Introduction
Gastrointestinal stromal tumors (GISTs) are the most
frequently occurring potentially malignant mesenchymal-derived
tumors of the gastrointestinal tract, which are derived from
interstitial cells of Cajal or their precursors and have an annual
incidence of 10–15 cases per million (1–3). The
pathogenesis of GIST is closely associated with mutations in the
type III tyrosine kinase receptor gene KIT and the platelet-derived
growth factor receptor a (PDGFRA) gene, which are associated with
nearly 95% of cases (4,5).
The most common primary sites of GIST are the
stomach, accounting for 60–70% of cases, and the small intestine
accounting for 20–30% (6). Since
the introduction of imatinib for the treatment GIST in 2002, the
survival rate of patients with gastrointestinal stromal tumors has
improved (7–9). However, GIST cells with the PDGFRA
D842V mutation have since been found to have primary resistance to
imatinib, and some cells in a non-proliferative quiescent state
acquire secondary resistance during long-term treatment with this
drug (5,10–13).
Consequently, during the course of imatinib treatment, disease
progression may occur, resulting in metastases outside the primary
site. GIST commonly metastasizes to the liver (50–60%) (14) and peritoneum (20–43%), but less
frequently to other sites, with metastases to lymph nodes, lungs
and bone being relatively rare (15–18).
Nevertheless, the ability to identify these rare sites of
metastasis early is essential, as subsequent functional impairment
at metastatic sites may occur, affecting clinical outcomes and
leading to a poor prognosis. Since, to the best of our knowledge,
no systematic review of the literature of rare metastatic sites for
GIST other than the liver or peritoneum yet exists in the
literature, the occurrence of these rare metastatic GIST sites and
their metastatic characteristics are not yet clear. Therefore, the
present study aimed to provide a systematic review of the rare
sites of metastatic GIST, in order to enrich understanding of this
type of stromal tumor and to improve the prognosis of patients with
GIST metastasis in rare sites.
Materials and methods
Inclusion criteria
Literature published from 2000 onwards on GIST in
humans with metastases to sites other than the liver or peritoneum
following an initial diagnosis of GIST, treated or not, were
included. The papers were required to have viewable abstracts
online and full text that it was possible to download.
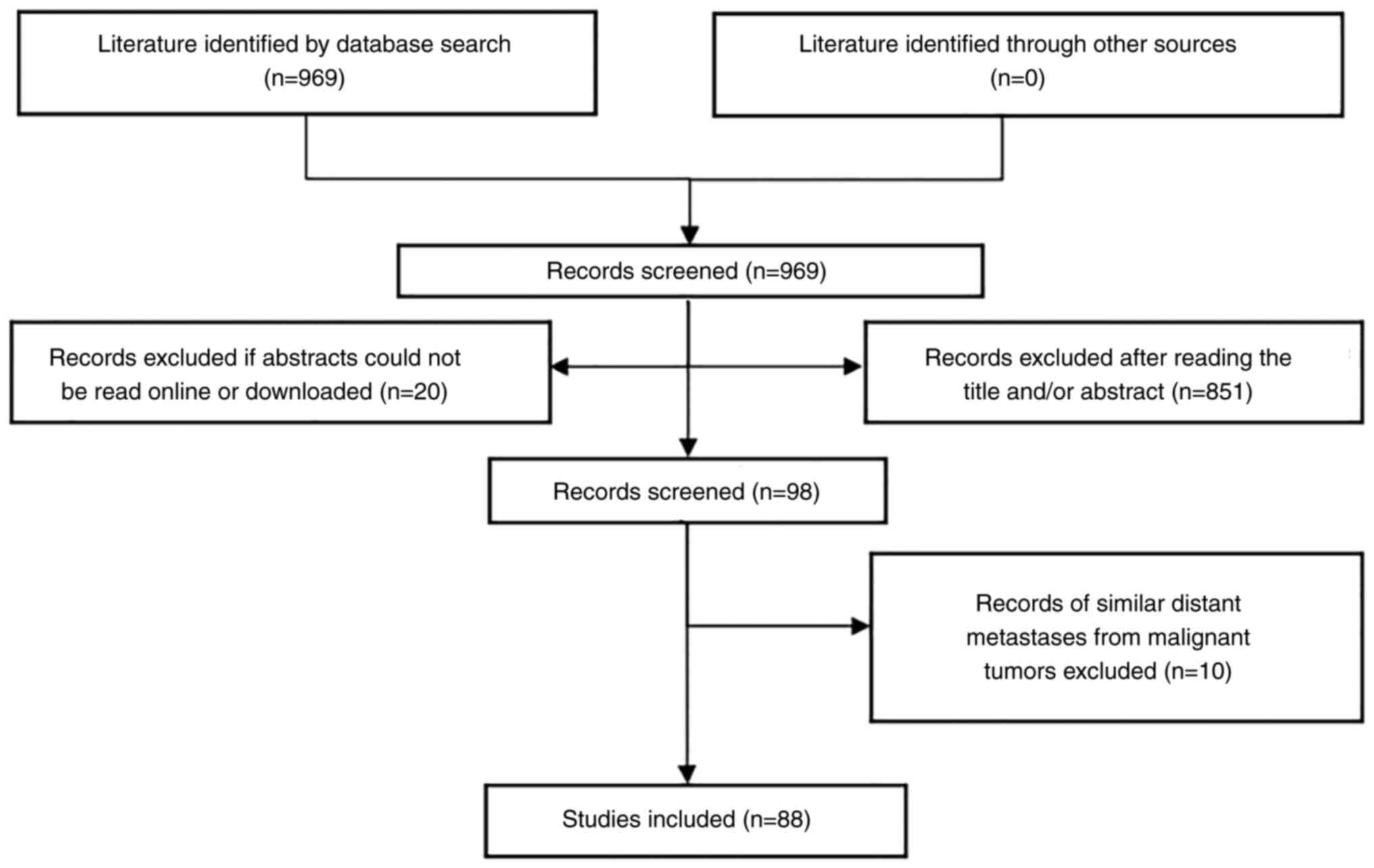
Search strategy
Cochrane and Medline databases were searched via
PubMed) using the following query: [‘gastrointestinal stromal
tumor’ (Title/Abstract) OR ‘GIST’ (Title/Abstract)] AND
[‘metastasis’ (Title/Abstract)]. A total of 969 articles were
retrieved, and based on the inclusion criteria, 88 articles with 98
cases were finally obtained. Considering that the literature
published prior to 2000 did not include complete clinical patient
information, only articles published on or after 2000 were
selected, with a search deadline of July 31, 2022 for published
literature. The screening flow chart is shown in Fig. 1.
Statistical analysis
The included articles were analyzed to record the
basic data used for the analysis. Study data included age, sex,
primary site, metastatic site, immunohistochemical staining for
CD117 and CD34, treatment of metastases and mean survival time.
Given the differences in management and the limited number of cases
identified, descriptive analyses were used and data were expressed
as mean or median values.
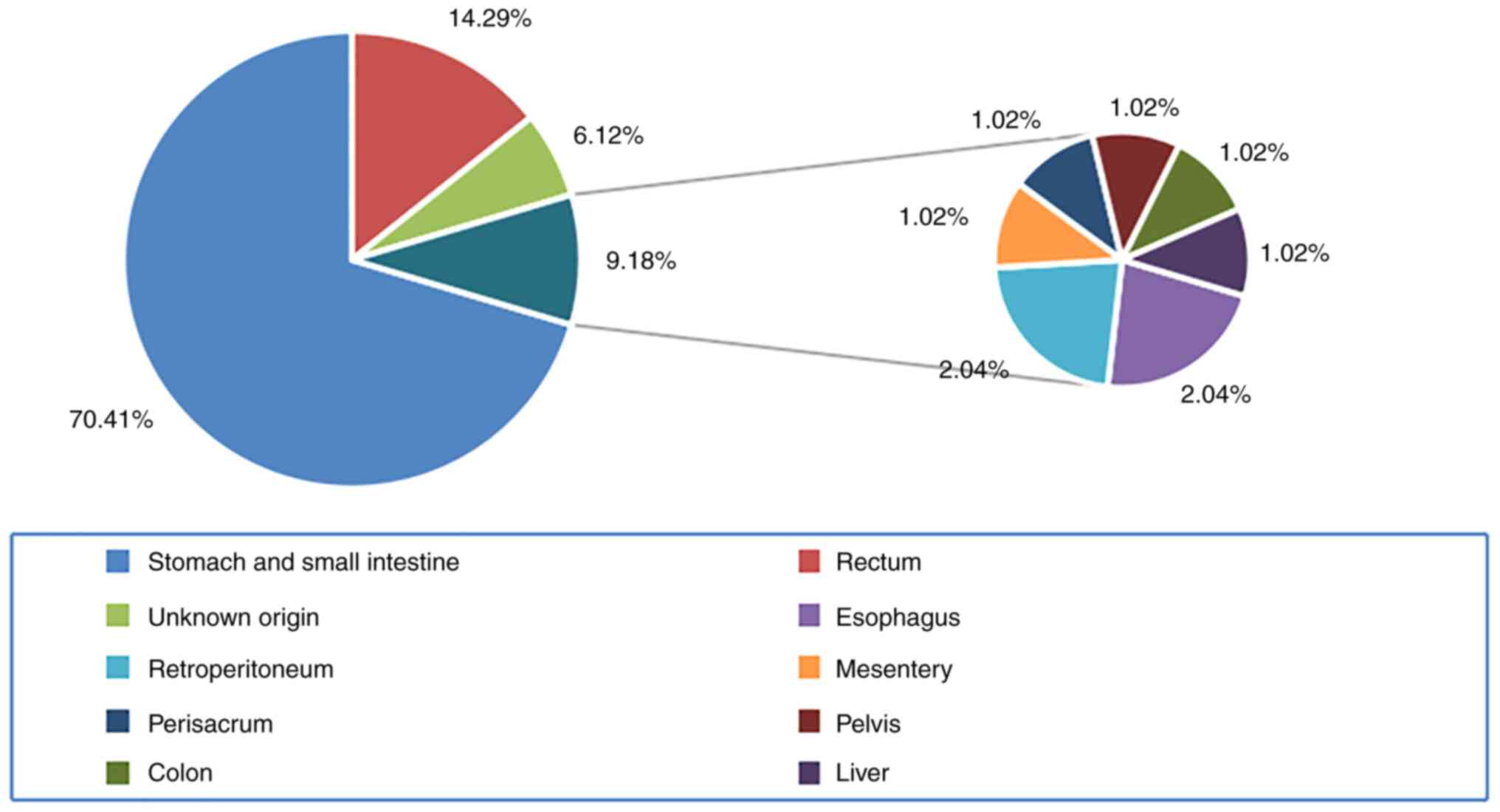
Rare metastatic sites and basic
characteristics of patients
It has been reported in the literature that >70%
of GISTs originate from the stomach or small intestine and 1–5%
from the colon and esophagus (19). The primary GIST sites found in the
present review included the stomach and small intestine in 69 cases
(70.41%), the rectum in 14 cases (14.29%), the esophagus in two
cases (2.04%), the colon in one case (1.02%), the retroperitoneum
in two cases (2.04%), the mesentery in one case (1.02%), the
perisacrum in one case (1.02%), the liver in one case (1.02%), the
pelvis in one case (1.02%) and unknown origin in six cases (6.12%).
The non-liver/peritoneum sites to which GIST metastasized are shown
in Fig. 2 and are similar to those
reported in the literature (19).
Since several metastatic sites were reported in some cases, the 98
cases included 118 metastatic sites. The 118 metastasis sites
included in the present review comprised: Bone (n=31), lung (n=10),
lymph nodes (n=13), intracranial sites (n=13), skin and
subcutaneous tissue (n=10), heart (n=7), skeletal muscle (n=7),
orbit and choroid (n=6), pancreas (n=3), spleen (n=2), bone marrow
(n=1), testis (n=3), scrotum (n=1), epididymis (n=1), penis (n=1),
ovary (n=2), cervix (n=1), kidney (n=1), bladder (n=1), adrenal
gland (n=2) and thyroid gland (n=2). The primary and metastatic
sites are summarized in Table I
(20–88). The mean age of the patients was
59.83 years (range, 17–85 years) and the median age of GIST onset
was 55–65 years (89,90). The patients included 61 males and
36 females, with a male-to-female ratio of 1.743. However, the sex
of one case could not be verified in the text (64).
 | Table I.Primary and metastatic sites of
gastrointestinal stromal tumors. |
Table I.
Primary and metastatic sites of
gastrointestinal stromal tumors.
| Primary site | Metastatic
site | (Refs.) |
|---|
| Small
intestine | Bone, lung, ovary,
lymph nodes, heart, skeletal muscle, intracranial sites, skin and
subcutaneous tissue, orbit, thyroid, scrotum, testes, bladder and
choroid | (18,20–53) |
| Stomach | Bone, lung, ovary,
lymph nodes, heart, intracranial sites, skin and subcutaneous
tissue, orbit, thyroid, adrenal gland, pancreas, spleen and
choroid | (23,28,33,54–73) |
| Rectum | Bone, lung,
skeletal muscle, heart, lung, kidney, eye socket, epididymis and
penis | (37,63,74–84) |
|
Retroperitoneum | Skin and lung | (45) |
| Pelvis | Lung | (85) |
| Perisacrum | Intracranial
sites | (86) |
| Esophagus | Intracranial sites
and lung | (87) |
| Colon | Lung | (88) |
| Liver | Adrenal gland | (84) |
Diagnosis of rare site metastasis of
GIST
The diagnosis of GIST with rare metastases is based
on clinical symptoms and signs, appropriate imaging and ultrasound
to determine the site of the lesion, and the results of puncture or
postoperative biopsy with molecular testing (6,91).
Clinical signs and symptoms of
different rare metastatic sites
In cases of GIST with metastasis at rare sites, the
symptoms will vary according to the organ affected by the
metastatic lesion. In cases with synchronous unusual site
metastases alongside the diagnosis of the primary GIST, the
manifestations of the metastatic site are often dominant. For
example, when intracranial GIST metastasis occurs, it usually
affects the nervous system, resulting in dizziness, headache,
memory impairment, loss of sensation and inability to move a single
limb, the inability to maintain body balance and abnormal gait and
posture, along with a series of neurological crements (27,32,35,40,51,61,70,87,87,92,93).
In cases of bone metastasis, pain manifests in the affected bone
area (29,37,48,52,53,63,69,75,80,94,95),
in cases of skeletal muscle involvement, a mass can be palpated in
the affected area (34,49,71,72,79),
and when metastasis occurs deep in the bone marrow, anemia may be
present (96). Furthermore, when
GIST metastasizes to the lungs, signs and symptoms that may be
observed include dyspnea, blood in the sputum, coughing and
shortness of breath (18,85,88,97).
When metastasis to superficial lymph nodes, skin or subcutaneous
tissue occurs, a mass may be superficially palpable (28,42,45,55,68,68,73,98).
However, when GIST metastasizes to the heart, although no clinical
signs are evident in the early stages (24,82,83,99,100), the late stages may manifest as
cardiogenic shock (43). When GIST
metastasizes to the orbit, a mass may be palpable around the orbit
(60) and may manifest as
periorbital pain (101), and with
involvement of the choroid, vision loss or diplopia may occur
(44,48,51,67).
Menstrual flow may increase when there is metastasis in the cervix
(102), and when the testicles,
penis or scrotum are involved, swelling of the testicles and
scrotum, difficulty in achieving an erection and obstruction of the
urinary tract are typical manifestations (21,38,64,74).
When GIST metastasizes to the adrenal gland, the secretion of
catecholamine hormones may become abnormal, and symptoms of
hypertension may occur (59,103). In cases of metastasis to the
thyroid gland, systemic manifestations such as weight loss,
weakness and respiratory distress can be observed (23). The presence of rare site GIST
metastasis may be initially discovered by the observation of the
aforementioned early symptoms.
Imaging of rare metastatic sites
In cases of extrahepatic/extraperitoneal GIST
metastasis, imaging examinations can be performed according to the
individual patient's symptoms and signs to clarify the site of
metastasis; however, the imaging manifestations vary depending on
the site. For example, when GIST metastasizes to the intracranial
area, computed tomography (CT) scans show high density with
cerebral edema and enhancement scans show homogeneous enhancement.
The magnetic resonance imaging (MRI) of cranial GIST metastasis
shows equivocal masses in T1- and T2-weighted terms, with
circumferential enhancement in T1-weighted sequences and
inhomogeneous enhancement in T2-weighted sequences (40,61,70,104), while the intracranial aggregation
of 18F-fluorodeoxyglucose is not reported as being
visible when examined using positron emission tomography (PET)
(27,86,87,92).
When GIST metastasizes to bone, it is primarily present in the
spine (17), with CT plain
scanning showing osteolytic bone destruction of the vertebral ody
(29,31,37,47,52,53,69,76,78,81,84,94,95).
Additionally, MRI reveals dural protrusion and compression of the
spinal cord, usually with spinal stenosis, T1 and T2 high signals
on enhancement scans and partial necrosis and non-uniform
enhancement of the lesion (29,31,48,63,76,78,81,95).
The PET-CT imaging of bone metastasis shows hypermetabolic changes
at the site of a vertebral lesion (37,47,62,63,69,75,76).
In cases with the involvement of skeletal muscle, T2-weighted
images show a mass with high signal intensity (71,72).
When GIST metastasizes to the lungs, a dense mass is visible in one
or both lungs (18,85,88,97),
and in the lymph nodes, GIST metastasis appears on CT images as a
hypodense mass with no enhancement when examined using enhanced MRI
(39,57,58)
and as a hypoechoic cystic or solid mass when examined using
ultrasound (28,33,29).
No enhancement is seen on chest enhancement CT images when GIST
metastasizes to the heart (85,100), and PET-CT reveals high
18F-fluorodeoxyglucose accumulation in the mass
(24,83), with echocardiograms showing a
hypoechoic mass in the ventricle or atrium (24,83,99,100). When GIST metastasizes to the
orbit, CT shows a hypodense mass with well-defined lesions, and
enhanced MRI shows uniform enhancement (20,60),
Optical coherence tomography may reveal edema of the optic disc and
retinal neuroepithelia (44),
while MRI presents a well-defined round nodule with isointensity to
eye muscles in T1-weighted sequences and high signal T2-weighted
sequences (44,82) and enhancement scans show
homogeneous enhancement (20).
Ultrasonography of metastasis to the orbit also shows a
well-defined homogeneous hypoechoic mass around the orbit without
retinal detachment (44). In cases
of choroidal involvement, funduscopic examination may reveal an
enlarged choroidal mass surrounded by a flat retinal detachment,
while ultrasonography reveals a choroidal mass with moderate-to-low
reflectivity (51,67). When GIST metastasizes to the
ovaries, transvaginal ultrasound detects a solid pelvic hypoechoic
mass with irregular margins, and energy Doppler ultrasound presents
a grade 3 blood flow signal (41).
In ovarian metastasis, the presence of a mass in the pelvis may
also be detected by CT, and enhanced CT shows heterogeneous
enhancement of the mass (41,102). When GIST metastasizes to the male
genital system, metastatic GIST in the scrotum appears as a
vascular-rich hypoechoic mass on ultrasound (38). In addition, CT may reveal multiple
satellite nodules distributed along the spermatic cord (74,77),
while contrast-enhanced T1-weighted MRI does not show mass
enhancement (64). Lastly, when
GIST metastasizes to the spleen, a low-density mass in the spleen
is shown using abdominal CT and enhancement is observed on enhanced
scans (59).
Pathological features and gene
mutation detection
Upon pathological examination, GIST can be
morphologically classified into three types: Spindle cell (70%),
epithelioid (20%) and mixed spindle and epithelioid types (10%)
(14,19,105). Spindle cells are microscopically
viewed as spindle-shaped with uniform cytoplasm, eosinophilic
cytoplasmic staining, ovoid nuclei and juxtaposed nuclear vesicles
(106). Epithelioid cells are
round with round or oval nuclei (107), and mixed types are observed as a
mixture of epithelial and spindle cells within pathological
sections, or as a transitional pattern between the two (91). In the present review, 57 cases
(58.16%) were of spindle cell type, 15 cases (15.31%) were of
epithelial cell type, 12 cases (12.24%) were of mixed cell type and
14 cases were of unknown type and 14 cases (14.29%) were of unknown
type. A total of 69 cases were immunohistochemically tested, with
62 cases being positive for CD117 and 54 cases being positive for
CD34, revealing that the latter is less often positive. In
addition, bone marrow biopsy is essential for the analysis of
gastrointestinal stromal tumors that have metastasized to the bone
marrow (96).
Therapy and prognosis for rare site GIST
metastases
Treatment and prognosis details described in the
literature for rare metastatic sites of GIST are shown in Table II (18,20–27,29–41,43,44,46,47,50–54,56–67,69–72,74,75,77–80,82–88,92,94–101,103,104,108–112). Treatment modalities included TKIs
alone, surgical treatment or resection alone, radiotherapy alone,
resection with TKIs, resection with radiation therapy, radiation
therapy with TKIs, and resection with radiation therapy and TKIs.
Surgical resection was performed at the primary site in 87 cases
(92.31%). Among these cases, 17 had surgical resection of both
primary and metastatic sites diagnosed at the same time, 67 had
postoperative metastases from rare sites, 52 had surgical resection
of rare metastatic site, and 39 cases had liver or peritoneal
metastases prior to the surgical resection of rare sites, of which
21 cases had surgical treatment. Notably, a recent study by Pantuso
et al (113) confirmed
that positive surgical margins had no effect on the overall and
recurrence-free survival of GIST patients. Therefore, surgical
resection is an important treatment modality for GIST. In addition
to surgical treatment, TKIs are also very valuable in pre- or
postoperative adjuvant therapy. The TKI drugs imatinib, sunitinib,
regorafenib and ripretinib have been approved for the first-,
second-, third- and fourth-line treatment of GIST, respectively
(114). A multicenter randomized
controlled trial clearly demonstrated that imatinib treatment at a
dose of 400 mg/day achieved objective remission in 81.6% of
patients with unresectable or metastatic GIST (115). Further, other studies have
confirmed that preoperative imatinib can effectively prevent tumor
rupture and reduce the incidence of surgical complications
(116,117). However, when patients experience
imatinib resistance or intolerable adverse effects, treatment with
the second-line drug sunitinib at a dose of 50 mg/day for 4 weeks
followed by 2 weeks without treatment, or at 37.5 mg/day
continuously is recommended (76,78).
One study demonstrated improved patient compliance for continuous
once-daily 37.5 mg sunitinib dosing compared with intermittent
sunitinib dosing in patients following imatinib failure (118). Furthermore, sunitinib may achieve
greater efficacy as a first-line therapy in patients with
intracranial GIST metastases due to the inability of imatinib to
cross the blood-brain barrier (BBB) (119,120); sunitinib can cross the BBB and
achieve a sufficient drug concentration for improved therapeutic
outcomes (35,121). While imatinib and sunitinib are
clinically beneficial for the majority of patients with metastatic
GIST, some patients experience progression as well as intolerable
adverse effects following treatment. The third-line treatment
regorafenib and the fourth-line treatment ripretinib have been
demonstrated to be effective in such patients (50,77,85),
Therefore, for patients with GIST at rare metastatic sites, TKIs
used alone or in combination can be selected or replaced according
to efficacy. In addition, radiotherapy may be used as an adjuvant
treatment when GIST metastasizes to the skull and bone. At a
typical dose of 30 Gy daily, radiation can effectively reduce tumor
size and alleviate symptoms, while creating optimal conditions for
surgery (40,61,62,78).
The administration of 4 mg zoledronic acid intravenously has also
been shown to reduce bone destruction in GIST bone metastases
(36,75).
 | Table II.Treatments and mean survival times of
patients with gastrointestinal stromal tumors at rare metastatic
sites. |
Table II.
Treatments and mean survival times of
patients with gastrointestinal stromal tumors at rare metastatic
sites.
| Metastatic
site | Therapies for
metastases | Mean survival time,
months | (Refs.) |
|---|
| Bone | R, TKIs, RT, R + RT
+ TKIs, R + TKIs and R + RT | 63.50 | (26,29,31,36,37,46,47,52,53,62,63,66,69,75,77,78,80,84,94,95) |
| Bone marrow | TKIs | 8.00 | (96) |
| Skeletal
muscle | R, R + TKIs and
RT+TKIs | 38.00 | (25,34,43,71,72,79) |
| Lymph nodes | R and R + TKIs | 33.20 | (22,23,27,30,33,39,54,57,58,108) |
| Heart | R and R + TKIs | 76.50 | (24,83,99,100) |
| Lung | R + TKIs | 80.00 | (18,50,56,85,88,97) |
| Intracranial
sites | R, R + TKIs, R +
RT, R + RT + TKIs | 35.81 | (27,32,35,40,51,61,70,86,87,92,104) |
| Skin or
subcutaneous tissue | R + TKIs | 60.00 | (42,45,55,68,73,98) |
| Orbit or
choroid | R, R + TKIs and R +
RT | 72.00 | (20,44,51,60,67,82,101,109) |
| Thyroid | R | 9.00 | (23) |
| Pancreas | R + TKIs | 57.00 | (65,110) |
| Inferior vena
cava | R + TKIs | 14.00 | (111) |
| Spleen | R + TKIs | 43.00 | (59,110) |
| Kidney | R + TKIs | 187.00 | (37) |
| Adrenal gland | R + TKIs | 12.50 | (59,103) |
| Ovary | R + TKIs | NA | (41,112) |
| Scrotum | TKIs | 24.00 | (38) |
| Testicle | R and TKIs | NA | (21,74) |
| Penis | R + TKIs | 48.00 | (64) |
| Bladder | R + TKIs | 62.00 | (46) |
Based on the limited information reported in the
literature, the mean survival time for patients with GIST at rare
metastatic sites was >61.50 months, with a mean survival time of
59.59 months for men and 63.78 months for women. Among all the
reported cases, 21 (15.31%) had a disease course ending in death.
When intracranial metastases were present, patients had a poor
prognosis with a mean survival time of 35.81 months, which may have
been associated with the inability of imatinib to penetrate the BBB
and maintain an effective therapeutic concentration. However, this
point requires confirmation by future randomized controlled
studies. The mean survival time of patients was 32.75 months for
those treated with TKIs alone, 73.11 months for resection alone,
65.17 months for radiotherapy alone, 86.33 months for resection
with TKIs, 36.4 months for resection with radiotherapy and 49.17
months for resection with radiotherapy and TKIs. The lower survival
rate for patients whose treatment included radiotherapy may have
been due to patients requiring radiotherapy being more symptomatic
and unable to undergo surgery in a timely manner. Also, if the
radiotherapy was administered as a palliative treatment, this may
have resulted in a lower mean survival time compared with that for
other treatment modalities. Although the mean survival times of
patients with GIST metastases in the thyroid, adrenal gland and
scrotum were markedly lower compared with those in other sites, the
number of cases was small and the representative times may be
higher in clinical practice; however, this pends confirmation with
additional studies.
Summary and prospects
In addition to the liver and peritoneum, GIST can
metastasize to rare sites, namely the bone, bone marrow, lungs,
lymph nodes, intracranial area, skin, subcutaneous tissue, heart,
skeletal muscle, orbit, pancreas, spleen, testes, scrotum,
epididymis, penis, ovaries, cervix, kidneys, bladder, adrenal
glands and thyroid. Based on the symptoms of the patients along
with imaging and ultrasound examinations, the primary and
metastatic site can be determined on a basic level; however,
diagnosis must be confirmed by the immunohistochemical detection of
CD117 and CD34. For primary localized GIST, surgery is the most
important treatment, sometimes combined with pre- or postoperative
neo-/adjuvant treatment, but for metastatic GIST, TKIs are the
principal treatment. TKIs may be combined with surgery and/or with
radiotherapy as an adjuvant treatment in cases of bone and
intracranial metastases. In patients with a poor prognosis due to
intracranial metastases, the use of sunitinib as the first-line
treatment may improve prognosis; however, further studies are
needed to confirm this.
The present review was constrained by the low
incidence of GIST and the limited number of cases collected,
unpublished data and associated literature not being available in
the English language. However, rare metastatic sites of GIST other
than the liver and peritoneum were summarized and reviewed, which
may assist with their diagnosis and serve as a reference for
selection of the appropriate treatment modality and estimation of
prognosis. In addition, more high-quality research evidence such as
large-sample, blinded randomized controlled trials is required, to
improve clinicians' understanding of the management of GISTs with
rare metastases.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
XY, XL and KW conceived the study and drafted the
manuscript. XY made substantial contributions to the interpretation
of the data, drafting the manuscript and revising it critically for
important intellectual content. XL helped to organize the data
collected, helped to collect information regarding the survival
time of the patients and helped to write the manuscript. All
authors revised the manuscript. Data authentication is not
applicable. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Demetri GD, von Mehren M, Antonescu CR,
DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF,
Schuetze S, et al: NCCN Task Force report: Update on the management
of patients with gastrointestinal stromal tumors. J Natl Compr Canc
Netw. 8 (Suppl 2):S1–S44. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Søreide K, Sandvik OM, Søreide JA, Giljaca
V, Jureckova A and Bulusu VR: Global epidemiology of
gastrointestinal stromal tumours (GIST): A systematic review of
population-based cohort studies. Cancer Epidemiol. 40:39–46. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Graadt van Roggen JF, van Velthuysen ML
and Hogendoorn PC: The histopathological differential diagnosis of
gastrointestinal stromal tumours. J Clin Pathol. 54:96–102. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Corless CL, Fletcher JA and Heinrich MC:
Biology of gastrointestinal stromal tumors. J Clin Oncol.
22:3813–3825. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Klug LR, Khosroyani HM, Kent JD and
Heinrich MC: New treatment strategies for advanced-stage
gastrointestinal stromal tumours. Nat Rev Clin Oncol. 19:328–341.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nishida T, Yoshinaga S, Takahashi T and
Naito Y: Recent progress and challenges in the diagnosis and
treatment of gastrointestinal stromal tumors. Cancers (Basel).
13:31582021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Debiec-Rychter M, Sciot R, Le Cesne A,
Schlemmer M, Hohenberger P, van Oosterom AT, Blay JY, Leyvraz S,
Stul M, Casali PG, et al: KIT mutations and dose selection for
imatinib in patients with advanced gastrointestinal stromal
tumours. Eur J Cancer. 42:1093–1103. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Blanke CD, Demetri GD, von Mehren M,
Heinrich MC, Eisenberg B, Fletcher JA, Corless CL, Fletcher CD,
Roberts PJ, Heinz D, et al: Long-term results from a randomized
phase II trial of standard-versus higher-dose imatinib mesylate for
patients with unresectable or metastatic gastrointestinal stromal
tumors expressing KIT. J Clin Oncol. 26:620–625. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Keung EZ, Raut CP and Rutkowski P: The
landmark series: Systemic therapy for resectable gastrointestinal
stromal tumors. Ann Surg Oncol. 27:3659–3671. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Antonescu CR, Besmer P, Guo T, Arkun K,
Hom G, Koryotowski B, Leversha MA, Jeffrey PD, Desantis D, Singer
S, et al: Acquired resistance to imatinib in gastrointestinal
stromal tumor occurs through secondary gene mutation. Clin Cancer
Res. 11:4182–4190. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Serrano C, Mariño-Enríquez A, Tao DL,
Ketzer J, Eilers G, Zhu M, Yu C, Mannan AM, Rubin BP, Demetri GD,
et al: Complementary activity of tyrosine kinase inhibitors against
secondary kit mutations in imatinib-resistant gastrointestinal
stromal tumours. Br J Cancer. 120:612–620. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wardelmann E, Merkelbach-Bruse S, Pauls K,
Thomas N, Schildhaus HU, Heinicke T, Speidel N, Pietsch T, Buettner
R, Pink D, et al: Polyclonal evolution of multiple secondary KIT
mutations in gastrointestinal stromal tumors under treatment with
imatinib mesylate. Clin Cancer Res. 12:1743–1749. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Desai J, Shankar S, Heinrich MC, Fletcher
JA, Fletcher CD, Manola J, Morgan JA, Corless CL, George S, Tuncali
K, et al: Clonal evolution of resistance to imatinib in patients
with metastatic gastrointestinal stromal tumors. Clin Cancer Res.
13:5398–5405. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
McDonnell MJ, Punnoose S, Viswanath YKS,
Wadd NJ and Dhar A: Gastrointestinal stromal tumours (GISTs): An
insight into clinical practice with review of literature. Frontline
Gastroenterol. 8:19–25. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rubin BP: Gastrointestinal stromal
tumours: An update. Histopathology. 48:83–96. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
DeMatteo RP, Maki RG, Singer S, Gonen M,
Brennan MF and Antonescu CR: Results of tyrosine kinase inhibitor
therapy followed by surgical resection for metastatic
gastrointestinal stromal tumor. Ann Surg. 245:347–352. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yang J, Yan J, Zeng M, Wan W, Liu T and
Xiao JR: Bone metastases of gastrointestinal stromal tumor: A
review of published literature. Cancer Manag Res. 12:1411–1417.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kassimi M, Berrada S, Habi J, Guerroum H,
Chihabeddine M and Mahi M: Gastrointestinal stromal tumor of the
small intestine with lung metastasis. Radiol Case Rep. 17:32–34.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors: Review on morphology, molecular pathology,
prognosis, and differential diagnosis. Arch Pathol Lab Med.
130:1466–1478. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Akiyama K, Numaga J, Kagaya F, Takazawa Y,
Suzuki S, Koseki N, Kato S, Kaburaki T and Kawashima H: Case of
optic nerve involvement in metastasis of a gastrointestinal stromal
tumor. Jpn J Ophthalmol. 48:166–168. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dorić M, Radović S, Babić M, Hukić A,
Kuskunović S, Tomić I and Selak I: Testicular metastasis of
gastrointestinal stromal tumor of the jejunum. Bosn J Basic Med
Sci. 7:176–179. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
El Demellawy D, Shokry P, Ing A and
Khalifa M: Polypoid gastrointestinal stromal tumor of small bowel
metastasizing to mesenteric lymph nodes: A case report. Pathol Res
Pract. 204:197–201. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Peparini N, Di Matteo FM, Maturo A,
Marzullo A and Campana FP: Unusual metastasis of gastrointestinal
stromal tumor misdiagnosed as anaplastic thyroid carcinoma. Int J
Surg. 6:415–417. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cauchi C, Trent JC, Edwards K, Davey M,
Lopez M, Yu JQ and von Mehren M: An unusual site of metastasis from
gastrointestinal stromal tumor. Rare Tumors. 2:e582010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cichowitz A, Thomson BN and Choong PF:
GIST metastasis to adductor longus muscle. ANZ J Surg. 81:490–491.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lolli C, Pantaleo MA, Nannini M, Saponara
M, Pallotti MC, Scioscio VD, Barbieri E, Mandrioli A and Biasco G:
Successful radiotherapy for local control of progressively
increasing metastasis of gastrointestinal stromal tumor. Rare
Tumors. 3:e492011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Naoe H, Kaku E, Ido Y, Gushima R, Maki Y,
Saito H, Yokote S, Gushima R, Nonaka K, Hoshida Y, et al: Brain
metastasis from gastrointestinal stromal tumor: A case report and
review of the literature. Case Rep Gastroenterol. 5:583–589. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vassos N, Agaimy A, Hohenberger W and
Croner RS: Extraabdominal lymph node metastasis in gastrointestinal
stromal tumors (GIST). J Gastrointest Surg. 15:1232–1236. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Slimack NP, Liu JC, Koski T, McClendon J
Jr and O'Shaughnessy BA: Metastatic gastrointestinal stromal tumor
to the thoracic and lumbar spine: First reported case and surgical
treatment. Spine J. 12:e7–e12. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kang KY and Lee W: Gastrointestinal
stromal tumor with extensive lymphatic metastasis: A case report. J
Gastric Cancer. 13:192–195. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ishi Y, Nakayama N, Kobayashi H, Yamaguchi
S, Terasaka S and Houkin K: Successful removal of a metastatic
gastrointestinal stromal tumor in the craniovertebral junction
using an occipital artery to posterior inferior cerebellar artery
bypass. Case Rep Neurol. 6:139–143. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sato K, Tanaka T, Kato N, Ishii T, Terao T
and Murayama Y: Metastatic cerebellar gastrointestinal stromal
tumor with obstructive hydrocephalus arising from the small
intestine: A case report and review of the literature. Case Rep
Oncol Med. 2014:3431782014.PubMed/NCBI
|
|
33
|
Shafizad A, Mohammadianpanah M, Nasrolahi
H, Mokhtari M and Mousavi SA: Lymph node metastasis in
gastrointestinal stromal tumor (GIST): To report a case. Iran J
Cancer Prev. 7:171–174. 2014.PubMed/NCBI
|
|
34
|
Suzuki K, Yasuda T, Nagao K, Hori T,
Watanabe K, Kanamori M and Kimura T: Metastasis of gastrointestinal
stromal tumor to skeletal muscle: A case report. J Med Case Rep.
8:2562014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Takeuchi H, Koike H, Fujita T, Tsujino H
and Iwamoto Y: Sunitinib treatment for multiple brain metastases
from jejunal gastrointestinal stromal tumor: Case report. Neurol
Med Chir (Tokyo). 54:664–669. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Aktan M, Koc M, Yavuz BB and Kanyilmaz G:
Two cases of gastrointestinal stromal tumor of the small intestine
with liver and bone metastasis. Ann Transl Med.
3:2592015.PubMed/NCBI
|
|
37
|
Nakajima T, Sugiyama T, Baba H, Hatta H,
Nishida T, Miwa S, Hayashi S, Tsuneyama K and Imura J: Bone
metastasis in gastrointestinal stromal tumors preferentially occurs
in patients with original tumors in sites other than the stomach.
Int J Clin Exp Pathol. 8:5955–5959. 2015.PubMed/NCBI
|
|
38
|
Thomas R and Swamy S: Rare case of
gastrointestinal stromal tumor presenting with scrotal metastasis.
Indian J Surg. 77 (Suppl 1):S188–S189. 2015. View Article : Google Scholar
|
|
39
|
Ma C, Hao SL, Liu XC, Nin JY, Wu GC, Jiang
LX, Fancellu A, Porcu A and Zheng HT: Supraclavicular lymph node
metastases from malignant gastrointestinal stromal tumor of the
jejunum: A case report with review of the literature. World J
Gastroenterol. 23:1920–1924. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Badri M, Chabaane M, Gader G, Bahri K and
Zammel I: Cerebellar metastasis of gastrointestinal stromal tumor:
A case report and review of the literature. Int J Surg Case Rep.
42:165–168. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
De Leo A, Nannini M, Dondi G, Santini D,
Urbini M, Gruppioni E, De Iaco P, Perrone AM and Pantaleo MA:
Unusual bilateral ovarian metastases from ileal gastrointestinal
stromal tumor (GIST): A case report. BMC Cancer. 18:3012018.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kim YJ, Lee WJ, Won CH, Choi JH and Lee
MW: Metastatic cutaneous duodenal gastrointestinal stromal tumor: A
possible clue to multiple metastases. Ann Dermatol. 30:345–347.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Miyazaki S, Ogimoto A, Matsukage S and
Ohshima K: Extracardiac tumor from duodenal primary
gastrointestinal stromal tumor. Intern Med. 57:1327–1328. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yu Y, Ji X, Li W and Wu C: Orbital
metastasis from a gastrointestinal stromal tumor: A case report. Am
J Ophthalmol Case Rep. 16:1005282019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Liu P, Tan F, Liu H, Ge J, Liu S, Lei T
and Zhao X: Skin metastasis of gastrointestinal stromal tumors: A
case series and literature review. Cancer Manag Res. 12:7681–7690.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lo YT, Mak DSK and Nolan CP: Surgical
management of vertebral metastatic gastrointestinal stromal tumor:
Case illustration, literature review, and pooled analysis. Surg
Neurol Int. 11:3432020. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Yilmaz MT, Gultekin M, Yalcin S, Tuncel M,
Gedikoglu G, Yildiz F and Cengiz M: Stereotactic ablative
radiotherapy for bone metastasis of gastrointestinal stromal tumor:
Case report and review of the literature. Rep Pract Oncol
Radiother. 25:331–335. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Braunstein C, Sirveaux F, Kalbacher E,
Aubry S, Delroeux D, Hubert P, Marie B, Meynard G, Mihai I and
Chaigneau L: Humeral metastasis as the only recurrence of a 5-year
resected gastrointestinal stromal tumor: A case report. J Med Case
Rep. 15:4282021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhu G, Sun W, Liu Y, Wang H and Ye S:
Skeletal muscle metastasis from a gastrointestinal stromal tumor: A
case report. Medicine (Baltimore). 100:e270112021. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Meng Y, Li LL, Wang H and Zhao X:
Ripretinib in the treatment of advanced gastrointestinal stromal
tumor with metastases in liver, lung and bone: A case report.
Zhonghua Wei Chang Wai Ke Za Zhi. 24:823–824. 2021.(In Chinese).
PubMed/NCBI
|
|
51
|
Hughes B, Yip D, Goldstein D, Waring P,
Beshay V and Chong G: Cerebral relapse of metastatic
gastrointestinal stromal tumor during treatment with imatinib
mesylate: Case report. BMC Cancer. 4:742004. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lutz JC, El-Bouihi M, Vidal N, Fricain JC,
Robert M, Deminière C and Zwetyenga N: Mandibular metastases from
an ileum stromal tumor. Rev Stomatol Chir Maxillofac. 109:399–402.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Feki J, Bouzguenda R, Ayedi L, Bradi M,
Boudawara T, Daoud J and Frikha M: Bone metastases from
gastrointestinal stromal tumor: A case report. Case Rep Oncol Med.
2012:5098452012.PubMed/NCBI
|
|
54
|
Canda AE, Ozsoy Y, Nalbant OA and Sagol O:
Gastrointestinal stromal tumor of the stomach with lymph node
metastasis. World J Surg Oncol. 6:972008. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kroep JR, Bovée JV, van der Molen AJ,
Hogendoorn PC and Gelderblom H: Extra-abdominal subcutaneous
metastasis of a gastrointestinal stromal tumor: Report of a case
and a review of the literature. J Cutan Pathol. 36:565–569. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kurashina K, Hosoya Y, Sakurai S, Endo S,
Lefor A and Yasuda Y: Gastrointestinal stromal tumor of the stomach
with extremely slow-growing hematogenous metastasis. Int J Clin
Oncol. 14:262–265. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Yamada E, Oyaizu T and Miyashita T: A case
of gastrointestinal stromal tumor of the stomach with lymph node
metastasis followed up for 7 years without evidence of recurrence
after surgery. Nihon Shokakibyo Gakkai Zasshi. 107:743–749.
2010.(In Japanese). PubMed/NCBI
|
|
58
|
Zhang Q, Yu JW, Yang WL, Liu XS and Yu JR:
Gastrointestinal stromal tumor of stomach with inguinal lymph nodes
metastasis: A case report. World J Gastroenterol. 16:1808–1810.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Kim HG, Ryu SY, Joo JK, Kang H, Lee JH and
Kim DY: Recurring gastrointestinal stromal tumor with splenic
metastasis. J Korean Surg Soc. 81 (Suppl 1):S25–S29. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Woo D, Leong J, Waring D, Sharma A and
Martin P: Orbital gastrointestinal stromal tumor metastasis. Orbit.
31:129–131. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Drazin D, Spitler K, Jeswani S, Shirzadi
A, Bannykh S and Patil C: Multiple intracranial metastases from a
gastric gastrointestinal stromal tumor. J Clin Neurosci.
20:471–473. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Heymann S, Imperiale A, Schlund-Schoettel
E, Sauer B and Dourthe LM: A rare case of bone metastasis from
gastro-intestinal stromal tumour: Place of radiotherapy. Cancer
Radiother. 18:55–58. 2014.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Suzuki K, Yasuda T, Nagao K, Hori T,
Watanabe K, Kanamori M and Kimura T: Bone metastasis of a
gastrointestinal stromal tumor: A report of two cases. Oncol Lett.
9:1814–1818. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Carlson J, Alobuia W and Mizell J: Rectal
gastrointestinal stromal tumor with metastasis to the penis: Case
report and review of literature. Int J Surg Case Rep. 29:172–175.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Hagiwara N, Matsutani T, Nomura T, Fujita
I, Kanazawa Y, Ueda J, Arai H, Kakinuma D, Kanno H, Naito Z and
Uchida E: Pancreatic metastasis from gastrointestinal stromal tumor
of the stomach: A case report. J Nippon Med Sch. 83:133–138. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Fujisawa T, Matsumoto Y, Nishizawa A and
Takata M: A case of liver and bone metastases after complete
resection of gastric GIST effectively treated with radiotherapy and
imatinib mesylate. Nihon Shokakibyo Gakkai Zasshi. 110:1258–1264.
2013.(In Japanese). PubMed/NCBI
|
|
67
|
Gentile CM, Lombardi AA and Croxatto JO:
Choroidal metastasis from gastrointestinal stromal tumour: A case
report. Br J Ophthalmol. 92:156–157. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Shabahang M and Livingstone AS: Cutaneous
metastases from a gastrointestinal stromal tumor of the stomach:
Review of literature. Dig Surg. 19:64–65. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Friedrich RE and Zustin J: Late metastasis
of gastrointestinal stromal tumour to the oral cavity. Anticancer
Res. 30:4283–4288. 2010.PubMed/NCBI
|
|
70
|
Jagannathan JP, Ramaiya NH, Shinagare AB,
Hornick JL and George S: Intracranial metastasis from pediatric GI
stromal tumor. J Clin Oncol. 30:e122–e125. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Jin SS, Jeong HS, Noh HJ, Choi WH, Choi
SH, Won KY, Kim DP, Park JC, Joung MK, Kim JG, et al:
Gastrointestinal stromal tumor solitary distant recurrence in the
left brachialis muscle. World J Gastroenterol. 21:6404–6408. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Mutlu H, Balkarlı H, Musri FY, Salim DK,
Eryılmaz MK, Ünal B and Coşkun HŞ: Gastrointestinal stromal tumor
and isolated anterior tibial muscle metastasis as first recurrence.
J Cancer Res Ther. 11:10372015. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Aickara DJ, McBride J, Morrison B and
Romanelli P: Multidrug resistant gastrointestinal stromal tumor
with multiple metastases to the skin and subcutaneous soft tissue:
A case report and review of literature. J Cutan Pathol. 47:398–401.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Perrone N, Serafini G, Vitali A, Lacelli
F, Sconfienza L and Derchi LE: Gastrointestinal stromal tumor
metastatic to the scrotum. J Ultrasound Med. 27:961–964. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Tezcan Y and Koç M: Gastrointestinal
stromal tumor of the rectum with bone and liver metastasis: A case
study. Med Oncol. 28 (Suppl 1):S204–S206. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Selcukbiricik F, Tural D, Ozturk MA,
Dervisoglu S, Sager S, Hız M and Mandel NM: Gastrointestinal
stromal tumor of the rectum with scapular metastasis: A case
report. J Med Case Rep. 6:1452012. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Ahmad A, Libbey NP, Somasundar P and Katz
SC: Gastrointestinal stromal tumour metastatic to the epididymis.
BMJ Case Rep. 2015:bcr20152115552015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Gupta S, Bi WL and Dunn IF: Metastatic
gastrointestinal stromal tumor to the skull. World Neurosurg.
89:725.e11–e16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Savvidou OD, Chloros GD, Agrogiannis GD,
Korkolopoulou P, Panagopoulos GN and Papagelopoulos PJ: Skeletal
muscle metastasis of a GIST: A case report and review of the
literature. Case Rep Surg. 2016:78675452016.PubMed/NCBI
|
|
80
|
Saraireh H, Tayyem O, Al Asad O, Nawgiri R
and Alawin I: A rare case of a metastatic gastrointestinal stromal
tumor (GIST): A case report and review of the literature. J
Gastrointest Cancer. 50:926–934. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Kong Y, Ma XW, Zhang QQ, Zhao Y and Feng
HL: Gastrointestinal stromal tumor with multisegmental spinal
metastases as first presentation: A case report and review of the
literature. World J Clin Cases. 9:1490–1498. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Mikuni M, Wakuta M, Masaki T, Hirose Y,
Takasu H, Kawano H, Aoki R, Ota M and Kimura K: Surgical resection
of intraorbital metastasis of a gastrointestinal stromal tumor
resistant to chemotherapy. Am J Ophthalmol Case Rep. 25:1013532022.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Takasaki T, Tsuji T and Nakayama S: A case
of gastrointestinal stromal tumor metastasized to the left
ventricular myocardium. Surg Case Rep. 8:762022. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Shimizu T, Murakami H, Sangsin A, Demura
S, Kato S, Shinmura K, Yokogawa N, Oku N, Kitagawa R and Tsuchiya
H: En bloc corpectomy for late gastrointestinal stromal tumor
metastasis: A case report and review of the literature. J Med Case
Rep. 12:3002018. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Akolkar S, Melitas C and Piper M: Pelvic
gastrointestinal stromal tumor with pulmonary metastasis. ACG Case
Rep J. 6:e002052019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Kaku S, Tanaka T, Ohtuka T, Seki K,
Sawauchi S, Numoto RT, Murakami S, Komine K and Abe T: Perisacral
gastrointestinal stromal tumor with intracranial metastasis. Case
report. Neurol Med Chir (Tokyo). 46:254–257. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Carvalho J, Teixeira M, Silva FT, Esteves
A, Ribeiro C and Guerra D: Esophageal gastrointestinal stromal
tumor with rare intracranial metastasis. Case Rep Gastrointest Med.
2020:88420062020.PubMed/NCBI
|
|
88
|
Xu D, Lin X and Qiu X: The epithelioid
gastrointestinal stromal tumor with pulmonary metastasis: A rare
case report and literature review. Medicine (Baltimore).
99:e193462020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
von Mehren M and Joensuu H:
Gastrointestinal stromal tumors. J Clin Oncol. 36:136–143. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Blay JY, Kang YK, Nishida T and von Mehren
M: Gastrointestinal stromal tumours. Nat Rev Dis Primers. 7:222021.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Al-Share B, Alloghbi A, Al Hallak MN,
Uddin H, Azmi A, Mohammad RM, Kim SH, Shields AF and Philip PA:
Gastrointestinal stromal tumor: A review of current and emerging
therapies. Cancer Metastasis Rev. 40:625–641. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Hamada S, Itami A, Watanabe G, Nakayama S,
Tanaka E, Hojo M, Yoshizawa A, Hirota S and Sakai Y: Intracranial
metastasis from an esophageal gastrointestinal stromal tumor.
Intern Med. 49:781–785. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
O'Halloran PJ, Hannon AM, Bartels C,
McCawley N, Agha A, Brett F, Leader M, Broe P and Javadpour M:
Gastrointestinal stromal tumor metastases to the pituitary: A rare
entity. Br J Neurosurg. 31:603–604. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Waterman BR, Kusnezov N, Dunn JC and Hakim
MN: Aggressive gastrointestinal stromal tumor with spinal
metastases: A case report. Mil Med. 180:e618–e621. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Prayson RA: Metastatic gastrointestinal
stromal tumor to the thoracic spine. Clin Neuropathol. 38:294–296.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Bajel A, Simpson I, Longano A, Roy S and
Richardson G: Bone marrow metastasis in gastro-intestinal stromal
tumour. Br J Haematol. 147:22009. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Acar T, Efe D, Okuş A, Öcal İ and Harman
M: A rare solid tumor of the retroperitoneum with venous extension
and lung metastasis: Extra-gastrointestinal stromal tumor. Turk J
Gastroenterol. 26:358–359. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Zhou J, Yang Z, Yang CS and Lin H:
Paraneoplastic focal segmental glomerulosclerosis associated with
gastrointestinal stromal tumor with cutaneous metastasis: A case
report. World J Clin Cases. 9:8120–8126. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Tamura Y, Tada H, Kato H, Iino K, Hayashi
K, Kawashiri MA, Takemura H and Yamagishi M: Huge metastatic
gastrointestinal stromal tumor occupying the right ventricle. Circ
J. 82:1469–1470. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Siamkouris D, Schloesser M, Yousef A and
Offers E: A rare case of gastrointestinal stromal tumor with a
liver metastasis infiltrating the inferior vena cava and extending
to the right atrium with an early recurrence after surgical
extraction. Case Rep Cardiol. 2019:26234032019.PubMed/NCBI
|
|
101
|
Roelofs KA, Medlicott S, Henning JW and
Weis E: Gastrointestinal stromal tumor metastasis to the orbit.
Ophthalmic Plast Reconstr Surg. 34:e131–e133. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Gupta N, Mittal S, Lal N, Misra R, Kumar L
and Bhalla S: A rare case of primary mesenteric gastrointestinal
stromal tumor with metastasis to the cervix uteri. World J Surg
Oncol. 5:1372007. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Xu L, Zhang M and Xu M: Primary hepatic
gastrointestinal stromal tumor with right adrenal gland invasion: A
case report and systematic literature review. Medicine (Baltimore).
98:e154822019. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Prablek M, Srinivasan VM, Srivatsan A,
Holdener S, Oneissi M, Heck KA, Jalali A, Mandel J, Viswanathan A
and Patel AJ: Gastrointestinal stromal tumor with intracranial
metastasis: Case presentation and systematic review of literature.
BMC Cancer. 19:11192019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Hirota S: Differential diagnosis of
gastrointestinal stromal tumor by histopathology and
immunohistochemistry. Transl Gastroenterol Hepatol. 3:272018.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Fletcher CD, Berman JJ, Corless C,
Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti
H, Rubin BP, et al: Diagnosis of gastrointestinal stromal tumors: A
consensus approach. Hum Pathol. 33:459–465. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Foo WC, Liegl-Atzwanger B and Lazar AJ:
Pathology of gastrointestinal stromal tumors. Clin Med Insights
Pathol. 5:23–33. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Kubo N and Takeuchi N: Gastrointestinal
stromal tumor of the stomach with axillary lymph node metastasis: A
case report. World J Gastroenterol. 23:1720–1724. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Brundridge WL, Heymann HB, Spengler A,
DeBacker CM and Holck DEE: Gastrointestinal stromal tumor
metastatic to the orbit. Orbit. 41:637–641. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Ogawa S, Nishihara M, Nakanishi T, Maeda T
and Hirota S: A rare case of extraluminally pedunculated
gastrointestinal stromal tumor with postoperative metastasis to
pancreas. J Surg Case Rep. 2021:rjab4222021. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Yin XN, Yin Y, Wang J, Shen CY, Chen X,
Zhao Z, Cai ZL and Zhang B: Gastrointestinal stromal tumor
metastasis at the site of a totally implantable venous access port
insertion: A rare case report. World J Clin Cases. 8:5007–5012.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Yamaguchi T, Kinoshita J, Saito H, Shimada
M, Terai S, Moriyama H, Okamoto K, Nakamura K, Tajima H, Ninomiya
I, et al: Gastrointestinal stromal tumor metastasis to the ovary: A
case report. SAGE Open Med Case Rep.
9:2050313X2110125112021.PubMed/NCBI
|
|
113
|
Pantuso G, Macaione I, Taverna A, Guercio
G, Incorvaia L, Di Piazza M, Di Grado F, Cilluffo G, Badalamenti G
and Cipolla C: Surgical treatment of primary gastrointestinal
stromal tumors (GISTs): Management and prognostic role of R1
resections. Am J Surg. 220:359–364. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Senchak J, Ahr K and von Mehren M:
Gastrointestinal stromal tumors: What is the best sequence of TKIs?
Curr Treat Options Oncol. 23:749–761. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Demetri GD, von Mehren M, Blanke CD, Van
den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA,
Singer S, Janicek M, et al: Efficacy and safety of imatinib
mesylate in advanced gastrointestinal stromal tumors. N Engl J Med.
347:472–480. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Tang S, Yin Y, Shen C, Chen J, Yin X,
Zhang B, Yao Y, Yang J and Chen Z: Preoperative imatinib mesylate
(IM) for huge gastrointestinal stromal tumors (GIST). World J Surg
Oncol. 15:792017. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Wang SY, Wu CE, Lai CC, Chen JS, Tsai CY,
Cheng CT, Yeh TS and Yeh CN: Prospective evaluation of neoadjuvant
imatinib use in locally advanced gastrointestinal stromal tumors:
Emphasis on the optimal duration of neoadjuvant imatinib use,
safety, and oncological outcome. Cancers (Basel). 11:4242019.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Zhang C, Zhang C, Zhang T, Liu H, Zhong J,
Wang Z, Wang L and Hong L: Second-line sunitinib for Chinese
patients with advanced gastrointestinal stromal tumor: 37.5 mg
schedule outperformed 50 mg schedule in adherence and prognosis.
Transl Cancer Res. 10:3206–3217. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Petzer AL, Gunsilius E, Hayes M,
Stockhammer G, Duba HC, Schneller F, Grünewald K, Poewe W and Gastl
G: Low concentrations of STI571 in the cerebrospinal fluid: A case
report. Br J Haematol. 117:623–625. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Wolff NC, Richardson JA, Egorin M and
Ilaria RL Jr: The CNS is a sanctuary for leukemic cells in mice
receiving imatinib mesylate for Bcr/Abl-induced leukemia. Blood.
101:5010–5013. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Zhou Q and Gallo JM: Quantification of
sunitinib in mouse plasma, brain tumor and normal brain using
liquid chromatography-electrospray ionization-tandem mass
spectrometry and pharmacokinetic application. J Pharm Biomed Anal.
51:958–964. 2010. View Article : Google Scholar : PubMed/NCBI
|