Introduction
Hepatopancreatoduodenectomy (HPD), first reported in
1974 for the treatment of locally advanced gallbladder cancer, is
currently performed in a limited number of medical centers due to
the complexity of the operation, high incidence of complications
and high mortality rate (1). HPD
has a high surgical resection rate. According to literature reports
(2,3), in 1979 to 1996, among 32 patients who
underwent HPD surgery, radical resection can reach 20 patients
(63%). However, due to immature surgical experience and medical
equipment, complications occurred in 29 patients (91%) and
perioperative deaths occurred in 15 patients (47%) after surgery.
With the advancement of surgical technology and the accumulation of
experience, clinical doctors have reduced the surgical resection
range, achieving the same cure rate while significantly reducing
the incidence of postoperative complications and mortality. Over
the following eight years, the incidence of postoperative
complications decreased to 31% and the postoperative mortality rate
decreased to zero (2). With the
progress of laparoscopic technology, various types of complex
laparoscopic hepatectomy and laparoscopic pancreaticoduodenectomy
have been widely used, but there are few reports on the use of
laparoscopic HPD (LHPD) (3–6). To the best of our knowledge, the
present study is the first to report a synchronous primary
malignant tumor originating in the left hepatic and common bile
ducts treated using LHPD.
Case presentation
A 63-year-old male was admitted to Affiliated Jinhua
Hospital, Zhejiang University School of Medicine (Jinhua, China) in
October 2022 with right upper abdominal distension and pain
associated with yellow sclera for 1 week. Physical examination
demonstrated yellow skin and sclera. Laboratory testing
demonstrated that bilirubin and transaminase levels were elevated
and tumor marker testing demonstrated elevated CA199 levels
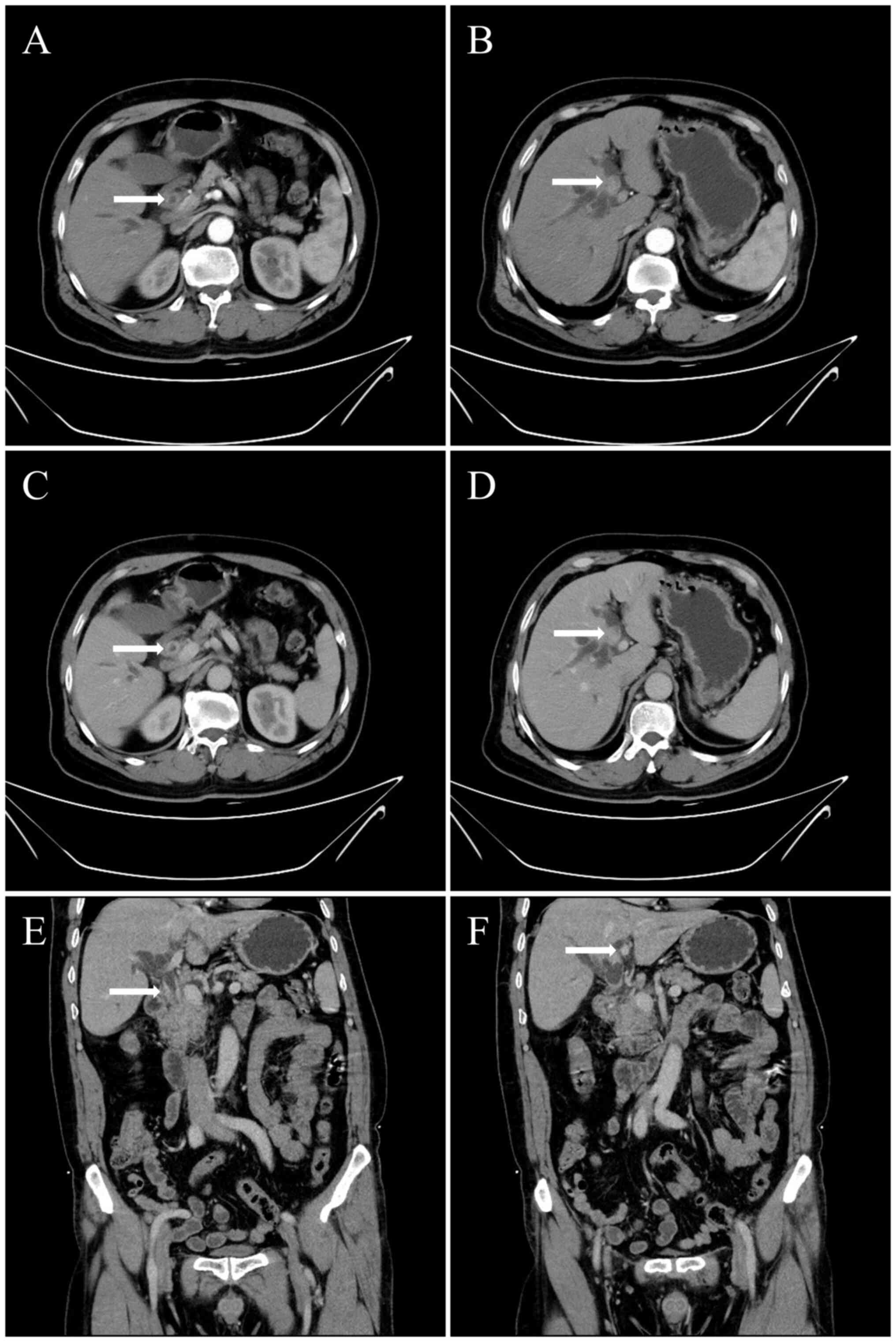
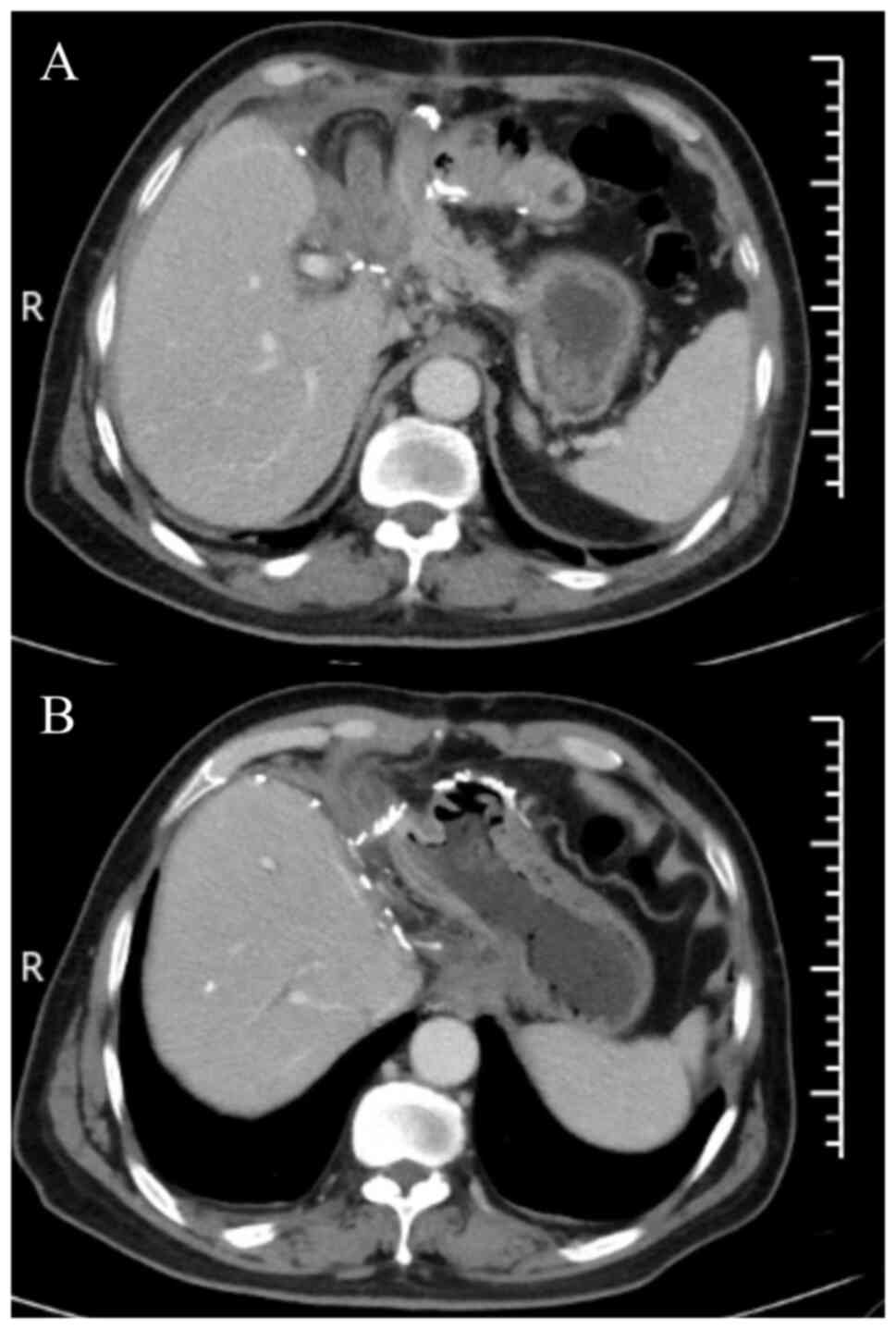
(Table I). Upper abdominal enhanced
computed tomography (CT; Fig. 1),
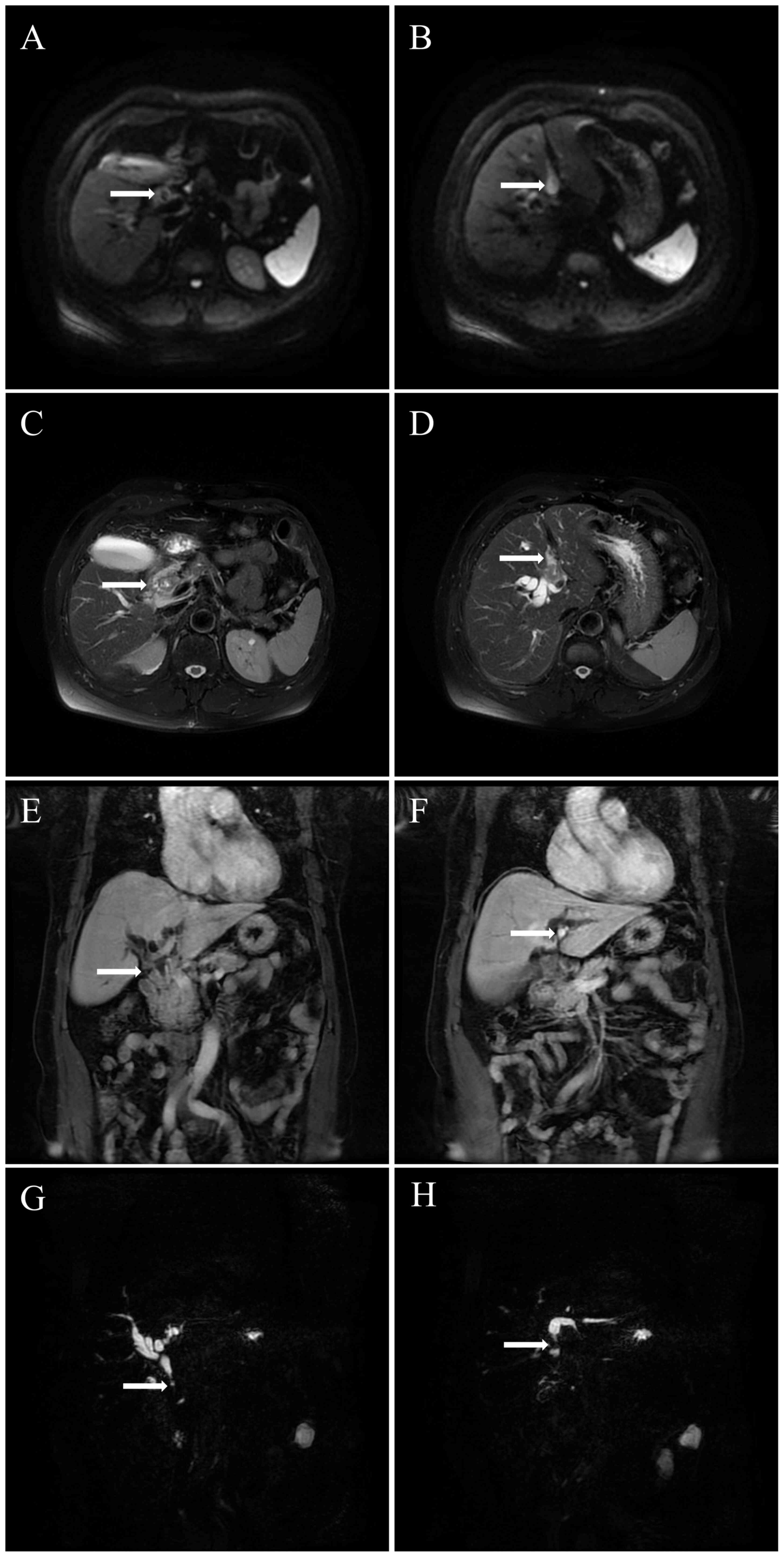
enhanced magnetic resonance imaging (MRI) and magnetic resonance
cholangiopancreatogram (MRCP; Fig.
2) demonstrated that the local wall of the middle and lower
segments of the common bile duct were thickened, the lumen was
narrow and the enhancement of common bile duct wall was visible.
The intrahepatic and extrahepatic bile ducts above the stenosis
were dilated, local wall of the left hepatic duct was thickened and
the enhancement of left hepatic duct wall was visible. After
reviewing patient medical history and imaging, the patient was
diagnosed with cholangiocarcinoma arising in the left liver and in
the middle and lower segment of the common bile duct. The liver
function was Child B grade according to the Child-Pugh
classification (7), therefore,
laparoscopic left hemihepatectomy and caudate lobectomy and
pancreatoduodenectomy were performed.
 | Table I.Preoperative hematological laboratory
results. |
Table I.
Preoperative hematological laboratory
results.
| Laboratory test | Result | Reference value |
|---|
| Hemoglobin, g/l | 120.0 | 120.0–165.0 |
| Albumin, g/l | 35.0 | 35.0–51.0 |
| TBil, µmol/l | 110.4 | 3.4–17.1 |
| DBil, µmol/l | 74.6 | 1.7–10.2 |
| ALT, U/l | 179.6 | 0.0–40.0 |
| AST, U/l | 85.5 | 0.0–40.0 |
| CEA, ng/ml | 5.7 | <5.0 |
| CA199, U/ml | 199.6 | <37.0 |
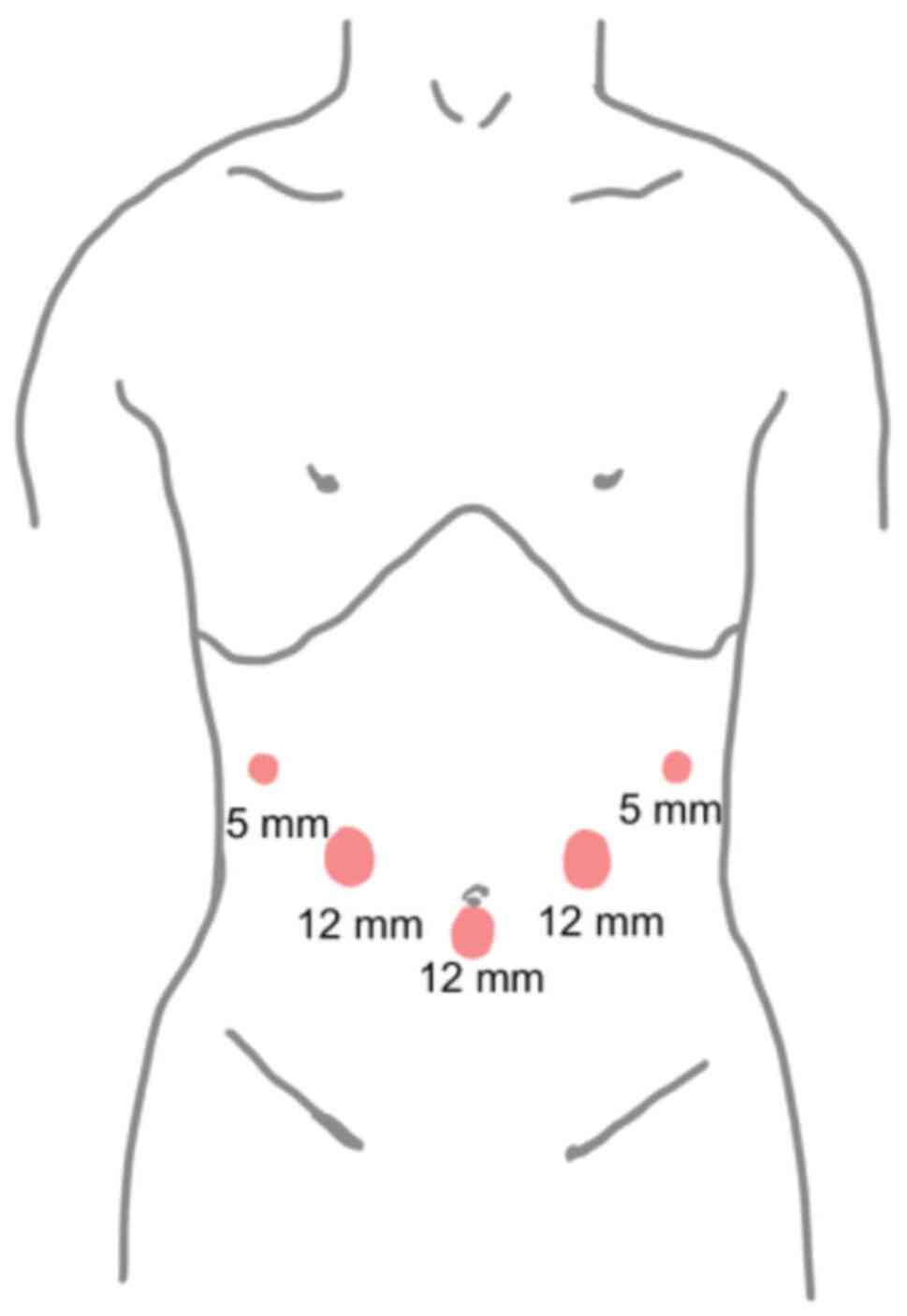
The position of the abdominal puncture hole for the
patient undergoing the surgery was the same as that of the
laparoscopic pancreaticoduodenal surgery, which was a V-shaped
five-hole method (8) (Fig. 3) with the patient in a supine split
leg position. The chief surgeon was on the right of the patient
while the first assistant was on the left side of the patient with
a supporting hand between the patient's legs. After administration
of general anesthesia, the patient was placed in a flat position
with the head high and legs apart. The laparoscope was placed under
the umbilicus and surgical instruments were placed under the left
and right costal margins and outside the rectus abdominis. First,
the gallbladder triangle, artery and bed were separated. After the
lesser omentum was opened, the lymph nodes of groups 6, 8a, 8p,
13a, 13b, 14a, 14b, 17a and 17b were removed along the upper edge
of the pancreas. To ligate and disconnect the right gastric and
gastroduodenal artery, the proper hepatic, gastroduodenal and left
and right hepatic arteries were separated. The common hepatic
artery was suspended to the left to expose the main portal vein and
lymph nodes of group 12 were cleaned. After confirmation that the
tumor was consistent with the preoperative image without vascular
invasion, pancreatoduodenectomy was performed via the superior
mesenteric vein approach. The left hepatic artery and left branch
of the portal vein were disconnected and the pancreaticoduodenal
specimen was placed in the left upper quadrant of the abdominal
cavity. The liver parenchyma was dissected along the gallbladder
bed and the segment IV branch of middle hepatic vein was ligated
and disconnected. The liver parenchyma was dissected along the
middle hepatic vein trunk to the head to expose the right front and
rear bile ducts. Next, the caudate lobe along the right side of the
inferior vena cava was disconnected and the left hepatic vein was
cut using an Endo-GIA Stapler. The left half of the liver, left
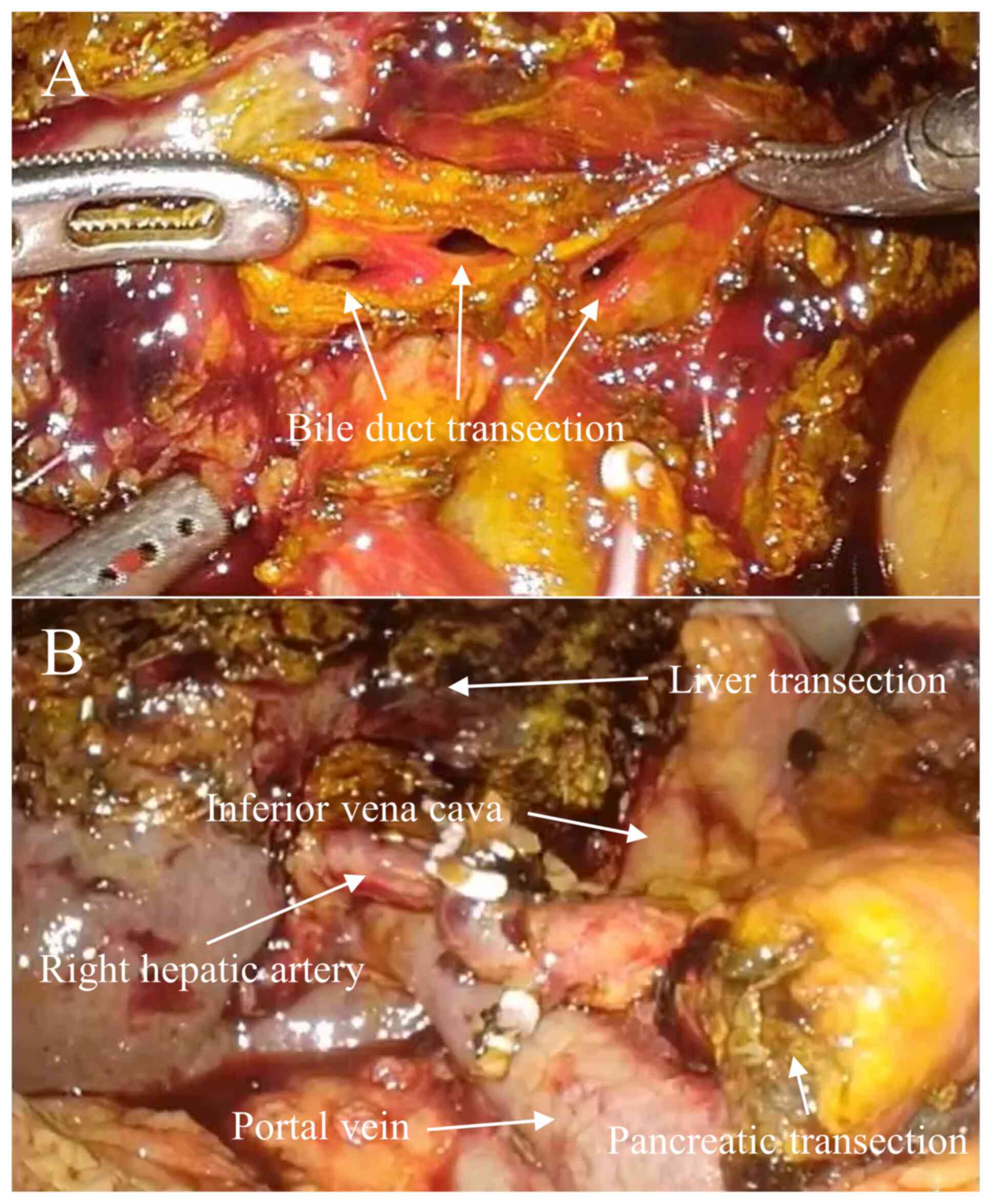
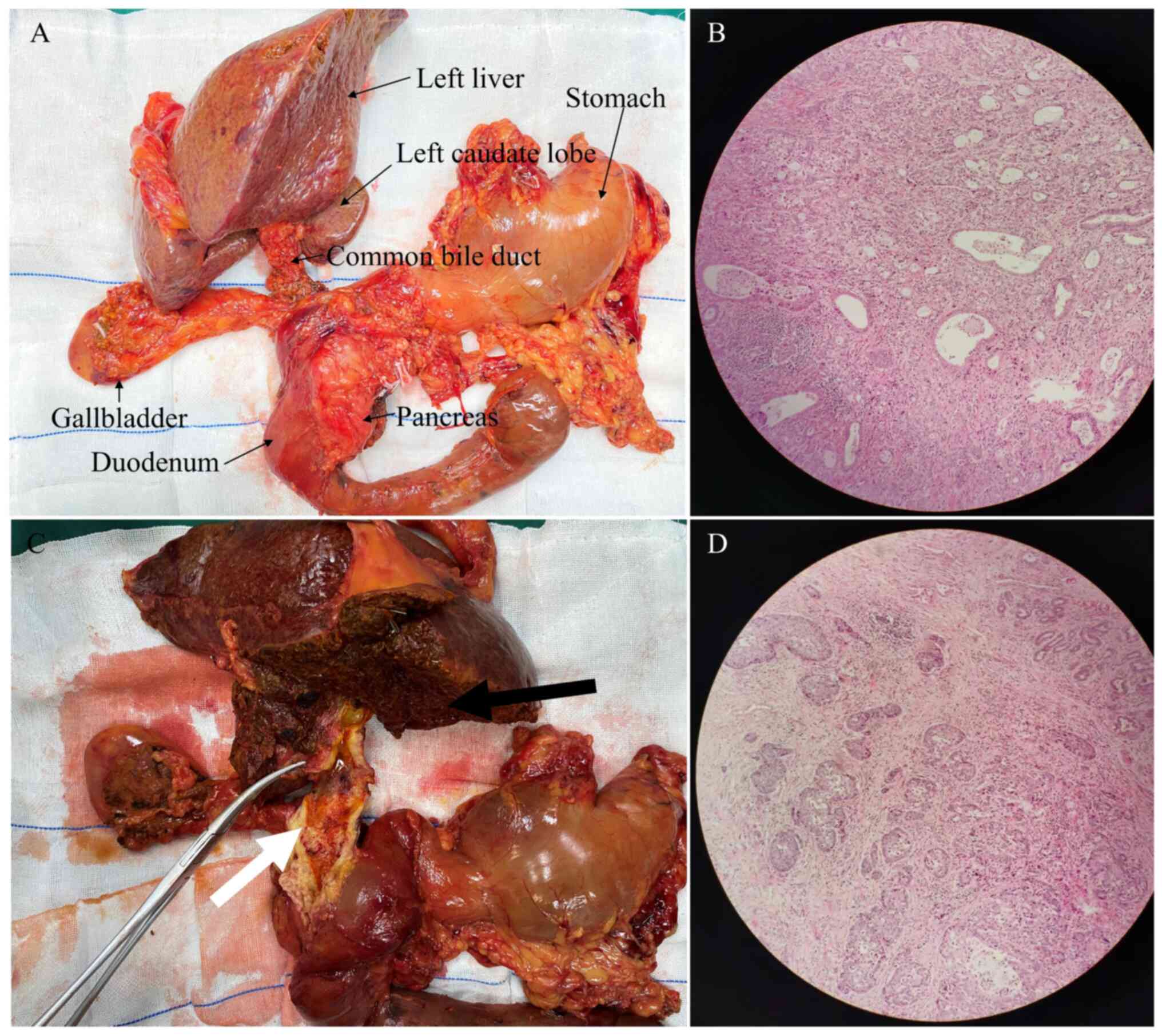
caudate lobe and pancreaticoduodenum were removed (Figs. 4 and 5A
and 5C). For surgical excision of pathological specimens,
specimens were placed in the left upper abdomen and reconstruction
process was completed under laparoscopy. The pancreaticojejunal
anastomosis was performed using double-pouch sutures (9). After the right anterior and posterior
bile ducts were reshaped, the cholangiojejunal anastomosis was
continuously sutured using 4-0 Purdis sutures. The posterior wall
of the greater curvature of the stomach and mesenteric margin of
the small intestine were anastomosed laterally using a linear
cutting closure device. An incision of 3–4 cm in the upper abdomen
was made to remove specimens for pathology. After washing the
abdominal cavity with distilled water, drainage tubes were placed
before and after the cholangiojejunostomy and
pancreaticojejunostomy.
The operation took 540 min and the bleeding volume
of the patient was ~500 ml. After the operation, the patient was
transferred to the intensive care unit for monitoring and
treatment. The patient was moved to the general ward on the second
day after the operation and diet was returned to normal on the
third day after the operation. There was no bile leakage or
gastrointestinal dysfunction after the operation, however, a minor
pancreatic fistula was observed. The drainage tube in front of the
biliary intestinal anastomosis was removed 7 days after surgery and
the drainage tube behind the biliary intestinal anastomosis was
removed 12 days after surgery. The drainage tube in front of the
pancreatic intestinal anastomosis was removed 15 days after surgery
and the drainage tube behind the pancreatic intestinal anastomosis
was removed 19 days after surgery. The patient was discharged 16
days after the operation. To study the number of lymph node
metastases, the dewaxed sample was placed in a hematoxylin staining
solution with a concentration of 0.5% and stained at room
temperature for 10 min, then placed in an eosin staining solution
with a concentration of 0.05% and stained at room temperature for 2
min, and finally observed under a light microscope (Leica DM IL
LED). The results demonstrated that a total of 36 lymph nodes were
removed during surgery, including eight lymph nodes demonstrating
cancer metastasis. According to the pathological findings, the
tumor at the left hepatic duct was diagnosed a poorly
differentiated adenocarcinoma with squamous cell carcinoma and the
tumor at common bile duct was diagnosed as poorly differentiated
adenocarcinoma (Fig. 5B and D).
Synchronous primary cancer was considered and the pathological
stage was T4N1M0. The patient received chemotherapy with
gemcitabine (1,000 mg/m2 at day 1 and day 8,
oxaliplatin, 130 mg/m2 at day 2) for 1 month after
surgery but was unable to tolerate this treatment. At 4 months
after surgery, the patient's postoperative tumor marker results are
within the expected range and the postoperative CT results
demonstrated no tumor recurrence (Fig.
6).
Discussion
HPD is a complex operation in the field of
hepatobiliary and pancreatic surgery. Due to the high incidence of
complications and mortality (1),
this surgical method is controversial. A previous study reported
that the mortality rate after HPD is 26% and the complication rate
is 87% (10). For certain patients
with locally advanced cholangiocarcinoma, the operation is the only
treatment option to cure the disease (11). Ebata et al (1) reported that the 5-year survival rate
of 85 consecutive patients with cholangiocarcinoma after HPD
treatment was 37.4%. Sakamoto et al (12) and Jiang et al (13) reported that the 5-year survival rate
of cholangiocarcinoma after HPD treatment is 45%, significantly
higher compared with non-resectable tumors. To date, HPD treatment
for synchronous primary cholangiocarcinoma is rarely performed; to
the best of our knowledge, only one case of synchronous primary
cholangiocarcinoma has previously been reported (3,5)
(Table II). To the best of our
knowledge, the present study reported the first case of synchronous
primary cholangiocarcinoma treated with LHPD.
 | Table II.Articles on LPD surgery. |
Table II.
Articles on LPD surgery.
| Patient
diagnosis | Operation | First author and
year | (Refs.) |
|---|
| Extrahepatic
cholangiocarcinoma | LPD + LRH | Zhang et al,
2014 | (3) |
| Extrahepatic
cholangiocarcinoma | LPD + LLH | Chong et al,
2019 | (5) |
| Gallbladder
cancer | LPD + LSH | James et al,
2021 | (6) |
| Gallbladder cancer
and extrahepatic cholangiocarcinoma | LPD + LSH | Yao et al,
2022 | (4) |
HPD involves simultaneous hepatectomy and
pancreatoduodenectomy so is highly technical, has a long operation
time and is associated with large volume of bleeding during
operation. A previous study reported that the average operation
time is 850 min and the intraoperative bleeding volume is 1.8 l
(14). The present study adopted a
double-main surgeon method. The surgeon on the left completed the
hilar anatomy, pancreatectomy and pancreaticojejunostomy and the
surgeon on the right completed the uncinate process anatomy, liver
parenchyma disconnection and cholangiojejunostomy. In the present
case, the operation time was 540 min and the bleeding volume was
~500 ml, which improved the operation efficiency and ensured the
safety and quality of the procedure.
Liver failure is the primary cause of death after
liver surgery (15). Ebata et
al (1) performed portal vein
embolization (PVE) on 78.8% of patients with an estimated
hepatectomy volume >60%, with a mortality rate of 2.4%. The
aforementioned study suggested that PVE may avoid liver failure in
patients with HPD with extensive hepatectomy. Nagaraj et al
(16) reported two cases of central
hepatectomy with liver parenchyma preservation, which increased 55
and 25% of remnant liver volumes, respectively, and avoided liver
failure. Preoperative biliary drainage (PBD) is a controversial
procedure (17). A previous study
reported that PBD increases risk of postoperative infection and
does not improve the mortality and complication rate following
hepatectomy (18). However, another
study reported that PBD is not associated with postoperative
infection (19). Accurate
preoperative evaluation is important for LHPD. Thin slice CT, MRI
and three-dimensional (3D) reconstruction and cholangiography
should be performed routinely to evaluate the scope and stage of
the tumor (20,21). Liver function should be also
evaluated by 15-min indocyanine green retention rate and the
residual liver ratio should be calculated using the resulting CT
images (22).
Pancreatic leakage is a major complication of
pancreatectomy. Pancreaticojejunostomy is difficult as the pancreas
of patients with cholangiocarcinoma is soft and the pancreatic duct
is thin (23). A previous study
reported the incidence of pancreatic leakage in patients with HPD
is 69.4% (1). Aoki et al
(24) reported that the mortality
rate of patients with HPD following secondary
pancreaticojejunostomy is low (1/52 patients). Secondary
pancreaticojejunostomy can reduce complications such as pancreatic
leakage, infection and bleeding, as pancreatic enzymes are not
activated by enterokinase (24). In
hepatectomy after pancreaticoduodenectomy, the obstruction of the
hepatic hilus causes congestion of the residual pancreas and
promotes pancreatic leakage and it is recommended that hepatectomy
be performed first (25). A
previous study reported that the incidence of pancreatic leakage in
patients with HPD with small-scale hepatectomy is similar to that
of patients undergoing pancreaticoduodenectomy, but the incidence
of pancreatic leakage in patients with HPD with large-scale
hepatectomy is higher compared with patients with HPD with
small-scale hepatectomy (31.4 vs. 21.0%, respectively) (26). This suggests that large-scale
hepatectomy could delay healing of wounds such as pancreatic
anastomosis. The surgery in the present study routinely placed
pancreatic duct stents consistent with pancreatic duct diameters
and performed precise pancreaticojejunal double-pouch anastomosis
using 3D laparoscopy. The incidence of pancreatic leakage at
Affiliated Jinhua Hospital, Zhejiang University School of Medicine
from 2013 to 2021 was ~10% after pancreaticoduodenectomy (9).
In conclusion, the present study demonstrated that
it is feasible to perform LHPD in a center with proficiency in
laparoscopy via precise preoperative evaluation and strengthening
perioperative management.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SY and YB conceived and designed the study. BW and
YB conducted the surgery. YB and BW analyzed and interpreted the
data. SY and YB reviewed the manuscript. SY and BW confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent to participate was obtained
from the patients for this study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of any potentially identifiable images
or data included in this article.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
LHPD
|
laparoscopic
hepatopancreatoduodenectomy
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
MRCP
|
magnetic resonance
cholangiopancreatogram
|
|
PVE
|
portal vein embolization
|
|
PBD
|
preoperative biliary drainage
|
|
3D
|
three-dimensional
|
References
|
1
|
Ebata T, Yokoyama Y, Igami T, Sugawara G,
Takahashi Y, Nimura Y and Nagino M: Hepatopancreatoduodenectomy for
cholangiocarcinoma: A single-center review of 85 consecutive
patients. Ann Surg. 256:297–305. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ota T, Araida T, Yamamoto M and Takasaki
K: Operative outcome and problems of right hepatic lobectomy with
pancreatoduodenectomy for advanced carcinoma of the biliary tract.
J Hepatobiliary Pancreat Surg. 14:155–158. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang MZ, Xu XW, Mou YP, Yan JF, Zhu YP,
Zhang RC, Zhou YC, Chen K, Jin WW, Matro E and Ajoodhea H:
Resection of a cholangiocarcinoma via laparoscopic
hepatopancreato-duodenectomy: A case report. World J Gastroenterol.
20:17260–17264. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yao GL: Laparoscopic
hepatopancreaticoduodenectomy for synchronous gallbladder cancer
and extrahepatic cholangiocarcinoma: A case report. World J Surg
Oncol. 20:1902022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chong EH and Choi SH: Hybrid laparoscopic
and robotic hepatopancreaticoduodenectomy for cholangiocarcinoma. J
Gastrointest Surg. 23:1947–1948. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
James M, Kalayarasan R, Gnanasekaran S and
Pottakkat B: Laparoscopic hepatopancreatoduodenectomy for locally
advanced gall bladder cancer. J Minim Access Surg. 17:369–372.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bolukbas FF, Bolukbas C, Horoz M, Gumus M,
Erdogan M, Zeyrek F, Yayla A and Ovunc O: Child-Pugh classification
dependent alterations in serum leptin levels among cirrhotic
patients: A case controlled study. BMC Gastroenterol. 4:232004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang M, Zhang H, Wu Z, Zhang Z and Peng B:
Laparoscopic pancreaticoduodenectomy: Single-surgeon experience.
Surg Endosc. 29:3783–3794. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhou H, Yu S, Wu X and Li X: Application
of purse string suture pancreaticojejunostomy for undilated
pancreatic duct in total laparoscopic pancreaticoduodenectomy. BMC
Surg. 22:1952022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Welch JC, Gleeson EM, Karachristos A and
Pitt HA: Hepatopancreatoduodenectomy in North America: Are the
outcomes acceptable? HPB (Oxford). 22:360–367. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Moris D, Palta M, Kim C, Allen PJ, Morse
MA and Lidsky ME: Advances in the treatment of intrahepatic
cholangiocarcinoma: An overview of the current and future
therapeutic landscape for clinicians. CA Cancer J Clin. 73:198–222.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sakamoto Y, Nara S, Kishi Y, Esaki M,
Shimada K, Kokudo N and Kosuge T: Is extended hemihepatectomy plus
pancreaticoduodenectomy justified for advanced bile duct cancer and
gallbladder cancer? Surgery. 153:794–800. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jiang Y, Zeng Z, Zeng J, Liu C, Qiu J, Li
Y, Tang J, Mo N, Du L and Ma J: Efficacy and safety of first-line
chemotherapies for patients with advanced biliary tract carcinoma:
A systematic review and network meta-analysis. Front Oncol.
11:7361132021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dai WC, Chok KS, Cheung TT, Chan AC, Chan
SC and Lo CM: Hepatopancreatoduodenectomy for advanced
hepatobiliary malignancies: A single-center experience.
Hepatobiliary Pancreat Dis Int. 16:382–386. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Schreckenbach T, Liese J, Bechstein WO and
Moench C: Posthepatectomy liver failure. Dig Surg. 29:79–85. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nagaraj K, Goto Y, Kojima S, Sakai H,
Hisaka T, Akagi Y and Okuda K: Central
hepatopancreatoduodenectomy-oncological effectiveness and
parenchymal sparing option for diffusely spreading bile duct
cancer: Report of two cases. BMC Surg. 21:232021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhu L, Yang Y, Cheng H, Cai Z, Tang N, Mao
L, Fu X and Qiu Y: The role of preoperative biliary drainage on
postoperative outcome after pancreaticoduodenectomy in patients
with obstructive jaundice. Gland Surg. 12:593–608. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ferrero A, Lo Tesoriere R, Viganò L,
Caggiano L, Sgotto E and Capussotti L: Preoperative biliary
drainage increases infectious complications after hepatectomy for
proximal bile duct tumor obstruction. World J Surg. 33:318–325.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sugawara G, Ebata T, Yokoyama Y, Igami T,
Takahashi Y, Takara D and Nagino M: The effect of preoperative
biliary drainage on infectious complications after hepatobiliary
resection with cholangiojejunostomy. Surgery. 153:200–210. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Awad S, Fagan S, Abudayyeh S, Karim N,
Berger D and Ayub K: Preoperative evaluation of hepatic lesions for
the staging of hepatocellular and metastatic liver carcinoma using
endoscopic ultrasonography. Am J Surg. 184:601–605. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gefter W: Magnetic resonance imaging in
the evaluation of lung cancer. Semin Roentgenol. 25:73–84. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shimizu A, Motoyama H, Kubota K, Notake T,
Fukushima K, Ikehara T, Hayashi H, Yasukawa K, Kobayashi A and
Soejima Y: Safety and oncological benefit of
hepatopancreatoduodenectomy for advanced extrahepatic
cholangiocarcinoma with horizontal tumor spread: Shinshu university
experience. Ann Surg Oncol. 28:2012–2025. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gai YW, Wang HT and Tan XD:
Pancreaticojejunostomy conducive to biological healing in minimally
invasive pancreaticoduodenectomy. J Gastrointest Surg.
26:1967–1981. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Aoki T, Sakamoto Y, Kohno Y, Akamatsu N,
Kaneko J, Sugawara Y, Hasegawa K, Makuuchi M and Kokudo N:
Hepatopancreaticoduodenectomy for biliary cancer: Strategies for
near-zero operative mortality and acceptable long-term outcome. Ann
Surg. 267:332–337. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fukami Y, Kaneoka Y, Maeda A, Takayama Y
and Onoe S: Major hepatopancreatoduodenectomy with simultaneous
resection of the hepatic artery for advanced biliary cancer.
Langenbecks Arch Surg. 401:471–478. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Andrianello S, Paiella S, Allegrini V,
Ramera M, Pulvirenti A, Malleo G, Salvia R and Bassi C:
Pancreaticoduodenectomy for distal cholangiocarcinoma: Surgical
results, prognostic factors, and long-term follow-up. Langenbecks
Arch Surg. 400:623–628. 2015. View Article : Google Scholar : PubMed/NCBI
|