Introduction
Cervical cancer (CC) is the fourth most common
cancer in women. According to Globacon, in 2020, CC affected
604,127 patients and was responsible for 341,831 deaths (1). This disease typically occurs in
sexually active females aged 30–45, but also presents beyond this
age range. A number of well-established risk factors include a
positive human papilloma virus (HPV) test, multiple sexual
partners, smoking, early coitarche, lack of screening and
immunosuppression (2,3).
In the microenvironment of the cervix, a junction of
columnar epithelium representing the endocervix and squamous
epithelium representing the exocervix exists which is known as the
transformation zone and remains the most susceptible zone to
neoplastic proliferation in the cervix (4). HPV contributes to, but it is not the
sole contributor to the development of CC. In fact, only
approximately 5% of HPV infected individuals develop carcinoma yet
more than 90% of all cases of CC are attributed to HPV (5,6). It
should also be noted that not all HPV strains inevitably give rise
to cancer. HPV strains 6 and 11 may cause warts and papillomatosis
of the respiratory tract. HPV strains −16, −18, −31, −33, −45, −52,
−58 on the other hand are associated with carcinogenesis of the
cervix (7). HPV-16 and HPV-18
produce the E6 and E7 gene products, which in turn inhibit the p53
and Rb proteins respectively (8).
CC is often asymptomatic, allowing time for it to
progress to a more invasive malignancy. With the gradual
progression of the cancer, some symptoms emerge which include among
others abnormal vaginal bleeding, dyspareunia, abnormal discharge,
haematuria, urinary incontinence, lower abdominal pain and general
fatigue (9,10). The diagnosis for CC involves
initial screening with a Papanicolaou (Pap) smear/cytology which
has 55% sensitivity for CINII and 97% sensitivity for CINIII. If an
abnormality is detected on Pap smear, this is followed up by
colposcopy with biopsy, which is considered to be the gold standard
for definitive diagnosis. The Pap test demonstrates low sensitivity
for initial dysplastic events such as CINI, and therefore some
physicians may opt for colposcopy with biopsy after a positive HPV
test (11). Histological
examination of a cervical biopsy categorises CC into two types of
carcinomas: squamous cell carcinoma, which constitutes up to 85% of
cancer samples and adenocarcinoma which reaches up to 25% of cases
in certain areas (12). CC is
typically preceded by cervical intraepithelial neoplasia (CIN)
I–III, which can also be visualised on histology (13).
The staging system employed in CC follows The
International Federation of Gynaecology and Obstetrics (FIGO)
system and the management of CC is dependent on the staging of the
tumour based on the FIGO system (14). For IA cervical cancer, the
preferred mode of treatment is conisation which may include cold
knife conisation, loop excision conisation or laser (loop excision
is usually the treatment of choice at this stage) (15). Regarding stages IA2-IB2, a more
radical approach is taken, involving hysterectomy, bilateral
salpingectomy as well as possible bilateral oophorectomy and pelvic
lymphadenectomy (16). For stages
IB3-IVA, management includes external beam radiotherapy (EBRT),
intracavitary brachytherapy and concomitant cisplatin
chemotherapy.
Studies have shown that there is an unequal
distribution of CC among different parts of the world as well as
based on ethnic background (17,18).
This inequality may be due to a variety of factors such as lack of
education related to both HPV and CC, lack of screening, genetic
predisposition as well as exposure to more risk factors or cultural
beliefs in certain geographical regions; yet probably one of the
most important factors for a higher mortality rate in
underdeveloped countries vs. developed countries is the lack of
implementation of primary and secondary prevention programmes.
The aims of this narrative review are to examine
geographical differences in the epidemiology of CC, provide an
overview of the most effective primary and secondary preventive
measures available, describe the barriers existing in resource
depleted countries (at the health system, the community and the
individual levels) and describe the possible strategies that can be
developed to further improve prevention and diminish the impact of
this gynaecological malignancy.
Epidemiology and geographical inequalities
in the burden of CC
The global age-standardised incidence for cervical
cancer for the year 2020 stands at 11.1 per 100,000 women while the
age-standardised mortality rates is 14.8 per 100,000 women, with
substantial variations from country to country (19). It is pertinent to note that while
the worldwide prevalence of CC was reported as 604,127 cases in the
year 2020, 85% of the cases were reported in low- and middle-income
countries (20).
The general trend elicited is that the higher the
Human Development Index (HDI), the lower the incidence and
mortality rates of CC. The HDI is a measure of a country's
successes based on a range of social and economic factors. A value
of 0 indicates poor performance, while a value of 1 indicates
extremely high development. The main components of this index lie
in the public health of the nation, education attainability and
living standards (21). Some
examples which highlight this HDI based inequality are Malawi,
Zambia, Zimbabwe and Tanzania which reported an astonishing
incidence of over 40 per 100,000-woman years as well as an HDI
below 0.5 in 2018. In the same year, approximately 84% of CC cases
and 88% of CC related deaths occurred in countries with an HDI
below 0.8. Malawi and Eswatini both have an HDI below 0.65 and
exhibited an incidence of 72 and 75 per 100,000-women years in 2018
respectively. Meanwhile China and India have their HDIs fluctuating
between 0.65 and 0.8 and demonstrated an incidence of 11 and 15 per
100,000-woman years respectively in the same year. These numbers
can be immediately contrasted with a high HDI country such as
Germany (0.95), where CC incidence stood at roughly 8 per
100,000-woman years. Interestingly, China and India together
contributed towards 35% of the disease burden worldwide. At the
same time, countries with a high HDI over 0.8, such as Australia,
New Zealand and Finland, exhibited a 2–4-fold lower incidence and
mortality standing roughly at 7 and 3 per 100,000-woman years
respectively when examined during the same year (22).
If trends are to be examined, high HDI countries
such as Switzerland exhibited a decrease in CC incidence, from
0.98% in 1993–1997 to 0.37% in 2008–2012 (23). The initial incidence was already
relatively low, but over the years it decreased further. Looking at
middle to high HDI countries such as Singapore, a larger drop can
be observed: the incidence experienced a 9.5-fold decrease from
44.8 per 100,000-person years in 1968 to 4.7 per 100,000-person
years in 2012 in ethnically Indian women residing in Singapore. It
is also remarkable that during this time period the decrease in
incidence per 100,000-person years did not even plateau (24). Unfortunately, the trend differs for
low HDI countries such as Uruguay. In the latter, there was a
shallow decline in the incidence of CC from 17.6 to 14.8 per
100,000-person years in the period of 2002–2015. One could argue
that such a drastic difference in incidence reduction per person
years between the Singaporean subpopulation and Uruguay is due to
examining a larger time frame in the former study, so it would be
unfair to draw conclusions about Uruguay since the study was
shorter. This however is a false assumption since the decrease in
incidence of CC for the Singaporean population between 2005 and
2010 was 50% (from 10 to 5 per 100,000-person years), while the
decrease in the incidence in CC in the Uruguay population mentioned
above was 16% during the period of 2002 and 2015. Hence, in a high
HDI country there was a larger incidence reduction of CC during a
period of 5 years compared to a country with low HDI country during
a period of 13 years (25). The
plateau in incidence for Uruguay and other low HDI countries,
despite globalisation of HPV vaccinations and updated screening
protocols, warrant a discussion regarding geographical
inequalities.
Studies have shown that there is an unequal
distribution of CC among different parts of the world also based on
ethnic background. A study conducted during the period of 1999 to
2015 has shown that African-American women have substantially
higher incidence (10.8 per 100,000) and mortality (4.4 per 100,000)
rates than White American women (7.4 per 100,000; 2.1 per 100,000
respectively) (26). This is
despite both groups of women residing in the Untited States of
America, where screening and vaccination programs are in place. In
comparison, rates in Sub-Saharan Africa are even more dismal: CC
constituted the number one cause of death among women with a
mortality rate of 30 per 100,000 for the year 2018 (27). This inequality may be due to a
variety of factors such as lack of education in the field,
genetics, exposure to more risk factors or cultural beliefs in
certain geographical regions; yet probably one of the most
important factors for a higher mortality rate in women in
Sub-Saharan Africa compared to Caucasian women residing in first
world countries is the lack of a stable implemented screening
program or inaccessibility to such a programme in the former.
The worldwide prevalence of HPV stands at 12%, while
the prevalence in regions such as sub-Saharan Africa reaches 24%.
According to WHO, HPV infection with genotypes 16 and 18 is a
direct cause of 70% of CC cases. In low HDI countries such as
Ethiopia (0.49), a total of 90.2% of CC cases are attributed to HPV
16 and 18, 20% higher than the global average (28). This raises the issue of lack of
vaccination against HPV strains in such geographical areas, which
could have reduced the incidence of CC.
Primary prevention and barriers faced by
developing countries
The purpose of primary prevention is to prevent a
disease from ever occurring. Thus, primary prevention targets
healthy individuals and focuses on interventions that are performed
before development of a condition and include psychoeducation and
vaccination (29). The European
guidelines offer randomized control trial (RCT) and expert opinion
supported recommendations for primary prevention, with the focus on
HPV vaccination. The guidelines state that HPV vaccinations are
best implemented through largescale national programmes, with the
target age for vaccination being 10–13 years of age. Monitoring and
evaluation of the safety and effectiveness of the HPV vaccine
should also be implemented in for long term evaluation and hence
improvement of the vaccination programme in each country. The
coverage target was set at a minimum of 70% with a strong
preference for over 80%. Lastly, it was recommended that European
countries focus on synergising HPV screening and vaccination as a
potential method for lowering the financial burden of HPV related
disease (30).
Vaccinations
The most effective method for CC primary prevention
is HPV vaccination. The Food and Drug Administration has approved
three different vaccines Cervarix, Gardasil and Gardasil 9
(31). Cervarix is a bivalent
vaccine that covers HPV 16 and 18, the two most commonly involved
strains in CC pathogenesis. Gardasil on the other hand is
quadrivalent, covering for HPV 6, 11, 16 and 18. In the past few
years, HPV 31 and 33 have emerged as important types with higher
predictive values than HPV18 in causing CC. Specifically, studies
conducted in New Mexico and Sweden have shown that HPV 31 and 33
have a higher positive predictive value for CIN2+ and CIN3+
compared to HPV18. HPV 39, 56, 59, 66 and 68 have been shown to
have an ‘intermediate risk’ and HPV 66 has been shown to carry very
little risk. Lastly, Gardasil 9, offers a more extensive spectrum
of coverage with the addition of HPV 31, 33, 45, 52 and 58 to the
list of strains. Vaccination does not only protect from HPV derived
CC, but also yields protection from pre-cancerous and cancerous
lesions of the lower genital tract, anal area, head and neck, as
well as prevention of genital warts (32). Furthermore, studies proposed that
even late vaccination provides a better population-based protection
against HPV as opposed to no vaccination (33). Therefore, efforts should be
invested to further develop vaccines that will cover a greater
range of HPV strains involved in cervical carcinogenesis (34).
When vaccination levels are compared across
countries there is a clear discrepancy seen between high HDI and
low HDI countries. A study estimated that in 2019, New Zealand and
Australia vaccinated 86% of females with the first dose and 77%
with the second dose. During the same year, Sub Saharan Africa as a
whole vaccinated 31 and 20% of females with the first and second
doses respectively. The study also highlighted that during the same
year higher HDI countries such as in the Untited States of America
and New Zealand had a ratio of males to females getting the
vaccination closer to 1, meanwhile countries like Panama and
Uruguay had ratios of male to female vaccination of 0.6 and 0.2
respectively (35).
Barriers to vaccination in low-income
countries
This section tackles barriers associated with
primary prevention strategies such as: cost of vaccination and
implementation of such programs in low-income countries, sex as a
barrier to male vaccination uptake, distance and transportation
related issues leading to lower uptake of vaccination and lack of
knowledge and stigma related to HPV vaccination in societies where
this is still viewed as a taboo topic.
Financial cost of vaccination
The costs of vaccinations may also pose a major
barrier to lowering the incidence of CC. In a study conducted among
Chinese women, the high cost of the HPV vaccine served as one of
the components of women's hesitancy to get vaccinated (36). This obstacle applies to several low
HDI countries in which the individuals are expected to cover the
cost of the vaccination. Studies have shown that governmentally
sponsored programmes can be cost effective. In a study conducted in
Thailand it was shown that if a catch-up program was implemented to
vaccinate young women who were not previously vaccinated, it would
cost less than 10,000 Thai Baht per Quality-of-Life Points
(QUALYs). The recommended threshold for Thailand according to its
government stood at 160,000 Thai Baht per QUALY proving that the
implementation of a vaccination program would be cost effective
(37). Therefore, it is important
to consider the ultimate benefits of developing vaccination
programmes for the health outcomes of the general population and
the cost-effectiveness of such programmes.
Sex and HPV vaccinations
HPV vaccination was initially introduced in the
Untited States of America in 2006 and was approved as a ‘females
only’ vaccine since its aim was the prevention of CC. Following the
initial introduction of the vaccine to women, it was soon realised
that the latter did not stop men from infecting women with the
virus and vice versa, and it became clear that it was pertinent to
have both sexes protected. The initial notion was that if all women
were vaccinated the latter could provide herd immunity for men, but
this assumption was false (due to incomplete vaccination in all
females) as well as the fact that homosexual men would still be
vulnerable to infection with HPV (38). Therefore, in the year 2009, HPV
vaccination was approved as a sex-neutral vaccination. The current
guidelines by the Advisory Committee on Immunization Practices
recommend vaccination of young girls and boys at age 9–14 years old
with the two-dose option (39).
While low rates of HPV vaccination generally may be
a problem of more rural communities, the feminisation of HPV
persists in high HDI countries. According to a study in the Untited
States of America in 2014 approximately 60% of females aged 13 to
17 received at least one dose of the vaccine compared to only 42%
of their male counterparts. The catch-up programme in 2012 showed
even lower levels of vaccination with 34% of women and 5.5% of men
aged 18 to 26 respectively (38).
School based vaccinations should be considered in an
effort to increase vaccination rates among young people. By
following a school-based vaccination programme, Australia was able
to reach a vaccination coverage of 86% of females and 78% of males
respectively. This success could also be attributed to strong
community acceptance for the vaccine as a tool for cancer
prevention in both sexes (40).
Distance and transportation
Another point of concern for low HDI country parents
was having to take their child out of school for multiple doses of
the vaccine, especially taking into consideration the transport
limitations addressed above (41).
Lack of knowledge and stigma
Studies have reported that parents and spouses of
women participating in prevention programs in resource-depleted
settings were concerned regarding HPV vaccination since in their
opinion this would affect the fertility of the women. Some also
believed that HPV vaccination had association with the human
immunodeficiency virus (HIV), which is also stigmatised and hence
served as a barrier to screening. Some parents also believed that
intimate examinations and HPV vaccination in their daughters would
initiate early coitarche and this led to reluctancy in medical
follow-up. In these communities, diagnoses of CC may also be viewed
as a death sentence despite advancements in treatment, so some
women opt out of prevention programs under the belief that they
would rather die not knowing or that it is a religion-guided fate
(41). Another misconception
conveyed is that only women need to get the vaccine as this is
purely a biologically female problem (42).
Psychoeducation
Psychoeducation of the general population about CC
and its associated risk factors is a form of primary prevention
that is not given enough attention. To highlight this, a study in
Kenya was performed in which one third of the interviewed women
aged 15–24 did not know what CC even is (30). Lack of education and poverty are
greatly associated with this knowledge gap, but even high HDI
countries have individuals with limited understanding on how to
protect themselves from CC. Interestingly, according to a study in
the United Kingdom, information leaflets increase knowledge on CC
symptomatology, lower overall anxiety and prompt help-seeking
(43). Nevertheless, some
individuals may find CC related information too challenging and
hence feel discouraged to partake in HPV vaccination or screening.
For example, another United Kingdom based study aimed to identify
the challenges associated with the National Health Service leaflet.
Some of the main issues encountered included not understanding the
benefits or results of screening, the risks of screening and HPV
infection, or complex terminology (44). Other leaflets in Scandinavian
countries such as Norway, Finland were reported to not address the
HPV related information that was truly sought after by the
audience, such as psychosocial information or unbiased alternatives
to vaccination and screening (45).
Ngu et al (46) conducted a study in which
participants were allocated into groups. The firs group was offered
counselling along with a leaflet, whereas the second group was only
provided with a leaflet. The study then compared CC related
anxiety, depression and screening related knowledge levels in the
two groups of women. In this study, the two groups were followed up
with a questionnaire pre-intervention, a week after and 6 months
after the intervention. The researchers reported that the
counselling group had a higher score in knowledge on screening and
HPV at 1 week follow-up; yet at a 6-month follow-up both the
intervention and control groups had approximately the same level of
knowledge on CC screening and risks. Meanwhile CC related anxiety
gradually decreased in both groups equally (46). This trial demonstrates that it is
not mandatory to implement costly information services such as
personal counselling, and that even leaflets with basic guidelines
could be impactful in low HDI regions. Very limited information can
be found on the effects of psychoeducational programs and leaflets
on populations in resource depleted settings, which implies that
psychoeducation programmes are not common in low income countries.
Of course, such programs may not be the sufficient to achieve CC
elimination, but they may be beneficial. Therefore, educational
interventions from a young age could be a powerful tool for
prevention of CC incidence.
Barriers to psychoeducation
The cost of educational programme can be a
significant obstacle to lowering the burden of CC. A randomised
cluster trial among uninsured Hispanic women examined the benefits
of having a group-based educational session which is also
culturally appropriate by a professional in the field.
Additionally, the study also provided free of charge screening for
all the women in the study. While the benefits of these
interventions were clear, the funding was provided by the Institute
conducting the research (47).
Hence, the cost of such interventions would be something
inaccessible for these women in their normal setting. Another study
in Peru highlighted that while in person educational interventions
may be costly, an online alternative could have been a solution.
However, some young women in low HDI countries do not even have
access to internet, let alone information on CC primary prevention
(48).
Secondary prevention and challenges faced by
developing countries
Secondary prevention emphasizes early disease
detection and its target is healthy-appearing individuals with
subclinical forms of the disease. Secondary prevention screens to
identify preneoplastic high grade lesions such as CIN II and III as
well as identify CC in its earliest form, preferably before the
onset of symptoms and signs, with screening being the most widely
established form of secondary prevention in the context of CC
(29). It is crucial for screening
to cover a high coverage of the target population, specifically in
the age groups of 25 to 65 years of age. Secondary prevention
should also involve compliance with repeating screening tests
according to the CC prevention program of the country as well as
monitoring the results for comparison in order to see if there is
evolution of any possible lesions and following up carefully
screen-positive women.
Screening methods for CC range from conventional
methods that have been available for many years, such as cytology,
HPV testing and visual inspection with acetic acid (VIA), to more
recent advancements such as self-sample kits and screening for
methylation markers which are still undergoing research. Cytology
is the most conventional method of secondary prevention due to its
high uptake in several countries, while HPV testing for DNA
sequences of the 12/14 high-risk HPV types is still under
implementation in many countries (49). Self-sample kits constitute a
different way of collecting cervico-vaginal cells (suitable for HPV
testing and not for cytology) and represents a more comfortable
method to increase women's participation to screening especially
among stigmatised populations (50). While methylation markers are under
study and currently used for triage of screen-positive women and
are not as a primary screening tool. Since they are expensive and
require well equipped laboratories, they are less suitable for
middle-low income countries; yet more research in this field could
be beneficial for CC patients. Different methods of screening
therefore entail varying costs, and different requirements for
infrastructure as well and expertise of personnel, which may be
important obstacles in the implementation of successful screening
programs in developing countries (49).
There is variation in screening uptake in Europe,
with some countries having a fully implemented nation-wide
screening program such as the Netherlands and Turkey, while France
is still implementing a screening program that would be accessible
to hard-to-reach populations, reduce CC incidence and deaths by
30%, and reach an 80% screened population coverage over the next 10
years from 2019 (51,52). Belgium and Switzerland have had a
mean stable screening coverage of 70.9 and 73.1% during 2008–2012,
respectively (53).
In the Untited States of America there was a decline
in in overall screening in all age groups from 2010–2014. For
example, women aged 30–39 had a decrease in screening uptake from
88 to 77.5% over the 4-year period, yet rates of co-testing were
the highest compared to all other age groups standing at 44.4% in
2014 (54). The significance of
screening is supported by a population-based control trial in New
Mexico which highlighted that there were 83 and 48% lower odds
ratio of developing non-localised CC and localised CC for women
screened 3 years prior to detection compared to women who did not
undergo screening (55). Another
retrospective study on a population also in New Mexico showed that
out of 504 women diagnosed between 2009–2016, only 36% were
screened at some point in their life. This result again reinforces
the point of early detection and treatment as key for preventing
debilitating complications and indeed this study confirmed that
screening could have prevented 35% of these cases (56).
A cluster randomised trial in India with over
130,000 women also highlighted the benefit and statistical
significance of screening for CC. There were 34 deaths from CC in
the HPV testing group vs. 64 deaths in the control group, hazard
ratio 0.52; 95% confidence interval 0.33–0.83 (57). Bhutan on the other hand was one of
the first low to middle income countries to introduce a national
HPV vaccination program in 2010, which also became sex neutral in
2020. However, despite being free of charge, screening uptake was
only 59.2% among woman aged 18–69 years old and only increased to
66% in 2017, supporting the need for greater efforts to be
implemented to achieve a higher vaccination rate (58).
Apart from lowering disease burden and mortality,
screening methods are economically more efficient than detecting
the cancer at later stages and resorting to more costly, technical
treatments. In fact, in the Untited States of America, it was
estimated that a perfect compliance to screening at 3-year
intervals would increase the incremental net monetary benefits from
$759 to $1,645 as well as gain cheaper QUALYs (59).
Recent developments in screening
methods
Cytology
Cytology has been a conventional method of screening
since the 1940s, with many countries such as the UK and US
developing screening programs based around this test.
Unfortunately, though, this screening method has plenty of
drawbacks such as high false negative rates due to sampling and
interpretation errors, as well as artefacts impeding visualisation
of the samples. This led to the emergence of alternative
cytology-based techniques such as liquid based cytology, which
holds numerous advantages over the conventional method. It has been
shown to be faster, more efficient, more accurate, with fewer
artefacts that could obscure the results as well as an overall
higher detection rate of 97.60% as opposed to conventional cytology
with a 71.96% detection rate respectively (60). It has been estimated that the
liquid-based preparations have a sensitivity of 61–66% and a
specificity of 82–90% as opposed to the conventional cytology
preparation which has sensitivity of 51% and specificity of 57%
(61). It has also been suggested
that double reading of cytology slides could be implemented to
avoid missing out on potential high grade squamous intraepithelial
lesions (HSIL+). A study conducted in Mexico reported that 3,914
women with positive high-risk HPV were triaged with liquid-based
cytology. The study detected a 20.9% increase in HSIL+ cases when
double reading was done (62).
Visualisation with acetic acid or
Lugol's iodine
Another widely applied form of screening is
visualisation with either acetic acid or Lugol's iodine, which is
utilised extensively even today in marginalised populations. The
technique has numerous benefits such as low cost, safety, immediate
real time results permitting a single visit, as well as the
possibility for a screen and treat approach without the fear of
losing patients to follow-up (63). A further advantage of this
technique is that it can be performed by healthcare personnel such
as nurses and midwives after short training programs, without the
need for a doctor to be present for the procedure to be
implemented. This is especially crucial in resource depleted
countries. The most remarkable limitation of this technique lies on
its sensitivity and specificity, which were reported to be only
69.6 and 51.0% respectively for lesions of CIN II and above in a
study carried out in Kenya (64).
These rates are lower than the sensitivity and specificity of
traditional liquid-based cytology. Another drawback may be that the
healthcare personnel performing the technique may not be
experienced enough to distinguish VIA positive from VIA negative
patients. Recently in a study by Kudva et al (65) an Android Device based screening
method was proposed to address this issue. The novel technique
suggests that during VIA examination the health care provider uses
a speculum with an Android device attached to acquire images of the
cervix prior to and after acetic acid application, as well as the
patient's identification details. Upon acquisition, these images
are sent to a medical expert in the field, who after examination
deems them VIA positive or negative. In a clinical study involving
more than 100 women in India, it was found that the algorithm
offered a sensitivity of 99.05% and a specificity of 97.16%
(65).
HPV DNA genome assays
Testing for high-risk HPV genomes is a relatively
reliable option for detection of CIN. Despite studies demonstrating
that HPV testing has a lower specificity (89.9%) than cytology
(96.3%) for CINII, this screening method still has a number of
advantages (66). However, in
accordance with the most recent guidelines, primary HPV testing
must be performed by assays targeting all the high-risk types (HPV
16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 68), that have been
clinically validated according to the international recommendations
published in 2009 and in a recent study by Arbyn et al
(67), a list of 11 DNA assays
fulfilled all requirements in order to serve as a primary screening
tool.
Ronco et al (68) conducted a pooled analysis of 4
major European trials comparing HPV testing to cytology. The
results of this study showed that where cumulative incidence was
investigated, HPV screening was superior to cytology at 3.5 and 5.5
year follow-up. The experimental group (HPV screening) and control
group (cytology screening) had to have negative tests at the
starting point. At the 2 follow-ups the experimental group had a
cumulative incidence of CC of 4.6 and 8.7 per 100,000 women while
the cumulative incidence of the control group was 15.4 and 36.0 per
100,000 women respectively. Therefore, there was a discrepancy of
approximately 70% across the two methods (68). It should be noted that HPV
screening offers the option of self-sampling for HPV, thereby
eliminating the need for a health care provider and the time
consuming and possibly anxiety-inducing waiting period for the
patient's appointment. This could be particularly relevant for
women from backgrounds in which such procedures are highly
stigmatised.
An example of testing for HPV DNA includes the
careHPV testing system (Qiagen), which can evaluate 90 samples from
patients simultaneously. It is a fast and portable system designed
specifically for low-income countries. A prospective cohort study
investigated whether self-sampling specimens were of lower quality
than physician obtained specimens. However, the analysis of the
results showed that there was little difference in sensitivity
between the two groups; yet the comfort level of the self-sampling
group was significantly higher (69). Another study held in Vancouver also
aimed to test the feasibility of using self-assessment kits in
women for detecting HPV DNA. Women from shelters and women centres
were recruited and 28.5% of these women tested positive for the
virus. Approximately 14% of the participants never had a
cytological analysis before compared to the local general
population in which 8.3% never carried out cytology (70). Hence this screening method should
be considered for implementation in certain geographical regions
with higher stigma surrounding collecting cervical swabs.
Recently efforts have been made to develop tests to
investigate the presence of HPV in the urine. A study in the UK
compared the presence of HPV in urine vs cervical samples. The
results of the study showed that the detection of HPV in the urine
was comparable to the detection of the virus in cervical samples;
yet urine samples had lower sensitivity. Despite the lower
sensitivity, developing methods that detect HPV in urine may prove
useful for women not attending cervical screening (71).
One noteworthy drawback in HPV testing alone as a
primary screening test is the proportion of women with a positive
result due to only a transient infection with a viral HPV strain,
which however may not be clinically relevant. To exemplify this, in
a study of over 30,000 screened women 11% were initially shown to
be HPV positive but upon subsequent re-testing the prevalence of
high-risk HPV was 1.5% (72). Part
of the decrease could be attributed to the fact that general HPV
screening is not specific enough and will identify all types of HPV
strains instead of only the high-risk strains.
Based on the above-mentioned data, one could suggest
that combining 2 high sensitivity and specificity screening methods
would yield better prospects. In a study conducted in Mexico 3
screening groups (liquid-based cytology, HPV genotype 16/18
screening and both combined) were compared and the respective
sensitivity and specificity for each of the 3 groups were 42.9 and
74%, 58.3 and 54.4%, 86.6 and 34%. The referral rate for colposcopy
as the next step was 29% for the group with both screening methods
as compared to liquid-based cytology alone which was 12% (73). Meanwhile another study in New
Mexico has shown that in women aged 30–64 years with negative
cytology, the proportion of screening tests that were co-tests
(i.e., using two screening methods instead of one) rose from 5.6%
in 2008 to 84.3% in 2019. However, despite the increase in
co-tests, it has been demonstrated to be unnecessary in primary
screening, since it does not increase sensitivity and does not
affect specificity while at the same time it increases the
financial cost and may cause a major financial impact especially
for low HDI countries (74).
A promising advancement in tertiary prevention is
the combination of HPV screening along with p16INK4a immunostaining
which is a promising biomarker for the triage of HPV positive
women. Analysis from trials suggests that using these 2 methods
simultaneously vs. using cytology alone results in a 53% higher
detection rate of CINII-CINIII (75). However, this is still a novel
screening suggestion and warrants further trials. p16INK4a
immunohistochemistry also plays a role on classifying CINII as
either high grade or low grade, which can be particularly relevant
for women under 30 years old since low grade CINII in this age
group commonly relies on surveillance as opposed to more radical
interventions. The p16 immunohistochemistry positivity was
associated with higher severity CIN and higher risk HPV strains
with P-value being below 0.001 in studies, which is beneficial
information in terms of patient management (76). A particularly interesting aspect of
p16 immunohistochemistry in another study was that it was positive
in CC in cases where HPV was negative. This indicates that p16
immunohistochemistry could be possibly used as a screening marker
when other more conventional tests fail (69). However, there are only a few RCTs
to assess the efficacy of implementation of these particular
sequences of tests, which WHO acknowledges as a field for further
investigation.
HPV RNA assays
Research is currently conducted to investigate
whether HPV RNA assays can be used as an adjunctive method for
cervical cancer screening. A study has shown that the specificity
for HPV RNA assay was 96.3% compared to the specificity of ordinary
HPV DNA assay which was 94.8%. These results support the use of RNA
assays as an effective concurrent CC screening method to be used
alongside other more conventional screening methods that have high
sensitivity but lower specificity (70). Another study evaluated the accuracy
of the mRNA HPV biomarker in cervical smears to identify cervical
intraepithelial neoplasia (CIN) 2 or 3 and cervical cancer. The
results showed that the HPV mRNA test exhibited overall percentage
agreement with histological diagnosis of 89.8%. It was concluded
that the HPV mRNA assays may be an adequate tool in the secondary
screening of cervical cancer (77).
Methylation biomarkers
A new field of investigation lies in the emergence
of methylation markers as a screening method for CC. Over the last
few years, it has been noted that alterations in host and viral DNA
methylation levels occur during the development of the carcinoma,
so establishing the specific changes in the DNA methylation
involved could provide insight on early detection and treatment
(78).
A study among Slovenian HPV positive women was
carried out to screen for certain clusters of methylation markers
and yielded some promising results. Methylation markers C13orf18,
EPB41L3, JAM3 had 80% sensitivity and 66% specificity for CINII and
greater, while the SOX1 and ZSCAN1 combination demonstrated 63%
sensitivity and 84% specificity for the same CIN type. Furthermore,
the markers for both groups had higher sensitivity as the neoplasia
progressed from CINII to CINIII (79). Another study investigating the
methylation status of PAX1, ZNF582, SOX1, and NKX6-1 found that
dual methylation of PAX1 and ZNF582 showed a 100% association with
cervical pathological processes. The sensitivity and specificity
for these markers in identification of CINIII were 78.85 and 73.55%
respectively (80). It is worth
noting that methylation marker studies aside from being very
specific and sensitive, they can accurately detect CIN3 and
malignancy irrespective of geographic context and setting (81).
In a blinded case-control study, methylation markers
as a screening tool were compared to HPV with cytology screening
based on sensitivity and specificity. The results demonstrated that
the sensitivity and specificity for CINIII methylation markers were
93.2 and 41.8% as opposed to combined HPV and cytology which were
86.4 and 49.8% respectively (82).
These results propose that methylation markers may be more
sensitive than conventional CC screening tests. In another study,
the methylation status of selected sites on HPV16 and human genes
in DNA were examined. The results showed that methylation of viral
HPV16L1 and host sites, EPB4L3 and LMX1, strongly discriminates
CIN2/3 from NILM/CIN1 and cancer from CIN2/3 and may therefore be
used as both a diagnostic as well as a prognostic marker (83). Despite the promising results,
plenty of work persists in identifying the most sensitive cluster
of methylation markers that would be predictive of CC at earlier
stages.
Barriers to screening in low resource
countries and strategies for improvement
European guidelines offer ample information for
screening strategies at country level such as which screening tests
to utilise, age range for screening, management upon positive
tests, but it is up to each individual country to integrate these
costly recommendations. Upon diagnosis of CC there are two clear
groups identified: women of higher socio-economic status who test
positive early and women with a vulnerable socio-economical profile
who often test positive further in the course of their disease. In
European countries this disparity is addressed via individual
invite of the target population to screening based on a central
nation registry, which insures equal access to the screening
programme. Low income countries face higher difficulty due to
financial limitations and higher burden of CC and still have room
for improvement. Adequate targeting of infrastructure, geographical
inaccessibility, structured time-management in clinics, patient
education and effective communication between provider and patient,
combination of vaccination and screening, analysing and improving
screening programmes could offer considerable improvement in
screening in vulnerable countries (84).
Lack of infrastructure and financial
resources
Lack of infrastructure and limited financing may
pose a challenge for screening. In a study comparing resources for
screening in hospitals in Eastern, Southern and Central Africa, it
was found that some financial limitations persist in these areas.
In some Tanzanian hospitals for example, there was a shortage of
fixating agents for cytology. Other hospitals also reported lack of
cytology technicians. Out of the 12 African hospitals examined only
2 offered cryotherapy and loop excision, meanwhile all the others
could only offer core biopsy (85). Another study in rural Kenya
provided evidence that lack of staff, inadequate training, limited
space, lack of supplies for screening lack of an autoclave were
common challenges. Moreover, the majority of staff members desired
more training in the field (86).
Geographic accessibility burden
In some low HDI countries, reaching a facility with
a screening programme may be a considerable obstacle. A study in
Mexico showcased that woman who resided in rural areas had a
significantly greater geographic accessibility burden when compared
to nonrural areas (4.4 vs. 2.5 km for screening; 9.9 vs. 4.2 km for
colposcopy; and 14.8 vs. 6.6 km for precancer treatment services,
all P<0.001).
Furthermore, women in rural areas had to cover an
extra 5.7 and 8.2 km for access to colposcopy and precancer
treatment services respectively (87). Another study in Kenya showcased
that some women needed up to 8 h to travel to the nearest screening
site as well as rely on taxi services. The cost of the taxi itself
would be equal to the wages a woman would make in agricultural work
(88). Therefore, lack of
transportation should also be considered as a barrier.
Waiting times in the clinic
The waiting time in rural clinics may also be an
obstacle to screening. For example, in a study in Serbia it was
shown that although medical personnel were available, waiting time
for screening could take up to 4 h. Apart from having to wait in
overcrowded waiting areas, women felt that the providers did not
answer their queries or show the anticipated respect to the
patients, which also contributed to women not wanting to attend
follow-up appointments (89).
Lack of trust of patients to
healthcare teams
The study by Urasa and Darj (90) conducted in Tanzania addressed the
lack of knowledge of nurses regarding the aetiology of CC and how
the latter hindered the trust of the patients. Lack of knowledge
from the medical personnel made the women more reluctant to undergo
screening, especially since this is viewed as a taboo topic in the
community (90). The study
emphasised the importance of training and continuous professional
development of the healthcare team involved in CC screening.
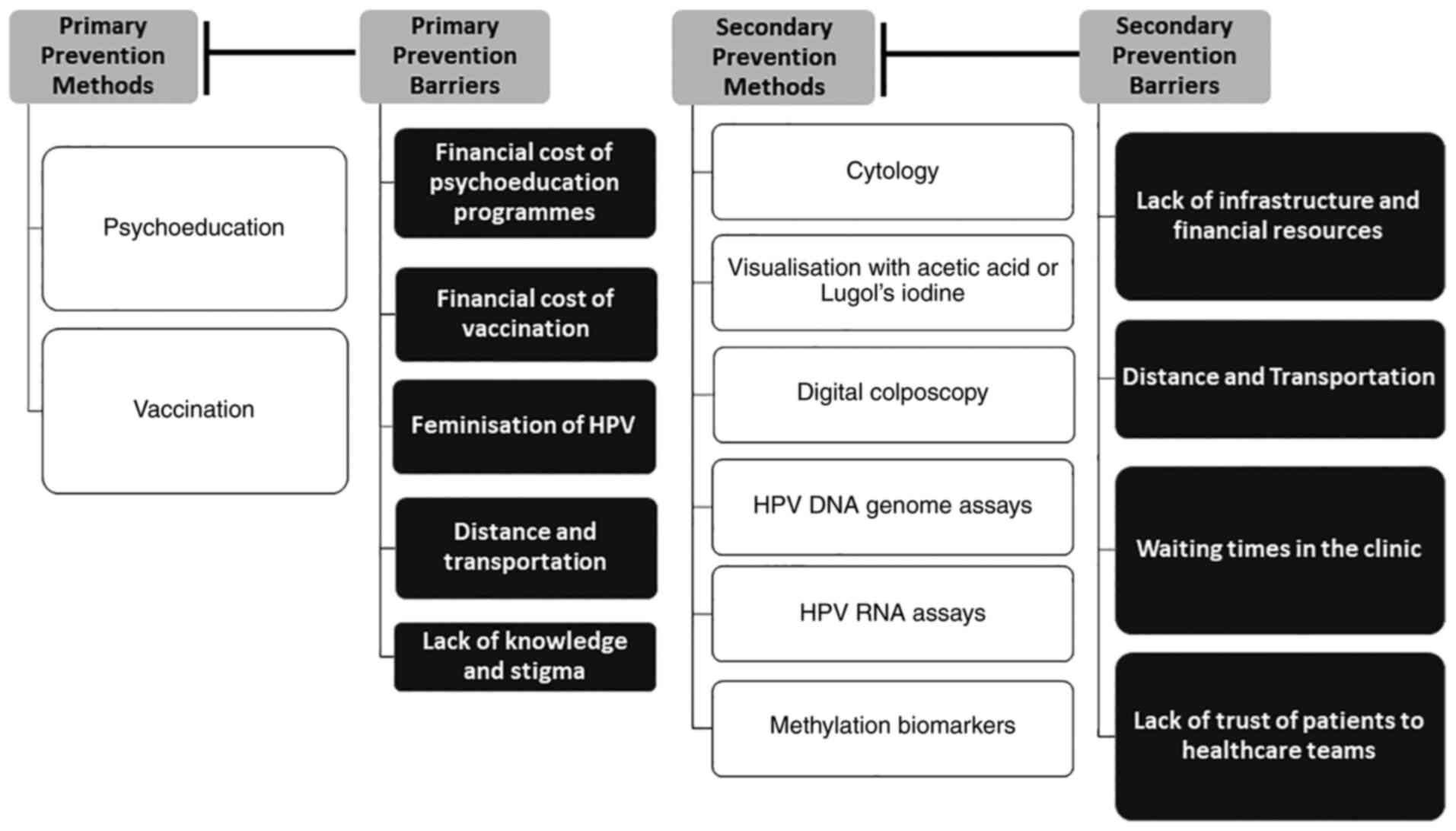
Conclusion
Despite CC contributing so greatly to the overall
cancer mortality rate, it is also one of the most well researched
cancers, with a plethora of prevention methods. It is clear that
there is a disparity in primary and secondary prevention programmes
in high vs. low HDI countries. Despite the development of effective
methods of primary and secondary prevention, numerous obstacles are
faced which should be addressed to ensure the prevention programmes
are effective (Fig. 1). Lack of
psychoeducation, access to vaccination, stigma but mostly the lack
of implementation of a stable and accessible screening program in
low HDI countries due to the lack of infrastructure and financial
costs involved is the epicentre of the problem. Research has
focused on addressing the needs of developing countries by trying
to develop novel and economically more cost-effective and
accessible screening methods. The effectiveness of vaccines for CC
as well as the multiple screening options related to it, should
call for immediate enforcement of well-structured and easily
accessible primary and secondary prevention programmes by policy
makers, especially in more resource depleted countries which
currently have the highest incidence of invasive pathology.
Introduction of such prevention programmes across all geographical
regions and maintenance of high adherence rates by women via
continuous psychoeducation would lead to CC becoming a worry of the
past.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AB, CA and CC were all involved in the
conceptualization of the current manuscript. AB and CC were
involved in the literature search and review of the resources that
were used in the current manuscript. AB, CA and CC were involved in
the writing and revision of the manuscript. All authors read and
approved the final manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Authors' information
Dr Constantina Constantinou: Orcid ID:
0000-0001-6167-4023.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Globocan 2020, . New Global Cancer Data.
Uicc.org. 2021.https://www.uicc.org/news/globocan-2020-new-global-cancer-dataSeptember
18–2021
|
|
2
|
Al Jishi T and Sergi C: Current
perspective of diethylstilbestrol (DES) exposure in mothers and
offspring. Reprod Toxicol. 71:71–77. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Adcock R, Cuzick J, Hunt WC, McDonald RM
and Wheeler CM; New Mexico HPV Pap Registry Steering Committee, :
Role of HPV genotype, multiple infections, and viral load on the
risk of high-grade cervical Neoplasia. Cancer Epidemiol Biomarkers
Prev. 28:1816–1824. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Doorbar J, Egawa N, Griffin H, Kranjec C
and Murakami I: Human papillomavirus molecular biology and disease
association. Rev Med Virol. 25 (Suppl):S2–S23. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Galloway D and Laimins L: Human
papillomaviruses: Shared and distinct pathways for pathogenesis.
Cur Opin Virol. 14:87–92. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Plummer M, de Martel C, Vignat J, Ferlay
J, Bray F and Franceschi S: Global burden of cancers attributable
to infections in 2012: A synthetic analysis. Lancet Glob Health.
4:e609–e616. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wagner M, Bennetts L, Patel H, Welner S,
de Sanjose S and Weiss T: Global availability of data on HPV
genotype-distribution in cervical, vulvar and vaginal disease and
genotype-specific prevalence and incidence of HPV infection in
females. Infect Agent Cancer. 10:132015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yuan Y, Cai X, Shen F and Ma F: HPV
post-infection microenvironment and cervical cancer. Cancer Lett.
497:243–254. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cohen O, Schejter E, Agizim R, Schonman R,
Chodick G, Fishman A and Hershko Klement A: Postcoital bleeding is
a predictor for cervical dysplasia. PLoS One. 14:e02173962019.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reed N, Balega J, Barwick T, Buckley L,
Burton K, Eminowicz G, Forrest J, Ganesan R, Harrand R, Holland C,
et al: British Gynaecological Cancer Society (BGCS) cervical cancer
guidelines: Recommendations for practice. Eur J Obstet Gynecol
Reprod Biol. 256:433–465. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Issa Z, Aloan H and Al Niyazee A: Accuracy
of Pap smear in cervical cancer screening. World Family Med J.
17:16–20. 2019. View Article : Google Scholar
|
|
12
|
Johnson CA, James D, Marzan A and Armaos
M: Cervical cancer: An overview of pathophysiology and management.
Semin Oncol Nurs. 35:166–174. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pkhakadze G, Bokhua Z, Asatiani T,
Muzashvili T and Burkadze G: Evaluation of the risk of cervical
intraepithelial neoplasia progression based on cell proliferation
index, epithelial-mesenchymal transition and co-infections.
Georgian Med News. 178–184. 2020.PubMed/NCBI
|
|
14
|
Bhatla N, Aoki D, Sharma DN and
Sankaranarayanan R: Cancer of the cervix Uteri. Int J Gynaecol
Obstet. 143:22–36. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li X, Xia L, Chen X, Fu Y and Wu X: Simple
conization and pelvic lymphadenectomy in early-stage cervical
cancer: A retrospective analysis and review of the literature.
Gynecol Oncol. 158:231–235. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Landoni F, Maneo A, Zapardiel I, Zanagnolo
V and Mangioni C: Class I versus class III radical hysterectomy in
stage IB1-IIA cervical cancer. A prospective randomized study. Eur
J Surg Oncol. 38:203–209. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gopalani SV, Janitz AE and Campbell JE:
Cervical cancer incidence and mortality among Non-Hispanic African
American and white women, United States, 1999–2015. J Natl Med
Assoc. 112:632–638. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lott BE, Trejo MJ, Baum C, McClelland DJ,
Adsul P, Madhivanan P, Carvajal S, Ernst K and Ehiri J:
Interventions to increase uptake of cervical screening in
Sub-Saharan Africa: A scoping review using the Integrated
Behavioral Model. BMC Public Health. 20:6542020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
International agency for research on
cancer, . Cervix uteri fact sheet. 2020.https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdfOctober
28–2021
|
|
20
|
Aylward J Global burden of cervical
cancer, . In TogetHER for Health. 2021.https://togetherforhealth.org/global-burden-cervical-cancer/November
28–2021
|
|
21
|
Keenan M: Human Development Index (HDI).
Salem Press Encyclopedia. 2021.https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=ers&AN=98402115&site=eds-liveSeptember
28–2021
|
|
22
|
Arbyn M, Weiderpass E, Bruni L, de Sanjosé
S, Saraiya M, Ferlay J and Bray F: Estimates of incidence and
mortality of cervical cancer in 2018: A worldwide analysis. Lancet
Glob Health. 8:e191–e203. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Burton-Jeangros C, Cullati S, Manor O,
Courvoisier DS, Bouchardy C and Guessous I: Cervical cancer
screening in Switzerland: Cross-sectional trends (1992–2012) in
Social Inequalities. Eur J Public Health. 27:167–173.
2017.PubMed/NCBI
|
|
24
|
Lam JO, Lim WY, Chow KY and D'Souza G:
Incidence, trends and ethnic differences of oropharyngeal, anal and
cervical cancers: Singapore, 1968–2012. PLoS One. 10:e01461852015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Garau M, Musetti C, Alonso R and Barrios
E: Trends in cancer incidence in Uruguay: 2002–2015. Colomb Med
(Cali). 50:224–238. 2019.PubMed/NCBI
|
|
26
|
Gopalani S, Janitz A and Campbell J:
Cervical Cancer Incidence and Mortality among Non-Hispanic African
American and White Women, United States, 1999–2015. J Natl Med
Assoc. 112:632–638. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lott B, Trejo M, Baum C, McClelland D,
Adsul P, Madhivanan P, Carvajal S, Ernst K and Ehiri J:
Interventions to increase uptake of cervical screening in
sub-Saharan Africa: A scoping review using the integrated
behavioral model. BMC Public Health. 20:6542020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lekoane K, Kuupiel D, Mashamba-Thompson T
and Ginindza T: Evidence on the prevalence, incidence, mortality
and trends of human papilloma virus-associated cancers in
Sub-Saharan Africa: Systematic scoping review. BMC Cancer.
19:5632019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kisling LA: Prevention strategies.
StatPearls. 2021.https://www.ncbi.nlm.nih.gov/books/NBK537222/September
15–2021
|
|
30
|
Von Karsa L, Arbyn M, De Vuyst H, Dillner
J, Dillner L, Franceschi S, Patnick J, Ronco G, Segnan N, Suonio E,
et al: European guidelines for quality assurance in cervical cancer
screening. Summary of the supplements on HPV screening and
vaccination. Papillomavirus Res. 1:22–31. 2015. View Article : Google Scholar
|
|
31
|
Banday A, Jeelani S and Hruby V: Cancer
vaccine adjuvants-recent clinical progress and future perspectives.
Immunopharmacol Immunotoxicol. 37:1–11. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bogani G, Leone Roberti Maggiore U,
Signorelli M, Martinelli F, Ditto A, Sabatucci I, Mosca L, Lorusso
D and Raspagliesi F: The role of human papillomavirus vaccines in
cervical cancer: Prevention and treatment. Crit Rev Oncol Hematol.
122:92–97. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bosch F, Robles C, Díaz M, Arbyn M,
Baussano I, Clavel C, Ronco G, Dillner J, Lehtinen M, Petry K, et
al: HPV-FASTER: Broadening the scope for prevention of HPV-related
cancer. Nat Rev Clin Oncol. 13:119–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Cuzick J and Wheeler C: Need for expanded
HPV genotyping for cervical screening. Papillomavirus Res.
2:112–115. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bruni L, Saura-Lázaro A, Montoliu A,
Brotons M, Alemany L, Diallo MS, Afsar OZ, Lamontagne DS, Mosina L,
Contreras M, et al: HPV vaccination introduction worldwide and WHO
and UNICEF estimates of national HPV immunization coverage
2010–2019. Prev Med. 144:1063992021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Siu J, Fung T and Leung L: Social and
cultural construction processes involved in HPV vaccine hesitancy
among Chinese women: A qualitative study. Int J Equity Health.
18:1472019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Termrungruanglert W, Khemapech N,
Vasuratna A, Havanond P, Deebukkham P, Kulkarni A and Pavelyev A:
The epidemiologic and economic impact of a quadrivalent human
papillomavirus vaccine in Thailand. PLoS One. 16:e02458942021.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Daley E, Vamos C, Zimet G, Rosberger Z,
Thompson E and Merrell L: The Feminization of HPV: Reversing gender
biases in US Human papillomavirus vaccine policy. Am J Public
Health. 106:983–984. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Daley E, Vamos C, Thompson E, Zimet G,
Rosberger Z, Merrell L and Kline N: The feminization of HPV: How
science, politics, economics and gender norms shaped U.S. HPV
vaccine implementation. Papillomavirus Res. 3:142–148. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Patel C, Brotherton J, Pillsbury A,
Jayasinghe S, Donovan B, Macartney K and Marshall H: The impact of
10 years of human papillomavirus (HPV) vaccination in Australia:
What additional disease burden will a nonavalent vaccine prevent?
Euro Surveill. 23:17007372018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chidyaonga-Maseko F, Chirwa M and Muula A:
Underutilization of cervical cancer prevention services in low and
middle income countries: A review of contributing factors. Pan Afr
Med J. 21:2312015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Jaiswal J, LoSchiavo C, Maiolatesi A,
Kapadia F and Halkitis P: Misinformation, Gendered perceptions, and
low healthcare provider communication around HPV and the HPV
vaccine among young sexual minority Men in New York City: The P18
cohort study. J Community Health. 45:702–711. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Morris M, Friedemann Smith C, Boxell E,
Wardle J, Simon A and Waller J: Quantitative evaluation of an
information leaflet to increase prompt help-seeking for
gynaecological cancer symptoms. BMC Public Health. 16:3742016.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Okan Y, Petrova D, Smith S, Lesic V and
Bruine de Bruin W: How do Women interpret the NHS information
leaflet about cervical cancer screening? Med Decis Making.
39:738–754. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kolthoff S, Hestbech M, Jørgensen K and
Brodersen J: Do invitations for cervical screening provide
sufficient information to enable informed choice? A cross-sectional
study of invitations for publicly funded cervical screening. J R
Soc Med. 109:274–281. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ngu S, Wei N, Kwan T, Chu M, Tse K, Chan K
and Ngan H: Impact of different educational interventions on
psychosocial well-being of women with a positive high-risk human
papillomavirus and normal cervical cytology: A randomised trial. J
Psychosom Obstet Gynaecol. 39:146–155. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Calderón-Mora J, Byrd TL, Alomari A,
Salaiz R, Dwivedi A, Mallawaarachchi I and Shokar N: Group versus
individual culturally tailored and theory-based education to
promote cervical cancer screening among the underserved Hispanics:
A cluster randomized trial. Am J Health Promot. 34:15–24. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Clavé Llavall A, de Wildt G, Meza G,
Tattsbridge J and Jones L: Nurses' and teachers' perceived barriers
and facilitators to the uptake of the human papilloma virus (HPV)
vaccination program in Iquitos, Peru: A qualitative study. PLoS
One. 16:e02552182021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Catarino R, Petignat P, Dongui G and
Vassilakos P: Cervical cancer screening in developing countries at
a crossroad: Emerging technologies and policy choices. World J Clin
Oncol. 6:281–290. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Tranberg M, Bech B, Blaakær J, Jensen J,
Svanholm H and Andersen B: Preventing cervical cancer using HPV
self-sampling: Direct mailing of test-kits increases screening
participation more than timely opt-in procedures-a randomized
controlled trial. BMC Cancer. 18:2732018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Maver P and Poljak M: Primary HPV-based
cervical cancer screening in Europe: Implementation status,
challenges, and future plans. Clin Microbiol Infect. 26:579–583.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Woronoff A, Molinié F and Trétarre B:
Implementation of national cervical cancer screening program in
France. Bull Cancer. 106:253–261. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
De Prez V, Jolidon V, Willems B, Cullati
S, Burton-Jeangros C and Bracke P: Cervical cancer (over)screening
in Belgium and Switzerland: Trends and social inequalities. Eur J
Public Health. 30:410–415. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Watson M, Benard V and Flagg E: Assessment
of trends in cervical cancer screening rates using healthcare
claims data: United States, 2003–2014. Prev Med Rep. 9:124–130.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Landy R, Sasieni PD, Mathews C, Wiggins
CL, Robertson M, McDonald YJ, Goldberg DW, Scarinci IC, Cuzick J
and Wheeler CM; New Mexico HPV Pap Registry Steering Committee, :
Impact of screening on cervical cancer incidence: A
population-based case-control study in the United States. Int J
Cancer. 147:887–896. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Landy R, Mathews C, Robertson M, Wiggins
CL, Mcdonald YJ, Goldberg DW, Scarinci IC, Cuzick J, Sasieni PD and
Wheeler CM: A state-wide population-based evaluation of cervical
cancers arising during opportunistic screening in the United
States. Gynecol Oncol. 159:344–353. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sankaranarayanan R, Nene B, Shastri S,
Jayant K, Muwonge R, Budukh AM, Hingmire S, Malvi SG, Thorat R,
Kothari A, et al: HPV screening for cervical cancer in rural India.
N Engl J Med. 360:1385–1394. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Dorji T, Tshomo U, Gyamtsho S, Tamang S,
Wangmo S and Pongpirul K: Gender-neutral HPV elimination, cervical
cancer screening, and treatment: Experience from Bhutan. Int J
Gynaecol Obstet. Apr 30–2021.(Epubs ahead of print). doi:
10.1002/ijgo.13728. PubMed/NCBI
|
|
59
|
Kim JJ, Campos NG, Sy S, Burger EA, Cuzick
J, Castle PE, Hunt WC, Waxman A and Wheeler CM; New Mexico HPV Pap
Registry Steering Committee, : Inefficiencies and High-value
improvements in U.S. Cervical cancer screening practice. Ann
Internal Med. 163:589–597. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Singh U, Anjum, Qureshi S, Negi N, Singh
N, Goel M and Srivastava K: Comparative study between liquid-based
cytology & conventional Pap smear for cytological follow up of
treated patients of cancer cervix. Indian J Med Res. 147:263–267.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Karimi-Zarchi M, Peighmbari F, Karimi N,
Rohi M and Chiti Z: A Comparison of 3 ways of conventional pap
smear, liquid-based cytology and colposcopy vs cervical biopsy for
early diagnosis of premalignant lesions or cervical cancer in women
with abnormal conventional pap test. Int J Biomed Sci. 4:205–210.
2013.PubMed/NCBI
|
|
62
|
Ramírez-Palacios P, Chen A, Flores YN,
Crespi CM, Lazcano-Ponce E, Alvarez-Escobedo D, Torres-Ibarra L,
Rivera-Paredez B, León-Maldonado L, Hernández-López R, et al:
Benefit of double-reading cytology smears as a triage strategy
among high-risk human papillomavirus-positive women in Mexico.
Cancer Cytopathol. 128:715–724. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Lee H, Kang Y and Ju W: Cervical cancer
screening in developing countries: Using visual inspection methods.
Clin J Oncol Nurs. 20:79–83. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Orang'o E, Wachira J, Asirwa F, Busakhala
N, Naanyu V, Kisuya J, Otieno G, Keter A, Mwangi A and Inui T:
Factors associated with uptake of visual inspection with acetic
Acid (VIA) for cervical cancer screening in western Kenya. PLoS
One. 11:e01572172016. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Kudva V, Prasad K and Guruvare S: Andriod
device-based cervical cancer screening for resource-poor settings.
J Digital Imaging. 31:646–654. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Koliopoulos G, Nyaga V, Santesso N, Bryant
A, Martin-Hirsch P, Mustafa R, Schünemann H, Paraskevaidis E and
Arbyn M: Cytology versus HPV testing for cervical cancer screening
in the general population. Cochrane Database Syst Rev.
8:CD0085872017.PubMed/NCBI
|
|
67
|
Arbyn M, Simon M, Peeters E, Xu L, Meijer
CJLM, Berkhof J, Cuschieri K, Bonde J, Ostrbenk Vanlencak A, Zhao
F, et al: 2020 list of human papillomavirus assays suitable for
primary cervical cancer screening. Clin Microbiol Infect.
27:1083–1095. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Ronco G, Dillner J, Elfström KM, Tunesi S,
Snijders PJ, Arbyn M, Kitchener H, Segnan N, Gilham C, Giorgi-Rossi
P, et al: Efficacy of HPV-based screening for prevention of
invasive cervical cancer: Follow-up of four European randomised
controlled trials. Lancet. 383:524–532. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Castle PE, Pierz AJ, Adcock R, Aslam S,
Basu P, Belinson J, Cuzick J, El-Zein M, Ferreccio C, Firnhaber C,
et al: A pooled analysis to compare the clinical characteristics of
human papillomavirus-positive and -negative cervical precancers.
Cancer Prev Res. 13:829–840. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Reid JL, Wright TC, Stoler MH, Cuzick J,
Castle PE, Dockter J, Getman D and Giachetti C: Human
papillomavirus oncogenic mRNA testing for cervical cancer
screening. Am J Clin Pathol. 144:473–483. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Cuzick J, Cadman L, Ahmad AS, Ho L, Terry
G, Kleeman M, Lyons D, Austin J, Stoler MH, Vibat CRT, et al:
Performance and diagnostic accuracy of a urine-based human
papillomavirus assay in a referral population. Cancer Epidemiol
Biomarkers Prev. 26:1053–1059. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Torres-Ibarra L, Lazcano-Ponce E, Franco
EL, Cuzick J, Hernandez-Avila M, Lorincz A, Rivera B, Ramírez P,
Mendiola-Pastrana I, Rudolph S, et al: Triage strategies in
cervical cancer detection in Mexico: Methods of the FRIDA study.
Salud Publica Mex. 58:197–210. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Torres-Ibarra L, Cuzick J, Lorincz AT,
Spiegelman D, Lazcano-Ponce E, Franco E, Moscicki A, Mahmud S,
Wheeler C, Rivera-Paredez B, et al: Comparison of HPV-16 and HPV-18
genotyping and cytological testing as triage testing within human
papillomavirus-based screening in Mexico. JAMA Netw Open.
2:e19157812019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Cuzick J, Du R, Adcock R, Kinney W, Joste
N, McDonald R, English K, Torres S, Saslow D and Wheeler C; New
Mexico HPV Pap Registry Steering Committee, : Uptake of co-testing
with HPV and cytology for cervical screening: A population-based
evaluation in the United States. Gynecol Oncol. 162:555–559. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Kyrgiou M, Arbyn M, Bergeron C, Bosch F,
Dillner J, Jit M, Kim J, Poljak M, Nieminen P, Sasieni P, et al:
Cervical screening: ESGO-EFC position paper of the European Society
of Gynaecologic Oncology (ESGO) and the European Federation of
Colposcopy (EFC). Br J Cancer. 123:510–517. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Castle PE, Adcock R, Cuzick J, Wentzensen
N, Torrez-Martinez N, Torres S, Stoler M, Ronnett B, Joste N,
Darragh T, et al: Relationships of p16 immunohistochemistry and
other biomarkers with diagnoses of cervical abnormalities:
Implications for LAST terminology. Arch Pathol Lab Med.
144:725–734. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Macedo AC, Gonçalves JC, Bavaresco DV,
Grande AJ, Chiaramonte Silva N and Rosa MI: Accuracy of mRNA HPV
tests for triage of precursor lesions and cervical cancer: A
systematic review and meta-analysis. J Oncol. 2019:69350302019.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Shah UJ, Nasiruddin M, Dar SA, Khan MK,
Akhter MR, Singh N, Rabaan AA and Haque S: Emerging biomarkers and
clinical significance of HPV genotyping in prevention and
management of Cervical Cancer. Microb Pathog. 143:1041312020.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
van Leeuwen RW, Oštrbenk A, Poljak M, van
der Zee AG, Schuuring E and Wisman GB: DNA methylation markers as a
triage test for identification of cervical lesions in a high risk
human papillomavirus positive screening cohort. Int J Cancer.
144:746–754. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Tian Y, Yuan Wu NY, Liou YL, Yeh CT, Cao
L, Kang YN, Wang HJ, Li Y, Chu TY, Li W, et al: Utility of gene
methylation analysis, cytological examination, and HPV-16/18
genotyping in triage of high-risk human papilloma virus-positive
women. Oncotarget. 8:62274–62285. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Banila C, Lorincz AT, Scibior-Bentkowska
D, Clifford GM, Kumbi B, Beyene D, Wheeler CM, Cuschieri K, Cuzick
J and Nedjai B: Clinical performance of methylation as a biomarker
for cervical carcinoma in situ and cancer diagnosis: A worldwide
study. Int J Cancer. 150:290–302. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Cook DA, Krajden M, Brentnall AR, Krajden
M, Gondara L, Chan T, Law J, Smith L, Niekerk D, Ogilvie G, et al:
Evaluation of a validated methylation triage signature for human
papillomavirus positive women in the HPV FOCAL cervical cancer
screening trial. Int J Cancer. 144:2587–2595. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Louvanto K, Franco EL, Ramanakumar AV,
Vasiljević N, Scibior-Bentkowska D, Koushik A, Cuzick J, Coutlée F
and Lorincz AT; Biomarkers of Cervical Cancer Risk Study Team, :
Methylation of viral and host genes and severity of cervical
lesions associated with human papillomavirus type 16. Int J Cancer.
136:E638–E645. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Vale D, Teixeira J, Bragança J, Derchain
S, Sarian L and Zeferino L: Elimination of cervical cancer in low-
and middle-income countries: Inequality of access and fragile
healthcare systems. Int J Gynecol Obstet. 152:7–11. 2020.
View Article : Google Scholar
|
|
85
|
Ngwalle EW, Mgaya HN, Mpanju-Shumbusho W,
Chirenje ZM, Kirumbi L, Lebelle T and Kaggwa S: Situation analysis
for diagnosis and treatment of cervical cancer in mainland
Tanzania. East Afr Med J. 78:60–64. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Rosser JI, Hamisi S, Njoroge B and Huchko
MJ: Barriers to cervical cancer screening in rural Kenya:
Perspectives from a provider survey. J Community Health.
40:756–761. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
McDonald YJ, Goldberg DW, Scarinci IC,
Castle PE, Cuzick J, Robertson M and Wheeler CM: Health Service
Accessibility and risk in cervical cancer prevention: Comparing
rural versus nonrural residence in New Mexico. J Rural Health.
33:382–392. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Bingham A, Bishop A, Coffey P, Winkler J,
Bradley J, Dzuba I and Agurto I: Factors affecting utilization of
cervical cancer prevention services in low-resource settings. Salud
Publica Mex. 45 (Suppl 3):S408–S416. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Markovic M, Kesic V, Topic L and Matejic
B: Barriers to cervical cancer screening: A qualitative study with
women in Serbia. Soc Sci Med. 61:2528–2535. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Urasa M and Darj E: Knowledge of cervical
cancer and screening practices of nurses at a regional hospital in
Tanzania. Afr Health Sci. 11:48–57. 2011.PubMed/NCBI
|