Introduction
Herpes simplex virus (HSV) infection is one of the
most common viral infections worldwide, affecting approximately 67%
of the world population under age 50 (1). HSV usually causes skin and mucosal
lesions that heal spontaneously, but poses complex diagnostic
challenges for clinicians when underlying disease, especially
malignancies, are hidden (2).
Recent epidemiological studies have revealed the potential
involvement of viral infections in cancer development, indicating
that chronic viral infections may contribute to carcinogenesis
through various mechanisms (3).
Oral squamous cell carcinoma (SCC) remains a
significant global health problem with increasing incidence,
especially among younger adults. Traditional risk factors include
tobacco use, alcohol consumption, and human papillomavirus (HPV)
infection. The relationship between HSV infection and oral
malignancies has attracted attention in recent years, particularly
regarding its potential role in masking or modifying pre-existing
lesions (4). Although the molecular
mechanisms underlying this association have not been fully
elucidated, emerging evidence suggests that virus-induced
inflammation, immunomodulation, and direct cellular effects may
contribute to malignant transformation (5).
The relationship between viral infection and
carcinogenesis is particularly important in the oral cavity, where
persistent inflammatory responses and repeated tissue damage can
create a microenvironment that favors the progression of the
tumorigenesis cascade (6).
Persistent viral infection can alter local immune responses,
promote cellular proliferation, and progression of pre-existing
dysplastic changes (7).
However, the contribution of HSV to the development
of oral SCC has not yet been clearly elucidated. In this report, we
describe a rare case in which an HSV-induced ulcer led to the
diagnosis of tongue SCC. This case demonstrates the importance of
thorough evaluation of persistent oral lesions, especially in
patients with significant risk factors such as smoking and alcohol
consumption.
Case report
A 37-year-old man presented to the Department of
Oral and Maxillofacial Surgery, Asahikawa Medical University
(Asahikawa, Japan) in June 2017 with a three-day history of tongue
pain and a low-grade fever of 37°C. The patient reported that he
had noticed a white lesion on the left border of tongue more than
10 years ago, but had not sought medical attention because it was
asymptomatic. Recently, the lesion became painful, and he visited
his dentist, who suspected a tongue tumor and referred him to our
department for further examination. The patient had no significant
medical history but reported a 20-year history of heavy smoking (40
cigarettes per day) and alcohol consumption, averaging
approximately 3 units per day, mainly whiskey and spirits.
The patient appeared well-nourished and normal
built, with a recorded temperature of 37.3°C. Intraoral examination
revealed no sharp cusps or broken teeth, and there were no signs of
traumatic occlusion or parafunctional habits. No ill-fitting dental
prostheses or sharp edges of dental restorations that could cause
chronic irritation to the tongue were observed. A shallow ulcer,
measuring 28×20 mm in diameter, with induration and intense
tenderness to touch was observed on the left lateral border of the
tongue (Fig. 1). Residual
leukoplakia and erythema were present around the ulcer. Extraoral
examination revealed a soybean-sized swollen left submandibular
lymph node with mild tenderness. The left superior internal jugular
lymph node was also thumb-sized and palpable.
Contrast-enhanced computed tomography (CT) confirmed
a shallow enhancing lesion in the left tongue, and the left
submandibular and upper internal jugular lymph nodes were also
enlarged (Fig. 2A-C). Blood tests
revealed mild leukocytosis (WBC: 10,500/µl) with 75% neutrophils
and a slight increase in C-reactive protein (CRP: 0.6 mg/dl). Liver
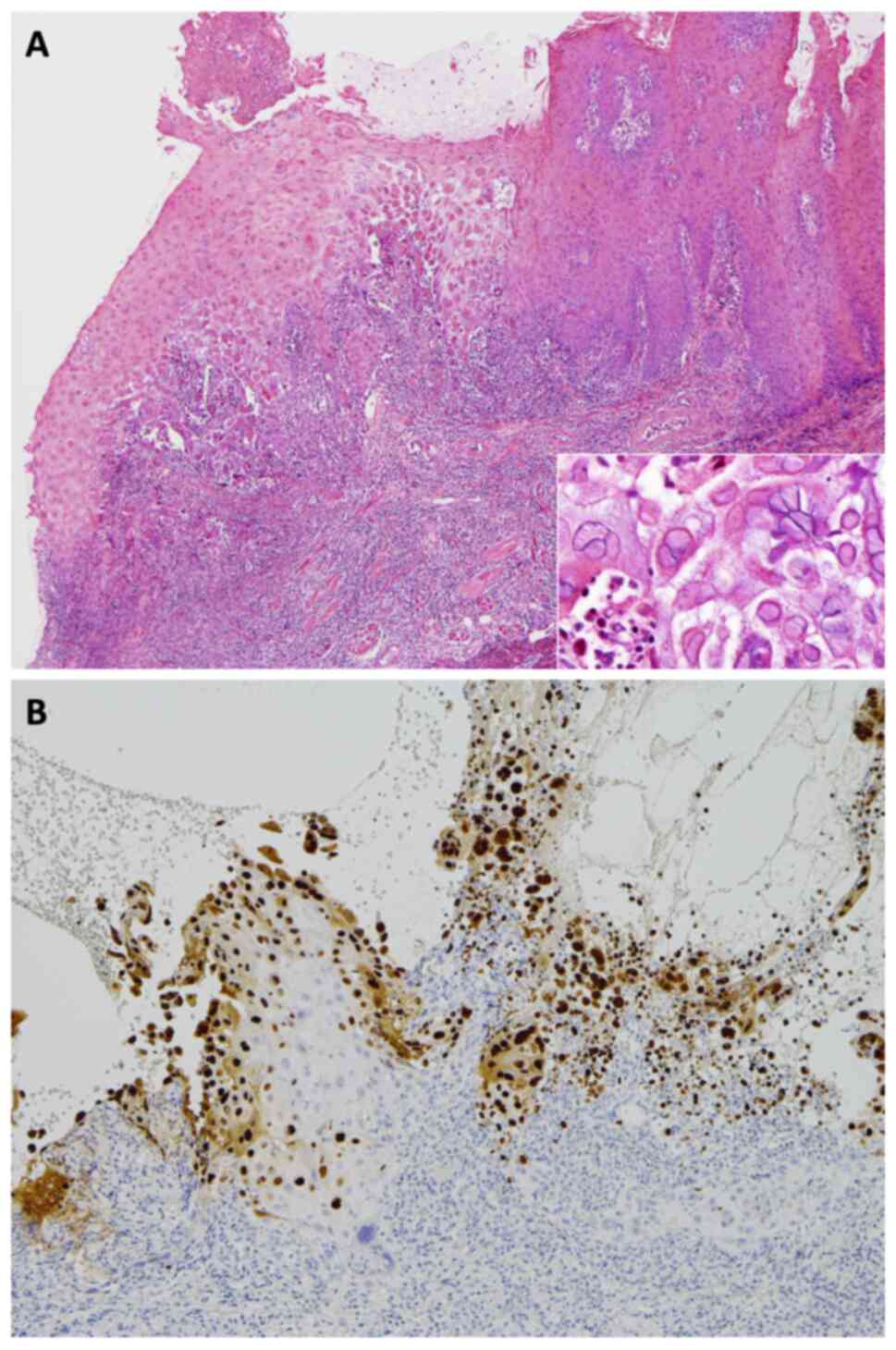
and renal function tests were within normal limits. A biopsy of the
tongue ulcer was performed, and histopathological examination
revealed typical features of HSV infection, including
multinucleation, molding of nuclear contours, and intranuclear
inclusions, which were positive for HSV1 by immunohistochemistry
(Fig. 3A and B). Serological
testing showed elevated HSV IgM levels and low HSV IgG levels,
suggesting primary HSV infection. The patient's clinical symptoms
subsided within 1 week without antiviral treatment, and a follow-up
examination demonstrated increasing HSV IgG titers.
Two months later, magnetic resonance imaging (MRI)
revealed decrease in signal intensity at the site of lesion and
shrinkage of the affected lymph nodes. However, leukoplakia and
erythroplakia persisted (Fig. 4),
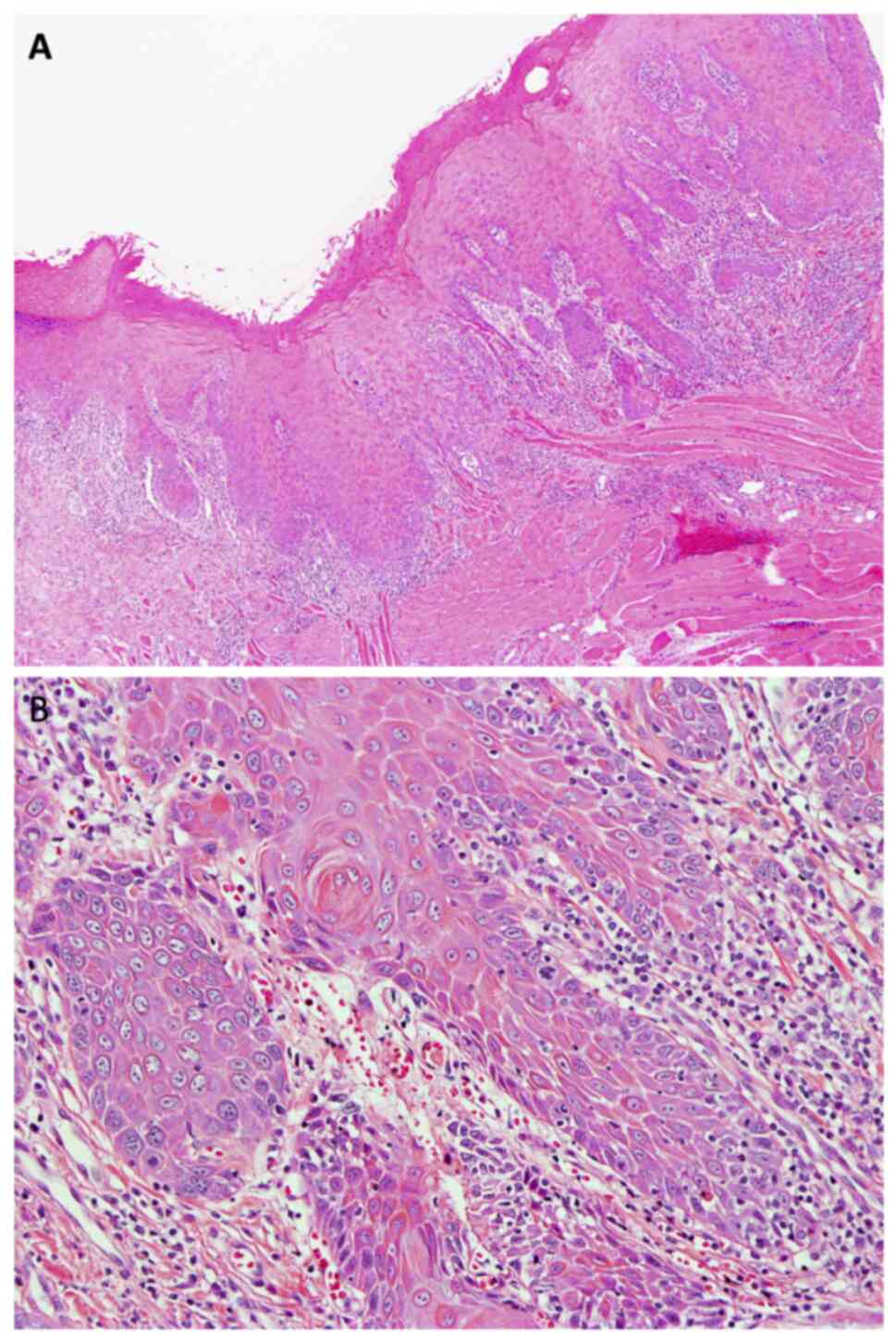
necessitating a second biopsy. Histopathological diagnosis showed
atypical squamous epithelium with inflammation but could not
confirm malignancy (Fig. 5A and B).
Due to the suspicious clinical findings, the patient was advised to
undergo partial glossectomy.
Before resection, Lugol's iodine staining was
performed to differentiate the lesion. Unstained area corresponding
to the leukoplakia and erythroplakia were identified (Fig. 6). A partial glossectomy was
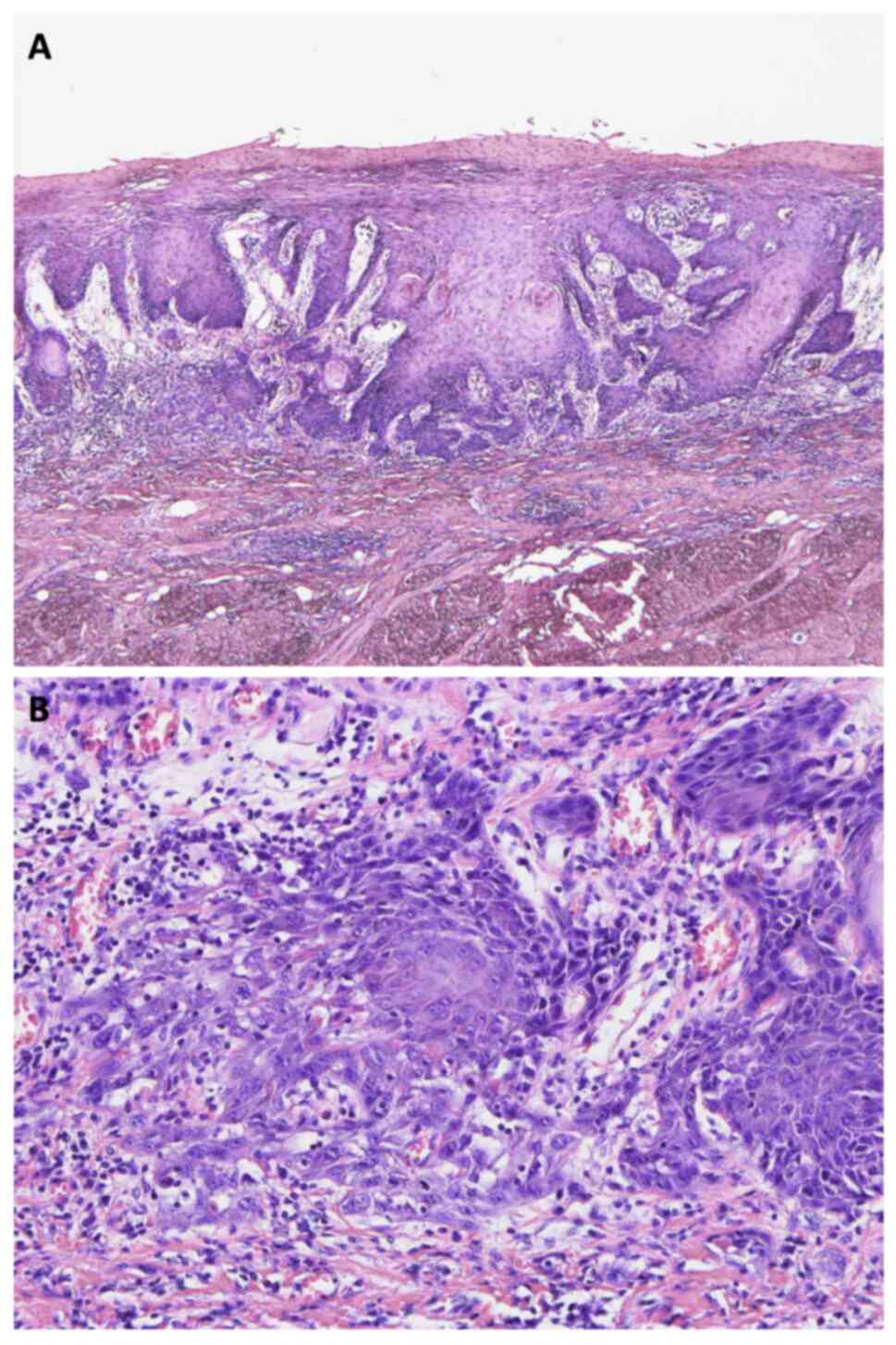
performed with a 10-mm safety margin. Histopathological analysis of
the resected specimen confirmed squamous cell carcinoma (pT1N0M0)
with tumor-free margins (Fig. 7A and
B). Notably, no HSV-infected cells were detected in the
resected specimen.
The patient's postoperative course was uneventful,
with no pain and surgical site healed completely. One month after
surgery, fluorodeoxyglucose positron emission tomography (FDG-PET)
and upper gastrointestinal endoscopy were performed, which showed
no signs of recurrence, metastasis, or synchronous malignancy. The
patient has been followed up for 7 year after surgery and has shown
no signs of recurrence or metastasis.
Discussion
This case of oral SCC in a 37-year-old patient
raises several important clinical and biological considerations.
Despite the patient's significant smoking and alcohol history, the
early age of onset suggests additional underlying factors may have
contributed to carcinogenesis. Growing evidence indicates that
early-onset oral cancer may be associated with genetic
predisposition and immune system alterations (8), including mutations in tumor suppressor
genes such as TP53 and CDKN2A (9).
The TP53 pathway, in particular, plays a crucial role in DNA damage
response and cell cycle regulation, while CDKN2A regulates the cell
cycle through the p16 and p14ARF proteins (10). Disruption of these pathways can lead
to compromised genome stability and altered immune surveillance
(11). Although we did not perform
genetic or detailed immunological analyses in our patient, such
evaluations might prove valuable in similar cases to better
understand the pathogenesis of early-onset oral cancer,
particularly in the context of environmental risk factors. The case
was further complicated by HSV infection, which initially masked
the underlying malignancy, highlighting the challenges in early
detection of oral cancer when concurrent pathologies are
present.
The patient's extensive history of smoking and
alcohol consumption represents significant risk factors for oral
carcinogenesis. Tobacco smoke contains numerous carcinogens,
particularly tobacco-specific nitrosamines (TSNAs), which can form
DNA adducts leading to mutations in critical genes (12). Alcohol acts synergistically by
serving as a solvent for these carcinogens, increasing cellular
permeability, and generating acetaldehyde, a potent carcinogen
(13). This combined exposure can
lead to accumulation of oxidative stress, activation of
pro-inflammatory pathways, and disruption of DNA repair mechanisms
(14). The chronic exposure to
these agents can create a field cancerization effect, potentially
explaining the early onset of malignancy in this case despite the
patient's young age (15,16).
The transition from an asymptomatic leukoplakia to a
painful lesion after 10 years coincided with HSV infection. The
acute pain was attributed to the viral-induced inflammation and
ulceration, as evidenced by the elevated inflammatory markers and
the characteristic histopathological features of HSV infection. The
resolution of pain following viral clearance, while suspicious
features persisted, supports this interpretation. This temporal
relationship between viral infection and symptom onset illustrates
how HSV infection can alter the clinical presentation of
pre-existing lesions.
In this case, considering the long-standing history
of leukoplakia, it is more likely that HSV infection occurred in
the context of pre-existing dysplastic changes rather than being a
causative factor. Several lines of evidence support this
interpretation: First, the patient had a 10-year history of
leukoplakia prior to HSV infection. Second, while the viral-related
symptoms resolved completely, the underlying suspicious features
persisted. Third, the final surgical specimen showed no evidence of
HSV-infected cells, suggesting that the viral infection was a
temporary event superimposed on a pre-existing pathological
process. Recent molecular biology studies have elucidated various
interactions between HSV infection and existing neoplastic tissue.
HSV infection may trigger specific immune responses and create a
pro-inflammatory microenvironment, potentially contributing to
tumor progression (17).
Furthermore, HSV proteins may interact with cellular regulatory
machinery inhibit normal cell cycle control and apoptotic pathways
(18). In the present case, HPV
testing was not performed, which is a limitation of our study. HPV
is recognized as one of the major risk factors for oral squamous
cell carcinoma, particularly in younger patients (7). Recent studies have suggested that
co-infection with HSV and HPV may increase carcinogenic risk. HSV
infection can cause persistent inflammation and create local
immunosuppressive conditions that may promote persistent HPV
infection (19). Furthermore, HSV
envelope proteins have been suggested to inhibit cellular tumor
suppression mechanisms, potentially enhancing the expression of
HPV-derived oncogenes (20,21). Considering these mechanisms, if our
patient had been HPV-positive, dual viral infection might have
contributed to carcinogenesis. Future similar cases should consider
HPV testing as part of the diagnostic workup.
The immunological aspects of viral-cancer
interactions are particularly noteworthy. Chronic viral infections
may modulate the immune system, creating conditions favorable for
tumor development and progression (22). This immune modulation may be
particularly important in patients with additional risk factors,
such as patient's history of heavy smoking and alcohol
consumption.
The diagnostic challenges presented by this case
demonstrate the importance of a strong suspicion of underlying
malignancy in cases of persistent or atypical viral infections,
especially in high-risk patients. The synergistic effect of
multiple risk factors has been shown to significantly increase the
likelihood of malignant transformation (23).
The initial misleading biopsy results in this case
highlight important technical considerations in the diagnosis of
oral cancer. The timing, location, and method of biopsy can
significantly impact diagnostic accuracy, particularly in the
presence of concurrent HSV infection. Biopsies performed during
acute inflammation may be compromised by necrotic tissue and
inflammatory changes, potentially obscuring underlying malignancy.
Additionally, sampling from the center of ulcerative lesions may
miss diagnostic tissue, as these areas often contain primarily
inflammatory or necrotic material. In retrospect, multiple biopsies
from the periphery of the lesion, including apparently healthy
marginal tissue, might have provided more accurate initial results.
Furthermore, when initial biopsies are inconclusive but clinical
suspicion remains high, repeat biopsies after the resolution of
acute inflammation should be considered. This approach, along with
careful selection of biopsy sites guided by clinical features such
as induration or color changes, may help avoid diagnostic delays in
similar cases.
From a clinical perspective, this case provides
several important insights. The presence of persistent leukoplakia
or dysplastic lesions requires careful attention. As demonstrated
in our case, HSV infection can potentially delay the diagnosis of
underlying malignancy, emphasizing the need for thorough clinical
follow-up. This is particularly important when patients present
with a long-standing history of oral lesions, even if they were
previously asymptomatic.
Additionally, comprehensive risk assessment should
consider not only traditional factors such as smoking and alcohol
consumption, but also the potential impact of viral infections. The
presence of ulceration, leukoplakia, and erythroplakia should raise
suspicion and warrant further investigations, including serial
biopsies, to rule out malignancy. A holistic understanding of these
combined risk factors can help clinicians in identifying high-risk
patients and tailor surveillance accordingly. Finally, this case
illustrates the value of repeat examinations and imaging when
initial findings appear benign but clinical suspicion remains high.
This approach allows for early detection of progressing pathology,
allowing for timely intervention and improved patient outcomes.
In conclusion, this case demonstrates the complex
interplay between viral infection and oral cancer and emphasizes
the importance of thorough evaluation and follow-up in cases of
persistent oral lesions. The presence of HSV infection should not
deter clinicians from considering potential malignancies,
especially in patients with additional risk factors. Further
studies are needed to fully elucidate the mechanisms by which viral
infection influence the development and progression of cancer in
the oral cavity.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MT and MA conceived and designed the study. HS, MT
and SY analyzed and confirmed the imaging examination results. HS,
MT and SY analyzed and confirmed the pathological data. MM and SM
performed the surgery and provided surgical expertise to the study.
HS, MT and SY confirm the authenticity of all the raw data. HS
drafted the manuscript, and MT, SY and MA revised it before
submission. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
the publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
James C, Harfouche M, Welton NJ, Turner
KM, Abu-Raddad LJ, Gottlieb SL and Looker KJ: Herpes simplex virus:
Global infection prevalence and incidence estimates, 2016. Bull
World Health Organ. 98:315–329. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kamala KA, Ashok L and Annigeri RG: Herpes
associated erythema multiforme. Contemp Clin Dent. 2:372–375. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zapatka M, Borozan I, Brewer DS, Iskar M,
Grundhoff A, Alawi M, Desai N, Sültmann H, Moch H; PCAWG Pathogens,
; et al: The landscape of viral associations in human cancers. Nat
Genet. 52:320–330. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koivikko T, Rodrigues PC, Vehvilainen M,
Hyvönen P, Sundquist E, Arffman RK, Al-Samadi A, Välimaa H, Salo T
and Risteli M: Detection of herpes simplex virus in oral tongue
squamous cell carcinoma. Front Pharmacol. 14:11821522023.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cao S, Wylie KM, Wyczalkowski MA, Karpova
A, Ley J, Sun S, Mashl RJ, Liang WW, Wang X, Johnson K, et al:
Dynamic host immune response in virus-associated cancers. Commun
Biol. 2:1092019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Niklander SE: Inflammatory mediators in
oral cancer: Pathogenic mechanisms and diagnostic potential. Front
Oral Health. 2:6422382021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fakhry C, Blackford AL, Neuner G, Xiao W,
Jiang B, Agrawal A and Gillison ML: Association of oral human
papillomavirus DNA persistence with cancer progression after
primary treatment for oral cavity and oropharyngeal squamous cell
carcinoma. JAMA Oncol. 5:985–992. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Huang Y, Zhao J, Mao G, Lee GS, Zhang J,
Bi L, Gu L, Chang Z, Valentino J and Li GM: Identification of novel
genetic variants predisposing to familial oral squamous cell
carcinomas. Cell Discov. 5:572019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Adorno-Farias D, Morales-Pison S,
Gischkow-Rucatti G, Margarit S and Fernandez-Ramires R: Genetic and
epigenetic landscape of early-onset oral squamous cell carcinoma:
Insights of genomic underserved and underrepresented populations.
Genet Mol Biol. 47 (Suppl 1):e202400362024.PubMed/NCBI
|
|
10
|
Wang H, Guo M, Wei H and Chen Y: Targeting
p53 pathways: Mechanisms, structures, and advances in therapy.
Signal Transduct Target Ther. 8:922023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Borrero LJ and El-Deiry WS: Tumor
suppressor p53: Biology, signaling pathways, and therapeutic
targeting. Biochim Biophys Acta Rev Cancer. 1876:1885562021.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hecht SS: DNA adduct formation from
tobacco-specific N-nitrosamines. Mutat Res. 424:127–142. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rumgay H, Murphy N, Ferrari P and
Soerjomataram I: Alcohol and cancer: Epidemiology and biological
mechanisms. Nutrients. 13:31732021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mansoori AA and Jain SK: Molecular links
between alcohol and tobacco induced DNA damage, gene polymorphisms
and patho-physiological consequences: A systematic review of
hepatic carcinogenesis. Asian Pac J Cancer Prev. 16:4803–4812.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Muto M, Katada C, Yokoyama T, Yano T, Oda
I, Ezoe Y, Tanabe S, Shimizu Y, Doyama H, Koike T, et al: Field
effect of alcohol, cigarette smoking, and their cessation on the
development of multiple dysplastic lesions and squamous cell
carcinoma: A long-term multicenter cohort study. Gastro Hep Adv.
1:265–276. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hamilton AC, Donnelly DW, Fitzpatrick D
and Coleman HG: Early-Onset cancers in adults: A review of
epidemiology, supportive care needs and future research priorities.
Cancers (Basel). 14:40212022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang L, Wang W, Wang R, Zhang N, Shang H,
Bi Y, Chen D, Zhang C, Li L, Yin J, et al: Reshaping the immune
microenvironment by oncolytic herpes simplex virus in murine
pancreatic ductal adenocarcinoma. Mol Ther. 29:744–761. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Agelidis AM and Shukla D: Cell entry
mechanisms of HSV: What we have learned in recent years. Future
Virol. 10:1145–1154. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Guidry JT and Scott RS: The interaction
between human papillomavirus and other viruses. Virus Res.
231:139–147. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Walker JD, Sehgal I and Kousoulas KG:
Oncolytic herpes simplex virus 1 encoding 15-prostaglandin
dehydrogenase mitigates immune suppression and reduces ectopic
primary and metastatic breast cancer in mice. J Virol.
85:7363–7371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pisani S, Imperi M, Seganti L, Superti F,
Tinari A, Bucci M and Degener AM: Effect of HSV-2 infection on the
expression of HPV 16 genes in CaSki cells. Int J Immunopathol
Pharmacol. 17:65–70. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zuniga EI, Macal M, Lewis GM and Harker
JA: Innate and adaptive immune regulation during chronic viral
infections. Annu Rev Virol. 2:573–597. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Prabhu A, Obi KO and Rubenstein JH: The
synergistic effects of alcohol and tobacco consumption on the risk
of esophageal squamous cell carcinoma: A meta-analysis. Am J
Gastroenterol. 109:822–827. 2014. View Article : Google Scholar : PubMed/NCBI
|