Introduction
Neuroblastoma (NB) is the most common solid
extracranial tumor in children and accounts for approximately 15%
of pediatric cancer-associated deaths. Treatments are tailored for
NB patients based on the risk of relapse and death. The
International Neuroblastoma Risk Group (INRG) Classification System
(1) was developed for pretreatment
risk stratification. It used seven risk criteria including the
image-based stage (INRG Staging System) (2), age, histologic category, grade of
tumor differentiation, MYCN status, presence/absence of 11q
aberrations, and tumor cell ploidy, and stratified NB patients into
very low-risk, low-risk, intermediate-risk, and high-risk (HR)
groups. Approximately half of the NB patients were classified into
HR group, whose long-term survival remains no more than 50% despite
aggressive multimodal therapy. This is because more than half of
HR-NB patients experience relapse/regrowth and relapsed/regrown
patients were rarely rescued with less than 10% probability
(3–5). Relapse/regrowth is thought to occur
due to the activation of chemoresistant minimal residual disease
(MRD) remaining in the body following systemic and local cancer
therapy. To improve outcomes for HR-NB patients, a more accurate
MRD evaluation is required to monitor the disease burden and
treatment response (6,7).
MRD in HR-NB patients was commonly evaluated by
detecting neuroblastoma-associated mRNAs (NB-mRNAs) with
quantitative PCR (qPCR) because no common genetic aberration is
identified in NB cells (8,9). Currently, several sets of NB-mRNAs
were shown to possess a significant prognostic value for MRD in
bone marrow (BM) samples (BM-MRD) (10–13).
In addition, we also reported that 7NB-mRNAs (CRMP1, DBH, DDC,
GAP43, ISL1, PHOX2B, and TH mRNAs) quantitated by droplet digital
PCR (ddPCR) had significant and better prognostic information
(14). Although MRD evaluation was
clinically performed with peripheral blood (PB) samples in other
cancer types, MRD in PB samples (PB-MRD) in HR-NB patients was
believed to show a far lower level than BM-MRD and its clinical
significance was not clear (7).
Here, we report an HR-NB case presenting higher levels of PB-MRD
than BM-MRD before 1st and 2nd relapse/regrowth.
Case report
Patient and samples
The patient was a 3-year-old female diagnosed with
INRG stage M (2), HR-NB (1). Disease evaluation was conducted based
on the International Neuroblastoma Response Criteria (15). All PB and BM samples were obtained
with written informed consent. The use of human samples for the
present study was approved by the Ethics Committee at Kobe
University Graduate School of Medicine and the study was conducted
in accordance with the Guidelines for the Clinical Research of Kobe
University Graduate School of Medicine.
Pathological examination
Tumor tissue samples were fixed with 10% buffered
formalin for 24 h at room temperature, paraffin-infiltrated
overnight, and embedded in the paraffin by auto-processer
(Tissue-Tek, Sakura Finetek Japan, Tokyo, Japan) according to
manufacturer's instructions. For Hematoxylin and Eosin (HE)
staining, tissue blocks were sectioned at 3 µm, dewaxed, and
stained by HE at room temperature by auto-stainer (Tissue-Tek,
Sakura Finetek Japan) according to manufacturer's instructions. For
immunostaining, tissue blocks were sectioned at 3 µm, dewaxed, and
heated for 20 min in Bond Epitope Retrieval Solution 2 (Leica
Biosystems, Nussloch, Germany). The sectioned slides were incubated
with an anti-Synaptophysin primary antibody (Clone 27G12, Leica
Biosystems) without dilution, stained with Bond Polymer Refine
Detection kit (Leica Biosystems), and counterstained with
hematoxylin using Bond-Max automation system (Leica Biosystems)
according to manufacturer's instructions. The stained slides were
evaluated by pathologist using BX53 microscope (Evident, Tokyo,
Japan) at ×200 or ×400 magnification.
7NB-mRNAs ddPCR assay
7NB-mRNA ddPCR assay was performed using a QX200
ddPCR system (Bio-Rad Laboratories, Hercules, CA) in a total volume
of 20 µl consisting of 10 µl 2X ddPCR Supermix for probes (Bio-Rad
Laboratories), 3.3 µl each of 3 µmol/l sense and antisense primers,
0.5 µl of 10 µmol/l Universal Probe Library probe (Roche, Mannheim,
Germany), and 1 µl sample cDNA (corresponding to 12.5 ng total RNA)
according to the manufacturer's instructions. The expressions of 7
NB-mRNAs (CRMP1, DBH, DDC, GAP43, ISL1, PHOX2B, and TH) and a
reference gene mRNA (HPRT1) were determined based on the absolute
quantification method according to the Minimum Information for
Publication of Quantitative Digital PCR Experiments (MIQE)
guideline (16,17), and the level of 7NB-mRNAs (combined
signature) was calculated as the weighted sum of 7 relative copy
numbers (level of each NB-mRNA), in which the reciprocal of 90
percentile in non-NB control PB and BM sample was used for the
weighting for each NB-mRNA, as described previously (14). The following primer and probe sets
used in the present case: CRMP1 (accession number NM_001014809)
5′-CCAATCCCTTTATGCTGACG-3′ (forward),
5′-GGAACGATTAAGTTCTCTCCTATTTG-3′ (reverse), and Universal Probe
Library number 65 probe (Roche), DBH (accession number NM_000787)
5′-TGGGGACACTGCCTATTTTG-3′ (forward), 5′-TTCTGGGGTCCTCTGCAC-3′
(reverse), and Universal Probe Library number 3 probe (Roche), DDC
(accession number NM_000790) 5′-CTGGAGAAGGGGGAGGAGT-3′ (forward),
5′-GCCGATGGATCACTTTGGT-3′ (reverse), and Universal Probe Library
number 49 probe (Roche), GAP43 (accession number NM_002045)
5′-GAGGATGCTGCTGCCAAG-3′ (forward), 5′-GGCACTTTCCTTAGGTTTGGT-3′
(reverse), and Universal Probe Library number 26 probe (Roche),
ISL1 (accession number NM_002202) 5′-AAGGACAAGAAGCGAAGCAT-3′
(forward), 5′-TTCCTGTCATCCCCTGGATA-3′ (reverse), and Universal
Probe Library number 66 probe (Roche), PHOX2B (accession number
NM_003924) 5′-CTACCCCGACATCTACACTCG-3′ (forward),
5′-CTCCTGCTTGCGAAACTTG-3′ (reverse), and Universal Probe Library
number 17 probe (Roche), TH (accession number NM_199292)
5′-TCAGTGACGCCAAGGACA-3′ (forward), 5′-GTACGGGTCGAACTTCACG-3′
(reverse), and Universal Probe Library number 42 probe (Roche),
HPRT1 (accession number NM_000194) 5′-TGACCTTGATTTATTTTGCATACC-3′
(forward), 5′-CGAGCAAGACGTTCAGTCCT-3′ (reverse), and Universal
Probe Library number 73 probe (Roche).
Clinical course
The patient was admitted to Kobe children's hospital
because of fever and leg pain. She had no remarkable medical
history and did not show any remarkable abnormalities. Initial
laboratory test detected the elevated levels of urine VMA 500 µg/mg
Cre, urine HVA 331 µg/mg Cre and serum NSE 553 µg/l. Computed
tomography (CT) images demonstrated a left adrenal gland mass
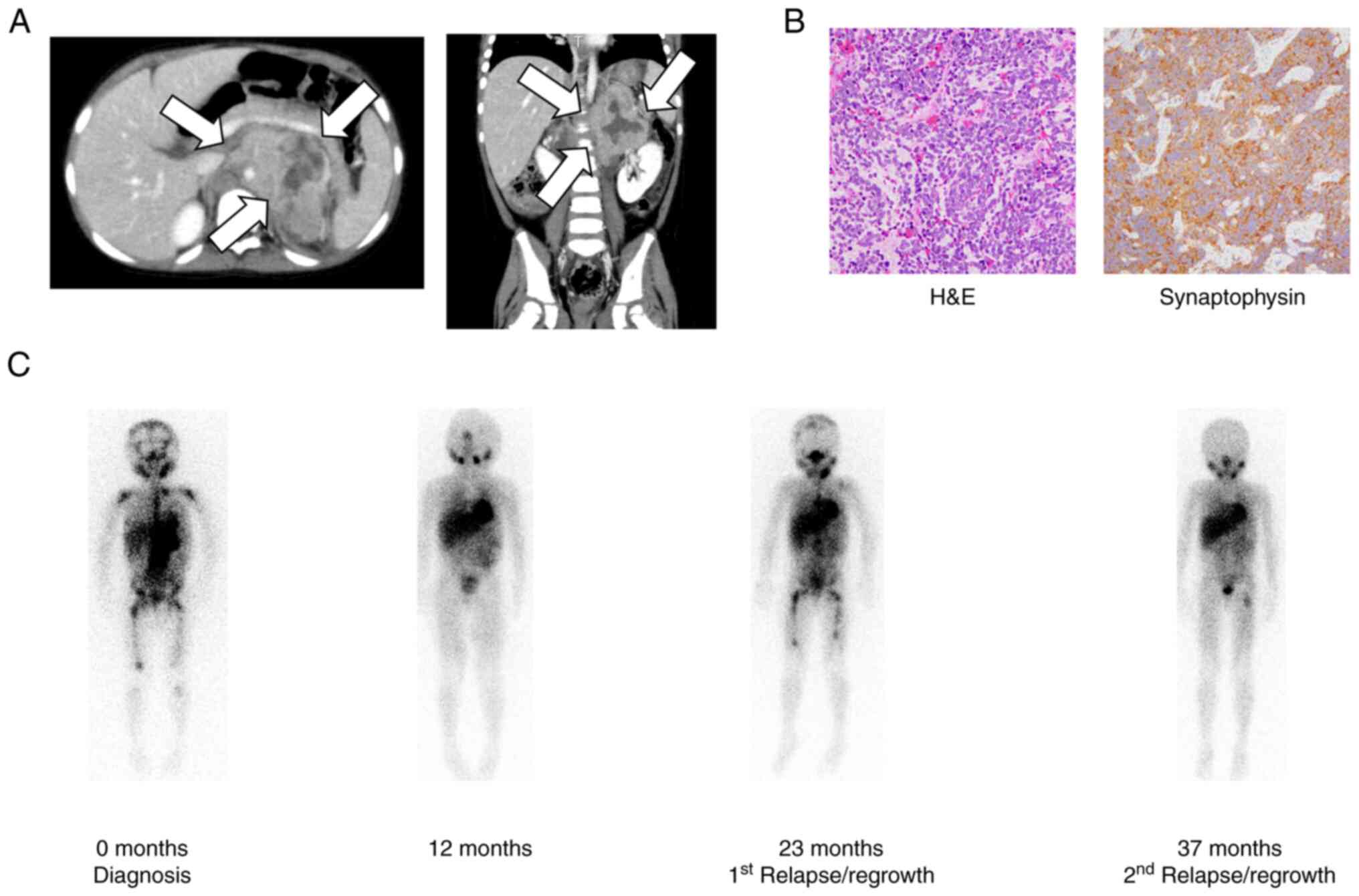
(Fig. 1A).
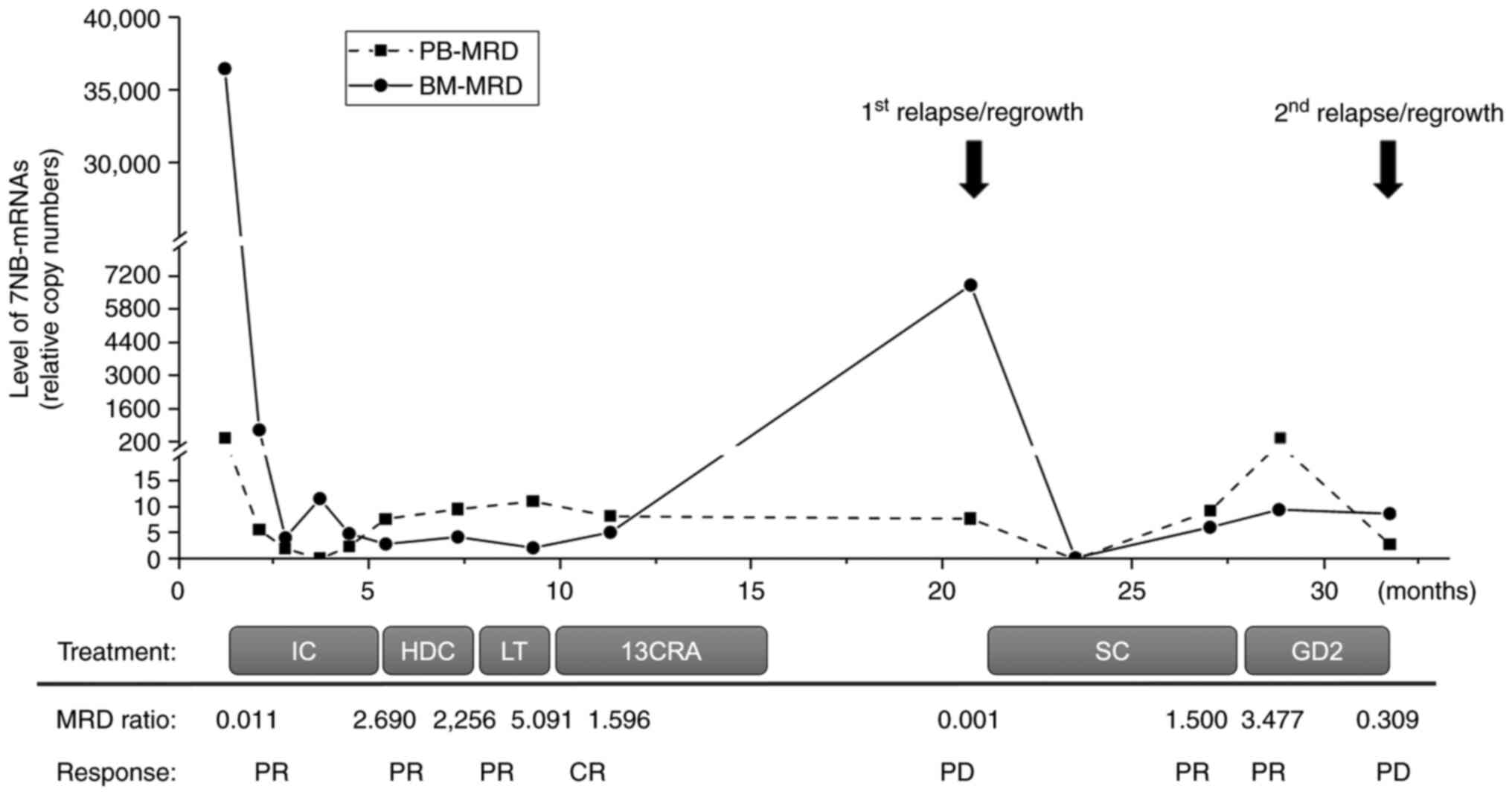
123I-metaiodobenzylguanidine (123I-MIBG)
scintigraphy revealed multiple bone metastases in the humerus,
femur, pelvis, skull, and vertebrae (Fig. 1B). She underwent an open biopsy of
the adrenal tumor (Fig. 1C). A
pathological examination revealed a poorly differentiated NB with
intermediate mitosis-karyorrhexis index (MKI) and non-amplified
MYCN status. BM examination showed metastatic NB cells. Based on
these findings, she was diagnosed as HR-NB according to the INRG
Classification System (1).
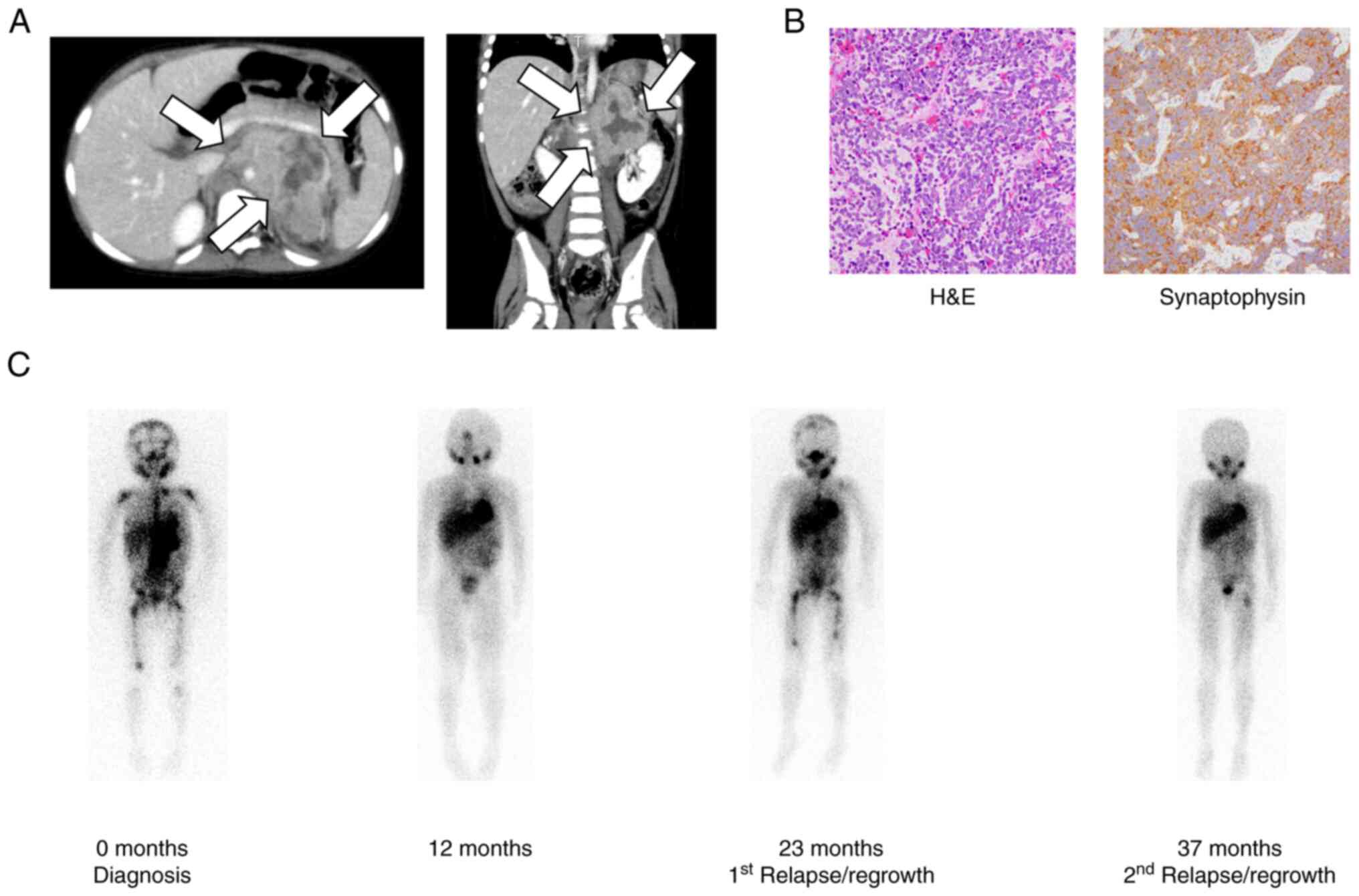 | Figure 1.(A) CT images of an abdominal tumor at
diagnosis. A tumor with a diameter of ~6 cm (white arrows) was
detected in the left adrenal gland. (B) Pathological examination of
the adrenal tumor. Small round tumor cells were arranged in nests
separated by slender fibers (original magnification, ×200).
Immunostaining was positive for synaptophysin (original
magnification, ×400). (C) Representative MIBG images during the
entire course of treatment. MIBG-avid lesions were detected in left
adrenal gland, right and left upper carpal bones, spine, pelvis,
and right and left thigh bones at 0 months, disappeared at 12
months, and reappeared in the left upper carpal bones, spine,
pelvis, and right and left thigh bones at 23 months and in the left
thigh bone at 37 months. H&E, hematoxylin and eosin staining;
MIBG, metaiodobenzylguanidine. |
Following the diagnosis of HR-NB, she was treated
according to the nationwide standard protocol. Induction
chemotherapy with one cycle of 05A1 regimen (1,200 mg/m2
cyclophosphamide (CPA), 1.5 mg/m2 vincristine (VCR), 40
mg/m2 pirarubicin (THP), 100 mg/m2 cisplatin
(CDDP)) (18), two cycles of 05A3
regimen (2,400 mg/m2 CPA, 1.5 mg/m2 VCR, 40
mg/m2 THP, 100 mg/m2 CDDP) (18), and two cycles of ICE regimen (800
mg/m2 carboplatin (CBDCA), 9,000 mg/m2
ifosfamide (IFO), 500 mg/m2 etoposide (VP16)) (19) was completed, and MIBG-avid lesions
were disappeared expect for the primary lesion. High-dose
chemotherapy (12.4 mg/kg busulfan (BU), 180 mg/m2
melphalan (L-PAM)) with autologous peripheral blood stem cell
transplantation (PBSCT) followed by gross total resection of the
primary tumor and radiation therapy with proton beam (30.6 Gy) was
performed, and she achieved complete remission. Maintenance therapy
with 13-cis-retinoic acid (13CRA: 6 cycles of a 28-day cycle of 14
consecutive 160 mg/m2/day administration) followed this
induction and consolidation therapy.
She developed lower limb pain 6 months after the
completion of maintenance therapy. NB cells and MIBG-avid lesions
were detected in BM and multiple bones, respectively, and she was
diagnosed with 1st relapse/regrowth. Salvage chemotherapy with 4
cycles of TI regimen (500 mg/m2 temozolomide (TMZ), 200
mg/m2 irinotecan (CPT-11)) and 5 cycles of TC regimen
(3.75 mg/m2 topotecan, 1,250 mg/m2 CPA) was
undertaken, and she achieved partial remission. Anti-GD2
immunotherapy (6 cycles of a 28-day cycle of alternating 300
mg/m2 dinutuximab with 70 µg/kg filgrastim or 300
mg/m2 dinutuximab with 7,000,000 IU/m2
teceleukin) was initiated, but she developed lower limb pain again
during 4 cycles of the regimen. BM examination did not reveal NB
cells, but MIBG-avid lesions appeared in a thigh bone. She was
diagnosed with 2nd relapse/regrowth.
MRD monitoring
PB-MRD and BM-MRD were consecutively monitored
during the entire course of treatment until 2nd relapse/regrowth
(Fig. 2). Both PB-MRD and BM-MRD
were highly elevated at diagnosis and decreased with induction
chemotherapy. PB-MRD was approximately 100 times lower than BM-MRD
at diagnosis (PB-MRD/BM-MRD designated as MRD ratio 0.011) and
after 1 cycle of induction chemotherapy (MRD ratio 0.008) and
decreased to the bottom after 3 cycles of induction chemotherapy.
PB-MRD was reelevated and became higher than BM-MRD after 5 cycles
of induction chemotherapy and remained higher than BM-MRD during
consolidation and maintenance therapy and follow-up (MRD ratio
2.690, 2.256, 5.091, and 1.596). At 1st relapse/regrowth (MRD ratio
0.001), PB-MRD became almost 1,000 times lower than BM-MRD. With
salvage chemotherapy, both PB-MRD and BM-MRD decreased and were
reelevated. PB-MRD became higher than BM-MRD during salvage
chemotherapy and anti-GD2 immunotherapy (MRD ratio 1.500 and
3.477). but lower than BM-MRD at 2nd relapse/regrowth (MRD ratio
0.309).
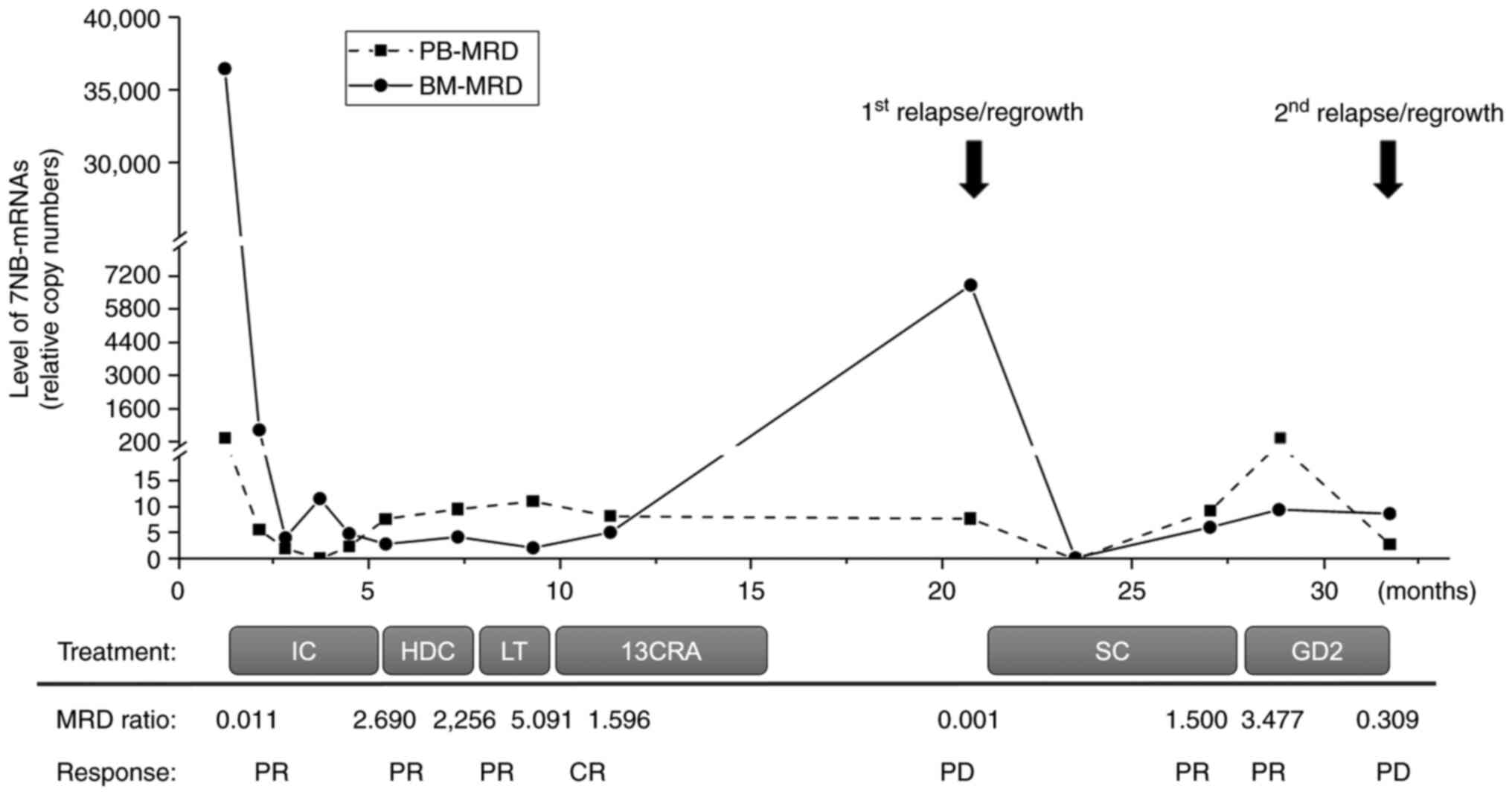 | Figure 2.Consecutive PB-MRD and BM-MRD
monitoring. Month 0 was defined as the time of diagnosis.
7NB-mRNAs, 7 neuroblastoma-associated mRNAs; 13CRA, 13-cis-retinoic
acid; BM-MRD, MRD in bone marrow samples; CR, complete response;
GD2, anti-GD2 immunotherapy; HDC, high-dose chemotherapy; IC,
induction chemotherapy; LT, local therapy; MRD, minimal residual
disease; MRD ratio, PB-MRD/BM-MRD; PB-MRD, MRD in peripheral blood
samples; PD, progressive disease; PR, partial response; SC, salvage
chemotherapy. |
Discussion
MRD is defined as residual cancer cells that remain
in patients following local and systemic therapies. These cancer
cells exist as cancer stem cells (CSCs) in primary and metastatic
lesions, circulating tumor cells (CTCs) in PB, and disseminated
tumor cells (DTCs) in BM (6,7). Since
consecutive sampling of primary and metastatic lesions is very
difficult, PB and BM samples are commonly used to evaluate MRD in
many cancer types. Although a prognostic value of PB-MRD has been
established for acute lymphoblastic leukemia (ALL) (20), acute myeloid leukemia (AML)
(21), and chronic myelogenous
leukemia (CML) (22), it depends on
cancer types in nonhematopoietic solid tumors.
In HR-NB patients, NB cells were pathologically
detected in PB at diagnosis and during chemotherapy (23,24).
Expression of two sets of NB-mRNAs in PB samples collected at
diagnosis was shown to predict patient outcome (11,25).
Although a significant correlation between PB-MRD and BM-MRD was
reported by quantitating 5NB-mRNAs (CHGA, DCX, DDC, PHOX2B, TH
mRNAs) with qPCR (13) and
7NB-mRNAs (CRMP1, DBH, DDC, GAP43, ISL1, PHOX2B, and TH mRNAs) with
ddPCR (14,26), respectively, the level of PM-MRD was
approximately 10–100 times lower than BM-MRD, raising concern about
the sensitivity of PB-MRD. Accordingly, the clinical significance
of PB-MRD is not clear for HR-NB patients.
In the present case, PB-MRD was almost 100–1,000
times lower than BM-MRD at diagnosis and 1st relapse/regrowth (MRD
ratio 0.011 and 0.001) and after 1 cycle of induction chemotherapy
(MRD ratio 0.008). It became higher than BM-MRD before 1st and 2nd
relapse/regrowth (MRD ratio 5.091, and 3.477). Although PB-MRD was
generally believed to be lower than BM-MRD, it was not always true.
PB-MRD (median 5.2) was reported to be higher than BM-MRD (median
3.8) during induction and consolidation therapy in 27 PB and 89 BM
samples from 14 and 19 HR-NB patients (14). The amount of DTCs in BM aspirates
(=BM-MRD) is almost proportional to the amount of NB cells
pathologically detected in BM, whereas CTCs are derived from both
primary and metastatic NB tumors residing anywhere in the patient's
body including BM. It is generally recognized that the amount of
CTCs (=PB-MRDs) is very limited and difficult to predict by
pathological BM examination, MIGB scintigraphy, and CT/magnetic
resonance imaging (MRI) imaging. Based on the present case's
observation, we suggest the following scenario: PB-MRD will be
~1,000 times lower than BM-MRD when NB cells macroscopically
metastasize/invade into BM, whereas PB-MRD can become higher than
BM-MRD in at least some patients when NB cells residing in BM are
macroscopically eradicated by induction, consolidation, and
maintenance therapy. What determines the balance between CTCs and
NB tumors (i.e., how many NB cells are released from tumor mass as
CTCs) is still an open question and may depend on each patient's
specific condition, such as the BM microenvironment after high-dose
chemotherapy with autologous PBSCT. Although only a single case's
observation, it is tempting to speculate that the elevated PB-MRD
before relapse/regrowth implicates the emergence of
relapse/regrowth-causing CTCs.
In conclusion, the present case highlights the fact
that PB-MRD can become higher than BM-MRD before relapse/regrowth
of HR-NB patients. Consecutive PB-MRD and BM-MRD monitoring during
the entire course of treatment will be warranted to clarify the
clinical significance of PB-MRD for HR-NB patients.
Acknowledgements
Not applicable.
Funding
The present study was supported by Grants-in-Aid for Scientific
Research (KAKENHI) from Japan Society for the Promotion of Science
(grant no. 21K07750).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SI treated the patient, obtained clinical samples,
analyzed data and wrote the manuscript. KHNW and CYM acquired and
analyzed data. TF, SH, SU, TI, TM, AN, NNak, NNin, AT and NY
treated the patient and acquired data. DH, YK and KN designed the
study and interpreted data. NNis conceived and designed the study,
analyzed and interpreted data, and wrote the manuscript. SI and
NNis confirmed the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The parents of the patient provided written informed
consent for participation in the study.
Patient consent for publication
The parents of the patient provided written informed
consent for the publication of any data and/or accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cohn SL, Pearson AD, London WB, Monclair
T, Ambros PF, Brodeur GM, Faldum A, Hero B, Iehara T, Machin D, et
al: The International Neuroblastoma Risk Group (INRG)
Classification system: An INRG task force report. J Clin Oncol.
27:289–297. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Monclair T, Brodeur GM, Ambros PF, Brisse
HJ, Cecchetto G, Holmes K, Kaneko M, London WB, Matthay KK,
Nuchtern JG, et al: The International Neuroblastoma risk group
(INRG) staging system: An INRG task force report. J Clin Oncol.
27:298–303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brodeur GM: Neuroblastoma: Biological
insights into a clinical enigma. Nat Rev Cancer. 3:203–216. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Maris JM, Hogarty MD, Bagatell R and Cohn
SL: Neuroblastoma. Lancet. 369:2106–2120. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tolbert VP and Matthay KK: Neuroblastoma:
Clinical and biological approach to risk stratification and
treatment. Cell Tissue Res. 372:195–209. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mordant P, Loriot Y, Lahon B, Castier Y,
Leseche G, Soria JC, Massard C and Deutsch E: Minimal residual
disease in solid neoplasia: New frontier or red-herring? Cancer
Treat Rev. 38:101–110. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Uemura S, Ishida T, Thwin KKM, Yamamoto N,
Tamura A, Kishimoto K, Hasegawa D, Kosaka Y, Nino N, Lin KS, et al:
Dynamics of minimal residual disease in neuroblastoma patients.
Front Oncol. 9:4552019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beiske K, Ambros PF, Burchill SA, Cheung
IY and Swerts K: Detecting minimal residual disease in
neuroblastoma patients-the present state of the art. Cancer Lett.
228:229–240. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Brownhill SC and Burchill SA: PCR-based
amplification of circulating RNAs as prognostic and predictive
biomarkers-Focus on neuroblastoma. Pract Lab Med. 7:41–44. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stutterheim J, Zappeij-Kannegieter L,
Versteeg R, Caron HN, van der Schoot CE and Tytgat GA: The
prognostic value of fast molecular response of marrow disease in
patients aged over 1 year with stage 4 neuroblastoma. Eur J Cancer.
47:1193–1202. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Viprey VF, Gregory WM, Corrias MV,
Tchirkov A, Swerts K, Vicha A, Dallorso S, Brock P, Luksch R,
Valteau-Couanet D, et al: Neuroblastoma mRNAs predict outcome in
children with stage 4 neuroblastoma: A European HR-NBL1/SIOPEN
study. J Clin Oncol. 32:1074–1083. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cheung NK, Ostrovnaya I, Kuk D and Cheung
IY: Bone marrow minimal residual disease was an early response
marker and a consistent independent predictor of survival after
anti-GD2 immunotherapy. J Clin Oncol. 33:755–763. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Marachelian A, Villablanca JG, Liu CW, Liu
B, Goodarzian F, Lai HA, Shimada H, Tran HC, Parra JA, Gallego R,
et al: Expression of five neuroblastoma genes in bone marrow or
blood of patients with relapsed/refractory neuroblastoma provides a
new biomarker for disease and prognosis. Clin Cancer Res.
23:5374–5383. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Thwin KKM, Ishida T, Uemura S, Yamamoto N,
Lin KS, Tamura A, Kozaki A, Saito A, Kishimoto K, Mori T, et al:
Level of seven neuroblastoma-associated mRNAs detected by droplet
digital PCR is associated with tumor relapse/regrowth of high-risk
neuroblastoma patients. J Mol Diagn. 22:236–246. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Park JR, Bagatell R, Cohn SL, Pearson AD,
Villablanca JG, Berthold F, Burchill S, Boubaker A, McHugh K,
Nuchtern JG, et al: Revisions to the International Neuroblastoma
Response Criteria: A consensus statement from the National cancer
institute clinical trials planning meeting. J Clin Oncol.
35:2580–2587. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bustin SA, Benes V, Garson JA, Hellemans
J, Huggett J, Kubista M, Mueller R, Nolan T, Pfaffl MW, Shipley GL,
et al: The MIQE guidelines: Minimum information for publication of
quantitative real-time PCR experiments. Clin Chem. 55:611–622.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huggett JF, Foy CA, Benes V, Emslie K,
Garson JA, Haynes R, Hellemans J, Kubista M, Mueller RD, Nolan T,
et al: The digital MIQE guidelines: Minimum information for
publication of quantitative digital PCR experiments. Clin Chem.
59:892–902. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kaneko M, Tsuchida Y, Mugishima H, Ohnuma
N, Yamamoto K, Kawa K, Iwafuchi M, Sawada T and Suita S:
Intensified chemotherapy increases the survival rates in patients
with stage 4 neuroblastoma with MYCN amplification. J Pediatr
Hematol Oncol. 24:613–621. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Donfrancesco A, Jenkner A, Castellano A,
Ilari I, Milano GM, De Sio L, Cozza R, Fidani P, Deb G, De
Laurentis C, et al: Ifosfamide/carboplatin/etoposide (ICE) as
front-line, topotecan/cyclophosphamide as second-line and oral
temozolomide as third-line treatment for advanced neuroblastoma
over one year of age. Acta Paediatr Suppl. 93:6–11. 2007.
View Article : Google Scholar
|
|
20
|
Coustan-Smith E, Sancho J, Hancock ML,
Razzouk BI, Ribeiro RC, Rivera GK, Rubnitz JE, Sandlund JT, Pui CH
and Campana D: Use of peripheral blood instead of bone marrow to
monitor residual disease in children with acute lymphoblastic
leukemia. Blood. 100:2399–2402. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kitamura K, Nishiyama T, Ishiyama K,
Miyawaki S, Miyazaki K, Suzuki K, Masaie H, Okada M, Ogawa H, Imai
K, et al: Clinical usefulness of WT1 mRNA expression in bone marrow
detected by a new WT1 mRNA assay kit for monitoring acute myeloid
leukemia: A comparison with expression of WT1 mRNA in peripheral
blood. Int J Hematol. 103:53–62. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jiang Q, Zhao XY, Qin YZ, Liu YR, Lai YY,
Jiang B and Huang XJ: The differences and correlations of BCR-ABL
transcripts between peripheral blood and bone marrow assays are
associated with the molecular responses in the bone marrow for
chronic myelogenous leukemia. Am J Hematol. 87:1065–1069. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Moss TJ and Sanders DG: Detection of
neuroblastoma cells in blood. J Clin Oncol. 8:736–740. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Seeger RC, Reynolds CP, Gallego R, Stram
DO, Gerbing RB and Matthay KK: Quantitative tumor cell content of
bone marrow and blood as a predictor of outcome in stage IV
neuroblastoma: A Children's Cancer Group Study. J Clin Oncol.
18:4067–4076. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yanez Y, Hervas D, Grau E, Oltra S, Perez
G, Palanca S, Bermudez M, Marquez C, Canete A and Castel V: TH and
DCX mRNAs in peripheral blood and bone marrow predict outcome in
metastatic neuroblastoma patients. J Cancer Res Clin Oncol.
142:573–580. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lin KS, Uemura S, Thwin KKM, Nakatani N,
Ishida T, Yamamoto N, Tamura A, Saito A, Mori T, Hasegawa D, et al:
Minimal residual disease in high-risk neuroblastoma shows a dynamic
and disease burden-dependent correlation between bone marrow and
peripheral blood. Transl Oncol. 14:1010192021. View Article : Google Scholar : PubMed/NCBI
|