|
1
|
Dzwierzynski WW: Melanoma risk factors and
prevention. Clin Plast Surg. 48:543–550. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ahmed B, Qadir MI and Ghafoor S: Malignant
Melanoma: Skin cancer-diagnosis, prevention, and treatment. Crit
Rev Eukaryot Gene Expr. 30:291–297. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bruno W, Dalmasso B, Barile M, Andreotti
V, Elefanti L, Colombino M, Vanni I, Allavena E, Barbero F, Passoni
E, et al: Predictors of germline status for hereditary melanoma: 5
years of multi-gene panel testing within the Italian Melanoma
Intergroup. ESMO Open. 7:1005252022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ismail H, Helby J, Hölmich LR, H Chakera
A, Bastholt L, Klyver H, Sjøgren P, Schmidt H, Schöllhammer L,
Nordestgaard BG and Bojesen SE: Genetic predisposition to long
telomeres is associated with increased mortality after melanoma: A
study of 2101 melanoma patients from hospital clinics and the
general population. Pigment Cell Melanoma Res. 34:946–954. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Guo W, Wang H and Li C: Signal pathways of
melanoma and targeted therapy. Signal Transduct Target Ther.
6:4242021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Craig S and Virós A: New biomarkers
improve stratification of patients with melanoma. Br J Dermatol.
182:5–6. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sun L and Arbesman J: Canonical signaling
pathways in melanoma. Clin Plast Surg. 48:551–560. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Phoon YP, Tannenbaum C and Diaz-Montero
CM: Immunobiology of Melanoma. Clin Plast Surg. 48:561–576. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Skudalski L, Waldman R, Kerr PE and
Grant-Kels JM: Melanoma: An update on systemic therapies. J Am Acad
Dermatol. 86:515–524. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen C, Hou J, Tanner JJ and Cheng J:
Bioinformatics methods for mass spectrometry-based proteomics data
analysis. Int J Mol Sci. 21:28732020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fu Y, Ling Z, Arabnia H and Deng Y:
Current trend and development in bioinformatics research. BMC
Bioinformatics. 21 (Suppl 9):S5382020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
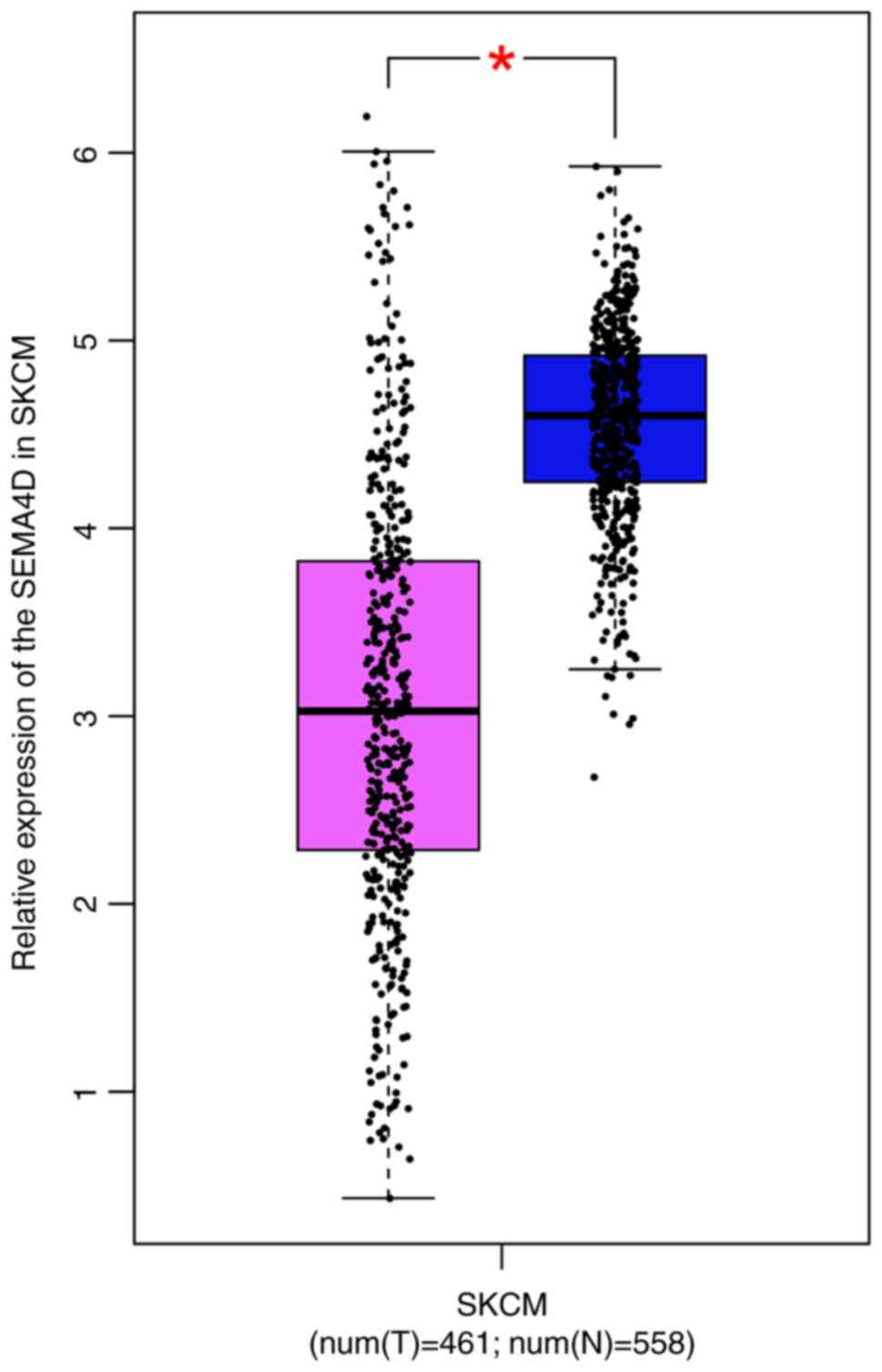
Lu Q, Cai P, Yu Y, Liu Z, Chen G and Zeng
Z: Sema4D correlates with tumour immune infiltration and is a
prognostic biomarker in bladder cancer, renal clear cell carcinoma,
melanoma and thymoma. Autoimmunity. 54:294–302. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang X, Jian W, Luo Q and Fang L:
CircSEMA4B inhibits the progression of breast cancer by encoding a
novel protein SEMA4B-211aa and regulating AKT phosphorylation. Cell
Death Dis. 13:7942022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hughes AJ and Herr AE: Microfluidic
Western blotting. Proc Natl Acad Sci USA. 109:21450–21455. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Castañeda-Reyes ED, Perea-Flores MJ,
Davila-Ortiz G, Lee Y and Gonzalez de Mejia E: Development,
characterization and use of liposomes as amphipathic transporters
of bioactive compounds for melanoma treatment and reduction of skin
inflammation: A review. Int J Nanomedicine. 15:7627–7650. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pereira J, Bessa C, Matos P and Jordan P:
Pro-Inflammatory cytokines trigger the overexpression of
tumour-related splice variant RAC1B in polarized colorectal cells.
Cancers (Basel). 14:13932022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ohno F, Nakahara T, Kido-Nakahara M, Ito
T, Nunomura S, Izuhara K and Furue M: Periostin links skin
inflammation to melanoma progression in humans and mice. Int J Mol
Sci. 20:1692019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rossi N, Lee KA, Bermudez MV, Visconti A,
Thomas AM, Bolte LA, Björk JR, de Ruijter LK, Newton-Bishop J,
Harland M, et al: Circulating inflammatory proteins associate with
response to immune checkpoint inhibition therapy in patients with
advanced melanoma. EBioMedicine. 83:1042352022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen Y, Zhang Y, Chen S, Liu W, Lin Y,
Zhang H and Yu F: Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
sensitize melanoma cells to MEK inhibition and inhibit metastasis
and relapse by inducing degradation of AXL. Pigment Cell Melanoma
Res. 35:238–251. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Karlsson MJ, Costa Svedman F, Tebani A,
Kotol D, Höiom V, Fagerberg L, Edfors F, Uhlén M, Egyhazi Brage S
and Maddalo G: Inflammation and apolipoproteins are potential
biomarkers for stratification of cutaneous melanoma patients for
immunotherapy and targeted therapy. Cancer Res. 81:2545–2555. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kalaora S, Nagler A, Wargo JA and Samuels
Y: Mechanisms of immune activation and regulation: Lessons from
melanoma. Nat Rev Cancer. 22:195–207. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang H, Chen Z, Zhang A, Gupte AA and
Hamilton DJ: The role of calcium signaling in melanoma. Int J Mol
Sci. 23:10102022. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rajabinejad M, Asadi G, Ranjbar S, Afshar
Hezarkhani L, Salari F, Gorgin Karaji A and Rezaiemanesh A:
Semaphorin 4A, 4C, and 4D: Function comparison in the autoimmunity,
allergy, and cancer. Gene. 746:1446372020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xie J, Wang Z and Wang W: Semaphorin 4D
induces an imbalance of Th17/Treg cells by activating the Aryl
hydrocarbon receptor in ankylosing spondylitis. Front Immunol.
11:21512020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu Y, Zhang WS, Tang ZH, Ye DD, Su S,
Zhang SM and Qiu J: Anti-inflammatory effects of the immobilization
of SEMA4D on titanium surfaces in an endothelial cell/macrophage
indirect coculture model. Biomed Mater. 17:0150052021. View Article : Google Scholar
|
|
26
|
Younis RH, Ghita I, Elnaggar M,
Chaisuparat R, Theofilou VI, Dyalram D, Ord RA, Davila E, Tallon
LJ, Papadimitriou JC, et al: Soluble Sema4D in plasma of head and
neck squamous cell carcinoma patients is associated with underlying
non-inflamed tumor profile. Front Immunol. 12:5966462021.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Maleki KT, Cornillet M and Björkström NK:
Soluble SEMA4D/CD100: A novel immunoregulator in infectious and
inflammatory diseases. Clin Immunol. 163:52–59. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chapoval SP, Vadasz Z, Chapoval AI and
Toubi E: Semaphorins 4A and 4D in chronic inflammatory diseases.
Inflamm Res. 66:111–117. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Willner N, Goldberg Y, Schiff E and Vadasz
Z: Semaphorin 4D levels in heart failure patients: A potential
novel biomarker of acute heart failure. ESC Heart Fail. 5:603–609.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Movila A, Mawardi H, Nishimura K, Kiyama
T, Egashira K, Kim JY, Villa A, Sasaki H, Woo SB and Kawai T:
Possible pathogenic engagement of soluble Semaphorin 4D produced by
γδT cells in medication-related osteonecrosis of the jaw (MRONJ).
Biochem Biophys Res Commun. 480:42–47. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yu Y, Zhou Y, Di C, Zhao C, Chen J, Su W,
Wu Q, Wu M, Su X and Xia Z: Increased airway epithelial
cell-derived exosomes activate macrophage-mediated allergic
inflammation via CD100 shedding. J Cell Mol Med. 25:8850–8862.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wu JH, Li YN, Chen AQ, Hong CD, Zhang CL,
Wang HL, Zhou YF, Li PC, Wang Y, Mao L, et al: Inhibition of
Sema4D/PlexinB1 signaling alleviates vascular dysfunction in
diabetic retinopathy. EMBO Mol Med. 12:e101542020. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lontos K, Adamik J, Tsagianni A, Galson
DL, Chirgwin JM and Suvannasankha A: The role of semaphorin 4D in
bone remodeling and cancer metastasis. Front Endocrinol (Lausanne).
9:3222018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Nishide M and Kumanogoh A: The role of
semaphorins in immune responses and autoimmune rheumatic diseases.
Nat Rev Rheumatol. 14:19–31. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lu JJ, Su YW, Wang CJ, Li DF and Zhou L:
Semaphorin 4D promotes the proliferation and metastasis of bladder
cancer by activating the PI3K/AKT pathway. Tumori. 105:231–242.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Nagarsheth N, Wicha MS and Zou W:
Chemokines in the cancer microenvironment and their relevance in
cancer immunotherapy. Nat Rev Immunol. 17:559–572. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Singh N, Baby D, Rajguru JP, Patil PB,
Thakkannavar SS and Pujari VB: Inflammation and cancer. Ann Afr
Med. 18:121–126. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Schmitt M and Greten FR: The inflammatory
pathogenesis of colorectal cancer. Nat Rev Immunol. 21:653–667.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Iyengar NM, Gucalp A, Dannenberg AJ and
Hudis CA: Obesity and cancer mechanisms: Tumor microenvironment and
inflammation. J Clin Oncol. 34:4270–4276. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Landskron G, De la Fuente M, Thuwajit P,
Thuwajit C and Hermoso MA: Chronic inflammation and cytokines in
the tumor microenvironment. J Immunol Res. 2014:1491852014.
View Article : Google Scholar : PubMed/NCBI
|