|
1
|
Cardoso R, Guo F, Heisser T, Hackl M, Ihle
P, De Schutter H, Van Damme N, Valerianova Z, Atanasov T, Májek O,
et al: Colorectal cancer incidence, mortality, and stage
distribution in European countries in the colorectal cancer
screening era: An international population-based study. Lancet
Oncol. 22:1002–1013. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2021. CA Cancer J Clin. 71:7–33. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xi Y and Xu P: Global colorectal cancer
burden in 2020 and projections to 2040. Transl Oncol.
14:1011742021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Murphy N, Ward HA, Jenab M, Rothwell JA,
Boutron-Ruault MC, Carbonnel F, Kvaskoff M, Kaaks R, Kühn T, Boeing
H, et al: Heterogeneity of colorectal cancer risk factors by
anatomical subsite in 10 european countries: Amultinational cohort
study. Clin Gastroenterol Hepatol. 17:1323–1331.e6. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gausman V, Dornblaser D, Anand S, Hayes
RB, O'Connell K, Du M and Liang PS: Risk factors associated with
early-onset colorectal cancer. Clin Gastroenterol Hepatol.
18:2752–2759.e2. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jacobs ET, Thompson PA and Martínez ME:
Diet, gender, and colorectal neoplasia. J Clin Gastroenterol.
41:731–746. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
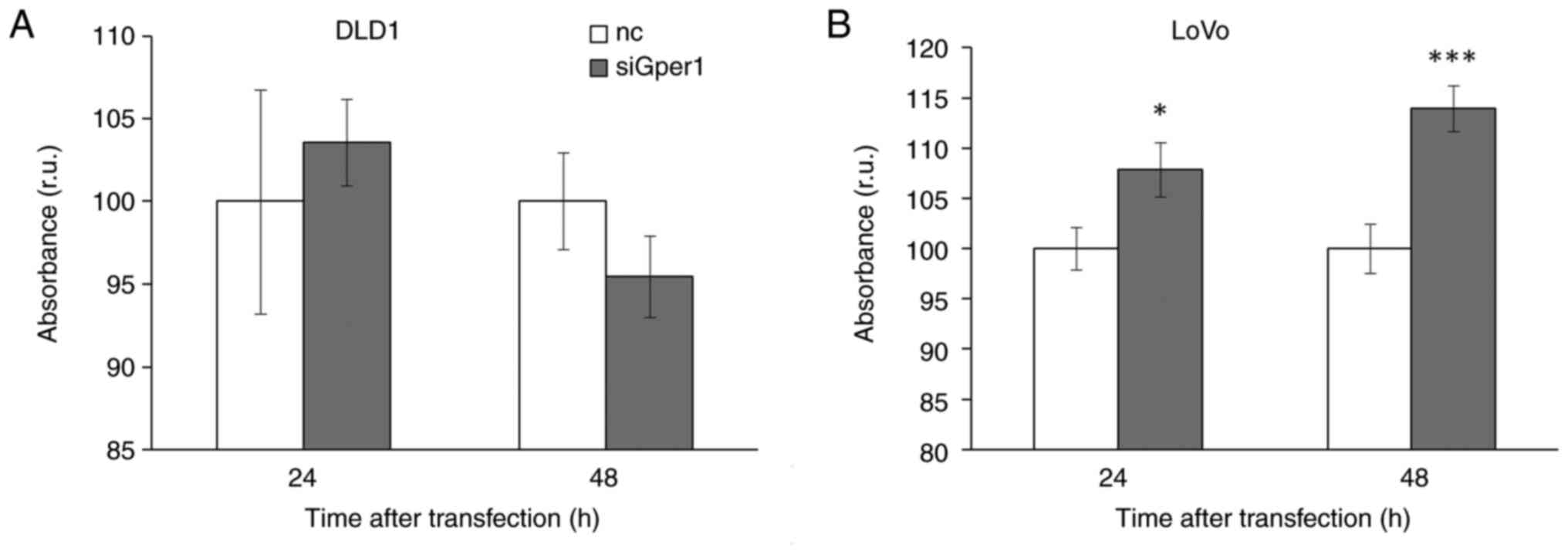
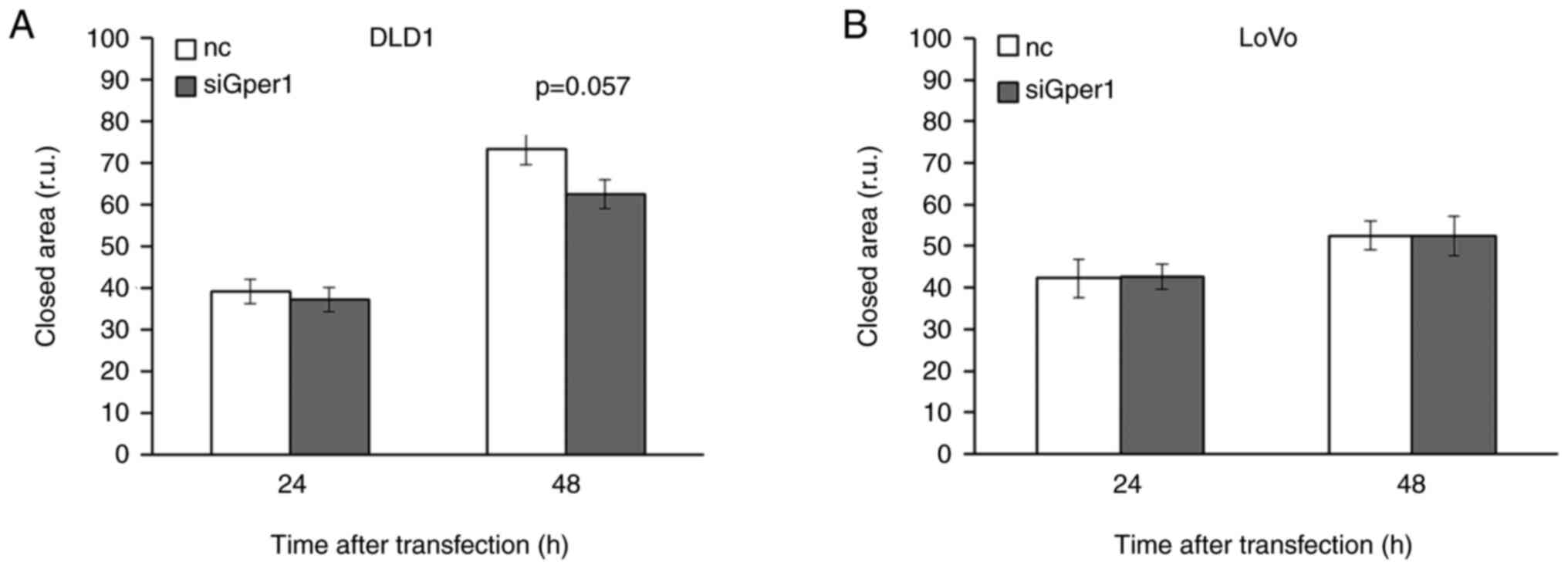
|
Quirt JS, Nanji S, Wei X, Flemming JA and
Booth CM: Is there a sex effect in colon cancer? Disease
characteristics, management, and outcomes in routine clinical
practice. Curr Oncol. 24:e15–e23. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lopes-Ramos CM, Quackenbush J and DeMeo
DL: Genome-wide sex and gender differences in cancer. Front Oncol.
10:5977882020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Høydahl Ø, Edna TH, Xanthoulis A, Lydersen
S and Endreseth BH: Long-term trends in colorectal cancer:
Incidence, localization, and presentation. BMC Cancer. 20:10772020.
View Article : Google Scholar : PubMed/NCBI
|
|
10
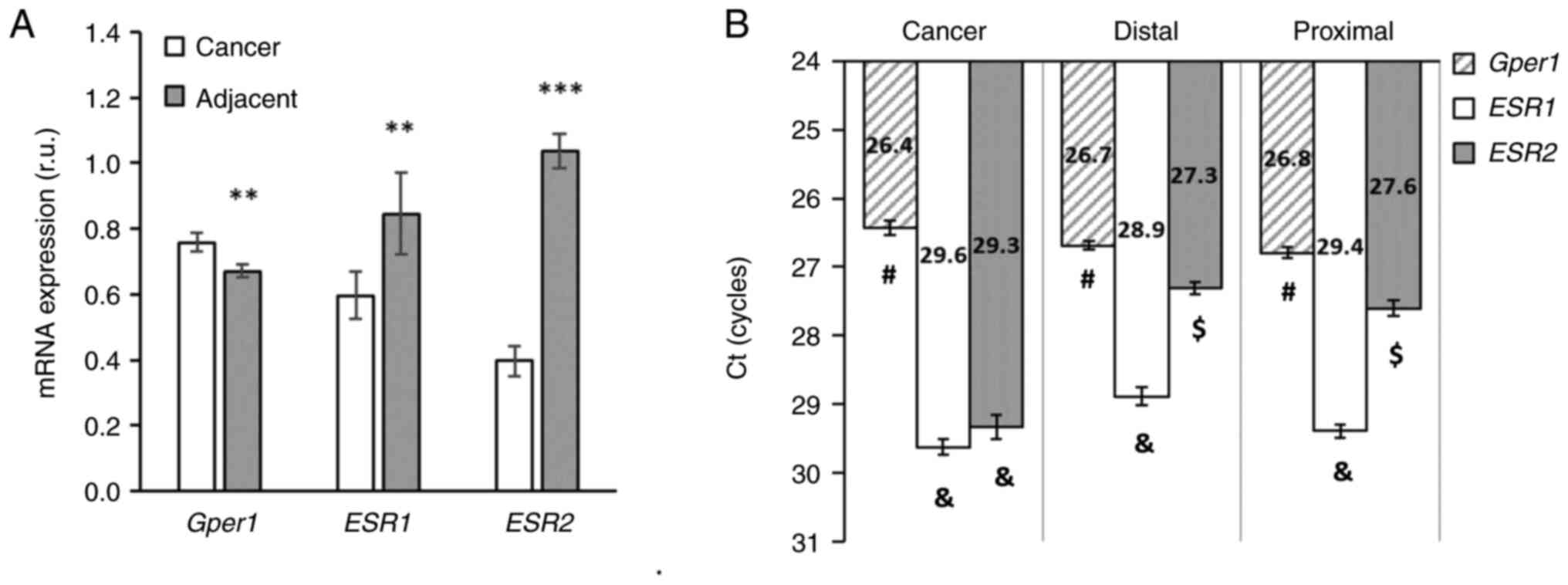
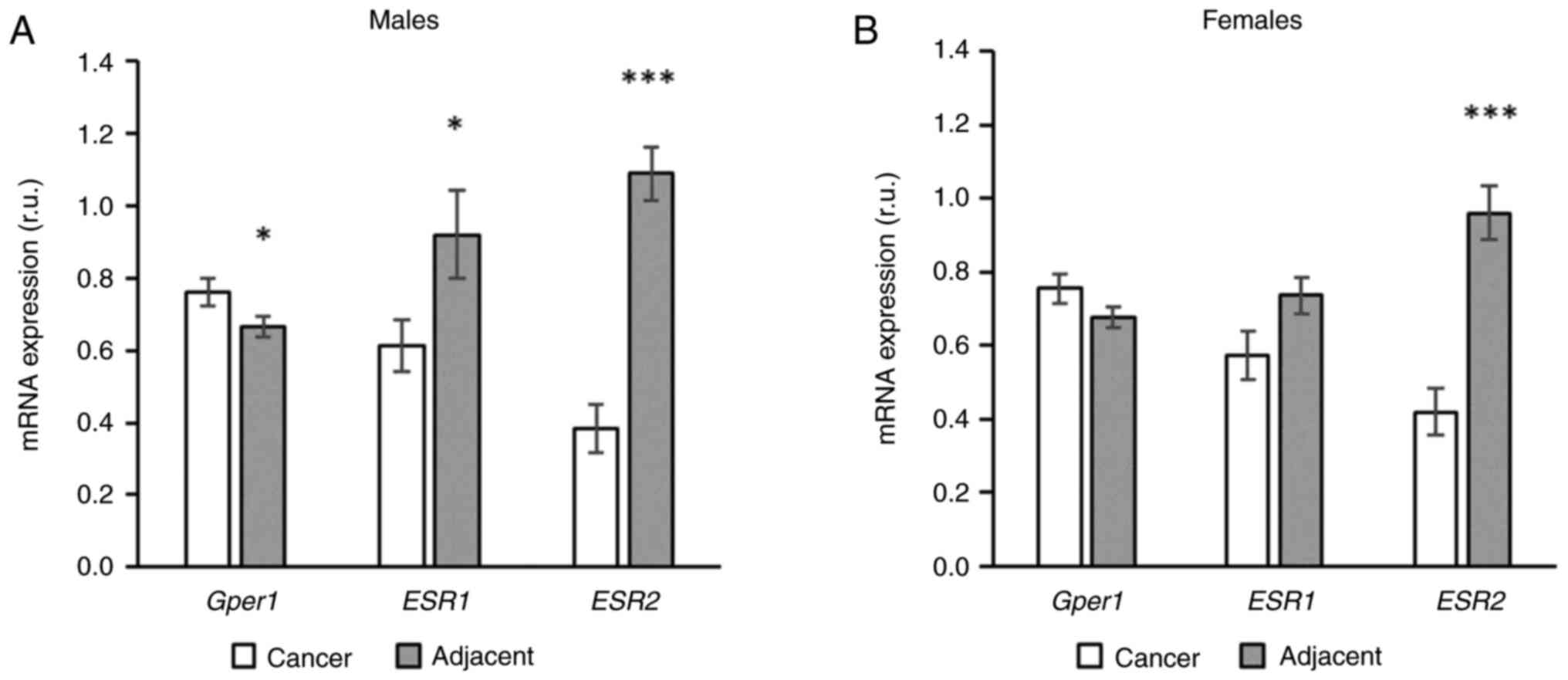
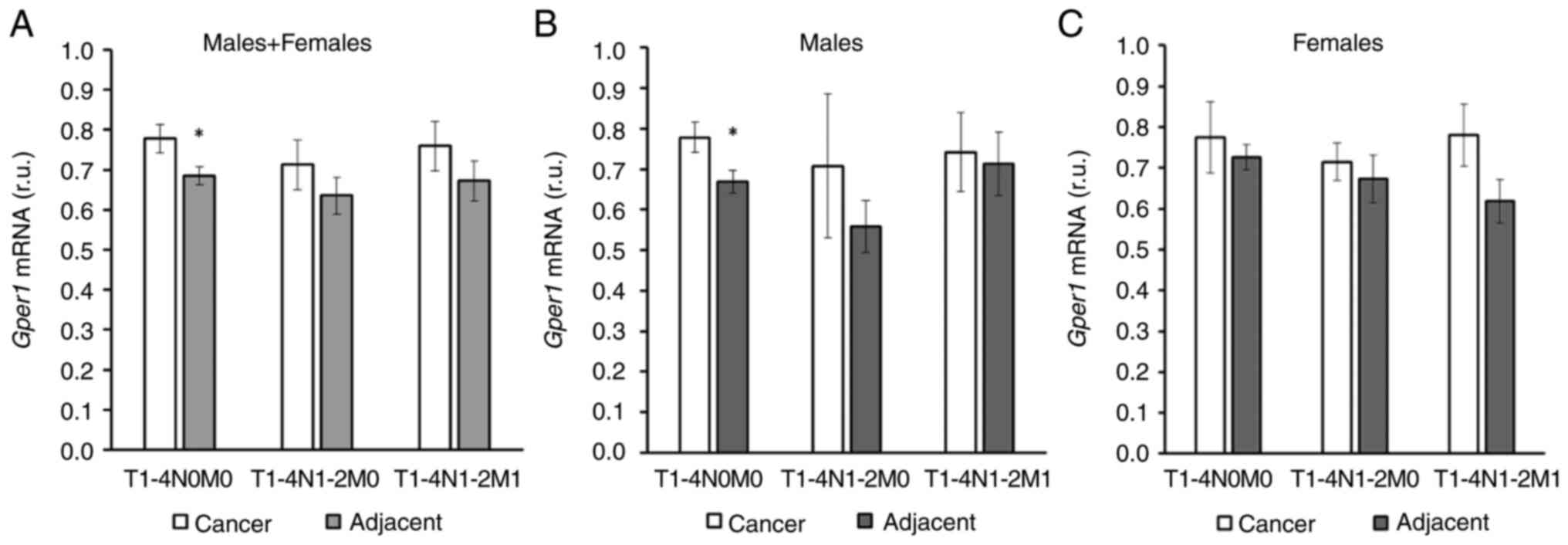
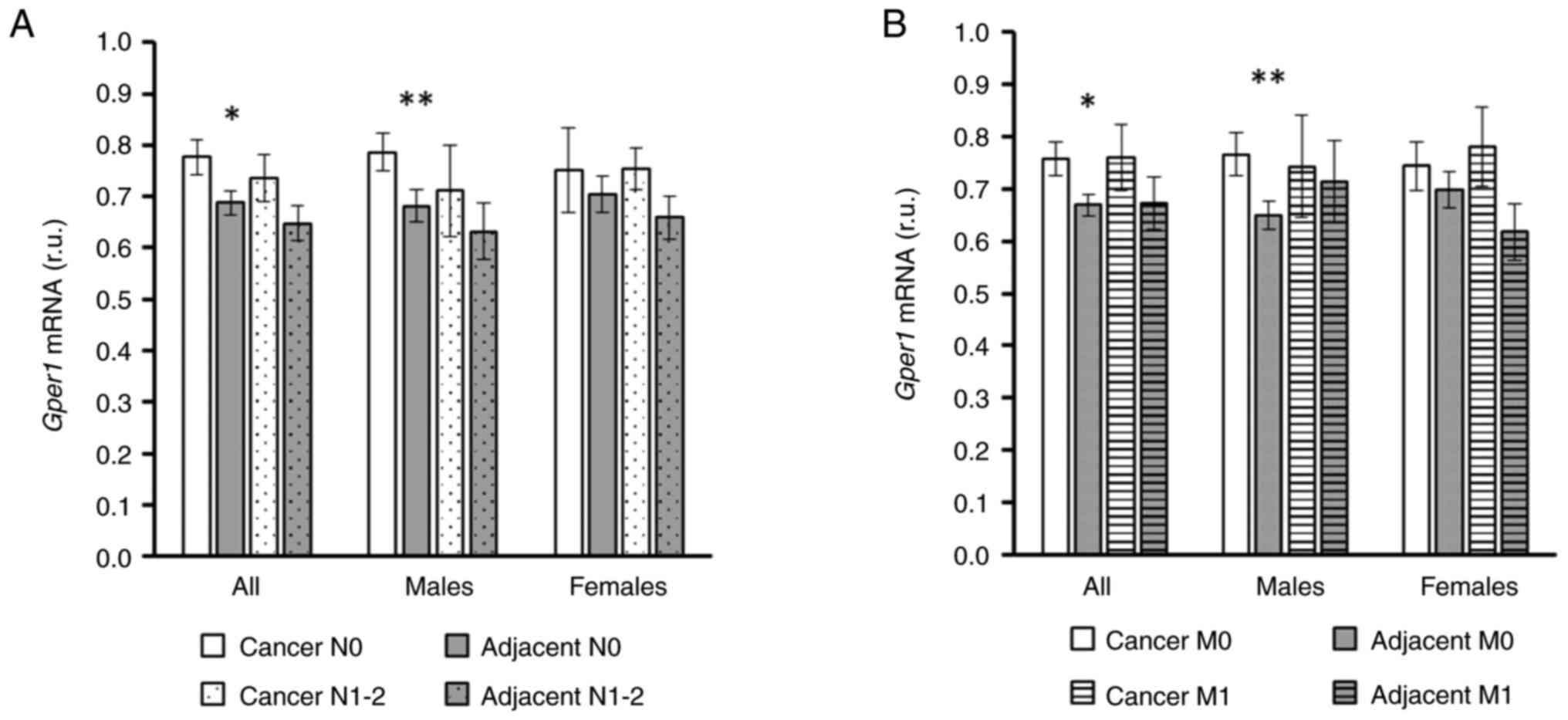
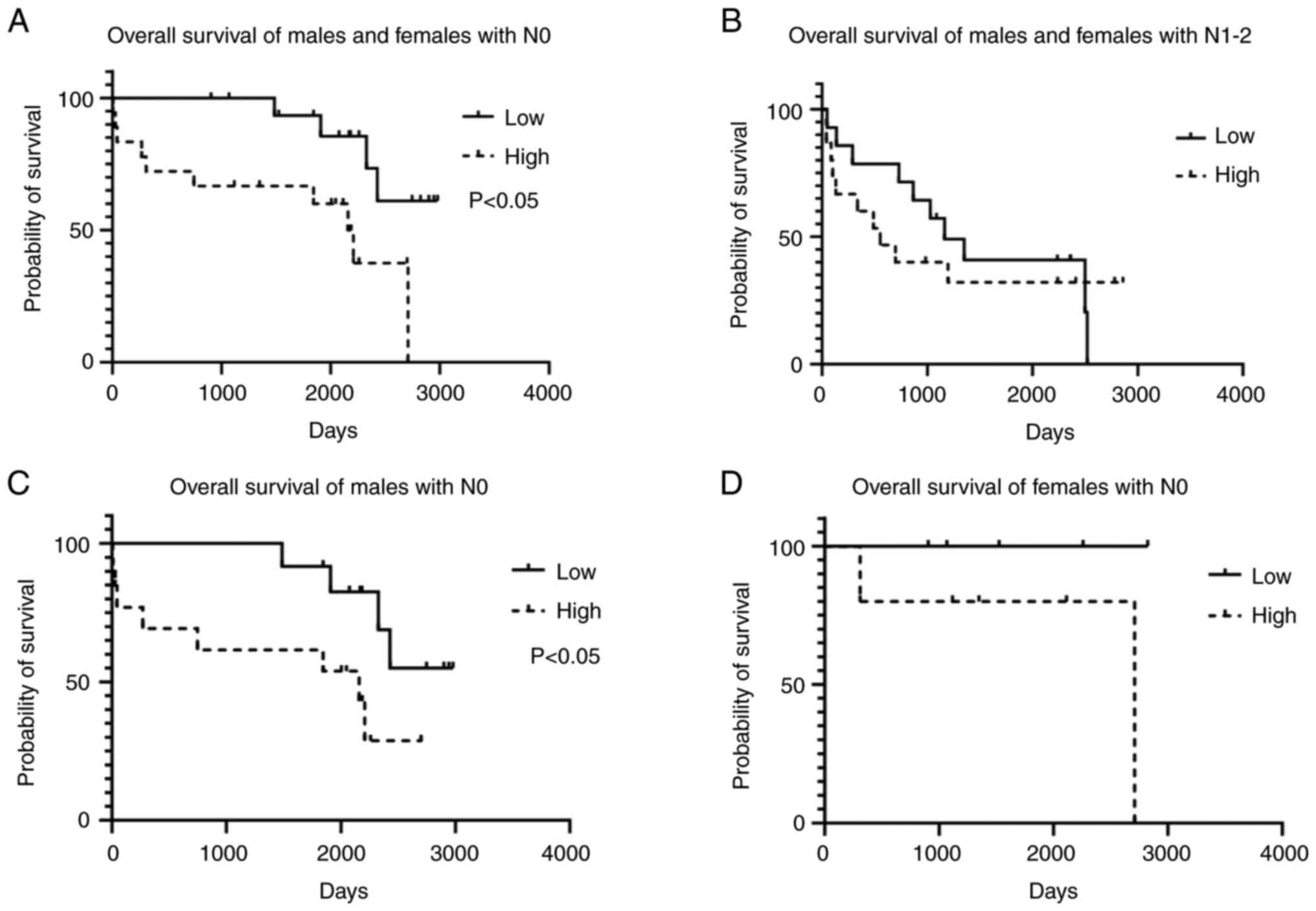
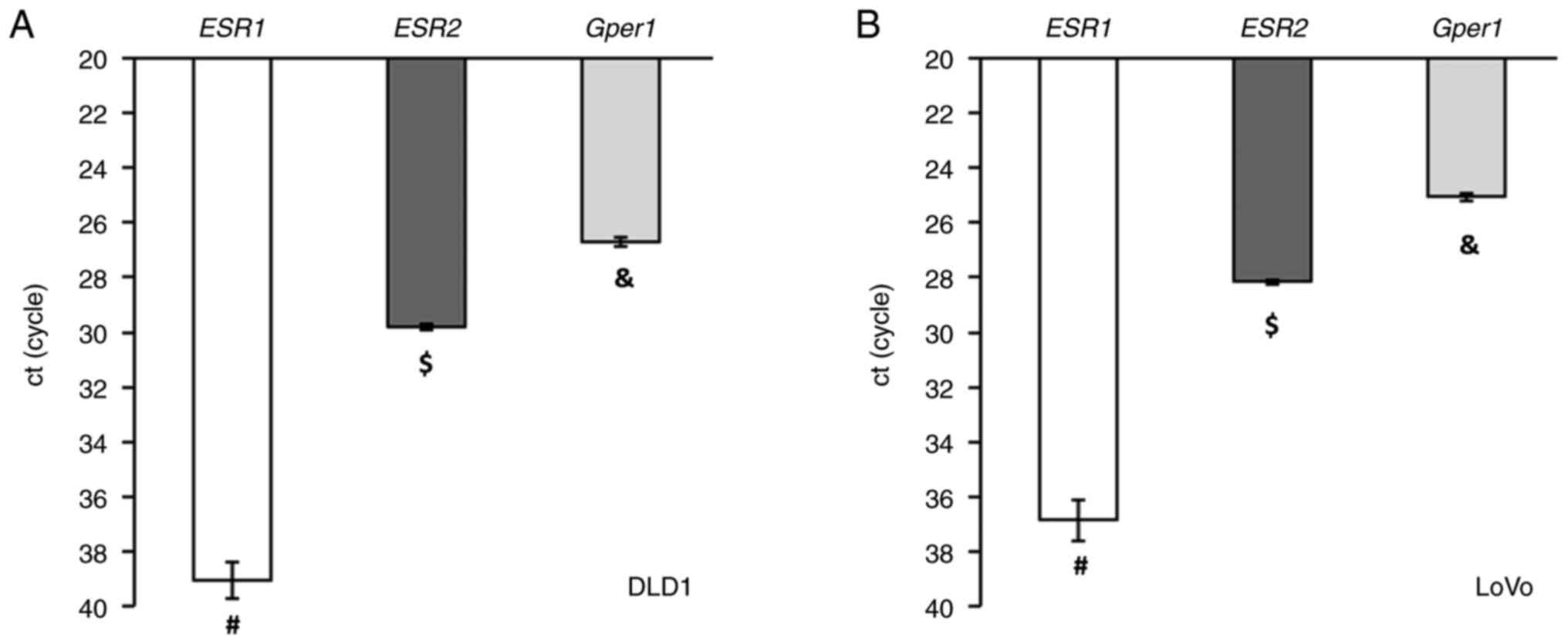
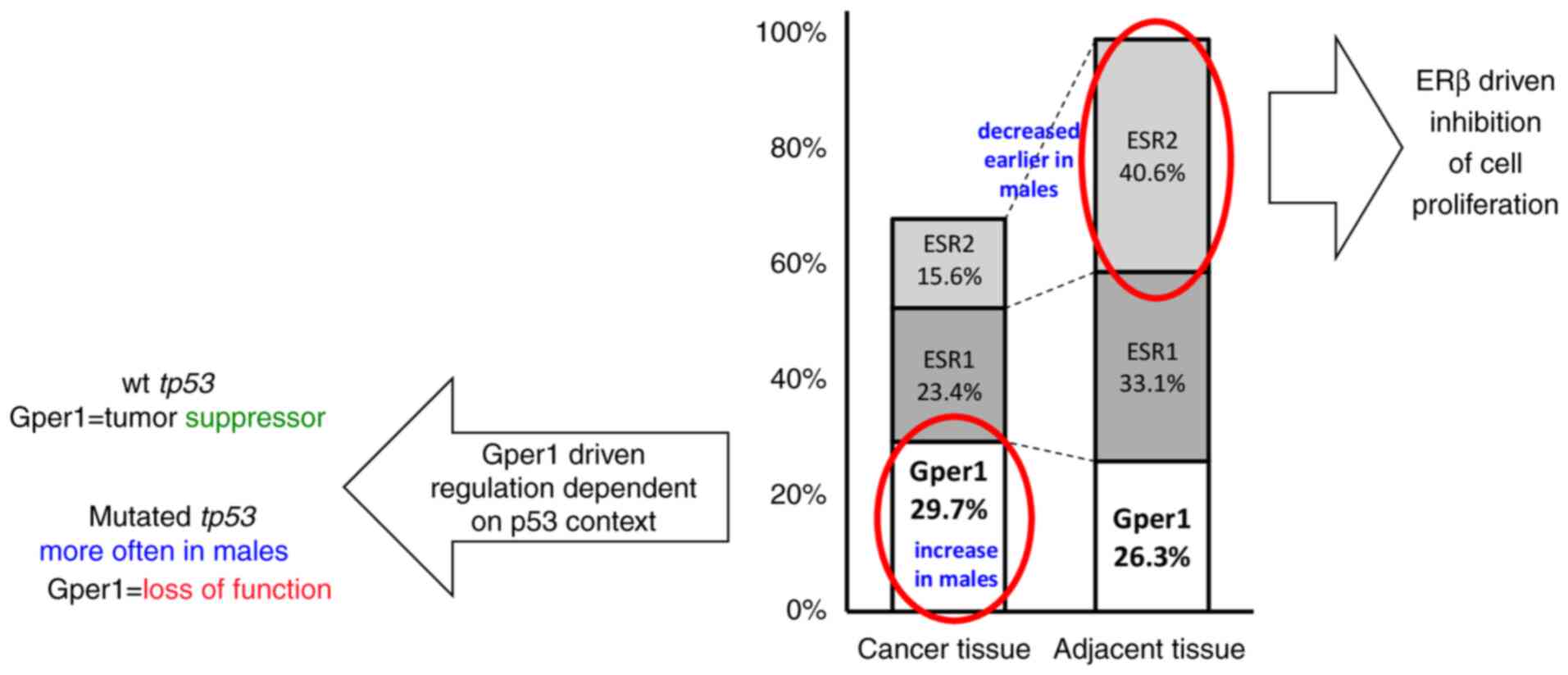
|
Johnson CM, Wei C, Ensor JE, Smolenski DJ,
Amos CI, Levin B and Berry DA: Meta-analyses of colorectal cancer
risk factors. Cancer Causes Control. 24:1207–1222. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Murphy N, Ward HA, Jenab M, Rothwell JA,
Boutron-Ruault MC, Carbonnel F, Kvaskoff M, Kaaks R, Kühn T, Boeing
H, et al: Heterogeneity of colorectal cancer risk factors by
anatomical subsite in 10 European countries: A multinational cohort
study. Clin Gastroenterol Hepatol. 17:1323–1331.e6. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Murphy N, Moreno V, Hughes DJ, Vodicka L,
Vodicka P, Aglago EK, Gunter MJ and Jenab M: Lifestyle and dietary
environmental factors in colorectal cancer susceptibility. Mol
Aspects Med. 69:2–9. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wele P, Wu X and Shi H: Sex-dependent
differences in colorectal cancer: With a focus on obesity. Cells.
11:36882022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Barzi A, Lenz AM, Labonte MJ and Lenz HJ:
Molecular pathways: Estrogen pathway in colorectal cancer. Clin
Cancer Res. 19:5842–5848. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nie X, Xie R and Tuo B: Effects of
estrogen on the gastrointestinal tract. Dig Dis Sci. 63:583–596.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Labadie JD, Harrison TA, Banbury B, Amtay
EL, Bernd S, Brenner H, Buchanan DD, Campbell PT, Cao Y, Chan AT,
et al: Postmenopausal hormone therapy and colorectal cancer risk by
molecularly defined subtypes and tumor location. JNCI Cancer
Spectr. 4:pkaa0422020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Qiu YA, Xiong J and Yu T: Role of G
Protein-coupled estrogen receptor in digestive system carcinomas: A
minireview. Onco Targets Ther. 14:2611–2622. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Prossnitz ER and Barton M: The G
protein-coupled oestrogen receptor GPER in health and disease: An
update. Nat Rev Endocrinol. 19:407–424. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Heldring N, Pike A, Andersson S, Matthews
J, Cheng G, Hartman J, Tujague M, Ström A, Treuter E, Warner M and
Gustafsson JA: Estrogen receptors: How do they signal and what are
their targets. Physiol Rev. 87:905–931. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fuentes N and Silveyra P: Estrogen
receptor signaling mechanisms. Adv Protein Chem Struct Biol.
116:135–170. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Otto C, Rohde-Schulz B, Schwarz G, Fuchs
I, Klewer M, Brittain D, Langer G, Bader B, Prelle K, Nubbemeyer R
and Fritzemeier KH: G protein-coupled receptor 30 localizes to the
endoplasmic reticulum and is not activated by estradiol.
Endocrinology. 149:4846–4856. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ahmadian Elmi M, Motamed N and Picard D:
Proteomic analyses of the G Protein-coupled estrogen receptor GPER1
reveal constitutive links to endoplasmic reticulum, glycosylation,
trafficking, and calcium signaling. Cells. 12:25712023. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mauvais-Jarvis F, Lange CA and Levin ER:
Membrane-initiated estrogen, androgen, and progesterone receptor
signaling in health and disease. Endocr Rev. 43:720–742. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ding Q, Chorazyczewski J, Gros R, Motulsky
HJ, Limbird LE and Feldman RD: Correlation of functional and
radioligand binding characteristics of GPER ligands confirming
aldosterone as a GPER agonist. Pharmacol Res Perspect.
10:e009952022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Leitman DC, Paruthiyil S, Vivar OI,
Saunier EF, Herber CB, Cohen I, Tagliaferri M and Speed TP:
Regulation of specific target genes and biological responses by
estrogen receptor subtype agonists. Curr Opin Pharmacol.
10:629–636. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
De Francesco EM, Lappano R, Santolla MF,
Marsico S, Caruso A and Maggiolini M: HIF-1α/GPER signaling
mediates the expression of VEGF induced by hypoxia in breast cancer
associated fibroblasts (CAFs). Breast Cancer Res. 15:R642013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rennert G, Rennert HS, Pinchev M, Lavie O
and Gruber SB: Use of hormone replacement therapy and the risk of
colorectal cancer. J Clin Oncol. 27:4542–4547. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Johnson JR, Lacey JV Jr, Lazovich D,
Geller MA, Schairer C, Schatzkin A and Flood A: Menopausal hormone
therapy and risk of colorectal cancer. Cancer Epidemiol Biomarkers
Prev. 18:196–203. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Symer MM, Wong NZ, Abelson JS, Milsom JW
and Yeo HL: Hormone replacement therapy and colorectal cancer
incidence and mortality in the prostate, lung, colorectal, and
ovarian cancer screening trial. Clin Colorectal Cancer.
17:e281–e288. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jang YC, Huang HL and Leung CY:
Association of hormone replacement therapy with mortality in
colorectal cancer survivor: A systematic review and meta-analysis.
BMC Cancer. 19:11992019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hang D, He X, Kværner AS, Chan AT, Wu K,
Ogino S, Hu Z, Shen H, Giovannucci EL and Song M: Plasma sex
hormones and risk of conventional and serrated precursors of
colorectal cancer in postmenopausal women. BMC Med. 19:182021.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Foster PA: Oestrogen and colorectal
cancer: Mechanisms and controversies. Int J Colorectal Dis.
28:737–749. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mori N, Keski-Rahkonen P, Gicquiau A,
Rinaldi S, Dimou N, Harlid S, Harbs J, Van Guelpen B, Aune D, Cross
AJ, et al: Endogenous circulating sex hormone concentrations and
colon cancer risk in postmenopausal women: A prospective study and
meta-analysis. JNCI Cancer Spectr. 5:pkab0842021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Das PK, Saha J, Pillai S, Lam AK, Gopalan
V and Islam F: Implications of estrogen and its receptors in
colorectal carcinoma. Cancer Med. 12:4367–4379. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mal R, Magner A, David J, Datta J,
Vallabhaneni M, Kassem M, Manouchehri J, Willingham N, Stover D,
Vandeusen J, et al: Estrogen receptor beta (ERβ): A ligand
activated tumor suppressor. Front Oncol. 10:5873862020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Mahbub AA, Aslam A, Elzubier ME, El-Boshy
M, Abdelghany AH, Ahmad J, Idris S, Almaimani R, Alsaegh A,
El-Readi MZ, et al: Enhanced anti-cancer effects of oestrogen and
progesterone co-therapy against colorectal cancer in males. Front
Endocrinol (Lausanne). 13:9418342022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Refaat B, Aslam A, Idris S, Almalki AH,
Alkhaldi MY, Asiri HA, Almaimani RA, Mujalli A, Minshawi F, Alamri
SA, et al: Profiling estrogen, progesterone, and androgen receptors
in colorectal cancer in relation to gender, menopausal status,
clinical stage, and tumour sidedness. Front Endocrinol (Lausanne).
14:11872592023. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Campbell-Thompson M, Lynch IJ and Bhardwaj
B: Expression of estrogen receptor (ER) subtypes and ERbeta
isoforms in colon cancer. Cancer Res. 61:632–640. 2001.PubMed/NCBI
|
|
39
|
Maingi JW, Tang S, Liu S, Ngenya W and Bao
E: Targeting estrogen receptors in colorectal cancer. Mol Biol Rep.
47:4087–4091. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Herichová I, Jendrisková S, Pidíková P,
Kršková L, Olexová L, Morová M, Stebelová K and Štefánik P: Effect
of 17β-estradiol on the daily pattern of ACE2, ADAM17, TMPRSS2 and
estradiol receptor transcription in the lungs and colon of male
rats. PLoS One. 17:e02706092022. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Weyant MJ, Carothers AM, Mahmoud NN,
Bradlow HL, Remotti H, Bilinski RT and Bertagnolli MM: Reciprocal
expression of ERalpha and ERbeta is associated with
estrogen-mediated modulation of intestinal tumorigenesis. Cancer
Res. 61:2547–2551. 2001.PubMed/NCBI
|
|
42
|
Giroux V, Lemay F, Bernatchez G,
Robitaille Y and Carrier JC: Estrogen receptor beta deficiency
enhances small intestinal tumorigenesis in ApcMin/+ mice. Int J
Cancer. 123:303–311. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Weige CC, Allred KF and Allred CD:
Estradiol alters cell growth in nonmalignant colonocytes and
reduces the formation of preneoplastic lesions in the colon. Cancer
Res. 69:9118–9124. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Song CH, Kim N, Lee SM, Nam RH, Choi SI,
Kang SR, Shin E, Lee DH, Lee HN and Surh YJ: Effects of
17β-estradiol on colorectal cancer development after
azoxymethane/dextran sulfate sodium treatment of ovariectomized
mice. Biochem Pharmacol. 164:139–151. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Son HJ, Sohn SH, Kim N, Lee HN, Lee SM,
Nam RH, Park JH, Song CH, Shin E, Na HY, et al: Effect of estradiol
in an Azoxymethane/Dextran sulfate Sodium-treated mouse model of
colorectal cancer: Implication for sex difference in colorectal
cancer development. Cancer Res Treat. 51:632–648. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hartman J, Edvardsson K, Lindberg K, Zhao
C, Williams C, Ström A and Gustafsson JA: Tumor repressive
functions of estrogen receptor beta in SW480 colon cancer cells.
Cancer Res. 69:6100–6106. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Uhlén M, Fagerberg L, Hallström BM,
Lindskog C, Oksvold P, Mardinoglu A, Sivertsson Å, Kampf C,
Sjöstedt E, Asplund A, et al: Proteomics. Tissue-based map of the
human proteome. Science. 347:12604192015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Abancens M, Harvey BJ and McBryan J: GPER
agonist G1 prevents Wnt-induced JUN upregulation in HT29 colorectal
cancer cells. Int J Mol Sci. 23:125812022. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Muller C, Chaney MF, Cohen JV, Garyantes
T, Lin JJ, LoRusso P, Mita AC, Mita MM, Natale C, Orloff MM, et al:
Phase 1b study of the novel first-in-class G protein-coupled
estrogen receptor (GPER) agonist, LNS8801, in combination with
pembrolizumab in patients with immune checkpoint inhibitor
(ICI)-relapsed and refractory solid malignancies and dose
escalation update. J Clinical Oncol. 40 (16_suppl):S2574. 2022.
View Article : Google Scholar
|
|
50
|
Hall KA and Filardo EJ: The G
Protein-coupled estrogen receptor (GPER): A critical therapeutic
target for cancer. Cells. 12:24602023. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Liu Q, Chen Z, Jiang G, Zhou Y, Yang X,
Huang H, Liu H, Du J and Wang H: Epigenetic down regulation of G
protein-coupled estrogen receptor (GPER) functions as a tumor
suppressor in colorectal cancer. Mol Cancer. 16:872017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Bühler M, Fahrländer J, Sauter A, Becker
M, Wistorf E, Steinfath M and Stolz A: GPER1 links estrogens to
centrosome amplification and chromosomal instability in human colon
cells. Life Sci Alliance. 6:e2022014992022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Bustos V, Nolan ÁM, Nijhuis A, Harvey H,
Parker A, Poulsom R, McBryan J, Thomas W, Silver A and Harvey BJ:
GPER mediates differential effects of estrogen on colon cancer cell
proliferation and migration under normoxic and hypoxic conditions.
Oncotarget. 8:84258–84275. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Santolla MF, Lappano R, De Marco P, Pupo
M, Vivacqua A, Sisci D, Abonante S, Iacopetta D, Cappello AR, Dolce
V, et al: G protein-coupled estrogen receptor mediates the
up-regulation of fatty acid synthase induced by 17β-estradiol in
cancer cells and cancer-associated fibroblasts. J Biol Chem.
287:43234–43245. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Xie M, Liang JL, Huang HD, Wang MJ, Zhang
T and Yang XF: Low doses of nonylphenol promote growth of colon
cancer cells through activation of ERK1/2 via G Protein-coupled
receptor 30. Cancer Res Treat. 51:1620–1631. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Gilligan LC, Rahman HP, Hewitt AM, Sitch
AJ, Gondal A, Arvaniti A, Taylor AE, Read ML, Morton DG and Foster
PA: Estrogen activation by steroid sulfatase increases colorectal
cancer proliferation via GPER. J Clin Endocrinol Metab.
102:4435–4447. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Rouhimoghadam M, Lu AS, Salem AK and
Filardo EJ: Therapeutic perspectives on the modulation of G-protein
coupled estrogen receptor, GPER, Function. Front Endocrinol
(Lausanne). 11:5912172020. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Rodon J, Chaney M, Cohen J, Garyantes TK,
Ishizuka J, Lin JJ, Lorusso P, Mita A, Mita M, Muller C, et al: The
effect of LNS8801 in combination with pembrolizumab in patients
with treatment-refractory cutaneous melanoma. J Immuno Ther Cancer.
11 (Suppl 1):A6272023.
|
|
59
|
Shoushtari AN, Chaney MF, Cohen JV,
Garyantes T, Lin JJ, Ishizuka JJ, Mita AC, Mita MM, Muller C,
Natale C, et al: The effect of LNS8801 alone and in combination
with pembrolizumab in patients with metastatic uveal melanoma. J
Clin Oncol. 41 (16_Suppl):S9543. 2023. View Article : Google Scholar
|
|
60
|
Holm A, Grände PO, Ludueña RF, Olde B,
Prasad V, Leeb-Lundberg LM and Nilsson BO: The G protein-coupled
oestrogen receptor 1 agonist G-1 disrupts endothelial cell
microtubule structure in a receptor-independent manner. Mol Cell
Biochem. 366:239–249. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Wang C, Lv X, Jiang C and Davis JS: The
putative G-protein coupled estrogen receptor agonist G-1 suppresses
proliferation of ovarian and breast cancer cells in a
GPER-independent manner. Am J Transl Res. 4:390–402.
2012.PubMed/NCBI
|
|
62
|
Gui Y, Shi Z, Wang Z, Li JJ, Xu C, Tian R,
Song X, Walsh MP, Li D, Gao J, et al: The GPER agonist G-1 induces
mitotic arrest and apoptosis in human vascular smooth muscle cells
independent of GPER. J Cell Physiol. 230:885–895. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Mori T, Ito F, Matsushima H, Takaoka O,
Tanaka Y, Koshiba A, Kusuki I and Kitawaki J: G protein-coupled
estrogen receptor 1 agonist G-1 induces cell cycle arrest in the
mitotic phase, leading to apoptosis in endometriosis. Fertil
Steril. 103:1228–1235.e1. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Lv X, He C, Huang C, Hua G, Wang Z,
Remmenga SW, Rodabough KJ, Karpf AR, Dong J, Davis JS, et al: G-1
Inhibits breast cancer cell growth via targeting Colchicine-binding
site of tubulin to interfere with microtubule assembly. Mol Cancer
Ther. 16:1080–1091. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Torres-López L, Olivas-Aguirre M,
Villatoro-Gómez K and Dobrovinskaya O: The G-protein-coupled
estrogen receptor agonist G-1 inhibits proliferation and causes
apoptosis in leukemia cell lines of T lineage. Front Cell Dev Biol.
10:8114792022. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Haupt S, Caramia F, Herschtal A, Soussi T,
Lozano G, Chen H, Liang H, Speed TP and Haupt Y: Identification of
cancer sex-disparity in the functional integrity of p53 and its X
chromosome network. Nat Commun. 10:53852019. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Liu Y and Bodmer WF: Analysis of P53
mutations and their expression in 56 colorectal cancer cell lines.
Proc Natl Acad Sci USA. 103:976–981. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Schneider CA, Rasband WS and Eliceiri KW:
NIH Image to ImageJ: 25 years of image analysis. Nat Methods.
9:671–675. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Recchia AG, De Francesco EM, Vivacqua A,
Sisci D, Panno ML, Andò S and Maggiolini M: The G protein-coupled
receptor 30 is up-regulated by hypoxia-inducible factor-1alpha
(HIF-1alpha) in breast cancer cells and cardiomyocytes. J Biol
Chem. 286:10773–10782. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Jacenik D, Beswick EJ, Krajewska WM and
Prossnitz ER: G protein-coupled estrogen receptor in colon
function, immune regulation and carcinogenesis. World J
Gastroenterol. 25:4092–4104. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Foley EF, Jazaeri AA, Shupnik MA, Jazaeri
O and Rice LW: Selective loss of estrogen receptor beta in
malignant human colon. Cancer Res. 60:245–248. 2000.PubMed/NCBI
|
|
72
|
Jassam N, Bell SM, Speirs V and Quirke P:
Loss of expression of oestrogen receptor beta in colon cancer and
its association with Dukes' staging. Oncol Rep. 14:17–21.
2005.PubMed/NCBI
|
|
73
|
Mostafaie N, Kállay E, Sauerzapf E, Bonner
E, Kriwanek S, Cross HS, Huber KR and Krugluger W: Correlated
downregulation of estrogen receptor beta and the circadian clock
gene Per1 in human colorectal cancer. Mol Carcinog. 48:642–647.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Herichova I, Reis R, Hasakova K, Vician M
and Zeman M: Sex-dependent regulation of estrogen receptor beta in
human colorectal cancer tissue and its relationship with clock
genes and VEGF-A expression. Physiol Res. 68 (Suppl 3):S297–S305.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Hasakova K, Vician M, Reis R, Zeman M and
Herichova I: Sex-dependent correlation between survival and
expression of genes related to the circadian oscillator in patients
with colorectal cancer. Chronobiol Int. 35:1423–1434. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Williams C, DiLeo A, Niv Y and Gustafsson
JÅ: Estrogen receptor beta as target for colorectal cancer
prevention. Cancer Lett. 372:48–56. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Ya G, Wang H, Ma Y, Hu A, Ma Y, Hu J and
Yu Y: Serum miR-129 functions as a biomarker for colorectal cancer
by targeting estrogen receptor (ER) β. Pharmazie. 72:107–112.
2017.PubMed/NCBI
|
|
78
|
Issa JP, Ottaviano YL, Celano P, Hamilton
SR, Davidson NE and Baylin SB: Methylation of the oestrogen
receptor CpG island links ageing and neoplasia in human colon. Nat
Genet. 7:536–540. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Jiang H, Teng R, Wang Q, Zhang X, Wang H,
Wang Z, Cao J and Teng L: Transcriptional analysis of estrogen
receptor alpha variant mRNAs in colorectal cancers and their
matched normal colorectal tissues. J Steroid Biochem Mol Biol.
112:20–24. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Topi G, Ghatak S, Satapathy SR, Ehrnström
R, Lydrup ML and Sjölander A: Combined estrogen alpha and beta
receptor expression has a prognostic significance for colorectal
cancer patients. Front Med (Lausanne). 9:7396202022. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Kennelly R, Kavanagh DO, Hogan AM and
Winter DC: Oestrogen and the colon: Potential mechanisms for cancer
prevention. Lancet Oncol. 94:385–391. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Barton M, Filardo EJ, Lolait SJ, Thomas P,
Maggiolini M and Prossnitz ER: Twenty years of the G
protein-coupled estrogen receptor GPER: Historical and personal
perspectives. J Steroid Biochem Mol Biol. 176:4–15. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Harvey BJ and Harvey HM: Sex differences
in colon cancer: Genomic and nongenomic signalling of oestrogen.
Genes (Basel). 14:22252023. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Nüssler NC, Reinbacher K, Shanny N,
Schirmeier A, Glanemann M, Neuhaus P, Nussler AK and Kirschner M:
Sex-specific differences in the expression levels of estrogen
receptor subtypes in colorectal cancer. Gend Med. 5:209–217. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Deli T, Orosz M and Jakab A: Hormone
replacement therapy in cancer survivors-review of the literature.
Pathol Oncol Res. 26:63–78. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Topi G, Satapathy SR, Dash P, Fred Mehrabi
S, Ehrnström R, Olsson R, Lydrup ML and Sjölander A:
Tumour-suppressive effect of oestrogen receptor β in colorectal
cancer patients, colon cancer cells, and a zebrafish model. J
Pathol. 251:297–309. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Tirado-Garibay AC, Falcón-Ruiz EA,
Ochoa-Zarzosa A and López-Meza JE: GPER: An estrogen receptor key
in metastasis and tumoral microenvironments. Int J Mol Sc.
24:149932023. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ambrosini G, Natale CA, Musi E, Garyantes
T and Schwartz GK: The GPER agonist LNS8801 induces mitotic arrest
and apoptosis in uveal melanoma cells. Cancer Res Commun.
3:540–547. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Filardo EJ, Quinn JA, Bland KI and
Frackelton AR Jr: Estrogen-induced activation of Erk-1 and Erk-2
requires the G protein-coupled receptor homolog, GPR30, and occurs
via trans-activation of the epidermal growth factor receptor
through release of HB-EGF. Mol Endocrinol. 14:1649–1660. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Hsu LH, Chu NM, Lin YF and Kao SH:
G-Protein coupled estrogen receptor in breast cancer. Int J Mol
Sci. 20:3062019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Rubin Grandis J, Melhem MF, Gooding WE,
Day R, Holst VA, Wagener MM, Drenning SD and Tweardy DJ: Levels of
TGF-alpha and EGFR protein in head and neck squamous cell carcinoma
and patient survival. J Natl Cancer Inst. 90:824–832. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Uribe ML, Marrocco I and Yarden Y: EGFR in
cancer: Signaling mechanisms, drugs, and acquired resistance.
Cancers (Basel). 13:27482021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Janani B, Vijayakumar M, Priya K, Kim JH,
Prabakaran DS, Shahid M, Al-Ghamdi S, Alsaidan M, Othman Bahakim N,
Hassan Abdelzaher M and Ramesh T: EGFR-based targeted therapy for
colorectal cancer-promises and challenges. Vaccines (Basel).
10:4992022. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Giannopoulou E, Antonacopoulou A, Floratou
K, Papavassiliou AG and Kalofonos HP: Dual targeting of EGFR and
HER-2 in colon cancer cell lines. Cancer Chemother Pharmacol.
63:973–981. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Yuan HH, Han Y, Bian WX, Liu L and Bai YX:
The effect of monoclonal antibody cetuximab (C225) in combination
with tyrosine kinase inhibitor gefitinib (ZD1839) on colon cancer
cell lines. Pathology. 44:547–551. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Palumbo I, Piattoni S, Valentini V, Marini
V, Contavalli P, Calzuola M, Vecchio FM, Cecchini D, Falzetti F and
Aristei C: Gefitinib enhances the effects of combined radiotherapy
and 5-fluorouracil in a colorectal cancer cell line. Int J
Colorectal Dis. 29:31–41. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Chen X, Liu Y, Yang HW, Zhou S, Cheng C,
Zheng MW, Zhong L, Fu XY, Pan YL, Ma S, et al: SKLB-287, a novel
oral multikinase inhibitor of EGFR and VEGFR2, exhibits potent
antitumor activity in LoVo colorectal tumor model. Neoplasma.
61:514–22. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Chuang SC, Chen CH, Chou YS, Ho ML and
Chang JK: G Protein-coupled estrogen receptor mediates cell
proliferation through the cAMP/PKA/CREB pathway in murine bone
marrow mesenchymal stem cells. Int J Mol Sci. 21:64902020.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Berg KCG, Eide PW, Eilertsen IA,
Johannessen B, Bruun J, Danielsen SA, Bjørnslett M, Meza-Zepeda LA,
Eknæs M, Lind GE, et al: Multi-omics of 34 colorectal cancer cell
lines-a resource for biomedical studies. Mol Cancer. 16:1162017.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Moulder DE, Hatoum D, Tay E, Lin Y and
McGowan EM: The roles of p53 in mitochondrial dynamics and cancer
metabolism: The pendulum between survival and death in breast
cancer? Cancers (Basel). 10:1892018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Engeland K: Cell cycle regulation:
P53-p21-RB signaling. Cell Death Differ. 29:946–960. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Weißenborn C, Ignatov T, Ochel HJ, Costa
SD, Zenclussen AC, Ignatova Z and Ignatov A: GPER functions as a
tumor suppressor in triple-negative breast cancer cells. J Cancer
Res Clin Oncol. 140:713–23. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Rochette PJ, Bastien N, Lavoie J, Guérin
SL and Drouin R: SW480, a p53 double-mutant cell line retains
proficiency for some p53 functions. J Mol Biol. 352:44–57. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Berglind H, Pawitan Y, Kato S, Ishioka C
and Soussi T: Analysis of p53 mutation status in human cancer cell
lines: A paradigm for cell line cross-contamination. Cancer Biol
Ther. 7:699–708. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Hassin O, Nataraj NB, Shreberk-Shaked M,
Aylon Y, Yaeger R, Fontemaggi G, Mukherjee S, Maddalena M, Avioz A,
Iancu O, et al: Different hotspot p53 mutants exert distinct
phenotypes and predict outcome of colorectal cancer patients. Nat
Commun. 13:28002022. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Leroy B, Girard L, Hollestelle A, Minna
JD, Gazdar AF and Soussi T: Analysis of TP53 mutation status in
human cancer cell lines: A reassessment. Hum Mutat. 35:756–765.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Berger C, Qian Y and Chen X: The
p53-estrogen receptor loop in cancer. Curr Mol Med. 13:1229–1240.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Chen YC, Young MJ, Chang HP, Liu CY, Lee
CC, Tseng YL, Wang YC, Chang WC and Hung JJ: Estradiol-mediated
inhibition of DNMT1 decreases p53 expression to induce
M2-macrophage polarization in lung cancer progression. Oncogenesis.
11:252022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Weige CC, Allred KF, Armstrong CM and
Allred CD: P53 mediates estradiol induced activation of apoptosis
and DNA repair in non-malignant colonocytes. J Steroid Biochem Mol
Biol. 128:113–120. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Qin C, Nguyen T, Stewart J, Samudio I,
Burghardt R and Safe S: Estrogen up-regulation of p53 gene
expression in MCF-7 breast cancer cells is mediated by calmodulin
kinase IV-dependent activation of a nuclear factor
kappaB/CCAAT-binding transcription factor-1 complex. Mol
Endocrinol. 16:1793–809. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Berger CE, Qian Y, Liu G, Chen H and Chen
X: p53, a target of estrogen receptor (ER) α, modulates DNA
damage-induced growth suppression in ER-positive breast cancer
cells. J Biol Chem. 287:30117–30127. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Swetzig WM, Wang J and Das GM: Estrogen
receptor alpha (ERα/ESR1) mediates the p53-independent
overexpression of MDM4/MDMX and MDM2 in human breast cancer.
Oncotarget. 7:16049–16069. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Mancini F, Giorgini L, Teveroni E,
Pontecorvi A and Moretti F: Role of sex in the therapeutic
targeting of p53 circuitry. Front Oncol. 11:6989462021. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Konduri SD, Medisetty R, Liu W,
Kaipparettu BA, Srivastava P, Brauch H, Fritz P, Swetzig WM,
Gardner AE, Khan SA, et al: Mechanisms of estrogen receptor
antagonism toward p53 and its implications in breast cancer
therapeutic response and stem cell regulation. Proc Natl Acad Sci
USA. 107:15081–6. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Lu W and Katzenellenbogen BS: Estrogen
receptor-β modulation of the ERα-p53 loop regulating gene
expression, proliferation, and apoptosis in breast cancer. Horm
Cancer. 8:230–242. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Cerami E, Gao J, Dogrusoz U, Gross BE,
Sumer SO, Aksoy BA, Jacobsen A, Byrne CJ, Heuer ML, Larsson E, et
al: The cBio cancer genomics portal: An open platform for exploring
multidimensional cancer genomics data. Cancer Discov. 2:401–404.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Bilancio A, Bontempo P, Di Donato M, Conte
M, Giovannelli P, Altucci L, Migliaccio A and Castoria G: Bisphenol
A induces cell cycle arrest in primary and prostate cancer cells
through EGFR/ERK/p53 signaling pathway activation. Oncotarget.
8:115620–115631. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Wei W, Chen ZJ, Zhang KS, Yang XL, Wu YM,
Chen XH, Huang HB, Liu HL, Cai SH, Du J, et al: The activation of G
protein-coupled receptor 30 (GPR30) inhibits proliferation of
estrogen receptor-negative breast cancer cells in vitro and in
vivo. Cell Death Dis. 5:e14282014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Morelli E, Hunter ZR, Fulciniti M, Gullà
A, Perrotta ID, Zuccalà V, Federico C, Juli G, Manzoni M, Ronchetti
D, et al: Therapeutic activation of G protein-coupled estrogen
receptor 1 in Waldenström Macroglobulinemia. Exp Hematol Onco.
11:542022. View Article : Google Scholar
|
|
120
|
Giebler HA, Lemasson I and Nyborg JK: p53
recruitment of CREB binding protein mediated through phosphorylated
CREB: A novel pathway of tumor suppressor regulation. Mol Cell
Biol. 20:4849–4858. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Okoshi R, Ando K, Suenaga Y, Sang M, Kubo
N, Kizaki H, Nakagawara A and Ozaki T: Transcriptional regulation
of tumor suppressor p53 by cAMP-responsive element-binding
protein/AMP-activated protein kinase complex in response to glucose
deprivation. Genes Cells. 14:1429–1440. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Lee CW, Ferreon JC, Ferreon AC, Arai M and
Wright PE: Graded enhancement of p53 binding to CREB-binding
protein (CBP) by multisite phosphorylation. Proc Natl Acad Sci USA.
107:19290–19295. 2010. View Article : Google Scholar : PubMed/NCBI
|