|
1
|
Döhner H, Weisdorf DJ and Bloomfield CD:
Acute myeloid leukemia. N Engl J Med. 373:1136–1152. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liu H: Emerging agents and regimens for
AML. J Hematol Oncol. 14:492021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Peng C, Xu Y, Wu J, Wu D, Zhou L and Xia
X: TME-related biomimetic strategies against cancer. Int J
Nanomedicine. 19:109–135. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bawek S, Gurusinghe S, Burwinkel M and
Przespolewski A: Updates in novel immunotherapeutic strategies for
relapsed/refractory AML. Front Oncol. 14:13749632024. View Article : Google Scholar : PubMed/NCBI
|
|
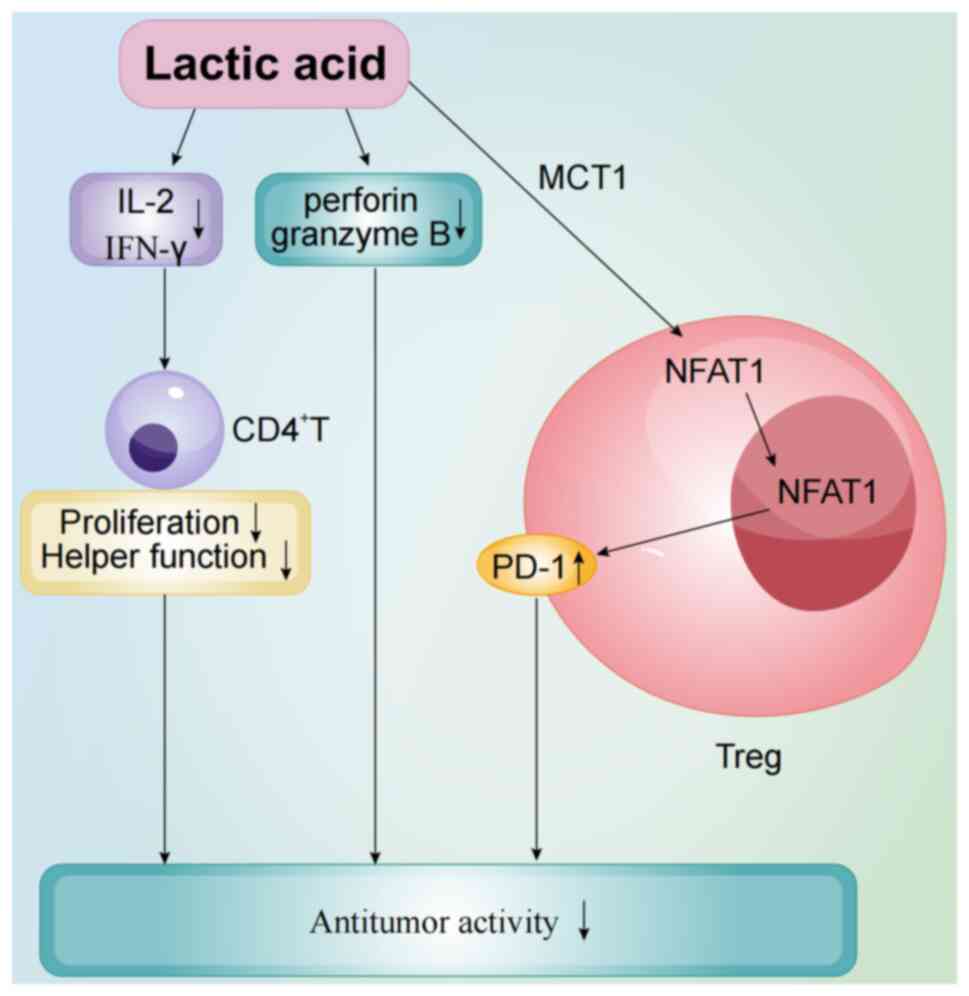
5
|
Menter T and Tzankov A: Tumor
microenvironment in acute myeloid leukemia: Adjusting niches. Front
Immunol. 13:8111442022. View Article : Google Scholar : PubMed/NCBI
|
|
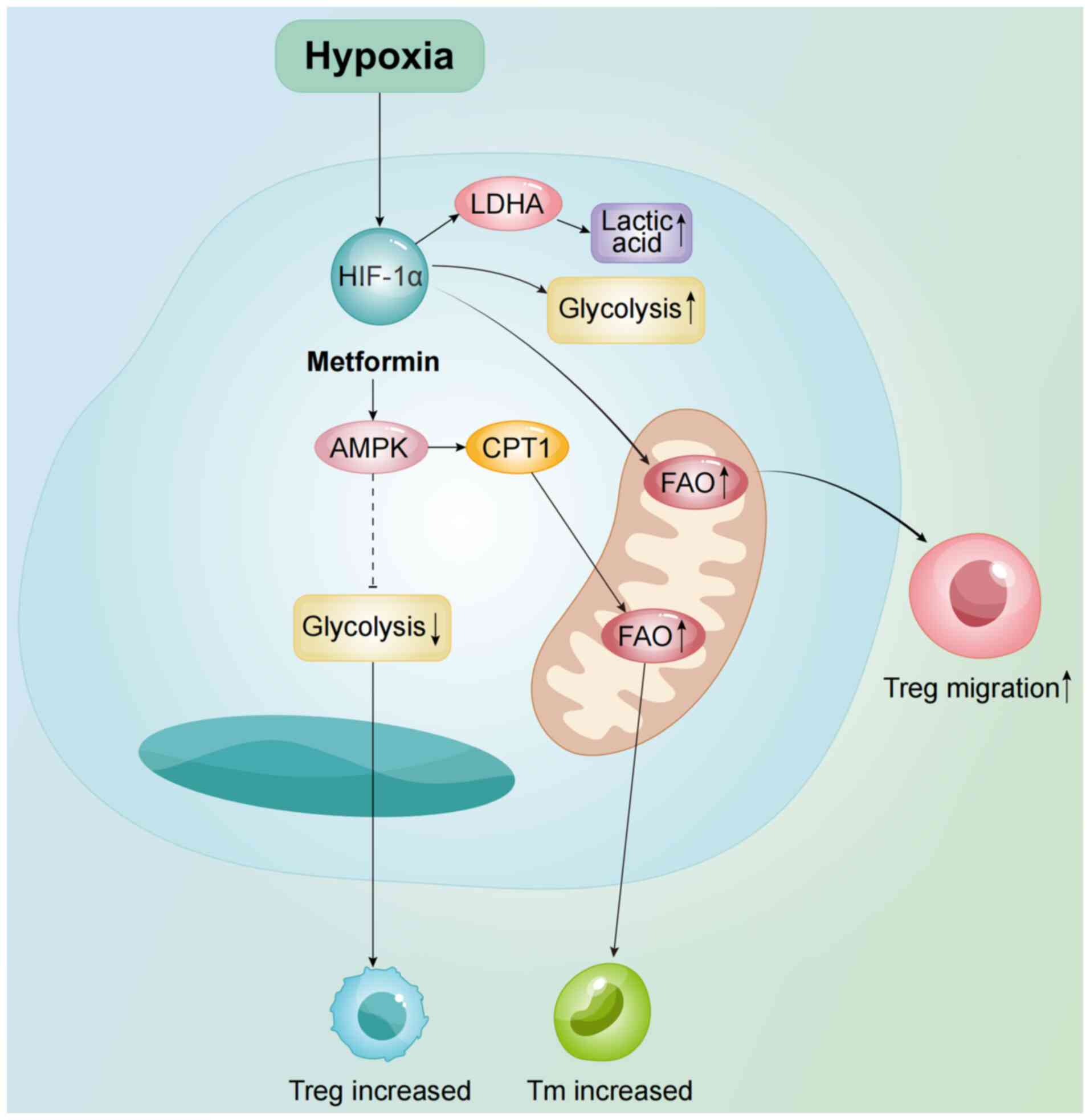
6
|
Lamble AJ and Lind EF: Targeting the
immune microenvironment in acute myeloid leukemia: A focus on T
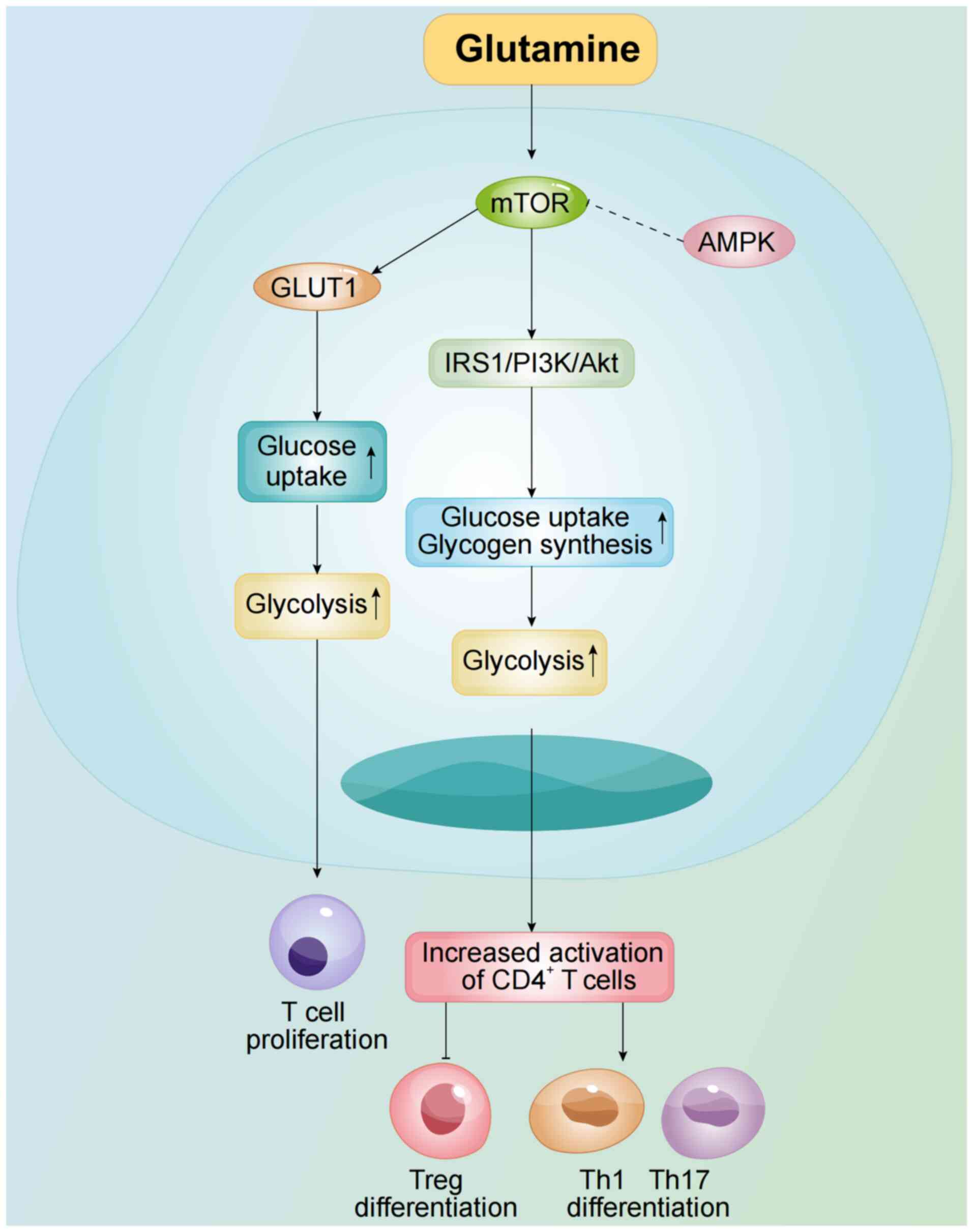
cell immunity. Front Oncol. 8:2132018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Korn C and Méndez-Ferrer S: Myeloid
malignancies and the microenvironment. Blood. 129:811–822. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rieger CT and Fiegl M: Microenvironmental
oxygen partial pressure in acute myeloid leukemia: Is there really
a role for hypoxia? Exp Hematol. 44:578–582. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yu S and Jiang J: Immune
infiltration-related genes regulate the progression of AML by
invading the bone marrow microenvironment. Front Immunol.
15:14099452024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zeng T, Cui L, Huang W, Liu Y, Si C, Qian
T, Deng C and Fu L: The establishment of a prognostic scoring model
based on the new tumor immune microenvironment classification in
acute myeloid leukemia. BMC Med. 19:1762021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chraa D, Naim A, Olive D and Badou A: T
lymphocyte subsets in cancer immunity: Friends or foes. J Leukoc
Biol. 105:243–255. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Plitas G and Rudensky AY: Regulatory T
cells: Differentiation and function. Cancer Immunol Res. 4:721–725.
2016. View Article : Google Scholar : PubMed/NCBI
|
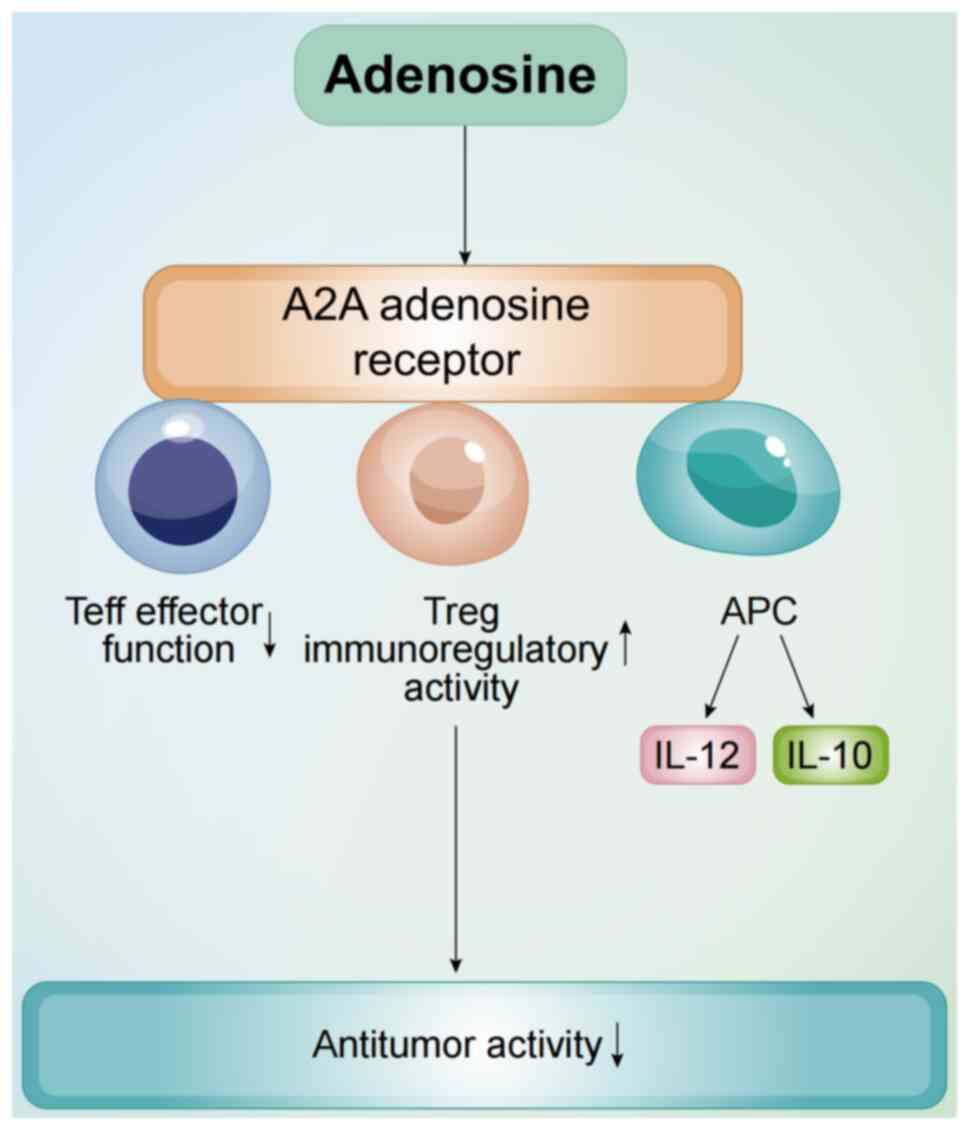
|
13
|
MacIver NJ, Michalek RD and Rathmell JC:
Metabolic regulation of T lymphocytes. Annu Rev Immunol.
31:259–283. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lochner M, Berod L and Sparwasser T: Fatty
acid metabolism in the regulation of T cell function. Trends
Immunol. 36:81–91. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Endo Y, Kanno T and Nakajima T: Fatty acid
metabolism in T-cell function and differentiation. Int Immunol.
34:579–587. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Geiger R, Rieckmann JC, Wolf T, Basso C,
Feng Y, Fuhrer T, Kogadeeva M, Picotti P, Meissner F, Mann M, et
al: L-arginine modulates T cell metabolism and enhances survival
and anti-tumor activity. Cell. 167:829–842.e13. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang J, He Y, Hu F, Hu C, Sun Y, Yang K
and Yang S: Metabolic reprogramming of immune cells in the tumor
microenvironment. Int J Mol Sci. 25:122232024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Halestrap AP: The monocarboxylate
transporter family-structure and functional characterization. IUBMB
Life. 64:1–9. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Uhl FM, Chen S, O'Sullivan D,
Edwards-Hicks J, Richter G, Haring E, Andrieux G, Halbach S,
Apostolova P, Büscher J, et al: Metabolic reprogramming of donor T
cells enhances graft-versus-leukemia effects in mice and humans.
Sci Transl Med. 12:eabb89692020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ju HQ, Zhan G, Huang A, Sun Y, Wen S, Yang
J, Lu WH, Xu RH, Li J, Li Y, et al: ITD mutation in FLT3 tyrosine
kinase promotes Warburg effect and renders therapeutic sensitivity
to glycolytic inhibition. Leukemia. 31:2143–2150. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Herst PM, Howman RA, Neeson PJ, Berridge
MV and Ritchie DS: The level of glycolytic metabolism in acute
myeloid leukemia blasts at diagnosis is prognostic for clinical
outcome. J Leukoc Biol. 89:51–55. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Herst PM, Hesketh EL, Ritchie DS and
Berridge MV: Glycolytic metabolism confers resistance to combined
all-trans retinoic acid and arsenic trioxide-induced apoptosis in
HL60rho0 cells. Leuk Res. 32:327–333. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jones RG and Thompson CB: Tumor
suppressors and cell metabolism: A recipe for cancer growth. Genes
Dev. 23:537–548. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Röhrig F and Schulze A: The multifaceted
roles of fatty acid synthesis in cancer. Nat Rev Cancer.
16:732–749. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Heintzman DR, Fisher EL and Rathmell JC:
Microenvironmental influences on T cell immunity in cancer and
inflammation. Cell Mol Immunol. 19:316–326. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zha C, Yang X, Yang J, Zhang Y and Huang
R: Immunosuppressive microenvironment in acute myeloid leukemia:
Overview, therapeutic targets and corresponding strategies. Ann
Hematol. 103:4883–4899. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Böttcher M, Baur R, Stoll A, Mackensen A
and Mougiakakos D: Linking immunoevasion and metabolic
reprogramming in B-cell-derived lymphomas. Front Oncol.
10:5947822020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fischer K, Hoffmann P, Voelkl S,
Meidenbauer N, Ammer J, Edinger M, Gottfried E, Schwarz S, Rothe G,
Hoves S, et al: Inhibitory effect of tumor cell-derived lactic acid
on human T cells. Blood. 109:3812–3819. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen Y, Feng Z, Kuang X, Zhao P, Chen B,
Fang Q, Cheng W and Wang J: Increased lactate in AML blasts
upregulates TOX expression, leading to exhaustion of CD8+ cytolytic
T cells. Am J Cancer Res. 11:5726–6742. 2021.PubMed/NCBI
|
|
30
|
Voskoboinik I, Whisstock JC and Trapani
JA: Perforin and granzymes: Function, dysfunction and human
pathology. Nat Rev Immunol. 15:388–400. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sradhanjali S and Reddy MM: Inhibition of
pyruvate dehydrogenase kinase as a therapeutic strategy against
cancer. Curr Top Med Chem. 18:444–453. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rostamian H, Khakpoor-Koosheh M,
Jafarzadeh L, Masoumi E, Fallah-Mehrjardi K, Tavassolifar MJ, M
Pawelek J, Mirzaei HR and Hadjati J: Restricting tumor lactic acid
metabolism using dichloroacetate improves T cell functions. BMC
Cancer. 22:392022. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kumagai S, Koyama S, Itahashi K,
Tanegashima T, Lin YT, Togashi Y, Kamada T, Irie T, Okumura G, Kono
H, et al: Lactic acid promotes PD-1 expression in regulatory T
cells in highly glycolytic tumor microenvironments. Cancer Cell.
40:201–218.e9. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yang P, Sun Y, Zhang M, Hu L, Wang X, Luo
L, Qiao C, Wang J, Xiao H, Li X, et al: The inhibition of
CD4+ T cell proinflammatory response by lactic acid is
independent of monocarboxylate transporter 1. Scand J Immunol.
94:e131032021. View Article : Google Scholar
|
|
35
|
Jiang F, Mao Y, Lu B, Zhou G and Wang J: A
hypoxia risk signature for the tumor immune microenvironment
evaluation and prognosis prediction in acute myeloid leukemia. Sci
Rep. 11:146572021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liu X, Wang L, Kang Q, Feng C and Wang J:
A hypoxia-related genes prognostic risk model, and mechanisms of
hypoxia contributing to poor prognosis through immune
microenvironment and drug resistance in acute myeloid leukemia.
Front Pharmacol. 15:13394652024. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Augustin RC, Delgoffe GM and Najjar YG:
Characteristics of the tumor microenvironment that influence immune
cell functions: Hypoxia, oxidative stress, metabolic alterations.
Cancers (Basel). 12:38022020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Jacque N, Ronchetti AM, Larrue C, Meunier
G, Birsen R, Willems L, Saland E, Decroocq J, Maciel TT, Lambert M,
et al: Targeting glutaminolysis has antileukemic activity in acute
myeloid leukemia and synergizes with BCL-2 inhibition. Blood.
126:1346–1356. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Carr EL, Kelman A, Wu GS, Gopaul R,
Senkevitch E, Aghvanyan A, Turay AM and Frauwirth KA: Glutamine
uptake and metabolism are coordinately regulated by ERK/MAPK during
T lymphocyte activation. J Immunol. 185:1037–1044. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Klysz D, Tai XG, Robert PA, Craveiro M,
Cretenet G, Oburoglu L, Mongellaz C, Floess S, Fritz V, Matias MI,
et al: Glutamine-dependent α-ketoglutarate production regulates the
balance between T helper 1 cell and regulatory T cell generation.
Sci Signal. 8:ra972015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Sun LY, Li XJ, Sun YM, Huang W, Fang K,
Han C, Chen ZH, Luo XQ, Chen YQ and Wang WT: LncRNA ANRIL regulates
AML development through modulating the glucose metabolism pathway
of AdipoR1/AMPK/SIRT1. Mol Cancer. 17:1272018. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Balihodzic A, Barth DA, Prinz F and
Pichler M: Involvement of long non-coding RNAs in glucose
metabolism in cancer. Cancers (Basel). 13:9772021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Pavlova NN, Zhu J and Thompson CB: The
hallmarks of cancer metabolism: Still emerging. Cell Metab.
34:355–377. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Cunningham I and Kohno B: 18 FDG-PET/CT:
21st century approach to leukemic tumors in 124 cases. Am J
Hematol. 91:379–384. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wang R, Feng W, Wang H, Wang L, Yang X,
Yang F, Zhang Y, Liu X, Zhang D, Ren Q, et al: Blocking migration
of regulatory T cells to leukemic hematopoietic microenvironment
delays disease progression in mouse leukemia model. Cancer Lett.
469:151–161. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bakker E, Qattan M, Mutti L, Demonacos C
and Krstic-Demonacos M: The role of microenvironment and immunity
in drug response in leukemia. Biochim Biophys Acta. 1863:414–426.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhang M, Yang Y, Liu J, Guo L, Guo Q and
Liu W: Bone marrow immune cells and drug resistance in acute
myeloid leukemia. Exp Biol Med (Maywood). 250:102352025. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ciciarello M, Corradi G, Forte D, Cavo M
and Curti A: Emerging bone marrow microenvironment-driven
mechanisms of drug resistance in acute myeloid leukemia: Tangle or
chance? Cancers (Basel). 13:53192021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Feske S, Colucci F and Coetzee WA: Do
KATP channels have a role in immunity? Front Immunol.
15:14849712024. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Feske S, Wulff H and Skolnik EY: Ion
channels in innate and adaptive immunity. Annu Rev Immunol.
33:291–353. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Eil R, Vodnala SK, Clever D, Klebanoff CA,
Sukumar M, Pan JH, Palmer DC, Gros A, Yamamoto TN, Patel SJ, et al:
Ionic immune suppression within the tumour microenvironment limits
T cell effector function. Nature. 537:539–543. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Vodnala SK, Eil R, Kishton RJ, Sukumar M,
Yamamoto TN, Ha NH, Lee PH, Shin M, Patel SJ, Yu Z, et al: T cell
stemness and dysfunction in tumors are triggered by a common
mechanism. Science. 363:eaau01352019. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Almeida L, Lochner M, Berod L and
Sparwasser T: Metabolic pathways in T cell activation and lineage
differentiation. Semin Immunol. 28:514–524. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Fukushi A, Kim HD, Chang YC and Kim CH:
Revisited metabolic control and reprogramming cancers by means of
the warburg effect in tumor cells. Int J Mol Sci. 23:100372022.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Riether C: Regulation of hematopoietic and
leukemia stem cells by regulatory T cells. Front Immunol.
13:10493012022. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Epperly R, Gottschalk S and Velasquez MP:
A bump in the road: how the hostile AML microenvironment affects
CAR T cell therapy. Front Oncol. 10:2622020. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Han Y, Dong Y, Yang Q, Xu W, Jiang S, Yu
Z, Yu K and Zhang S: Acute myeloid leukemia cells express ICOS
ligand to promote the expansion of regulatory T cells. Front
Immunol. 9:22272018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhou Q, Bucher C, Munger ME, Highfill SL,
Tolar J, Munn DH, Levine BL, Riddle M, June CH, Vallera DA, et al:
Depletion of endogenous tumor-associated regulatory T cells
improves the efficacy of adoptive cytotoxic T-cell immunotherapy in
murine acute myeloid leukemia. Blood. 114:3793–3802. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Liu SY, Liao S, Liang L, Deng J and Zhou
Y: The relationship between CD4+ T cell glycolysis and
their functions. Trends Endocrinol Metab. 34:345–360. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Cao J, Liao S, Zeng F, Liao Q, Luo G and
Zhou Y: Effects of altered glycolysis levels on CD8+ T
cell activation and function. Cell Death Dis. 14:4072023.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Yao CC, Sun RM, Yang Y, Zhou HY, Meng ZW,
Chi R, Xia LL, Ji P, Chen YY, Zhang GQ, et al: Accumulation of
branched-chain amino acids reprograms glucose metabolism in
CD8+ T cells with enhanced effector function and
anti-tumor response. Cell Rep. 42:1121862023. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Rabbani N and Thornalley PJ:
Methylglyoxal, glyoxalase 1 and the dicarbonyl proteome. Amino
Acids. 42:1133–1142. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Palanissami G and Paul SFD: AGEs and RAGE:
Metabolic and molecular signatures of the glycation-inflammation
axis in malignant or metastatic cancers. Explor Target Antitumor
Ther. 4:812–849. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Waghela BN, Vaidya FU, Ranjan K, Chhipa
AS, Tiwari BS and Pathak C: AGE-RAGE synergy influences programmed
cell death signaling to promote cancer. Mol Cell Biochem.
476:585–598. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bakhtiyari M, Liaghat M, Aziziyan F,
Shapourian H, Yahyazadeh S, Alipour M, Shahveh S,
Maleki-Sheikhabadi F, Halimi H, Forghaniesfidvajani R, et al: The
role of bone marrow microenvironment (BMM) cells in acute myeloid
leukemia (AML) progression: Immune checkpoints, metabolic
checkpoints, and signaling pathways. Cell Commun Signal.
21:2522023. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wang R, Liu Z, Fan Z and Zhan H: Lipid
metabolism reprogramming of CD8+ T cell and therapeutic
implications in cancer. Cancer Lett. 567:2162672023. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Jameson SC and Masopust D: Understanding
subset diversity in T cell memory. Immunity. 48:214–226. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kaech SM and Cui W: Transcriptional
control of effector and memory CD8+ T cell differentiation. Nat Rev
Immunol. 12:749–761. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
D'Cruz LM, Rubinstein MP and Goldrath AW:
Surviving the crash: Transitioning from effector to memory CD8+ T
cell. Semin Immunol. 21:92–98. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Mougiakakos D: The induction of a
permissive environment to promote T cell immune evasion in acute
myeloid leukemia: The metabolic perspective. Front Oncol.
9:11662019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Noviello M, Manfredi F, Ruggiero E, Perini
T, Oliveira G, Cortesi F, De Simone P, Toffalori C, Gambacorta V,
Greco R, et al: Bone marrow central memory and memory stem T-cell
exhaustion in AML patients relapsing after HSCT. Nat Commun.
10:10652019. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Abbas HA, Hao D, Tomczak K, Barrodia P, Im
JS, Reville PK, Alaniz Z, Wang W, Wang R, Wang F, et al: Single
cell T cell landscape and T cell receptor repertoire profiling of
AML in context of PD-1 blockade therapy. Nat Commun. 12:60712021.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Pearce EL, Walsh MC, Cejas PJ, Harms GM,
Shen H, Wang LS, Jones RG and Choi Y: Enhancing CD8 T-cell memory
by modulating fatty acid metabolism. Nature. 460:103–107. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Raud B, McGuire PJ, Jones RG, Sparwasser T
and Berod L: Fatty acid metabolism in CD8+ T cell
memory: Challenging current concepts. Immunol Rev. 283:213–231.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
van der Windt GJW, Everts B, Chang CH,
Curtis JD, Freitas TC, Amiel E, Pearce EJ and Pearce EL:
Mitochondrial respiratory capacity is a critical regulator of CD8+
T cell memory development. Immunity. 36:68–78. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Araki K, Turner AP, Shaffer VO, Gangappa
S, Keller SA, Bachmann MF, Larsen CP and Ahmed R: mTOR regulates
memory CD8 T-cell differentiation. Nature. 460:108–112. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Li P, Yin YL, Li D, Woo Kim S and Wu G:
Amino acids and immune function. Br J Nutr. 98:237–252. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Wang Y, Bai C, Ruan Y, Liu M, Chu Q, Qiu
L, Yang C and Li B: Coordinative metabolism of glutamine carbon and
nitrogen in proliferating cancer cells under hypoxia. Nat Commun.
10:2012019. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Leone RD, Zhao L, Englert JM, Sun IM, Oh
MH, Sun IH, Arwood ML, Bettencourt IA, Patel CH, Wen J, et al:
Glutamine blockade induces divergent metabolic programs to overcome
tumor immune evasion. Science. 366:1013–1021. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Munn DH, Shafizadeh E, Attwood JT,
Bondarev I, Pashine A and Mellor AL: Inhibition of T cell
proliferation by macrophage tryptophan catabolism. J Exp Med.
189:1363–1372. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Murray PJ: Amino acid auxotrophy as a
system of immunological control nodes. Nat Immunol. 17:132–139.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Di Marcantonio D, Martinez E, Kanefsky JS,
Huhn JM, Gabbasov R, Gupta A, Krais JJ, Peri S, Tan Y, Skorski T,
et al: ATF3 coordinates serine and nucleotide metabolism to drive
cell cycle progression in acute myeloid leukemia. Mol Cell.
81:2752–2764.e6. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Yabushita T and Goyama S: Nucleic acid
metabolism: The key therapeutic target for myeloid tumors. Exp
Hematol. 142:1046932025. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Capelletti MM, Montini O, Ruini E,
Tettamanti S, Savino AM and Sarno J: Unlocking the heterogeneity in
acute leukaemia: Dissection of clonal architecture and metabolic
properties for clinical interventions. Int J Mol Sci. 26:452024.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Wu HL, Gong Y, Ji P, Xie YF, Jiang YZ and
Liu GY: Targeting nucleotide metabolism: A promising approach to
enhance cancer immunotherapy. J Hematol Oncol. 15:452022.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Wang H, Wei Y and Wang N: Purinergic
pathways and their clinical use in the treatment of acute myeloid
leukemia. Purinergic Signal. Mar 6–2024.(Epub ahead of print).
View Article : Google Scholar
|
|
87
|
Ohta A: A metabolic immune checkpoint:
Adenosine in tumor microenvironment. Front Immunol. 7:1092016.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Evans DR and Guy HI: Mammalian pyrimidine
biosynthesis: Fresh insights into an ancient pathway. J Biol Chem.
279:33035–33038. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Santi A, Caselli A, Paoli P, Corti D,
Camici G, Pieraccini G, Taddei ML, Serni S, Chiarugi P and Cirri P:
The effects of CA IX catalysis products within tumor
microenvironment. Cell Commun Signal. 11:812013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Pollizzi KN, Patel CH, Sun IH, Oh MH,
Waickman AT, Wen J, Delgoffe GM and Powell JD: mTORC1 and mTORC2
selectively regulate CD8+ T cell differentiation. J Clin
Invest. 125:2090–2108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Dabi YT, Andualem H, Degechisa ST and
Gizaw ST: Targeting metabolic reprogramming of T-cells for enhanced
anti-tumor response. Biologics. 16:35–45. 2022.PubMed/NCBI
|
|
92
|
Saravia J, Raynor JL, Chapman NM, Lim SA
and Chi H: Signaling networks in immunometabolism. Cell Res.
30:328–342. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Yan Y, Huang L, Liu Y, Yi M, Chu Q, Jiao D
and Wu K: Metabolic profiles of regulatory T cells and their
adaptations to the tumor microenvironment: Implications for
antitumor immunity. J Hematol Oncol. 15:1042022. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Castro I, Sampaio-Marques B and Ludovico
P: Targeting metabolic reprogramming in acute myeloid leukemia.
Cells. 8:9672019. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Ahmadian M, Suh JM, Hah N, Liddle C,
Atkins AR, Downes M and Evans RM: PPARγ signaling and metabolism:
The good, the bad and the future. Nat Med. 19:557–566. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Angela M, Endo Y, Asou HK, Yamamoto T,
Tumes DJ, Tokuyama H, Yokote K and Nakayama T: Fatty acid metabolic
reprogramming via mTOR-mediated inductions of PPARγ directs early
activation of T cells. Nat Commun. 7:136832016. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Tabe Y, Konopleva M and Andreeff M: Fatty
acid metabolism, bone marrow adipocytes, and AML. Front Oncol.
10:1552020. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Chowdhury PS, Chamoto K, Kumar A and Honjo
T: PPAR-induced fatty acid oxidation in T cells increases the
number of tumor-reactive CD8+ T cells and facilitates
anti-PD-1 therapy. Cancer Immunol Res. 6:1375–1387. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhang JZ, Behrooz A and Ismail-Beigi F:
Regulation of glucose transport by hypoxia. Am J Kidney Dis.
34:189–202. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Miska J, Lee-Chang C, Rashidi A, Muroski
ME, Chang AL, Lopez-Rosas A, Zhang P, Panek WK, Cordero A, Han Y,
et al: HIF-1α is a metabolic switch between glycolytic-driven
migration and oxidative phosphorylation-driven immunosuppression of
tregs in glioblastoma. Cell Rep. 27:226–237.e4. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Nagao A, Kobayashi M, Koyasu S, Chow CCT
and Harada H: HIF-1-dependent reprogramming of glucose metabolic
pathway of cancer cells and its therapeutic significance. Int J Mol
Sci. 20:2382019. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Wu H, Zhao X, Hochrein SM, Eckstein M,
Gubert GF, Knöpper K, Mansilla AM, Öner A, Doucet-Ladevèze R,
Schmitz W, et al: Mitochondrial dysfunction promotes the transition
of precursor to terminally exhausted T cells through
HIF-1α-mediated glycolytic reprogramming. Nat Commun. 14:68582023.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Pan F, Barbi J and Pardoll DM:
Hypoxia-inducible factor 1: A link between metabolism and T cell
differentiation and a potential therapeutic target. Oncoimmunology.
1:510–515. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Alatrash G, Daver N and Mittendorf EA:
Targeting immune checkpoints in hematologic malignancies. Pharmacol
Rev. 68:1014–1025. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Stahl M and Goldberg AD: Immune checkpoint
inhibitors in acute myeloid leukemia: Novel combinations and
therapeutic targets. Curr Oncol Rep. 21:372019. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Zhou Q, Munger ME, Highfill SL, Tolar J,
Weigel BJ, Riddle M, Sharpe AH, Vallera DA, Azuma M, Levine BL, et
al: Program death-1 signaling and regulatory T cells collaborate to
resist the function of adoptively transferred cytotoxic T
lymphocytes in advanced acute myeloid leukemia. Blood.
116:2484–2493. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Sadelain M, Brentjens R and Rivière I: The
basic principles of chimeric antigen receptor design. Cancer
Discov. 3:388–398. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Riddell SR, Jensen MC and June CH:
Chimeric antigen receptor-modified T cells: Clinical translation in
stem cell transplantation and beyond. Biol Blood Marrow Transplant.
19 (1 Suppl):S2–S5. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Suryadevara CM, Desai R, Farber SH, Choi
BD, Swartz AM, Shen SH, Gedeon PC, Snyder DJ, Herndon JE II, Healy
P, et al: Preventing Lck activation in CAR T cells confers treg
resistance but requires 4-1BB signaling for them to persist and
treat solid tumors in nonlymphodepleted hosts. Clin Cancer Res.
25:358–368. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Mussai F, Wheat R, Sarrou E, Booth S,
Stavrou V, Fultang L, Perry T, Kearns P, Cheng P, Keeshan K, et al:
Targeting the arginine metabolic brake enhances immunotherapy for
leukaemia. Int J Cancer. 145:2201–2208. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Beavis PA, Henderson MA, Giuffrida L,
Mills JK, Sek K, Cross RS, Davenport AJ, John LB, Mardiana S,
Slaney CY, et al: Targeting the adenosine 2A receptor enhances
chimeric antigen receptor T cell efficacy. J Clin Invest.
127:929–941. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Leone RD, Sun IM, Oh MH, Sun IH, Wen J,
Englert J and Powell JD: Inhibition of the adenosine A2a receptor
modulates expression of T cell coinhibitory receptors and improves
effector function for enhanced checkpoint blockade and ACT in
murine cancer models. Cancer Immunol Immunother. 67:1271–1284.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Mussai F, De Santo C, Abu-Dayyeh I, Booth
S, Quek L, McEwen-Smith RM, Qureshi A, Dazzi F, Vyas P and
Cerundolo V: Acute myeloid leukemia creates an arginase-dependent
immunosuppressive microenvironment. Blood. 122:749–758. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Patsoukis N, Bardhan K, Chatterjee P, Sari
D, Liu B, Bell LN, Karoly ED, Freeman GJ, Petkova V, Seth P, et al:
PD-1 alters T-cell metabolic reprogramming by inhibiting glycolysis
and promoting lipolysis and fatty acid oxidation. Nat Commun.
6:66922015. View Article : Google Scholar : PubMed/NCBI
|