Introduction
In pancreatic cancer, pancreatic undifferentiated
carcinoma is a rare subtype, and in previous studies, the rate of
pancreatic undifferentiated carcinoma varied between reported
series from 0.1 to 0.7% (1,2), with an age-adjusted prevalence of
0.027/100000 persons (3). It has
been divided into two categories based on the last WHO
Classification: osteoclast-like giant cell carcinoma and
pleomorphic giant cell carcinoma (4,5).
Undifferentiated carcinoma with osteoclast-like giant cells (OGCs)
of the pancreas (UCOGCP) accounts for less than 1% of all
pancreatic malignancies, which is an aggressive malignant variant
of pancreatic ductal adenocarcinoma and commonly encountered in
middle-aged and elderly males (6–8). In
contrast to pancreatic tumors without OGCs, UCOGCP can grow to a
larger size and be accompanied by polypoid growth or cystic lesion
(5); thus, it is frequently
diagnosed at an advanced stage, which prevents effective resection.
It is for this reason that the prognosis of the UCOGCP was
initially thought worse than that of invasive ductal carcinoma
(9). The initial clinical symptoms
of UCOGCP are often atypical, making an accurate early diagnosis
difficult and easily misdiagnosed. Early detection of the tumor is
important for the improvement of outcomes, and effective tools are
needed for this purpose, such as imaging examination, which serves
a significant role in evaluating the location and nature of the
tumor in a noninvasive manner, assisting clinicians in formulating
and adjusting treatment plans. However, the clinical and imaging
features of UCOGCP are poorly understood. Herein, we describe an
exceedingly rare case of rapidly progressive UCOGCP to summarize
the clinicopathological and radiologic features of this rare
neoplasm and, consequently, raise awareness of early diagnosis.
Case report
A 78-year-old male patient presented to our hospital
with chronic intermittent pain in the left upper abdomen for one
year and progressive aggravation for one month. The patient had
been diagnosed with pancreatitis at a local hospital 1 year ago,
and the pain symptoms were relieved after medical treatment. One
month prior, he presented with marked left upper abdominal pain
that increased while standing upright or walking. The patient had
no history of trauma, high blood pressure, or diabetes, nor did he
have a family history of pancreatic cancer. Physical examination
revealed that his heart rate, body temperature and blood pressure
were 87 bpm, 36.2°C, and 140/80 mmHg, respectively. The abdomen was
soft and had left upper abdominal tenderness without abdominal
muscle tension or rebound tenderness. Laboratory tests showed the
following levels (reference range for normal): carbohydrate antigen
199 (CA199), serum amylase, and serum potassium levels were 1968
U/ml (0–37 U/ml), 332 U/L (35–135 U/L), and 3.1 mmol/l (3.5–5.5
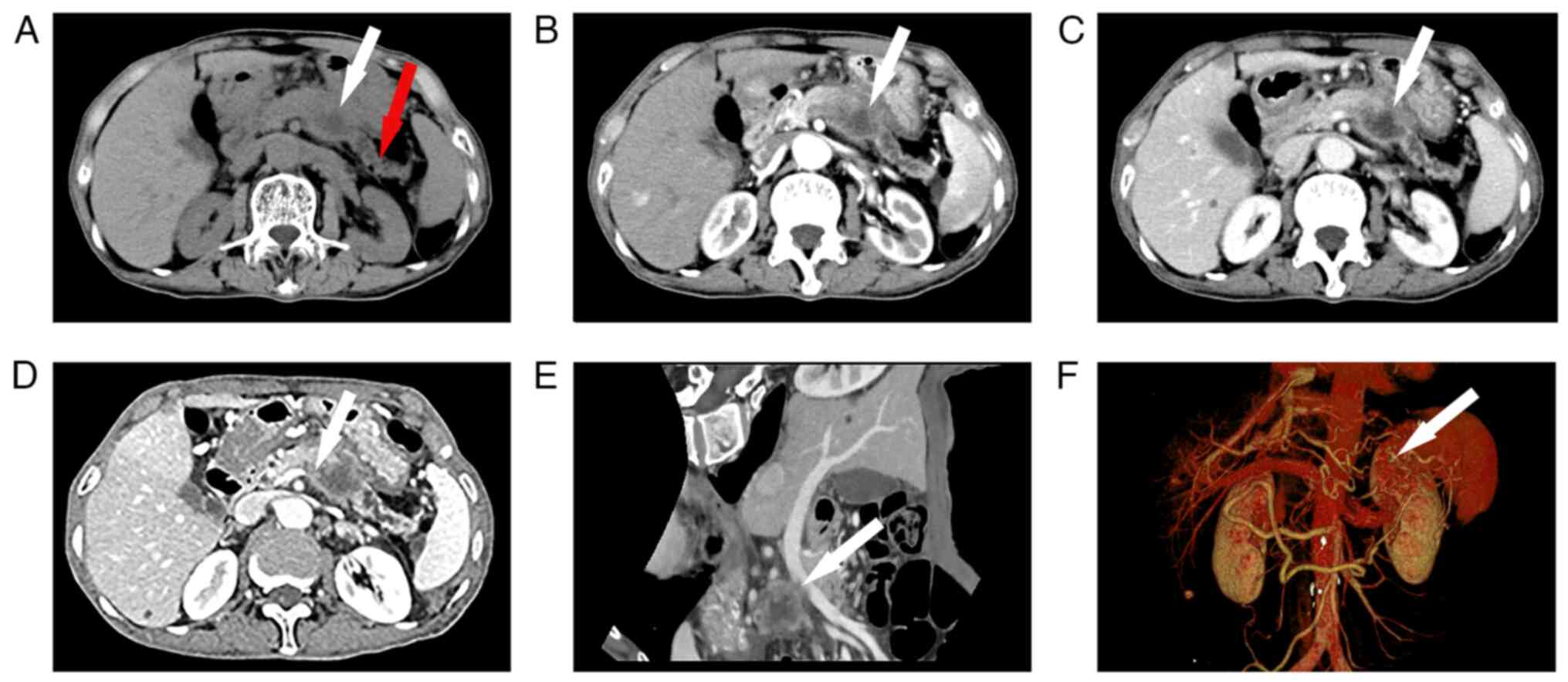
mmol/l), respectively. Abdominal computed tomography (CT) revealed
an irregular mass located in the pancreatic body and tail with no
clear boundary, pancreatic body and tail atrophy, and the
pancreatic duct dilation significantly. CT enhancement scan showed
a central region with non-enhancement low-density but enhancement
of the surrounding region of the tumor (Fig. 1A-C). On CT angiography, the
structure of the splenic vein was not clearly displayed, and portal
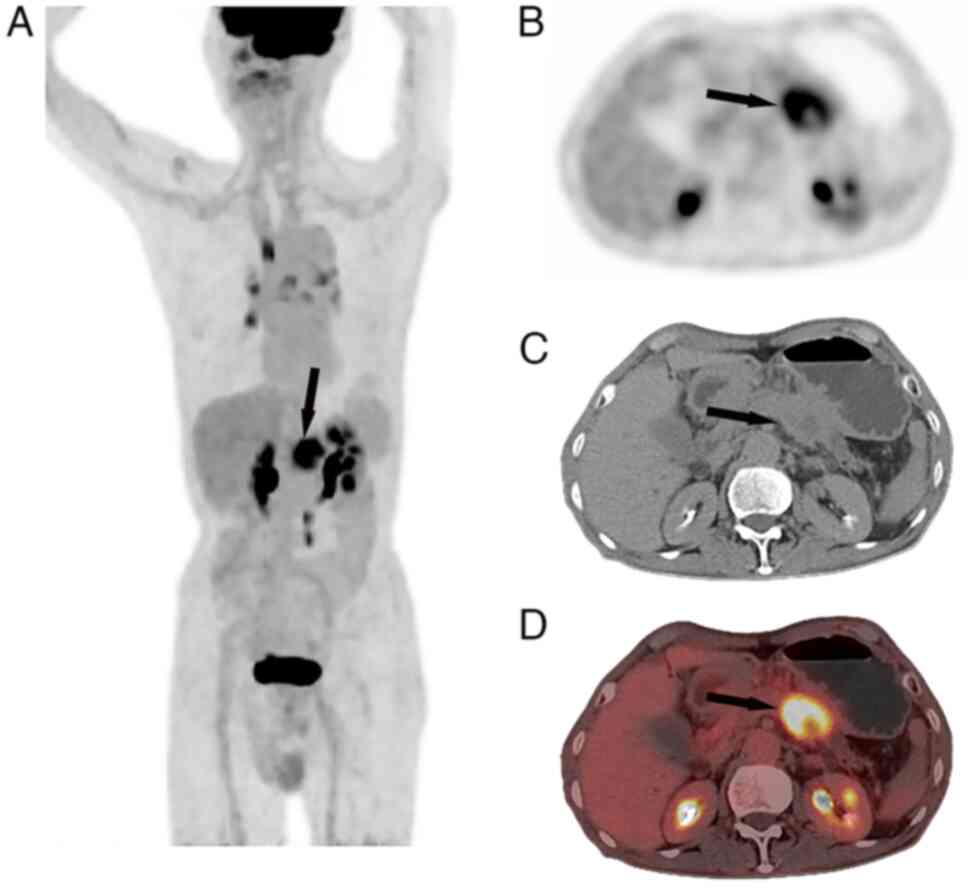
vein stenosis with portal hypertension (Fig. 1D-F). 18F-FDG (F-18-deoxyglucose)
positron emission tomography (PET)/CT revealed a semisolid (cystic
with solid fractions) mass measuring 4.5×3.5 cm on CT images with a
maximum standardized uptake value of 7.9 in the pancreatic body
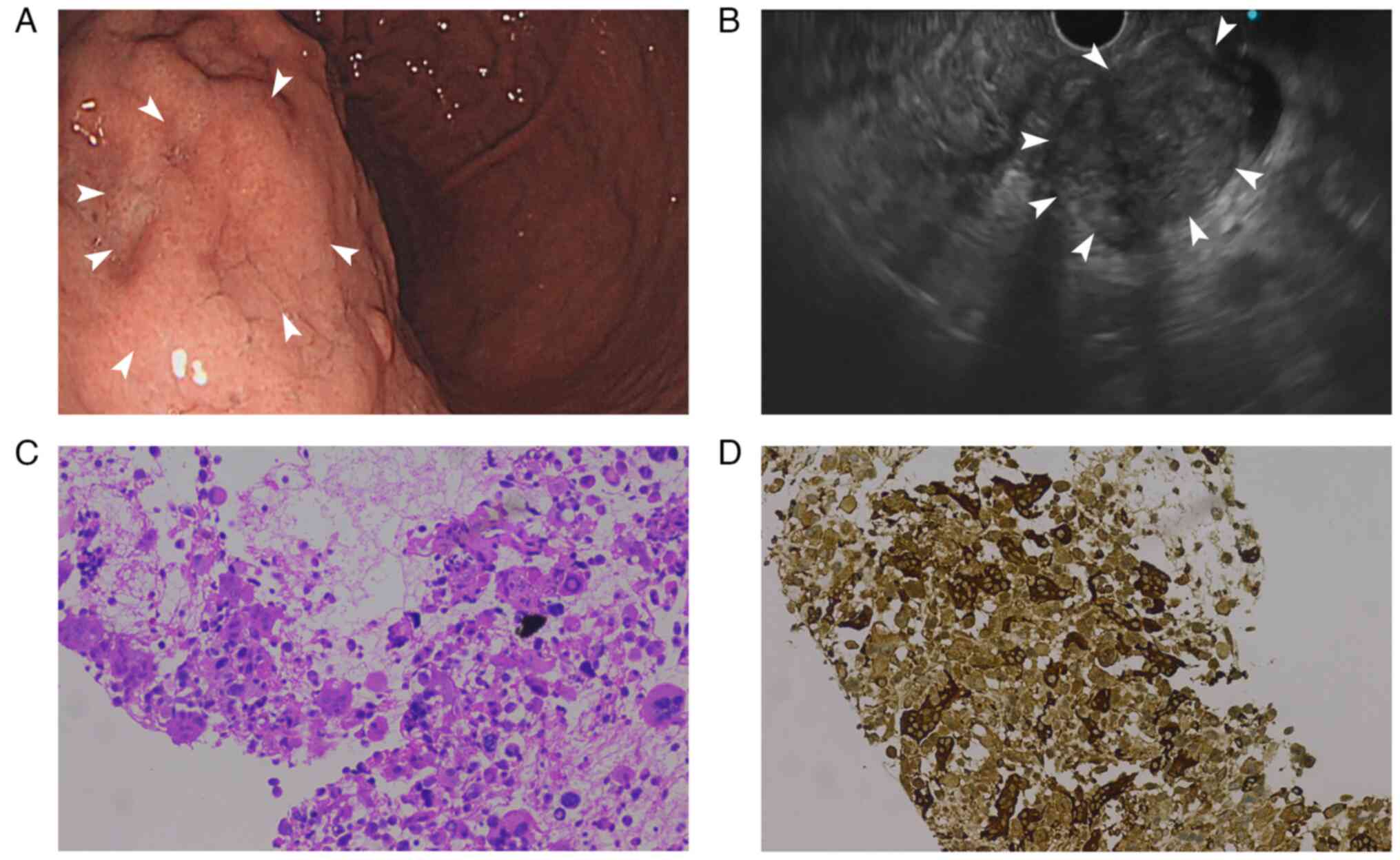
(Fig. 2). Endoscopic
ultrasonography (EUS) showed that the posterior wall of the upper
portion of the gastric body was raised from the surface of the
pancreas, revealing gastric varices (Fig. 3A). Ultrasonography showed an
ill-defined hypoechoic mass lesion in the pancreatic body measuring
4.5×3.5 cm (Fig. 3B). Endoscopic
ultrasound-guided tissue sampling for histological examination
confirmed the presence of highly pleomorphic neoplastic cells and
non-neoplastic osteoclast-like giant cells. Immunohistochemical
staining revealed CD68 reactivity in OGCs, and the Ki-67 labeling
index was 15% (Fig. 3C and D).
Unfortunately, at the time of diagnosis, the patient's disease had
advanced beyond the time of surgical intervention. According to the
guidelines of the Chinese Society of Clinical Oncology, patients
were treated with the following chemotherapy regimen: gemcitabine
was administered on the first day and eighth day as an intravenous
infusion over 30 min at a dose of 1200 mg, and tegafur, gimeracil,
and oteracil potassium capsules were administered continuously at a
dose of 80 mg/day orally for 14 consecutive days (3 weeks for a
treatment course). Unfortunately, despite receiving chemotherapy,
the patient showed a poor response to systemic chemotherapy because
his condition quickly worsened, and he died 6 months after hospital
discharge.
Discussion
Undifferentiated carcinoma of the pancreas (UCPs),
also known as giant cell carcinoma, pleomorphic large cell
carcinoma, or sarcomatous carcinoma, is a highly malignant tumor
with poor prognosis (10). UCPs are
arranged in two categories depending on the presence or absence of
OGCs because OGCs may have different clinical features and affect
the prognosis of patients (5).
UCOGCP is an exceedingly rare non-endocrine tumor prevalent in
elderly patients with no sex differences (11). The clinical findings are
nonspecific, including weight loss, abdominal pain, a palpable
mass, and fatigue, as they may also be present in nonmalignant
infectious or inflammatory conditions as well as other types of
cancers. Since the atypical imaging characteristics of these
pancreatic lesions, it is challenging to make preoperative
diagnosis, many cases reported in the literature were diagnosed
after surgery (11).
UCOGCP is a unique variant of pancreatic ductal
adenocarcinoma, and the histopathological and clinical features of
UCOGCP was differ from those of normal ductal adenocarcinoma
(12). Histologically, UCOGCP
comprises three main cell types: multinucleated OGCs
(non-neoplastic cells without cytologic atypia), mononuclear cells,
and rapidly proliferating tumor cells. OGCs are mainly found in
regions adjacent to hemorrhage or necrosis, and the existence of
OGCs is the representative histological feature of UCOGCP. However,
the origin of OGCs is controversial, and some cytological studies
have shown that OGCs are of epithelial origin, suggesting that they
may be involved in a metaplastic process (5). Immunohistochemically, it has been
reported that some tumor cells in UCOGCP express vimentin, keratin,
and p53-positive, while OGCs in UCOGCP were positive for vimentin
and expression of CD68 but negative for keratin and p53 (10). The clinical findings can be
summarized as follows: (I) there are no specific clinical symptoms,
common symptoms include abdominal pain, weight loss, and fatigue,
and gastrointestinal symptoms and jaundice have been reported
occasionally; (II) the vast majority of reported cases showed
masses larger than 3 cm, which suggests that the tumor tends to
grow rapidly and cause hemorrhage, necrosis, or cystic
degeneration; (III) the average age of onset is 60–70 years
(8,13); (IV) UCOGCP can occur in any part of
the pancreas but they are slightly more common in the tail and
body. Among the serum tumor biomarkers, serum levels of CA199 were
significantly increased in our case, which is different from those
previously reported (8), suggesting
that the specificity of preoperative CA199 may not be high and it
is very limited in helping clinical diagnosis.
Imaging examinations, including CT, magnetic
resonance imaging (MRI), EUS, and PET/CT, are essential and helpful
for determining the correct preoperative diagnosis, and they assist
in the development or modification of treatment strategies.
However, there are currently very few reports on imaging findings
of UCOGCP. In non-contrast CT scans, according to the components of
the mass, UCOGCP appeared as solid, cystic-based, or mixed
cystic-solid lesions with relatively clear margins, but it can also
invade neighboring tissues and organs, thereby exhibiting poorly
defined boundaries with surrounding tissues (14,15);
also, cystic changes and intratumoral hemorrhage can be seen in
larger lesions. On contrast-enhanced CT images, cystic lesions
commonly exhibit slight peripheral enhancement, and the internal
solid components of mixed cystic-solid lesions are continuously
enhanced in the arterial, portal venous, and delayed phases;
delayed enhancement style in enhanced CT scans has certain guiding
significance for the differential diagnosis of pancreatic tumors,
while a tumor manifests as cystic-solid performance,
well-circumscribed, with calcification, and contrast-enhanced thick
wall, thus, the possibility of a UCOGCP should be considered
(15,16). Three-dimensional reconstruction CT
techniques (3D CT) play an important role in assessing the spatial
location and extent of a lesion, which is crucial for the success
of a surgical procedure. In our case, using 3D CT technology, we
were able to comprehensively evaluate the condition of the patient
and the tumor progression. According to a literature review, on
MRI, UCOGCP typically exhibits hypointense on T1-weighted imaging
and T2-weighted imaging, and on diffusion-weighted imaging; a
cystic component of UCOGCP was hyperintense on T2-weighted imaging,
which played a certain role in distinguishing UCOGCP from other
tumors (17). However, other tumor
components, including hemosiderin, dense fibrosis, hyalinization,
and necrotic calcification/ossification, may alter the MRI signal
to cause difficulties in the differential diagnosis between UCOGCP
and others (18,19). EUS has become an essential tool for
clinical applications in oncology and is currently used for the
rapid diagnosis and treatment of pancreatic cancer via
ultrasound-guided needle biopsies of suspected tumors in patients
who cannot undergo surgery (20).
In addition, compared to other pancreatic malignancies, UCOGCP
tends to be larger; thus, endoscopic ultrasound-guided fine-needle
aspiration of tumors can be practical, safe, and provide high
diagnostic accuracy (21). Abnormal
metabolism is one of the most prominent characteristics of tumors,
and PET/CT is very sensitive to alterations in local metabolism,
has been widely used for diagnosis, staging, and therapeutic
response assessment in oncology, and can detect neoplasms in the
absence of marked anatomic changes. UCOGCP is often detected at an
advanced stage; therefore, the tumor volume is usually large, and
resection is not suitable. If detected in the early stages, the
chances of cure by surgical resection may increase. Based on the
literature, there have been few reports on the detection of UCOGCP
using PET/CT, and the smallest lesion visualized using PET/CT was
1.0 cm (22). Therefore, a
comprehensive consideration of the results of various imaging tests
can assist in clinical evaluation and decision-making among
validated treatment options and significantly improve patient
outcomes.
To date, there is no standard treatment regimen for
UCOGCP and the preferred treatment option is surgical resection.
However, the primary tumor lesions in these patients tend to be
relatively large, the surgical outcomes are unsatisfactory, and
predicted survival is very short. Although a few patients achieve
relatively long-term disease-free survival, the majority die
because of rapid disease progression within one year after surgery
(23,24). When surgery is not an option or the
patient rejects surgery, chemotherapy may be an option. However, as
there have not been many reports on this rare disease, there is no
standard chemotherapy program for UCOGCP, and pancreatic cancer
responds poorly to most chemotherapeutic agents (25). In our case, the patient had already
lost the opportunity for surgical removal of the tumor and was
forced to accept chemotherapy, but the prognosis is unfortunately
still not very encouraging. Thus, a more in-depth investigation of
how to improve treatment efficacy and choose the optimal treatment
for patients is required.
UCOGCP must be differentiated from several other
pancreatic tumors. Typically, pancreatic carcinomas are hypodense
masses with mild enhancement, and serum levels of CA199 are often
elevated. Solid pseudopapillary tumors of the pancreas are mostly
found in young women and are commonly located in the pancreatic
body and tail. A contrast-enhanced CT scan showed centripetal
enhancement. Pancreatic serous cystadenomas often manifest as
multilocular cystic masses with uneven walls and internal septation
thickness on imaging. Other differential diagnoses include
neuroendocrine tumors, pancreatic pseudocysts, and several other
rare tumors (16). However, owing
to the rarity and overlapping radiological features of these
pancreatic tumors, it is difficult to make an accurate differential
diagnosis.
Clinically, UCOGCP is rare and commonly found in
middle-aged and elderly populations. The clinical symptoms of
UCOGCP are not typical, and the major imaging findings of this
tumor include a large mixed cystic and solid mass in the pancreas.
Imaging examination, such as CT, PET/CT, EUS, can help to make
early diagnosis, develop individualized treatment plans and improve
the prognosis of patients with UCOGCP. However, a definitive
diagnosis should be concluded based on pathological examinations.
Since UCOGCP is commonly diagnosed and treated at an advanced
stage, surgical treatment, radiotherapy, and chemotherapy may have
difficulty achieving ideal therapeutic effects; thus, early
diagnosis and intervention are crucial for the survival of patients
with UCOGCP. In the future, studies with larger sample sizes are
required to better understand UCOGCP.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HR, GC, HL and TZ conceived and designed the study.
YH, QY, YX and JL made substantial contributions to acquisition of
data, and analysis and interpretation of data. YH and QY confirm
the authenticity of all the raw data. HR and GC drafted the
manuscript. HL and TZ critically revised the manuscript for
important intellectual content and gave final approval of the
version to be published. All authors agreed to the journal to which
the article was submitted and agreed to take responsibility for all
aspects of the work. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Affiliated Hospital of Zunyi Medical University
(ethical approval no. KLL-2022-777; Zunyi, China).
Patient consent for publication
Written informed consent was obtained from the
patient for his information to be published in this case
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Imaoka H, Ikeda M, Maehara K, Umemoto K,
Ozaka M, Kobayashi S, Terashima T, Inoue H, Sakaguchi C, Tsuji K,
et al: Risk stratification and prognostic factors in patients with
unresectable undifferentiated carcinoma of the pancreas.
Pancreatology. 21:738–745. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shiihara M, Higuchi R, Izumo W, Furukawa T
and Yamamoto M: A comparison of the pathological types of
undifferentiated carcinoma of the pancreas. Pancreas. 49:230–235.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Clark CJ, Graham RP, Arun JS, Harmsen WS
and Reid-Lombardo KM: Clinical outcomes for anaplastic pancreatic
cancer: A population-based study. J Am Coll Surg. 215:627–634.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang X, Miao J, Wang S, Shen R, Zhang S,
Tian Y, Li M, Zhu D, Yao A, Bao W, et al: Single-cell RNA-seq
reveals the genesis and heterogeneity of tumor microenvironment in
pancreatic undifferentiated carcinoma with osteoclast-like
giant-cells. Mol Cancer. 21:1332022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nagtegaal ID, Odze RD, Klimstra D, Paradis
V, Rugge M, Schirmacher P, Washington KM, Carneiro F and Cree IA;
WHO Classification of Tumours Editorial Board, : The 2019 WHO
classification of tumours of the digestive system. Histopathology.
76:182–188. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Demetter P, Marechal R, Puleo F, Delhaye
M, Debroux S, Charara F, Gomez Galdon M, Van Laethem JL and Verset
L: Undifferentiated pancreatic carcinoma with osteoclast-like giant
cells: What do we know so far? Front Oncol. 11:6300862021.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Luchini C, Pea A, Lionheart G, Mafficini
A, Nottegar A, Veronese N, Chianchiano P, Brosens LA, Noë M,
Offerhaus GJA, et al: Pancreatic undifferentiated carcinoma with
osteoclast-like giant cells is genetically similar to, but
clinically distinct from, conventional ductal adenocarcinoma. J
Pathol. 243:148–154. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gao HQ, Yang YM, Zhuang Y and Liu P:
Locally advanced undifferentiated carcinoma with osteoclast-like
giant cells of the pancreas. World J Gastroenterol. 21:694–698.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Paal E, Thompson LD, Frommelt RA,
Przygodzki RM and Heffess CS: A clinicopathologic and
immunohistochemical study of 35 anaplastic carcinomas of the
pancreas with a review of the literature. Ann Diagn Pathol.
5:129–140. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Saito H, Kashiyama H, Murohashi T, Sasaki
K, Misawa R and Ohwada S: Case of six-year disease-free survival
with undifferentiated carcinoma of the pancreas. Case Rep
Gastroenterol. 10:472–478. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang KY, Choi JI, Choi MH, Park MY, Rha
SE, Byun JY, Jung ES and Lall C: Magnetic resonance imaging
findings of undifferentiated carcinoma with osteoclast-like giant
cells of pancreas. Clin Imaging. 40:148–151. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jo S: Huge undifferentiated carcinoma of
the pancreas with osteoclast-like giant cells. World J
Gastroenterol. 20:2725–2730. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang L, Lee JM, Yoon JH, Joo I, Kang HJ,
Han JK and Jeon SK: Huge and recurrent undifferentiated carcinoma
with osteoclast-like giant cells of the pancreas. Quant Imaging Med
Surg. 8:457–460. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang J and Luo J: Osteoclast-like giant
cell undifferentiated carcinoma of the pancreas: A case report. Int
J Clin Exp Pathol. 14:179–185. 2021.PubMed/NCBI
|
|
15
|
Zhan K, Zhang S, Hu P, Chen J, Liu W and
Niu Z: Undifferentiated carcinoma of the pancreas with osteoclast
like giant cells: Literature review with CT/MR imaging findings in
3 cases. Radiol Case Rep. 17:2529–2533. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gao Y, Cai B, Yin L, Song G, Lu Z, Guo F,
Chen J, Xi C, Wei J, Wu J, et al: Undifferentiated carcinoma of
pancreas with osteoclast-like giant cells: One center's experience
of 13 cases and characteristic pre-operative images. Cancer Manag
Res. 14:1409–1419. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fukukura Y, Kumagae Y, Hirahara M,
Hakamada H, Nagano H, Nakajo M, Kamimura K, Nakajo M, Higashi M and
Yoshiura T: CT and MRI features of undifferentiated carcinomas with
osteoclast-like giant cells of the pancreas: A case series. Abdom
Radiol (NY). 44:1246–1255. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Treadwell JR, Zafar HM, Mitchell MD,
Tipton K, Teitelbaum U and Jue J: Imaging tests for the diagnosis
and staging of pancreatic adenocarcinoma: A meta-analysis.
Pancreas. 45:789–795. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sato K, Urakawa H, Sakamoto K, Ito E,
Hamada Y and Yoshimitsu K: Undifferentiated carcinoma of the
pancreas with osteoclast-like giant cells showing intraductal
growth and intratumoral hemorrhage: MRI features. Radiol Case Rep.
14:1283–1287. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Moutinho-Ribeiro P, Liberal R and Macedo
G: Endoscopic ultrasound in pancreatic cancer treatment: Facts and
hopes. Clin Res Hepatol Gastroenterol. 43:513–521. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gao L, Li ZS, Jin ZD, Man XH, Zhang MH and
Zhu MH: Undifferentiated carcinoma with osteoclast-like giant cells
of the pancreas diagnosed by endoscopic ultrasonography-guided
fine-needle aspiration. Chin Med J (Engl). 122:1598–1600.
2009.PubMed/NCBI
|
|
22
|
Fu LP, Cheng AP, Wang XG, Fu JL and Jin L:
18F-FDG PET/CT in the detection of undifferentiated carcinoma with
osteoclast-like giant cells of the pancreas. Clin Nucl Med.
42:615–616. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wada T, Itano O, Oshima G, Chiba N,
Ishikawa H, Koyama Y, Du W and Kitagawa Y: A male case of an
undifferentiated carcinoma with osteoclast-like giant cells
originating in an indeterminate mucin-producing cystic neoplasm of
the pancreas. A case report and review of the literature. World J
Surg Oncol. 9:1002011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Suda K, Takase M, Oyama T, Mitsui T and
Horike S: An osteoclast-like giant cell tumor pattern in a mucinous
cystadenocarcinoma of the pancreas with lymph node metastasis in a
patient surviving over 10 years. Virchows Arch. 438:519–520. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wolfgang CL, Herman JM, Laheru DA, Klein
AP, Erdek MA, Fishman EK and Hruban RH: Recent progress in
pancreatic cancer. CA Cancer J Clin. 63:318–348. 2013. View Article : Google Scholar : PubMed/NCBI
|