Introduction
Hepatocellular carcinoma (HCC) is the fourth leading
cause of global cancer-related mortality, and its associated death
rate is anticipated to increase persistently over the next decade
(1). HCC typically manifests as a
latent progression with inconspicuous symptoms, often resulting in
diagnosis at an advanced stage (2).
Currently, the internationally endorsed first-line therapies for
advanced liver cancer include sorafenib, lenvatinib and other
pharmaceutical drugs. The results of the IMbrave150 trial revealed
that the combination of atezolizumab and bevacizumab was more
clinically significant than sorafenib alone in terms of life,
function and disease symptoms, making it an important current
first-line treatment option (3).
Nevertheless, the efficacy of these primary interventions is
limited, frequently culminating in the emergence of drug resistance
shortly after treatment (4). In
cases where patients exhibit intolerance or encounter failure with
first-line approaches, secondary options such as regorafenib,
cabozantinib, or nivolumab monotherapy may be considered (5).
Regorafenib, an innovative oral multi-kinase
inhibitor, has demonstrated inhibitory effects on diverse protein
kinases, including those implicated in tumor angiogenesis and
tumorigenesis. It exhibited antiproliferative, antiangiogenic,
antitumor and anti-metastatic activities in rat models (6). A pivotal randomized, double-blind,
placebo-controlled phase 3 trial (7) substantiated the significant
enhancement of overall survival (OS) in patients with progressive
HCC after sorafenib treatment. Consequently, it was approved as a
pioneering second-line targeted therapy, with subsequent clinical
trials corroborating its efficacy in patients with late-stage HCC
(8).
Research posits that regorafenib plus programmed
death-1 (PD-1) inhibitors augment survival benefits for patients
with late-stage HCC compared with that for those undergoing
regorafenib monotherapy (9). The
underlying mechanism lies in regorafenib's facilitation of the
antitumor immune response of PD-1 inhibitors by modulating the
IFN-γ/NSDHL/SREBP1/TGF-β1 axis (10). In a murine liver cancer model, this
combined approach substantially elevated the expression of CXCL10
in HCC cells, fostering the normalization of the tumor vascular
system and amplifying the infiltration of CXCR3+CD8 T
cells, thereby effectively impeding tumor growth (11).
In practical clinical settings, the amalgamation of
regorafenib with PD-1 inhibitors is progressively gaining traction
as a second-line treatment for late-stage HCC. However, reported
cases remain limited (12), and
comprehensive investigations examining the relative efficacy and
safety of these treatment modalities are currently lacking.
Therefore, the objective of the present meta-analysis was to
compare the efficacy and safety of regorafenib with or without PD-1
inhibitors as second-line therapy in advanced-stage HCC. The
present study aimed to provide a thorough basis for clinical
decision-making.
Materials and methods
Search strategy
To gather the pertinent literature, a thorough
investigation of PubMed (https://pubmed.ncbi.nlm.nih.gov/), Embase (https://www.embase.com), Web of Science (https://webofscience.com) and Cochrane Library
(https://www.cochranelibrary.com/)
databases was conducted in October 2023. The search strategy was
not limited by language or other factors (Table SI). The utilized keywords
encompassed ‘liver neoplasms’, ‘hepatocellular carcinoma’,
‘regorafenib’. ‘Stivarga’, ‘immune checkpoint inhibitors’,
‘programmed death-1’, and ‘PD-1’. The research design and
implementation adhered to the guidelines established by the
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
(13).
Inclusion and exclusion criteria
Inclusion criteria were as follows: i) Population:
Patients with advanced HCC who failed first-line therapy
(sorafenib, lenvatinib, pabolizumab, atezolizumab + bevacizumab).
These patients had Eastern Cooperative Oncology Group Performance
Status scores ranging from 0 to 1; ii) the study encompassed either
prospective or retrospective clinical investigations; and iii) the
intervention administered to the participants in blue could be
regorafenib or a treatment referred to as R-P.4. The outcomes
assessed included OS, progression-free survival (PFS), objective
response rate (ORR), disease control rate (DCR) and occurrence of
adverse events (AE).
Exclusion criteria were as follows: i) Any malignant
tumor other than HCC, current or historical; ii) use of alternative
targeted medications aside from regorafenib in second-line therapy;
iii) non-clinical studies, including case reports, reviews,
meta-analyses, systematic reviews, letters, guidelines and basic
experiments; and iv) studies lacking sufficient resulting data or
in which data extraction is not feasible.
Data extraction
The authors Zhao Li and Jie Wang individually
reviewed the literature, collected data and cross-verified the data
using a standardized protocol after obtaining the relevant
articles. Endnote X9 software was used for literature review.
Disagreements were resolved through discussion or by referring to
the opinions of a third author. The extracted information included
the first author's name, publication year, racial composition of
the study population, study design, sample size, patient numbers,
and clinical outcomes, such as survival, tumor control and adverse
reactions. If crucial information was missing, the corresponding
author was contacted via email to obtain unpublished data.
Literature quality assessment
The cohort studies included in this meta-analysis
were independently assessed by two authors using the
Newcastle-Ottawa Scale. Subsequently, they engaged in discussions
to establish a consensus. The scores assigned to the
Newcastle-Ottawa Scale ranged from zero to nine, where scores
between one and five were indicative of low quality and scores
between six and nine signified high quality.
Statistical analysis and bias
assessment
Stata/MP software version 17.0 (StataCorp LP) was
used for statistical analysis. Hazard ratios (HR) and their
corresponding 95% confidence intervals (CI) were used as the
primary outcome measures (OS and PFS), with the log HR and its
variance summarized using inverse variance-weighted averages.
Secondary outcome measures (ORR, DCR and AE) were represented using
relative risk (RR) and their corresponding 95% CI. To assess the
heterogeneity of the included studies, Q-tests and
I2-tests were used (14). If there was no heterogeneity
(P>0.05 or I2<50%), a fixed-effects model was used
for meta-analysis. Otherwise, a random effects model was used.
Sensitivity analysis was conducted by sequentially excluding each
study. Potential publication bias was evaluated using Egger's and
Begg's tests.
Results
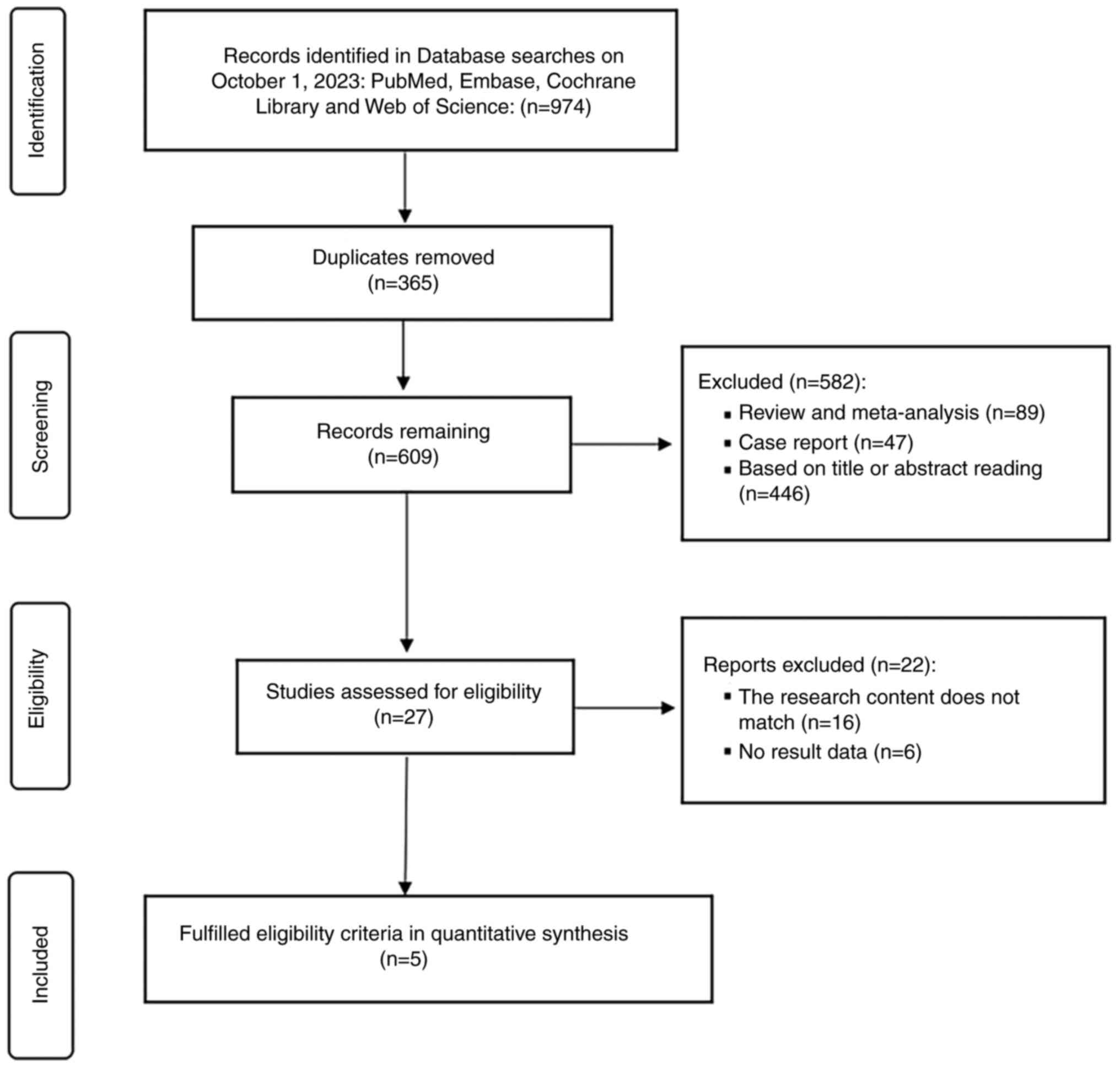
Literature search and selection
A preliminary search of these four databases yielded
974 articles. After automated and manual checks, 365 duplicate
studies, 136 meta-analyses, systematic reviews and case reports
were excluded. The remaining articles underwent independent title
and abstract reviews by two authors, resulting in a detailed
examination of the full text of the 27 studies that aligned with
the research criteria. A total of 16 studies were excluded with
inconsistent content and six studies without sufficient outcome
data. Finally, the meta-analysis included five articles (15–19).
The Preferred Reporting Items for Systematic Reviews and
Meta-Analyses flowchart illustrating the process of including the
studies in the analysis is displayed in Fig. 1.
Study characteristics and quality
assessment
All five studies included in the analysis were
conducted in China and were retrospective cohort studies. These
studies encompassed a total of 444 patients with advanced HCC. The
regorafenib plus programmed death-1 inhibitors (R-P) and
regorafenib groups comprised 270 and 174 patients, respectively.
The decision to use monotherapy or combination therapy for
regorafenib is primarily determined by the attending physician in
consultation with the patient, taking into consideration the
patient's condition. There was no statistical difference in
baseline clinical characteristics between the two groups in the
five studies, which was comparable. Except for the study by Tu
et al (19), which included
two patients with Child-Pugh class C HCC in both the regorafenib
and R-P groups, all other patients had a Child-Pugh score of A-B.
The basic characteristics of the included studies are summarized in
Table I. In terms of quality
assessment, all five retrospective cohort studies were rated as
high-quality (Table II).
 | Table I.Demographic characteristics of
included studies. |
Table I.
Demographic characteristics of
included studies.
| Study | Country | Study type | Treatment | Sample size | Age, years | Male | HBV positive | AFP (<400
ng/ml) | Child-Pugh class
A | BCLC stage B | ECOG PS 0 | PVTT | EHM | (Refs.) |
|---|
| Huang et al
2022 | China | RCS | R-P | 58 | 54
(41–62)a | 51 | 48 | NA | 37 | NA | 35 | 40 | 37 | (15) |
|
|
|
| R | 55 | 51
(47–63)a | 50 | 49 | NA | 35 | NA | 27 | 31 | 29 |
|
| Li et al
2023 | China | RCS | R-P | 38 |
51.2±10.3b | 28 | 30 | 17 | NA | 8 | 23 | 27 | 14 | (16) |
|
|
|
| R | 32 |
53.3±13.1b | 26 | 27 | 30 | NA | 11 | 17 | 19 | 15 |
|
| Liu et al
2022 | China | RCS | R-P | 48 | 54
(47–60)a | 39 | 33 | 29 | NA | 8 | 29 | 11 | 39 | (17) |
|
|
|
| R | 30 | 55
(47–61)a | 27 | 23 | 15 | NA | 7 | 20 | 6 | 23 |
|
| Yan et al
2023 | China | RCS | R-P | 94 | 55.5
(48.0–62.7)a | 85 | NA | NA | 65 | 16 | 37 | 46 | 47 | (18) |
|
|
|
| R | 39 | 58
(51.5–63.0)a | 34 | NA | NA | 27 | 5 | 16 | 15 | 22 |
|
| Tu et al
2022 | China | RCS | R-P | 32 | 50.3
(34.4–69.0)a | 29 | 30 | 16 | 23 | 4 | 9 | 10 | 28 | (19) |
|
|
|
| R | 18 | 53
(34.4–71.0)a | 14 | 18 | 4 | 7 | 0 | 2 | 7 | 15 |
|
 | Table II.Assessment of cohort studies using
Newcastle-Ottawa scale. |
Table II.
Assessment of cohort studies using
Newcastle-Ottawa scale.
| Selection |
|
|
|
|
|
|
|---|
| Comparability |
Exposure/outcome |
|
|
|---|
| Represent
activeness of cohorts | Selection of
control cohort | Ascertainment of
exposure | Outcome not present
at start |
|
|
|
|
|---|
| Comparability of
cohort | Assessment of
outcome | Length of
follow-up | Adequacy of
follow-up | Total score | Study |
|---|
| * | * | * | * | ** | * | * |
| 8 | Huang et al
2022 (15) |
| * | * | * | * | ** | * | * |
| 8 | Li et al
2023 (16) |
| * | * | * | * | ** | * | * | * | 9 | Liu et al
2022 (17) |
| * | * | * | * | ** | * | * | * | 9 | Yan et al
2023 (18) |
| * | * | * | * | ** | * |
|
| 7 | Tu et al
2022 (19) |
Survival
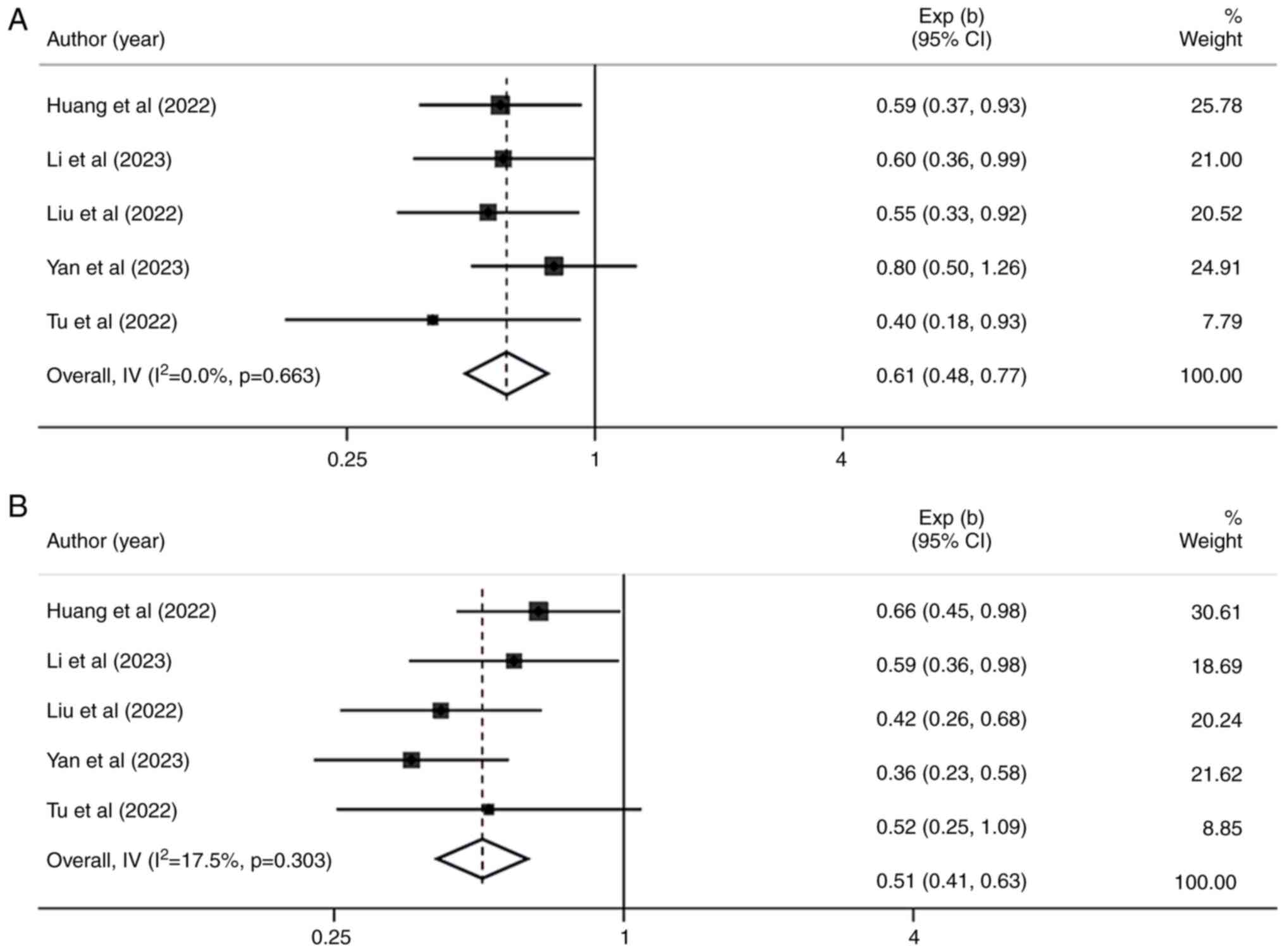
All the included studies reported differences in OS
and PFS between the two groups. Heterogeneity between studies was
extremely low and using a fixed-effect model analysis revealed
that, compared with regorafenib monotherapy, patients with
late-stage HCC receiving R-P treatment had an extension in OS (HR,
0.61; 95% CI, 0.48–0.77; I2=0.0%; P=0.663) (Fig. 2A). Similarly, R-P treatment improved
PFS in late-stage HCC compared with regorafenib monotherapy (HR,
0.51; 95% CI, 0.41–0.63; I2 =17.5%; P=0.303) (Fig. 2B).
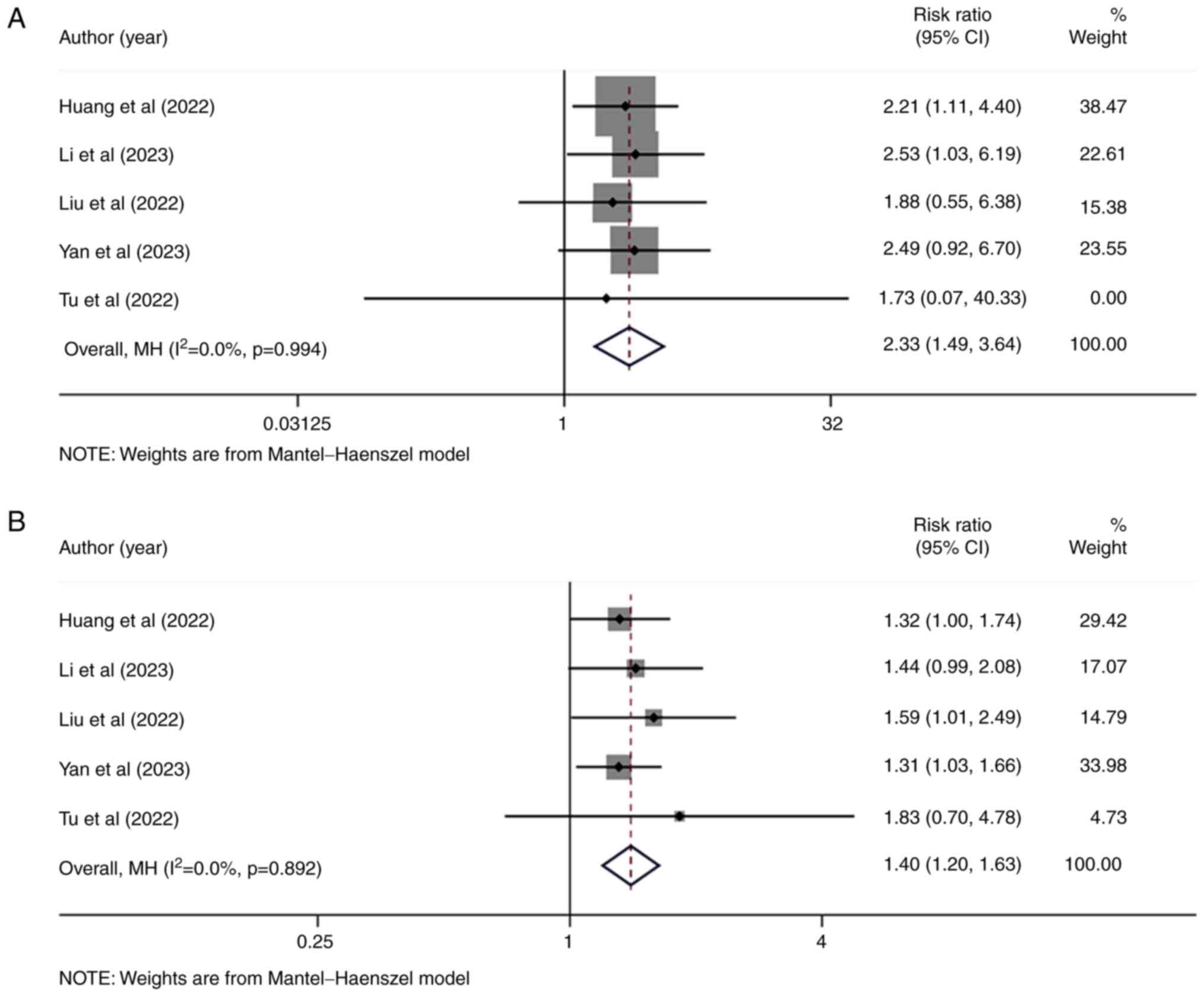
Tumor response
All five studies reported differences in objective
response and DCRs between the two treatment methods. Based on
heterogeneity test results, a fixed-effect model analysis revealed
that the ORR in the R-P group was higher than in the regorafenib
group (RR, 2.33; 95% CI, 1.49–3.64; I2=0.0%; P=0.994)
(Fig. 3A). Similarly, the DCR in
the R-P group was higher than in the regorafenib group (RR, 1.40;
95% CI, 1.20–1.63; I2=0.0%; P=0.892) (Fig. 3B). These results indicated that,
compared with regorafenib monotherapy, R-P treatment can
significantly improve tumor response in patients with late-stage
HCC.
Safety
In terms of AE, the risk of hypothyroidism, rash and
thrombocytopenia was higher with R-P treatment than with
regorafenib monotherapy. The most common AE for both regorafenib
monotherapy and R-P treatment was hand-foot skin reaction, with a
similar risk of occurrence (RR, 1.05; 95% CI, 0.80–1.38;
I2=0%; P=0.632) (Table
III).
 | Table III.Summary of treatment-related adverse
events. |
Table III.
Summary of treatment-related adverse
events.
|
|
| Rate of events
(%) |
|
|
|
|---|
|
| Number of
studies |
| Relative risk (95%
confidence interval) |
|
|
|---|
| Adverse events | R-P | Regorafenib | P-value | I2
(%) |
|---|
| Hypertension | 5 | 14.8 | 17.8 | 0.99
(0.65–1.50) | 0.391 | 2.8 |
| Diarrhea | 5 | 21.1 | 20.7 | 1.10
(0.77–1.59) | 0.867 | 0 |
| Fatigue | 5 | 22.6 | 20.1 | 1.29
(0.90–1.85) | 0.208 | 32 |
| Hand-foot skin
reaction | 5 | 32.6 | 31.6 | 1.05
(0.80–1.38) | 0.632 | 0 |
| Elevated
transaminases | 5 | 21.5 | 20.1 | 1.26
(0.88–1.79) | 0.994 | 0 |
| Hypothyroidism | 5 | 15.7 | 8.6 | 2.35
(1.36–4.05) | 0.811 | 0 |
|
Thrombocytopenia | 4 | 11.4 | 7.4 | 1.54
(0.74–3.23) | 0.918 | 0 |
| Rash | 4 | 13.4 | 6.4 | 2.59
(1.35–4.99) | 0.280 | 21.8 |
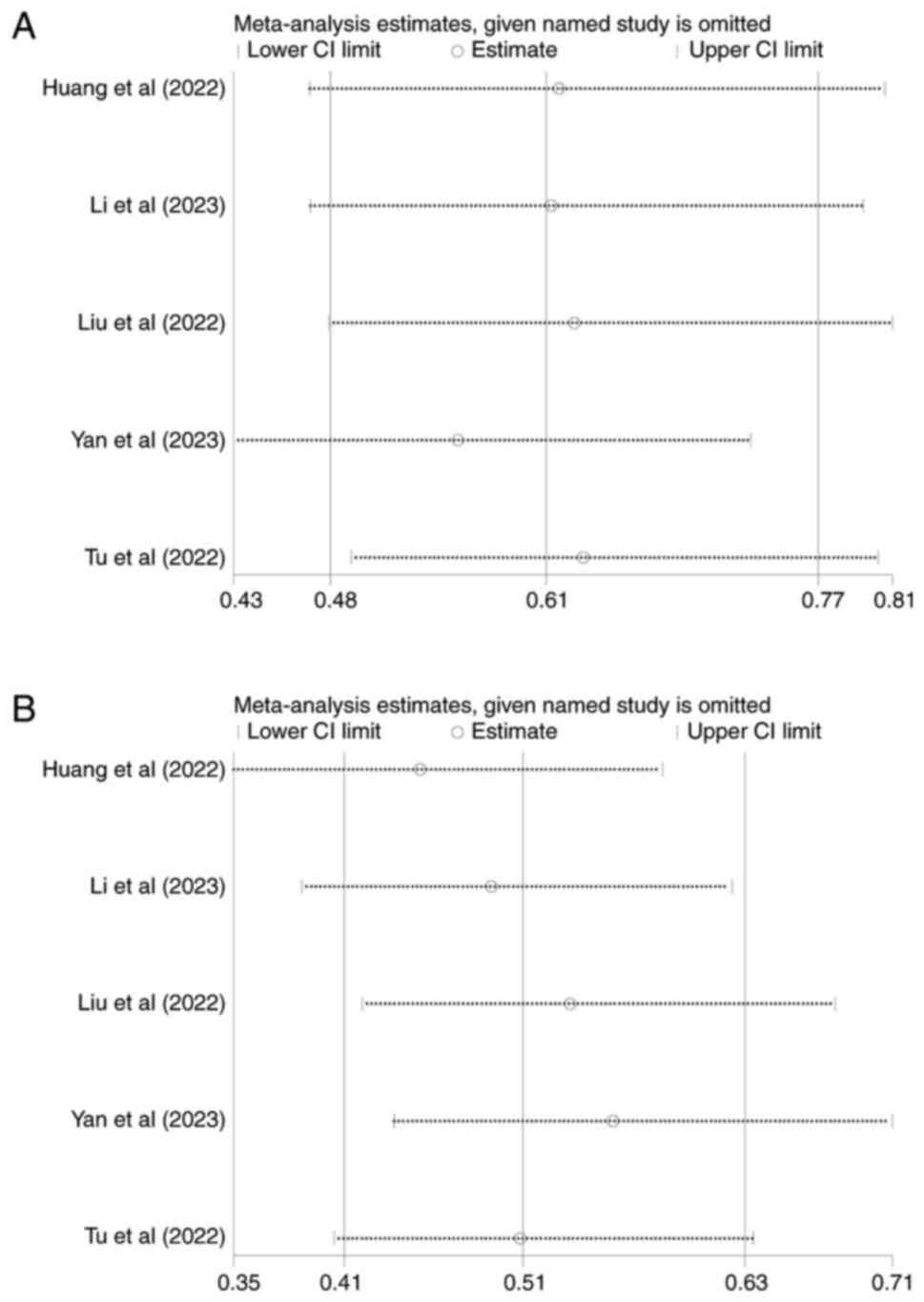
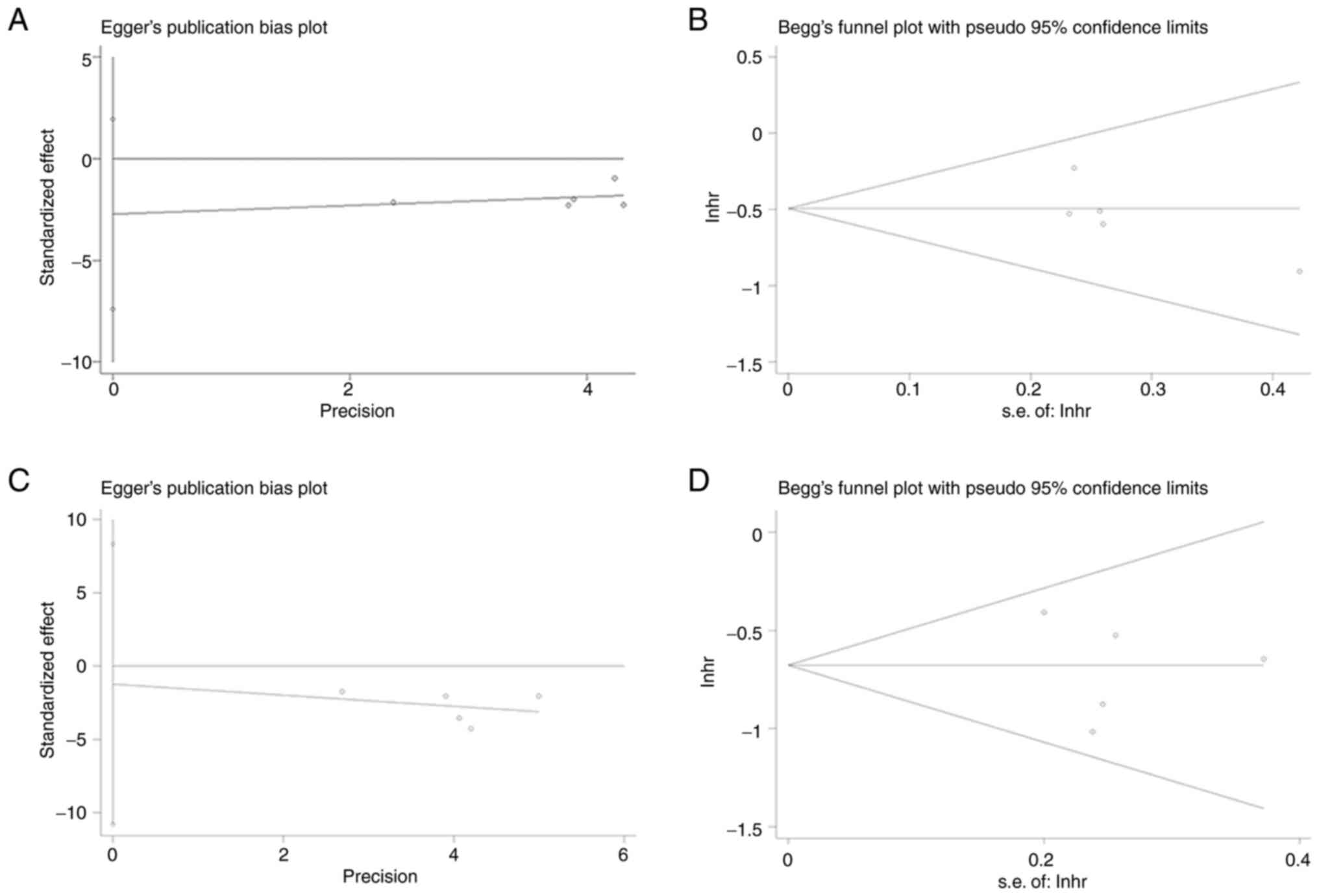
Sensitivity analysis and publication
bias
Sensitivity analyses were conducted for the primary
outcome measures (OS and PFS). The meta-analysis results remained
stable when each study was sequentially excluded as there were no
significant changes in the effect size for OS, PFS, or 95% CI
(Fig. 4). The OS and PFS tests for
publication bias indicated that there was no potential publication
bias since the P-values for Egger's test were 0.160 and 0.710,
respectively, and the P-values for Begg's test were 0.226 and
1.000, respectively (Fig. 5).
Discussion
HCC is one of the most common types of cancer
worldwide, typically diagnosed at advanced stages, necessitating
systemic treatment (20). Current
first-line therapeutic options include sorafenib, lenvatinib and
combinations of atezolizumab and bevacizumab (21). Selecting an appropriate second-line
treatment after the initial therapy fails is pivotal for enhancing
patient survival outcomes.
Second-line treatments include regorafenib,
cabozantinib and ramucirumab. Regorafenib, an oral tyrosine kinase
inhibitor, was initially approved for treating metastatic
colorectal cancer in the randomized, placebo-controlled phase 3
CORRECT trial. The trial was confirmed in an expanded Asian patient
population in the randomized, placebo-controlled, phase 3 CONCUR
trial (22). In the phase 3 CORRECT
trial, patients with metastatic colorectal cancer randomly assigned
to either regorafenib 160 mg or placebo revealed a survival
benefit, with a median OS of 6.4 months in the regorafenib group
and 5.0 months in the placebo group (23). Regorafenib was the first oral drug
approved for patients with HCC who did not respond to sorafenib.
However, owing to its lower ORR and moderate improvement in OS,
there is a clear need for a more efficacious second-line treatment
(24). There is growing hope for
the potential of immunotherapy as a second-line treatment for liver
cancer, as the results of a phase 2 clinical trial (KEYNOTE-224)
revealed that pembrolizumab is effective and well-tolerated in
patients with HCC who have failed in getting treated with sorafenib
(25). However, PD-1 inhibitor
monotherapy has a low response rate across different populations of
patients with HCC. In a phase 3 clinical trial evaluating
pembrolizumab as a second-line treatment for advanced HCC
(KEYNOTE-240), neither OS nor PFS met the predefined primary
endpoints. The publication of results from a phase III clinical
trial (26) introduced the
combination of targeted therapy and immunotherapy as a burgeoning
option, providing a fresh outlook for the second-line treatment of
advanced HCC.
The exploration of combined molecular targeted drugs
and PD-1 inhibitors has emerged as a research hotspot, yielding
encouraging results with the combination of atezolizumab and
bevacizumab (3). Regorafenib has
immunomodulatory effects (27): M1
macrophage polarization, enhanced CD8+ T cell
proliferation and activation, other than the inhibition of STAT3
activity, and increased the expression of C-X-C motif chemokine
ligand 10 in combination with anti-PD-1 agents, extending both
tumor penetration and the survival of activated CD8+ T
cells. Moreover, JAK1/2STAT1 and MAPK signals can be effectively
inhibited, and the expression of PD-L1 in tumors can be reduced,
thus improving the efficacy of PD-1 inhibitors (28). Given regorafenib's unique
therapeutic mechanisms targeting tumor cell proliferation and
spread as well as tumor angiogenesis and tumor-associated immune
evasion, combination therapy with PD-1 inhibitors is a promising
new therapeutic strategy, and several clinical trials are
investigating the efficacy and safety of combination therapy based
on regorafenib plus immune checkpoint inhibitors (29). To date, no comprehensive
meta-analysis has compared the effectiveness and safety of the two
methods.
A meta-analysis was performed to compare the
effectiveness and safety of R-P and regorafenib in patients with
advanced HCC following unsuccessful initial treatment. The results
of the present analysis revealed that, compared with regorafenib,
R-P significantly extends the survival period for patients with
advanced HCC post first-line treatment failure, while concurrently
augmenting tumor response. A recent multicenter, single-arm, phase
2 RENOBATE trial reported supportive results in treating
unresectable HCC with the combination of regorafenib and
nebuliumab, demonstrating efficacy and safety, with an ORR of 31.0%
and a median PFS of 7.38 months (30). Notably, low heterogeneity was
observed among the included studies. The investigation conducted by
Yan et al (18) found no
statistically significant differences in OS between the R-P group
and the regorafenib group (OS, 12.0 months; 95% CI, 10.0–22.0) vs.
14.0 months (95% CI, 14.0–16.0; P=0.32). This lack of significance
may be attributed to the study's nearly four-year duration, which
resulted in varying first-line treatment strategies over different
periods. For example, in the initial stages, patients mostly
received single-drug treatment with molecular-targeted drugs as the
first option, whereas patients in advanced stages primarily
underwent combination therapy involving both molecular-targeted
drugs and immune checkpoint inhibitors, which significantly
affected the experimental results. This disparity was further
confirmed by a subgroup analysis. In the investigation by Tu et
al (19), the PFS of the R-P
group exceeded that of the regorafenib group (3.7 months; 95% CI,
2.74–4.72; vs. 2.1 months; 95% CI, 1.12–3.01; P=0.078), although
the difference did not achieve statistical significance. This lack
of significance may be attributed to the continued favorable tumor
response and survival outcomes demonstrated by PD-1 inhibitors when
sequentially combined with molecular targeted drug therapies
(31). Consequently, the
administration of regorafenib within a few months of PD-1 inhibitor
failure yielded synergistic effects, thereby mitigating the
disparity between the two groups.
These findings indicated that the combination of
molecular targeted agents with PD-1 inhibitor dual therapy
surpasses molecular targeted agents' monotherapy in conferring
survival benefits and eliciting a tumor response. This conclusion
is consistent with the outcomes of the meta-analysis by Yu et
al (32), in which the
combination of lenvatinib with PD-1 inhibitors significantly
improved survival benefits and tumor response, as opposed to using
lenvatinib alone, in patients with advanced HCC. A recent
single-center study conducted at a single center (33) provided additional validation that
the combination of regorafenib and PD-1 inhibitors is highly
effective in treating patients with advanced HCC after initial
treatment failure. This treatment approach has revealed commendable
results, with an increased tumor remission rate and a low incidence
of severe AE. The residual liver function is a well-known limiting
factor for systemic therapy and its indications/contraindications.
The results of Cox univariate and multivariate analyses from three
of the five included studies indicated that Child-Pugh B is an
independent risk factor for OS. However, most of the patients
included in all studies were classified as Child-Pugh grade A,
which may be attributed to the significant difference in the number
of Child-Pugh grade A and B patients, as well as the small sample
size. Therefore, a comparison between Child-Pugh grade A and B was
not conducted. Given that both the current meta-analysis and the
aforementioned studies were based on clinical retrospective
research, these conclusions require further validation and
confirmation through large-scale prospective multicenter randomized
clinical trials. Fortunately, an ongoing prospective, multicenter,
randomized controlled clinical trial for second-line treatment of
liver cancer (34) has the
potential to provide robust supportive evidence for the efficacy of
R-P treatment.
Concerning treatment-related AE, the R-P regimen
resulted in a higher incidence of hypothyroidism, rash and
thrombocytopenia than in regorafenib monotherapy. Nevertheless, the
occurrence rates of these AEs in both groups were relatively low
and were successfully controlled by changing the dosage and
providing supportive treatment (35). No significant differences in the
risk of adverse reactions were observed between the two groups in
other categories. Based on the present analysis of all included
studies, there were no statistically significant differences in the
occurrence of severe AE (grade 3/4) between the two groups, which
further affirmed the safety profile of the R-P regimen. In summary,
R-P treatment yields clinical benefits for patients with advanced
HCC following first-line treatment failure, while maintaining a
commendable safety profile.
However, the present study has some limitations.
First, the total number of included studies was restricted, and the
sample size was relatively small, potentially impacting the
comprehensiveness of the results. Second, all the included studies
were retrospective, introducing the potential for selection bias.
Third, the PD-1 inhibitor types varied among the studies, affecting
the uniformity of the treatment approach. The fact that all PD-1
inhibitors used in the present study have been recommended for
treating HCC (36) further enhances
the authors' trust in the dependability of the findings.
In conclusion, the findings of the present study
suggested that in patients with advanced HCC after first-line
treatment failure, R-P treatment demonstrates advantages in terms
of survival benefit and tumor response compared with regorafenib
monotherapy. In addition, the adverse reactions were manageable.
Therefore, the R-P treatment regimen could emerge as a new
therapeutic option. Large-scale randomized controlled studies are
necessary to further validate the efficacy of this treatment
approach.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by the Beijing Medical Health
Public Welfare Association (grant no. XBZQ-23007).
Availability of data and materials
The data generated in the present study may be found
in the PROSPERO under the accession number CRD42024498866 or the
following URL (www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=498866).
Authors' contributions
ZLi, JW, JZ and ZL conceived and designed the study.
ZLi, JW, JZ and ZLe confirm the authenticity of all the raw data.
ZLi and JZ conducted the data collection. ZLi and JW conducted
statistical analysis. ZLi and JW played a role in interpreting the
data. ZLi and ZLe were responsible for drafting and revising the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Alawyia B and Constantinou C:
Hepatocellular carcinoma: A narrative review on current knowledge
and future prospects. Curr Treat Options Oncol. 24:711–724. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Llovet JM, Kelley RK, Villanueva A, Singal
AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J and
Finn RS: Hepatocellular carcinoma. Nat Rev Dis Primers. 7:62021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Galle PR, Finn RS, Qin S, Ikeda M, Zhu AX,
Kim TY, Kudo M, Breder V, Merle P, Kaseb A, et al: Patient-reported
outcomes with atezolizumab plus bevacizumab versus sorafenib in
patients with unresectable hepatocellular carcinoma (IMbrave150):
An open-label, randomised, phase 3 trial. Lancet Oncol.
22:991–1001. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kudo M, Finn RS, Qin S, Han KH, Ikeda K,
Piscaglia F, Baron A, Park JW, Han G, Jassem J, et al: Lenvatinib
versus sorafenib in first-line treatment of patients with
unresectable hepatocellular carcinoma: A randomised phase 3
non-inferiority trial. Lancet. 391:1163–1173. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Xia J, Gelfond J and Arora SP: Second-line
treatment with nivolumab, cabozantinib, regorafenib, or best
supportive care in patients with advanced hepatocellular carcinoma:
Analysis at a Hispanic-majority NCI-designated cancer center. J
Gastrointest Oncol. 12:2943–2951. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wilhelm SM, Dumas J, Adnane L, Lynch M,
Carter CA, Schütz G, Thierauch KH and Zopf D: Regorafenib (BAY
73–4506): A new oral multikinase inhibitor of angiogenic, stromal
and oncogenic receptor tyrosine kinases with potent preclinical
antitumor activity. Int J Cancer. 129:245–255. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bruix J, Qin S, Merle P, Granito A, Huang
YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, et al:
Regorafenib for patients with hepatocellular carcinoma who
progressed on sorafenib treatment (RESORCE): A randomised,
double-blind, placebo-controlled, phase 3 trial. Lancet. 389:56–66.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Naruto K, Kawaoka T, Amioka K, Ogawa Y,
Chihiro K, Yoshikawa Y, Ando Y, Suehiro Y, Kosaka Y, Uchikawa S, et
al: Clinical outcomes of 2nd- and 3rd-Line regorafenib for advanced
hepatocellular carcinoma. Oncology. 99:491–498. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kudo M: Recent trends in the management of
hepatocellular carcinoma with special emphasis on treatment with
Regorafenib and immune checkpoint inhibitors. Dig Dis. 34:714–730.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xie L, Liu M, Cai M, Huang W, Guo Y, Liang
L, Cai W, Liu J, Liang W, Tan Y, et al: Regorafenib enhances
anti-tumor efficacy of immune checkpoint inhibitor by regulating
IFN-γ/NSDHL/SREBP1/TGF-β1 axis in hepatocellular carcinoma. Biomed
Pharmacother. 159:1142542023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shigeta K, Matsui A, Kikuchi H, Klein S,
Mamessier E, Chen IX, Aoki S, Kitahara S, Inoue K, Shigeta A, et
al: Regorafenib combined with PD1 blockade increases CD8 T-cell
infiltration by inducing CXCL10 expression in hepatocellular
carcinoma. J Immunother Cancer. 8:e0014352020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Solimando AG, Susca N, Argentiero A,
Brunetti O, Leone P, De Re V, Fasano R, Krebs M, Petracci E, Azzali
I, et al: Second-line treatments for advanced hepatocellular
carcinoma: A systematic review and Bayesian network meta-analysis.
Clin Exp Med. 22:65–74. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372:n712021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Higgins JP, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang J, Guo Y, Huang W, Hong X, Quan Y,
Lin L, Zhou J, Liang L, Zhang Y, Zhou J, et al: Regorafenib
combined with PD-1 blockade immunotherapy versus Regorafenib as
second-line treatment for advanced hepatocellular carcinoma: A
multicenter retrospective study. J Hepatocell Carcinoma. 9:157–170.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li J, Jia Y, Shao C, Li Y and Song J:
Clinical efficacy and safety of an immune checkpoint inhibitor in
combination with regorafenib therapy as second-line regimen for
patients with unresectable hepatocellular carcinoma. Ther Clin Risk
Manag. 19:329–339. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu K, Wu J, Xu Y, Li D, Huang S and Mao
Y: Efficacy and safety of Regorafenib with or without PD-1
inhibitors as second-line therapy for advanced hepatocellular
carcinoma in real-world clinical practice. Onco Targets Ther.
15:1079–1094. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yan T, Huang C, Peng C, Duan X, Ji D, Duan
Y, Zhang W, Zhao H, Gao K, Yang X, et al: A multi-center
retrospective study on the efficacy and safety of regorafenib vs.
regorafenib combined with PD-1 inhibitors as a second-line therapy
in patients with advanced hepatocellular carcinoma. Ann Transl Med.
11:1092023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tu X, Yang J and Zheng Y, Liang C, Tao Q,
Tang X, Liu Z, Jiang L, He Z, Xie F and Zheng Y: Immunotherapy
combination with regorafenib for refractory hepatocellular
carcinoma: A real-world study. Int Immunopharmacol. 113:1094012022.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yang C, Zhang H, Zhang L, Zhu AX, Bernards
R, Qin W and Wang C: Evolving therapeutic landscape of advanced
hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol.
20:203–222. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Vogel A, Meyer T, Sapisochin G, Salem R
and Saborowski A: Hepatocellular carcinoma. Lancet. 400:1345–1362.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Grothey A, Blay JY, Pavlakis N, Yoshino T
and Bruix J: Evolving role of regorafenib for the treatment of
advanced cancers. Cancer Treat Rev. 86:1019932020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Grothey A, Van Cutsem E, Sobrero A, Siena
S, Falcone A, Ychou M, Humblet Y, Bouché O, Mineur L, Barone C, et
al: Regorafenib monotherapy for previously treated metastatic
colorectal cancer (CORRECT): An international, multicentre,
randomised, placebo-controlled, phase 3 trial. Lancet. 381:303–312.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Heo YA and Syed YY: Regorafenib: A review
in hepatocellular carcinoma. Drugs. 78:951–958. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhu AX, Finn RS, Edeline J, Cattan S,
Ogasawara S, Palmer D, Verslype C, Zagonel V, Fartoux L, Vogel A,
et al: Pembrolizumab in patients with advanced hepatocellular
carcinoma previously treated with sorafenib (KEYNOTE-224): A
non-randomised, open-label phase 2 trial. Lancet Oncol. 19:940–952.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Finn RS, Ryoo BY, Merle P, Kudo M,
Bouattour M, Lim HY, Breder V, Edeline J, Chao Y, Ogasawara S, et
al: Pembrolizumab as second-line therapy in patients with advanced
hepatocellular carcinoma in KEYNOTE-240: A randomized,
double-blind, phase III trial. J Clin Oncol. 38:193–202. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Granito A, Forgione A, Marinelli S,
Renzulli M, Ielasi L, Sansone V, Benevento F, Piscaglia F and
Tovoli F: Experience with regorafenib in the treatment of
hepatocellular carcinoma. Therap Adv Gastroenterol.
14:175628482110169592021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu RY, Kong PF, Xia LP, Huang Y, Li ZL,
Tang YY, Chen YH, Li X, Senthilkumar R, Zhang HL, et al:
Regorafenib promotes antitumor immunity via inhibiting PD-L1 and
IDO1 expression in melanoma. Clin Cancer Res. 25:4530–4541. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Stefanini B, Ielasi L, Chen R, Abbati C,
Tonnini M, Tovoli F and Granito A: TKIs in combination with
immunotherapy for hepatocellular carcinoma. Expert Rev Anticancer
Ther. 23:279–291. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kim HD, Jung S, Lim HY, Ryoo BY, Ryu MH,
Chuah S, Chon HJ, Kang B, Hong JY, Lee HC, et al: Regorafenib plus
nivolumab in unresectable hepatocellular carcinoma: The phase 2
RENOBATE trial. Nat Med. 30:699–707. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li J, Huang L, Ge C, Zhu X, Qiu M, Chen C,
Wei S and Yan Y: Simultaneous and sequential use of molecular
targeted agents plus immune checkpoint inhibitors for advanced
hepatocellular carcinoma: A real-world practice in China. J
Hepatocell Carcinoma. 10:949–958. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yu X, Wei C, Cui R and Jiang O: Lenvatinib
plus immune checkpoint inhibitors versus Lenvatinib monotherapy as
treatment for advanced hepatocellular carcinoma: A meta-analysis.
Int J Clin Exp Pathol. 16:321–331. 2023.PubMed/NCBI
|
|
33
|
Zhao J, Guo Y, Feng T, Rong D, Kong X,
Huang T, Lopez-Lopez V, Yarmohammadi H, Sakamoto Y, Zhu D, et al:
Efficacy and safety of regorafenib in combination with immune
checkpoint inhibitor therapy as second-line and third-line regimen
for patients with advanced hepatocellular carcinoma: A
retrospective study. J Gastrointest Oncol. 14:2549–2558. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Nct, . Regorafenib Plus Sintilimab vs.
Regorafenib as the Second-line Treatment for HCC. https://clinicaltrials.gov/show/NCT047189092021
|
|
35
|
Yoo C, Park JW, Kim YJ, Kim DY, Yu SJ, Lim
TS, Lee SJ, Ryoo BY and Lim HY: Multicenter retrospective analysis
of the safety and efficacy of regorafenib after progression on
sorafenib in Korean patients with hepatocellular carcinoma. Invest
New Drugs. 37:567–572. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Llovet JM, Castet F, Heikenwalder M, Maini
MK, Mazzaferro V, Pinato DJ, Pikarsky E, Zhu AX and Finn RS:
Immunotherapies for hepatocellular carcinoma. Nat Rev Clin Oncol.
19:151–172. 2022. View Article : Google Scholar : PubMed/NCBI
|