Introduction
Worldwide, breast cancer is the second most commonly
diagnosed cancer when statistics for both sexes are combined. For
women, breast cancer is the most commonly diagnosed cancer and the
leading cause of mortality (1). In
Asia, the most common cancer types in women are breast, lung,
cervical, colorectal and stomach cancer. The mortality-to-incidence
ratios are the highest in lung, liver and stomach cancer, and the
lowest in colorectal, breast and prostate cancer (2). In 2012, there were 639,824 cases of
breast cancer recorded in Asian countries, with 228,926 deaths.
Malaysia recorded 5,410 cases of breast cancer, with 2,572 deaths,
in 2012 (3). Based on Malaysia's
2016 National Cancer Registry, a total of 21,634 cases of female
breast cancer were diagnosed over a period of 4 years between 2012
and 2016 compared with 18,206 cases in the 2007–2011 report. Breast
cancer is the most common cancer and has accounted for 34.1% of all
cancer cases among women in Malaysia. The age-standardised rate was
increased from 31.1 per 100,000 population in 2007–2011 to 34.1
between 2012 and 2016 (4).
Malaysia is a developing country made up of three
main ethnicities: Malay, Chinese and Indian. Multi-ethnicity in
Malaysia started after the establishment of the Straits Settlements
in Penang, Malacca and Singapore, and later on, the acquisition of
the Malay territories by the British. These British colonizers
brought in a number of labourers from China and India to work on
the land (5). The Chinese migrants
were placed to work in tin mines, whilst the Indian population
laboured in the rubber plantations.
With regard to the breast cancer incidence rate
among the three major ethnic groups, the incidence is highest among
the Chinese (40.7 per 100,000 individuals) followed by the Indians
(38.1 per 100,000 individuals) and the Malays (31.5 per 100,000
individuals). The overall lifetime risk is 1 in 22 for the Chinese,
1 in 23 for the Indians and 1 in 30 for the Malays (4). The Malays have been observed to be
significantly younger at the time of cancer presentation (average,
50 years old) compared with the Chinese (average, 57 years old) and
Indians (average 56 years old). The Malays also have a more
advanced stage at diagnosis compared with the other two ethnic
groups (6). The Malay ethnicity was
observed to be a poor prognostic factor in breast cancer,
conferring 1.5 times the risk of death compared with the Chinese
ethnicity (7). Similarly, it was
noted that the Malays had a lower survival rate of 39.7% compared
with 48.2% in the Chinese and 47.2% in the Indians (8). These Malay women presented with the
more advanced stages compared with the women of the other two
ethnicities, and had the worst survival rate (9,10).
Singapore, which is a multi-ethnic country similar to Malaysia,
also reported a similar breast cancer incidence rate that was
higher among Chinese women compared with that among the Malays and
Indians (11). Table I shows the statistics of breast
cancer among the different ethnic groups.
 | Table I.Statistics of breast cancer and
genetic mutations among the different ethnic groups in
Malaysia. |
Table I.
Statistics of breast cancer and
genetic mutations among the different ethnic groups in
Malaysia.
| Statistic | Malay | Chinese | Indian | (Refs.) |
|---|
| Incidence (per
100,000) in a 5-year period |
|
|
|
(4) |
|
2007-2011 | 27.2 | 41.5 | 37.1 |
|
|
2012-2016 | 31.5 | 40.7 | 38.1 |
|
| Overall lifetime
risk | 1 in 30 | 1 in 22 | 1 in 23 |
(4) |
| Age at
presentation, years | 50 | 57 | 56 |
(6) |
|
| 46 | 51 | 53 |
(9) |
| Metastatic disease
at presentation, % | 14.2 | 9.2 | 11.9 |
(6) |
|
| 16 | 9 | 4 |
(9) |
| Median tumour size
at diagnosis, mm | 35 | 25 | 30 |
(9) |
| Oestrogen
receptor-positive tumours, % | 52.5 | 58.1 | 52.5 |
(9) |
| Oestrogen
receptor-negative tumours, % | 47.5 | 41.9 | 47.5 |
(9) |
| High-grade tumours,
% | 44.7 | 39.4 | 43.9 |
(9) |
| Malaysian 5-year
survival rate, % | 39.7 | 48.2 | 47.2 |
(8) |
| Malaysian average
survival time, years | 6.41 | 7.10 | 6.45 | (10) |
| Malaysian-Singapore
5-year survival rate, % | 58.5 | 75.8 | 68 |
(9) |
| BRCA1 and 2
mutations, % | 23.5 | 63.1 | 11.8 | (65) |
Although there has been ethnic integration, and the
occurrence of marriages between ethnicities, each group has largely
retained its own unique culture and way of life. In Malaysia, the
statistical data combines the Malays with the smaller indigenous
groups to form the Bumiputera group. The Malays (Bumiputera) now
make up 69.6% of the population, the Chinese 22.6% and the Indians
6.8%, with the remaining percentage being constituted from the
other ethnic minorities. The total population now stands at 32.6
million people (12)
According to a review of the literature, to the best
of our knowledge, there has been only one paper discussing the
possible causes or correlation between the lifestyle and culture of
the three ethnicities in Malaysia and breast cancer risk (13). However, this paper lacks references
for a number of the points that were raised. A large part of this
paper discussed the general lifestyles that had led to Malaysian
women developing cancer as a whole, but did not compare the
practices between the different ethnicities, as the title had
suggested.
The present review comprehensively analyses
different cultural practices and how they may have affected the
risk, stage at presentation and outcome of women with breast cancer
in Malaysia, a multi-ethnic developing country. The significant
ethnic differences appear to be in the type of daily food and
cooking methods, contraception, fertility rates, breast-feeding
practices, confinement period and care, postmenopausal intake and
influence of the traditional healer, which are all discussed.
Dietary habits
As in most cases, dietary practices play a big role
with regard to health. The three ethnic races in Malaysia have
their preferences in food preparation. The Malays and the Indians
use a lot of turmeric or curcumin in their routine cooking,
consisting of curries and other spicy gravies. Curcumin is a
polyphenol from the plant Curcuma longa. Although not a
phyto-oestrogen, it has been shown to inhibit the proliferation of
various breast cancer cell lines and also to induce the apoptosis
of breast cancer cells (14).
Curcumin has also been found to minimise the risk of metastases in
breast cancer by downregulating the inflammatory cytokines C-X-C
motif chemokine ligand 1 and 2 via nuclear factor-κB, an
inflammation- and cell survival-related transcription factor
(15).
The typical Chinese diet does not include turmeric.
Instead, a lot of soya (soy) products, consisting of soya sauce,
bean curd and soya-bean drink, are used. Soya beans fall in the
isoflavones category of phyto-oestrogens. In a dose-response
meta-analysis report, each increment of 10 mg/day soy isoflavone
was associated with a 3% decreased breast cancer risk (16). Phyto-oestrogens are very weak
mimickers of natural oestrogens, with an affinity for oestrogen
receptors of 1,000-10,000 times lower than oestradiol (17). There are two types of oestrogen
receptors (ERs), ER-α and ER-β. Stimulation of ER-α causes an
increase in tumour growth, but stimulation of ER-β causes tumour
regression. Oestradiol has equal affinity for both types of ERs.
Tamoxifen has double the affinity for ER-β compared with that for
ER-α. However, phyto-oestrogens have five times greater affinity
for ER-β compared with that for ER-α (18). A bi-phasic behaviour of isoflavones
has also been observed in vitro, whereby a low dose
stimulated the growth of MCF-7 cells (ER-positive breast cancer
cell line), but not MDA-MB cells (ER-negative breast cancer cell
line). At high doses, isoflavones inhibit the growth of both
ER-positive and -negative cell lines (19,20).
Another important Chinese cooking ingredient is sesame, which is
consumed as seeds and as sesame oil (21). Sesame seeds contain a lignan, which
is also a type of phyto-oestrogen. However, its chemical compound,
enterolactone, is metabolized in the gut and may have limited
effects on humans (17).
In another study, a low dietary fibre intake was
associated with higher risks of developing breast cancer (22). In a nutrient-wide association study,
it was reported that a high intake of fibre and fruits was
associated with a lower breast cancer risk (23). It was found that the total
consumption of vegetables and fruits differ amongst the different
ethnic groups in Malaysia. The Malays have the highest consumption,
followed by the Chinese and the Indians (24), and this may influence breast cancer
risk in these ethnic groups.
In Malaysia, alcohol consumption is significantly
higher among males compared with females. Among the three ethnic
groups, binge drinking was recorded to be highest in the Indians
(54%), followed by the Chinese at 39% and the Malays at 8%
(25). The Malay women, who are
Muslims, do not consume alcohol as it is forbidden in Islam. Some
Chinese women consume alcohol on social occasions and some Indian
women in the estates consume illicit alcohol (samsu) (26). Frequent and high consumption of
alcohol are risk factors for breast cancer, as shown in a study
among premenopausal women in Japan (27). Similarly, one report identified
alcohol as one of the environmental factors related to cancer
(28). Due to the differences in
alcohol consumption among the ethnic groups, breast cancer risk and
incidence may also differ.
Confinement diet
Across the three ethnicities, the confinement period
is traditionally regarded important in order to protect the
well-being of the woman, as it allows the body to recuperate and
recover from childbirth. At the time, certain dietary practices are
observed. ‘Hot foods’ are recommended. ‘Hot foods’ refer to spicy
food, with the effect of making the one eating it sweat easily. The
Malay confinement period lasts 44 days in which the new mother
would be required to wear a special corset (bengkung)
(29). Firstly, two large rectangle
pieces of cloth are sewn together with a central compartment filled
with spices; this is placed over the front of the belly. Next, a
long plain piece of cloth is wrapped snugly around the body, over
the spice-filled piece, starting from the upper down to the lower
abdomen. The new mother would undergo whole body massage daily.
Warm compression from heated stones would be placed on the
abdominal wall for several minutes at a time, daily, over 3–7 days;
this is similar to the application of a hot water bottle. The
confinement diet consists of not only young tubers of turmeric, but
also its young shoots. Other foods consist of the snake-head fish
(ikan haruan), anchovies, meat, ginger, black pepper and a herb
locally known as Kacip Fatimah [Labisia pumila (LP)]. This
herb has been found to have cytotoxic activity against the MCF-7
breast cancer cell line (30,31),
prostate cancer cell lines (32,33) and
melanoma cells (34). It has also
been found to have anti-fungal and anti-inflammatory properties
(30), including bronchodilatory
properties (35).
The confinement period for Chinese women is a month.
The confinement diet consists of large amounts of ginger and
sesame, as well as special brews in the form of rice wine in which
chicken and pork trotters had been simmered. Some women are also
given additional drinks such as Dom Pérignon, a French wine, which
is highly regarded by the Chinese to be good for women during
confinement (21).
During the confinement period, Chinese women are
also given Ginseng (Panax ginseng) and Dong Quai or Tong
Kuei (Angelica sinensis). Traditionally known as ‘female
ginseng’, Dong Quai is often given to women at other times too.
Amongst its indicated properties are the improvement of fertility
and libido, and the treatment of dysmenorrhoea and premenstrual
syndrome (21). Amato et al
(36) showed that, in vitro,
Dong Quai and Ginseng increased breast cancer cell line
multiplication by 16 and 27 times, respectively. However, recent
studies (37,38) have shown conflicting findings. Dong
Quai did not exert significant stimulatory effects on breast cancer
in both an in vivo breast tumour xenograft-bearing nude
mouse model and in an in vitro human breast cancer cell
line. However, precaution is required if Dong Quai is to be used in
oestrogen receptor-positive breast cancer patients due to its
ability to induce oestrogen receptor-α expression and its
tumorigenic potential via promotion of cancer stem cell activity in
oestrogen receptor-positive breast cancer (39,40).
Ginseng has also been shown to inhibit the proliferation of breast
cancer cell lines in a time- and dose-dependent manner by
activating the apoptotic pathway (41).
Similar to the Chinese, the Indian women undergo a
confinement of 30 days. However, their diet is very different from
that of Chinese women. Indian women avoid ‘cooling foods’ such as
cucumber, murungai (Moringa oleifera) fruits and grapes, but
are encouraged to consume more spices such as black pepper,
cardamon, aniseed, turmeric and ginger (42). In a study conducted in Singapore,
Indian women were also observed to increase their consumption of
garlic (43). A high consumption of
garlic has been shown to have an inverse association with breast
cancer, as reported in a study conducted among women aged 39–70
years in Puerto Rico (44).
Fertility rate
The fertility rates of the three ethnicities differ,
with the highest amongst Malay women and the lowest among Chinese
women (12). There is a close
association between breast cancer and parity, whereby increased
parity or fertility lessens breast cancer risk (28).
In 2014, it was found that 52% of Malaysian women
practiced family planning consisting of both non-modern and modern
methods. The most favoured modern contraception was the oral
contraceptive pill (OCP) at 13.2% usage (45). Contraceptive practices also differed
between the ethnicities, with the pill being used the most by
Chinese women (45.6%), followed by the Indian (32.2%) and Malay
(28.2%) women (46). Use of the OCP
has been shown to increase breast cancer risk (28).
Breastfeeding
Breastfeeding is beneficial to both the mother and
the child. For the mother, there is an association with a decreased
breast cancer risk if the baby is breastfed for >6 months
(28). Local data have shown that a
higher percentage of Malays tend to breastfeed longer compared with
the percentage of Chinese (47). In
one study, it was determined that Chinese women who were working,
from a high income family and with male infants were less likely to
breastfeed their baby (48). In a
study that analysed a group of 682 women (Malays, 60.9%; Chinese,
18.7%; and Indians, 16%), it was found that exclusive breastfeeding
for the first 6 months was practised by 52.5% of the Malays, 15.6%
of the Chinese and 35.8% of the Indians (49).
Postmenopausal diet
Similar to during the confinement period, LP is also
commonly taken by Malay women postmenopause. The menopause is
associated with several symptoms and mental health changes
(vasomotor symptoms and cognitive function), as well as changes in
physiological systems and functions (cardiovascular and bone
health) (50). In rats who were
given LP and oestrogen, the collagen fibres that held the
adipocytes together became fragmented causing lipolysis. This
showed that there is a possible role for LP in preventing
postmenopausal obesity (51).
Additionally, a study by Fazliana et al (52) showed that the plant caused an
increase in the production of leptin, leading to weight loss and
improvement in insulin sensitivity. Nadia et al (53) demonstrated the anti-oxidative role of
LP, and Abdul Kadir et al (54) found it to lower serum triglyceride
levels. High triglyceride levels have been shown to be associated
with coronary heart disease in postmenopausal women (55,56).
A study comparing LP with premarin, one of the
medications used for hormone replacement therapy, showed that LP
did not prevent the loss of bone mass (57). However, another study in animal
models showed it to be comparable to premarin in preventing
osteoporotic fractures in oestrogen-deficient states (58). A pilot study on women administered LP
extracts demonstrated no increase in mammographic density (59). This is important, as an increase in
mammographic density would make interpretation more difficult and
has been shown to increase breast cancer risk (60,61).
Just like in Chinese women during the confinement
period, Chinese postmenopausal women take Dong Quai to treat
vasomotor symptoms (21). As shown
by Amato et al (36), these
menopausal women now have an added risk of developing breast cancer
due to this consumption.
Traditional healer
According to the Malay culture, the traditional
healer or medicine man, known as a ‘bomoh’, is much respected in
society. This is especially so among the rural population (62). Often, the services of the healer is
sought after for numerous illnesses in both children and adults.
These include physical illnesses, spiritual illnesses and those
believed to be related to sorcery or black-magic. Even family
related issues like infidelity, separation, divorce or the search
for a life partner often involve seeking the advice of the
healer.
In Malaysia, the highest users of traditional and
complementary treatment are the Sabah Natives, followed by the
Malays (63). Among all patients
with breast cancer, there are several reasons for seeking
traditional healers, including recommendations from family members
and friends, sanction from family, perceived benefit and
compatibility, healer credibility, and reservation towards Western
medicine and system delays (64).
For physical lesions, one of the common taboos
conveyed by these healers is contact of the affected body part with
metal objects. Those who follow these orders would not come to
hospital, as often a biopsy would need to be taken, which would
involve the use of metal needles. When the treatment from a
particular healer did not work or the illness did not go away, a
second or third bomoh would be consulted. Only after failing these
treatments, which could lead to a delay of 6 to 12 months, would
these women present themselves to a hospital. This accounts for the
late diagnosis at stages 3 or 4 for Malay women with breast cancer.
As expected, these women with more advanced diseases have poorer
outcomes. Among the three ethnicities, the Malay women are the
worst affected in this regard (8–10).
Genetic mutations
Genetic research performed by Thirthagiri et
al (65) discovered that Chinese
women had the highest incidence of BRCA1 and 2 mutations at 63.1%,
followed by Malay women at 23.1% and Indian women at 11.8%. Among
the Chinese women, there was an equal proportion of BRCA1 and 2
mutations. There was more BRCA2 mutations among the Malays. These
mutations led to early onset breast cancer (age ≤40 years). A total
of 27 deleterious mutations were detected (14 in BRCA1 and 13 in
BRCA2), and 47 variants of uncertain clinical significance were
identified (16 in BRCA1 and 31 in BRCA2). This study may
significantly contribute to the current statistical evidence on
incidence of breast cancer by ethnicity.
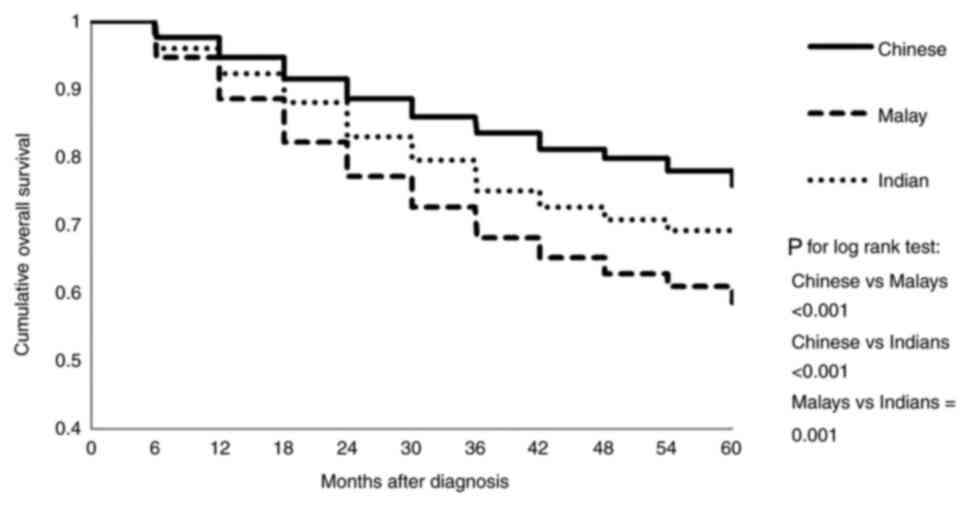
Cumulative overall survival
The cumulative overall survival of Malaysian and
Singaporean women (9) was
demonstrated in a full model adjusted for socio-demographic
factors, tumour characteristics and treatment (Fig. 1). The findings showed that the
cumulative overall survival rate was lowest for Malay women. This
data was also supported by results from other previous studies
(8,10).
Comparison between three ethnic groups
Chinese women who have the lowest fertility rate,
highest OCP use, poorest breast feeding practices and highest
alcohol intake are associated with increased breast cancer risks.
Soya seems to be associated with decreased cellular proliferation
in vitro. However, a diet rich in soya alone, as one
beneficial factor, would not be able to overcome all the other
negative lifestyle practices. With the added factor of having the
highest incidence of BRCA1 and 2 genetic mutations amongst the
three ethnicities, it is not unexpected that Chinese women have the
highest risk of breast cancer.
In comparison, Malay women have the highest
fertility rate, lowest OCP usage, best breast feeding practices, no
alcohol consumption and the intake of a herb (Kacip Fatimah) with
in vitro cytotoxic properties. All of these are in favour of
lowering breast cancer risks. The setback among this group is a
strong belief in the traditional healer, which causes late
presentation to hospitals and poor survival outcomes.
The practices observed by Indian women come between
those practiced by the Chinese and the Malays, which put them
second highest in terms of breast cancer risk. Table II summarizes the differences in
cultural practices among the three ethnic groups and the influence
on breast cancer risk.
 | Table II.Cultural practices of the three major
ethnic groups in Malaysia and breast cancer risks. |
Table II.
Cultural practices of the three major
ethnic groups in Malaysia and breast cancer risks.
| A, Dietary
habits |
|---|
|
|---|
| Ethnicity | Practice | Breast cancer
risk |
|---|
| Malay | Turmeric/curcumin
consumption | Reduced risk:
Curcumin inhibits proliferation and induces apoptosis of breast
cancer cell lines (14) |
|
| High consumption of
vegetables and fruits | Reduced risk: High
dietary fibre reduces breast cancer risk in a study of Malaysians
compared with controls (22) Women,
aged 25 to 70 years, followed-up for 15 years, in the European
Prospective Investigation into Cancer and Nutrition Study showed
that high fibre intake reduced breast cancer risk (23) |
| Chinese | Soy product
consumption | Reduced risk: A
meta-analysis of Chinese women (aged 30–79 years) followed up for
10 years and other studies in Asia and Western countries found that
an increase in soy intake reduced breast cancer risk (16) |
|
| Alcohol
consumption | Increased risk:
Alcohol consumption is a risk factor for breast cancer in
premenopausal women (25) |
| Indian | Turmeric/curcumin
consumption | Reduced risk: As
aforementioned (14) |
|
| Alcohol
consumption | Increased risk: As
aforementioned (25) |
|
| B, Confinement
diet |
|
|
Ethnicity |
Practice | Breast cancer
risk |
|
| Malay | Turmeric/curcumin
consumption | Reduced risk: As
aforementioned (14) |
|
| Kacip Fatimah
(Labisia pumila) consumption | Reduced risk:
Cytotoxic activity against the MCF-7 breast cancer cell line
(30,31) |
| Chinese | Alcohol
consumption | Increased risk: As
aforementioned (25) |
|
| Ginseng and Dong
Quai (Angelica sinensis) consumption | Conflicting
reports: Recent studies showed that Dong Quai did not induce breast
cancer but caution use in oestrogen receptor-positive breast cancer
patients, while ginseng inhibits growth of breast cancer cell lines
(37,38) |
| Indian |
Turmeric/curcumin | Reduced risk: As
aforementioned (14) |
|
| C, Fertility
rate |
|
|
Ethnicity |
Practice | Breast cancer
risk |
|
| Malay | Highest parity
rate, lowest usage of OCP | Reduced risk:
Increased parity lessens breast cancer risks (28) |
| Chinese | Lowest parity rate,
highest usage of OCP | Increased risk: Use
of OCP increase breast cancer risk (28) |
| Indian | Parity and usage of
OCP ranking between that of the Malays and the Chinese | Medium risk |
|
| D,
Breastfeeding |
|
|
Ethnicity |
Practice | Breast cancer
risk |
|
| Malay | Most practiced | Reduced risk:
Decrease breast cancer risk if breastfeeding for >6 months
(28) |
| Chinese | Least
practiced | Increased risk: No
breast feeding protective effect against breast cancer (27) |
| Indian | In between the
Malays & the Chinese | Reduced risk:
Decrease breast cancer risk if breastfeeding for >6 months
(28) |
|
| E,
Postmenopausal diet |
|
|
Ethnicity |
Practice | Breast cancer
risk |
|
| Malay | Kacip Fatimah
(Labisia pumila) consumption | Reduced risk: As
aforementioned (30,31) |
| Chinese | Dong Quai
(Angelica sinensis) consumption | Conflicting
reports: As aforementioned (37) |
| Indian | Data not
available | Data not
available |
|
| F, Traditional
healer |
|
|
Ethnicity |
Practice | Breast cancer
risk |
|
| Malay | Strong belief | Increased risk:
These women had the worst outcome (8–10) |
| Chinese | No strong
belief | No increased
risk |
| Indian | No strong
belief | No increased
risk |
A large part of the aforementioned herbal research
showed findings from in vitro studies and animal models,
with limited studies in humans. Although this is a commendable
start, further clinical trials need to be completed in order to
produce more robust data to facilitate the use of such herbs in the
clinical setting. From the current data, LP appears a safer option
than hormone replacement therapy, which is associated with elevated
breast cancer risks according to the Women's Health Initiative
study, plus increased risks of stroke and thromboembolic diseases
(66).
The peak age of breast cancer in Malay women is
lower compared with that in Chinese and Indian women (6,9). This
may be related to the different cancer subtypes among the ethnic
groups. The luminal A subtype occurs significantly more frequently
in the Chinese than in the Malays. However, the percentage of
triple-negative subtype cases is significantly higher in the Malays
than in the Chinese (67).
Triple-negative breast cancer has been associated with a younger
age at the time of diagnosis and a more advanced disease stage
(68). However, when Asians as a
whole are considered, the peak age of breast cancer incidence is
between 40 and 50 years old, as opposed to between 60 and 70 years
old in Western countries (69).
Biological, genetic and the environmental factors may contribute to
these differences.
Conclusion
Based on the data presented, the three ethnicities
have distinct cultural practices that may influence breast cancer
occurrence. The lowest incidence of breast cancer in the Malays may
be attributable to their lifestyle and cultural practices. However,
the Malays present with the disease at an advanced stage and have a
low survival rate. It is hoped that the three ethnicities will
learn from each other and adjust their cultural practices. This
would mean continuing the beneficial praticises and abandoning the
detrimental ones. This is a challenging task and may take a longer
time, as often traditional changes occur more easily with a newer
generation. Some individuals may have sensitive sentiments attached
to their cultural practices and will oppose changes. The government
and non-government organisations would need to work together to
educate the public to increase their breast cancer awareness and
advocate the best lifestyle practices. This would be the best way
forward in an attempt to decrease the incidence of breast cancer
and improve the outcome at a national level as Malaysia strives
forward to become a developed country in the future. Besides
Malaysia, the aforementioned information may be beneficial to
Asians worldwide who share a similar lifestyle and diet.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors' contributions
NA conceptualized the study and prepared the
original and final drafts. NM reviewed and edited the article. All
authors have read and approved the manuscript. Data authentication
is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018. GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ng CJ, Teo CH, Abdullah N, Tan WP and Tan
HM: Relationships between cancer pattern, country income and
geographical region in Asia. BMC Cancer. 15:6132015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ghoncheh M, Momenimovahed Z and Salehiniya
H: Epidemiology, incidence and mortality of breast cancer in Asia.
Asian Pac J Cancer Prev. 17((S3)): 47–52. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Azizah AM, Hashimah B, Nirmal K, Siti
Zubaidah AR, Puteri NA, Nabihah A, Sukumaran R, Balqis B, Nadia
SMR, Sharifah SSS, et al: Malaysian National Cancer Registry Report
2012–2016. National Cancer Institute. Ministry of Health;
Putrajaya, Malaysia: 2019, https://www.moh.gov.my/moh/resources/Penerbitan/Laporan/Umum/2012-2016%20(MNCRR)/MNCR_2012-2016_FINAL_(PUBLISHED_2019).pdfSeptember
17–2021
|
|
5
|
Razaleigh MK, Abdul Ghafar D, Salasiah
Hanin H, Fariza MS, Badlihisham MN, Muhammad Faisal A, Siti Rugayah
T, Zainab I, Ideris E, Anuar P, et al: The history of ethnic
relationship in Malaysia. Adv in Nat Appl Sci. 6:504–510. 2012.
|
|
6
|
Deniel A, Hakim NA, Md Nordin NA, Tg Abu
Bakar Sidik TMI, Subramaniam S, Kamaruzaman ND and Ros Suzana AB:
Ethnic differences in presentation of breast cancer patients
treated in Hospital Kuala Lumpur, Malaysia. Ann Oncol. 26 (Suppl
9):ix16–ix33. 2015. View Article : Google Scholar
|
|
7
|
Taib NA, Akmal M, Mohamed I and Yip CH:
Improvement in survival of breast cancer patients-trends over two
time periods in a single institution in an Asia Pacific country,
Malaysia. Asian Pac J Cancer Prev. 12:345–349. 2011.PubMed/NCBI
|
|
8
|
Ibrahim NI, Dahlui M, Aina EN and Al-Sadat
N: Who are the breast cancer survivors in Malaysia? Asian Pac J
Cancer Prev. 13:2213–2218. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bhoo-Pathy N, Hartman M, Yip CH, Saxena N,
Taib NA, Lim SE, Iau P, Adami HO, Bulgiba AM, Lee SC and Verkooijen
HM: Ethnic differences in survival after breast cancer in South
East Asia. PLoS One. 7:e309952012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Al-Naggar RA, Isa ZM, Shah SA, Nor MI,
Chen R, Ismail F and Al-Dubai SA: Eight year survival among breast
cancer Malaysian women in University Kebangsaan Malaysia medical
centre. Asian Pac J Cancer Prev. 10:1075–1078. 2009.PubMed/NCBI
|
|
11
|
National Registry of Diseases Office, .
Singapore Cancer Registry Annual Registry Report Trends in Cancer
Incidence in Singapore 2010–2014. (NRDO); Singapore: 2015
|
|
12
|
Department of Statistics Malaysia: Current
Population Estimates, Malaysia, . 2021.https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=155&bul_id=ZjJOSnpJR21sQWVUcUp6ODRudm5JZz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09September
19–2021
|
|
13
|
Shadiya MSB, Gogilawani W, Akbariah MM and
Saidatul S: Causes of breast cancer: Comparison between the three
races in Malaysia. J Health Sci. 2:19–29. 2012.
|
|
14
|
Hu S, Xu Y, Meng L, Huang L and Sun H:
Curcumin inhibits proliferation and promotes apoptosis of breast
cancer cells. Exp Ther Med. 16:1266–1272. 2018.PubMed/NCBI
|
|
15
|
Bachmeier BE, Mohrenz IV, Mirisola V,
Schleifer E, Romeo F, Hohneke C, Jochum M, Nerlich AG and Pfeffer
U: Curcumin downregulates the inflammatory cytokines CXCL1 and −2
in breast cancer cells via NFkappaB. Carcinogenesis. 29:779–789.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wei Y, Lv J, Guo Y, Bian Z, Gao M, Du H,
Yang L, Chen Y, Zhang X, Wang T, et al: Soy intake and breast
cancer risk: A prospective study of 300,000 Chinese women and a
dose-response meta-analysis. Eur J Epidemiol. 35:567–578. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rice S and Whitehead SA: Phytoestrogens
and breast cancer-promoters or protectors? Endocr Relat Cancer.
13:995–1015. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kuiper GG, Lemmen JG, Carlsson B, Corton
JC, Safe SH, van der Saag PT, van der Burg B and Gustafsson JA:
Interaction of estrogenic chemicals and phytoestrogens with
estrogen receptor beta. Endocrinology. 1399:4252–4263. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nakagawa H, Yamamoto D, Kiyozuka Y, Tsuta
K, Uemura Y, Hioki K, Tsutsui Y and Tsubura A: Effects of genistein
and synergistic action in combination with eicosapentaenoic acid on
the growth of breast cancer cell lines. J Cancer Res Clin Oncol.
126:448–454. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dampier K, Hudson EA, Howells LM, Manson
MM, Walker RA and Gescher A: Differences between human breast cell
lines in susceptibility towards growth inhibition by genistein. Br
J Cancer. 85:618–624. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Poh BK, Wong YP and Norimah AK: Postpartum
dietary intake and food taboos among chinese women attending
maternal and child health clinics and maternity hospital, Kuala
Lumpur. Mal J Nutr. 11:1–21. 2005.
|
|
22
|
Suzana S Jr, Azhar Y and Fatimah A:
Association between dietary fibre and cancer: A case-control study
in Malaysia. Malays J Nutr. 10:173–182. 2004.PubMed/NCBI
|
|
23
|
Heath AK, Muller DC, van den Brandt PA,
Papadimitriou N, Critselis E, Gunter M, Vineis P, Weiderpass E,
Fagherazzi G, Boeing H, et al: Nutrient-wide association study of
92 foods and nutrients and breast cancer risk. Breast Cancer Res.
22:52020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nurul Izzah A, Aminah A, Md Pauzi A, Lee
YH, Wan Rozita WM and Siti Fatimah D: Patterns of fruits and
vegetable consumption among adults of different ethnics in
Selangor, Malaysia. Int Food Res J. 19:1095–1107. 2012.
|
|
25
|
Mutalip MH, Kamarudin RB, Manickam M, Abd
Hamid HA and Saari RB: Alcohol consumption and risky drinking
patterns in Malaysia: Findings from NHMS 2011. Alcohol Alcohol.
49:593–599. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Asunta M: The alcohol problem in Malaysia:
The Globe. GAPA Bangkok consultation: Alcohol in Asia. (3-4)The
Global Alcohol Policy Alliance; London: 2001
|
|
27
|
Iwase M, Matsuo K, Koyanagi YNY, Ito H,
Tamakoshi A, Wang C, Utada M, Ozasa K, Sugawara Y, Tsuji I, et al:
Alcohol consumption and breast cancer risk in Japan: A pooled
analysis of eight population-based cohort studies. Int J Cancer.
148:2736–2747. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Parkin DM, Boyd L and Walker LC: 16. The
fraction of cancer attributable to lifestyle and environmental
factors in the UK in 2010. Br J Cancer. 105 (Suppl 2):S77–S81.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shariffah SSJ: Beliefs and practices
surrounding postpartum period among Malay women. Proc Social Sci
Res. 49–417. 2014.
|
|
30
|
Karimi E, Jaafar HZ and Ahmad S:
Antifungal, anti-inflammatory and cytotoxicity activities of three
varieties of Labisia pumila benth: From microwave obtained
extracts. BMC Complement Altern Med. 13:202013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Mainasara MM, Abu Bakar MF and Linatoc AC:
Malaysian medicinal plants' potential for breast cancer therapy.
Asian J Pharm Clin Res. 11:101–117. 2018. View Article : Google Scholar
|
|
32
|
Jamaludin N, Hasham R, Ware I, Sarmidi MR
and Abd Aziz R: Antiproliferative properties of Aqueous Labisia
Pumila extract on prostate cancer cell lines. J Teknologi.
77:61–66. 2015.
|
|
33
|
Shenouda NS, Zhou C, Browning JD, Ansell
PJ, Sakla MS, Lubahn DB and Macdonald RS: Phytoestrogens in common
herbs regulate prostate cancer cell growth in vitro. Nutr Cancer.
49:200–208. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lope Pihie AH, Zakaria ZA and Othman F:
Antiproliferative and proapoptotic effects of Labisia pumila
ethanol extract and its active fraction in human melanoma HM3KO
cells. Evid Based Complement Alternat Med. 2012:1234702012.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Patrick NO and Sophia OE: In vivo and in
vitro anti-asthmatic effects of dichloromethane crude extract from
the leaves of Labisia pumila. Global J Pharmacol. 6:126–130.
2012.
|
|
36
|
Amato P, Christophe S and Mellon PL:
Estrogenic activity of herbs commonly used as remedies for
menopausal symptoms. Menopause. 9:145–150. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen JY, Wang YH, Hidajah AC and Li CY: A
population-based case-control study on the association of Angelica
sinensis exposure with risk of breast cancer. J Tradit Complement
Med. 10:454–459. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhou WJ, Wang S, Hu Z, Zhou ZY and Song
CJ: Angelica sinensis polysaccharides promotes apoptosis in human
breast cancer cells via CREB-regulated caspase-3 activation.
Biochem Biophys Res Commun. 467:562–569. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhu H, You J, Wen Y, Jia L, Gao F, Ganeson
K and Chen J: Tumorigenic risk of Angelica sinensis on ER-positive
breast cancer growth through ER-induced stemness in vitro and in
vivo. J Ethnopharmacol. 13:1144152021. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yue GG, Wong LS, Leung HW, Gao S, Tsang
JY, Lin ZX, Law BK, Tse GM and Lau CB: Is danggui safe to be taken
by breast cancer patients?-A skepticism finally answered by
comprehensive preclinical evidence. Front Pharmacol. 10:7062019.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Al Shabanah OA, Alotaibi MR, Al Rejaie SS,
Alhoshani AR, Almutairi MM, Alshammari MA and Hafez MM: Inhibitory
effect of ginseng on breast cancer cell line growth via
up-regulation of cyclin dependent kinase inhibitor, p21 and p53.
Asian Pac J Cancer Prev. 17:4965–4971. 2016.PubMed/NCBI
|
|
42
|
Mohd Yusoff Z, Amat A, Naim D and Othman
S: Postnatal care practices among the Malays, Chinese and Indians:
A comparison. SHS Web of Conferences. 45:050022018. View Article : Google Scholar
|
|
43
|
Chen LW, Low YL, Fok D, Han WM, Chong YS,
Gluckman P, Godfrey K, Kwek K, Saw SM, Soh SE, et al: Dietary
changes during pregnancy and the postpartum period in Singaporean
Chinese, Malay and Indian women: The GUSTO birth cohort study.
Public Health Nutr. 17:1930–1938. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Desai G, Schelske-Santos M, Nazario CM,
Rosario-Rosado RV, Mansilla-Rivera I, Ramirez-Marrero F, Nie J,
Myneni AA, Zhang ZF, Freudenheim JL and Mu L: Onion and garlic
intake and breast cancer, a case-control study in puerto rico. Nutr
Cancer. 72:791–800. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Choudhry UK: Traditional practices of
women from India: Pregnancy, childbirth and newborn care. J Obstet
Gynecol Neonatal Nurs. 26:533–539. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
National Population & Family
Development Board of Malaysia, . 2004.http://www.frham.org.my/pdf/publication/Country%20Profile%20Final.pdfMarch
28–2020
|
|
47
|
Ishak S, Adzan NA, Quan LK, Shafie MH,
Rani NA and Ramli KG: Knowledge and beliefs about breastfeeding are
not determinants for successful breastfeeding. Breastfeed Med.
9:308–312. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Tan KL: Knowledge, attitude and practice
on breastfeeding in Klang, Malaysia. Int Med J Malaysia.
8:2009.
|
|
49
|
Tan KL: Factors associated with exclusive
breastfeeding among infants under six months of age in Peninsular
Malaysia. Int Breastfeed J. 6:22011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
El Khoudary SR, Greendale G, Crawford SL,
Avis NE, Brooks MM, Thurston RC, Karvonen-Gutierrez C, Waetjen LE
and Matthews K: The menopause transition and women's health at
midlife: A progress report from the Study of Women's Health Across
the Nation (SWAN). Menopause. 26:1213–1227. 2019.PubMed/NCBI
|
|
51
|
Ayida AW, Wan Nazimoom WM, Farihah HS and
Azian AL: Effect of ovariectomy Labisia pumila var alata
treatment and estrogen replacement therapy morphology of adipose
tissue in ovariectomized Sprague Dawley rats. J Med Biol Sci.
1:2006.
|
|
52
|
Fazliana M, Wan Nazaimoon WM, Gu HF and
Ostenson CG: Labisia pumila extract regulates body weight
and adipokines in ovariectomized rats. Maturitas. 62:91–97. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Nadia ME, Nazrun AS, Norazlina M, Isa NM,
Norliza M and Ima Nirwana S: The anti-inflammatory,
phytoestrogenic, and antioxidative role of Labisia pumila in
prevention of postmenopausal osteoporosis. Adv Pharmacol Sci.
2012:7069052012.PubMed/NCBI
|
|
54
|
Abdul Kadir A, Nik Hazlina NH, Wan
Mohammad WB, Mohd DM, Wan Mohammad WM, Hassan II, Shukor N,
Kamaruddin NA and Wan Mohamud WN: The effect of Labisia
pumila var alata on postmenopausal women: A pilot study. Evid
Based Complement Alternat Med. 2012:2165252012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Pardhe BD, Ghimire S, Shakya J, Pathak S,
Shakya S, Bhetwal A, Khanal PR and Parajuli NP: Elevated
cardiovascular risks among postmenopausal women: A community based
case control study from Nepal. Biochem Res Int. 2017:38249032017.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Masson W, Siniawski D, Lobo M, Molinero G
and Huerín M: Association between triglyceride/HDL cholesterol
ratio and carotid atherosclerosis in postmenopausal middle-aged
women. Endocrinol Nutr. 63:327–332. 2016.(In English, Spanish).
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Shuid AN, Ping LL, Muhammad N, Mohamed N
and Soelaiman IN: The effects of Labisia pumila var. alata
on bone markers and bone calcium in a rat model of post-menopausal
osteoporosis. J Ethnopharmacol. 133:538–542. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Fathilah SN, Abdullah S, Mohamed N and
Shuid AN: Labisia pumila prevents complications of
osteoporosis by increasing bone strength in a rat model of
postmenopausal osteoporosis. Evid Based Complement Alternat Med.
2012:9480802012. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Keat TB, Nik Mahdi NM, Basheer LM and Nik
Hussain NH: Effect of Kacip Fatimah (Labisia pumila) water
extract on mammographic density-A pilot study. Malaysian J Med Sci
Supplement. 14:51–51. 1p. 2007.
|
|
60
|
Yaghjyan L, Colditz GA, Collins LC,
Schnitt SJ, Rosner B, Vachon C and Tamimi RM: Mammographic breast
density and subsequent risk of breast cancer in postmenopausal
women according to tumor characteristics. J Natl Cancer Inst.
103:1179–1189. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Hou XY, Niu HY, Huang XL and Gao Y:
Correlation of breast ultrasound classifications with breast cancer
in Chinese women. Ultrasound Med Biol. 42:2616–2621. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ariff KM and Khoo SB: Cultural health
beliefs in a rural family practice: A Malaysian perspective. Aust J
Rural Health. 14:2–8. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Salihah Y, Siti Aishah H and Wan Norhayati
WO: Traditional and complementary treatments among Malay, Chinese
and Indian chronic diseases: A systematic review. Mal J Med Health
Sci. 15 (Suppl 1):S178–S183. 2019.
|
|
64
|
Muhamad M, Merriam S and Suhami N: Why
breast cancer patients seek traditional healers. Int J Breast
Cancer. 2012:6891682012. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Thirthagiri E, Lee SY, Kang P, Lee DS, Toh
GT, Selamat S, Yoon SY, Taib NA, Thong MK, Yip CH and Teo SH:
Evaluation of BRCA1 and BRCA2 mutations and risk-prediction models
in a typical Asian country (Malaysia) with a relatively low
incidence of breast cancer. Breast Cancer Res. 10:R592008.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Anderson GL, Limacher M, Assaf AR,
Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R,
Caan B, et al: Effects of conjugated equine estrogen in
postmenopausal women with hysterectomy: The women's health
initiative randomized controlled trial. JAMA. 291:1701–1712. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Devi CR, Tang TS and Corbex M: Incidence
and risk factors for breast cancer subtypes in three distinct
South-East Asian ethnic groups: Chinese, Malay and natives of
Sarawak, Malaysia. Int J Cancer. 131:2869–2877. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Boyle P: Triple-negative breast cancer:
Epidemiological considerations and recommendations. Ann Oncol. 23
(Suppl 6):vi7–vi12. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Leong SP, Shen ZZ, Liu TJ, Agarwal G,
Tajima T, Paik NS, Sandelin K, Derossis A, Cody H and Foulkes WD:
Is breast cancer the same disease in Asian and Western countries?
World J Surg. 34:2308–2324. 2010. View Article : Google Scholar : PubMed/NCBI
|