Introduction
Primary lymphomas of the uterine cervix are rare,
accounting for 0.5-1% of all extranodal Non-Hodgkin's Lymphomas
(NHL) (1). Even less common are
primary cervical lymphomas of the follicular subtype, comprising
8.5% of all primary cervical NHLs (2). The most common presenting symptom is
abnormal vaginal bleeding (2,3). Due
to the rarity of the disease, it can be confused with other
malignancies, such as squamous cell carcinoma or inflammatory
processes. There is no established therapeutic protocol. Thus,
different approaches, including surgery, radiotherapy and
chemotherapy (either alone or in combination), are often employed
(3). Herein, we present a rare case
of primary cervical follicular lymphoma that was managed
surgically.
Case report
The patient was a 54-year-old, gravida 1 para 1,
postmenopausal woman, who presented for her annual gynecological
check-up without any symptoms. The patient had a history of
rheumatoid arthritis, Crohn's disease, primary biliary cirrhosis,
pulmonary fibrosis, nodular goiter and hemophilia (Factor XI=41%)
and was being treated with methotrexate, ursodeoxycholic acid, and
levothyroxine. During a routine Papanicolaou smear test, cytology
revealed numerous dysplastic cells with possible koilocytic atypia
and dyskeratosis, characterized initially as Cervical
Intraepithelial Neoplasia (CIN) I–II owing to human papillomavirus
(HPV) infection. Transvaginal ultrasonography (TVUS) showed a
thickened, barrel-shaped cervix with a diameter of 2 cm and
widespread hyperechogenicity. The patient subsequently underwent
colposcopy, during which significant vaginal atrophy and stenosis
along with a friable ectocervical mucosa was noted (Fig. 1).
The patient was admitted to the Second Department of
Obstetrics and Gynecology at Aretaieio University Hospital (Athens,
Greece) in February 2020. A wide surgical biopsy was performed and
the histopathological results were consistent with the diagnosis of
non-Hodgkin B-cell follicular lymphoma (Grade 1/2). Under
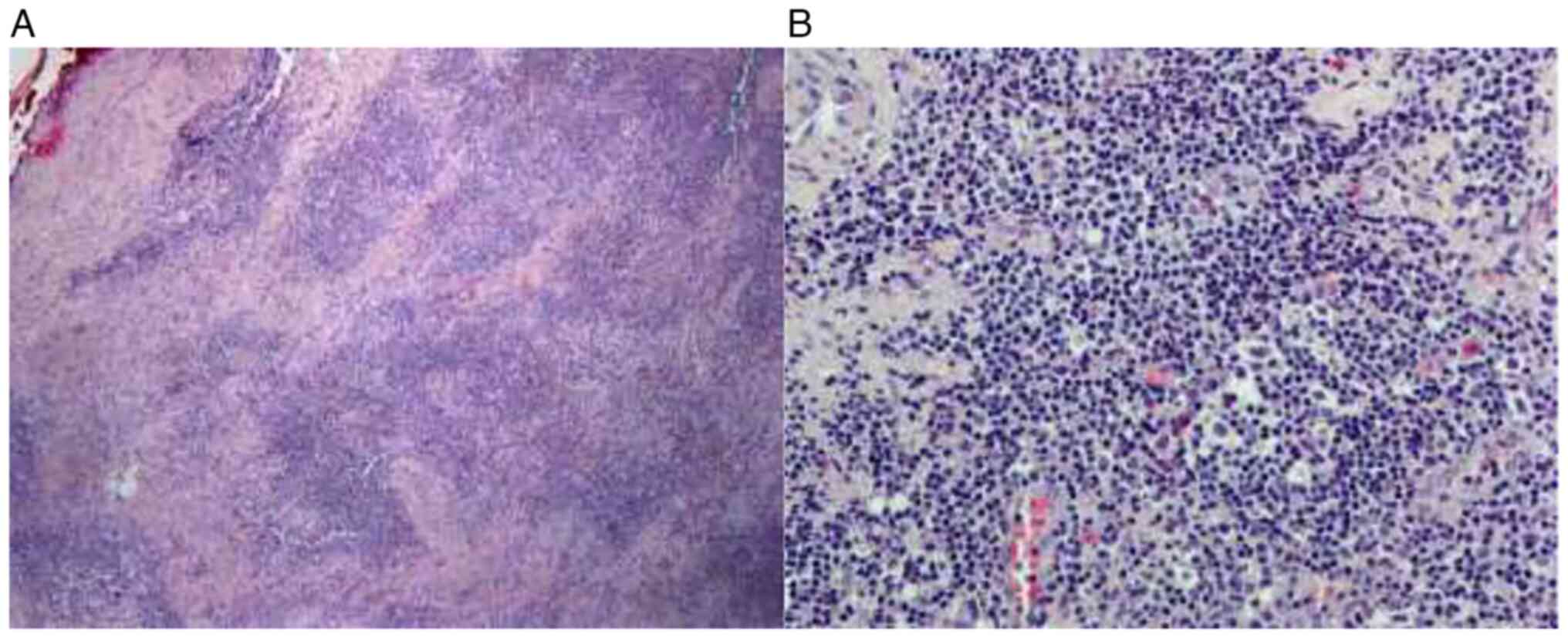
microscopical examination, the normal architecture of the lymph
node was effaced due to the presence of multiple nodular formations
(Fig. 2) mimicking secondary
follicles with expanded ‘follicle-centers’, but with loss of
polarity, absence of macrophages and therefore loss of the
‘starry-sky’ pattern which characterizes normal follicles. The
cellular composition of the nodules included centrocytes and
scattered centroblasts (the latter not exceeding 6 per ten high
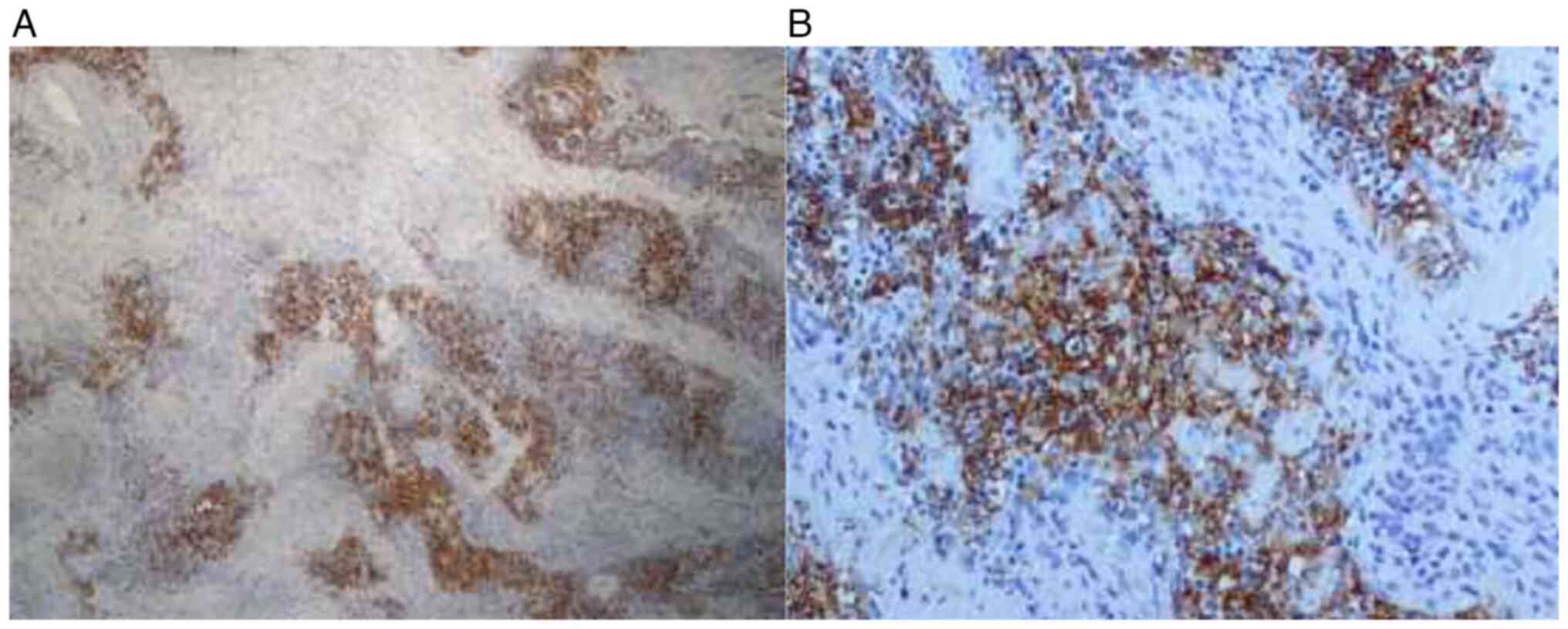
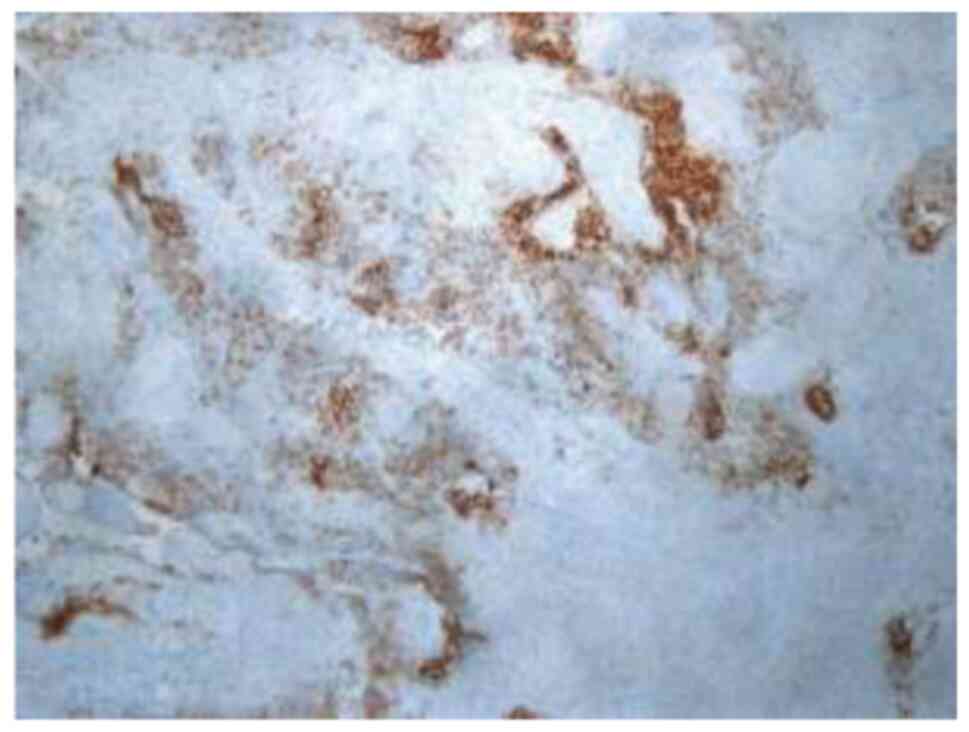
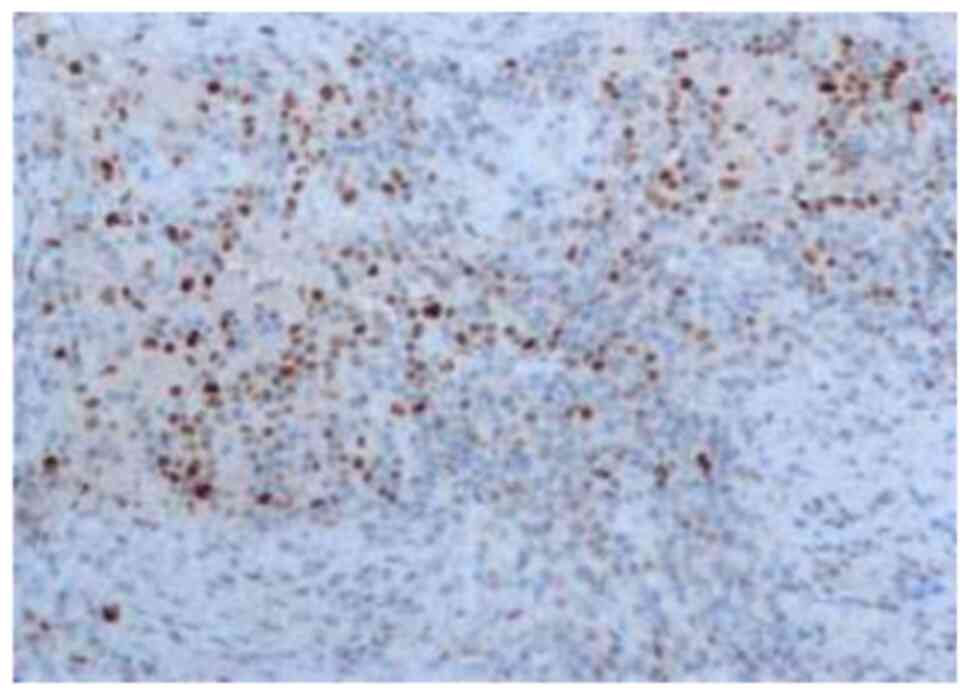
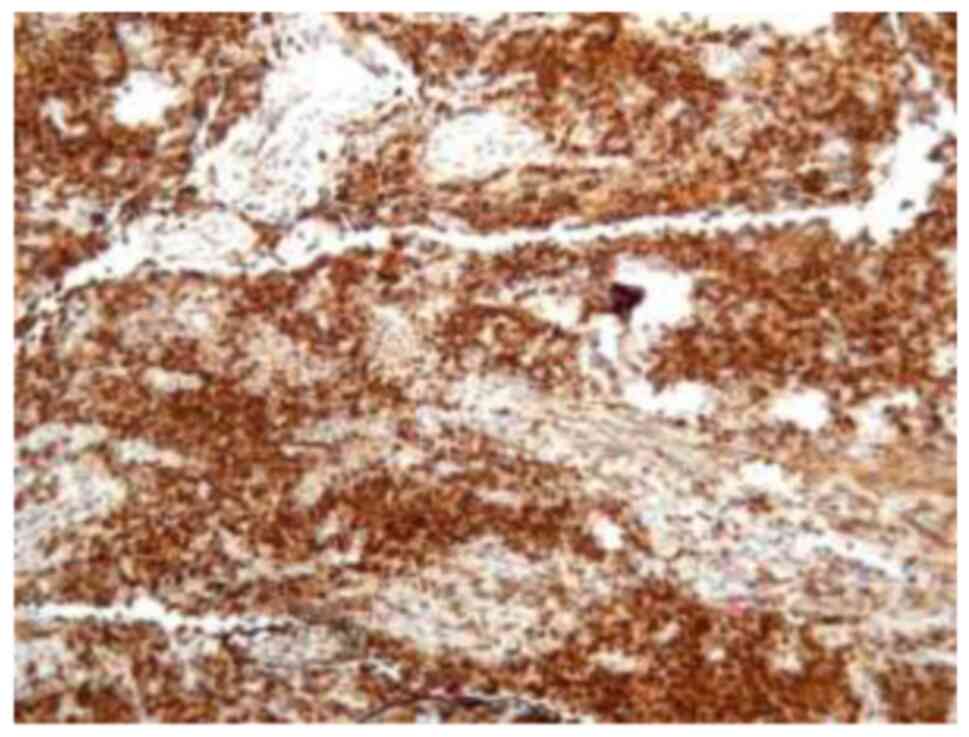
power fields), with an immunophenotype: CD20+ (Fig. 3), CD23+ (Fig. 4), bcl-6+ (Fig. 5), bcl-2+ (Fig. 6), CD5-, Cyclin D1-. Notably cells
with similar morphologic and immunophenotyping features were found
outside the nodules, either singly or in aggregates. The Ki67
labeling index was 15% (Fig. 7),
allowing for the diagnosis of classical follicular lymphoma
(according to the new, 2022, 5th edition of the World Health
Organization Classification of Haematolymphoid Tumours). The
resection margins were positive. A computed tomography scan of the
thorax and the abdominal cavity showed no lymphadenopathy or
hepatosplenomegaly and the patient was staged as Ann Arbor IEA. The
patient was evaluated by a hematologist who suggested treatment
with rituximab. However, due to intolerable side effects, the
treatment was discontinued and the patient was scheduled for
cervical conization under general anesthesia. The resection margins
of the specimen were negative and no further treatment took place.
After 2 years of close follow-up monitoring, the patient has no
evidence of disease.
Discussion
Follicular lymphoma is the second most common type
of primary female genital tract non-Hodgkin lymphoma, after diffuse
large-B-cell lymphoma (4,5), which according to the new, 5th edition
of the World Health Organization Classification of Haematolymphoid
Tumours is no longer mandatory for classification purposes
(6). The diagnostic algorithm
encompasses architecture, morphology/cellular composition, and
immunophenotypic features of the neoplastic B-lymphocytes such as
expression of CD10, BCL-2 and BCL-6 (7), while molecular techniques which detect
the t (14;18) translocation involving the IgH/bcl-2 genes are not
required for the diagnosis and are used only in equivocal cases.
Detectable monoclonal immunoglobulin expression by the neoplastic
cells is not a regular feature of follicular lymphoma (in contrast
with marginal zone lymphoma), although is sometimes described in
rare cases, posing for differential diagnosis with marginal zone
derivation lymphomas.
Clinical manifestations of primary cervical
lymphomas are abnormal vaginal bleeding, abdominal/pelvic
discomfort, dyspareunia, vaginal discharge and less often, back
pain (3). The definitive diagnosis
of cervical non-Hodgkin lymphoma is not possible using Pap smear
testing alone, as the tumor originates in the stroma, often leaving
the overlying squamous epithelium unaffected (8). Nonetheless, the disease can coexist
with cytological abnormalities. Cervical biopsy and
immunophenotyping is necessary to distinguish primary NHLs of the
uterine cervix from other malignant and inflammatory diseases.
For the staging of cervical lymphomas, both the Ann
Arbor system and the International Federation of Gynecology and
Obstetrics (FIGO) system have been used, with few studies claiming
superior sensitivity of the Ann Arbor system (9). For the assessment of patient
prognosis, the Follicular Lymphoma International Prognostic Index
(FLIPI) can be utilized. Taking into account five ‘poor’ prognostic
factors, namely: age >60 years, hemoglobin <12 g/dl, serum
lactate dehydrogenase (LDH) higher than normal, Ann Arbor stage
III/IV and number of involved nodal areas >4, the risk of death
can be estimated. Having 0–1 risk factors places a patient at ‘low’
risk, 2–3 risk factors at ‘intermediate’ risk and 4–5 at ‘high’
risk (10). Our patient, having had
no risk factors, was considered to be of low risk.
There is no established protocol for the treatment
of primary cervical non-Hodgkin lymphomas. Treatment options
include chemotherapy, radiotherapy and surgery, either alone or in
combination, while for recurrent disease, immunotherapy and stem
cell transplantation can also be employed (11). For early-stage follicular lymphoma
patients, watchful waiting can be an acceptable approach without
deleterious effects on the patients' overall survival (12). Regardless, most patients receive
CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and
prednisone) with or without rituximab (13). Rituximab, an anti-CD20 monoclonal
antibody, can be used in the CD20(+) primary lymphomas of the
cervix, either combined with chemotherapy or as monotherapy, with
significant response rates and a relatively favorable side effect
profile (14). Since the
introduction of rituximab, the overall survival of patients with
follicular lymphoma has improved drastically (15). For localized pelvic disease,
radiotherapy alone can be employed due to high response rates and
low morbidity (13). In some cases
of cervical lymphomas, surgery can be an acceptable and effective
approach (3,7).
In conclusion, primary cervical follicular lymphoma
is a rare malignancy, without an established therapeutic protocol.
Surgery, chemotherapy and radiotherapy, either alone or in
combination, have been proposed as possible therapeutical options.
In the case of our patient, the disease was limited to the uterine
cervix without regional expansion or metastasis. The patient was
managed primarily by surgery and 2 years later remains without
evidence of disease recurrence. Although quite rare, clinicians and
pathologists should consider lymphomas of the female genital tract
as a possible diagnosis, when dealing with pathologies of the
female genital tract. By avoiding misdiagnosis, they can provide
the patient with the best possible therapeutic interventions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TP and AM were involved in project development, data
collection and management, data analysis and manuscript writing.
PC, CK and NV were involved in project development, data collection
and management, data analysis and manuscript editing. OS and LM
reviewed and prepared the case's histopathological reports. AM and
CK confirm the authenticity of all the raw data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
participation.
Patient consent for publication
The patient provided written informed consent for
the publication of all relevant data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
NHL
|
non-Hodgkin lymphoma
|
|
CIN
|
cervical intraepithelial neoplasia
|
|
TVUS
|
transvaginal ultrasound
|
|
FLIPI
|
Follicular Lymphoma International
Prognostic Index
|
|
HPV
|
human papillomavirus
|
|
LDH
|
lactate dehydrogenase
|
References
|
1
|
Freeman C, Berg JW and Cutler SJ:
Occurrence and prognosis of extranodal lymphomas. Cancer.
29:252–260. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Korcum AF, Karadogan I, Aksu G, Aralasmak
A and Erdogan G: Primary follicular lymphoma of the cervix uteri: A
review. Ann Hematol. 86:623–630. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Perren T, Farrant M, McCarthy K, Harper P
and Wiltshaw E: Lymphomas of the cervix and upper vagina: A report
of five cases and a review of the literature. Gynecol Oncol.
44:87–95. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kosari F, Daneshbod Y, Parwaresch R, Krams
M and Wacker HH: Lymphomas of the female genital tract: A study of
186 cases and review of the literature. Am J Surg Pathol.
29:1512–1520. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Swerdlow SH, Campo E, Pileri SA, Harris
NL, Stein H, Siebert R, Advani R, Ghielmini M, Salles GA, Zelenetz
AD and Jaffe ES: The 2016 revision of the World Health Organization
classification of lymphoid neoplasms. Blood. 127:2375–2390. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Polyatskin IL, Artemyeva AS and Krivolapov
YA: Revised WHO classification of tumors of hematopoietic and
lymphoid tissues, 2017 (4th edition): lymphoid tumors. Arkh Patol.
81:59–65. 2019.(In Russian). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Freedman A and Jacobsen E: Follicular
lymphoma: 2020 Update on diagnosis and management. Am J Hematol.
95:316–327. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dursun P, Gultekin M, Bozdag G, Usubutun
A, Uner A, Celik NY, Yuce K and Ayhan A: Primary cervical lymphoma:
Report of two cases and review of the literature. Gynecol Oncol.
98:484–489. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lagoo AS and Robboy SJ: Lymphoma of the
female genital tract: Current status. Int J Gynecol Pathol.
25:1–21. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Solal-Céligny P, Roy P, Colombat P, White
J, Armitage JO, Arranz-Saez R, Au WY, Bellei M, Brice P, Caballero
D, et al: Follicular lymphoma international prognostic index.
Blood. 104:1258–1265. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mann R, Roberts WS, Gunasakeran S and
Tralins A: Primary lymphoma of the uterine cervix. Gynecol Oncol.
26:127–134. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Advani R, Rosenberg SA and Horning SJ:
Stage I and II follicular non-Hodgkin's lymphoma: Long-term
follow-up of no initial therapy. J Clin Oncol. 22:1454–1459. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hilal Z, Hartmann F, Dogan A, Cetin C,
Krentel H, Schiermeier S, Schultheis B and Tempfer CB: Lymphoma of
the cervix: Case report and review of the literature. Anticancer
Res. 36:4931–4940. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ardeshna KM, Qian W, Smith P, Braganca N,
Lowry L, Patrick P, Warden J, Stevens L, Pocock CF, Miall F, et al:
Rituximab versus a watch-and-wait approach in patients with
advanced-stage, asymptomatic, non-bulky follicular lymphoma: An
open-label randomised phase 3 trial. Lancet Oncol. 15:424–435.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Junlén HR, Peterson S, Kimby E, Lockmer S,
Lindén O, Nilsson-Ehle H, Erlanson M, Hagberg H, Rådlund A, Hagberg
O and Wahlin BE: Follicular lymphoma in Sweden: Nationwide improved
survival in the rituximab era, particularly in elderly women: A
Swedish lymphoma registry study. Leukemia. 29:668–676. 2015.
View Article : Google Scholar : PubMed/NCBI
|