Introduction
Papillary thyroid cancer (PTC) is the most common
histological type of thyroid cancer (1,2) and is
generally associated with a low malignancy rate and favorable
prognosis; the survival rate after treatment exceeds 98% (3–7).
Although the majority of patients with PTC can survive long-term,
the tumor occasionally exhibits aggressive behavior, including
metastasis to distant organs (8,9).
However, such cases are rare, ~5% of cases of papillary thyroid
carcinoma result in distant metastasis (10). Distant metastases from PTC
frequently involve the lungs, bones and brain (11–13).
Although bone metastases are less common compared with lung
metastases, they remain a clinically important complication that
can affect both quality of life and survival. Bone metastases occur
in 1–7% of all PTC cases (14).
Although the overall incidence of bone metastases in thyroid cancer
is low, their presence can significantly influence both treatment
strategies and prognosis. Bone metastases not only result in
skeletal pain and functional impairment, but can also increase the
risk of pathological fractures due to local bone destruction. The
femur, as a load-bearing bone, is particularly vulnerable to such
complications (15,16). Reports of femoral fractures due to
bone metastases from thyroid cancer are rare (17) because distant metastasis of PTC is
uncommon. Another reason is that the femur, as a strong and robust
long bone, typically requires extensive structural compromise
before a fracture occurs (18).
The present report describes the case of a
53-year-old female patient who was admitted to the hospital with
left hip pain and limited mobility after a fall, which was
ultimately diagnosed with an intertrochanteric fracture of the left
femur, thyroid cancer with bone metastases, hyperthyroidism and
lung metastases. The rarity of this case lies in the occurrence of
a femoral fracture secondary to PTC metastasis. This clinical
scenario not only presents challenges in diagnosis and treatment,
but also offers novel insights into the metastatic behavior of
thyroid cancer. Through a detailed analysis of the present case,
the present report aims to enhance the understanding of bone
metastases in PTC and explore the implications for patient
management and prognosis.
Case report
The present report describes the case of a
53-year-old woman who was admitted to Nanxishan Hospital (Guilin,
China) in August 2024 with left hip pain and limited mobility that
had persisted for >16 h after a fall. The patient had no history
of orthopedic trauma or orthopedic disease and had not been
diagnosed with hyperthyroidism prior to admission. On admission, a
physical examination revealed an externally rotated shortening
deformity of the left lower limb, marked tenderness on palpation of
the left hip, limitation of hip joint range of motion, positive
longitudinal percussion tenderness and difficulty cooperating with
a hip and knee examination due to pain.
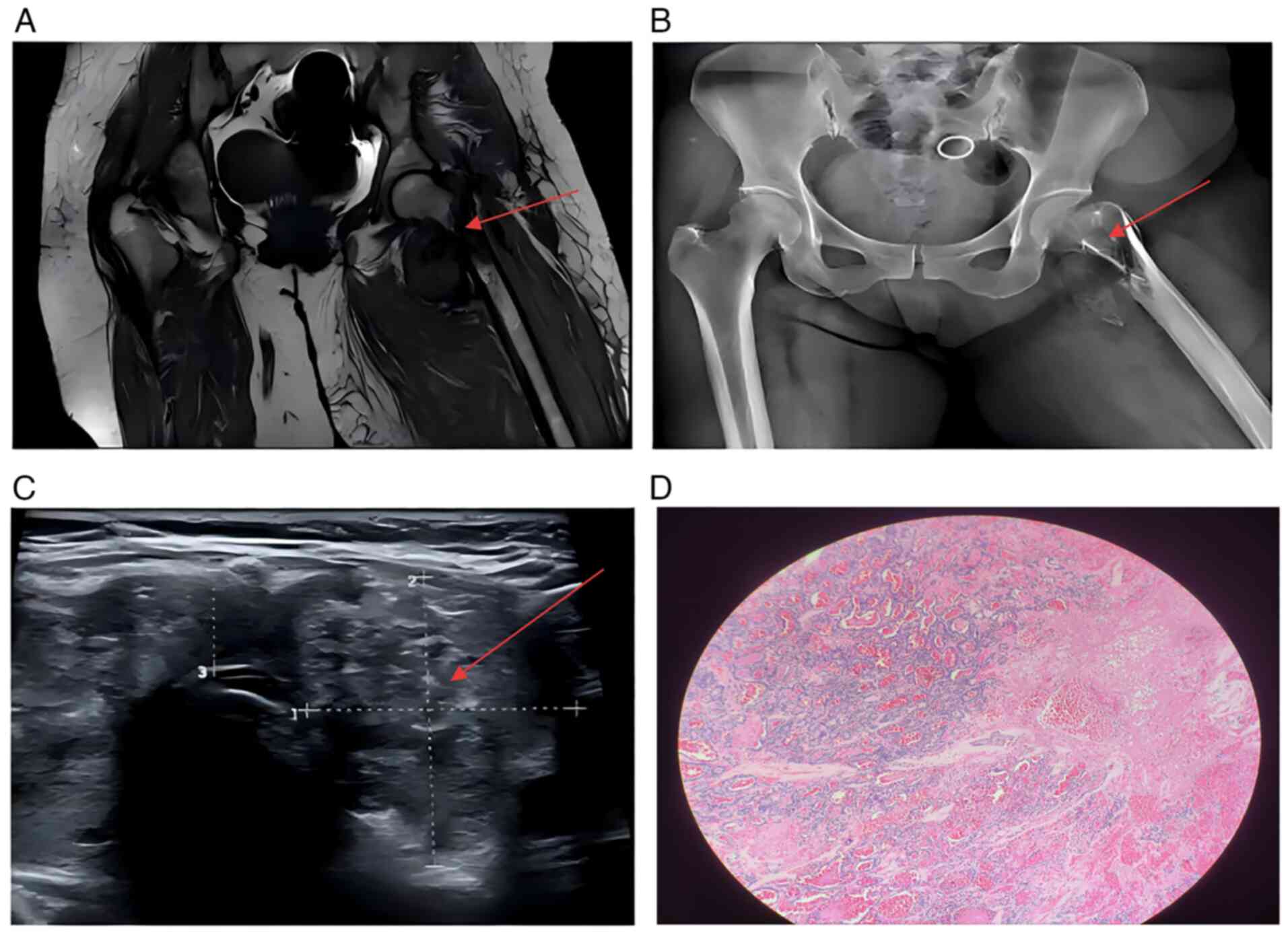
Radiographs suggested an intertrochanteric fracture
of the left femur (Fig. 1B). MRI
revealed multiple abnormal signal shadows in the left proximal
femur, left acetabulum, left suprapubic ramus and right femoral
neck, consistent with multiple bone metastases, a pathological
fracture of the left femur and local soft-tissue mass formation
(Fig. 1A). CT further demonstrated
a small displacement of the left femoral neck and a pathological
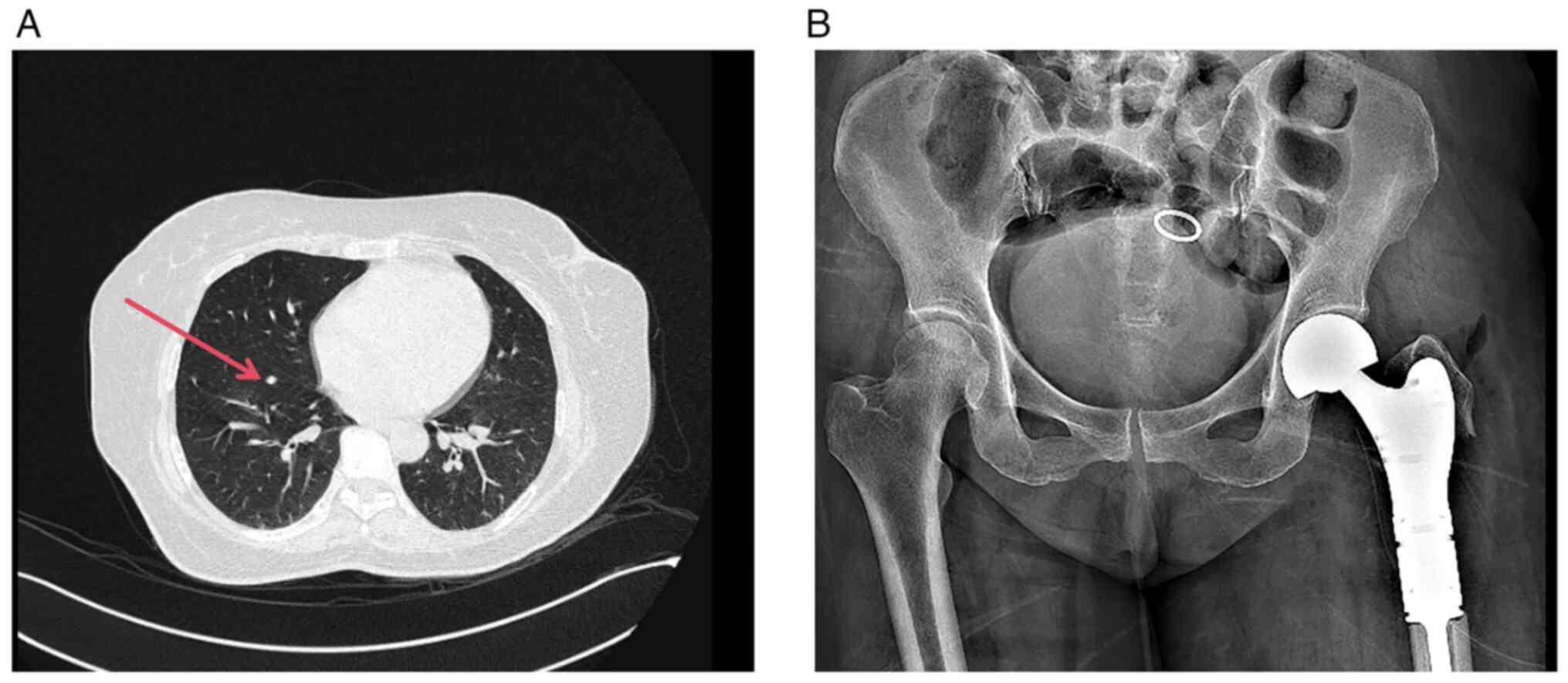
fracture (Fig. 1B). Lung CT
revealed nodules of variable sizes in both lungs (Fig. 2A), suggesting possible pulmonary
metastases whereas ultrasonography showed multiple thyroid nodules
[Thyroid Imaging Reporting and Data System (19) grade 5].
Laboratory test results were as follows for thyroid
function: Thyroid-stimulating hormone, 0.01 uIU/ml (normal range,
0.27–4.2 uIU/ml); free thyroxine, 29.90 pmol/l (normal range, 12–22
pmol/l); free triiodothyronine, 6.2 pmol/l (normal range, 3.1–6.8
pmol/l); thyroxine, 146 nmol/l (normal range, 66–181 nmol/l);
triiodothyronine, 2.17 nmol/l (normal range, 1.3–3.1 nmol/l);
thyroid peroxidase antibody, 170.00 IU/ml (normal range, ≤34
IU/ml); thyroglobulin antibody, 1,578 IU/ml (normal range, 0–115
IU/ml); serum thyroglobulin, >500 ng/ml (normal range, 3.5–77
ng/ml); serum calcium, 2.01 mmol/l (normal range, 2.15–2.55
mmol/l); and alkaline phosphatase, 41 U/l (normal range, 50–135
U/l).
After comprehensive evaluation, including history
taking, physical examination, imaging and laboratory review, the
patient was diagnosed with the following: i) An intertrochanteric
fracture of the left femur; ii) suspected thyroid cancer with bone
metastases; and iii) hyperthyroidism. Given the complexity and
urgency of the patient's condition, a detailed treatment plan was
developed. First, treatment for hyperthyroidism (thiamazole tablets
20 mg orally once a day for 4 days) was initiated to stabilize
thyroid function. Surgical intervention may be appropriate for
pathological fractures caused by malignant tumors, even if survival
is <6 weeks (20). Therefore,
after the patient's hyperthyroid symptoms were effectively
controlled, a bone tumor resection and left artificial femoral head
replacement were performed 5 days post-admission. The surgery
proceeded and the patient recovered uneventfully (Fig. 2B). Postoperative pathological
examination was performed. Samples were fixed in 10% neutral
buffered formalin at room temperature for 24 h. They were then
dehydrated, embedded in paraffin, sectioned at a thickness of 4 µm,
deparaffinized and rehydrated. Slices were subjected to hematoxylin
and eosin staining at room temperature for 1.5 min and then
observed under a light microscope. Histology confirmed PTC with
metastasis to the left femoral head (Fig. 1D).
Regarding treatment of the primary thyroid cancer,
an elective palliative thyroidectomy was recommended after
postoperative recovery to further control disease progression.
However, the patient declined the surgical intervention after being
fully informed of the risks and prognosis. The patient did not
consent to postoperative chemotherapy or radiotherapy and did not
undergo palliative treatment for thyroid cancer. At 1 year
post-surgery, follow-up through telephone revealed that the patient
was in good general condition. The patient was ambulatory with the
use of crutches and was able to perform normal daily activities.
Further follow-up by telephone is being performed every three
months.
Discussion
The present report describes a rare case of an
intertrochanteric fracture of the left femur caused by PTC,
providing clinical insights. Although PTC typically has a favorable
prognosis and is less likely to metastasize to distant organs
(21) the present case illustrates
that even well-differentiated PTC can metastasize aggressively,
with serious consequences for the patient's quality of life and
overall survival time if timely treatment is not provided. In the
present case, the patient presented with a femoral fracture, where
further investigation revealed metastatic PTC, underscoring the
need for early and aggressive surgical management in such
cases.
In addition, femoral fractures are associated with
osteoporosis, particularly among older adults (22). However, the underlying cause in the
present case was femoral metastasis from PTC, a rare and
under-reported phenomenon. Although PTC often metastasizes to the
lungs and bones, there are few reports in the literature of femoral
fractures as the initial manifestation (13). The present case underscores the need
to include metastatic disease in the differential diagnosis of
femoral fractures, especially in patients with a history of
cancer.
The co-occurrence of hyperthyroidism complicated the
treatment plan in the present case. Hyperthyroidism disrupts bone
metabolism and increases bone fragility, thereby raising the risk
of pathological fractures (23).
Therefore, in the management of these patients, controlling thyroid
function to normal levels is critical for maintaining bone
health.
Several studies have reported associations between
thyroid cancer and femoral fractures, most frequently in the
context of follicular or columnar cell variants (24–26).
However, PTC presenting initially with a pathological fracture
remains uncommon. A previous study revealed the molecular
mechanisms underlying PTC metastasis and recurrence by
comprehensively analyzing the expression profiles of microRNAs and
mRNAs in PTC. It was found that the ribosomal signaling pathway and
p53 signaling pathway serve key roles in bone metastasis and
recurrence of PTC (27). These
findings provide novel biomarkers and potential therapeutic targets
for the prognostic assessment of PTC bone metastases and the
development of personalized therapeutic strategies, which may hold
important clinical translational value.
In conclusion, the present case not only
demonstrates the rarity of pathological femoral fractures due to
bone metastasis from PTC, but also highlights the need for
comprehensive, multimodal evaluation in similar complex
presentations to ensure accurate diagnosis and appropriate
treatment planning. Patients with thyroid cancer, especially those
at risk for metastasis, should undergo early screening, prompt
therapeutic intervention and regular follow-up to improve both
quality of life and prognosis.
Since the present patient refused palliative thyroid
cancer resection and subsequent treatment, it was impossible to
assess the local control rate and survival benefit of this
intervention. Although this decision respects the autonomy of
patient, it has objectively resulted in the following consequences:
It is difficult to assess the actual benefits of palliative
resection in delaying the progression of thyroid cancer (such as
the potential for prolonging survival). This decision increased the
complexity and risk of future treatment, underscoring the
importance of comprehensive communication with patients and their
families when formulating individualized treatment plans. As this
is a single case report, the results cannot be extrapolated to a
wider population. Although the patient retained basic functional
abilities at the 1-year follow-up after surgery, the limited
observation period was insufficient to reveal the tumor's long-term
development.
In conclusion, the present case report highlights
the fact that PTC can lead to rare intertrochanteric fractures of
the femur, emphasizing the importance of early detection and timely
treatment, even in cases of PTC, which is generally associated with
favorable outcomes. Early and aggressive intervention should be
recommended for patients with PTC to reduce the risk of metastatic
spread, maintain quality of life and prevent life-threatening
complications. Healthcare professionals should consider the
possibility of malignant metastasis in patients presenting with
atypical fractures. The present report highlights the rarity and
seriousness of PTC bone metastases and the importance of early
detection and treatment.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article
Authors' contributions
JC designed the study, advised on patient treatment,
analyzed patient data and wrote the manuscript. JC and MZ obtained
medical images (e.g. MRI and CT scans). JC and MZ collected and
read the literature, and revised the manuscript. Both authors have
read and approved the manuscript. JC and MZ confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Su Y, Mei L, Wu Y, Li C, Jiang T, Zhao Y,
Feng X, Sun T, Li Y, Wang Z and Ji Y: Xenotropic and polytropic
retrovirus receptor 1 (XPR1) promotes progression of papillary
thyroid carcinoma via the BRAF-ERK1/2-P53 signaling pathway. J
Endocrinol Invest. 48:633–652. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhao C, Bo J, Li T, Tian J, Long T, He Y,
Chen S and Liu C: Blue light-driven cell cycle arrest in thyroid
cancer via Retinal-OPN3 complex. Cell Commun Signal. 22:5302024.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen DW and Yeh MW: Disparities in thyroid
care. Endocrinol Metab Clin North Am. 51:229–241. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
He J, Wang Y, Chen X, Chen W and Zhou J:
Value of thyroid cancer history in the prognosis of pancreatic
cancer: A SEER population-based study. Sci Rep. 13:57712023.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Powell BL, Craig JB and Muss HB: Thyroid
cancer. Am Fam Physician. 30:185–192. 1984.PubMed/NCBI
|
|
6
|
Zhao X, Bie F, Luo C and Zhang JE:
Distress, illness perception and coping style among thyroid cancer
patients after thyroidectomy: A cross-sectional study. Eur J Oncol
Nurs. 69:1025172024. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Carnazza M, Quaranto D, DeSouza N,
Moscatello AL, Garber D, Hemmerdinger S, Islam HK, Tiwari RK, Li XM
and Geliebter J: The current understanding of the molecular
pathogenesis of papillary thyroid cancer. Int J Mol Sci.
26:46462025. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang Y, Yang J, Chen S, Wang W and Teng L:
Identification and validation of a prognostic signature for thyroid
cancer based on ferroptosis-related genes. Genes (Basel).
13:9972022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ambrosi F, Righi A, Ricci C, Erickson LA,
Lloyd RV and Asioli S: Hobnail variant of papillary thyroid
carcinoma: A literature review. Endocr Pathol. 28:293–301. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Su H, Li Y, Men Q, Hao J and Zhang F:
Analysis of risk factors for distant metastasis of column cell
subtypes of thyroid papillary carcinoma. Eur Arch Otorhinolaryngol.
282:4259–4264. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kato S, Demura S, Shinmura K, Yokogawa N,
Shimizu T and Tsuchiya H: Current management of bone metastases
from differentiated thyroid cancer. Cancers (Basel). 13:44292021.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cascio V, Doerfler WR and Taneja C:
Diagnosis and management of brain metastasis from thyroid cancer.
Endocr Oncol. 5:e2500022025.PubMed/NCBI
|
|
13
|
Song HJ, Xue YL, Qiu ZL and Luo QY:
Uncommon metastases from differentiated thyroid carcinoma. Hell J
Nucl Med. 15:233–240. 2012.PubMed/NCBI
|
|
14
|
Carbone A, Verrienti A, Cito DS, Corazza C
and Bruno R: Excellent RAI therapeutic response on a patient
presenting skull metastasis of follicular thyroid cancer after 15
years. Endocrine. 87:468–473. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Iñiguez-Ariza NM, Bible KC and Clarke BL:
Bone metastases in thyroid cancer. J Bone Oncol. 21:1002822020.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Osorio M, Moubayed SP, Su H and Urken ML:
Systematic review of site distribution of bone metastases in
differentiated thyroid cancer. Head Neck. 39:812–818. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang X and Chen Y, Zeng D, Liang R, Liao
Z, Wei G, Hao W, Lu W and Chen Y: Complete resorption of the
humerus in metastatic thyroid carcinoma: A case report. BMC
Musculoskelet Disord. 25:1772024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sass JO, Saemann M, Kebbach M, Soodmand E,
Wree A, Bader R and Kluess D: The morphology of the femur
influences the fracture risk during stumbling and falls on the
hip-A computational biomechanical study. Life (Basel).
14:8412024.PubMed/NCBI
|
|
19
|
Tessler FN, Middleton WD and Grant EG:
Thyroid imaging reporting and data system (TI-RADS): A User's
guide. Radiology. 287:29–36. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hashimoto K, Nishimura S, Ito T, Kakinoki
R and Goto K: Treatment algorithm for metastatic malignancies in
the lower extremities. Mol Clin Oncol. 21:5120241 View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sapuppo G, Martorana F, Tirrò E, Le Moli
R, Masucci R, Baldeschi L, Spatola C, Belfiore A, Vigneri P and
Pellegriti G: Orbital metastasis from thyroid cancer: A case report
and review of the literature. Ann Palliat Med. 11:3346–3355. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rachner TD, Khosla S and Hofbauer LC:
Osteoporosis: Now and the future. Lancet. 377:1276–1287. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Delitala AP, Scuteri A and Doria C:
Thyroid hormone diseases and osteoporosis. J Clin Med. 9:10342020.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Genton CY, Dutoit M, Portmann L, Gillet M
and Guillou L: Pathologic fracture of the femur neck as first
manifestation of a minute columnar cell carcinoma of the thyroid
gland. Pathol Res Pract. 194:861–866. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fortson JK, Brown J, Patel VG, Lawrence GE
and Rosenthal M: Pathologic fracture of the femur as a presenting
sign of metastatic follicular carcinoma of the thyroid. Am Surg.
76:E137–E138. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hatfield JS, Bonneau PN, Shakir MKM and
Hoang TD: Atypical femur fracture unmasking follicular thyroid
cancer in a 54-year-old woman. AACE Clin Case Rep. 9:213–215.
2023.PubMed/NCBI
|
|
27
|
Zhang YJ, Ma YS, Xia Q, Yu F, Lv ZW, Jia
CY, Jiang XX, Zhang L, Shao Y, Xie WT, et al: MicroRNA-mRNA
integrated analysis based on a case of well-differentiated thyroid
cancer with both metastasis and metastatic recurrence. Oncol Rep.
40:3803–3811. 2018.PubMed/NCBI
|