Introduction
The most common subtypes of soft-tissue sarcomas are
liposarcoma, leiomyosarcoma, malignant fibrous histiocytoma and
fibrosarcoma (1,2). Liposarcoma is a rare malignancy that
originates from the adipose tissue and accounts for <1% of all
malignancies (3,4). It may occur anywhere in the adipose
tissue. The World Health Organization classifies it histologically
into well-differentiated, myxoid/round cell, pleomorphic and
dedifferentiated subtypes (5,6). The
incidence of liposarcoma has gradually increased and the disease is
more common in middle-aged and older individuals (7). Most liposarcomas grow slowly and the
huge space in the retroperitoneum and abdominal cavity provides
sufficient space for their growth. Giant liposarcomas eventually
surround large blood vessels and vital organs (8,9).
Retroperitoneal liposarcoma is usually asymptomatic until it is
large enough to compress the surrounding organs, and there is no
evidence that chemotherapy or radiotherapy improves survival
(10,11). The present study reports a case of
giant retroperitoneal liposarcoma. Giant liposarcoma is rare but is
occasionally reported in developing countries, where the tumor
grows irregularly, and there are no conventional surgical methods
and techniques to manage these large retroperitoneal malignancies.
The present study reported a case of a 6-kg giant retroperitoneal
liposarcoma measuring 32×30 cm.
Case report
The patient was a 51-year-old female with a body
mass index of 17.58 kg/m2. The patient observed a mass
in the upper left abdomen for 3 days, and visited Hexi University
Affiliated Zhangye People's Hospital (Zhangye, China) in March 2022
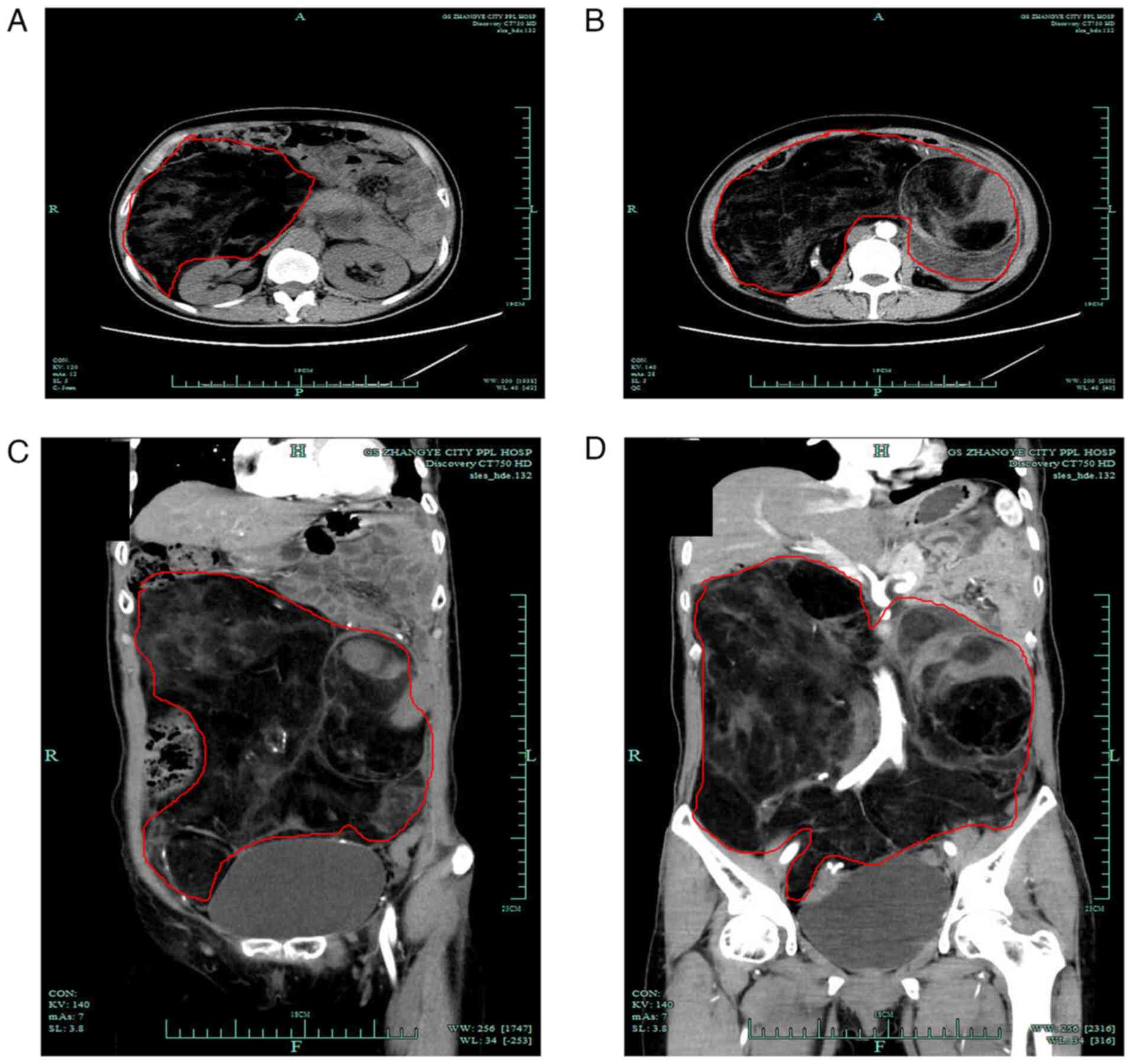
for treatment. Computed tomography (CT) revealed a giant
retroperitoneal liposarcoma measuring 32 cm in size (Fig. 1). After a multidisciplinary team
discussion, surgical treatment was decided and preoperative
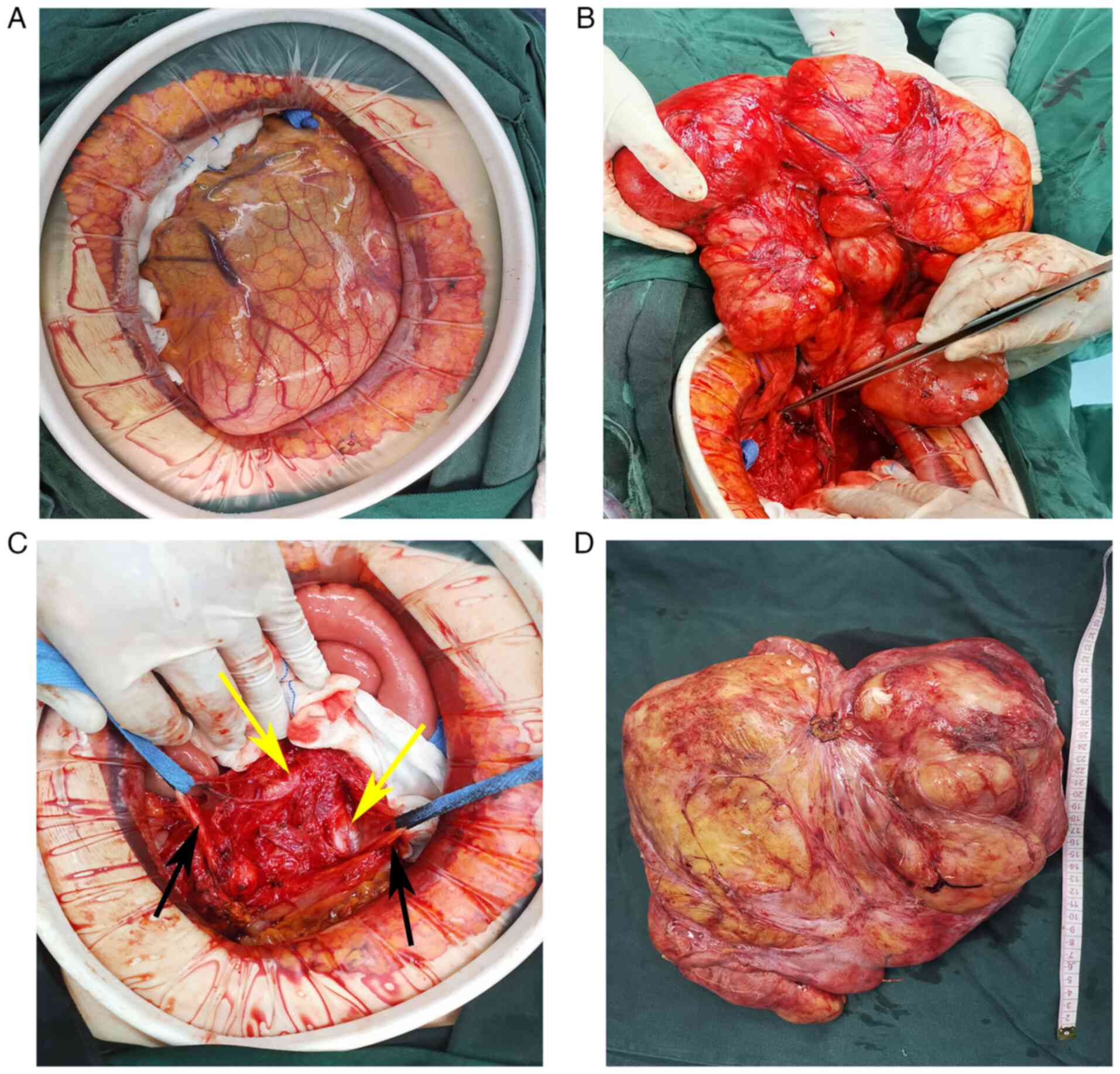
preparations were performed. Open surgery was performed under
general anesthesia. During the surgery, the tumor was found to be
located in the retroperitoneum, the small intestine had been pushed
to the upper left corner of the abdomen and the tumor extended from
the gastrocolic ligament to the deep pelvic cavity. The texture of
the tumor in the left upper corner was hard (the patient went to
the hospital after palpitating that mass) and the other parts of
the tumor were soft like fat. The left ureter that was pushed by
the tumor and had deviated to the right was repositioned during the
procedure (Fig. 2). The abdominal
cavity was closed after no other injury was found on exploration.
The patient returned to the ward without being sent to the
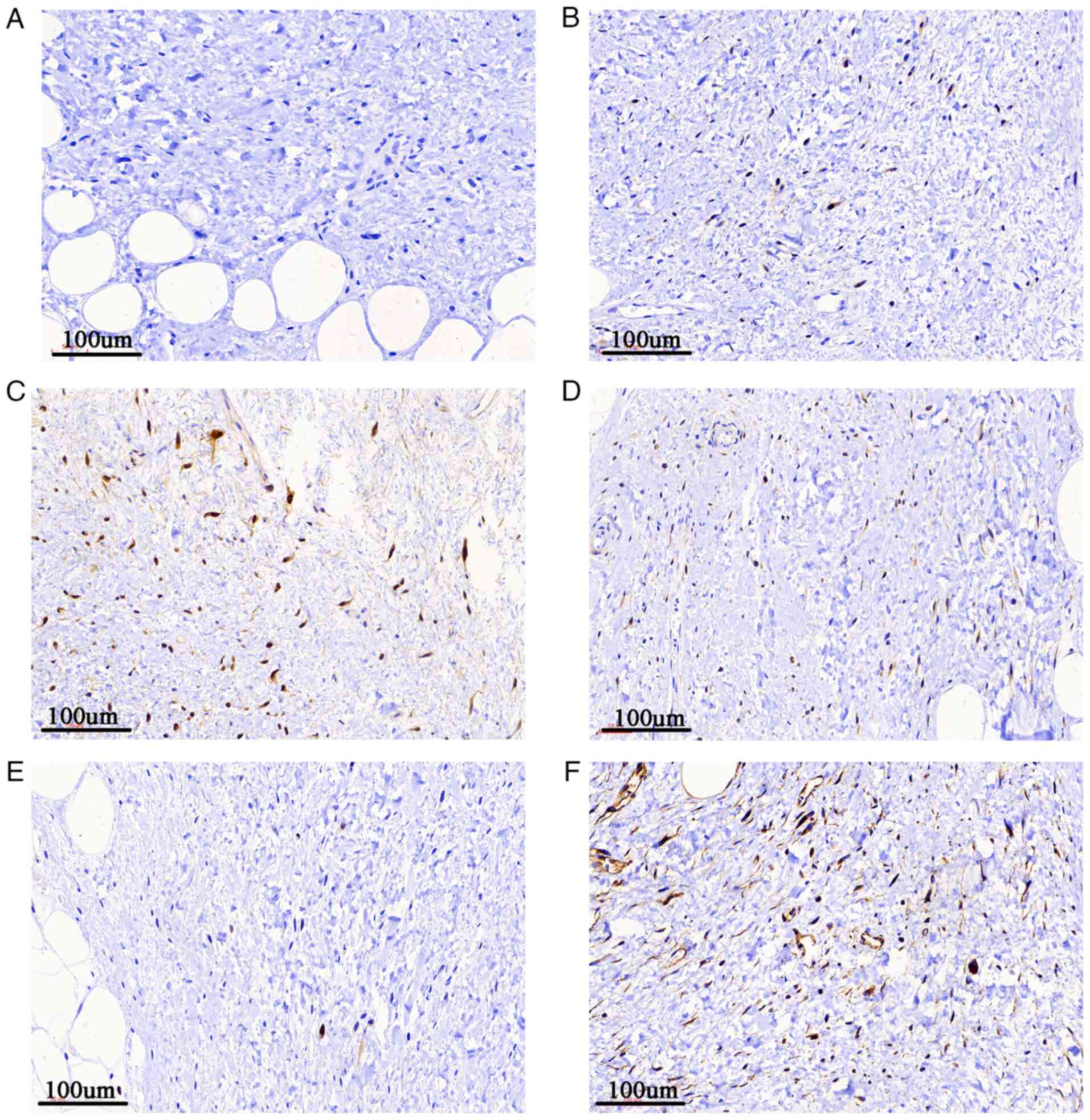
intensive care unit. Postoperative pathological examination
indicated retroperitoneal well-differentiated liposarcoma, while
immunohistochemistry, performed as previously described (12), revealed S-100(−) (cat. no.
Kit-0007), MDM-2(+) (cat. no. MAB-0074), vimentin(+) (cat. no.
MAB-0735), CDK4(+) (cat. no. RMA-0771), p16(+) (cat. no. MAB-0673)
and STAT6(+) (cat. no. RMA-0845) (all Fuzhou Maixin Biotech Co.,
Ltd.) results (Fig. 3). The
patient had occasional diarrhea in the early stage, and during the
follow-up, has been recovering well without any adverse events or
obvious discomfort. The patient and the patient's family were
satisfied with the recovery and the patient is still being followed
up.
Discussion
Retroperitoneal liposarcoma is a rare mesenchymal
tumor type that usually occurs in individuals aged 40–60 years
(12,13). Retroperitoneal liposarcoma may grow
very large prior to the onset of clinical symptoms, as the latent
space of the retroperitoneum and abdominal cavity is large and
loose. In case there are no bony borders, retroperitoneal
liposarcomas grow recklessly. However, retroperitoneal liposarcomas
with a diameter of >30 cm are rare. Most cases are discovered
incidentally due to tumor compression symptoms, such as abdominal
distension, indigestion and dyspnea. In the present case, the
patient experienced an abdominal mass 3 days prior to visiting the
hospital for treatment, indicating that the disease was insidious.
Patients generally have no obvious symptoms, particularly when the
tumor size is small. Due to its low morbidity and special
anatomical location, the tumor is bulky and deep, making resection
difficult. Complete surgical removal of the tumor may be highly
challenging, while the majority of surgeons lack experience in
handling such large tumors. Complete tumor resection during surgery
is key to treating this disease; otherwise, it easily relapses, and
surgery is the only cure after recurrence. Notably, performing
surgery bears great difficulty and a residual tumor increases the
risk of relapse. In the present case, the left ureter was
compressed and deviated to the far right. Therefore, during the
operation, the large blood vessels and tumor tissue were carefully
and accurately identified, particularly the iliac blood vessels and
intestinal blood vessels, and the ureter was protected because
giant tumors disorganize the normal anatomical relationship; the
relationship between the abdominal cavity and the retroperitoneum
complex, the incision margin is not easy to identify and the
surrounding blood vessels and ureters require to be protected.
CT is the most commonly used imaging test for
diagnosis and preoperative evaluation (14). There is no clear evidence in the
literature to support the need for histological biopsy of suspected
retroperitoneal tumors because, with or without biopsy, such large
tumors require surgical resection, which is the only curative
option. Liposarcoma is histologically subdivided into
well-differentiated, myxoid/round cell, pleomorphic and
dedifferentiated subtypes (15).
The 5-year survival rate of patients with well-differentiated
retroperitoneal liposarcoma is ~90%. The postoperative pathological
examination of the patient of the present study indicated
well-differentiated liposarcoma and the patient's prognosis was
expected to be favorable after complete resection, while
dedifferentiated, myxoid and pleomorphic liposarcoma have an annual
survival rate lower than that of well-differentiated liposarcoma
(15,16).
Studies have indicated that radiotherapy reduces the
risk of local recurrence; however, the supporting data are limited.
The STRASS study suggested that preoperative radiotherapy and
surgery did not prolong the recurrence-free survival of patients
compared with surgery alone but aggravated the adverse reactions in
patients. Therefore, preoperative radiotherapy should not be
considered a standard treatment for retroperitoneal sarcoma
(17). The role of chemotherapy in
retroperitoneal liposarcoma remains controversial, as no studies
have demonstrated a significant improvement in survival (18). The main factors affecting patients'
prognosis are tumor grade and degree of surgical resection. Radical
resection should be performed, and if necessary, the tumor should
be removed together with the surrounding organs, such as the
kidney, to ensure the completeness of tumor resection. Incomplete
piecemeal resection may lead to a significant reduction in patient
prognosis and should be avoided intraoperatively.
In conclusion, retroperitoneal liposarcoma is an
atypical, rare and aggressively growing tumor. CT may be reliably
used for diagnosis and complete resection is the gold standard
treatment. A tumor diameter of >30 cm should not be considered a
contraindication for surgical resection; however, treating this
disease with radiotherapy or chemotherapy remains controversial. In
the present study, surgical resection of a large tumor was
successful without postoperative complications and the patient was
satisfied with the treatment outcomes. However, the long-term
effects of the treatment require to be further evaluated.
Acknowledgements
Not applicable.
Funding
This study was funded by the Gansu Province Science and
Technology Planning Project (grant no. 20JR10RG310).
Availability of data and materials
The data sets used and/or analyzed during the
current study are available from the corresponding author on
reasonable request.
Authors' contributions
XYW and YJQ contributed substantially to the
conceptualization of the study. XYW performed the surgery, YJQ
obtained the medical images, and they both contributed to the
drafting of the manuscript and critical revisions for intellectual
content. SOY and JQ contributed substantially to the
conceptualization and design of the study. ST and JXY assisted in
the completion of the surgery, collected clinical information and
assisted with drafting the manuscript. XYW, YJQ, ST and JXY
approved the final version of the manuscript for publication. ST
and JXY confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Hexi University Affiliated Zhangye People's Hospital (Zhangye,
China). Written informed consent was obtained from the patient.
Patient consent for publication
Written informed consent was obtained for
publication of the patient's data and images in this case
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2021. CA Cancer J Clin. 71:7–33. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ray-Coquard I, Serre D, Reichardt P,
Martin-Broto J and Bauer S: Options for treating different soft
tissue sarcoma subtypes. Future Oncol. 14:25–49. 2018. View Article : Google Scholar
|
|
3
|
Thway K: Well-differentiated liposarcoma
and dedifferentiated liposarcoma: An updated review. Semin Diagn
Pathol. 36:112–121. 2019. View Article : Google Scholar
|
|
4
|
Mansfield SA, Pollock RE and Grignol VP:
Surgery for abdominal well-differentiated liposarcoma. Curr Treat
Options Oncol. 19:12018. View Article : Google Scholar
|
|
5
|
Kallen ME and Hornick JL: The 2020 WHO
classification: What's new in soft tissue tumor pathology? Am J
Surg Pathol. 45:e1–e23. 2021. View Article : Google Scholar
|
|
6
|
Improta L, Tzanis D, Bouhadiba T,
Abdelhafidh K and Bonvalot S: Overview of primary adult
retroperitoneal tumours. Eur J Surg Oncol. 46:1573–1579. 2020.
View Article : Google Scholar
|
|
7
|
Bock S, Hoffmann DG, Jiang Y, Chen H and
Il'yasova D: Increasing incidence of liposarcoma: A
population-based study of National surveillance databases,
2001–2016. Int J Environ Res Public Health. 17:27102020. View Article : Google Scholar
|
|
8
|
Herrera-Almario G, Cabrera LF,
Londono-Schimmer EE and Pedraza M: Giant retroperitoneal
liposarcoma surgical management. Ann R Coll Surg Engl. 104:e54–e56.
2022. View Article : Google Scholar
|
|
9
|
Qiao Z, Zhan R, Pang Y and Wu J: Giant
retroperitoneal dedifferentiated liposarcoma in an old man. Asian J
Surg. 44:1076–1078. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wu YX, Liu JY, Liu JJ, Yan P, Tang B, Cui
YH, Zhao YL, Shi Y, Hao YX, Yu PW and Qian F: A retrospective,
single-center cohort study on 65 patients with primary
retroperitoneal liposarcoma. Oncol Lett. 15:1799–1810. 2018.
|
|
11
|
Lee ATJ, Thway K, Huang PH and Jones RL:
Clinical and molecular spectrum of liposarcoma. J Clin Oncol.
36:151–159. 2018. View Article : Google Scholar
|
|
12
|
Yao JX, Chen X, Zhu YJ, Wang H, Hu XY and
Guo JM: Prognostic value of vimentin is associated with
immunosuppression in metastatic renal cell carcinoma. Front Oncol.
10:11812020. View Article : Google Scholar
|
|
13
|
Cheung KT, Mitchell C and Wong E:
Retroperitoneal liposarcoma in a nonagenarian. Autops Case Rep.
11:e20202242020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang Q, Juan YH, Li Y, Xie JJ, Liu H,
Huang H, Liu Z, Zheng J, Saboo US, Saboo SS and Liang C:
Multidetector computed tomography features in differentiating
exophytic renal angiomyolipoma from retroperitoneal liposarcoma: A
Strobe-compliant observational study. Medicine (Baltimore).
94:e15212015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mascarenhas MRM, Mutti LA, Paiva JMG,
Enokihara MMSES, Rosa IP and Enokihara MY: Giant atypical lipoma.
An Bras Dermatol. 92:546–549. 2017. View Article : Google Scholar
|
|
16
|
Haddox CL and Riedel RF: Recent advances
in the understanding and management of liposarcoma. Fac Rev.
10:12021. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bonvalot S, Gronchi A, Le Pechoux C,
Swallow CJ, Strauss D, Meeus P, van Coevorden F, Stoldt S, Stoeckle
E, Rutkowski P, et al: Preoperative radiotherapy plus surgery
versus surgery alone for patients with primary retroperitoneal
sarcoma (EORTC-62092: STRASS): A multicentre, open-label,
randomised, phase 3 trial. Lancet Oncol. 21:1366–1377. 2020.
View Article : Google Scholar
|
|
18
|
Crago AM and Dickson MA: Liposarcoma:
Multimodality management and future targeted therapies. Surg Oncol
Clin N Am. 25:761–773. 2016. View Article : Google Scholar : PubMed/NCBI
|