Introduction
Esophageal carcinoma (EC) is one of the leading
causes of cancer-associated mortalities, and the majority of EC in
China are squamous cell carcinoma (SCC) (1). The characteristics of esophageal SCC
are quite different from those of esophageal adenocarcinoma (EAC).
The gene expression of ESCC is most semblable to that of head and
neck squamous cell carcinoma, while EAC is most semblable to
gastric adenocarcinoma (2).
Esophageal SCC predominate in the upper and middle third of the
esophagus and are associated with nitrosamine compounds, hot food,
smoking and alcohol exposure, etc.
The symptoms are usually not obvious in early stage
of EC. Therefore, most patients are diagnosed with advanced
disease, resulting in poor survival. The common sites of metastasis
are the lymph node, lung, liver and bones. Certain unexpected sites
have been reported, such as the skin, eyes, muscles and breasts
(3). Metastasis to the pelvic
cavity from esophageal SCC is extremely rare, and the clinical
manifestations are not typical. The standards for the diagnosis of
these unexpected sites are less established. The present study
reports a rare case of esophageal squamous cell carcinoma (SCC)
with rectal metastasis, which may help us to have a better
understanding for this disease.
Case presentation
A 65-year-old man was admitted to the Department of
Radiation Oncology, First Affiliated Hospital of Anhui Medical
University (Hefei, China) with dysphagia for >1 month at March
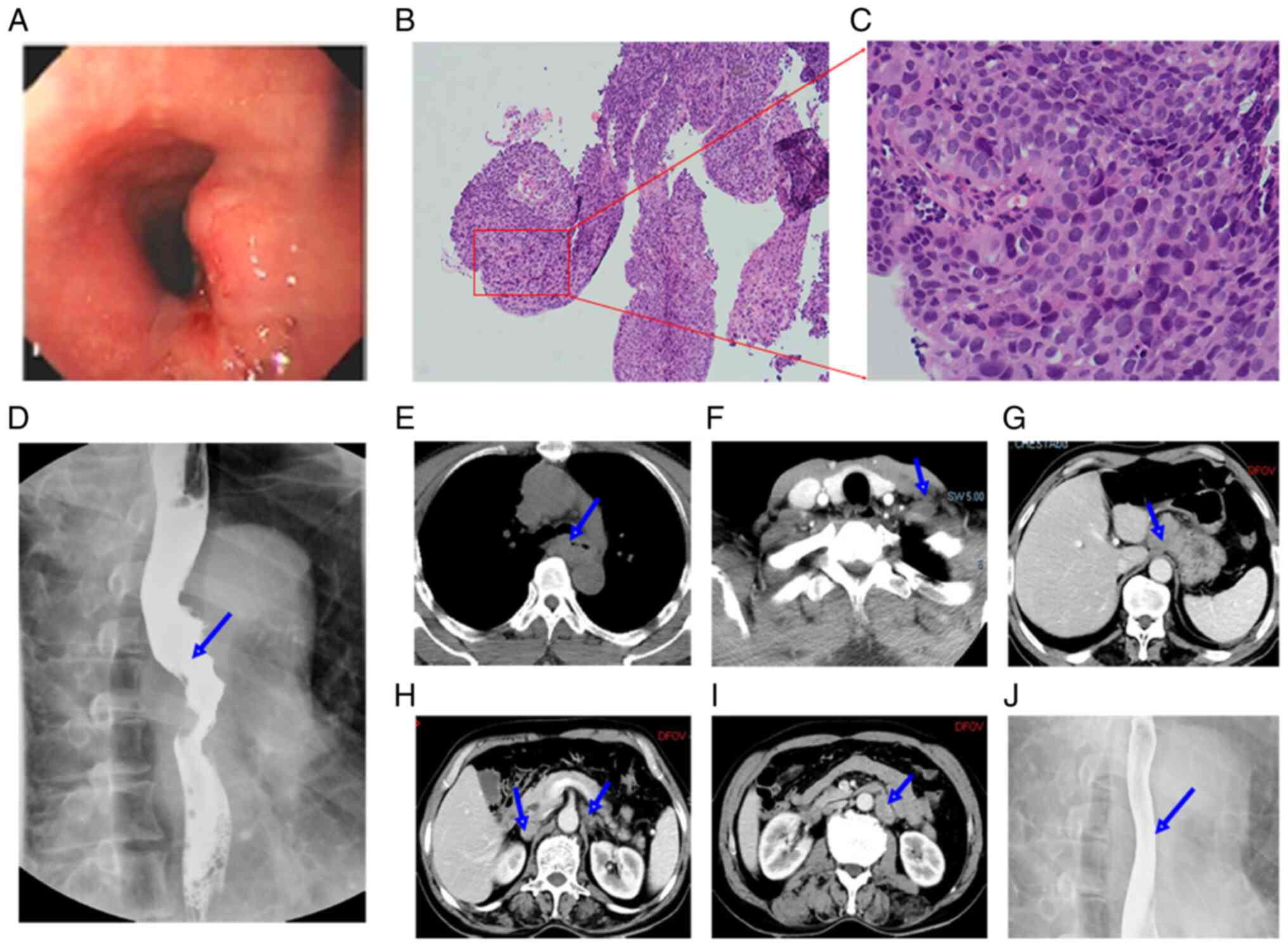
2018. Esophagoscopic evaluation revealed a protruding lesion of
esophageal wall located 25-cm from the incisors, precluding passage
of the endoscope (Fig. 1A).
Histopathological findings showed SCC after biopsy (Fig. 1B and C). The barium swallow showed
irregular esophageal stricture and destruction of esophageal mucosa
in the upper-middle segment (Fig.
1D). A thickened esophageal wall and an enlarged lymph node in
the left supraclavicular area were found on computed tomography
(CT) scans of the neck, chest and upper abdomen (Fig. 1E and F). Fine-needle aspiration
biopsy of this lymph node was performed, and a diagnosis of SCC was
rendered. After a systematic evaluation, the patient received
definite intensity modulated radiotherapy (IMRT) with 64.0 Gy in 32
fractions and two concurrent cycles of chemotherapy with paclitaxel
and platinum. In addition, 2 additional cycles of adjuvant
chemotherapy using the same regimens were admitted thereafter.
The patient achieved a clinical complete response;
however, 1 year later, numerous enlarged paraaortic lymph nodes
with no symptoms were found by a follow-up CT scan (Fig. 1G-I). The esophageal mucosa was
normal (Fig. 1J) and there were no
signs of metastatic spread in other sites. The patient received
IMRT with 50.0 Gy in 25 fractions to the retroperitoneal area and
two cycles of chemotherapy with carboplatin and Tigeo capsule.
Lymph node stations in the present study were based on the Japanese
Classification of Esophageal Cancer of 11th edition (4).
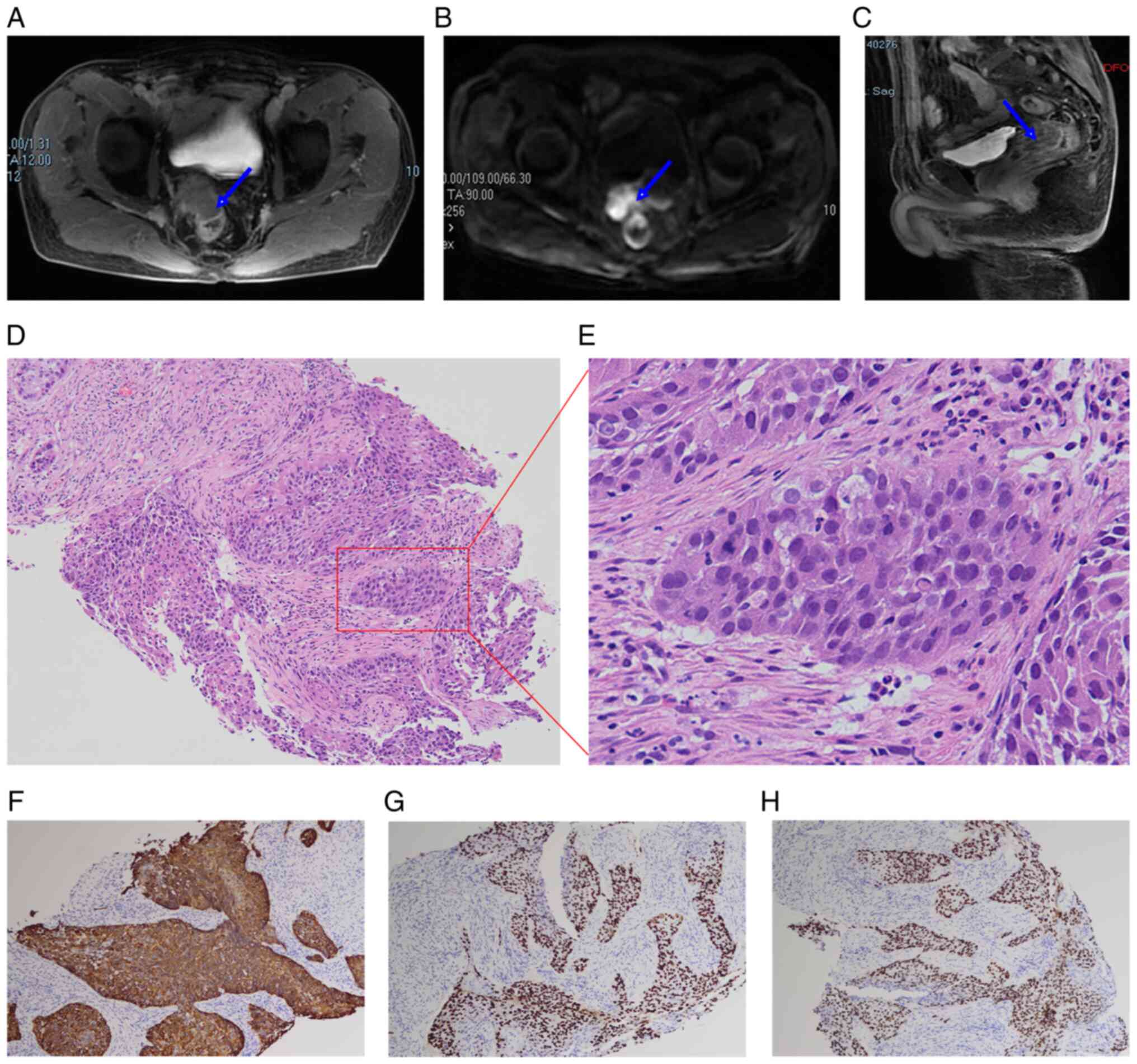
The patient was not followed up regularly and
returned to the hospital 8 months later. A mass in front of the
rectum was found by a follow-up CT scan at the People's Hospital of
Huoqiu County (Huoqiu, China). There were no symptoms of
discomfort. A pelvic enhanced magnetic resonance (MR) scan revealed
a mass in front of the rectum on the right side without invasion of
the rectal mucosa (Fig. 2A-C).
Serum tumor makers indicated that his carcinoembryonic antigen
(CEA) level was slightly elevated (6.1 ng/ml). To make a definite
diagnosis, a transrectal ultrasound-guided biopsy of the mass
instead of colonoscopy was performed because the rectal mucosa was
intact on MR images. Histopathological findings showed SCC with
identical cytomorphology to the primary esophageal tumour (Fig. 2D and E). Immunohistochemical
findings include positive CK5/6, p40 and p63 staining (Fig. 2F-H) and negative CK7, CDX-2 and
Villin staining, which was consistent with a metastatic lesion from
esophageal SCC. A CT scan of the neck, chest and abdomen
demonstrated no obvious residual tumour. After a discussion with
the patient, palliative IMRT with 36.0 Gy in 18 fractions and a
cycle of concurrent chemotherapy with the Tigeo capsule was
administered. Further treatment was refused because of diarrhea and
a decrease in platelets (32×109/l). After discharge, the
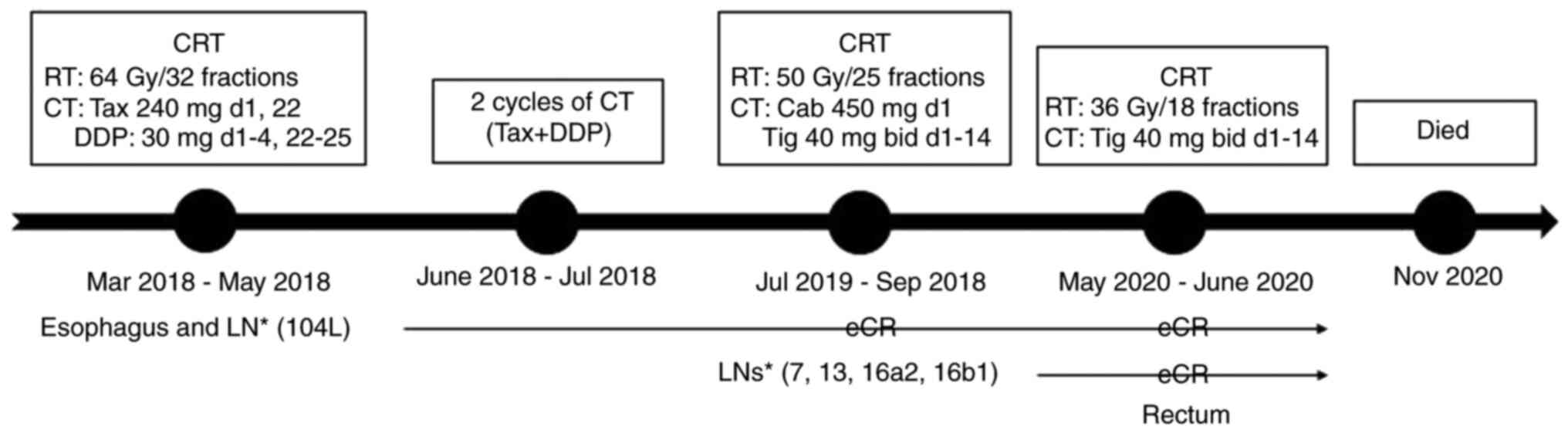
patient died 5 months later. The treatment timeline was shown in
Fig. 3.
Discussion
EC is the seventh most common cancer and sixth most
common cause of cancer-associated mortalities worldwide in 2020
(5). SCC and adenocarcinoma are the
most common histological subtypes with quite different aetiologies
(2). China has a high incidence
rate, accounting for ~50% of the global total cases, and >90% of
cases are SCC (1). Despite
improvements in diagnosis and treatments, overall survival is still
poor for EC. One important reason is that most patients are
diagnosed at an advanced stage, making radical treatment
difficult.
There are five main routes of metastasis for EC: i)
Direct invasion; ii) lymphatic system; iii) hematogenous; iv)
transperitoneal; and v) intraluminal implantation. The common
metastatic sites are the lymph node, lungs, liver and bones.
Occasionally, brain metastasis can be found in EC (6). Additionally, some unexpected sites
have been reported, such as the skin, eyes, muscles and breasts
(3). Table I summarizes the reported cases of
colonic metastasis from esophageal SCC (7–14). To
the best of our knowledge, rectal metastasis from esophageal SCC
has not been previously reported.
 | Table I.Published cases of colonic metastasis
from esophageal squamous cell carcinoma. |
Table I.
Published cases of colonic metastasis
from esophageal squamous cell carcinoma.
| Authors (year) | Age, years | Sex | Location | Symptom | Treatment | Survival from colonic
metastasis | (Refs.) |
|---|
| Iwase et al,
2004 | 51 | Man | Sigmoid | Bleeding | Chemotherapy | 1 year | (7) |
| Shimada et al,
2014 | 64 | Man | Transverse | None | Resection | 2.5 months | (8) |
| Hasegawa et al,
2015 | 77 | Man | Transverse | Pain | Resection | 2 months | (9) |
| Garg et al,
2017 | 60 | Man | Ascending | Bleeding | Radiation | 6 months | (10) |
| Fang et al,
2017 | 63 | Man | Sigmoid | Pain, nausea | Unknown | Unknown | (11) |
| Wiseman et al,
2020 | 71 | Woman | Rectosigmoid | None | Radiation | 6 months | (12) |
| Chen et al,
2022 | 68 | Man | Ascending | None | Unknown | Unknown | (13) |
| Zhang et al,
2022 | 73 | Woman | Transverse | None | Chemotherapy | Unknown | (14) |
Although it is rare, primary rectal SCC can also be
found, accounting for ~0.3% of all rectal cancer (15). The etiology of primary rectal SCC
remains unclear, and the most prominent theory is chronic
inflammation leading to squamous metaplasia and subsequent
carcinoma (16). To diagnose
primary rectal SCC, four criteria were proposed by researchers
(15,17): i) Absence of SCC in any other organ
that may spread directly to rectum; ii) the affected rectum should
not be involved in any squamous-lined fistula tract; iii) exclusion
of the tumor being from proximal extension of anal SCC; and iv)
confirmation of SCC by histopathology.
Given that rectal cancer can be SCC, metastatic
rectal SCC should be discriminated from primary rectal SCC. Primary
rectal SCC lesions usually have an appearance of lesions
infiltrating from the mucosa gradually to the deep wall of the
rectum. Histologically, it is not possible to determine whether it
is of rectal or metastatic origin based on morphological
characteristics. Features that led to classifying the present case
as metastasis included the intact overlying mucosa of the rectum
and histological features identical to those of esophageal tumour
cells.
Metastatic involvement of the rectum out from pelvic
tumors is rare. There are cases of metastatic rectal cancer from
breast cancer (18),
gastroesophageal adenocarcinoma (19) and gastric cancer (20). The hematogenous spread of
circulating tumour cells is a plausible explanation for these
distant metastases. Due to the complex lymphatic drainage of the
esophagus, lymphatic spread may be another potential explanation
(21). In the present case, there
were extensive abdominal lymph node metastases without involvement
of common distant organs. Therefore, retrograde lymphatic spread of
cancer cells to the rectum should be considered, as has been
proposed in cases of a Krukenburg tumor (22).
A pelvic examination is not usually a part of the
workup for EC (23). The present
case may heighten the awareness of unexpected metastasis to the
pelvis, especially for patients with extensive abdominal lymph node
metastases. Positron emission tomography (PET) may be helpful in
detecting these unusual metastases (9,11). It
is a limitation that PET was not performed in the present case
report. For rectal tumors, MRI can help to find the tumour location
and morphology and identify its relationship with surrounding
structures (24). Biopsy is
requested to determine the histological type and molecular markers
of the tumour.
For patients with stage IV ESCC, systematic therapy
or palliative care is recommended based on the Karnofsky
performance in the National Comprehensive Caner Network (NCCN)
guidelines (25). To improve
quality of life and survival, a multidisciplinary approach is
usually needed. The present patient received chemoradiotherapy to
the rectum because the well-controlled tumor in other sites after
chemoradiotherapy. In recent years, immunotherapy with PD-1
inhibitors has demonstrated promising activity in recurrent or
metastatic esophageal SCC (26,27).
To the best of our knowledge, the present case is
the first report of esophageal SCC with middle rectal metastasis.
It is of utmost importance to take a biopsy of this unexpected
lesion for histological analysis, which can help to discriminate
metastatic from primary cancer. The goal of treatment with
multidisciplinary approach is palliative therapy to improve quality
of life and survival for this metastatic disease.
Acknowledgements
Not applicable.
Funding
The present study was supported by University Natural Science
Research Project of Anhui Province (grant no. KJ2021A0300).
Availability of data and materials
All data generated or analyzed during this study are
available from the corresponding author on reasonable request.
Authors' contributions
YW contributed to the conception and design of the
work. MK, LZ, SW and YZ collected the data and wrote the original
draft. MK, MY and YW contributed to the interpretation of data. YW
revised the manuscript. SW and YW confirm the authenticity of all
the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of First Affiliated Hospital of Anhui Medical University,
Hefei, China (approval no. PJ2023-10-39).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of anonymized data and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Li J, Xu J, Zheng Y, Gao Y, He S, Li H,
Zou K, Li N, Tian J, Chen W and He J: Esophageal cancer:
Epidemiology, risk factors and screening. Chin J Cancer Res.
33:535–547. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cancer Genome Atlas Research Network;
Analysis Working Group: Asan University; BC Cancer Agency; Brigham
and Women's Hospital; Broad Institute; Brown University; Case
Western Reserve University; Dana-Farber Cancer Institute; Duke
University, et al, . Integrated genomic characterization of
oesophageal carcinoma. Nature. 541:169–175. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shaheen O, Ghibour A and Alsaid B:
Esophageal cancer metastases to unexpected sites: A systematic
review. Gastroenterol Res Pract. 2017:16573102017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Japan Esophageal Society, . Japanese
Classification of Esophageal Cancer, 11th Edition: part I.
Esophagus. 14:1–36. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ai D, Zhu H, Ren W, Chen Y, Liu Q, Deng J,
Ye J, Fan J and Zhao K: Patterns of distant organ metastases in
esophageal cancer: A population-based study. J Thorac Dis.
9:3023–3030. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Iwase H, Indo T, Shimada M, Tsuzuki T,
Nakarai K, Kaida S, Doi R, Okeya M and Kato E: Esophageal cancer
with colonic metastasis successfully treated by chemoradiotherapy
followed by chemotherapy with S-1 and cisplatin. Int J Clin Oncol.
9:398–402. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shimada Y, Okumura T, Hojo S, Sukegawa K,
Nagata T, Hayashi S and Tsukada K: Synchronous asymptomatic colonic
metastasis from primary esophageal squamous cell carcinoma. J Surg
Case Rep. 2014:rjt1172014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hasegawa H, Oshikiri T, Yasuda T, Sumi Y,
Fujino Y, Tominaga M and Kakeji Y: Colonic metastasis after
resection of primary esophageal squamous cell carcinoma: report of
a case. Esophagus. 12:383–386. 2015. View Article : Google Scholar
|
|
10
|
Garg N, Stoehr C, Zhao YS, Rojas H and
Hsueh CT: Metastatic squamous cell carcinoma of colon from
esophageal cancer. Exp Hematol Oncol. 6:112017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fang N, Wang YL, Zeng L, Wu ZJ and Liu LL:
Colonic metastasis from esophageal squamous cell carcinoma
demonstrated with 18F-FDG PET/CT. Clin Nucl Med. 42:456–457. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wiseman D, Ferri L, Lakatos PL, Fiset PO
and Bessissow T: Esophageal squamous cell carcinoma with colonic
metastases. ACG Case Rep J. 7:e003352020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen YH, Lin CY, Chen YT, Wu IC and Wang
YK: Unusual metastases of esophageal squamous cell carcinoma. Clin
Nucl Med. 47:354–356. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang Y, Dam A and Nakanishi Y: A case of
esophageal squamous cell carcinoma metastasized to the colonic
anastomotic site of right hemicolectomy. ACG Case Rep J.
9:e007332022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Astaras C, Bornand A and Koessler T:
Squamous rectal carcinoma: A rare malignancy, literature review and
management recommendations. ESMO Open. 6:1001802021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vyas N, Ahmad S, Bhuiyan K, Catalano C,
Alkhawam H, Sogomonian R, Nguyen J, Walfish A and Aron J: Primary
squamous cell carcinoma of the rectum: A case report and literature
review. J Community Hosp Intern Med Perspect. 6:317082016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Williams GT, Blackshaw AJ and Morson BC:
Squamous carcinoma of the colorectum and its genesis. J Pathol.
129:139–147. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Amin AA, Reddy A, Jha M and Prasad K:
Rectal metastasis from breast cancer: An interval of 17 years. BMJ
Case Rep. 2011:bcr01201136832011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Makker J, Karki N, Sapkota B, Niazi M and
Remy P: rare presentation of gastroesophageal carcinoma with rectal
metastasis: A case report. Am J Case Rep. 17:611–615. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Watanabe Y, Iwamoto R, Kitagawa S,
Kinoshita S, Ueno M, Mineta S, Okamoto Y, Uraoka M, Kubota H,
Higashida M, et al: A resected case of rectal metastasis from
gastric cancer. Gan To Kagaku Ryoho. 46:2378–2379. 2019.(In
Japanese). PubMed/NCBI
|
|
21
|
Wang Y, Zhu L, Xia W and Wang F: Anatomy
of lymphatic drainage of the esophagus and lymph node metastasis of
thoracic esophageal cancer. Cancer Manag Res. 10:6295–6303. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Al-Agha OM and Nicastri AD: An in-depth
look at Krukenberg tumor: An overview. Arch Pathol Lab Med.
130:1725–1730. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gollub MJ, Lefkowitz R, Moskowitz CS,
Ilson D, Kelsen D and Felderman H: Pelvic CT in patients with
esophageal cancer. AJR Am J Roentgenol. 184:487–490. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Horvat N, Carlos Tavares Rocha C, Clemente
Oliveira B, Petkovska I and Gollub MJ: MRI of rectal cancer: Tumor
staging, imaging techniques, and management. Radiographics.
39:367–387. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ajani JA, D'Amico TA, Bentrem DJ, Cooke D,
Corvera C, Das P, Enzinger PC, Enzler T, Farjah F, Gerdes H, et al:
Esophageal and esophagogastric junction cancers, version 2.2023,
NCCN clinical practice guidelines in oncology. J Natl Compr Canc
Netw. 21:393–422. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sun JM, Shen L, Shah MA, Enzinger P,
Adenis A, Doi T, Kojima T, Metges JP, Li Z, Kim SB, et al:
Pembrolizumab plus chemotherapy versus chemotherapy alone for
first-line treatment of advanced oesophageal cancer (KEYNOTE-590):
A randomised, placebo-controlled, phase 3 study. Lancet.
398:759–771. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Doki Y, Ajani JA, Kato K, Xu J, Wyrwicz L,
Motoyama S, Ogata T, Kawakami H, Hsu CH, Adenis A, et al: Nivolumab
combination therapy in advanced esophageal squamous-cell carcinoma.
N Engl J Med. 386:449–462. 2022. View Article : Google Scholar : PubMed/NCBI
|