura A: Multiple HPV subtypes infection in
Japanese oral Squamous cell carcinoma. J Oral Maxillofac Surg Med
Pathol. 26:128–132. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
International Union Against Cancer (UICC),
. TNM classification of malignant tumours. 7th edition. Sobin LH,
Gospodarowicz MK and Wittekind C: Willey-Blackwell; Hoboken: pp.
25–29. 2009
|
|
25
|
Yamakawa-Kakuta Y, Kawanata H, Doi Y,
Fujimori T and Imai Y: Does the expression of HPV16/18 E6/E7 in
head and neck squamous cell carcinomas relate to their
clinicopathological characteristics? Int J Oncol. 35:983–988.
2009.PubMed/NCBI
|
|
26
|
Myers JE, Guidry JT, Scott ML, Zwolinska
K, Raikhy G, Prasai K, Bienkowska-Haba M, Bodily JM, Sapp MJ and
Scott RS: Detecting episomal or integrated human papillomavirus 16
DNA using an exonuclease V-qPCR-based assay. Virology. 537:149–156.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Anaya-Saavedra G, Ramírez-Amador V,
Irigoyen-Camacho ME, García-Cuellar CM, Guido-Jiménez M,
Méndez-Martínez R and García-Carrancá A: High association of human
papillomavirus infection with oral cancer: A case-control study.
Arch Med Res. 39:189–197. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Iamaroon A, Pattanaporn K, Pongsiriwet S,
Wanachantararak S, Prapayasatok S, Jittidecharaks S, Chitapanarux I
and Lorvidhaya V: Analysis of 587 cases of oral squamous cell
carcinoma in northern Thailand with a focus on young people. Int J
Oral Maxillofac Surg. 33:84–88. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lee SY, Cho NH, Choi EC, Baek SJ, Kim WS,
Shin DH and Kim SH: Relevance of human papilloma virus (HPV)
infection to carcinogenesis of oral tongue cancer. Int J Oral
Maxillofac Surg. 39:678–683. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Doorbar J: The papillomavirus life cycle.
J Clin Virol. 32 Suppl 1:S7–S15. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ibieta BR, Lizano M, Fras-Mendivil M,
Barrera JL, Carrillo A, Ma Ruz-Godoy L and Mohar A: Human papilloma
virus in oral squamous cell carcinoma in a Mexican population. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod. 99:311–315. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Llamas-Martínez S, Esparza-Gómez G,
Campo-Trapero J, Cancela-Rodríguez P, Bascones-Martínez A,
Moreno-López LA, García-Núñez JA and Cerero-Lapiedra R: Genotypic
determination by PCR-RFLP of human papillomavirus in normal oral
mucosa, oral leukoplakia and oral squamous cell carcinoma samples
in Madrid (Spain). Anticancer Res 28 (6A). 3733–3741. 2008.
|
|
33
|
Uobe K, Masuno K, Fang YR, Li LJ, Wen YM,
Ueda Y and Tanaka A: Detection of HPV in Japanese and Chinese oral
carcinomas by in situ PCR. Oral Oncol. 37:146–152. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Marur S, D'Souza G, Westra WH and
Forastiere AA: HPV-associated head and neck cancer: A virus-related
cancer epidemic. Lancet Oncol. 11:781–789. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Fakhry C, Westra WH, Li S, Cmelak A, Ridge
JA, Pinto H, Forastiere A and Gillison ML: Improved survival of
patients with human papillomavirus-positive head and neck squamous
cell carcinoma in a prospective clinical trial. J Natl Cancer Inst.
100:261–269. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Elango KJ, Suresh A, Erode EM,
Subhadradevi L, Ravindran HK, Iyer SK, Iyer SK and Kuriakose MA:
Role of human papilloma virus in oral tongue squamous cell
carcinoma. Asian Pac J Cancer Prev. 12:889–896. 2011.PubMed/NCBI
|
|
37
|
Lee LA, Huang CG, Liao CT, Lee LY, Hsueh
C, Chen TC, Lin CY, Fan KH, Wang HM, Huang SF, et al: Human
papillomavirus-16 infection in advanced oral cavity cancer patients
is related to an increased risk of distant metastases and poor
survival. PLoS One. 7:e407672012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Schlecht NF, Brandwein-Gensler M, Nuovo
GJ, Li M, Dunne A, Kawachi N, Smith RV, Burk RD and Prystowsky MB:
A comparison of clinically utilized human papillomavirus detection
methods in head and neck cancer. Mod Pathol. 24:1295–1305. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Pannone G, Rodolico V, Santoro A, Lo Muzio
L, Franco R, Botti G, Aquino G, Pedicillo MC, Cagiano S, Campisi G,
et al: Evaluation of a combined triple method to detect causative
HPV in oral and oropharyngeal squamous cell carcinomas: p16
immunohistochemistry, consensus PCR HPV-DNA, and in situ
hybridization. Infect Agent Cancer. 7:42012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
de Spíndula-Filho JV, da Cruz AD,
Oton-Leite AF, Batista AC, Leles CR, de Cássia Gonçalves Alencar R,
Saddi VA and Mendonça EF: Oral squamous cell carcinoma versus oral
verrucous carcinoma: An approach to cellular proliferation and
negative relation to human papillomavirus (HPV). Tumor Biol.
32:409–416. 2011. View Article : Google Scholar
|
|
41
|
Koyama K, Uobe K and Tanaka A: Highly
sensitivity detection of HPV-DNA in paraffin sections of human oral
carcinomas. J Oral Pathol Med. 36:18–24. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Friedrich RE, Sperber C, Jäkel T, Röser K
and Löning T: Basaloid lesions of oral squamous epithelial cells
and their association with HPV infection and P16 expression.
Anticancer Res. 30:1605–1612. 2010.PubMed/NCBI
|
|
43
|
Ndiaye C, Mena M, Alemany L, Arbyn M,
Castellsagué X, Laporte L, Bosch FX, de Sanjose S and Trottier H:
HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck
cancers: A systematic review and meta-analysis. Lancet Oncol.
15:1319–1331. 2014. View Article : Google Scholar : PubMed/NCBI
|