Introduction
Esophageal cancer is a malignant tumor with one of
the highest incidences and mortality rates globally. According to
the Global Cancer Statistics Report 2022, esophageal cancer has the
seventh-highest incidence rate and the sixth-highest total
mortality rate worldwide (1).
Notably, China alone accounts for >50% of esophageal cancer
cases globally (2,3). Therefore, studying the treatment and
recovery methods has clinical significance.
Although advanced therapies such as targeted therapy
and immunotherapy have seen rapid development, radiotherapy (a
traditional treatment) is still widely used for esophageal cancer
owing to its considerable efficacy. However, radiotherapy damages
adjacent normal tissues, resulting in radiation-related side
effects such as radiation-induced lung and esophageal injuries,
threatening the quality of life of patients (4,5).
Notably, the probability of radiation esophagitis in the irradiated
field, including the esophagus, is as high as 100% (6). It has been suggested that
intensity-modulated conformal radiotherapy (IMCRT) can greatly
reduce the damage to normal tissues and key organs. It can also
decrease the incidence of radiation esophagitis (7). However, IMCRT may lead to acute
radiation esophagitis (ARE), one of the most common
radiotherapy-related complications. ARE can cause dysphagia, pain
and esophageal perforation and may even lead to the termination of
the treatment. Hence, ARE poses a serious threat to the quality of
life and health of patients (8).
Therefore, it is essential to perform early prevention and timely
intervention for ARE in these patients.
Esophageal cancer has the highest incidence of
malnutrition among all tumor types. A previous study has also
reported that malnutrition is associated with the occurrence of ARE
in patients with esophageal cancer (9). Due to large variations in case
selection, previous studies have employed diverse nutritional
indicators to assess the nutritional status of patients. However,
this has led to significant heterogeneity among conclusions, making
it challenging to suggest a common effective treatment method
(10). Notably, the metabolic
process in patients with esophageal cancer can cause malnutrition
too, further inducing the systemic inflammatory response (11–13).
Therefore, malnutrition and systemic inflammatory response may
interact and serve an important role in tumor progression and
treatment. In spite of their importance, the association between
nutritional indicators and systemic inflammatory indicators in the
development of ARE in patients with esophageal cancer has not yet
been elucidated.
The present study retrospectively analyzed the
factors associated with radiation esophagitis in patients with
esophageal cancer. Specifically, the present study aimed to develop
a risk-prediction model for ARE using prognostic nutritional index
(PNI) along with neutrophil to lymphocyte ratio (NLR) and platelet
to lymphocyte ratio (PLR). Furthermore, the target of the present
work was to develop methods for early detection of people at high
risk of ARE and to propose targeted preventive interventions to
reduce the incidence of radiation esophagitis in such patients.
Materials and methods
Study design
In the training cohort, 225 patients with esophageal
cancer received radiotherapy at the First Affiliated Hospital of
Anhui Medical University (Hefei, China) from January 2018 to
December 2022. In the validation cohort, 169 patients with
esophageal cancer received radiotherapy at Gaoxin Hospital, the
First Affiliated Hospital of Anhui Medical University from January
2023 to April 2024. Esophageal cancer was segmented according to
the 7th edition of the American Joint Committee on Cancer (AJCC)
Cancer Staging system (14). Both
squamous cell carcinoma and adenocarcinoma were adopted in this
study.
The following inclusion criteria were used: i)
Pathologically-confirmed esophageal cancer; ii) suitability for
radiotherapy (in doses of 45–60 Gy) along with chemotherapy; and
iii) complete clinical and follow-up data. Furthermore, the
following exclusion criteria were used: i) Recurrent esophageal
cancer; ii) other primary malignant tumors; and iii) missing
baseline information, such as routine blood and blood biochemistry
results before radiotherapy.
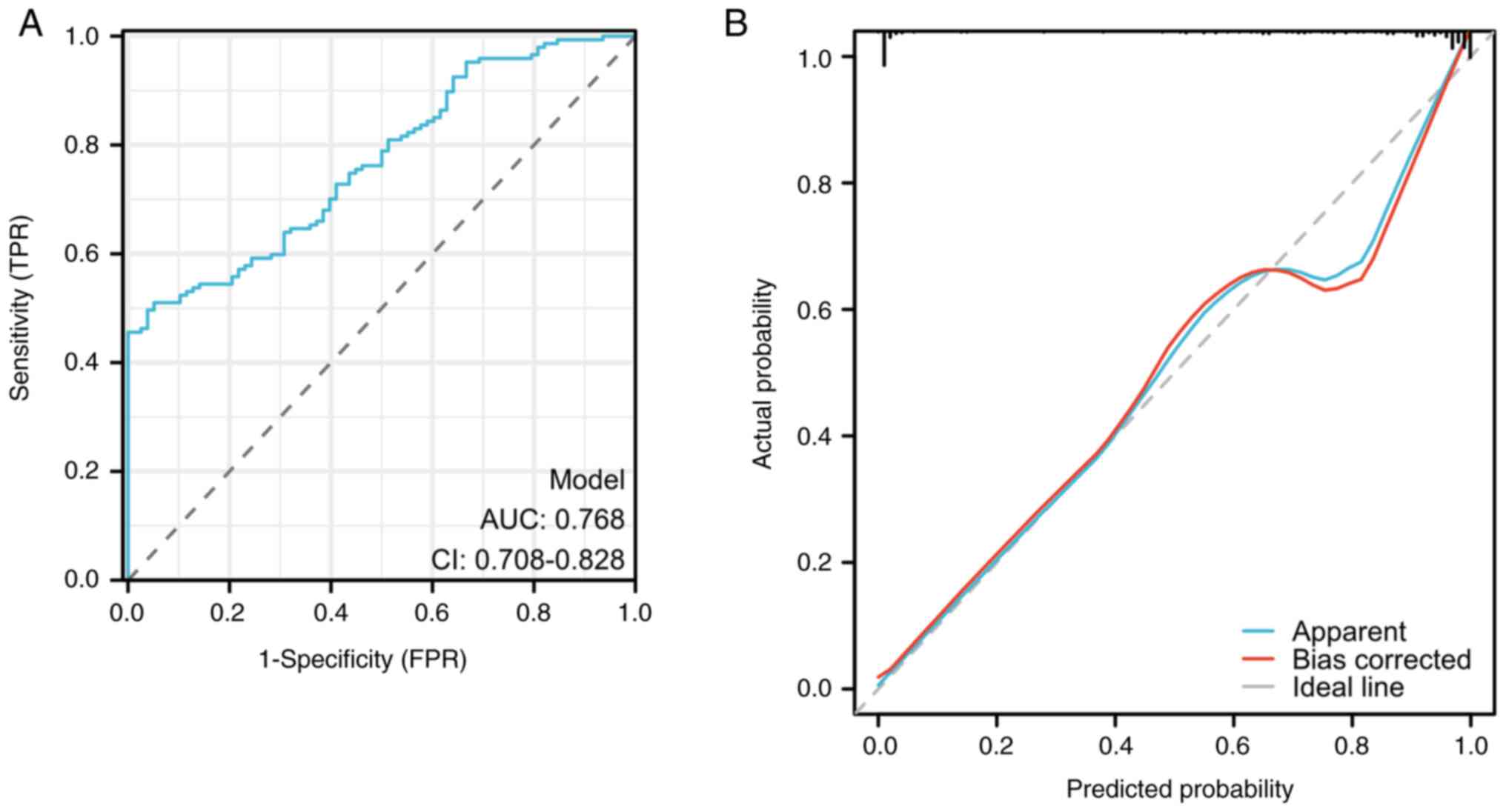
External verification
External verification was performed using 169
patients with esophageal cancer who received radiotherapy at Gaoxin
Hospital, the First Affiliated Hospital of Anhui Medical
University. The model was evaluated based on two aspects:
Discrimination and calibration. The receiver operating
characteristic (ROC) curve was used for discrimination evaluation,
and the calibration curve was used for calibration evaluation.
Treatment procedure
All patients received IMCRT using a 6MVX linear
accelerator pedal. After reviewing radiological (X-ray barium meal,
CT and/or PET/CT scanning) images and endoscopic or endoscopic
ultrasonographical manifestation of the patients, the tumor target
area was outlined using a Philips Pinnacle 3 workstation (Phillips
Healthcare), a treatment planning system. It required a 95%
planning target volume to reach the prescribed dose. In the whole
group, the radiotherapy dosage was applied in fractions of 1.8–2.2
Gy five times a week, up to total doses of 45–60 Gy.
Evaluation criteria
The following evaluation criteria were used: i)
Parameter information was collected using follow-up data and the
hospital information system, specifically regarding sex, age,
alcohol consumption, smoking, comorbidities, tumor-node-metastasis
(TNM) stage (14), concurrent
chemotherapy and pathological type; ii) all patients had routine
blood and blood biochemistry laboratory indexes assessed 1 week
before radiotherapy, including neutrophil counts, lymphocyte
counts, platelet counts and albumin levels. PNI [serum albumin
(g/l) + 5× total number of lymphocytes in peripheral blood
(×109/l)], NLR (neutrophil count/peripheral blood
lymphocyte count), and PLR (peripheral blood platelet
count/peripheral blood lymphocyte count) were calculated; iii)
before performing radiotherapy on the patients, the age-adjusted
Charlson Comorbidity Index (ACCI) (15) was calculated using a scoring system
based on patient comorbidities. All comorbidity and age scores were
added up to obtain the ACCI score. The higher the score, the higher
the number of comorbidities, and the worse the basal status; and
iv) ARE was evaluated according to the toxicity criteria of the
radiation therapy oncology group (RTOG) and the European
organization for research and treatment of cancer (EORTC) (16), the primary study endpoint was the
occurrence of ARE. Follow-up was performed ≤3 months after the end
of radiotherapy.
Statistical analysis
SPSS 28.0 software (IBM Corp.) was used to analyze
the data. Continuous variables that conformed to normal
distribution are expressed as mean ± standard deviation and were
analyzed using an independent sample t-test. Data that did not
conform to normal distribution are expressed as the median
(interquartile range) and were assessed using the Mann-Whitney U
test. Categorical variables are expressed as n (%) and were
assessed using the Pearson χ2 or Fisher's exact test.
The Youden index (sensitivity + specificity −1) was calculated
using the ROC curve to determine the optimal threshold of PNI
before radiotherapy (the maximum point of the Youden index
corresponds to the PNI value). All patients included in the present
study were categorized into either high-PNI (H-PNI; >48.2) or
low-PNI (L-PNI; ≤48.2) groups. The relationship between
pre-radiotherapy PNI and the incidence and severity of ARE in
patients with esophageal cancer was assessed using the
χ2 test and Spearman's correlation analysis. A
multifactorial logistic regression model was used to evaluate the
independent risk factors for the occurrence of ARE in patients with
esophageal cancer. A column-line graphical model was produced by
using the R (R3.5.3) software package (The R Foundation). The
predictive efficacy of the model was assessed using calibration
curves and decision curves. P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline characteristics of
patients
In the training cohort, 60 (26.7%) patients were
women and 165 (73.3%) were men, with a median age of 63 years
(interquartile range, 61–69 years). A total of 84 patients (37.3%)
were smokers and 54 (24.0%) consumed alcohol. In the validation
cohort, 43 (25.4%) patients were women and 126 (74.6%) were men,
with a median age of 61 years (interquartile range, 60–68 years). A
total of 56 patients (33.1%) were smokers and 39 (23.1%) consumed
alcohol. Comparing the general clinicopathological characteristics,
there were no statistically significant differences between the two
groups in terms of sex, age, smoking and alcohol consumption, ACCI,
chemotherapy status, TNM stage, histological type, PNI, NLR and PLR
(P>0.05; Table I).
 | Table I.Baseline characteristics of all
patients in the training and validation cohorts. |
Table I.
Baseline characteristics of all
patients in the training and validation cohorts.
| Clinicopathological
characteristic | Training cohort
(n=225) | Validation cohort
(n=169) | P-value |
|---|
| Age, years | 63 (61–69) | 61 (60–68) | 0.356 |
| Sex |
|
|
|
| Male | 165 (73.3) | 126 (74.6) | 0.817 |
|
Female | 60 (26.7) | 43 (25.4) |
|
| Smoker |
|
|
|
| Yes | 84 (37.3) | 56 (33.1) | 0.397 |
| No | 141 (62.7) | 113 (66.9) |
|
| Alcohol
consumption |
|
|
|
| Yes | 54 (24.0) | 39 (23.1) | 0.905 |
| No | 171 (76.0) | 130 (76.9) |
|
| ACCI score |
|
|
|
| 1-2 | 63 (28.0) | 45 (26.6) | 0.873 |
| 3-4 | 121 (53.8) | 90 (53.3) |
|
| 5-7 | 41 (18.2) | 34 (20.1) |
|
| Chemotherapy |
|
|
|
| Yes | 96 (42.7) | 72 (42.6) | 0.990 |
| No | 129 (57.3) | 97 (57.4) |
|
| TNM stage |
|
|
|
| ≥III | 66 (29.3) | 50 (29.6) | 0.957 |
|
<III | 159 (70.7) | 119 (70.4) |
|
| Histological
type |
|
|
|
|
Adenocarcinoma | 55 (24.4) | 41 (24.3) | 0.966 |
| Squamous
cell carcinoma | 170 (75.6) | 128 (75.7) |
|
| PNI | 46.3±5.1 | 45.9±4.4 | 0.911 |
| NLR | 2.8±1.7 | 2.6±1.9 | 0.937 |
| PLR | 119.6±47.8 | 117.2±53.3 | 0.985 |
Relationship between pre-radiotherapy
PNI and ARE in patients with esophageal cancer
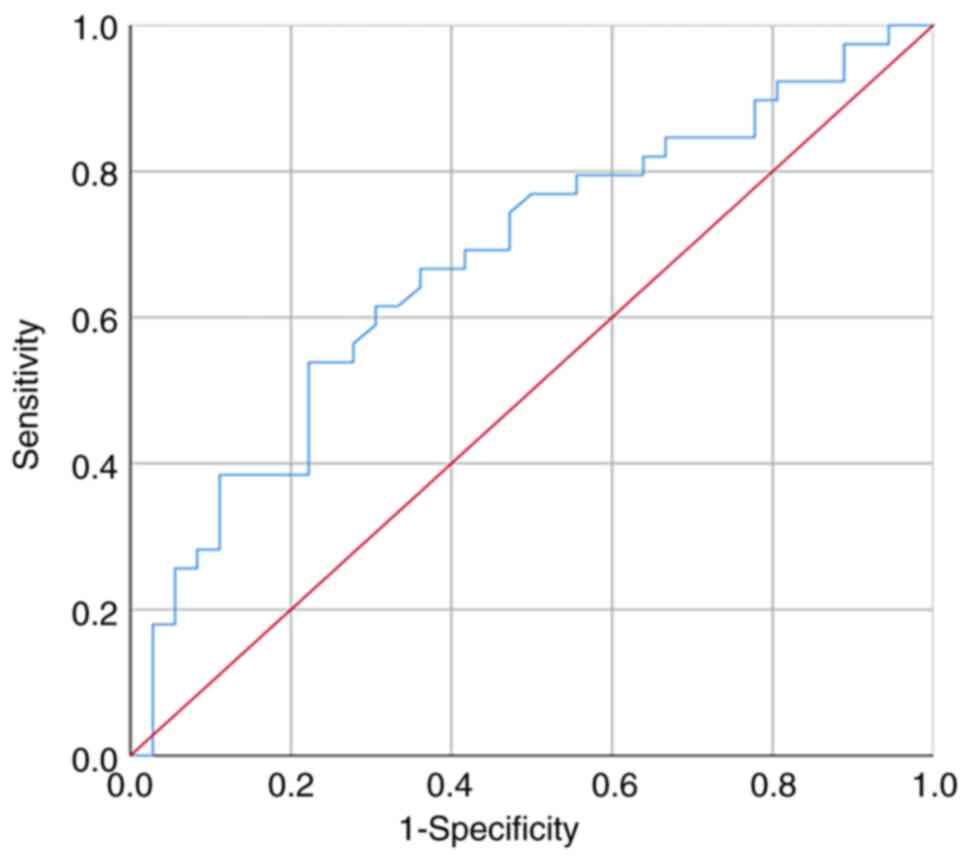
The optimal cutoff value of PNI before radiotherapy
was 48.2 with an AUC of 0.677, a sensitivity of 66%, and a
specificity of 69%. The maximum value of the Youden index was
determined as 0.35 by plotting the ROC curve of PNI (Fig. 1). The patients were divided into the
following groups based on their PNI cutoff value before
radiotherapy: Well-nourished group (H-PNI group; n=108; PNI
>48.2) and the malnourished group (L-PNI group; n=117; PNI
≤48.2). The χ2 test results revealed that
pre-radiotherapy PNI was significantly associated with the
occurrence of ARE in patients with esophageal cancer, the incidence
of ARE in H-PNI group was lower than that in L-PNI group (52.8% vs.
76.9%; χ2=14.46; P<0.001; Table II). In addition, Spearman's
correlation analysis demonstrated the negative correlation of
pre-radiotherapy PNI with the grade of ARE after radiotherapy, with
higher PNI indicating a lower grade of ARE (P<0.001; Table III).
 | Table II.Relation between prognostic
nutritional index and the incidence of acute radiation
esophagitis. |
Table II.
Relation between prognostic
nutritional index and the incidence of acute radiation
esophagitis.
| ARE | n | H-PNI (n=108) | L-PNI (n=117) | χ2
value | P-value |
|---|
| Yes | 147 | 57 | 90 | 14.46 | <0.001 |
| No | 78 | 51 | 27 |
|
|
 | Table III.Spearman's correlation analysis
between prognostic nutritional index and acute radiation
esophagitis grades. |
Table III.
Spearman's correlation analysis
between prognostic nutritional index and acute radiation
esophagitis grades.
| ARE grade | n | H-PNI (n=108) | L-PNI (n=117) | Spearman's
correlation index | P-value |
|---|
| 0 | 78 | 51 | 27 | −0.352 | <0.001 |
| I | 42 | 27 | 15 |
|
|
| II | 42 | 15 | 27 |
|
|
| III | 63 | 15 | 48 |
|
|
| IV | 0 | 0 | 0 |
|
|
Analysis of factors affecting ARE in
patients with esophageal cancer
A univariate analysis was performed on all 225
patients based on clinicopathological parameters. The results
revealed that PNI, NLR and PLR are major risk factors for ARE in
patients undergoing intensity-modulated radiotherapy for esophageal
cancer (Table IV). Multifactorial
logistic regression analysis demonstrated that PNI, NLR and PLR are
independent risk factors affecting ARE in patients treated with
radiotherapy for esophageal cancer (Table IV).
 | Table IV.Logistic analysis of factors
affecting acute radiation esophagitis in patients with esophageal
cancer. |
Table IV.
Logistic analysis of factors
affecting acute radiation esophagitis in patients with esophageal
cancer.
|
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|---|
| Characteristic | n | Odds ratio (95%
CI) | P-value | Odds ratio (95%
CI) | P-value |
|---|
| Age | 225 | 0.993
(0.959–1.029) | 0.705 |
|
|
| Sex |
|
|
|
|
|
|
Male | 165 | Reference |
|
|
|
|
Female | 60 | 1.201
(0.640–2.256) | 0.569 |
|
|
| Smoker |
|
|
|
|
|
|
Yes | 84 | Reference |
|
|
|
| No | 141 | 0.910
(0.515–1.609) | 0.746 |
|
|
| Alcohol
consumption |
|
|
|
|
|
|
Yes | 54 | Reference |
|
|
|
| No | 171 | 1.565
(0.835–2.931) | 0.162 |
|
|
| ACCI score |
|
|
|
|
|
|
1-2 | 63 | Reference |
|
|
|
|
3-4 | 121 | 1.397
(0.738–2.646) | 0.305 |
|
|
|
5-7 | 41 | 0.869
(0.389–1.939) | 0.731 |
|
|
| Chemotherapy |
|
|
|
|
|
|
Yes | 96 | Reference |
|
|
|
| No | 129 | 0.978
(0.561–1.704) | 0.937 |
|
|
| TNM stage |
|
|
|
|
|
|
≥III | 66 | Reference |
|
|
|
|
<III | 159 | 1.337
(0.738–2.424) | 0.338 |
|
|
| Histological
type |
|
|
|
|
|
|
Adenocarcinoma | 55 | Reference |
|
|
|
|
Squamous cell carcinoma | 170 | 1.503
(0.805–2.807) | 0.201 |
|
|
| PNI | 225 | 0.839
(0.789–0.893) |
<0.001a | 0.864
(0.809–0.924) |
<0.001a |
| NLR | 225 | 1.952
(1.371–2.779) |
<0.001a | 1.795
(1.209–2.667) | 0.004a |
| PLR | 225 | 1.019
(1.010–1.029) |
<0.001a | 1.011
(1.000–1.022) | 0.046a |
Modeling and evaluation for predicting
ARE in patients treated with IMCRT for esophageal cancer
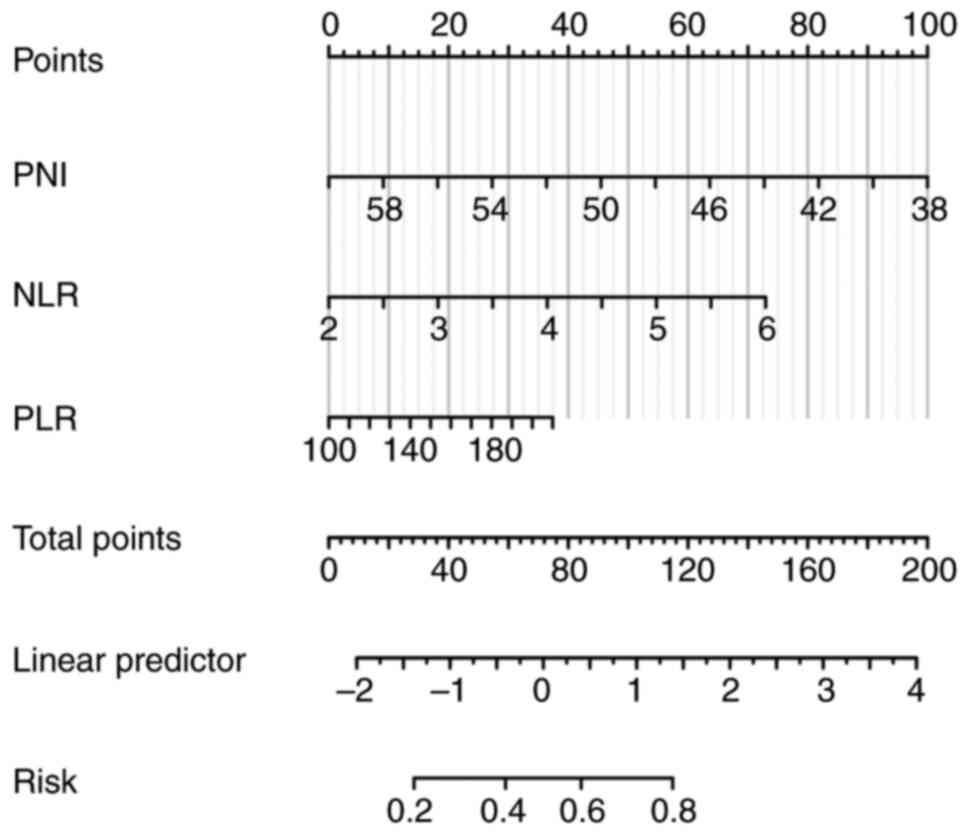
The risk of ARE in patients undergoing IMCRT for
esophageal cancer was modeled as a histogram based on three
independent predictors (Fig. 2),
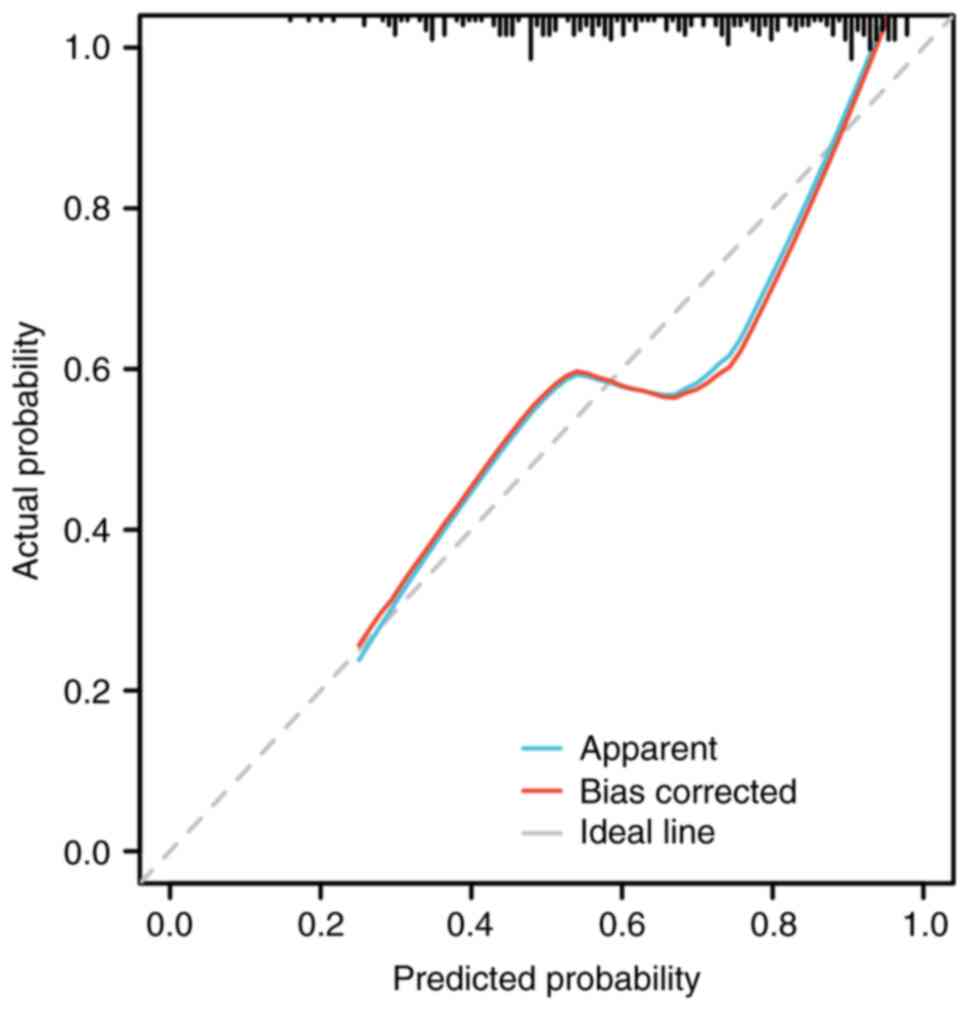
with a total score of 254 points in three columns. The calibration
curve tended to be close to the ideal curve, indicating that the
predicted values were in good agreement with the actual values and
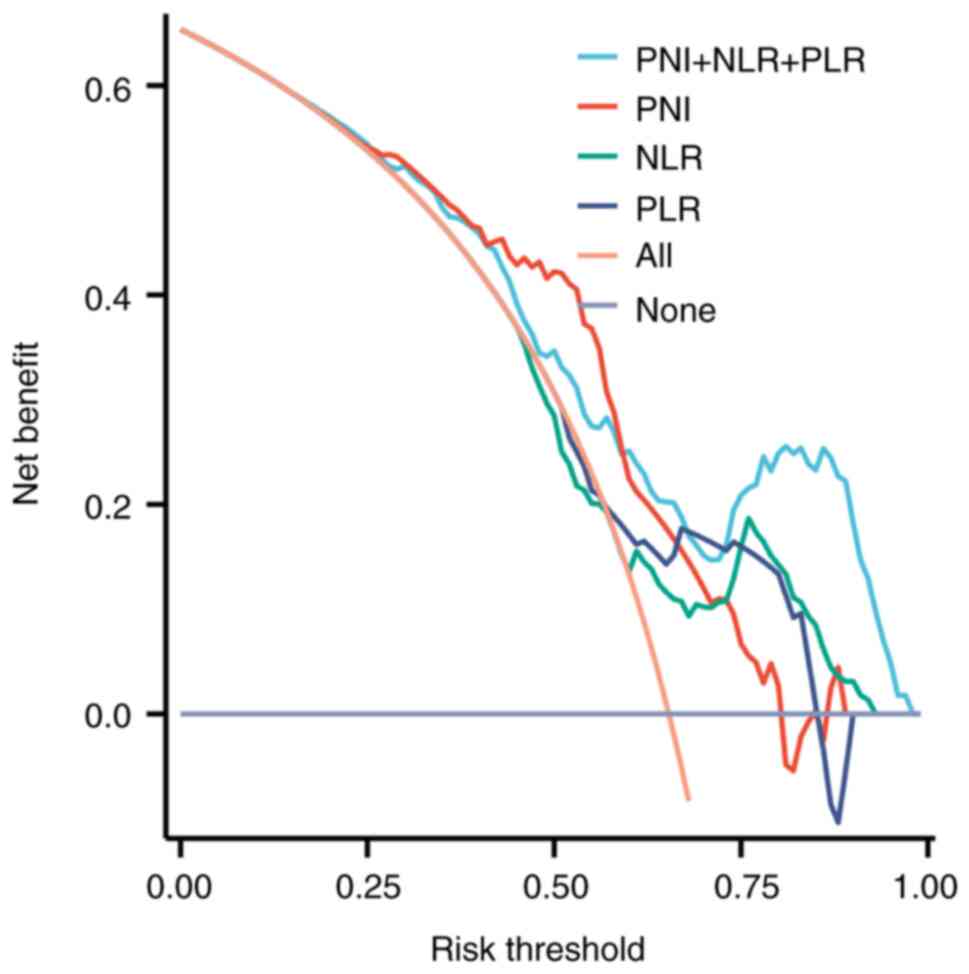
that the predictive accuracy of the model was good (Fig. 3). The clinical decision curve
demonstrated that when the risk threshold was between 0.25 and 1.0,
the net benefit was >0, which is clinically significant
(Fig. 4). The smaller the risk
threshold, the larger the net benefit of the model, and the better
the clinical application effect. Therefore, this column diagram
indicated good clinical value for predicting the occurrence of ARE
in patients undergoing IMCRT for esophageal cancer.
External validation of the ARE model
for patients treated with IMCRT for esophageal cancer
A total of 169 patients with esophageal cancer were
enrolled from Gaoxin Hospital, the First Affiliated Hospital of
Anhui Medical University, who underwent IMCRT as the external
validation set of the model. The C-statistic was 0.768, indicating
a high degree of discrimination (Fig.
5A) and the calibration curve was close to the ideal curve
(Fig. 5B), indicating good
predictive accuracy of the model.
Discussion
Generally, ~21% of patients with esophageal cancer
discontinue radiotherapy due to severe ARE (17). A previous study reported that the
occurrence of ARE is associated with the radiotherapy dose
(18). However, the risk of ARE is
not the same even when the radiotherapy dose is similar, suggesting
that the occurrence of ARE may be related to other factors besides
dose. Therefore, to avoid the effect of the radiotherapy dose, the
present study chose a population with a relatively consistent dose
as the study population. The clinical data of 225 patients with
esophageal cancer from January 2018 to December 2022 were
retrospectively analyzed and an operating characteristic PNI curve
was generated for the patients. Based on the results obtained, the
patients were categorized in two groups using a PNI value of 48.2
as the cutoff point: H-PNI group (n=108) and the L-PNI group
(n=117). The incidence and severity of ARE were significantly lower
in the H-PNI group (n=57) than they were in the L-PNI group (n=90).
Further analysis of the correlation between PNI before radiotherapy
and the incidence and severity of ARE revealed a statistically
significant difference in the severity of ARE between the H-PNI and
L-PNI groups.
Risk-prediction column-line diagrams have the
characteristics of clear visualization, quantification and
graphical presentation. Hence, they are widely used in the
diagnosis, treatment, and prognostic assessment of several diseases
(19–21). The present study performed
univariate and multivariate logistic regression analyses to
comprehensively evaluate the risk factors associated with ARE in
patients with esophageal cancer. The results identified the
nutrition-related index, PNI, and the systemic inflammation-related
indexes, NLR and PLR, as independent risk factors for the incidence
of ARE in patients that had undergone IMCRT. Subsequently, a
column-line prediction model was constructed. When the calibration
curve was used to evaluate the predictive power of the nomogram, it
approached the ideal curve, indicating that the predicted value was
in good agreement with the actual value, and that the predictive
accuracy of this model was good. In addition, external verification
confirmed that this model exhibited a high degree of discrimination
and calibration. Therefore, the results indicate that this nomogram
model can be employed to predict the occurrence of ARE in patients
undergoing IMCRT for esophageal cancer. In clinical practice,
according to the predicted probability of the model, patients with
a high incidence of ARE can be prophylactically treated with agents
such as antibiotics and radioprotectants. In addition, nursing care
can be strengthened to minimize the incidence of ARE. In certain
patients with esophageal stenosis, gastrostomy and gastroenteritis
tubes can be considered before performing radiotherapy to ensure
adequate nutritional supply during radiotherapy. Patients were
closely monitored during their radiotherapy treatments, assessed
weekly, and promptly managed based on the results.
The nutritional status of patients with esophageal
cancer gradually deteriorates during radiotherapy. Consequently,
the risk of malnutrition gradually increases, which in turn can
further trigger the onset of ARE (7). Therefore, the relationship between ARE
and malnutrition deserves an in-depth investigation. However, there
are differences in the current findings. Wang et al
(22) identified malnutrition as a
major risk factor for the development of radiation esophagitis in
patients undergoing radiotherapy for esophageal cancer. However, no
measurement tool for malnutrition was mentioned. Cao et al
(23) used the Patient Subjective
Global Assessment for assessing the nutritional status and reported
that malnutrition increased the incidence of radiation esophagitis.
However, Wang et al (22)
used the same tool and reported that malnutrition had no
significant association with acute side effects or the short-term
efficacy of radiotherapy in patients (9). PNI, which now finds wide applications
in the evaluation of several solid tumors, can comprehensively
reflect the nutritional status of the body, is noninvasive, and is
easily obtained (24–26). However, the application of PNI in
ARE in esophageal cancer is still in its infancy.
Esophageal cancer is often associated with a
systemic inflammatory state. This affects metabolic processes,
leading to malnutrition, which further induces a systemic
inflammatory response, forming a vicious circle (27,28).
NLR and PLR are among the most commonly used indicators to assess
the systemic inflammatory status of patients with cancer (29,30).
Several studies have reported a strong association between poor
prognosis and NLR/PLR in patients with esophageal cancer (31,32).
Both PNI, a nutritional index, and NLR/PLR, a systemic inflammatory
index, impact patients with esophageal cancer. However, no study
has yet confirmed the association between ARE and the nutritional
index along with systemic inflammatory index in patients with
esophageal cancer, to the best of our knowledge.
The present study has certain limitations: i) It is
a retrospective study resulting in an inevitable selection bias;
ii) the present study had limited inclusion of factors and there
may be certain confounding factors that were not included; and iii)
the present study aimed to collect laboratory indicators before
radiotherapy in patients and construct a risk prediction model for
the occurrence of ARE. It provides a certain reference basis for
the early detection of individuals with a high risk of ARE and for
reducing the occurrence of ARE. In the future, the indicators will
be tested weekly during radiotherapy to assess the occurrence of
ARE and provide timely management to ensure the smooth progress of
radiotherapy. Furthermore, under the premise of ensuring the
authenticity and objectivity of the data, the sample size is still
limited. A prospective study with a larger sample size in multiple
centers should be performed to clarify the value of the model for
predicting ARE in this group of patients, exploring additional risk
factors, and providing interventions to mitigate the occurrence of
ARE.
In summary, PNI, NLR and PLR are independent risk
factors affecting ARE in patients undergoing IMCRT. In the present
study, the risk-predicting nomogram model based on the risk factors
had a high clinical application value and could accurately and
intuitively predict the risk degree of ARE in patients with
esophageal cancer.
Acknowledgements
The authors would like to thank Dr Mei Kang (Gaoxin
Hospital of Anhui Medical University, Hefei, China) for their
assistance in patient data collection.
Funding
The present study was financially supported by the Natural
Science Foundation of Anhui Provincial Department of Education
(grant no. KJ2023A0172) and the Graduate Student Youth Cultivation
Program of School of Nursing, Anhui Medical University (grant no.
hlqm12023076).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
LW, WL and SL conceived and designed the study. LW,
XM, MY and YW collected and analyzed the data. LW, MY, YW and SL
wrote the manuscript. LW and SL confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
All procedures performed in the present study
involving human participants were in accordance with the 1964
Helsinki Declaration and its later amendments or comparable ethical
standards. The protocol was approved by the Ethics Committee of
Anhui Medical University (Hefei, China; approval no. 82240081,
2024-07-31). Due to the retrospective nature of the present study,
informed consent was waived.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar
|
|
2
|
Zhu H, Ma X, Ye T, Wang H, Wang Z, Liu Q
and Zhao K: Esophageal cancer in China: Practice and research in
the new era. Int J Cancer. 152:1741–1751. 2023. View Article : Google Scholar
|
|
3
|
Li R, Sun J, Wang T, Huang L, Wang S, Sun
P and Yu C: Comparison of secular trends in esophageal cancer
mortality in China and Japan during 1990–2019: An age-period-cohort
analysis. Int J Environ Res Public Health. 19:103022022. View Article : Google Scholar
|
|
4
|
Tonoiso C, Ikushima H, Kubo A, Kawanaka T,
Funatani S, Kudo T, Yoshida T, Miyamoto H, Harada M, Takayama T and
Tangoku A: Clinical outcomes and prognostic factors of definitive
radiotherapy for esophageal cancer. J Med Invest. 66:99–105. 2019.
View Article : Google Scholar
|
|
5
|
de Groot C, Beukema JC, Langendijk JA, van
der Laan HP, van Luijk P, van Melle JP, Muijs CT and Prakken NHJ:
Radiation-Induced myocardial fibrosis in long-term esophageal
cancer survivors. Int J Radiat Oncol Biol Phys. 110:1013–1021.
2021. View Article : Google Scholar
|
|
6
|
Alizade-Harakiyan M, Jangjoo AG,
Jafari-Koshki T, Fatemi A and Mesbahi A: Radiobiological modeling
of acute esophagitis after radiation therapy of head, neck, and
thorax tumors: The influence of chemo-radiation. J Cancer Res Ther.
18:1706–1715. 2022. View Article : Google Scholar
|
|
7
|
Zhou P, Du Y, Zhang Y, Zhu M, Li T, Tian
W, Wu T and Xiao Z: Efficacy and safety in proton therapy and
photon therapy for patients with esophageal cancer: A
meta-analysis. JAMA Netw Open. 6:e23281362023. View Article : Google Scholar
|
|
8
|
Zheng X, Guo W, Wang Y, Zhang J, Zhang Y,
Cheng C, Teng X, Lam S, Zhou T, Ma Z, et al: Multi-omics to predict
acute radiation esophagitis in patients with lung cancer treated
with intensity-modulated radiation therapy. Eur J Med Res.
28:1262023. View Article : Google Scholar
|
|
9
|
Wang SA, Dai WS, Zhu JY, Gao B, Ren W and
Chen X: Nasogastric tube feeding improves nutritional status and
physical state in esophageal cancer patients during
chemoradiotherapy: A retrospective study. Support Care Cancer.
31:3412023. View Article : Google Scholar
|
|
10
|
Vidal-Casariego A, Calleja-Fernandez A,
Ballesteros-Pomar MD and Cano-Rodriguez I: Efficacy of glutamine in
the prevention of oral mucositis and acute radiation-induced
esophagitis: A retrospective study. Nutr Cancer. 65:424–429. 2013.
View Article : Google Scholar
|
|
11
|
Sui Q, Zhang X, Chen C, Tang J, Yu J, Li
W, Han K, Jiang W, Liao L, Kong L, et al: Inflammation promotes
resistance to immune checkpoint inhibitors in high microsatellite
instability colorectal cancer. Nat Commun. 13:73162022. View Article : Google Scholar
|
|
12
|
Li J, Zhang Y, Xu Q, Wang G, Jiang L, Wei
Q, Luo C, Chen L and Ying J: Systemic inflammatory markers of
resectable colorectal cancer patients with different mismatch
repair gene status. Cancer Manag Res. 13:2925–2935. 2021.
View Article : Google Scholar
|
|
13
|
Kim HS and Ku JH: Systemic inflammatory
response based on neutrophil-to-lymphocyte ratio as a prognostic
marker in bladder cancer. Dis Markers. 2016:83452862016. View Article : Google Scholar
|
|
14
|
Rice TW, Blackstone EH and Rusch VW: 7th
edition of the AJCC cancer staging manual: Esophagus and
esophagogastric junction. Ann Surg Oncol. 17:1721–1724. 2010.
View Article : Google Scholar
|
|
15
|
Charlson ME, Pompei P, Ales KL and
MacKenzie CR: A new method of classifying prognostic comorbidity in
longitudinal studies: Development and validation. J Chronic Dis.
40:373–383. 1987. View Article : Google Scholar
|
|
16
|
Cox JD, Stetz J and Pajak TF: Toxicity
criteria of the Radiation Therapy Oncology Group (RTOG) and the
European Organization for Research and Treatment of Cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar
|
|
17
|
Beukema JC, van Luijk P, Widder J,
Langendijk JA and Muijs CT: Is cardiac toxicity a relevant issue in
the radiation treatment of esophageal cancer? Radiother Oncol.
114:85–90. 2015. View Article : Google Scholar
|
|
18
|
Ishida N, Osawa S, Miyazu T, Kaneko M,
Tamura S, Tani S, Yamade M, Iwaizumi M, Hamaya Y, Furuta T and
Sugimoto K: Photodynamic therapy using talaporfin sodium for local
failure after chemoradiotherapy or radiotherapy for esophageal
cancer: A single center experience. J Clin Med. 9:15092020.
View Article : Google Scholar
|
|
19
|
Danieli M and Gronchi A: Staging systems
and nomograms for soft tissue sarcoma. Curr Oncol. 30:3648–3671.
2023. View Article : Google Scholar
|
|
20
|
Li S, Zhang H, Liao X, Yan X, Chen L, Lin
Y and Peng Y: The occurrence of early atrial fibrillation after
cardiac valve operation and the establishment of a nomogram model.
Front Cardiovasc Med. 10:10368882023. View Article : Google Scholar
|
|
21
|
Gu X, Shen H, Bai W, Xiang Z, Li X, Zhang
R, Shi F, Li H, Zhu G and Guo S: Endometrial cancer prognosis
prediction using correlation models based on CDK family genes.
Front Genet. 13:10216002022. View Article : Google Scholar
|
|
22
|
Wang B, Jiang X, Tian D and Geng W:
Enteral nutritional support in patients undergoing
chemoradiotherapy for esophageal carcinoma. Future Oncol.
16:2949–2957. 2020. View Article : Google Scholar
|
|
23
|
Cao J, Xu H, Li W, Guo Z, Lin Y, Shi Y, Hu
W, Ba Y, Li S, Li Z, et al: Nutritional assessment and risk factors
associated to malnutrition in patients with esophageal cancer. Curr
Probl Cancer. 45:1006382021. View Article : Google Scholar
|
|
24
|
Okadome K, Baba Y, Yagi T, Kiyozumi Y,
Ishimoto T, Iwatsuki M, Miyamoto Y, Yoshida N, Watanabe M and Baba
H: Prognostic nutritional index, tumor-infiltrating lymphocytes,
and prognosis in patients with esophageal cancer. Ann Surg.
271:693–700. 2020. View Article : Google Scholar
|
|
25
|
Wang Z, Wang Y, Zhang X and Zhang T:
Pretreatment prognostic nutritional index as a prognostic factor in
lung cancer: Review and meta-analysis. Clin Chim Acta. 486:303–310.
2018. View Article : Google Scholar
|
|
26
|
Wang X and Wang Y: The prognostic
nutritional index is prognostic factor of gynecological cancer: A
systematic review and meta-analysis. Int J Surg. 67:79–86. 2019.
View Article : Google Scholar
|
|
27
|
Yao J, Cui Q, Fan W, Ma Y, Chen Y, Liu T,
Zhang X, Xi Y, Wang C, Peng L, et al: Single-cell transcriptomic
analysis in a mouse model deciphers cell transition states in the
multistep development of esophageal cancer. Nat Commun.
11:37152020. View Article : Google Scholar
|
|
28
|
O'Sullivan KE, Phelan JJ, O'Hanlon C,
Lysaght J, O'Sullivan JN and Reynolds JV: The role of inflammation
in cancer of the esophagus. Expert Rev Gastroenterol Hepatol.
8:749–760. 2014. View Article : Google Scholar
|
|
29
|
Shavakhi M, Nourigheimasi S, Dioso E,
Goutnik M, Lucke-Wold B, Khanzadeh S and Heidari F: Prognostic role
of neutrophil to lymphocyte ratio in nonalcoholic fatty liver
disease: A systematic review and meta-analysis. Can J Gastroenterol
Hepatol. 2022:15540792022. View Article : Google Scholar
|
|
30
|
Demirel ME and Akunal Turel C: The role of
the multi-inflammatory index as a novel predictor of hospital
mortality in acute ischemic stroke. Cureus. 15:e432582023.
|
|
31
|
Sun Y and Zhang L: The clinical use of
pretreatment NLR, PLR, and LMR in patients with esophageal squamous
cell carcinoma: Evidence from a meta-analysis. Cancer Manag Res.
10:6167–6179. 2018. View Article : Google Scholar
|
|
32
|
Ishibashi Y, Tsujimoto H, Einama T,
Mochizuki S, Kouzu K, Nomura S, Ito N, Harada M, Sugasawa H, Shinto
E, et al: Correlation between immunoinflammatory measures and
periostin expression in esophageal squamous cell carcinoma: A
single-center, retrospective cohort study. Ann Surg Oncol.
28:1228–1237. 2021. View Article : Google Scholar
|