Introduction
Radiotherapy (RT) is used to manage cervical cancer,
either postoperatively or as a primary treatment (1), and major improvements in definitive RT
have improved survival rates over the past 15–20 years (2). Pelvic insufficiency fracture (PIF) is a
late complication of the therapy (3). According to a meta-analysis by Sapienza
et al (4), the overall
incidence of PIF is between 10–18%, and the most common site for
PIF is the sacrum. PIF can lead to intractable pain and limited
mobility, which can seriously impact the quality of life of
cervical cancer survivors (5). Risk
factors associated with cervical cancer include age, postmenopausal
period, low body weight and osteoporosis (5–14).
Recently, intensity-modulated radiation therapy (IMRT) has been
introduced to reduce acute and chronic gastrointestinal disorders
(15). However, the most effective
method in reducing PIF remains unclear.
Considering the increased number of cervical cancer
survivors (16), it is important to
clarify what factors increase the risk of PIF after RT for patients
with cervical cancer, and detect PIF in the early phase before
patients develop any symptoms. Most reports on PIF have used
computed tomography (CT) and magnetic resonance imaging (MRI) as
inspection methods (5–10,12–14,17–21).
According to Lapina and Tiškevičius (22), the sensitivity and specificity in PIF
diagnosis are 100 and 95.3% for MRI and 74.6 and 89.7% for CT,
respectively. Recently, positron emission tomography (PET) is
attracting great interest as an imaging test for the follow-up of
cervical cancer recurrence (23).
However, to the best of our knowledge, only a few reports have used
PET (5,11,19,21), and
PET/MRI is yet to be investigated (4). The present study aimed to identify risk
factors for PIF and investigate its incidence rate. In addition,
the usefulness of PET/MRI in PIF diagnosis was assessed.
Materials and methods
Patient characteristics
The present study investigated 149 patients with
cervical cancer who received definitive or adjuvant RT with/without
concurrent chemotherapy between January 2013 and December 2018, and
were followed up for more than one month after RT at Kobe
University Hospital. Data collection ended in May 2020. The median
follow-up period was 32 months (range, 1–87 months), and the median
age of all patients was 66 years (age range, 34–90 years). The
histopathological type was squamous cell carcinoma (SCC) in 121
cases (81.2%), adenocarcinoma in 26 cases (17.4%), adenosquamous in
one case (0.7%) and clear cell carcinoma in one case (0.7%). The
median body mass index (BMI) was 21 (range, 14–40). A total of 27
cases (18.1%) were in The International Federation of Gynecology
and Obstetrics (FIGO) stage (24)
was I, 62 cases in stage II (41.6%), 40 cases in stage III (26.8%)
and 20 cases in stage IV (13.4%). A total of 123 patients (82.6%)
received RT as a definitive treatment, 26 (17.4%) received RT as
postoperative adjuvant therapy, and 110 (73.8%) received concurrent
chemoradiotherapy. Table I presents
patient characteristics, according to the presence or absence of
PIF. Notably, no significant differences were observed between both
groups.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | Fracture (+)
(n=31) | Fracture (−)
(n=118) | P-value |
|---|
| Median age (range),
years | 69 (44–87) | 66 (34–90) | 0.0727 |
| Median age of
menopause (range), years | 50 (40–57) | 50 (40–60) | 0.3720 |
| Menopausal
status |
|
| 0.2938 |
|
Postmenopause | 28 (90.3%) | 94 (79.7%) |
|
|
Premenopause | 2 (6.5%) | 20 (16.9%) |
|
|
Unknown | 1 (3.2%) | 4 (3.4%) |
|
| Body mass index,
kg/m2 | 20.9
(16.8–34.8) | 21.0
(13.7–40.3) | 0.5858 |
| Parity | 2 (0–5) | 2 (0–6) | 0.4134 |
| Medical
history |
|
|
|
|
Diabetes mellitus | 2 (6.5%) | 15 (12.7%) | 0.5265 |
|
Rheumatoid arthritis | 0 (0.0%) | 4 (3.4%) | 0.5804 |
|
Osteoporosis | 3 (9.7%) | 14 (11.9%) | 1 |
| Hormone replacement
therapy | 0 (0.0%) | 10 (8.5%) | 0.1224 |
| Histopathological
type |
|
| 0.1571 |
|
Squamous cell carcinoma | 27 (87.1%) | 94 (79.7%) |
|
|
Adenocarcinoma | 3 (9.7%) | 23 (19.5%) |
|
|
Adenosquamous | 1 (3.2%) | 0 (0.0%) |
|
| Clear
cell carcinoma | 0 (0.0%) | 1 (0.8%) |
|
| FIGO stage |
|
| 0.0552 |
| I | 2 (6.5%) | 25 (21.2%) |
|
| II | 14 (45.2%) | 48 (40.7%) |
|
|
III | 13 (41.9%) | 27 (22.9%) |
|
| IV | 2 (6.5%) | 18 (15.3%) |
|
| Treatment |
|
| 0.2129 |
|
Adjuvant CCRT | 0 (0.0%) | 12 (10.2%) |
|
|
Adjuvant RT | 2 (6.5%) | 12 (10.2%) |
|
|
Definitive CCRT | 22 (71.0%) | 76 (64.4%) |
|
|
Definitive RT | 7 (22.6%) | 18 (15.3%) |
|
| ICBT |
|
| 0.2009 |
|
Yes | 28 (90.3%) | 94 (79.7%) |
|
| No | 3 (9.7%) | 24 (20.3%) |
|
| Lymph node
boost |
|
| 1 |
|
Yes | 11 (35.5%) | 43 (36.4%) |
|
| No | 20 (64.5%) | 75 (63.6%) |
|
| IMRT |
|
| 0.1069 |
|
Yes | 2 (6.5%) | 23 (19.5%) |
|
| No | 29 (93.5%) | 95 (80.5%) |
|
| PET/CT |
|
| 0.1561 |
|
Yes | 13 (41.9%) | 68 (57.6%) |
|
| No | 18 (58.1%) | 50 (42.4%) |
|
| PET/MRI |
|
| 0.6859 |
|
Yes | 15 (48.4%) | 51 (43.2%) |
|
| No | 16 (51.6%) | 67 (56.8%) |
|
The inclusion criteria were as follows: Patients
whose medical records and prognosis could be obtained from medical
records, and patients who had a definite diagnosis of cervical
cancer and were followed up for at least one month after the end of
radiotherapy. The exclusion criteria were as follows: Patients who
were offered to not participate in this study based on publicly
available information, and patients participating in or planning to
participate in clinical studies involving drug therapy
interventions.
Treatment
For definitive RT, external beam RT (EBRT) was
performed using the four-field box technique, and intracavitary
brachytherapy (ICBT) was subsequently performed using a remote
after-loading system, in combination with EBRT, using the central
shield by anteroposterior/posteroanterior field technique at 10 MV
photons. The upper limit of the standard irradiation field was the
upper edge of the 5th lumbar vertebra, and the lower limit was at
least 3 cm below the lower edge of the obturator foramen or the
lower edge of the vaginal infiltration. The outer side of the
anterior-posterior irradiation field was 1.5–2 cm outside the inner
edge of the pelvis, and the anterior edge of the lateral
irradiation field was ~0.5 cm in front of the anterior pubic
symphysis. A total dose of EBRT (TrueBeam™; Varian Medical Systems)
at 50.4 Gy (range, 40.0–50.4 Gy) and ICBT (Micro Selectron™;
Nucletron BV) at 24 Gy (range, 18–30 Gy) was administered. For
postoperative adjuvant RT, IMRT (TrueBeam™, Varian Medical Systems)
was performed with a total dose of 50.4 Gy (range, 50.4–60.0 Gy). A
total dose of 10.0 Gy (range, 3.6–16.2 Gy) lymph node boost
(TrueBeam™; Varian Medical Systems) was given to 54 patients
(36.2%) with positive lymph node metastasis. For concurrent
chemoradiotherapy, cisplatin (Cisplatin Maruko™; Yakult Honsha Co.,
Ltd.) was administered once a week for 5–6 cycles at 40
mg/m2.
Follow-up and diagnostic criteria of
PIF
For cervical cancer, follow-up started 1 month after
the end of radiation therapy, and in principle, it was continued
for 5 years in the outpatient department. Follow-up was conducted
every 1 to 3 months in the 1st and 2nd years, every 3 to 6 months
in the 3rd year, and every 6 months in the 4 to 5th years. Patients
underwent imaging tests twice a year for the first 2 years and then
annually thereafter. CT, MRI, PET/CT or PET/MRI were used as
follow-up imaging methods. At the discretion of the two
radiologists and two gynecologists, a recurrent check or follow-up
was performed, and a CT, PET/CT or PET/MRI was selected. In
addition, an MRI was selected depending on the symptoms, such as
buttock or lower back pains. During the median follow-up period,
121 patients (81.2%) underwent imaging with PET, while 66 patients
(44.3%) underwent imaging with PET/MRI. Patients who received
multiple types of tests for the recurrence check or follow-up were
excluded from the analysis.
The diagnostic criteria for PIF was as follows: CT
for a fracture line or osteosclerosis without osteolytic changes,
MRI for T1 hypointensity and T2 hyperintensity without a soft
tissue mass, and PET for mild and diffuse fluorodeoxyglucose (FDG)
accumulation. All images were diagnosed by two radiologists at Kobe
University Hospital.
Statistical analysis
Statistical analysis was performed using R version
4.0.0 (https://cran.r-project.org/bin/windows/base/). For
each factor in the fracture (n=31) and non-fracture groups (n=118),
χ2 or Fisher's exact tests were used to assess the
differences in frequency. The Mann-Whitney U test was used to
compare differences between continuous variables. Each exposure or
each predictor was assessed using the log-rank test as univariate
analysis. P<0.05 was considered to indicate a statistically
significant difference. This observational study complied with the
STROBE guidelines (25).
Results
Incidence
Among the 149 patients investigated in the present
study, 31 (20.8%) developed PIF, and the median time for developing
the condition was 17 months (range, 2–47 months). The median age of
the fracture group was 69 years, of which 28 patients (90.3%) were
postmenopausal. The median age of the non-fracture group was 66
years, of which 94 patients (79.7%) were postmenopausal. Notable,
no significant differences in age and postmenopausal status were
observed between the two groups. The median BMI was 20.9 in the
fracture group and 21.0 in the non-fracture group, and the median
number of deliveries was two in both the fracture and non-fracture
groups, respectively. With regards to medical history, two patients
(6.5%) had diabetes, while three (9.7%) had osteoporosis in the
fracture group, whereas 15 patients (12.7%) had diabetes, four
(3.4%) had rheumatic arthritis and 14 (11.9%) had osteoporosis in
the non-fracture group. There were no significant differences in
medical history between the two groups. No patients received
hormone replacement therapy (HRT) in the fracture group, while 10
patients received HRT in the non-fracture group. The
histopathological types were 27 cases (87.1%) of SCC, three (9.7%)
of adenocarcinoma and one (3.2%) of adenosquamous in the fracture
group, compared with 94 cases (79.7%) of SCC, 23 (19.5%) of
adenocarcinoma and one (0.8%) of clear cell carcinoma in the
non-fracture group. There were no significant differences in
histopathological types between the two groups. A total of two
cases (6.5%) were in FIGO stage I, 14 (45.2%) in stage II, 13
(41.9%) in stage III and two (6.5%) in stage IV in the fracture
group. Conversely, 25 cases (21.2%) were in FIGO stage I, 48
(40.7%) in stage II, 27 (22.9%) in stage III and 18 (15.3%) in
stage IV in the non-fracture group. These results suggest that the
FIGO stage was slightly higher in the fracture group compared with
the non-fracture group (P=0.0552). In the facture group, no
patients received adjuvant concurrent chemoradiotherapy (CCRT), two
(6.5%) received adjuvant RT, 22 (71.0%) received definitive CCRT
and seven (22.6%) received definitive RT. Conversely, in the
non-fracture group, 12 patients (10.2%) received adjuvant CCRT, 12
(10.2%) received adjuvant RT, 76 (64.4%) received definitive CCRT
and 18 (15.3%) received definitive RT. A total of 28 patients
(90.3%) received ICBT, 11 (35.5%) received a lymph node boost and
two (6.5%) received IMRT in the fracture group, whereas 94 patients
(79.7%) received ICBT, 43 (36.4%) received a lymph node boost and
23 (19.5%) received IMRT in the non-fracture group. Notably, no
significant differences in the type of treatment were observed
between the two groups. A total of 13 patients (41.9%) had PET/CT
as the imaging test, while 15 (48.4%) had PET/MRI in the fracture
group. Conversely, 68 patients (57.6%) had PET/CT as the imaging
test, while 51 (43.2%) had PET/MRI in the non-fracture group. There
were no significant differences in image examination between the
two groups (Table I).
Sites
Table II presents
the result of 31 patients who were diagnosed with PIF, 17 of which
(54.8%) were asymptomatic. A total of 28 patients has their
fracture site in the sacrum, nine in the pubis and four in the
lumber spinal vertebrae. A total of 11 patients (35.5%) had
multiple fractures (Table II),
while 17 (54.8%) were asymptomatic. Furthermore, 10 patients
(32.3%) were diagnosed with PIF on CT, one (3.2%) on MRI, 10
(32.3%) on PET/CT and 10 (32.3%) on PET/MRI. In addition, 12/17
patients (70.6%) with asymptomatic PIF were diagnosed by PET-CT or
PET-MRI.
 | Table II.Characteristics of PIF. |
Table II.
Characteristics of PIF.
| Patient | Age, years | Time, months | Site | Symptom | Diagnostic
medium | PET/CT
(SUVmax) | PET/MRI
(SUVmax) |
|---|
| 1 | 72 | 32 | Sacrum | Asymptomatic | CT | NA | NA |
| 2 | 66 | 28 | Sacrum | Buttocks pain | CT | NA | NA |
| 3 | 80 | 12 | Lumber spinal
vertebrae | Buttocks pain | PET/CT | 3.68 | NA |
| 4 | 82 | 38 | Sacrum | Buttocks pain | CT | NA | NA |
| 5 | 81 | 33 | Sacrumpubis | Buttocks pain | CT | NA | NA |
| 6 | 76 | 25 | Sacrum | Asymptomatic | PET/CT | 4.52 | NA |
| 7 | 87 | 12 | Sacrum | Buttocks pain | MRI | NA | NA |
| 8 | 61 | 15 | Sacrum | Buttocks pain | PET/CT | 4.81 | NA |
| 9 | 66 | 34 | Sacrumpubis | Asymptomatic | PET/CT | 4.30 | NA |
| 10 | 46 | 36 | Sacrumpubis | Buttocks pain | PET/MRI | NA | 5.96 |
| 11 | 67 | 4 | Sacrum | Asymptomatic | PET/CT | 4.11 | NA |
| 12 | 67 | 47 | Sacrumpubis | Asymptomatic | PET/CT | 4.81 | NA |
| 13 | 51 | 22 | Sacrum | Asymptomatic | CT | NA | NA |
| 14 | 58 | 14 | Sacrum | Buttocks pain | CT | NA | NA |
| 15 | 69 | 7 | Sacrum | Buttocks pain | PET/MRI | NA | 4.06 |
| 16 | 79 | 9 | Sacrumlumber spinal
vertebrae | Asymptomatic | PET/MRI | NA | 4.02 |
| 17 | 82 | 2 | Lumber spinal
vertebrae | Buttocks pain | CT | NA | NA |
| 18 | 60 | 32 | Sacrum | Buttocks pain | PET/MRI | NA | 1.21 |
| 19 | 66 | 29 | Sacrum | Asymptomatic | PET/MRI | NA | 3.92 |
| 20 | 69 | 13 | Sacrum | Asymptomatic | PET/MRI | NA | 5.23 |
| 21 | 70 | 29 | Sacrumpubis | Asymptomatic | CT | NA | NA |
| 22 | 75 | 15 | Sacrum | Asymptomatic | PET/MRI | NA | 2.50 |
| 23 | 52 | 18 | Sacrum | Asymptomatic | PET/CT | 3.04 | NA |
| 24 | 74 | 7 | Lumber spinal
vertebrae | Asymptomatic | PET/CT | 4.27 | NA |
| 25 | 73 | 23 | Sacrumpubis | Buttocks pain | PET/CT | 4.33 | NA |
| 26 | 44 | 17 | Sacrum | Asymptomatic | PET/MRI | NA | 3.39 |
| 27 | 80 | 8 | Sacrumpubis | Asymptomatic | CT | NA | NA |
| 28 | 62 | 21 | Sacrumpubis | Buttocks pain | PET/MRI | NA | 4.07 |
| 29 | 76 | 6 | Sacrumpubis | Buttocks pain | PET/CT | 4.34 | NA |
| 30 | 67 | 8 | Sacrumthoracic
spinal vertebrae | Asymptomatic | CT | NA | NA |
| 31 | 56 | 8 | Sacrum | Asymptomatic | PET/MRI | NA | 3.88 |
Analysis of risk factors
The associations between PIF, patient
characteristics and treatment related factors were assessed
(Table III). Univariate analysis
using the log-rank test demonstrated that age (≥60 years) was
significantly associated with PIF (P<0.05). However, BMI <21,
postmenopausal status, parity ≥3, SCC, FIGO stage ≥III, ICBT, a
lymph node boost, IMRT and definitive RT were not significant risk
factors for developing PIF.
 | Table III.Univariate analysis of risk factors
for PIF. |
Table III.
Univariate analysis of risk factors
for PIF.
| Variable | 95% CI | P-value |
|---|
| Age, years
(≥60) | 47-NA | <0.05 |
| BMI,
kg/m2 (<21) | NA-NA | 0.505 |
| Postmenopausal
status | NA-NA | 0.199 |
| Parity (≥3) | 33-NA | 0.289 |
| SCC | NA-NA | 0.622 |
| FIGO stage
(≥III) | 33-NA | 0.0732 |
| ICBT | 36-NA | 0.438 |
| Lymph node
boost | 36-NA | 0.188 |
| IMRT | NA-NA | 0.125 |
| Definitive
radiotherapy | NA-NA | 0.0816 |
Characteristics of PET/CT and PET/MRI
in PIF diagnosis
The association between PIF diagnosis and the method
of fracture detection, using either PET/CT or PET/MRI, was
assessed. The median maximum standardized uptake value
(SUVmax) of PIF sites on PET/CT was 4.32 (range,
3.04–4.81) and that on PET/MRI was 3.97 (range, 1.21–5.96), which
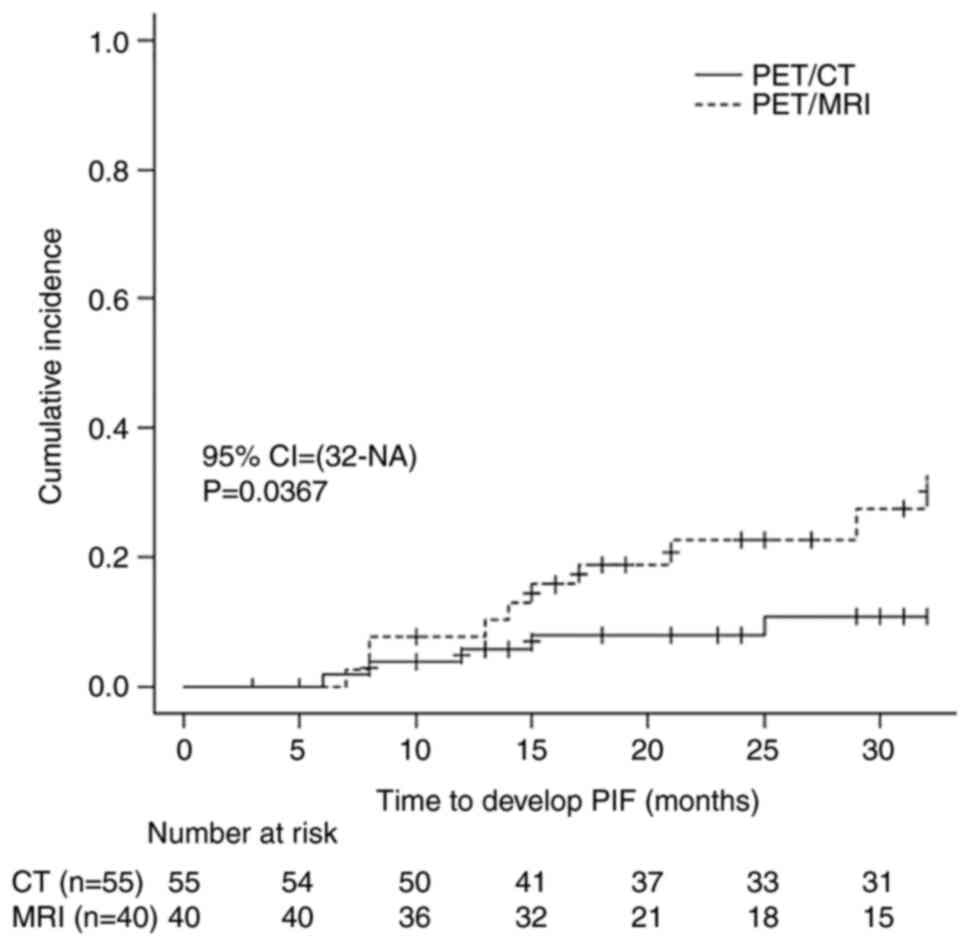
was not statistically significant (P=0.162; Table II). Kaplan-Meier analysis was
performed to compare patients who underwent image follow-up with
PET/CT or PET/MRI during the median follow-up period, except for
those who underwent both PET/CT and PET/MRI. The results
demonstrated that the detection time of PIF by PET/MRI (n=40) was
significantly earlier than that of PET/CT (n=55) (P=0.0367;
Fig. 1).
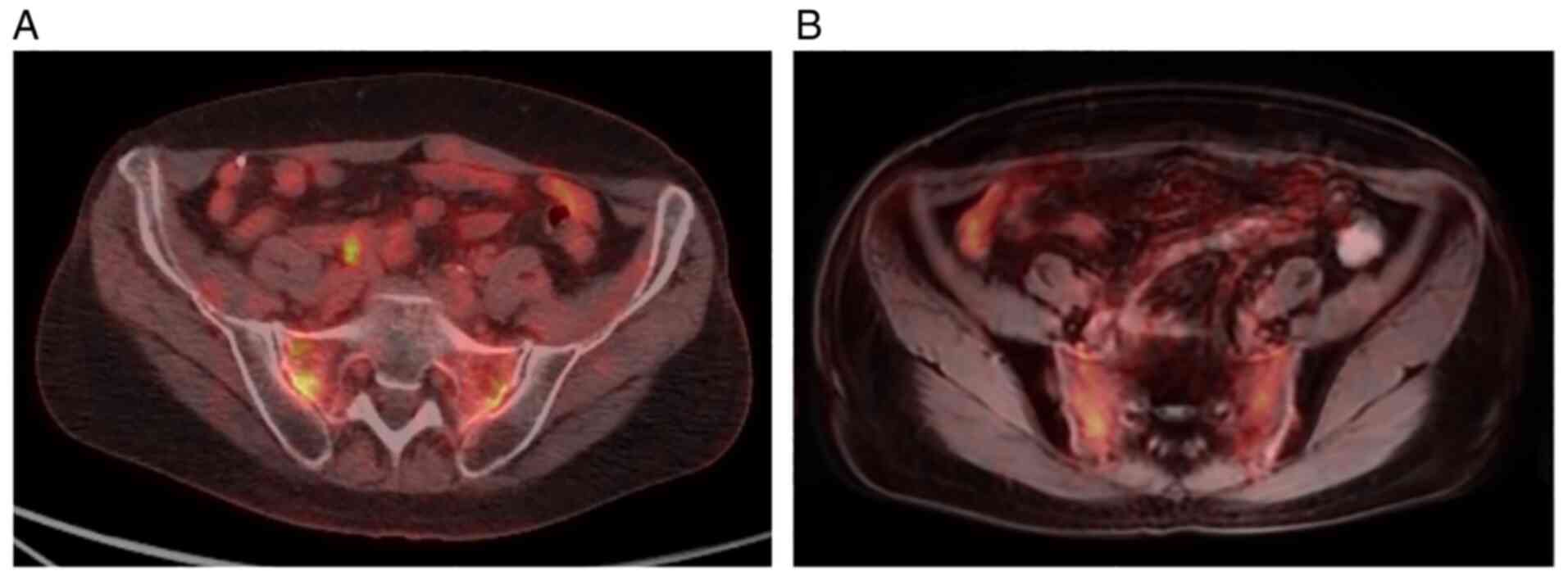
A diffuse linear FDG uptake
A diffuse linear FDG uptake was observed in parallel
with the sacroiliac joint as a characteristic pattern of sacral
fracture (Fig. 2). In addition, the
features of FDG uptake were similar between PET/CT and PET/MRI in
the present study (Fig. 2). The
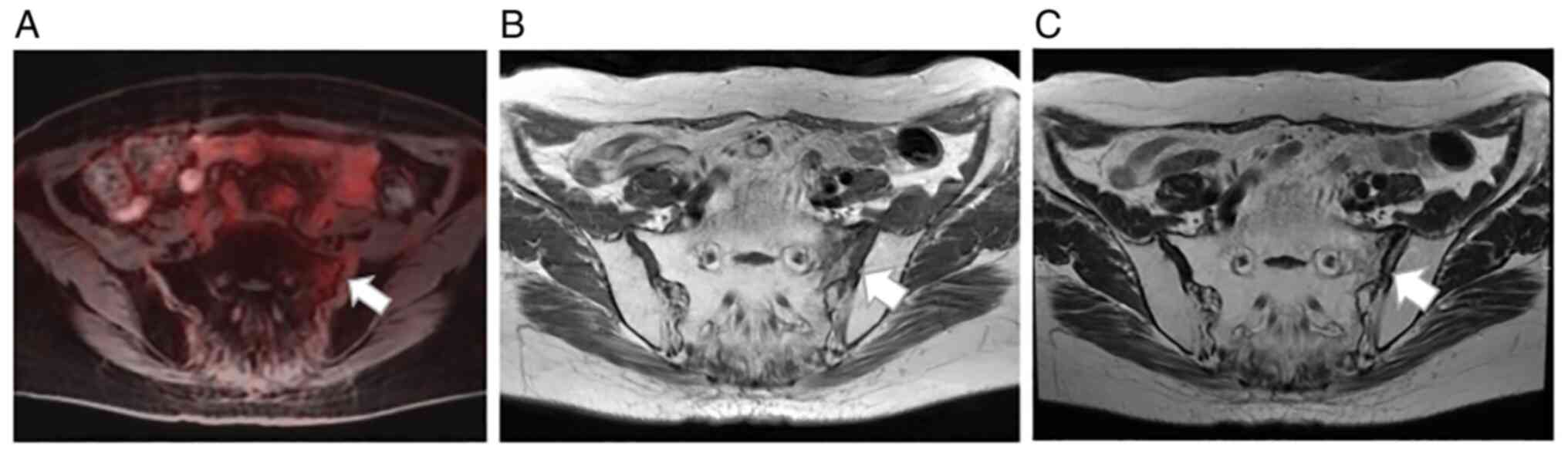
earliest MR sign, medullary edema, was seen and characterized as T1
hypointensity and T2 hyperintensity (Fig. 3).
Discussion
The results of the present study demonstrated that
PET/MRI was useful for early diagnosis of recurrent cervical
cancer, and for early detection of PIF compared with PET/CT.
Currently, a few studies have investigated the incidence and risk
factors of PIF via PET/CT as the imaging method; however, the
effects of PET/MRI have not yet been investigated (5,26–28). To
the best of our knowledge, the present study was the first to
report the incidence rate and risk factors of PIF via PET/MRI as
the imaging method.
Radiation therapy of the pelvis can cause
demineralization and decrease elastic resistance of the bone matrix
(28). According to a recent
meta-analysis, the overall incident rate of PIF was 14% (95%
confidence interval, 10–18%, based on 21 studies) (4). The incidence rate of PIF in the present
study was 20.8%, which was slightly higher than the meta-analysis.
Age has also been reported as a risk factor in several studies
(5–11), as well as the present study. However,
the results of the present study failed to exhibit significant
differences in other risk factors between the groups. This may have
been due to the small sample size used in the present study.
Previous studies have identified risk factors for PIF, including
postmenopausal status (6–8,10,12), low
body weight (5,9–11) and
osteoporosis (13,14). In the present study, no significant
differences were observed between the groups for some parameters
such as menopausal status or BMI.
This study was a retrospective study and thus relies
on medical records for information. However, data on the presence
or absence of osteoporosis was insufficient and thus was not
evaluated. Prospective studies are required to incorporate this
data by screening patients prior to chemoradiotherapy. It has been
reported that rheumatoid arthritis (RA) (12) and HRT (14) are risk factors for PIF. However, the
present study was unable to assess the associations between PIF and
RA or HRT as only a few patients had RA or had received HRT. Oh
et al reported that a high radiation dose is a risk factor
of PIF (11). At Kobe University
Hospital, both EBRT and IMRT are performed during the treatment
period in some cases and at the discretion of the radiation
oncologist; therefore, it was not possible to calculate the total
pelvic irradiation dose by simply adding the irradiation doses
together in the present study. Concurrent chemoradiotherapy is
considered a risk factor of PIF; however, no previous studies have
identified chemotherapy as a risk factor (7,12,17), and
neither did the present study. Ogino et al (29) reported that a history of three or
more deliveries is a risk factor of PIF, but we did not find a
significant difference in the present study. The sacrum is the
predominant site of PIF and is reported to account for 73.6% of
incidences (4). In the present
study, fractures in the sacrum occurred in 27/31 patients
(87.0%).
According to some reports, 43–77% of PIF cases are
symptomatic, and patients experience pain that affects their
quality of life (5,30,31).
Maintaining the quality of life for cancer survivors has become an
important issue in recent years. It is even more important in
patients with cervical cancer as it has a relatively young age of
onset and has a long survival time when completely cured (32). According to the results of the
present study, 45.2% of patients with PIF were symptomatic.
Treatment is generally conservative, with analgesic administration
and rehabilitation (33). Early
diagnosis and treatment may improve pain, immobilization and thus
mortality (33).
Imaging tests are rarely performed to solely
diagnose PIF, and PIF is often found when checking the recurrence
of cervical cancer. In previous reports, PET/CT was demonstrated to
be more sensitive in detecting recurrence or metastasis compared
with CT or MRI (34,35) PET/MRI has been reported to exhibit
comparable or better performance than PET/CT in detecting the
recurrence of gynecologic cancer (36). Furthermore, PET/MRI has the advantage
of lesion detection within the brain, breast, liver, kidneys, bone
and pelvic lesion compared with PET/CT (37). In addition, PET/MRI offers the
advantage of decreased radiation exposure compared with PET/CT
(38). It is important for patients
with cervical cancer to not only assess the detection of their
recurrent disease but also to avoid the radiation-induced
malignancies that can occur during a long follow-up period.
Currently, several studies have reported on the usefulness of CT
and MRI data in PIF diagnosis (20,22,39), and
according to Lapina and Tiškevičius (22), the sensitivity and specificity in PIF
diagnosis are 100 and 95.3% for MRI and 74.6 and 89.7% for CT,
respectively. Although the characteristics of PET/CT in PIF
diagnosis have been previously reported (5,27,28),
their value remains unclear. In the present study, 54.8% of
patients with PIF were asymptomatic, 70.6% of which were diagnosed
by PET-CT or PET-MRI. Conversely, a previous report has indicated
that only 39% of patients with asymptomatic PIF were diagnosed by
CT or MRI (20).
It has been reported that low-grade FDG uptake is
often observed at the fracture site (5). A diffuse linear FDG uptake is observed
in parallel with the sacroiliac joint as a characteristic pattern
of sacral fracture (Fig. 2). It is
important to distinguish between benign and malignant fractures.
The SUVmax value and the FDG uptake pattern differ
between malignant and benign fractures (40,41).
These reports are based on PET/CT and cannot be generally applied
to PET/MRI; however, the results of the present study demonstrated
no significant differences in the degree of SUVmax
between PET/CT and PET/MRI. In addition, the features of FDG uptake
were similar between PET/CT and PET/MRI in the present study
(Fig. 2). Furthermore, the results
demonstrated that PET/MRI may detect PIF earlier than PET/CT
(Fig. 1). This suggests that the
detection time of PIF is earlier in MRI compared with CT (22). According to Grangier et al
(42), the earliest MR sign,
medullary edema, which is characterized as T1 hypointensity and T2
hyperintensity, is seen as early as 18 days after the onset of
symptoms and persist as long as 516 days (Fig. 3). These findings suggest that PET/MRI
imaging may detect PIF at an earlier stage before patients have
developed symptoms compared with PET/CT, CT or MRI alone.
The present study is not without limitations. Given
that this study was retrospective, there may be data that has not
yet been revealed. Furthermore, the present study failed to conduct
a questionnaire to determine whether patients had any symptoms, and
only depended on medical records. Thus, patients may have had
symptoms, even in cases that were considered asymptomatic.
Furthermore, image follow-up was performed mainly for the purpose
of checking the recurrence of cervical cancer and not for PIF
examination. Given that the specific timing of image follow-up was
left to the attending physician, there may have been some variation
in the imaging timing for each patient. In addition, the attending
physician decided which imaging medium to follow up with, and since
it was not randomized, there may have been selection bias. Patients
who had many images taken due to recurrence may have had PIF found
earlier. There is also the possibility that SUVmax may
have had different values depending on the elapsed time after
fracture. Furthermore, PIF may have been found secondarily during
the recurrence check for cervical cancer, and it was not clear when
it occurred. In addition, measured SUVs on PET/CT and PET/MRI could
be significantly different even in the same patient due to the
difference in detectors and reconstruction methods. The present
study did not include dose volume histogram. In some cases, both
EBRT and IMRT were performed during the treatment period, and it
was not possible to calculate the total pelvic irradiation dose
simply by adding the irradiation doses. Therefore, it is possible
that the prescribed dose was clarified by using the dose volume
histogram. It has been reported that high irradiation dose is a
risk factor for PIF (30). In the
present study, it may have been possible to clarify whether the
prescribed dose is a risk factor of developing PIF or not by
analyzing the dose volume histogram.
In conclusion, the incidence of PIF after RT for
cervical cancer was 20.8% in the present study. Age was
significantly associated with the development of PIF. Furthermore,
PET/MRI, which offers the advantage of decreased radiation exposure
to the patient, may detect PIF at an earlier phase before patients
develop symptoms, thus allowing them to undergo early counseling
and treatment for bone health and to maintain a better quality of
life after cervical cancer treatment. However, further trials and
reports are required to establish the usefulness of PET/MRI in PIF
cases.
Acknowledgements
The authors of the present study would like to thank
Dr Sonoko Suda, Dr Keitaro Yamanaka, Dr Mamiko Sawada, Dr Masako
Tomimoto, Dr Keiichi Washio, Dr Maho Shimizu, Dr Ryosuke Takahashi,
Dr Satoshi Nagamata and Dr Yuka Murata for collecting the data.
They would also like to thank Dr Satoshi Senoh for technical advice
on radiation therapy. These persons were affiliated with Kobe
University Hospital.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
MA, MM, KS participated in data collection and
analyzed and interpreted patient data. RS, YU nad MN analyzed and
interpreted the radiological data. YT and MM confirm the
authenticity of all the raw data. YT contributed to the study
conception and design. MA and YT drafted the manuscript. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by Kobe University
Hospital Clinical and Translational Research Center (IRB no.
B200206, October 23rd, 2020). Given that this study was an
observational study using existing data, patient consent was
waived. All patient data were analyzed retrospectively, and no
tissues were examined. However, all study details were disclosed to
patients, and they were given the option to refuse registration via
e-mail.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Klaitong C, Meannuch E, Kaewbunperm U,
Klaiphibule P and Sinthusek T: EP-1512: Radiotherapy at pelvis
region in menopausal cervix cancer induce osteopenia/osteoporosis.
Radiother Oncol. 127 (Suppl 1):S819–S820. 2018. View Article : Google Scholar
|
|
2
|
Small W Jr and Kachnic L: Postradiotherapy
pelvic fractures cause for concern or opportunity for future
research? JAMA. 294:2635–2637. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Viswanathan AN, Lee LJ, Eswara JR,
Horowitz NS, Konstantinopoulos PA, Mirabeau-Beale KL, Rose BS, Von
Keudell AG and Wo JY: Complications of pelvic radiation in patients
treated for gynecologic malignancies. Cancer. 120:3870–3883. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sapienza LG, Salcedo MP, Ning MS, Jhingran
A, Klopp AH, Calsavara VF, Schmeler KM, Leite Gomes MJ, de Freitas
Carvalho E and Baiocchi G: Pelvic insufficiency fractures after
external beam radiation therapy for gynecologic cancers: A
meta-analysis and meta-regression of 3929 patients. Int J Radiat
Oncol Biol Phys. 106:475–484. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Park S, Kim J, Lee J and Park IK: Pelvic
insufficiency fracture after radiotherapy in patients with cervical
cancer in the era of PET/CT. Radiat Oncol J. 29:269–276. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ramlov A, Pedersen EM, Røhl L, Worm E,
Fokdal L, Lindegaard JC and Tanderup K: Risk factors for pelvic
insufficiency fractures in locally advanced cervical cancer
following intensity modulated radiation therapy. Int J Radiat Oncol
Biol Phys. 97:1032–1039. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bazire L, Xu H, Foy JP, Amessis M,
Malhaire C, Cao K, De La Rochefordiere A and Kirova YM: Pelvic
insufficiency fracture (PIF) incidence in patients treated with
intensity-modulated radiation therapy (IMRT) for gynaecological or
anal cancer: Single-institution experience and review of the
literature. Br J Radiol. 90:201608852017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cai ZX, Li Y, Yang ZH, Gong S, Zhang MD
and Chen JY: MRI and associated clinical characteristics of pelvic
insufficiency fracture in cervical carcinoma patients after
radiation therapy. Chinese J Med Imaging Technol. 31:1483–1486.
2015.
|
|
9
|
Tokumaru S, Toita T, Oguchi M, Ohno T,
Kato S, Niibe Y, Kazumoto T, Kodaira T, Kataoka M, Shikama N, et
al: Insufficiency fractures after pelvic radiation therapy for
uterine cervical cancer: An analysis of subjects in a prospective
multi-institutional trial, and cooperative study of the Japan
radiation oncology group (JAROG) and Japanese radiation oncology
Study Group (JROSG). Int J Radiat Oncol Biol Phys. 84:e195–e200.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schmeler KM, Jhingran A, Iyer RB, Sun CC,
Eifel PJ, Soliman PT, Ramirez PT, Frumovitz M, Bodurka DC and Sood
AK: Pelvic fractures after radiotherapy for cervical cancer:
Implications for survivors. Cancer. 116:625–630. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oh D, Huh SJ, Park W, Ju SG, Nam H and Lee
JE: Clinical outcomes in cervical cancer patients treated by
FDG-PET/CT-based 3-dimensional planning for the first brachytherapy
session. Medicine (Baltimore). 95:e38952016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yamamoto K, Nagao S, Suzuki K, Kogiku A,
Senda T, Yano H, Kitai M, Shiozaki T, Matsuoka K and Yamaguchi S:
Gynecologic Oncology Pelvic fractures after definitive and
postoperative radiotherapy for cervical cancer: A retrospective
analysis of risk factors. Gynecol Oncol. 147:585–588. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Weidenbacher B, Borm K and Oechsner M:
Pelvic fractures after radiotherapy for cervical cancer.
Strahlenther Onkol. 194:2018.
|
|
14
|
Shih KK, Folkert MR, Kollmeier MA,
Abu-Rustum NR, Sonoda Y, Leitao MM, Barakat RR and Alektiar KM:
Pelvic insufficiency fractures in patients with cervical and
endometrial cancer treated with postoperative pelvic radiation.
Gynecol Oncol. 128:540–543. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ta L, Jt G, Se D, Cc H and Hjn A: Effects
of pelvic radiotherapy for primary pelvic cancers (Review).
Cochrane Database Syst Rev. 2018.
|
|
16
|
Elit L and Reade CJ: Recommendations for
follow-up care for gynecologic cancer survivors. Obstet Gynecol.
126:1207–1214. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mehmood Q, Beardwood M, Swindell R,
Greenhalgh S, Wareham T, Barraclough L, Livsey J and Davidson SE:
Insufficiency fractures in patients treated with pelvic
radiotherapy and chemotherapy for uterine and cervical cancer. Eur
J Cancer Care (Engl). 23:43–50. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kuji S, Hirashima Y, Komeda S, Tanaka A,
Abe M, Takahashi N, Takekuma M, Asakura H, Harada H and Nishimura
T: Feasibility of extended-field irradiation and intracavitary
brachytherapy combined with weekly cisplatin chemosensitization for
IB2-IIIB cervical cancer with positive paraaortic or high common
iliac lymph nodes: A retrospective review. Int J Clin Oncol.
19:341–347. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jung J, Park G and Kim YS: Definitive
extended-field intensity-modulated radiotherapy with chemotherapy
for cervical cancer with para-aortic nodal metastasis. Anticancer
Res. 34:4361–4366. 2014.PubMed/NCBI
|
|
20
|
Uezono H, Tsujino K, Ota Y, Nagano F,
Soejima T, Moriki K and Sasaki R: Pelvic insufficiency fracture
after definitive radiotherapy for uterine cervical cancer:
Retrospective analysis of risk factors. J Radiat Res. 54:1102–1109.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim J, Lee KJ, Park KR, Ha B, Kim YJ, Jung
W, Lee R, Kim SC, Moon HS, Ju W, et al: Treatment outcomes after
adjuvant radiotherapy following surgery for patients with stage I
endometrial cancer. Radiat Oncol J. 34:265–272. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lapina O and Tiškevičius S: Sacral
insufficiency fracture after pelvic radiotherapy: A diagnostic
challenge for a radiologist. Med. 50:249–254. 2014.PubMed/NCBI
|
|
23
|
NCCN clinical practice guidelines in
oncology, . Cervical Cancer Version 4. Natl Compr Cancer Netw.
2019.
|
|
24
|
Pecorelli S, Zigliani L and Odicino F:
Revised FIGO staging for carcinoma of the cervix. Int J Gynecol
Obstet. 105:107–108. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Von Elm E, Altman DG, Egger M, Pocock SJ,
Gøtzsche PC and Vandenbrouckef JP; STROBE Initiative, : The
Strengthening the Reporting of Observational Studies in
Epidemiology (STROBE) Statement: Guidelines for reporting
observational studies. Bull World Health Organ. 85:867–872. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Halaç M, Mut SS, Sönmezoglu K, Ylmaz MH,
Ozer H and Uslu I: Avoidance of misinterpretation of an FDG
positive sacral insufficiency fracture using PET/CT scans in a
patient with endometrial cancer: A case report. Clin Nucl Med.
32:779–781. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Salavati A, Shah V, Wang ZJ, Yeh BM,
Costouros NG and Coakley FV: F-18 FDG PET/CT findings in
postradiation pelvic insufficiency fracture. J Clin Imaging.
35:139–142. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chung YK, Lee YK, Yoon BH, Suh DH and Koo
KH: Pelvic insufficiency fractures in cervical cancer after
radiation therapy: A meta-analysis and review. In Vivo (Brooklyn).
35:1109–1115. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ogino I, Okamoto N, Ono Y, Kitamura T and
Nakayama H: Pelvic insufficiency fractures in postmenopausal woman
with advanced cervical cancer treated by radiotherapy. Radiother
Oncol. 68:61–67. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kwon JW, Huh SJ, Yoon YC, Choi SH, Jung
JY, Oh D and Choe BK: Pelvic bone complications after radiation
therapy of uterine cervical cancer: Evaluation with MRI. AJR Am J
Roentgenol. 191:987–994. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kido A, Yoshida S, Shimoda E, Ishida Y,
Hasegawa M, Kobayashi H, Honoki K, Horikawa H and Tanaka Y: Walking
disability in patients with pelvic insufficiency fracture after
radiotherapy for uterine cervical cancer. Prog Rehabil Med.
1:201600092016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Thapa N, Maharjan M, Xiong Y, Jiang D,
Nguyen TP, Petrini MA and Cai H: Impact of cervical cancer on
quality of life of women in Hubei, China. Sci Rep. 8:119932018.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
van den Blink QU, Garcez K, Henson CC,
Davidson SE and Higham CE: Pharmacological interventions for the
prevention of insufficiency fractures and avascular necrosis
associated with pelvic radiotherapy in adults. Cochrane Database
Syst Rev. 4:CD0106042018.PubMed/NCBI
|
|
34
|
Choi HJ, Ju W, Myung SK and Kim Y:
Diagnostic performance of computer tomography, magnetic resonance
imaging, and positron emission tomography or positron emission
tomography/computer tomography for detection of metastatic lymph
nodes in patients with cervical cancer: Meta-analysis. Cancer Sci.
101:1471–1479. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pantola S, Kala S, Kala C, Sampath S and
Shukla M: Comparative study of positron emission
tomography/computed tomography and computed tomography in the
evaluation of post-treatment carcinoma cervix patients. Indian J
Nucl Med. 33:194–201. 2018.PubMed/NCBI
|
|
36
|
Broski SM, Goenka AH, Kemp BJ and Johnson
GB: Clinical PET/MRI: 2018 update. AJR Am J Roentgenol.
211:295–313. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Rosenkrantz AB, Friedman K, Chandarana H,
Melsaether A, Moy L, Ding YS, Jhaveri K, Beltran L and Jain R:
Current status of hybrid PET/MRI in oncologic imaging. Am J
Roentgenol. 206:162–172. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Schwartz M, Gavane SC, Bou-Ayache J, Kolev
V, Zakashansky K, Prasad-Hayes M, Taouli B, Chuang L and Kostakoglu
L: Feasibility and feasibility and diagnostic performance of hybrid
pet/mri compared with pet/ct for gynecological malignancies: A
prospective pilot study. Abdom Radiol. 43:3462–3467. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ugurluer G, Akbas T, Arpaci T, Ozcan N and
Serin M: Bone complications after pelvic radiation therapy:
Evaluation with MRI. J Med Imaging Radiat Oncol. 58:334–340. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
He X, Zhao L, Guo X, Zhao L, Wu J, Huang
J, Sun L, Xie C and Chen H: Differential diagnostic value of18F-FDG
PET/CT for benign and malignant vertebral compression fractures:
Comparison with magnetic resonance imaging. Cancer Manag Res.
10:2105–2115. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mauch JT, Carr CM, Cloft H and Diehn FE:
Review of the imaging features of benign osteoporotic and malignant
vertebral compression fractures. AJNR Am J Neuroradiol.
39:1584–1592. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Grangier C, Garcia J, Howarth NR, May M
and Rossier P: Role of MRI in the diagnosis of insufficiency
fractures of the sacrum and acetabular roof. Skeletal Radiol.
26:517–524. 1997. View Article : Google Scholar : PubMed/NCBI
|