Introduction
As a common gynecological cancer, the incidence rate
of endometrial cancer (EC) has increased in recent years (1). It has been reported that 70% of EC
cases occur in perimenopausal or postmenopausal women, while 4% of
cases occur in women <40 years old (2). Moore and Brewer (3) hypothesized that the underlying causes
of EC are obesity and hyperinsulinemia. Considering all EC stages,
the overall 5-year survival rate for EC is ~80% (4). Currently, there are few effective
detection strategies and treatments for EC. Therefore, the present
study aimed to identify novel therapeutics for the prevention and
treatment of EC.
Autophagy, which is also known as macroautophagy, is
a controversial biological pathway in human cancer cells due its
dual role as a self-protective and apoptotic mechanism (5). Autophagy induces apoptosis in tumor
cells if the conditions in the cell mean that it is no longer
viable, and this situation cannot be reversed (6). The role of autophagy has been
investigated in EC, and the autophagy machinery may serve as a
potential therapeutic target (5).
Zhang et al (7) reported
that four autophagy-related genes (cyclin dependent kinase
inhibitor 2A, protein tyrosine kinase 6, erb-b2 receptor tyrosine
kinase 2 and baculoviral IAP repeat containing 5) may potentially
be independent predictive biomarkers and therapeutic targets for
EC. Based on the results of the aforementioned studies, the present
study investigated the underlying mechanism of autophagy in EC.
Lidocaine, one of the most commonly used local
anesthetics, decreases the viability and migration of breast cancer
cells (8). Chang et al
(9) reported that lidocaine
suppresses the viability of breast cancer cells via induction of
apoptosis. Furthermore, lidocaine exhibits an inhibitory effect on
the proliferation, epithelial-mesenchymal transition, migration and
invasion of A2780 and SKOV3 ovarian cancer cells (10). Lidocaine has been investigated in
numerous types of cancer; however, to the best of our knowledge,
its effect in EC remains unclear. Furthermore, a recent study has
reported the promotive effects of lidocaine on autophagy in
different cell types. For example, in astrocytes, autophagy is
activated by lidocaine treatment (11). However, the effects of lidocaine on
autophagy in EC have not yet been reported. Therefore, the aim of
the present study was to also determine the association of
lidocaine and autophagy in EC.
Materials and methods
Cell culture and treatment
Human endometrial stromal cells (THESCs) and the
human endometrial cancer cell line RL95-2 were provided by the
Procell Life Science & Technology Co., Ltd. Cells were cultured
in DMEM (Gibco; Thermo Fisher Scientific, Inc.) containing 10% FBS
(Gibco; Thermo Fisher Scientific, Inc.) and 1%
penicillin-streptomycin at 37°C in a humidified incubator with 5%
CO2. Subsequently, lidocaine (Beijing Solarbio Science
& Technology Co., Ltd.) at different doss (5, 10 and 15 mM) was
used to treat RL95-2 cells for 24, 48 and 72 h at 37°C. To further
explore the underlying mechanism of lidocaine, 1 mM 3-methyladenine
(3-MA) (Beijing Solarbio Science & Technology Co., Ltd.), an
autophagy inhibitor, was used to treat RL95-2 cells for 3 min at
room temperature after lidocaine pre-treatment.
Cell Counting Kit-8 (CCK-8) assay
RL95-2 cells (4×103 cells/well) were
inoculated into 96-well plates and incubated for 24 h at 37°C.
Subsequently, 10 µl CCK-8 reagent (Beyotime Institute of
Biotechnology) was added to each well, and the cells were incubated
for an additional 2 h. The absorbance was quantified at 450 nm
using a microplate reader (Thermo Fisher Scientific, Inc.).
Colony formation assay
RL95-2 cells (3×105 cells/well) were
seeded into 6-well plates and maintained for 14 days to form
colonies at 37°C. After fixation and staining with 4%
paraformaldehyde for 30 min at room temperature and 0.5% crystal
violet solution for 10 min at 37°C, respectively, the number of
colonies (>50 cells were considered a colony) was counted under
a Nikon Eclipse E600 microscope (Nikon Corporation; magnification,
×100).
Wound healing assay
RL95-2 cells (3×105 cells/well) were
inoculated into 6-well plates and incubated at 37°C until the cells
reached 80–90% confluency. The cells were then incubated overnight
at 37°C with serum-free DMEM. Subsequently, a pipette tip was used
to create a linear scratch in the cell monolayer. With the aim of
removing cell debris, the cells were washed with PBS three times.
Cells were then incubated at 37°C with 5% CO2, and were
assessed at 0 and 24 h. The area occupied by the migrated cells was
observed using a light microscope (magnification, ×100) and
quantified with Image J software (v1.52; National Institutes of
Health).
Transwell assay
A Transwell assay was used to assess RL95-2 cell
invasion. The upper chamber was pre-coated with Matrigel (Corning,
Inc.) for 30 min at 37°C. Subsequently, RL95-2 cells
(5×105 cells/well) in serum-free DMEM were plated into
the upper chamber with 8-µm pores at 37°C with 5% CO2,
while DMEM supplemented with 10% FBS was added to the lower
chamber. Following 24 h of incubation, the cells were fixed with 4%
paraformaldehyde for 15 min at 37°C and stained with 0.1% crystal
violet for 10 min at 37°C. Images were captured using a light
microscope (magnification, ×100) and quantified with Image J
software (v1.52; National Institutes of Health).
TUNEL assay
A TUNEL assay was used to assess the effects of
lidocaine on RL95-2 cell apoptosis. In brief, fixation and
permeabilization of cells were performed using 4% paraformaldehyde
at room temperature for 30 min and 0.25% Triton-X-100 at room
temperature for 5 min, respectively. Subsequently, the cells that
were rinsed with PBS were incubated with TUNEL reagent at 37°C for
1 h in the dark. Next, 5 µg/ml DAPI was used to stain cell nuclei
at 37°C in the dark for 5 min and then 10 visual fields were
randomly selected. The number of apoptotic cells was totaled using
a fluorescence microscope (magnification, ×100).
Western blotting
Total protein was extracted from RL95-2 cells using
RIPA lysis buffer (Beijing Solarbio Science & Technology Co.,
Ltd.). The protein concentration was quantified using a BCA kit
(Thermo Fisher Scientific, Inc.). Protein samples (30 µg/lane) were
separated using 10% SDS-PAGE. Subsequently, the separated proteins
were transferred onto a PVDF membrane. The membranes were blocked
with 5% skimmed milk at room temperature for 2 h, and then
incubated with the primary antibodies against Bcl-2 (dilution,
1:1,000; cat. no. ab32124), Bax (dilution, 1:1,000; cat. no.
ab32503), cleaved caspase-3 (dilution, 1:500; cat. no. ab32042),
caspase-3 (dilution, 1:2,000; cat. no. ab184787), cleaved caspase-9
(dilution, 1:1,000; cat. no. ab2324), caspase-9 (dilution, 1:2,000;
cat. no. ab202068), p62 (dilution, 1:10,000; cat. no. ab109012),
LC3 (dilution, 1:2,000; cat. no. ab192890) and GAPDH (dilution,
1:2,500; cat. no. ab9485) (all from Abcam) at 4°C overnight.
Subsequently, the membranes were incubated with HRP-conjugated goat
anti-rabbit secondary antibody (dilution, 1:2,000; cat. no.
ab205718; Abcam) for 2 h at room temperature. Protein bands were
visualized with an ECL kit (Thermo Fisher Scientific, Inc.) and
analyzed using ImageJ (v1.51; National Institutes of Health).
Immunofluorescence staining
RL95-2 cells were fixed with 4% paraformaldehyde for
15 min at 4°C and permeabilized with 0.1% Triton X-100 for 15 min
at room temperature, following which blocking was performed with
10% goat serum (Beijing Solarbio Science & Technology Co.,
Ltd.) for 30 min at room temperature. Subsequently, the cells were
incubated with primary antibody against Beclin 1 (dilution, 1:100;
cat. no. ab62557; Abcam) at 4°C overnight. On the next day, RL95-2
cells were incubated with FITC-conjugated goat anti-rabbit
secondary antibody (dilution, 1:1,000; cat. no. ab6755; Abcam) for
1 h at room temperature. Next, the cells were counterstained with 5
µg/ml DAPI for 5 min at 37°C, and the samples were imaged using a
fluorescence microscope (Nikon Corporation).
Statistical analysis
All data are presented as the mean ± SD and were
analyzed using GraphPad Prism 8.0 software (GraphPad Software,
Inc.). One-way ANOVA and Tukey's post hoc test were used for
statistical comparisons among different groups. Each experiment was
repeated ≥3 times. P<0.05 was considered to indicate a
statistically significant difference.
Results
Lidocaine inhibits the proliferation
and migration of EC cells
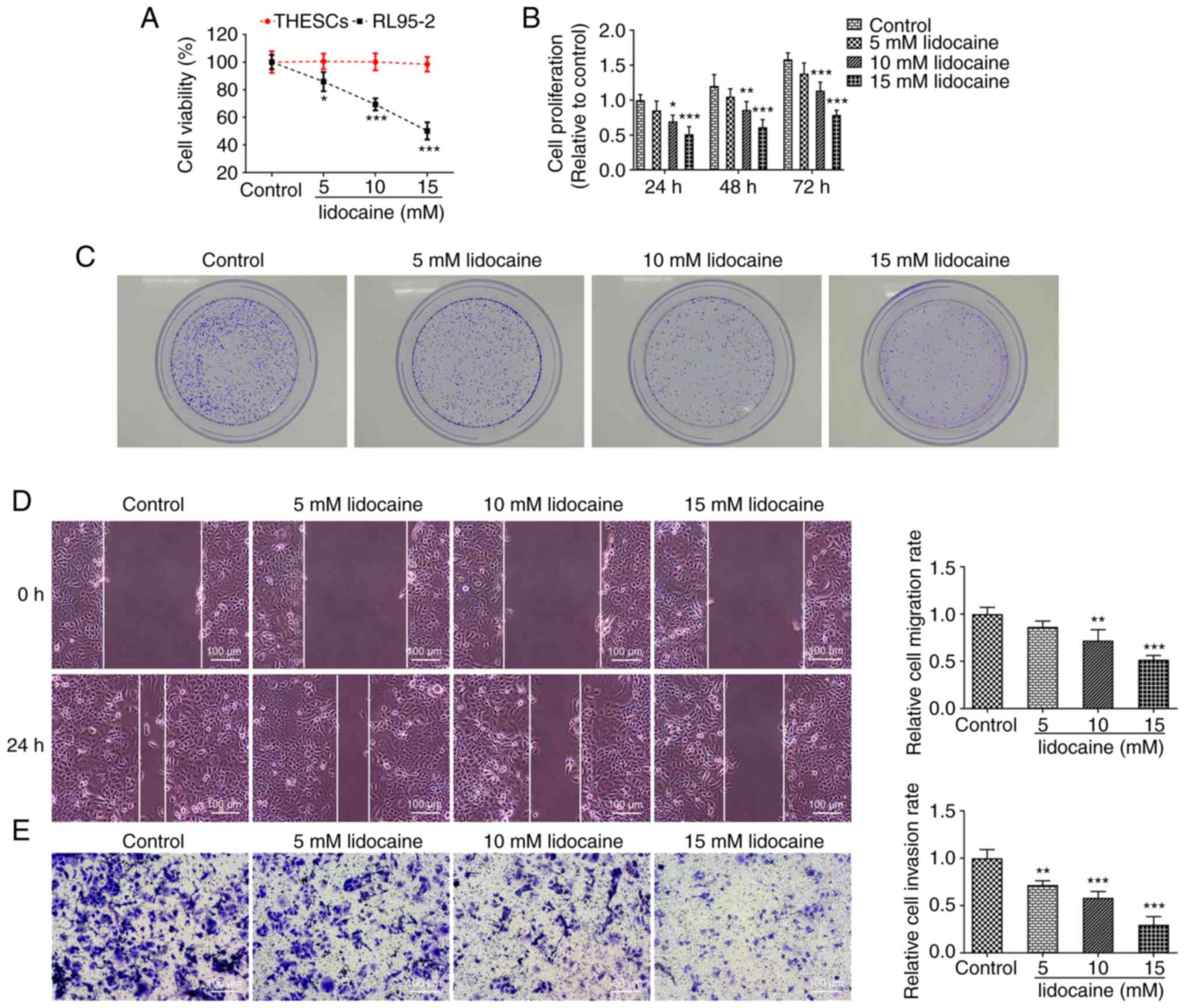
RL95-2 cell viability was first detected using a
CCK-8 assay. The results demonstrated that lidocaine markedly
reduced the viability of RL95-2 cells and exhibited an inhibitory
effect on cell viability in a dose-dependent manner. However, the
viability of THESCs remained similar following lidocaine
administration (Fig. 1A).
Furthermore, lidocaine suppressed the proliferation of RL95-2 cells
(Fig. 1B). When the lidocaine
concentration was 5 mM, there was no statistically significant
difference compared with the control at any of the three times
measured, although cell proliferation was inhibited. By contrast,
when the lidocaine concentration was 10 mM, the difference compared
with the control was statistically significant in a time-dependent
manner at 24 h (P<0.05), 48 h (P<0.01) or 72 h (P<0.001).
When the concentration of lidocaine was 15 mM, cell proliferation
was significantly inhibited at 24 h (P<0.001), 48 h (P<0.001)
and 72 h (P<0.001). The colony formation of RL95-2 cells was
also decreased by lidocaine treatment in a dose-dependent manner
(Fig. 1C).
To determine the effects of lidocaine on the
migration and invasion of RL95-2 cells, wound healing and Transwell
assays were performed. The results demonstrated that the migration
and invasion of RL95-2 cells were inhibited following lidocaine
treatment. Lidocaine at a concentration of 15 mM exhibited greater
inhibitory effects (P<0.001) on the migration and invasion of
RL95-2 cells compared with 5 or 10 mM (Fig. 1D and E).
Lidocaine promotes the apoptosis of EC
cells
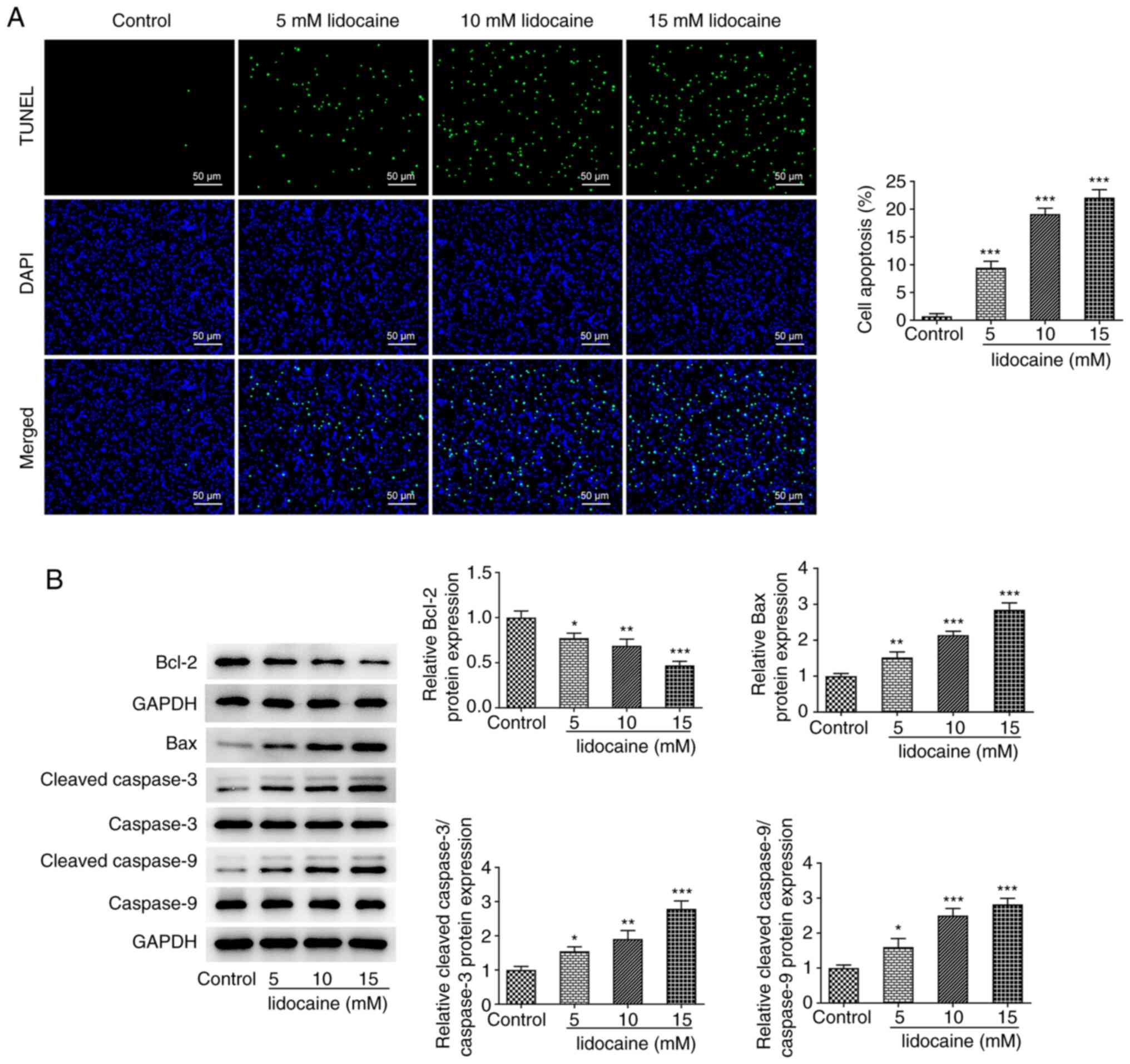
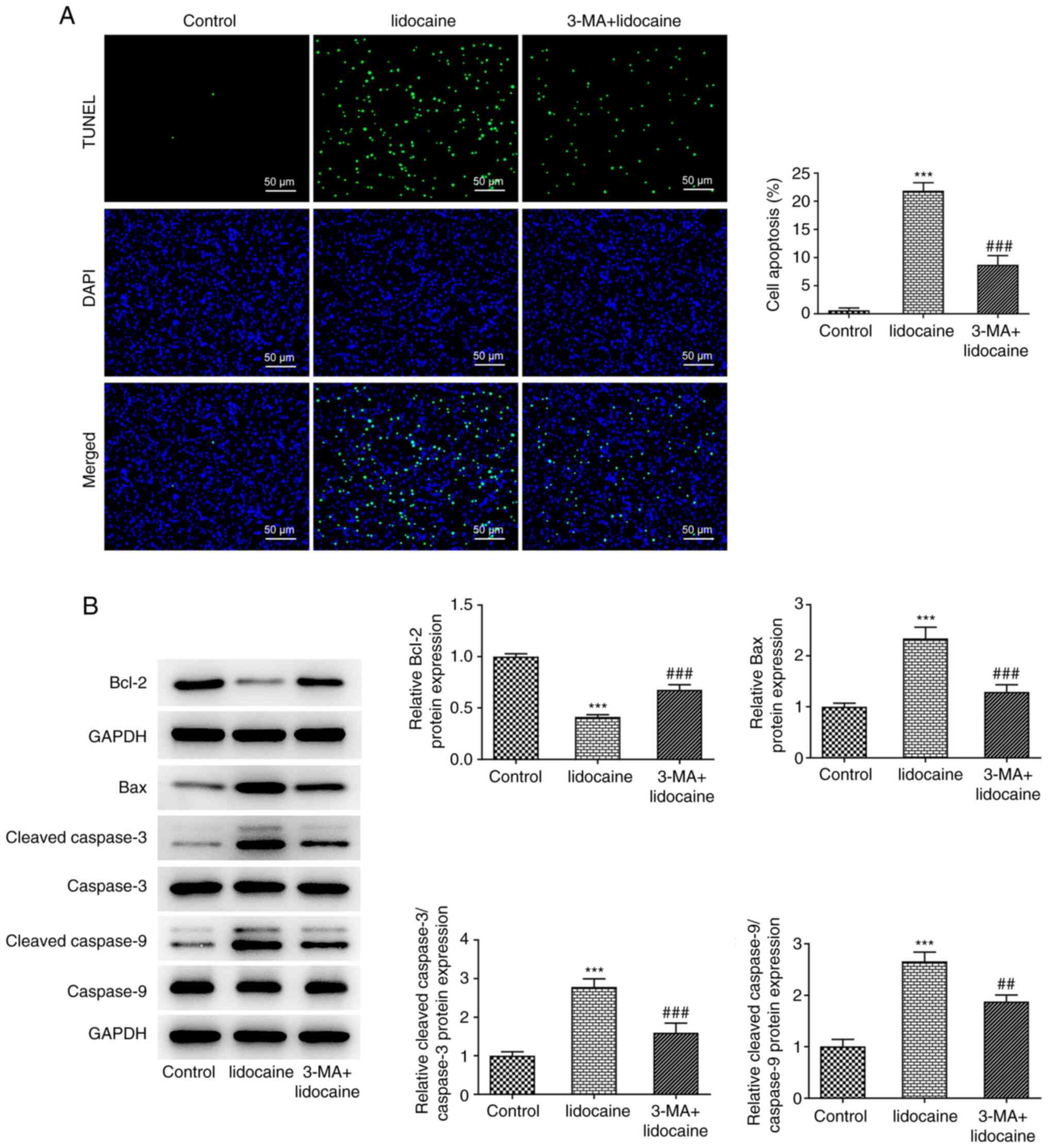
A TUNEL assay was performed to determine the effects
of lidocaine on the apoptosis of RL95-2 cells. The results
demonstrated that lidocaine treatment promoted the apoptosis of
RL95-2 cells in a dose-dependent manner (Fig. 2A). Furthermore, lidocaine treatment
downregulated Bcl-2 protein expression but upregulated the protein
levels of Bax, cleaved caspase-3 and cleaved caspase-9 (Fig. 2B). These results suggested that
lidocaine may promote the apoptosis of EC cells.
Lidocaine induces autophagy in EC
cells
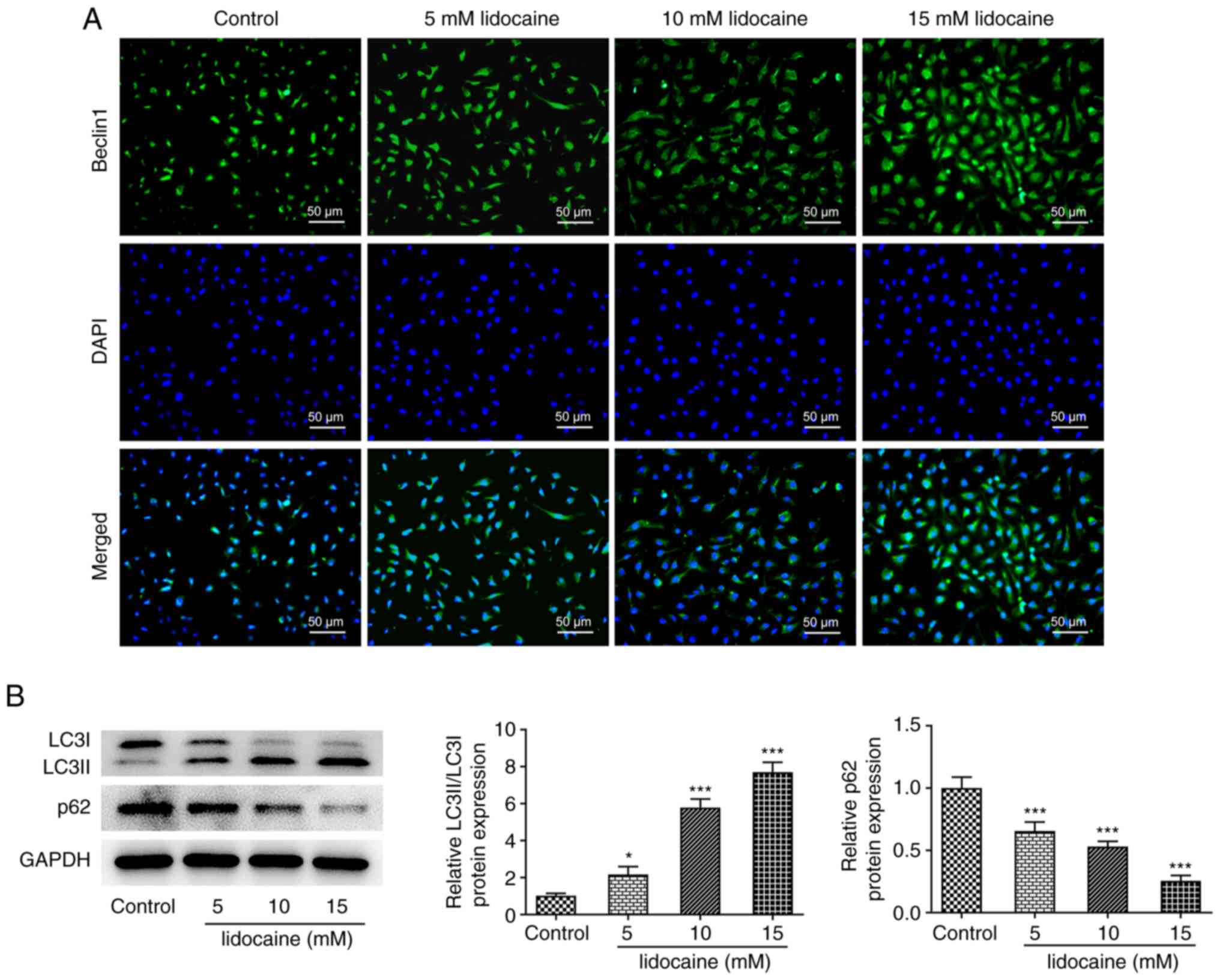
The protein expression levels of Beclin 1 were
markedly enhanced by lidocaine treatment in a dose-dependent manner
(Fig. 3A). Lidocaine also
regulated the protein expression levels of autophagy-related
proteins, as demonstrated by the upregulated protein expression
levels of LC3II/LC3I and downregulated p62 protein expression
compared with those of the control group (Fig. 3B). These results indicated that
lidocaine treatment may induce autophagy in EC cells.
Lidocaine inhibits the proliferation,
invasion and migration of EC cells by inducing autophagy
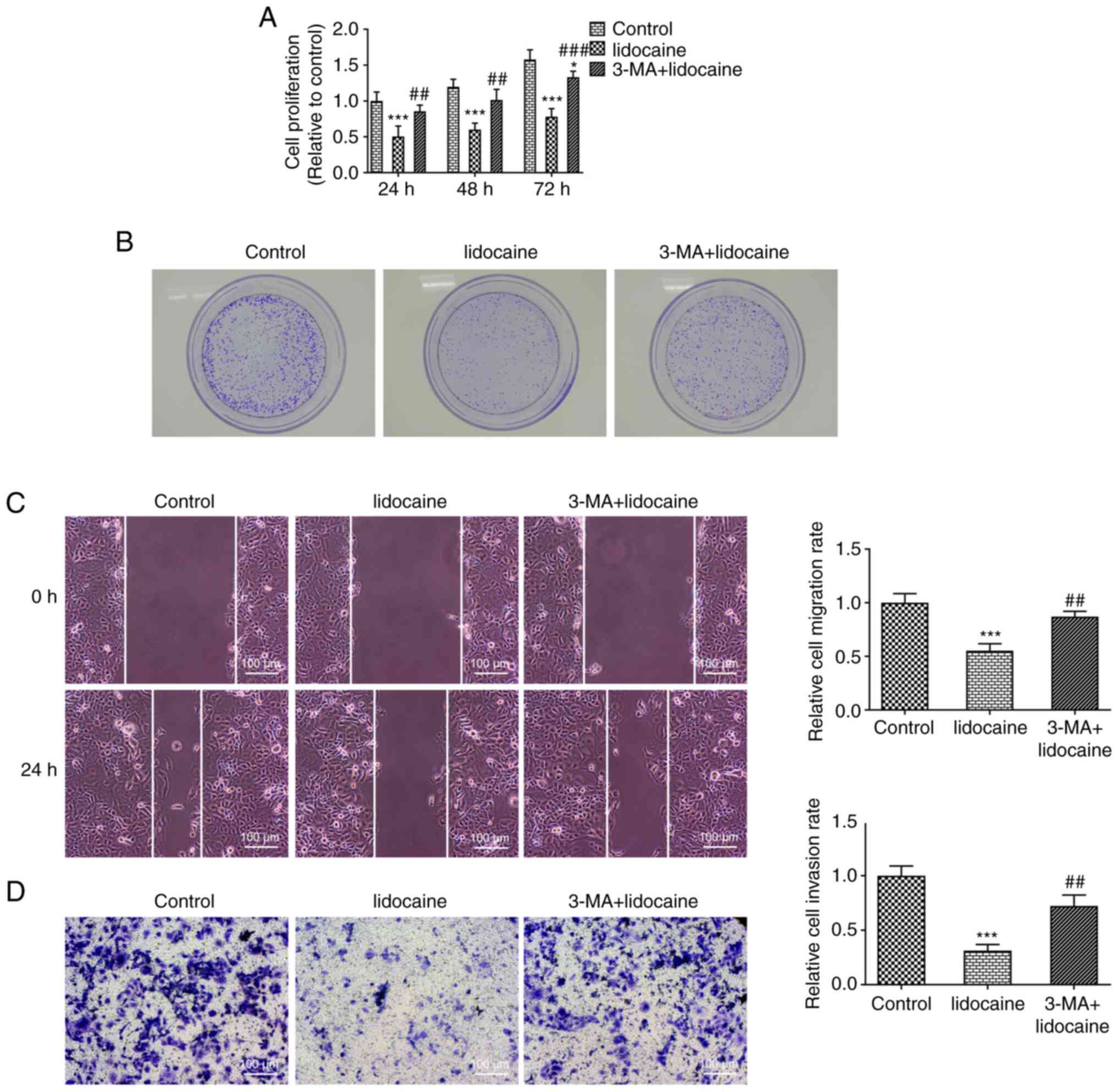
To investigate the mechanism of the effect of
lidocaine treatment on the proliferation, invasion and migration of
EC cells, 3-MA, an autophagy inhibitor, was used to treat RL95-2
cells. Compared with that of cells in the control group, the
proliferation of RL95-2 cells was significantly decreased following
lidocaine treatment, whereas 3-MA partially reversed the inhibitory
effects of lidocaine, as evidenced by the increased cell
proliferation of the 3-MA + lidocaine group (Fig. 4A). The decreased colony formation
observed in the lidocaine-treated group was also increased
following treatment with 3-MA (Fig.
4B). Furthermore, lidocaine reduced the migration and invasion
of RL95-2 cells compared with those of the control. This effect was
reversed following 3-MA treatment (Fig. 4C and D).
Lidocaine promotes EC cell apoptosis
by inducing autophagy
The increase in cell apoptosis following lidocaine
treatment was decreased by 3-MA treatment, which indicated that
3-MA inhibited apoptosis in lidocaine-treated RL95-2 cells
(Fig. 5A). Furthermore, lidocaine
downregulated Bcl-2 protein expression but upregulated the protein
levels of Bax, cleaved caspase-3 and cleaved caspase-9. These
effects were reversed when the cells were treated with 3-MA
(Fig. 5B). Overall, the present
results suggested that lidocaine may promote the apoptosis of EC
cells by inducing autophagy.
Discussion
As one of the most prevalent neoplasms in developed
countries, EC poses a serious threat to human health (12). To investigate the mechanism of EC,
EC cells were treated with lidocaine in the present study. CCK-8,
colony formation, wound healing and Transwell assays were performed
to detect the proliferation, colony formation, migration and
invasion of EC cells. In addition, 3-MA, an inhibitor of autophagy,
was used to treat EC cells to explore the effects of lidocaine on
autophagy. Overall, the current results demonstrated that lidocaine
exerted desirable anticancer effects on the proliferation,
migration, invasion and apoptosis of EC cells via the induction of
autophagy.
Lidocaine, a local anesthetic that is the first
choice of treatment for ventricular tachycardia and tremors, exerts
its efficacy within 1–3 min after administration, and its effects
last for 1–3 h (13,14). Clinically, lidocaine was initially
shown to have remarkable analgesic effects in laparoscopic and open
surgery, but it is now applied in different clinical settings,
including the perioperative period for spinal, breast, nose and
throat surgery (15–17).
Lidocaine has been widely investigated in numerous
cancer types. For example, lidocaine was demonstrated to exert an
antitumor effect in human gastric cancer, as evidenced by inhibited
cell proliferation, migration and invasion (18). Yang et al (19) reported that lidocaine may be a
novel therapy for the treatment of bladder cancer. Furthermore, it
has been demonstrated that lidocaine inhibits the malignant
development of cervical cancer by suppressing cell proliferation
and inducing apoptosis (20). In
the present study, the effects of lidocaine on RL95-2 cell
proliferation, migration, invasion and apoptosis were explored. It
was demonstrated that lidocaine markedly suppressed the viability,
proliferation and colony formation of RL95-2 cells in a
dose-dependent manner. Furthermore, lidocaine exhibited suppressive
effects on the migration and invasion of RL95-2 cells.
Autophagy, a conserved self-degradation system that
is critical for maintaining cellular homeostasis during stress
conditions, is associated with the progression of numerous diseases
(21). Autophagy serves an
important role in cell survival and maintenance by degrading
organelles, proteins and macromolecules, and by recycling
degradation products (22). In
addition, it serves a dichotomous role in cancer by suppressing the
growth of benign tumors but supporting the growth of advanced
cancer (23,24). Autophagy has been identified as a
potential therapeutic target for cancer (23,25).
Izdebska et al (26)
reported that lidocaine induced protective autophagy in the rat C6
glioma cell line. To understand the effects of lidocaine on
autophagy in EC cells, 3-MA was used to treat EC cells in the
present study. The results revealed that the protein expression
levels of Beclin 1 were markedly increased in lidocaine-treated
RL95-2 cells compared with in the control cells. Furthermore,
lidocaine treatment upregulated the protein expression levels of
LC3II/LC3I, but downregulated p62 protein expression compared with
those of the control cells. Therefore, these results suggested that
lidocaine may induce autophagy. The effects of lidocaine on the
proliferation and apoptosis in EC cells were reversed by 3-MA
treatment, which indicated that lidocaine may inhibit cell
proliferation and promote apoptosis in EC via autophagy
induction.
Apoptosis, a type of programmed cell death, serves
an indispensable role in a number of physiological and pathological
processes (27). Apoptosis
induction has been considered a target for cancer treatment
(28–30). Previous studies have reported that
lidocaine could induce apoptosis (31,32).
Therefore, the present study also investigated the effects of
lidocaine on apoptosis in EC. It was demonstrated that lidocaine
treatment promoted the apoptosis of EC cells in a dose-dependent
manner, which was inhibited by 3-MA treatment. Furthermore, the
downregulated Bcl-2 protein expression, and the upregulated protein
expression levels of Bax, cleaved caspase-3 and cleaved caspase-9
caused by lidocaine treatment were reversed following 3-MA
treatment.
In conclusion, lidocaine inhibited the proliferation
and migration of EC cells, and promoted apoptosis by inducing
autophagy. However, the absence of an animal model, the use of only
one type of EC cell line and the absence of deeper analysis of
signaling pathways are limitations of the present study. In future
studies, the current results will be validated in different EC
cells and the signaling pathways involved will be thoroughly
investigated. In conclusion, lidocaine may be a potential
therapeutic drug for the prevention and treatment of EC.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DL, YC, LQ and YD conceived and designed the study,
and acquired and interpreted the data. DL was a major contributor
in writing the manuscript. DL and YD confirm the authenticity of
all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Trojano G, Olivieri C, Tinelli R, Damiani
GR, Pellegrino A and Cicinelli E: Conservative treatment in early
stage endometrial cancer: A review. Acta Biomed. 90:405–410.
2010.
|
|
2
|
Bartosch C, Pires M, Jeronimo C and Lopes
JM: The role of pathology in the management of patients with
endometrial carcinoma. Future Oncol. 13:1003–1020. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moore K and Brewer MA: Endometrial cancer:
Is this a new disease? Am Soc Clin Oncol Educ Book. 37:435–442.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Amant F, Moerman P, Neven P, Timmerman D,
Van Limbergen E and Vergote I: Endometrial cancer. Lancet.
366:491–505. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nuñez-Olvera SI, Gallardo-Rincón D,
Puente-Rivera J, Salinas-Vera YM, Marchat LA, Morales-Villegas R
and López-Camarillo C: Autophagy machinery as a promising
therapeutic target in endometrial cancer. Front Oncol. 9:13262019.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Buytaert E, Callewaert G, Vandenheede JR
and Agostinis P: Deficiency in apoptotic effectors Bax and Bak
reveals an autophagic cell death pathway initiated by photodamage
to the endoplasmic reticulum. Autophagy. 2:238–240. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang J, Wang Z, Zhao R, An L, Zhou X,
Zhao Y and Wang H: An integrated autophagy-related gene signature
predicts prognosis in human endometrial Cancer. BMC Cancer.
20:10302020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu H, Dilger JP and Lin J: Lidocaine
suppresses viability and migration of human breast cancer cells:
TRPM7 as a target for some breast cancer cell lines. Cancers
(Basel). 13:2342021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chang YC, Liu CL, Chen MJ, Hsu YW, Chen
SN, Lin CH, Chen CM, Yang FM and Hu MC: Local anesthetics induce
apoptosis in human breast tumor cells. Anesth Analg. 118:116–124.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liu C, Yu M, Li Y, Wang H, Xu C, Zhang X,
Li M, Guo H, Ma D and Guo X: Lidocaine inhibits the metastatic
potential of ovarian cancer by blocking NaV 1.5-mediated EMT and
FAK/Paxillin signaling pathway. Cancer Med. 10:337–349. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yuan J and Fei Y: Lidocaine activates
autophagy of astrocytes and ameliorates chronic constriction
injury-induced neuropathic pain. J Biochem. 170:25–31. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J,
Murray T and Thun MJ: Cancer statistics, 2008. CA Cancer J Clin.
58:71–96. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Berk T and Silberstein SD: The use and
method of action of intravenous lidocaine and its metabolite in
headache disorders. Headache. 58:783–789. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lancaster RJ, Wren K, Hudson A, Leavitt K,
Albala M and Tischaefer D: Intravenous lidocaine for chronic
neuropathic pain a systematic review addressing nursing care. Pain
Manag Nurs. 21:194–200. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chu R, Umukoro N, Greer T, Roberts J,
Adekoya P, Odonkor CA, Hagedorn JM, Olatoye D, Urits I, Orhurhu MS,
et al: Intravenous lidocaine infusion for the management of early
postoperative pain: A comprehensive review of controlled trials.
Psychopharmacol Bull. 50 (4 Suppl 1):216–259. 2020.PubMed/NCBI
|
|
16
|
Chi PW, Hsieh KY, Tsai CW, Hsu CW, Bai CH,
Chen C and Hsu YP: Intranasal lidocaine for acute migraine: A
protocol for the systematic review of randomized clinical trials.
Medicine (Baltimore). 98:e156992019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li H, Yue Y, Qu Y and Mu D: Lidocaine for
postoperative sore throat: A meta-analysis of randomized controlled
trials. Minerva Anestesiol. 86:546–553. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ye L, Zhang Y, Chen YJ and Liu Q:
Anti-tumor effects of lidocaine on human gastric cancer cells in
vitro. Bratisl Lek Listy. 120:212–217. 2019.PubMed/NCBI
|
|
19
|
Yang X, Zhao L, Li M, Yan L, Zhang S, Mi
Z, Ren L and Xu J: Lidocaine enhances the effects of
chemotherapeutic drugs against bladder cancer. Sci Rep. 8:5982018.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhu J and Han S: Lidocaine inhibits
cervical cancer cell proliferation and induces cell apoptosis by
modulating the lncRNA-MEG3/miR-421/BTG1 pathway. Am J Transl Res.
11:5404–5416. 2019.PubMed/NCBI
|
|
21
|
Li YJ, Lei YH, Yao N, Wang CR, Hu N, Ye
WC, Zhang DM and Chen ZS: Autophagy and multidrug resistance in
cancer. Chin J Cancer. 36:522017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhu YN, Fan WJ, Zhang C, Guo F, Li W, Wang
YF, Jiang ZS and Qu SL: Role of autophagy in advanced
atherosclerosis (Review). Mol Med Rep. 15:2903–2908. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Onorati AV, Dyczynski M, Ojha R and
Amaravadi RK: Targeting autophagy in cancer. Cancer. 124:3307–3318.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
D'Arcy MS: Cell death: A review of the
major forms of apoptosis, necrosis and autophagy. Cell Biol Int.
43:582–592. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sui X, Kong N, Ye L, Han W, Zhou J, Zhang
Q, He C and Pan H: p38 and JNK MAPK pathways control the balance of
apoptosis and autophagy in response to chemotherapeutic agents.
Cancer Lett. 344:174–179. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Izdebska M, Hałas-Wiśniewska M, Zielińska
W, Klimaszewska-Wiśniewska A, Grzanka D and Gagat M: Lidocaine
induces protective autophagy in rat C6 glioma cell line. Int J
Oncol. 54:1099–1111. 2019.PubMed/NCBI
|
|
27
|
Majtnerova P and Rousar T: An overview of
apoptosis assays detecting DNA fragmentation. Mol Biol Rep.
45:1469–1478. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fisher DE: Apoptosis in cancer therapy:
Crossing the threshold. Cell. 78:539–542. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Brown JM and Attardi LD: The role of
apoptosis in cancer development and treatment response. Nat Rev
Cancer. 5:231–237. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tang T, Xia Q and Xi M: Dihydroartemisinin
and its anticancer activity against endometrial carcinoma and
cervical cancer: Involvement of apoptosis, autophagy and
transferrin receptor. Singapore Med J. 62:96–103. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Qu X, Yang L, Shi Q, Wang X, Wang D and Wu
G: Lidocaine inhibits proliferation and induces apoptosis in
colorectal cancer cells by upregulating mir-520a-3p and targeting
EGFR. Pathol Res Pract. 214:1974–1979. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bruse LM: CORR insights®:
Bupivacaine and lidocaine induce apoptosis in osteosarcoma tumor
cells. Clin Orthop Relat Res. 479:195–197. 2021. View Article : Google Scholar : PubMed/NCBI
|