Introduction
Cancer remains a global health challenge, posing a
formidable obstacle to increasing life expectancy. Among the
malignant tumors, lung cancer stands out as the foremost cause of
mortality, responsible for 18% of cases, and ranks second in
incidence worldwide, with 11.4% of cases (1).
The elevated mortality associated with lung cancer
can be attributed to its inherent high malignancy rate.
Additionally, the occurrence of complications further accelerates
disease progression and contributes to the mortality rate. In
individuals with cancer, infection represents the most prevalent
complication (2). Lower respiratory
tract infections occur with increased frequency in patients with
lung cancer, primarily due to factors such as airway obstruction,
mucosal surface damage and treatment-related interventions such as
radiotherapy and chemotherapy (3).
Treatment strategies for lung cancer, depending on
the disease phase, histology, genetic alterations and patient
conditions, encompass surgical intervention, radiotherapy,
chemotherapy, immunotherapy and targeted therapy, either as
standalone therapies or in combination (4,5).
Patients with early stage non-small cell lung cancer (NSCLC) who
are in otherwise good physical health often benefit from a curative
surgical resection (stage I, II and IIIA) (5). However, surgical treatment becomes
unfeasible for patients with advanced lung cancer.
Several studies have identified the causative agents
of lung infections induced by chemotherapy or radiotherapy,
including bacteria (most notably Pseudomonas aeruginosa,
Pseudomonas maltophilia and Nocardia spp), viruses
(respiratory syncytial virus, influenza viruses A and B, and
cytomegalovirus) and fungi (Aspergillus and Fusarium)
(6,7). Nevertheless, a comparative analysis of
pathogens and associated risk factors between the chemoradiotherapy
and targeted therapy groups is conspicuously lacking.
The present study therefore centers on elucidating
the impact of different lung cancer treatment modalities on
pathogenic profiles and distinct clinical characteristics in the
context of lower respiratory tract infections. Through a
retrospective analysis, the clinical and pathogenic attributes of
lung cancer coexisting with lower respiratory tract infections is
examined in the targeted therapy and chemoradiotherapy cohorts. The
insights gleaned from this investigation have the potential to
furnish a theoretical foundation for clinical interventions and
play a pivotal role in guiding the judicious selection of
antibacterial agents.
Materials and methods
Study population
The present retrospective analysis included 93
patients who were diagnosed with advanced lung cancer and
concurrent lower respiratory tract infection between January 1,
2019, and December 1, 2021. All patients were included from the
North China University of Science and Technology Affiliated
Hospital (Tangshan, China). Patients were categorized into two
groups based on their tumor treatment protocols: The targeted
therapy group, which received targeted lung cancer drugs
exclusively, and the chemoradiotherapy group, consisting of
patients treated with chemotherapy, radiotherapy or a combination
of both, with or without concurrent targeted therapy.
Tumor-Node-Metastasis staging (8th edition) was employed to
determine lung cancer staging (8).
Inclusion criteria
The inclusion criteria for the study were as
follows: i) An age ≥18 years; ii) a confirmed pathological
diagnosis of advanced lung cancer; iii) patients who received
appropriate antitumor therapy, including radiotherapy, chemotherapy
and targeted agents, but not immunotherapy; and iv) the
availability of complete clinical information.
Exclusion criteria
The exclusion criteria for the study were as
follows: i) The presence of autoimmune or immunodeficiency
diseases; ii) the coexistence of other systemic infections; iii)
concurrent systemic tumors; iv) unclear pathogenetic test results;
and v) the presence of severe complications and syndromes.
Clinical indicators and pathogenetic
features
Clinical information encompassed age, sex, smoking
and drinking history, pathological type, underlying diseases and
the duration of hospitalization. Nutritional and Biochemical
indicators included body mass index (BMI), hemoglobin (Hb) level,
lymphocyte count, and albumin (ALB), alanine aminotransferase (ALT)
and creatinine (Cr) levels. Infection indicators were erythrocyte
sedimentation rate (ESR), hypersensitive C-reactive protein
(hs-CRP), procalcitonin (PCT) and the percentage of neutrophils
(NEU%). Pathogenetic indicators consisted of serology, general
bacterial culture identification results and fungal culture
identification results, as analyzed using the Guide to Utilization
of the Microbiology Laboratory for Diagnosis of Infectious Diseases
for specimen retention, submission and interpretation (9). All indicators and data were collected
from hospital records.
Statistical analysis
Data analysis was performed using SPSS 22.0
statistical software (IBM Corp.). Normally distributed data are
presented as mean ± standard deviation, and non-normally
distributed data are expressed as median (interquartile range). The
unpaired t-test was employed for between-group comparisons when
data adhered to the normal distribution, while the Mann-Whitney
rank sum test was utilized for non-normally distributed data. Count
data are presented as n (%), and intergroup comparisons were
conducted using the χ2 test or Fisher's exact test.
P<0.05 was used to indicate a statistically significant
difference.
Results
General data comparison between
groups
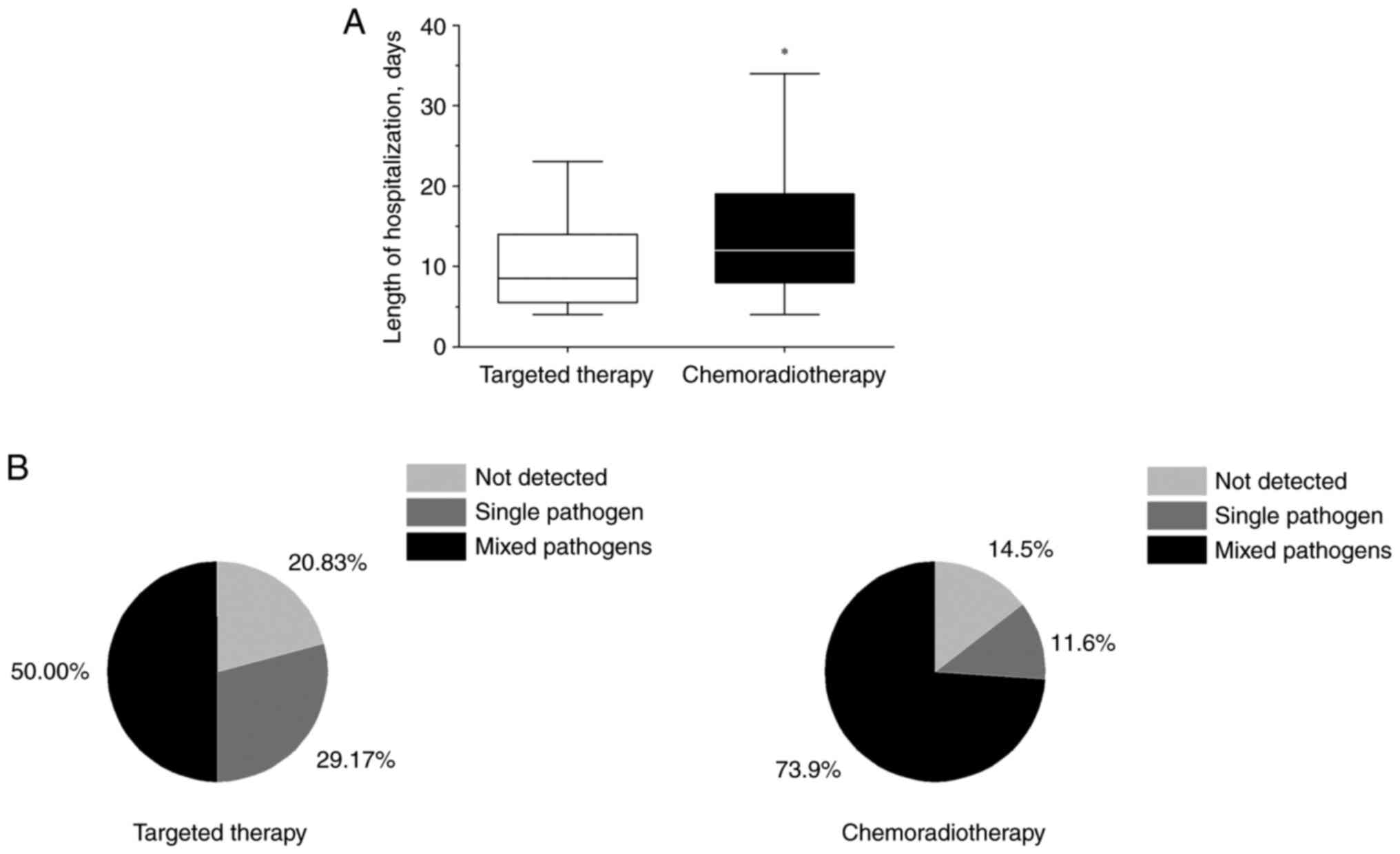
In the present study, a total of 93 cases were
included, with 24 in the targeted therapy group and 69 in the
chemoradiotherapy group. In the targeted therapy group, the median
length of hospitalization was 8.5 days (interquartile range,
5.25–14 days), while in the chemoradiotherapy group it was 12 days
(interquartile range, 8–19 days). Significant differences were
observed between the groups in terms of length of hospitalization
(P<0.05) (Fig. 1A). Notably, the
targeted therapy group exhibited a shorter hospital stay compared
with the chemoradiotherapy group. All patients treated with
targeted therapy had NSCLC, while 18 patients with
chemoradiotherapy had SCLC and 51 patients had NSCLC (P<0.05)
(Table I). Conversely, no
statistically significant differences were identified between the
two groups with regard to age, sex, BMI, alcohol consumption and
underlying diseases (P>0.05) (Table
I).
 | Table I.Clinical characteristics. |
Table I.
Clinical characteristics.
| Characteristic | Targeted therapy
(n=24) | Chemoradiotherapy
(n=69) | P-value |
|---|
| Mean age ± SD,
years | 65.21±6.21 | 64.88±8.23 | 0.86 |
| Sex, n (%) |
|
|
|
| Male | 16 (66.67) | 50 (72.46) | 0.59 |
|
Female | 8 (33.33) | 19 (27.54) | 0.59 |
| Mean BMI ± SD | 22.22±3.34 | 23.58±3.30 | 0.09 |
| Positive history of
alcohol consumption, n (%) | 6 (25.00) | 29 (42.03) | 0.14 |
| Pathology, n (%) |
|
|
|
| SCLC | 0 | 18 (26.09) | 0.01 |
|
NSCLC | 24 (100.00) | 51 (73.91) | 0.01 |
| Underlying diseases,
n (%) |
|
|
|
| Coronary
heart disease | 8 (33.33) | 14 (20.29) | 0.19 |
| COPD | 2 (8.33) | 4 (5.80) | 1.00 |
|
Cerebrovascular disease | 4 (16.67) | 17 (24.64) | 0.60 |
|
Diabetes | 5 (20.83) | 14 (20.29) | 0.96 |
|
Hypertensive disease | 11 (45.83) | 26 (37.68) | 0.48 |
Nutritional and biochemical indicator
comparisons
A significant difference was observed between the
two groups in terms of lymphocyte count (P<0.05). Specifically,
the targeted therapy group displayed a lymphocyte count of
1.86×109/l, while the chemoradiotherapy group had a
count of 0.99×109/l. Conversely, there were no
statistically significant differences between the two groups in
terms of Hb, ALB, ALT and Cr (P>0.05) (Table II).
 | Table II.Biochemical variables. |
Table II.
Biochemical variables.
| Variable | Targeted therapy
(n=24) | Chemoradiotherapy
(n=69) | P-value |
|---|
| Hb, g/l | 124.75±17.23 | 130.13±17.02 | 0.19 |
| Lymphocyte count
(×109/l) | 1.86
(1.00–2.41) | 0.99
(0.62–1.96) | 0.04 |
| ALB, g/l | 37.94±5.80 | 39.40±4.63 | 0.23 |
| ALT, U/l | 15
(12.25–33.75) | 17
(13.00–29.00) | 0.70 |
| Cr, µmol/l | 62.5
(44.00–79.25) | 62
(50.00–78.5) | 0.95 |
Infection indicator comparisons
No statistically significant differences were
detected between the two groups for ESR, hs-CRP, PCT and NEU%
(P>0.05) (Table III).
 | Table III.Infection indicators. |
Table III.
Infection indicators.
| Indicator | Targeted therapy
(n=24) | Chemoradiotherapy
(n=69) | P-value |
|---|
| ESR | 80
(25.50–94.00) | 55
(32.50–82.00) | 0.27 |
| hs-CRP | 47.71
(10.56–75.20) | 21.40
(6.10–74.30) | 0.46 |
| PCT | 0.08
(0.06–0.15) | 0.05
(0.03–0.10) | 0.08 |
| NEU% | 76.85
(64.60–84.73) | 69.3
(61.40–77.55) | 0.10 |
Pathogenetic indicator
comparisons
In the present study, pathogenetic testing was
conducted on a total of 93 patients, with 15 testing negative and
78 testing positive through pathogenetic culture or serum antibody
testing. The targeted therapy group exhibited 5 cases with
unspecified pathogens, while the chemoradiotherapy group had 10
such cases. Overall, a total of 152 pathogens were identified in
both groups.
Significant differences were observed between the
two groups regarding fungal infections (P<0.05), with a higher
prevalence in the chemoradiotherapy group compared with that in the
targeted therapy group (Table IV).
However, no statistically significant differences were noted
between the two groups in terms of viruses, Gram-negative bacteria,
Gram-positive bacteria, atypical pathogens and Mycobacterium
tuberculosis/non-tuberculous mycobacteria (P>0.05) (Table IV). In the targeted therapy group,
20.83% of results were recorded as not detected, a single pathogen
accounted for 29.17% and mixed pathogens accounted for 50%. In the
chemoradiotherapy group, 14.49% of results were recorded as not
detected, while a single pathogen accounted for 14.49% and mixed
pathogens accounted for 73.92%. There were more single-pathogen
infections in the targeted therapy group than in the
chemoradiotherapy group (P<0.05), while the chemoradiotherapy
group exhibited a higher incidence of mixed-pathogen infections
than the targeted therapy group (P<0.05) (Fig. 1B).
 | Table IV.Pathogenic characteristics. |
Table IV.
Pathogenic characteristics.
| Characteristic | Targeted
therapy |
Chemoradiotherapy | P-value |
|---|
| Total pathogens,
n | 34 | 118 |
|
| Virus, n (%) | 4 (11.76) | 20 (16.95) | 0.36 |
|
Respiratory syncytial
viruses | 1 (2.94) | 5 (4.24) | 0.96 |
|
Parainfluenza viruses | 0 (0.00) | 1 (0.85) | >0.99 |
| A and B
viruses | 2 (5.88) | 2 (1.69) | 0.59 |
|
Cytomegaloviruses | 1 (2.94) | 0 (0.00) | 0.26 |
|
Epstein-barr virus | 0 (0.00) | 6 (5.08) | 0.33 |
|
Coxsackie virus | 0 (0.00) | 4 (3.39) | 0.60 |
|
Others | 0 (0.00) | 2 (1.69) | >0.99 |
| Gram-negative, n
(%) | 21 (61.77) | 56 (47.46) | 0.69 |
|
Klebsiella
pneumoniae | 6 (17.65) | 21 (17.80) | 0.61 |
|
Pseudomonas
aeruginosa | 3 (8.82) | 8 (6.78) | >0.99 |
|
Acinetobacter
baumannii | 4 (11.76) | 9 (7.63) | 0.92 |
|
Haemophilus
influenzae | 3 (8.82) | 4 (3.39) | 0.53 |
|
Haemophilus
parainfluenzae | 1 (2.94) | 3 (2.54) | >0.99 |
|
Escherichia coli | 2 (5.88) | 6 (5.08) | >0.99 |
|
Others | 2 (5.88) | 5 (4.24) | >0.99 |
| Gram-positive, n
(%) | 2 (5.88) | 2 (1.69) | 0.59 |
|
Streptococcus
pneumoniae | 0 (0.00) | 0 (0.00) |
|
|
Staphylococcus
aureus | 2 (5.88) | 0 (0.00) | 0.07 |
|
Staphylococcus
haemolyticus | 0 (0.00) | 2 (1.69) | >0.99 |
|
Others | 0 (0.00) | 0 (0.00) |
|
| Atypical
pathogen | 1 (2.94) | 5 (4.24) | 0.96 |
|
Mycoplasma | 1 (2.94) | 5 (4.24) | 0.96 |
|
Others | 0 (0.00) | 0 (0.00) |
|
| Mycobacterium
tuberculosis/NTM | 0 (0.00) | 1 (0.85) | >0.99 |
| Fungi, n (%) | 6 (17.65) | 34 (28.81) | 0.04 |
|
Candida albicans | 4 (11.76) | 23 (19.49) | 0.20 |
|
Aspergillus | 1 (2.94) | 4 (3.39) | >0.99 |
|
Penicillium | 1 (2.94) | 4 (3.39) | >0.99 |
|
Others | 0 (0.00) | 3 (2.54) | 0.57 |
Discussion
Lung cancer is broadly categorized into SCLC and
NSCLC (10). The treatment
approaches for these two categories differ (11,12).
Among the various treatment modalities for advanced lung cancer,
targeted therapy and chemoradiotherapy are the most frequently
employed. Targeted drugs for cancer treatment can be classified
into two main categories (13): The
first category involves targeted antitumor angiogenesis, which
includes monoclonal antibodies against vascular endothelial growth
factor (VEGF) and endothelial inhibitors. These drugs function by
impeding tumor neo-angiogenesis, thereby inhibiting the growth,
proliferation and metastasis of tumor cells. An example of a
VEGF-targeted therapy is bevacizumab. While studies have generally
demonstrated the safety of bevacizumab combination therapy, it is
essential to note potential adverse events such as high blood
pressure or pulmonary hemorrhage (14). Bevacizumab reduces VEGF levels,
affecting endothelial repair and potentially weakening blood
vessels, thereby increasing the risk of rupture (15). The second category comprises small
molecules that act on the tumor cell signal transduction pathway by
inhibiting key components, effectively halting the proliferation of
tumor cells. Pathway-targeted therapy is particularly suitable for
patients with driver mutations and is associated with minimal
adverse effects, although it may be prone to secondary resistance.
In stage IV NSCLC, chemotherapy is commonly employed.
Chemotherapeutic drugs leverage the higher mitogenic activity of
tumor cells compared with host cells, rendering them more toxic to
tumors. The choice of medication is determined based on the
patient's physical condition, as indicated by their performance
status scores (16). However,
chemotherapy is associated with a relatively short survival period,
and patients treated with platinum-containing two-drug chemotherapy
typically survive for only 8–10 months. Cross-resistance is also a
consideration in this context (16). Radiotherapy constitutes a crucial
treatment modality for NSCLC, applicable as adjuvant or neoadjuvant
therapy across all stages of the disease (17).
Patients with lung cancer who have compromised
immune systems are susceptible to lower respiratory tract
infections. Thus, understanding the pathogenic and clinical aspects
of these infections is crucial for guiding the selection of
appropriate antimicrobial agents.
The present study identified a significant disparity
in case types between the two groups. Specifically, the targeted
therapy group exclusively comprised NSCLC cases, whereas the
chemoradiotherapy group consisted of 51 NSCLC cases and 18 SCLC
cases. This aligns with the existing literature indicating that
NSCLC is more prevalent than SCLC (18). It is important to note that targeted
therapy primarily focuses on NSCLC due to genetic mutations and
rearrangements (18). Consequently,
the SCLC patients in the present study did not receive targeted
therapies.
Additionally, a statistically significant difference
in lymphocyte count was observed between the two groups, with the
chemoradiotherapy group exhibiting lower lymphocyte levels.
Lymphocyte levels are indicative of systemic immune status and
inflammatory response, with reduced levels signifying
immunodeficiency (19,20).
Cytotoxic chemotherapeutic agents have the capacity
to directly or indirectly eliminate immune effector cells. Direct
impairment of immune cells by chemotherapy results in a reduction
of overall immune function (21).
The abrupt destruction of a substantial number of tumor cells
induced by chemotherapy leads to the release of significant amounts
of tumor antigens. This release, in turn, causes damage to effector
T cells. Radiotherapy, on the other hand, has the capability to
target and eliminate various immune cells in the body, including
CD4+ and CD8+ cells, contributing to a
decline in overall immune function. Within the tumor
microenvironment, CD8+ T cells play a pivotal role in
antitumor defense, while CD4+ T cells impede blood
vessel formation, hindering tumor progression (22,23).
Before the initiation of radiotherapy and chemotherapy, absolute
levels of natural killer (NK) cells and intracellular interferon-γ
levels are notably higher (24).
Therefore, managing advanced lung cancer concurrent with lower
respiratory tract infections is paramount for improving the patient
prognosis.
The present analysis of pathogenetic characteristics
revealed noteworthy differences between the two groups. Notably,
the pathogens causing lower respiratory tract infections in
patients with advanced lung cancer differed significantly from
those found in community-acquired pneumonia. Both groups exhibited
a high rate of Gram-negative bacterial infections, necessitating
empirical Gram-negative bacterial coverage in antibiotic selection.
Klebsiella pneumoniae was the most commonly isolated
pathogen in both groups and is a leading cause of sepsis,
bacteremia and abscess formation (25). Acinetobacter baumannii was
the second most common pathogen, with a higher detection rate in
the targeted therapy group than the chemoradiotherapy group.
Previous studies have associated Acinetobacter baumannii
with radiation pneumonitis in patients with cancer (26), and its presence indicates an
increased likelihood of mortality (27).
In addition, in the present study, both groups
showed a high detection rate of fungi, with significantly more
cases in the chemoradiotherapy group. Candida albicans was
the most frequent fungal infection in both groups, particularly in
immunocompromised hosts. Factors contributing to fungal infections
in lung cancer patients include underlying diseases,
immunodeficiency, prolonged use of broad-spectrum antibiotics and
glucocorticoid therapy during chemotherapy (28). Therefore, clinicians should consider
antifungal therapy when patients with advanced lung cancer and
lower respiratory tract infections do not respond to broad-spectrum
antibiotics.
Viral infections were less common in the present
study, likely due to the timeframe of the study, which did not
encompass the COVID-19 pandemic (29). However, it is important to note that
COVID-19 infections among patients with lung cancer have increased
significantly since 2023 (30).
Respiratory syncytial viruses, influenza A and B viruses, and
epstein-barr virus were the predominant viruses detected in the
present study. Awareness of viral infections, particularly
COVID-19, is crucial in patients with advanced lung cancer and
lower respiratory tract infections.
Mixed infections were prevalent in both groups in
the present study, consistent with previous findings by Qiao et
al (31). These polymicrobial
infections significantly impact quality of life and lead to severe
morbidity. The primary pattern of mixed infections involved a
combination of Gram-negative bacteria and fungi. The
chemoradiotherapy group exhibited fewer single infections, which
was possibly associated with host factors. Studies have shown that
peripheral blood leukocyte and neutrophil levels are significantly
reduced in patients treated with chemoradiotherapy, and bone marrow
haematopoiesis is impaired, resulting in decreased immune function
(32). Prolonged hospitalization
was observed in the chemoradiotherapy group following the
occurrence of lower respiratory tract infections.
The small sample size, the absence of lymphocyte
classification tests, and the absence of NK cell and leukocyte data
are limitations of the present study. Blood specimens were not
preserved from the collected patient samples, and routine
lymphocyte classification tests are not standard in hospital
procedures, contributing to the inadequacy of this data segment.
Patients receiving chemoradiotherapy exhibited a poorer overall
prognosis for lower respiratory tract infections compared with
those individuals receiving targeted therapy alone. These patients
were also more susceptible to multiple infections and
drug-resistant Gram-negative bacilli co-infections. Routine
bacterial and fungal studies should be considered in specialized
populations to improve patient management. The findings of the
present study provide valuable insights for the appropriate
selection of empiric antibiotics and antifungal agents in severely
ill patients.
Acknowledgements
Not applicable.
Funding
The present study was funded by a grant from Basic Research
Operating Expenses of Universities in Hebei Province (grant no.
JQN2021028).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
DZ and YH designed the research and revised the
manuscript. DZ and JD collected data and drafted the manuscript. JJ
performed the data analysis. HZ designed the research and revised
the manuscript critically for important intellectual content. DZ
and YH confirm the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The Ethics Committee of North China University of
Science and Technology Affiliated Hospital (Tangshan, China)
approved this study (approval no. 20221108017).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rolston KV: Infections in cancer patients
with solid tumors: A review. Infect Dis Ther. 6:69–83. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Honda Y: Lung cancer and respiratory
infections. Gan To Kagaku Ryoho. 47:750–753. 2020.(In Japanese).
PubMed/NCBI
|
|
4
|
Patel B and Priefer R: Impact of chronic
obstructive pulmonary disease, lung infection, and/or inhaled
corticosteroids use on potential risk of lung cancer. Life Sci.
294:1203742022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Alexander M, Kim SY and Cheng H: Update
2020: Management of non-small cell lung cancer. Lung. 198:897–907.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vento S, Cainelli F and Temesgen Z: Lung
infections after cancer chemotherapy. Lancet Oncol. 9:982–992.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Guckenberger M, Belka C, Bezjak A, Bradley
J, Daly ME, DeRuysscher D, Dziadziuszko R, Faivre-Finn C, Flentje
M, Gore E, et al: Practice recommendations for lung cancer
radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus
statement. Radiother Oncol. 146:223–229. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goldstraw P, Chansky K, Crowley J,
Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P,
Mitchell A, Bolejack V, et al: The IASLC lung cancer staging
project: Proposals for revision of the TNM stage groupings in the
forthcoming (eighth) edition of the TNM classification for lung
cancer. J Thorac Oncol. 11:39–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Miller JM, Binnicker MJ, Campbell S,
Carroll KC, Chapin KC, Gilligan PH, Gonzalez MD, Jerris RC, Kehl
SC, Patel R, et al: A guide to utilization of the microbiology
laboratory for diagnosis of infectious diseases: 2018 update by the
Infectious Diseases Society of America and the American Society for
Microbiology. Clin Infect Dis. 67:e1–e94. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Travis WD, Brambilla E, Burke AP, Marx A
and Nicholson AG: Introduction to the 2015 World Health
Organization classification of tumors of the lung, pleura, thymus,
and heart. J Thorac Oncol. 10:1240–1242. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Reinmuth N and Hoffmann H: Small Cell Lung
Cancer. TumorDiagnostik & Therapie. 43:307–320. 2022.(In
German).
|
|
12
|
Zhong J, Bai H, Wang Z, Duan J, Zhuang W,
Wang D, Wan R, Xu J, Fei K, Ma Z, et al: Treatment of advanced
non-small cell lung cancer with driver mutations: Current
applications and future directions. Front Med. 17:18–42. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Iijima Y, Bandow K, Sano M, Hino S, Kaneko
T, Horie N and Sakagami H: In vitro assessment of antitumor
potential and combination effect of classical and
molecular-targeted anticancer drugs. Anticancer Res. 39:6673–6684.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Piperdi B, Merla A and Perez-Soler R:
Targeting angiogenesis in squamous non-small cell lung cancer.
Drugs. 74:403–413. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kamba T and McDonald D: Mechanisms of
adverse effects of anti-VEGF therapy for cancer. Br J Cancer.
96:1788–1795. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zappa C and Mousa SA: Non-small cell lung
cancer: Current treatment and future advances. Transl Lung Cancer
Res. 5:288–300. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Uzel EK, Figen M and Uzel Ö: Radiotherapy
in lung cancer: Current and future role. Sisli Etfal Hastan Tip
Bul. 53:353–360. 2019.PubMed/NCBI
|
|
18
|
Howlader N, Noone A, Krapcho Me, Miller D,
Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, et al:
SEER cancer statistics review, 1975–2016. National Cancer
Institute; Bethesda, MD: 2019, https://seer.cancer.gov/csr/1975_2016/September
18–2023
|
|
19
|
Chen W, Zhong S, Shan B, Zhou S, Wu X,
Yang H and Ye S: Serum D-dimer, albumin and systemic inflammatory
response markers in ovarian clear cell carcinoma and their
prognostic implications. J Ovarian Res. 13:892020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dunn GP, Old LJ and Schreiber RD: The
immunobiology of cancer immunosurveillance and immunoediting.
Immunity. 21:137–148. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schiavoni G, Sistigu A, Valentini M,
Mattei F, Sestili P, Spadaro F, Sanchez M, Lorenzi S, D'Urso MT,
Belardelli F, et al: Cyclophosphamide synergizes with type I
interferons through systemic dendritic cell reactivation and
induction of immunogenic tumor apoptosis. Cancer Res. 71:768–778.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kadakia KC, Symanowski JT, Aktas A,
Szafranski ML, Salo JC, Meadors PL and Walsh D: Malnutrition risk
at solid tumor diagnosis: The malnutrition screening tool in a
large US cancer institute. Support Care Cancer. 30:2237–2244. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mozaffari F, Lindemalm C, Choudhury A,
Granstam-Björneklett H, Helander I, Lekander M, Mikaelsson E,
Nilsson B, Ojutkangas ML, Osterborg A, et al: NK-cell and T-cell
functions in patients with breast cancer: Effects of surgery and
adjuvant chemo-and radiotherapy. Br J Cancer. 97:105–111. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sun XY, Lin Y, Guo W and Yin XM:
Prognostic value of the geriatric nutritional risk index in
patients with non-small cell lung cancer: A meta-analysis. Nutr
Cancer. 74:3623–3633. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Worku M, Belay G and Tigabu A: Bacterial
profile and antimicrobial susceptibility patterns in cancer
patients. PLoS One. 17:e02669192022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mei T, Yang X, Yu Y, Tian X, Deng Q, Xu Y,
Zhou L, Zhou X, Liu Y, Zou B, et al: Secondary infections after
diagnosis of Severe Radiation Pneumonitis (SRP) among patients with
non-small cell lung cancer: Pathogen distributions, choice of
empirical antibiotics, and the value of empirical antifungal
treatment. Int J Radiat Oncol Biol Phys. 112:179–187. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Freire MP, de Oliveira Garcia D, Garcia
CP, Campagnari Bueno MF, Camargo CH, Kono Magri ASG, Francisco GR,
Reghini R, Vieira MF, Ibrahim KY, et al: Bloodstream infection
caused by extensively drug-resistant Acinetobacter baumannii in
cancer patients: High mortality associated with delayed treatment
rather than with the degree of neutropenia. Clin Microbiol Infect.
22:352–358. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhu Z and Zou X: Analysis of factors for
susceptibility to a pulmonary fungal infection in elderly patients
with lung cancer and the drug resistance of those fungi. J Pathog
Biol. 3:633–636. 2018.(In Chinese).
|
|
29
|
Wilson O and Flahault A: China's U-turn in
its COVID-19 policy. Anaesth Crit Care Pain Med. 42:1011972023.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Du Z, Wang Y, Bai Y, Wang L, Cowling BJ
and Meyers LA: Estimate of COVID-19 Deaths, China, December
2022-February 2023. Emerg Infect Dis. 29:2121–2124. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Qiao D, Wang Z, Lu Y, Wen X, Li H and Zhao
H: A retrospective study of risk and prognostic factors in relation
to lower respiratory tract infection in elderly lung cancer
patients. Am J Cancer Res. 5:423–432. 2015.PubMed/NCBI
|
|
32
|
Yu K, Sang QA, Lung PY, Tan W, Lively T,
Sheffield C, Bou-Dargham MJ, Liu JS and Zhang J: Personalized
chemotherapy selection for breast cancer using gene expression
profiles. Sci Rep. 7:432942017. View Article : Google Scholar : PubMed/NCBI
|