|
1
|
Li Y, Wu X, Yang P, Jiang G and Luo Y:
Machine learning for lung cancer diagnosis, treatment, and
prognosis. Genomics Proteomics Bioinformatics. 20:850–866. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bade BC and Dela Cruz CS: Lung cancer
2020: Epidemiology, etiology, and prevention. Clin Chest Med.
41:1–24. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Harðardottir H, Jonsson S, Gunnarsson O,
Hilmarsdottir B, Asmundsson J, Gudmundsdottir I, Saevarsdottir VY,
Hansdottir S, Hannesson P and Gudbjartsson T: Advances in lung
cancer diagnosis and treatment-a review. Laeknabladid. 108:17–29.
2020.(In Icelandic). View Article : Google Scholar
|
|
4
|
Abu Rous F, Singhi EK, Sridhar A, Faisal
MS and Desai A: Lung cancer treatment advances in 2022. Cancer
Invest. 41:12–24. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
5
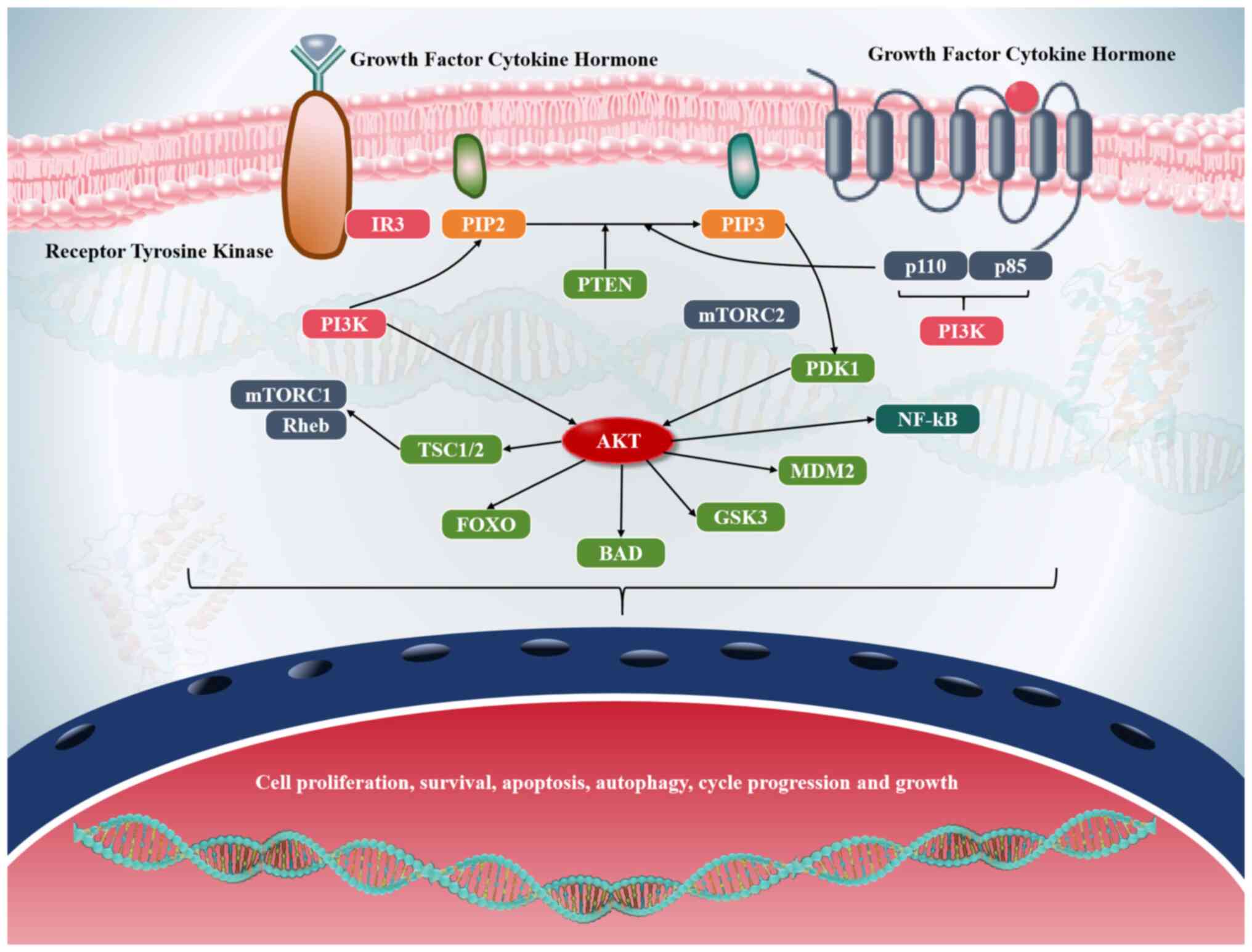
|
Wu F, Wang L and Zhou C: Lung cancer in
China: Current and prospect. Curr Opin Oncol. 33:40–46. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rodriguez-Canales J, Parra-Cuentas E and
Wistuba II: Diagnosis and molecular classification of lung cancer.
Cancer Treat Res. 170:25–46. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
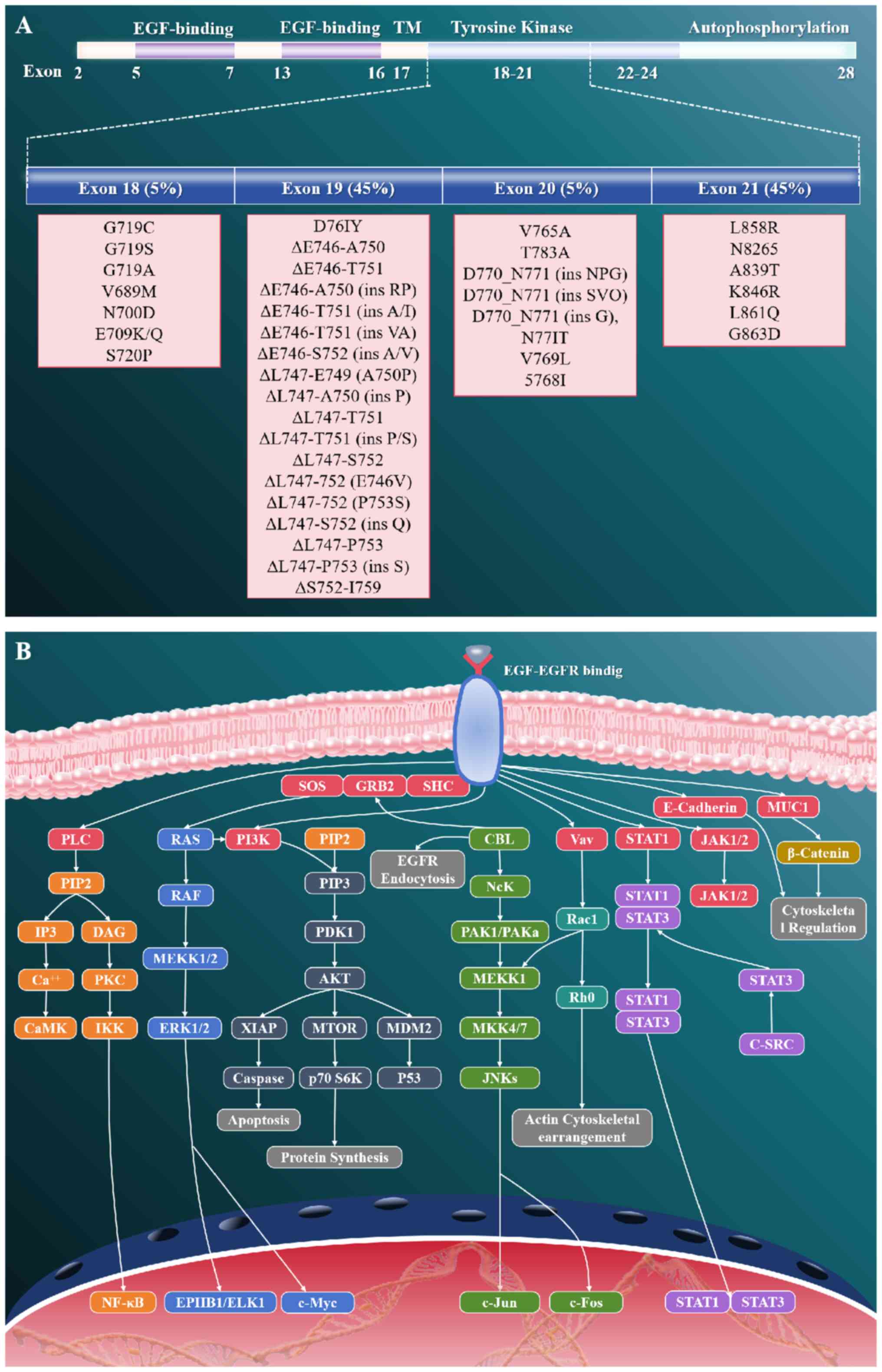
7
|
de Sousa VML and Carvalho L: Heterogeneity
in lung cancer. Pathobiology. 85:96–107. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Abolfathi H, Arabi M and Sheikhpour M: A
literature review of microRNA and gene signaling pathways involved
in the apoptosis pathway of lung cancer. Respir Res. 24:552023.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Niu Z, Jin R, Zhang Y and Li H: Signaling
pathways and targeted therapies in lung squamous cell carcinoma:
Mechanisms and clinical trials. Signal Transduct Target Ther.
7:3532022. View Article : Google Scholar : PubMed/NCBI
|
|
10
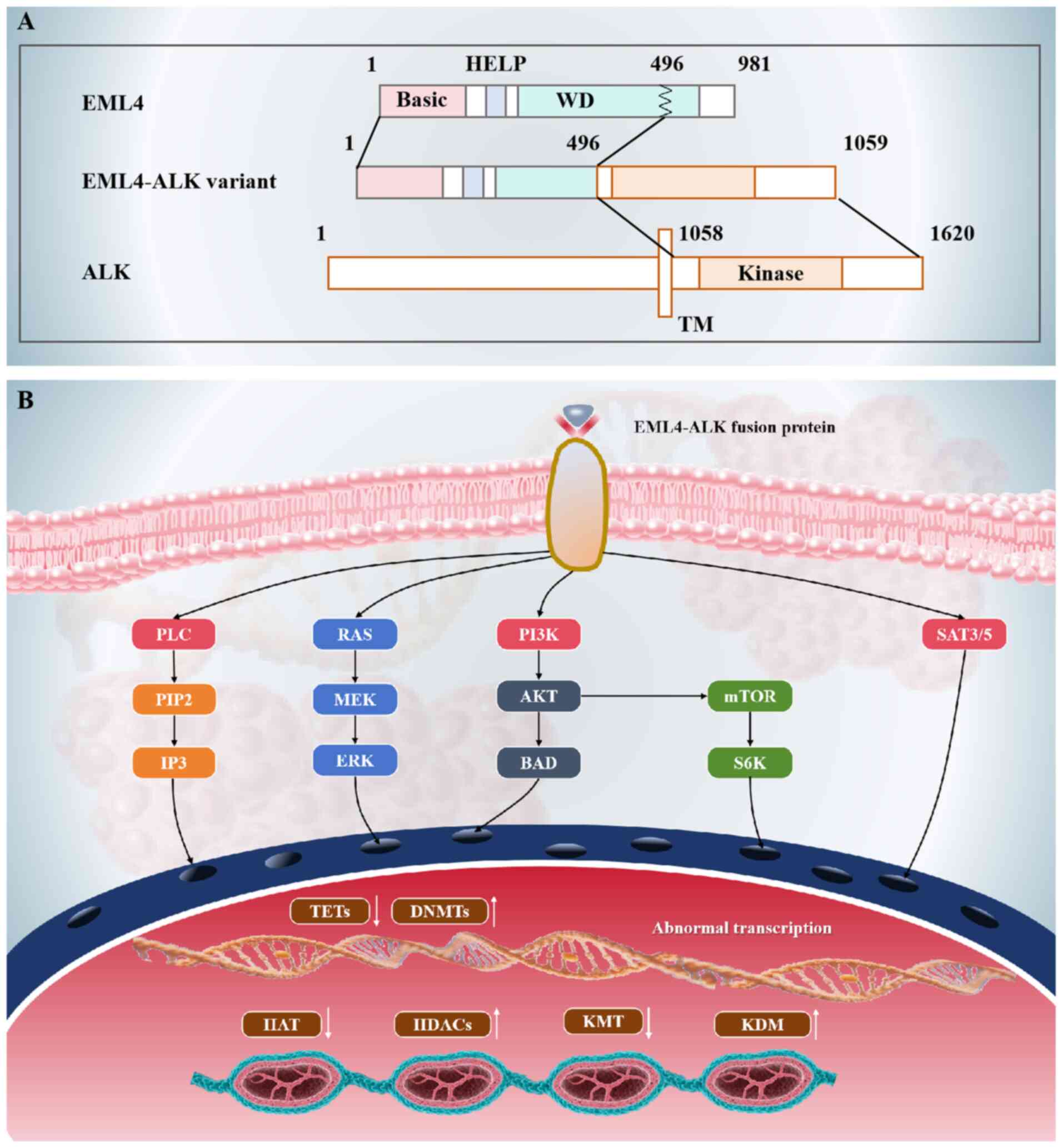
|
Yuan M, Zhao Y, Arkenau HT, Lao T, Chu L
and Xu Q: Signal pathways and precision therapy of small-cell lung
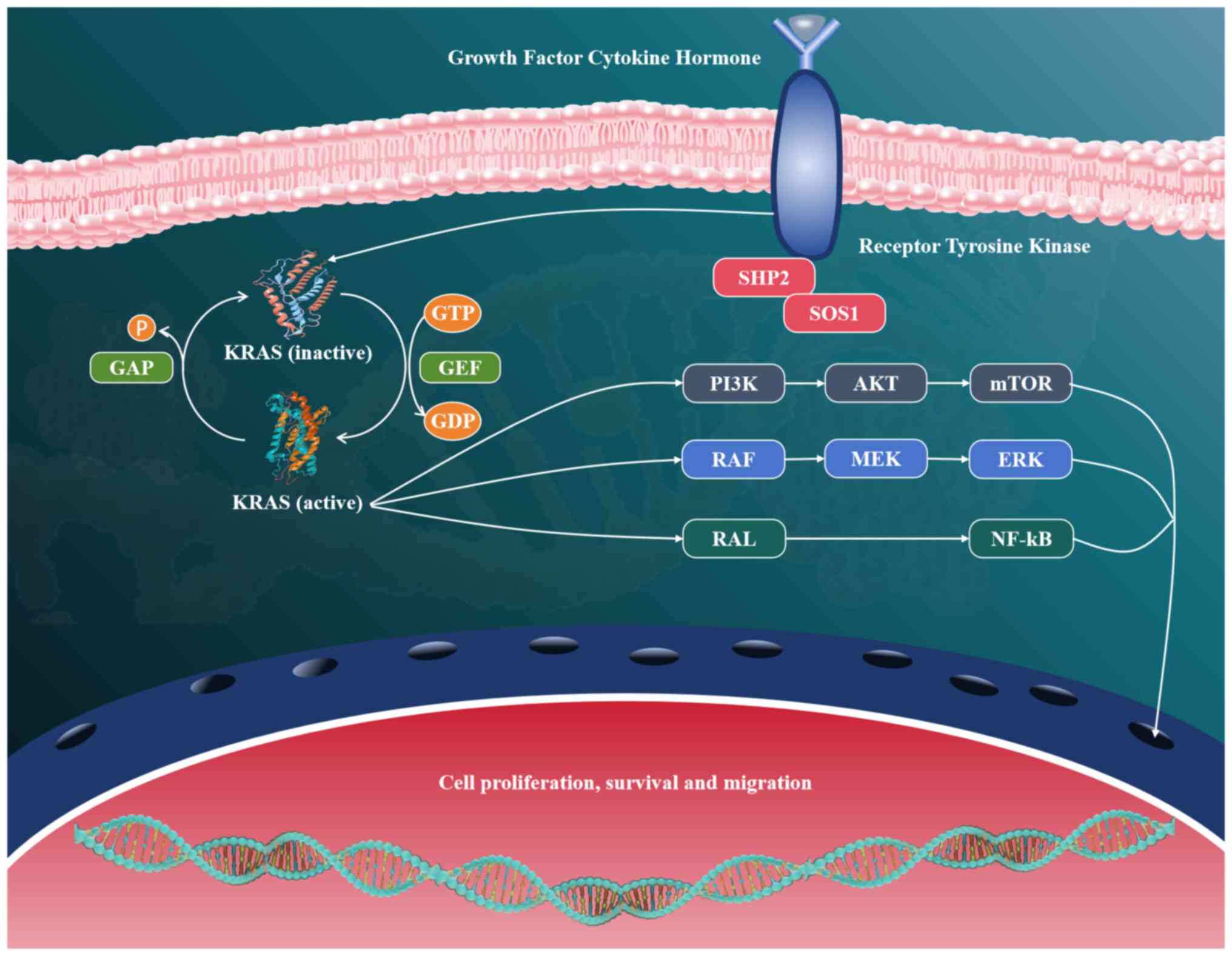
cancer. Signal Transduct Target Ther. 7:1872022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Masciale V, Banchelli F, Grisendi G,
Samarelli AV, Raineri G, Rossi T, Zanoni M, Cortesi M, Bandini S,
Ulivi P, et al: The molecular features of lung cancer stem cells in
dedifferentiation process-driven epigenetic alterations. J Biol
Chem. 300:1079942024. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hoque MO, Brait M, Rosenbaum E, Poeta ML,
Pal P, Begum S, Dasgupta S, Carvalho AL, Ahrendt SA, Westra WH and
Sidransky D: Genetic and epigenetic analysis of erbB signaling
pathway genes in lung cancer. J Thorac Oncol. 5:1887–1893. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
He H, He MM, Wang H, Qiu W, Liu L, Long L,
Shen Q, Zhang S, Qin S, Lu Z, et al: In utero and
childhood/adolescence exposure to tobacco smoke, genetic risk, and
lung cancer incidence and mortality in adulthood. Am J Respir Crit
Care Med. 207:173–182. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen CY, Huang KY, Chen CC, Chang YH, Li
HJ, Wang TH and Yang PC: The role of PM2.5 exposure in lung cancer:
Mechanisms, genetic factors, and clinical implications. EMBO Mol
Med. 17:31–40. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nagano T, Tachihara M and Nishimura Y:
Molecular mechanisms and targeted therapies including immunotherapy
for non-small cell lung cancer. Curr Cancer Drug Targets.
19:595–630. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Samarelli AV, Masciale V, Aramini B, Coló
GP, Tonelli R, Marchioni A, Bruzzi G, Gozzi F, Andrisani D,
Castaniere I, et al: Molecular mechanisms and cellular contribution
from lung fibrosis to lung cancer development. Int J Mol Sci.
22:121792021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ohmori T, Yamaoka T, Ando K, Kusumoto S,
Kishino Y, Manabe R and Sagara H: Molecular and clinical features
of EGFR-TKI-associated lung injury. Int J Mol Sci. 22:7922021.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schneider JL, Lin JJ and Shaw AT:
ALK-positive lung cancer: A moving target. Nat Cancer. 4:330–343.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Reck M, Carbone DP, Garassino M and
Barlesi F: Targeting KRAS in non-small-cell lung cancer: Recent
progress and new approaches. Ann Oncol. 32:1101–1110. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yoda S, Dagogo-Jack I and Hata AN:
Targeting oncogenic drivers in lung cancer: Recent progress,
current challenges and future opportunities. Pharmacol Ther.
193:20–30. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Herrera-Juárez M, Serrano-Gómez C,
Bote-de-Cabo H and Paz-Ares L: Targeted therapy for lung cancer:
Beyond EGFR and ALK. Cancer. 129:1803–1820. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yoneda K, Imanishi N, Ichiki Y and Tanaka
F: Treatment of non-small cell lung cancer with EGFR-mutations. J
UOEH. 41:153–163. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hosomi Y, Morita S, Sugawara S, Kato T,
Fukuhara T, Gemma A, Takahashi K, Fujita Y, Harada T, Minato K, et
al: Gefitinib alone versus gefitinib plus chemotherapy for
non-small-cell lung cancer with mutated epidermal growth factor
receptor: NEJ009 study. J Clin Oncol. 38:115–123. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Greenhalgh J, Bagust A, Boland A, Dwan K,
Beale S, Hockenhull J, Proudlove C, Dundar Y, Richardson M, Dickson
R, et al: Erlotinib and gefitinib for treating non-small cell lung
cancer that has progressed following prior chemotherapy (review of
NICE technology appraisals 162 and 175): A systematic review and
economic evaluation. Health Technol Assess. 19:1–134. 2015.
View Article : Google Scholar
|
|
25
|
Remon J, Besse B, Aix SP, Callejo A,
Al-Rabi K, Bernabe R, Greillier L, Majem M, Reguart N, Monnet I, et
al: Osimertinib treatment based on plasma T790M monitoring in
patients with EGFR-mutant non-small-cell lung cancer (NSCLC): EORTC
lung cancer group 1613 APPLE phase II randomized clinical trial.
Ann Oncol. 34:468–476. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Abdelgalil AA and Alkahtani HM:
Crizotinib: A comprehensive profile. Profiles Drug Subst Excip
Relat Methodol. 48:39–69. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Peters S, Camidge DR, Shaw AT, Gadgeel S,
Ahn JS, Kim DW, Ou SI, Pérol M, Dziadziuszko R, Rosell R, et al:
Alectinib versus crizotinib in untreated ALK-positive
non-small-cell lung cancer. N Engl J Med. 377:829–838. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Solomon BJ, Liu G, Felip E, Mok TSK, Soo
RA, Mazieres J, Shaw AT, de Marinis F, Goto Y, Wu YL, et al:
Lorlatinib versus crizotinib in patients with advanced ALK-positive
non-small cell lung cancer: 5-Year outcomes from the phase III
CROWN study. J Clin Oncol. 42:3400–3409. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Luo J, Ostrem J, Pellini B, Imbody D,
Stern Y, Solanki HS, Haura EB and Villaruz LC: Overcoming
KRAS-mutant lung cancer. Am Soc Clin Oncol Educ Book. 42:1–11.
2022.PubMed/NCBI
|
|
30
|
Jänne PA, Riely GJ, Gadgeel SM, Heist RS,
Ou SI, Pacheco JM, Johnson ML, Sabari JK, Leventakos K, Yau E, et
al: Adagrasib in non-small-cell lung cancer harboring a
KRASG12C mutation. N Engl J Med. 387:120–131. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Skoulidis F, Li BT, Dy GK, Price TJ,
Falchook GS, Wolf J, Italiano A, Schuler M, Borghaei H, Barlesi F,
et al: Sotorasib for lung cancers with KRAS p.G12C mutation. N Engl
J Med. 384:2371–2381. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Olivier T and Prasad V: Sotorasib in
KRAS(G12C) mutated lung cancer. Lancet. 403:1452024. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sanaei MJ, Razi S, Pourbagheri-Sigaroodi A
and Bashash D: The PI3K/Akt/mTOR pathway in lung cancer; oncogenic
alterations, therapeutic opportunities, challenges, and a glance at
the application of nanoparticles. Transl Oncol. 18:1013642022.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Iksen, Pothongsrisit S and Pongrakhananon
V: Targeting the PI3K/AKT/mTOR signaling pathway in lung cancer: An
update regarding potential drugs and natural products. Molecules.
26:41002021. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ghareghomi S, Atabaki V, Abdollahzadeh N,
Ahmadian S and Hafez Ghoran S: Bioactive PI3-kinase/Akt/mTOR
inhibitors in targeted lung cancer therapy. Adv Pharm Bull.
13:24–35. 2023.PubMed/NCBI
|
|
36
|
Tan AC: Targeting the PI3K/Akt/mTOR
pathway in non-small cell lung cancer (NSCLC). Thorac Cancer.
11:511–518. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen B, Song Y, Zhan Y, Zhou S, Ke J, Ao
W, Zhang Y, Liang Q, He M, Li S, et al: Fangchinoline inhibits
non-small cell lung cancer metastasis by reversing
epithelial-mesenchymal transition and suppressing the cytosolic
ROS-related Akt-mTOR signaling pathway. Cancer Lett.
543:2157832022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Li J, Zhang D, Wang S, Yu P, Sun J, Zhang
Y, Meng X, Li J and Xiang L: Baicalein induces apoptosis by
inhibiting the glutamine-mTOR metabolic pathway in lung cancer. J
Adv Res. 68:341–357. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Cheng W, Kang K, Zhao A and Wu Y: Dual
blockade immunotherapy targeting PD-1/PD-L1 and CTLA-4 in lung
cancer. J Hematol Oncol. 17:542024. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shen X, Huang S, Xiao H, Zeng S, Liu J,
Ran Z and Xiong B: Efficacy and safety of PD-1/PD-L1 plus CTLA-4
antibodies ± other therapies in lung cancer: A systematic review
and meta-analysis. Eur J Hosp Pharm. 30:3–8. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Vergnenegre A and Chouaid C: Economic
analyses of immune-checkpoint inhibitors to treat lung cancer.
Expert Rev Pharmacoecon Outcomes Res. 21:365–371. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Garon EB, Rizvi NA, Hui R, Leighl N,
Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L,
et al: Pembrolizumab for the treatment of non-small-cell lung
cancer. N Engl J Med. 372:2018–2028. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cascone T, Awad MM, Spicer JD, He J, Lu S,
Sepesi B, Tanaka F, Taube JM, Cornelissen R, Havel L, et al:
Perioperative nivolumab in resectable lung cancer. N Engl J Med.
390:1756–1769. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Felip E, Altorki N, Zhou C, Vallières E,
Martínez-Martí A, Rittmeyer A, Chella A, Reck M, Goloborodko O,
Huang M, et al: Overall survival with adjuvant atezolizumab after
chemotherapy in resected stage II–IIIA non-small-cell lung cancer
(IMpower010): A randomised, multicentre, open-label, phase III
trial. Ann Oncol. 34:907–919. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Zhang T, Li W, Diwu D, Chen L, Chen X and
Wang H: Efficacy and safety of first-line immunotherapy plus
chemotherapy in treating patients with extensive-stage small cell
lung cancer: A Bayesian network meta-analysis. Front Immunol.
14:11970442023. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
da Cunha Santos G, Shepherd FA and Tsao
MS: EGFR mutations and lung cancer. Annu Rev Pathol. 6:49–69. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Paez JG, Jänne PA, Lee JC, Tracy S,
Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, et
al: EGFR mutations in lung cancer: Correlation with clinical
response to gefitinib therapy. Science. 304:1497–1500. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Liu X, Wang P, Zhang C and Ma Z: Epidermal
growth factor receptor (EGFR): A rising star in the era of
precision medicine of lung cancer. Oncotarget. 8:50209–50220. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Agraso S, Lázaro M, Firvida XL, Santomé L,
Fernández N, Azpitarte C, Leon L, Garcia C, Hudobro G, Areses MC,
et al: Real-world data with afatinib in Spanish patients with
treatment-naïve non-small-cell lung cancer harboring exon 19
deletions in epidermal growth factor receptor (Del19 EGFR):
Clinical experience of the Galician lung cancer group. Cancer Treat
Res Commun. 33:1006462022.PubMed/NCBI
|
|
50
|
Matsui T, Tanizawa Y and Enatsu S: Exon 19
deletion and exon 21 L858R point mutation in EGFR Mutation-positive
non-small cell lung cancer. Gan To Kagaku Ryoho. 48:673–676.
2021.(In Japanese). PubMed/NCBI
|
|
51
|
Yu J, Zhang L, Peng J, Ward R, Hao P, Wang
J, Zhang N, Yang Y, Guo X, Xiang C, et al: Dictamnine, a novel
c-Met inhibitor, suppresses the proliferation of lung cancer cells
by downregulating the PI3K/AKT/mTOR and MAPK signaling pathways.
Biochem Pharmacol. 195:1148642022. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wen Z, Jiang R, Huang Y, Wen Z, Rui D,
Liao X and Ling Z: Inhibition of lung cancer cells and
Ras/Raf/MEK/ERK signal transduction by ectonucleoside triphosphate
phosphohydrolase-7 (ENTPD7). Respir Res. 20:1942019. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Qin BM, Chen X, Zhu JD and Pei DQ:
Identification of EGFR kinase domain mutations among lung cancer
patients in China: Implication for targeted cancer therapy. Cell
Res. 15:212–217. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Zhang Q, Dai HH, Dong HY, Sun CT, Yang Z
and Han JQ: EGFR mutations and clinical outcomes of chemotherapy
for advanced non-small cell lung cancer: A meta-analysis. Lung
Cancer. 85:339–345. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Wang C, Zhao K, Hu S, Dong W, Gong Y and
Xie C: Clinical outcomes of afatinib versus osimertinib in patients
with non-small cell lung cancer with uncommon EGFR mutations: A
pooled analysis. Oncologist. 28:e397–e405. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Sun H and Wu YL: Dacomitinib in
non-small-cell lung cancer: A comprehensive review for clinical
application. Future Oncol. 15:2769–2777. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Leonetti A, Sharma S, Minari R, Perego P,
Giovannetti E and Tiseo M: Resistance mechanisms to osimertinib in
EGFR-mutated non-small cell lung cancer. Br J Cancer. 121:725–737.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Skoulidis F and Papadimitrakopoulou VA:
Targeting the gatekeeper: Osimertinib in EGFR T790M
mutation-positive non-small cell lung cancer. Clin Cancer Res.
23:618–622. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Spagnolo CC, Ciappina G, Giovannetti E,
Squeri A, Granata B, Lazzari C, Pretelli G, Pasello G and Santarpia
M: Targeting MET in non-small cell lung cancer (NSCLC): A new old
story? Int J Mol Sci. 24:101192023. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Oh DY and Bang YJ: HER2-targeted
therapies-a role beyond breast cancer. Nat Rev Clin Oncol.
17:33–48. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Yin X, Li Y, Wang H, Jia T, Wang E, Luo Y,
Wei Y, Qin Z and Ma X: Small cell lung cancer transformation: From
pathogenesis to treatment. Semin Cancer Biol. 86:595–606. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Cheng WL, Feng PH, Lee KY, Chen KY, Sun
WL, Van Hiep N, Luo CS and Wu SM: The role of EREG/EGFR pathway in
tumor progression. Int J Mol Sci. 22:128282021. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Iqbal MA, Arora S, Prakasam G, Calin GA
and Syed MA: MicroRNA in lung cancer: Role, mechanisms, pathways
and therapeutic relevance. Mol Aspects Med. 70:3–20. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Lin L, Lu Q, Cao R, Ou Q, Ma Y, Bao H, Wu
X, Shao Y, Wang Z and Shen B: Acquired rare recurrent EGFR
mutations as mechanisms of resistance to osimertinib in lung cancer
and in silico structural modelling. Am J Cancer Res. 10:4005–4015.
2020.PubMed/NCBI
|
|
65
|
Mansour MA, AboulMagd AM, Abbas SH,
Abdel-Rahman HM and Abdel-Aziz M: Insights into fourth generation
selective inhibitors of (C797S) EGFR mutation combating non-small
cell lung cancer resistance: A critical review. RSC Adv.
13:18825–18853. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Singh D: Revolutionizing lung cancer
treatment: Innovative CRISPR-Cas9 delivery strategies. AAPS
PharmSciTech. 25:1292024. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Li L, Jiang H, Zeng B, Wang X, Bao Y, Chen
C, Ma L and Yuan J: Liquid biopsy in lung cancer. Clin Chim Acta.
554:1177572024. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Hsu PC, Jablons DM, Yang CT and You L:
Epidermal growth factor receptor (EGFR) pathway, yes-associated
protein (YAP) and the regulation of programmed death-ligand 1
(PD-L1) in non-small cell lung cancer (NSCLC). Int J Mol Sci.
20:38212019. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Elshatlawy M, Sampson J, Clarke K and
Bayliss R: EML4-ALK biology and drug resistance in non-small cell
lung cancer: A new phase of discoveries. Mol Oncol. 17:950–963.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Camidge DR, Dziadziuszko R, Peters S, Mok
T, Noe J, Nowicka M, Gadgeel SM, Cheema P, Pavlakis N, de Marinis
F, et al: Updated efficacy and safety data and impact of the
EML4-ALK fusion variant on the efficacy of alectinib in untreated
ALK-positive advanced non-small cell lung cancer in the global
phase III ALEX study. J Thorac Oncol. 14:1233–1243. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Paliouras AR, Buzzetti M, Shi L, Donaldson
IJ, Magee P, Sahoo S, Leong HS, Fassan M, Carter M, Di Leva G, et
al: Vulnerability of drug-resistant EML4-ALK rearranged lung cancer
to transcriptional inhibition. EMBO Mol Med. 12:e110992020.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Li K, Liu Y, Ding Y, Zhang Z, Feng J, Hu
J, Chen J, Lian Z, Chen Y, Hu K, et al: BCL6 is regulated by the
MAPK/ELK1 axis and promotes KRAS-driven lung cancer. J Clin Invest.
132:e1613082022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Gadgeel SM and Wozniak A: Preclinical
rationale for PI3K/Akt/mTOR pathway inhibitors as therapy for
epidermal growth factor receptor inhibitor-resistant non-small-cell
lung cancer. Clin Lung Cancer. 14:322–332. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Shi L, Zhu W, Huang Y, Zhuo L, Wang S,
Chen S, Zhang B and Ke B: Cancer-associated fibroblast-derived
exosomal microRNA-20a suppresses the PTEN/PI3K-AKT pathway to
promote the progression and chemoresistance of non-small cell lung
cancer. Clin Transl Med. 12:e9892022. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Tan AC and Tan DSW: Targeted therapies for
lung cancer patients with oncogenic driver molecular alterations. J
Clin Oncol. 40:611–625. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Ahn MJ, Kim HR, Yang JCH, Han JY, Li JYC,
Hochmair MJ, Chang GC, Delmonte A, Lee KH, Campelo RG, et al:
Efficacy and safety of brigatinib compared with crizotinib in asian
vs non-asian patients with locally advanced or metastatic
ALK-inhibitor-naive ALK+ non-small cell lung cancer: Final results
from the phase III ALTA-1L study. Clin Lung Cancer. 23:720–730.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Mok T, Camidge DR, Gadgeel SM, Rosell R,
Dziadziuszko R, Kim DW, Pérol M, Ou SHI, Ahn JS, Shaw AT, et al:
Updated overall survival and final progression-free survival data
for patients with treatment-naive advanced ALK-positive
non-small-cell lung cancer in the ALEX study. Ann Oncol.
31:1056–1064. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Baba K and Goto Y: Lorlatinib as a
treatment for ALK-positive lung cancer. Future Oncol. 18:2745–2766.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lin JJ, Zhu VW, Yoda S, Yeap BY, Schrock
AB, Dagogo-Jack I, Jessop NA, Jiang GY, Le LP, Gowen K, et al:
Impact of EML4-ALK variant on resistance mechanisms and clinical
outcomes in ALK-positive lung cancer. J Clin Oncol. 36:1199–1206.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Pinto JA, Raez LE and Domingo G: Clinical
consequences of resistance to ALK inhibitors in non-small cell lung
cancer. Expert Rev Respir Med. 14:385–390. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Shaw AT, Solomon BJ, Besse B, Bauer TM,
Lin CC, Soo RA, Riely GJ, Ou SHI, Clancy JS, Li S, et al: ALK
resistance mutations and efficacy of lorlatinib in advanced
anaplastic lymphoma kinase-positive non-small-cell lung cancer. J
Clin Oncol. 37:1370–1379. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Desai A and Lovly CM: Strategies to
overcome resistance to ALK inhibitors in non-small cell lung
cancer: A narrative review. Transl Lung Cancer Res. 12:615–628.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Balasundaram A and Doss GPC: A
computational examination of the therapeutic advantages of
fourth-generation ALK inhibitors TPX-0131 and repotrectinib over
third-generation lorlatinib for NSCLC with ALK F1174C/L/V
mutations. Front Mol Biosci. 10:13060462024. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Golding B, Luu A, Jones R and
Viloria-Petit AM: The function and therapeutic targeting of
anaplastic lymphoma kinase (ALK) in non-small cell lung cancer
(NSCLC). Mol Cancer. 17:522018. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Torres-Jiménez J, Espinar JB, de Cabo HB,
Berjaga MZ, Esteban-Villarrubia J, Fraile JZ and Paz-Ares L:
Targeting KRAS(G12C) in non-small-cell lung cancer: Current
standards and developments. Drugs. 84:527–548. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Chang YS, Tu SJ, Chen YC, Liu TY, Lee YT,
Yen JC, Fang HY and Chang JG: Mutation profile of non-small cell
lung cancer revealed by next generation sequencing. Respir Res.
22:32021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Mugarza E, van Maldegem F, Boumelha J,
Moore C, Rana S, Llorian Sopena M, East P, Ambler R, Anastasiou P,
Romero-Clavijo P, et al: Therapeutic KRASG12C inhibition
drives effective interferon-mediated antitumor immunity in
immunogenic lung cancers. Sci Adv. 8:eabm87802022. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ceddia S, Landi L and Cappuzzo F:
KRAS-mutant non-small-cell lung cancer: From past efforts to future
challenges. Int J Mol Sci. 23:93912022. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Bironzo P, Cani M, Jacobs F, Napoli VM,
Listì A, Passiglia F, Righi L, Di Maio M, Novello S and Scagliotti
GV: Real-world retrospective study of KRAS mutations in advanced
non-small cell lung cancer in the era of immunotherapy. Cancer.
129:1662–1671. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Ferrer I, Zugazagoitia J, Herbertz S, John
W, Paz-Ares L and Schmid-Bindert G: KRAS-mutant non-small cell lung
cancer: From biology to therapy. Lung Cancer. 124:53–64. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Xu K, Park D, Magis AT, Zhang J, Zhou W,
Sica GL, Ramalingam SS, Curran WJ and Deng X: Small molecule KRAS
agonist for mutant KRAS cancer therapy. Mol Cancer. 18:852019.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Brazel D, Arter Z and Nagasaka M: A long
overdue targeted treatment for KRAS mutations in NSCLC: Spotlight
on adagrasib. Lung Cancer (Auckl). 13:75–80. 2022.PubMed/NCBI
|
|
93
|
Di Federico A, Ricciotti I, Favorito V,
Michelina SV, Scaparone P, Metro G, De Giglio A, Pecci F, Lamberti
G, Ambrogio C and Ricciuti B: Resistance to KRAS G12C inhibition in
non-small cell lung cancer. Curr Oncol Rep. 25:1017–1029. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Canon J, Rex K, Saiki AY, Mohr C, Cooke K,
Bagal D, Gaida K, Holt T, Knutson CG, Koppada N, et al: The
clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity.
Nature. 575:217–223. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lee A: Sotorasib: A review in KRAS G12C
mutation-positive non-small cell lung cancer. Target Oncol.
17:727–733. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Mausey N and Halford Z: Targeted therapies
for previously ‘undruggable’ KRAS-mutated non-small cell lung
cancer: A review of sotorasib and adagrasib. Ann Pharmacother.
58:622–635. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Briere DM, Li S, Calinisan A, Sudhakar N,
Aranda R, Hargis L, Peng DH, Deng J, Engstrom LD, Hallin J, et al:
The KRASG12C inhibitor MRTX849 reconditions the tumor
immune microenvironment and sensitizes tumors to checkpoint
inhibitor therapy. Mol Cancer Ther. 20:975–985. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Shi Z, Weng J, Niu H, Yang H, Liu R, Weng
Y, Zhu Q, Zhang Y, Tao L, Wang Z, et al: D-1553: A novel
KRASG12C inhibitor with potent and selective cellular
and in vivo antitumor activity. Cancer Sci. 114:2951–2960. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Santarpia M, Ciappina G, Spagnolo CC,
Squeri A, Passalacqua MI, Aguilar A, Gonzalez-Cao M, Giovannetti E,
Silvestris N and Rosell R: Targeted therapies for KRAS-mutant
non-small cell lung cancer: From preclinical studies to clinical
development-a narrative review. Transl Lung Cancer Res. 12:346–368.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Yun J, Nakagawa R and Tham K:
KRAS-targeted therapy in the treatment of non-small cell lung
cancer. J Oncol Pharm Pract. 29:422–430. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Corral de la Fuente E, Olmedo Garcia ME,
Gomez Rueda A, Lage Y and Garrido P: Targeting KRAS in non-small
cell lung cancer. Front Oncol. 11:7926352022. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Tomasini P, Walia P, Labbe C, Jao K and
Leighl NB: Targeting the KRAS pathway in non-small cell lung
cancer. Oncologist. 21:1450–1460. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Li XQ, Cheng XJ, Wu J, Wu KF and Liu T:
Targeted inhibition of the PI3K/AKT/mTOR pathway by
(+)-anthrabenzoxocinone induces cell cycle arrest, apoptosis, and
autophagy in non-small cell lung cancer. Cell Mol Biol Lett.
29:582024. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Gong G, Ganesan K, Xiong Q and Zheng Y:
Antitumor effects of ononin by modulation of apoptosis in
non-small-cell lung cancer through inhibiting PI3K/Akt/mTOR
pathway. Oxid Med Cell Longev. 2022:51224482022. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Chandarlapaty S, Sawai A, Scaltriti M,
Rodrik-Outmezguine V, Grbovic-Huezo O, Serra V, Majumder PK,
Baselga J and Rosen N: AKT inhibition relieves feedback suppression
of receptor tyrosine kinase expression and activity. Cancer Cell.
19:58–71. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Bellmunt J, Maroto P, Bonfill T, Vazquez
F, Perez-Gracia JL, Juanpere N, Hernandez-Prat A, Hernandez-Llodra
S, Rovira A, Juan O and Rodriguez-Vida A: Dual mTOR1/2 inhibitor
sapanisertib (FTH-003/TAK-228) in combination with weekly
paclitaxel in patients with previously treated metastatic
urothelial carcinoma: A phase II open-label study: A phase II
open-label study. Clin Genitourin Cancer. 22:1021232024. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Al-Bustany HA, Muhammad HA, Chawsheen MA
and Dash PR: Fenretinide induces apoptosis and synergises the
apoptosis inducing effect of gemcitabine through inhibition of key
signalling molecules involved in A549 cell survival in in silico
and in vitro analyses. Cell Signal. 111:1108852023. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Curless BP, Uko NE and Matesic DF:
Modulator of the PI3K/Akt oncogenic pathway affects mTOR complex 2
in human adenocarcinoma cells. Invest New Drugs. 37:902–911. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Fang W, Huang Y, Gu W, Gan J, Wang W,
Zhang S, Wang K, Zhan J, Yang Y, Huang Y, et al: PI3K-AKT-mTOR
pathway alterations in advanced NSCLC patients after progression on
EGFR-TKI and clinical response to EGFR-TKI plus everolimus
combination therapy. Transl Lung Cancer Res. 9:1258–1267. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Pal I and Mandal M: PI3K and Akt as
molecular targets for cancer therapy: Current clinical outcomes.
Acta Pharmacol Sin. 33:1441–1458. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Xu Y, Hu Y, Xu T, Yan K, Zhang T, Li Q,
Chang F, Guo X, Peng J, Li M, et al: RNF8-mediated regulation of
Akt promotes lung cancer cell survival and resistance to DNA
damage. Cell Rep. 37:1098542021. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
He YM, Zhou XM, Jiang SY, Zhang ZB, Cao
BY, Liu JB, Zeng YY, Zhao J and Mao XL: TRIM25 activates AKT/mTOR
by inhibiting PTEN via K63-linked polyubiquitination in non-small
cell lung cancer. Acta Pharmacol Sin. 43:681–691. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Alharbi KS, Shaikh MAJ, Almalki WH, Kazmi
I, Al-Abbasi FA, Alzarea SI, Imam SS, Alshehri S, Ghoneim MM, Singh
SK, et al: PI3K/Akt/mTOR pathways inhibitors with potential
prospects in non-small-cell lung cancer. J Environ Pathol Toxicol
Oncol. 41:85–102. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Yan D, Huelse JM, Kireev D, Tan Z, Chen L,
Goyal S, Wang X, Frye SV, Behera M, Schneider F, et al: MERTK
activation drives osimertinib resistance in EGFR-mutant non-small
cell lung cancer. J Clin Invest. 132:e1505172022. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Coco S, Truini A, Alama A, Dal Bello MG,
Venè R, Garuti A, Carminati E, Rijavec E, Genova C, Barletta G, et
al: Afatinib resistance in non-small cell lung cancer involves the
PI3K/AKT and MAPK/ERK signalling pathways and
epithelial-to-mesenchymal transition. Target Oncol. 10:393–404.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Adachi Y, Watanabe K, Kita K, Kitai H,
Kotani H, Sato Y, Inase N, Yano S and Ebi H: Resistance mediated by
alternative receptor tyrosine kinases in FGFR1-amplified lung
cancer. Carcinogenesis. 38:1063–1072. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Yu Y, Shang Y, Shi S, He Y, Shi W, Wang M,
Wang Q, Xu D, Shi C and Chen H: Combination of arsenic trioxide and
apatinib synergistically inhibits small cell lung cancer by
down-regulating VEGFR2/mTOR and Akt/c-Myc signaling pathway via
GRB10. Hereditas. 161:292024. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Wu YY, Wu HC, Wu JE, Huang KY, Yang SC,
Chen SX, Tsao CJ, Hsu KF, Chen YL and Hong TM: The dual PI3K/mTOR
inhibitor BEZ235 restricts the growth of lung cancer tumors
regardless of EGFR status, as a potent accompanist in combined
therapeutic regimens. J Exp Clin Cancer Res. 38:2822019. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Zhang J, Hong Y and Shen J: Combination
treatment with perifosine and MEK-162 demonstrates synergism
against lung cancer cells in vitro and in vivo. Tumour Biol.
36:5699–5706. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Quan Z, Yang Y, Zheng H, Zhan Y, Luo J,
Ning Y and Fan S: Clinical implications of the interaction between
PD-1/PD-L1 and PI3K/AKT/mTOR pathway in progression and treatment
of non-small cell lung cancer. J Cancer. 13:3434–3443. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Wu J, Zhao X, Sun Q, Jiang Y, Zhang W, Luo
J and Li Y: Synergic effect of PD-1 blockade and endostar on the
PI3K/AKT/mTOR-mediated autophagy and angiogenesis in Lewis lung
carcinoma mouse model. Biomed Pharmacother. 125:1097462020.
View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Liu Q, Chen X, Qi M, Li Y, Chen W and
Zhang C, Wang J, Han Z and Zhang C: Combined cryoablation and PD-1
inhibitor synergistically enhance antitumor immune responses in
Lewis lung adenocarcinoma mice via the PI3K/AKT/mTOR pathway.
Biochim Biophys Acta Mol Basis Dis. 1870:1672622024. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Shi Z, Shen Y, Liu X and Zhang S:
Sinensetin inhibits the movement ability and tumor immune
microenvironment of non-small cell lung cancer through the
inactivation of AKT/β-catenin axis. J Biochem Mol Toxicol.
38:e700242024. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Santini FC and Hellmann MD: PD-1/PD-L1
axis in lung cancer. Cancer J. 24:15–19. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Kumar R, Collins D, Dolly S, McDonald F,
O'Brien MER and Yap TA: Targeting the PD-1/PD-L1 axis in non-small
cell lung cancer. Curr Probl Cancer. 41:111–124. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Yadav R, Khatkar R, Yap KCH, Kang CYH, Lyu
J, Singh RK, Mandal S, Mohanta A, Lam HY, Okina E, et al: The miRNA
and PD-1/PD-L1 signaling axis: An arsenal of immunotherapeutic
targets against lung cancer. Cell Death Discov. 10:4142024.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Lu M, Wang K, Ji W, Yu Y, Li Z, Xia W and
Lu S: FGFR1 promotes tumor immune evasion via YAP-mediated PD-L1
expression upregulation in lung squamous cell carcinoma. Cell
Immunol. 379:1045772022. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Qiao M, Jiang T, Liu X, Mao S, Zhou F, Li
X, Zhao C, Chen X, Su C, Ren S and Zhou C: Immune checkpoint
inhibitors in EGFR-mutated NSCLC: Dusk or dawn? J Thorac Oncol.
16:1267–1288. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Genova C, Dellepiane C, Carrega P,
Sommariva S, Ferlazzo G, Pronzato P, Gangemi R, Filaci G, Coco S
and Croce M: Therapeutic implications of tumor microenvironment in
lung cancer: Focus on immune checkpoint blockade. Front Immunol.
12:7994552022. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Sholl LM: Biomarkers of response to
checkpoint inhibitors beyond PD-L1 in lung cancer. Mod Pathol. 35
(Suppl 1):S66–S74. 2022. View Article : Google Scholar
|
|
131
|
Reck M, Rodríguez-Abreu D, Robinson AG,
Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe
S, et al: Updated analysis of KEYNOTE-024: Pembrolizumab versus
platinum-based chemotherapy for advanced non-small-cell lung cancer
with PD-L1 tumor proportion score of 50% or greater. J Clin Oncol.
37:537–546. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Ready NE, Ott PA, Hellmann MD,
Zugazagoitia J, Hann CL, de Braud F, Antonia SJ, Ascierto PA,
Moreno V, Atmaca A, et al: Nivolumab monotherapy and nivolumab plus
ipilimumab in recurrent small cell lung cancer: Results from the
checkmate 032 randomized cohort. J Thorac Oncol. 15:426–435. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Liu SV, Reck M, Mansfield AS, Mok T,
Scherpereel A, Reinmuth N, Garassino MC, De Castro Carpeno J,
Califano R, Nishio M, et al: Updated overall survival and PD-L1
subgroup analysis of patients with extensive-stage small-cell lung
cancer treated with atezolizumab, carboplatin, and etoposide
(IMpower133). J Clin Oncol. 39:619–630. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Tang S, Qin C, Hu H, Liu T, He Y, Guo H,
Yan H, Zhang J, Tang S and Zhou H: Immune checkpoint inhibitors in
non-small cell lung cancer: Progress, challenges, and prospects.
Cells. 11:3202022. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Passaro A, Brahmer J, Antonia S, Mok T and
Peters S: Managing resistance to immune checkpoint inhibitors in
lung cancer: Treatment and novel strategies. J Clin Oncol.
40:598–610. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Kejamurthy P and Devi KTR: Immune
checkpoint inhibitors and cancer immunotherapy by aptamers: An
overview. Med Oncol. 41:402023. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Li Y, Jiang M, Aye L, Luo L, Zhang Y, Xu
F, Wei Y, Peng D, He X, Gu J, et al: UPP1 promotes lung
adenocarcinoma progression through the induction of an
immunosuppressive microenvironment. Nat Commun. 15:12002024.
View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Ghorani E, Swanton C and Quezada SA:
Cancer cell-intrinsic mechanisms driving acquired immune tolerance.
Immunity. 56:2270–2295. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Giatromanolaki A, Kouroupi M, Pouliliou S,
Mitrakas A, Hasan F, Pappa A and Koukourakis MI: Ectonucleotidase
CD73 and CD39 expression in non-small cell lung cancer relates to
hypoxia and immunosuppressive pathways. Life Sci. 259:1183892020.
View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Best SA, Gubser PM, Sethumadhavan S,
Kersbergen A, Negrón Abril YL, Goldford J, Sellers K, Abeysekera W,
Garnham AL, McDonald JA, et al: Glutaminase inhibition impairs CD8
T cell activation in STK11-/Lkb1-deficient lung cancer. Cell Metab.
34:874–887.e6. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Zhu M, Kim J, Deng Q, Ricciuti B, Alessi
JV, Eglenen-Polat B, Bender ME, Huang HC, Kowash RR, Cuevas I, et
al: Loss of p53 and mutational heterogeneity drives immune
resistance in an autochthonous mouse lung cancer model with high
tumor mutational burden. Cancer Cell. 41:1731–1748.e8. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Zhu C, Zhuang W, Chen L, Yang W and Ou WB:
Frontiers of ctDNA, targeted therapies, and immunotherapy in
non-small-cell lung cancer. Transl Lung Cancer Res. 9:111–138.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Chu X, Tian W, Wang Z, Zhang J and Zhou R:
Co-inhibition of TIGIT and PD-1/PD-L1 in cancer immunotherapy:
Mechanisms and clinical trials. Mol Cancer. 22:932023. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Chen Y, Chen Z, Chen R, Fang C, Zhang C,
Ji M and Yang X: Immunotherapy-based combination strategies for
treatment of EGFR-TKI-resistant non-small-cell lung cancer. Future
Oncol. 18:1757–1775. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
West HJ, McCleland M, Cappuzzo F, Reck M,
Mok TS, Jotte RM, Nishio M, Kim E, Morris S, Zou W, et al: Clinical
efficacy of atezolizumab plus bevacizumab and chemotherapy in
KRAS-mutated non-small cell lung cancer with STK11, KEAP1, or TP53
comutations: Subgroup results from the phase III IMpower150 trial.
J Immunother Cancer. 10:e0030272022. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Judd J and Borghaei H: Combining
immunotherapy and chemotherapy for non-small cell lung cancer.
Thorac Surg Clin. 30:199–206. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Shang S, Liu J, Verma V, Wu M, Welsh J, Yu
J and Chen D: Combined treatment of non-small cell lung cancer
using radiotherapy and immunotherapy: Challenges and updates.
Cancer Commun (Lond). 41:1086–1099. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Chae YK, Arya A, Iams W, Cruz M, Mohindra
N, Villaflor V and Giles FJ: Immune checkpoint pathways in
non-small cell lung cancer. Ann Transl Med. 6:882018. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Raghav KPS and Moasser MM: Molecular
pathways and mechanisms of HER2 in cancer therapy. Clin Cancer Res.
29:2351–2361. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Nützinger J, Bum Lee J, Li Low J, Ling
Chia P, Talisa Wijaya S, Chul Cho B, Min Lim S and Soo RA:
Management of HER2 alterations in non-small cell lung cancer-the
past, present, and future. Lung Cancer. 186:1073852023. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Riudavets M, Sullivan I, Abdayem P and
Planchard D: Targeting HER2 in non-small-cell lung cancer (NSCLC):
A glimpse of hope? An updated review on therapeutic strategies in
NSCLC harbouring HER2 alterations. ESMO Open. 6:1002602021.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Ghezzi C, Chen BY, Damoiseaux R and Clark
PM: Pacritinib inhibits glucose consumption in squamous cell lung
cancer cells by targeting. FLT3.Sci Rep. 13:14422023. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Kuncman Ł, Orzechowska M, Milecki T,
Kucharz J and Fijuth J: High FLT3 expression increases immune-cell
infiltration in the tumor microenvironment and correlates with
prolonged disease-free survival in patients with non-small cell
lung cancer. Mol Oncol. 18:1316–1326. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Dhillon S: Gilteritinib: First global
approval. Drugs. 79:331–339. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Hu C, Zhang Y, Yang J, Xu Y, Deng T, Li Y,
Xu S, Wang S and Wang P: Ningetinib, a novel FLT3 inhibitor,
overcomes secondary drug resistance in acute myeloid leukemia. Cell
Commun Signal. 22:3552024. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Bruner JK, Ma HS, Li L, Qin ACR, Rudek MA,
Jones RJ, Levis MJ, Pratz KW, Pratilas CA and Small D: Adaptation
to TKI treatment reactivates ERK signaling in tyrosine
kinase-driven leukemias and other malignancies. Cancer Res.
77:5554–5563. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
He L, Wang X, Liu K, Wu X, Yang X, Song G,
Zhang B and Zhong L: Integrative PDGF/PDGFR and focal adhesion
pathways are downregulated in ERCC1-defective non-small cell lung
cancer undergoing sodium glycididazole-sensitized cisplatin
treatment. Gene. 691:70–76. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Catena R, Luis-Ravelo D, Antón I, Zandueta
C, Salazar-Colocho P, Larzábal L, Calvo A and Lecanda F: PDGFR
signaling blockade in marrow stroma impairs lung cancer bone
metastasis. Cancer Res. 71:164–174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Riess JW and Neal JW: Targeting FGFR,
ephrins, Mer, MET, and PDGFR-α in non-small cell lung cancer. J
Thorac Oncol. 6 (11 Suppl 4):S1797–S1798. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Kranthi Reddy S, Reddy SVG and Hussain
Basha S: Discovery of novel PDGFR inhibitors targeting non-small
cell lung cancer using a multistep machine learning assisted hybrid
virtual screening approach. RSC Adv. 15:851–869. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Xuan H, Jingshu G, Fang Y, Na L, Xiaolin
S, Zhaoyang Y, Meng W and Gongyan C: Somatic mutation of KIT is
rare in small cell lung cancer patients from Northeast China.
Histol Histopathol. 29:273–278. 2014.PubMed/NCBI
|
|
162
|
Miettinen M and Lasota J: KIT (CD117): A
review on expression in normal and neoplastic tissues, and
mutations and their clinicopathologic correlation. Appl
Immunohistochem Mol Morphol. 13:205–220. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Funkhouser AT, Strigenz AM, Blair BB,
Miller AP, Shealy JC, Ewing JA, Martin JC, Funk CR, Edenfield WJ
and Blenda AV: KIT mutations correlate with higher galectin levels
and brain metastasis in breast and non-small cell lung cancer.
Cancers (Basel). 14:27812022. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Yang L, Zhou F, Zheng D, Wang D, Li X,
Zhao C and Huang X: FGF/FGFR signaling: From lung development to
respiratory diseases. Cytokine Growth Factor Rev. 62:94–104. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Pacini L, Jenks AD, Lima NC and Huang PH:
Targeting the fibroblast growth factor receptor (FGFR) family in
lung cancer. Cells. 10:11542021. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Desai A and Adjei AA: FGFR signaling as a
target for lung cancer therapy. J Thorac Oncol. 11:9–20. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Peng M, Deng J and Li X: Clinical advances
and challenges in targeting FGF/FGFR signaling in lung cancer. Mol
Cancer. 23:2562024. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Biello F, Burrafato G, Rijavec E, Genova
C, Barletta G, Truini A, Coco S, Bello MG, Alama A, Boccardo F and
Grossi F: Fibroblast growth factor receptor (FGFR): A new target
for non-small cell lung cancer therapy. Anticancer Agents Med Chem.
16:1142–1154. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Cervantes-Villagrana RD, Mendoza V, Hinck
CS, de la Fuente-León RL, Hinck AP, Reyes-Cruz G, Vázquez-Prado J
and López-Casillas F: Betaglycan sustains HGF/Met signaling in lung
cancer and endothelial cells promoting cell migration and tumor
growth. Heliyon. 10:e305202024. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Huang G, Liu X, Jiang T, Cao Y, Sang M,
Song X, Zhou B, Qu H, Cai H, Xing D, et al: Luteolin overcomes
acquired resistance to osimertinib in non-small cell lung cancer
cells by targeting the HGF-MET-Akt pathway. Am J Cancer Res.
13:4145–4162. 2023.PubMed/NCBI
|
|
171
|
Moosavi F, Giovannetti E, Peters GJ and
Firuzi O: Combination of HGF/MET-targeting agents and other
therapeutic strategies in cancer. Crit Rev Oncol Hematol.
160:1032342021. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Yin J, Hu W, Fu W, Dai L, Jiang Z, Zhong
S, Deng B and Zhao J: HGF/MET regulated epithelial-mesenchymal
transitions and metastasis by FOSL2 in non-small cell lung cancer.
Onco Targets Ther. 12:9227–9237. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Fregni M, Ciribilli Y and Zawacka-Pankau
JE: The therapeutic potential of the restoration of the p53 protein
family members in the EGFR-mutated lung cancer. Int J Mol Sci.
23:72132022. View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Lin CC, Liao WT, Yang TY, Lu HJ, Hsu SL
and Wu CC: MicroRNA-10b modulates cisplatin tolerance by targeting
p53 directly in lung cancer cells. Oncol Rep. 46:1672021.
View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Zhang H, Zhang G, Xiao M, Cui S, Jin C,
Yang J, Wu S and Lu X: Two-polarized roles of transcription factor
FOSB in lung cancer progression and prognosis: Dependent on p53
status. J Exp Clin Cancer Res. 43:2372024. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Chantarawong W, Kuncharoen N, Tanasupawat
S and Chanvorachote P: Lumichrome inhibits human lung cancer cell
growth and induces apoptosis via a p53-dependent mechanism. Nutr
Cancer. 71:1390–1402. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Li L, Li P, Ma X, Zeng S, Peng Y and Zhang
G: Therapeutic restoring p53 function with small molecule for
oncogene-driven non-small cell lung cancer by targeting serine 392
phosphorylation. Biochem Pharmacol. 203:1151882022. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Wang J, Liu D, Sun Z, Ye T, Li J, Zeng B,
Zhao Q and Rosie Xing H: Autophagy augments the self-renewal of
lung cancer stem cells by the degradation of ubiquitinated p53.
Cell Death Dis. 12:982021. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Tang X, Li Y, Liu L, Guo R, Zhang P, Zhang
Y, Zhang Y, Zhao J, Su J, Sun L and Liu Y: Sirtuin 3 induces
apoptosis and necroptosis by regulating mutant p53 expression in
small-cell lung cancer. Oncol Rep. 43:591–600. 2020.PubMed/NCBI
|
|
180
|
Krishnamurthy N and Kurzrock R: Targeting
the Wnt/beta-catenin pathway in cancer: Update on effectors and
inhibitors. Cancer Treat Rev. 62:50–60. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
He Y, Jiang X, Duan L, Xiong Q, Yuan Y,
Liu P, Jiang L, Shen Q, Zhao S, Yang C and Chen Y: LncRNA PKMYT1AR
promotes cancer stem cell maintenance in non-small cell lung cancer
via activating Wnt signaling pathway. Mol Cancer. 20:1562021.
View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Li HJ, Ke FY, Lin CC, Lu MY, Kuo YH, Wang
YP, Liang KH, Lin SC, Chang YH, Chen HY, et al: ENO1 promotes lung
cancer metastasis via HGFR and WNT signaling-driven
epithelial-to-mesenchymal transition. Cancer Res. 81:4094–4109.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Li Z, Wu S and Liu W: Advances of
Wnt/β-catenin signaling pathway in lung cancer: A review. Altern
Ther Health Med. 30:238–247. 2024.
|
|
184
|
Chen J, Wang D, Chen H, Gu J, Jiang X, Han
F, Cao J, Liu W and Liu J: TMEM196 inhibits lung cancer metastasis
by regulating the Wnt/β-catenin signaling pathway. J Cancer Res
Clin Oncol. 149:653–667. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Shen Y, Yang Y, Zhao Y, Nuerlan S, Zhan Y
and Liu C: YY1/circCTNNB1/miR-186-5p/YY1 positive loop aggravates
lung cancer progression through the Wnt pathway. Epigenetics.
19:23690062024. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Malyla V, Paudel KR, De Rubis G, Hansbro
NG, Hansbro PM and Dua K: Cigarette smoking induces lung cancer
tumorigenesis via upregulation of the WNT/β-catenin signaling
pathway. Life Sci. 326:1217872023. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Yang J, Chen J, He J, Li J, Shi J, Cho WC
and Liu X: Wnt signaling as potential therapeutic target in lung
cancer. Expert Opin Ther Targets. 20:999–1015. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Zhang Y and Wang X: Targeting the
Wnt/β-catenin signaling pathway in cancer. J Hematol Oncol.
13:1652020. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Bugter JM, Fenderico N and Maurice MM:
Mutations and mechanisms of WNT pathway tumour suppressors in
cancer. Nat Rev Cancer. 21:5–21. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Neiheisel A, Kaur M, Ma N, Havard P and
Shenoy AK: Wnt pathway modulators in cancer therapeutics: An update
on completed and ongoing clinical trials. Int J Cancer.
150:727–740. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Song P, Gao Z, Bao Y, Chen L, Huang Y, Liu
Y, Dong Q and Wei X: Wnt/β-catenin signaling pathway in
carcinogenesis and cancer therapy. J Hematol Oncol. 17:462024.
View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Xue C, Yao Q, Gu X, Shi Q, Yuan X, Chu Q,
Bao Z, Lu J and Li L: Evolving cognition of the JAK-STAT signaling
pathway: Autoimmune disorders and cancer. Signal Transduct Target
Ther. 8:2042023. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Hu X, Li J, Fu M, Zhao X and Wang W: The
JAK/STAT signaling pathway: From bench to clinic. Signal Transduct
Target Ther. 6:4022021. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Erdogan F, Radu TB, Orlova A, Qadree AK,
de Araujo ED, Israelian J, Valent P, Mustjoki SM, Herling M,
Moriggl R and Gunning PT: JAK-STAT core cancer pathway: An
integrative cancer interactome analysis. J Cell Mol Med.
26:2049–2062. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Shen M, Xu Z, Xu W, Jiang K, Zhang F, Ding
Q, Xu Z and Chen Y: Inhibition of ATM reverses EMT and decreases
metastatic potential of cisplatin-resistant lung cancer cells
through JAK/STAT3/PD-L1 pathway. J Exp Clin Cancer Res. 38:1492019.
View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Wu Q, Wu W, Fu B, Shi L, Wang X and Kuca
K: JNK signaling in cancer cell survival. Med Res Rev.
39:2082–2104. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Patel MR, Dash A, Jacobson BA, Ji Y,
Baumann D, Ismail K and Kratzke RA: JAK/STAT inhibition with
ruxolitinib enhances oncolytic virotherapy in non-small cell lung
cancer models. Cancer Gene Ther. 26:411–418. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Ding Y, Yuan X, Wang Y and Yan J: CASQ2
alleviates lung cancer by inhibiting M2 tumor-associated macrophage
polarization and JAK/STAT pathway. J Biochem Mol Toxicol.
38:e238012024. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Saito A, Horie M and Nagase T: TGF-β
signaling in lung health and disease. Int J Mol Sci. 19:24602018.
View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Kim BN, Ahn DH, Kang N, Yeo CD, Kim YK,
Lee KY, Kim TJ, Lee SH, Park MS, Yim HW, et al: TGF-β induced EMT
and stemness characteristics are associated with epigenetic
regulation in lung cancer. Sci Rep. 10:105972020. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Huang Y, Chen Z, Lu T, Bi G, Li M, Liang
J, Hu Z, Zheng Y, Yin J, Xi J, et al: HIF-1α switches the
functionality of TGF-β signaling via changing the partners of smads
to drive glucose metabolic reprogramming in non-small cell lung
cancer. J Exp Clin Cancer Res. 40:3982021. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Deng X, Ma N, He J, Xu F and Zou G: The
role of TGFBR3 in the development of lung cancer. Protein Pept
Lett. 31:491–503. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Li J, Shen C, Wang X, Lai Y, Zhou K, Li P,
Liu L and Che G: Prognostic value of TGF-beta in lung cancer:
Systematic review and meta-analysis. BMC Cancer. 19:6912019.
View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Lai XN, Li J, Tang LB, Chen WT, Zhang L
and Xiong LX: MiRNAs and LncRNAs: Dual roles in TGF-β
signaling-regulated metastasis in lung cancer. Int J Mol Sci.
21:11932020. View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Cui Z, Ruan Z, Li M, Ren R, Ma Y, Zeng J,
Sun J, Ye W, Xu W, Guo X, et al: Obstructive sleep apnea promotes
the progression of lung cancer by modulating cancer cell invasion
and cancer-associated fibroblast activation via TGFβ signaling.
Redox Rep. 28:22798132023. View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Hedrick E, Mohankumar K and Safe S:
TGFβ-induced lung cancer cell migration is NR4A1-dependent. Mol
Cancer Res. 16:1991–2002. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Saito A, Horie M, Micke P and Nagase T:
The role of TGF-β signaling in lung cancer associated with
idiopathic pulmonary fibrosis. Int J Mol Sci. 19:36112018.
View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Yin Y, Dai H, Sun X, Xi Z, Zhang J, Pan Y,
Huang Y, Ma X, Xia Q and He K: HRG inhibits liver cancer lung
metastasis by suppressing neutrophil extracellular trap formation.
Clin Transl Med. 13:e12832023. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Liu W, Wang H, Bai F, Ding L, Huang Y, Lu
C, Chen S, Li C, Yue X, Liang X, et al: IL-6 promotes metastasis of
non-small-cell lung cancer by up-regulating TIM-4 via NF-κB. Cell
Prolif. 53:e127762020. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Wang Y, Liu F, Chen L, Fang C, Li S, Yuan
S, Qian X, Yin Y, Yu B, Fu B, et al: Neutrophil extracellular traps
(NETs) promote non-small cell lung cancer metastasis by suppressing
lncRNA MIR503HG to activate the NF-κB/NLRP3 inflammasome pathway.
Front Immunol. 13:8675162022. View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Zhang J, Zhao K, Zhou W, Kang R, Wei S,
Shu Y, Yu C, Ku Y, Mao Y, Luo H, et al: Tet methylcytosine
dioxygenase 2 (TET2) deficiency elicits EGFR-TKI (tyrosine kinase
inhibitors) resistance in non-small cell lung cancer. Signal
Transduct Target Ther. 9:652024. View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Rasmi RR, Sakthivel KM and Guruvayoorappan
C: NF-κB inhibitors in treatment and prevention of lung cancer.
Biomed Pharmacother. 130:1105692020. View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Liu X, Liu X, Zhuo C, Shen J, Lu K, Sha M,
Ye J, Huang J, Han H and Yu H: NAT10 promotes malignant progression
of lung cancer via the NF-κB signaling pathway. Discov Med.
35:936–945. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
214
|
Wei X, Liu Z, Shen Y, Dong H, Chen K, Shi
X, Chen Y, Wang B and Dong S: Semaphorin4A promotes lung cancer by
activation of NF-κB pathway mediated by PlexinB1. PeerJ.
11:e162922023. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Dimitrakopoulos FD, Kottorou AE, Kalofonou
M and Kalofonos HP: The fire within: NF-κB involvement in non-small
cell lung cancer. Cancer Res. 80:4025–4036. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
216
|
Li Y, Zu L, Wu H, Zhang F, Fan Y, Pan H,
Du X, Guo F and Zhou Q: MiR-192/NKRF axis confers lung cancer cell
chemoresistance to cisplatin via the NF-κB pathway. Thorac Cancer.
13:430–441. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Jin Y, Zhang Y, Huang A, Chen Y, Wang J,
Liu N, Wang X, Gong Y, Wang W and Pan J: Overexpression of SERPINA3
suppresses tumor progression by modulating SPOP/NF-κB in lung
cancer. Int J Oncol. 63:962023. View Article : Google Scholar : PubMed/NCBI
|
|
218
|
Wang Y, Zhang J, Li YJ, Yu NN, Liu WT,
Liang JZ, Xu WW, Sun ZH, Li B and He QY: MEST promotes lung cancer
invasion and metastasis by interacting with VCP to activate NF-κB
signaling. J Exp Clin Cancer Res. 40:3012021. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Xu X, Qiu Y, Chen S, Wang S, Yang R, Liu
B, Li Y, Deng J, Su Y, Lin Z, et al: Different roles of the
insulin-like growth factor (IGF) axis in non-small cell lung
cancer. Curr Pharm Des. 28:2052–2064. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Remsing Rix LL, Sumi NJ, Hu Q, Desai B,
Bryant AT, Li X, Welsh EA, Fang B, Kinose F, Kuenzi BM, et al:
IGF-binding proteins secreted by cancer-associated fibroblasts
induce context-dependent drug sensitization of lung cancer cells.
Sci Signal. 15:eabj58792022. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Jiang S, Xu Z, Shi Y, Liang S, Jiang X,
Xiao M, Wang K and Ding L: Circulating insulin-like growth factor-1
and risk of lung diseases: A Mendelian randomization analysis.
Front Endocrinol (Lausanne). 14:11263972023. View Article : Google Scholar : PubMed/NCBI
|
|
222
|
Xu J, Bie F, Wang Y, Chen X, Yan T and Du
J: Prognostic value of IGF-1R in lung cancer: A PRISMA-compliant
meta-analysis. Medicine (Baltimore). 98:e154672019. View Article : Google Scholar : PubMed/NCBI
|
|
223
|
Wang Z, Li W, Guo Q, Wang Y, Ma L and
Zhang X: Insulin-like growth factor-1 signaling in lung development
and inflammatory lung diseases. Biomed Res Int.
2018:60575892018.PubMed/NCBI
|
|
224
|
Peng Y and Tan J: The relationship between
IGF pathway and acquired resistance to tyrosine kinase inhibitors
in cancer therapy. Front Biosci (Landmark Ed). 28:1632023.
View Article : Google Scholar : PubMed/NCBI
|
|
225
|
Pal S, Yadav P, Sainis KB and Shankar BS:
TNF-α and IGF-1 differentially modulate ionizing radiation
responses of lung cancer cell lines. Cytokine. 101:89–98. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
226
|
Sun L, Yuan W, Wen G, Yu B, Xu F, Gan X,
Tang J, Zeng Q, Zhu L, Chen C and Zhang W: Parthenolide inhibits
human lung cancer cell growth by modulating the IGF-1R/PI3K/Akt
signaling pathway. Oncol Rep. 44:1184–1193. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
227
|
Das D, Xie L and Hong J: Next-generation
EGFR tyrosine kinase inhibitors to overcome C797S mutation in
non-small cell lung cancer (2019–2024). RSC Med Chem. 15:3371–3394.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
228
|
Das D, Wang J and Hong J: Next-generation
kinase inhibitors targeting specific biomarkers in non-small cell
lung cancer (NSCLC): A recent overview. ChemMedChem. 16:2459–2479.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
229
|
Wang N, Zhang Y, Mi Y, Deng H, Chen G,
Tang Z, Mao J, Cui S, Zhang Y and Wang L: Osimertinib for
EGFR-mutant lung cancer with central nervous system metastases: A
meta-analysis and systematic review. Ann Palliat Med. 9:3038–3047.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
230
|
Solomon BJ, Besse B, Bauer TM, Felip E,
Soo RA, Camidge DR, Chiari R, Bearz A, Lin CC, Gadgeel SM, et al:
Lorlatinib in patients with ALK-positive non-small-cell lung
cancer: Results from a global phase 2 study. Lancet Oncol.
19:1654–1667. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
231
|
Soejima K, Yasuda H and Hirano T:
Osimertinib for EGFR T790M mutation-positive non-small cell lung
cancer. Expert Rev Clin Pharmacol. 10:31–38. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
232
|
Yang JCH, Ahn MJ, Kim DW, Ramalingam SS,
Sequist LV, Su WC, Kim SW, Kim JH, Planchard D, Felip E, et al:
Osimertinib in pretreated T790M-positive advanced non-small-cell
lung cancer: AURA study phase II extension component. J Clin Oncol.
35:1288–1296. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
233
|
Ramalingam SS, Yang JCH, Lee CK, Kurata T,
Kim DW, John T, Nogami N, Ohe Y, Mann H, Rukazenkov Y, et al:
Osimertinib as first-line treatment of EGFR mutation-positive
advanced non-small-cell lung cancer. J Clin Oncol. 36:841–849.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
234
|
Araki T, Kanda S, Horinouchi H and Ohe Y:
Current treatment strategies for EGFR-mutated non-small cell lung
cancer: From first line to beyond osimertinib resistance. Jpn J
Clin Oncol. 53:547–561. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
235
|
Jänne PA, Planchard D, Kobayashi K, Cheng
Y, Lee CK, Valdiviezo N, Laktionov K, Yang TY, Yu Y, Kato T, et al:
CNS efficacy of osimertinib with or without chemotherapy in
epidermal growth factor receptor-mutated advanced non-small-cell
lung cancer. J Clin Oncol. 42:808–820. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
236
|
Ye Z and Guo J: Acquired ALK G1202R-, ALK
I1171N-, or EML4-ALK-mediated resistance to ensartinib in lung
adenocarcinoma but responded to lorlatinib: A case report. Front
Oncol. 13:10821152023. View Article : Google Scholar : PubMed/NCBI
|
|
237
|
Solomon BJ, Bauer TM, Mok TSK, Liu G,
Mazieres J, de Marinis F, Goto Y, Kim DW, Wu YL, Jassem J, et al:
Efficacy and safety of first-line lorlatinib versus crizotinib in
patients with advanced, ALK-positive non-small-cell lung cancer:
Updated analysis of data from the phase 3, randomised, open-label
CROWN study. Lancet Respir Med. 11:354–366. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
238
|
Bauer TM, Shaw AT, Johnson ML, Navarro A,
Gainor JF, Thurm H, Pithavala YK, Abbattista A, Peltz G and Felip
E: Brain penetration of lorlatinib: cumulative incidences of CNS
and non-CNS progression with lorlatinib in patients with previously
treated ALK-positive non-small-cell lung cancer. Target Oncol.
15:55–65. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
239
|
Rybarczyk-Kasiuchnicz A, Ramlau R and
Stencel K: Treatment of brain metastases of non-small cell lung
carcinoma. Int J Mol Sci. 22:5932021. View Article : Google Scholar : PubMed/NCBI
|
|
240
|
Ernani V and Stinchcombe TE: Management of
brain metastases in non-small-cell lung cancer. J Oncol Pract.
15:563–570. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
241
|
Lin JJ, Choudhury NJ, Yoda S, Zhu VW,
Johnson TW, Sakhtemani R, Dagogo-Jack I, Digumarthy SR, Lee C, Do
A, et al: Spectrum of mechanisms of resistance to crizotinib and
lorlatinib in ROS1 fusion-positive lung cancer. Clin Cancer Res.
27:2899–2909. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
242
|
Corvaja C, Passaro A, Attili I, Aliaga PT,
Spitaleri G, Signore ED and de Marinis F: Advancements in
fourth-generation EGFR TKIs in EGFR-mutant NSCLC: Bridging
biological insights and therapeutic development. Cancer Treat Rev.
130:1028242024. View Article : Google Scholar : PubMed/NCBI
|
|
243
|
Desai A and Peters S: Immunotherapy-based
combinations in metastatic NSCLC. Cancer Treat Rev. 116:1025452023.
View Article : Google Scholar : PubMed/NCBI
|
|
244
|
Passaro A, Jänne PA and Peters S:
Antibody-drug conjugates in lung cancer: Recent advances and
implementing strategies. J Clin Oncol. 41:3747–3761. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
245
|
Desai A, Abdayem P, Adjei AA and Planchard
D: Antibody-drug conjugates: A promising novel therapeutic approach
in lung cancer. Lung Cancer. 163:96–106. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
246
|
Merle G, Friedlaender A, Desai A and Addeo
A: Antibody drug conjugates in lung cancer. Cancer J. 28:429–435.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
247
|
Rosner S, Valdivia A, Hoe HJ, Murray JC,
Levy B, Felip E and Solomon BJ: Antibody-drug conjugates for lung
cancer: Payloads and progress. Am Soc Clin Oncol Educ Book.
43:e3899682023. View Article : Google Scholar : PubMed/NCBI
|
|
248
|
Marks S and Naidoo J: Antibody drug
conjugates in non-small cell lung cancer: An emerging therapeutic
approach. Lung Cancer. 163:59–68. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
249
|
Tarantino P, Carmagnani Pestana R, Corti
C, Modi S, Bardia A, Tolaney SM, Cortes J, Soria JC and Curigliano
G: Antibody-drug conjugates: Smart chemotherapy delivery across
tumor histologies. CA Cancer J Clin. 72:165–182. 2022.PubMed/NCBI
|
|
250
|
Weng W, Meng T, Zhao Q, Shen Y, Fu G, Shi
J, Zhang Y, Wang Z, Wang M, Pan R, et al: Antibody-exatecan
conjugates with a novel self-immolative moiety overcome resistance
in colon and lung cancer. Cancer Discov. 13:950–973. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
251
|
Verma S, Breadner D and Raphael J:
‘Targeting’ improved outcomes with antibody-drug conjugates in
non-small cell lung cancer-an updated review. Curr Oncol.
30:4329–4350. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
252
|
Parisi C, Mahjoubi L, Gazzah A and Barlesi
F: TROP-2 directed antibody-drug conjugates (ADCs): The revolution
of smart drug delivery in advanced non-small cell lung cancer
(NSCLC). Cancer Treat Rev. 118:1025722023. View Article : Google Scholar : PubMed/NCBI
|
|
253
|
Peters S, Loi S, André F, Chandarlapaty S,
Felip E, Finn SP, Jänne PA, Kerr KM, Munzone E, Passaro A, et al:
Antibody-drug conjugates in lung and breast cancer: Current
evidence and future directions-a position statement from the ETOP
IBCSG partners foundation. Ann Oncol. 35:607–629. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
254
|
Ricciuti B, Lamberti G, Andrini E, Genova
C, De Giglio A, Bianconi V, Sahebkar A, Chiari R and Pirro M:
Antibody-drug conjugates for lung cancer in the era of personalized
oncology. Semin Cancer Biol. 69:268–278. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
255
|
Pourjamal N, Yazdi N, Halme A, Joncour VL,
Laakkonen P, Saharinen P, Joensuu H and Barok M: Comparison of
trastuzumab emtansine, trastuzumab deruxtecan, and disitamab
vedotin in a multiresistant HER2-positive breast cancer lung
metastasis model. Clin Exp Metastasis. 41:91–102. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
256
|
Fu Z, Gao C, Xie J, Zhang C, Li S, Gu M
and Shi C: Incidence and risk of fatal adverse events in cancer
patients treated with HER2-targeted antibody-drug conjugates: A
systematic review and meta-analysis of randomized controlled
trials. BMC Cancer. 23:9602023. View Article : Google Scholar : PubMed/NCBI
|
|
257
|
Larsen ME, Lyu H and Liu B: HER3-targeted
therapeutic antibodies and antibody-drug conjugates in non-small
cell lung cancer refractory to EGFR-tyrosine kinase inhibitors.
Chin Med J Pulm Crit Care Med. 1:11–17. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
258
|
Chen Q, Jia G, Zhang X and Ma W: Targeting
HER3 to overcome EGFR TKI resistance in NSCLC. Front Immunol.
14:13320572024. View Article : Google Scholar : PubMed/NCBI
|
|
259
|
Belluomini L, Avancini A, Sposito M,
Milella M, Rossi A and Pilotto S: Antibody-drug conjugates (ADCs)
targeting TROP-2 in lung cancer. Expert Opin Biol Ther.
23:1077–1087. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
260
|
Paz-Ares LG, Juan-Vidal O, Mountzios GS,
Felip E, Reinmuth N, de Marinis F, Girard N, Patel VM, Takahama T,
Owen SP, et al: Sacituzumab govitecan versus docetaxel for
previously treated advanced or metastatic non-small cell lung
cancer: The randomized, open-label phase III EVOKE-01 study. J Clin
Oncol. 42:2860–2872. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
261
|
Kim YJ, Li W, Zhelev DV, Mellors JW,
Dimitrov DS and Baek DS: Chimeric antigen receptor-T cells are
effective against CEACAM5 expressing non-small cell lung cancer
cells resistant to antibody-drug conjugates. Front Oncol.
13:11240392023. View Article : Google Scholar : PubMed/NCBI
|
|
262
|
Zanchetta C, De Marchi L, Macerelli M,
Pelizzari G, Costa J, Aprile G and Cortiula F: Antibody-drug
conjugates in non-small cell lung cancer: state of the art and
future perspectives. Int J Mol Sci. 26:2212024. View Article : Google Scholar : PubMed/NCBI
|
|
263
|
Belluomini L, Sposito M, Avancini A,
Insolda J, Milella M, Rossi A and Pilotto S: Unlocking new horizons
in small-cell lung cancer treatment: The onset of antibody-drug
conjugates. Cancers (Basel). 15:53682023. View Article : Google Scholar : PubMed/NCBI
|
|
264
|
Blackhall F, Jao K, Greillier L, Cho BC,
Penkov K, Reguart N, Majem M, Nackaerts K, Syrigos K, Hansen K, et
al: Efficacy and safety of rovalpituzumab tesirine compared with
topotecan as second-line therapy in DLL3-high SCLC: Results from
the phase 3 TAHOE study. J Thorac Oncol. 16:1547–1558. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
265
|
Owen DH, Giffin MJ, Bailis JM, Smit MAD,
Carbone DP and He K: DLL3: An emerging target in small cell lung
cancer. J Hematol Oncol. 12:612019. View Article : Google Scholar : PubMed/NCBI
|
|
266
|
Morgensztern D, Besse B, Greillier L,
Santana-Davila R, Ready N, Hann CL, Glisson BS, Farago AF, Dowlati
A, Rudin CM, et al: Efficacy and safety of rovalpituzumab tesirine
in third-line and beyond patients with DLL3-expressing,
relapsed/refractory small-cell lung cancer: Results from the phase
II TRINITY study. Clin Cancer Res. 25:6958–6966. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
267
|
Lashari BH, Vallatharasu Y, Kolandra L,
Hamid M and Uprety D: Rovalpituzumab tesirine: A novel
DLL3-targeting antibody-drug conjugate. Drugs R D. 18:255–258.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
268
|
Zhao C, Zhang R, Yang H, Gao Y, Zou Y and
Zhang X: Antibody-drug conjugates for non-small cell lung cancer:
Advantages and challenges in clinical translation. Biochem
Pharmacol. 226:1163782024. View Article : Google Scholar : PubMed/NCBI
|
|
269
|
Neupane N, Thapa S, Bhattarai A, Ahuja K,
Schlam I, Mittal A, Tolaney SM and Tarantino P: Opportunities and
challenges for a histology-agnostic utilization of trastuzumab
deruxtecan. Curr Oncol Rep. 25:1467–1482. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
270
|
Desai A, Subbiah V, Roy-Chowdhuri S,
Sheshadri A, Deshmukh S and Peters S: Association of antibody-drug
conjugate (ADC) target expression and interstitial lung disease
(ILD) in non-small-cell lung cancer (NSCLC): Association or
causation or neither? Cancers (Basel). 16:37532024. View Article : Google Scholar : PubMed/NCBI
|
|
271
|
Attili I, Passaro A, Pavan A, Conte P, De
Marinis F and Bonanno L: Combination immunotherapy strategies in
advanced non-small cell lung cancer (NSCLC): Does biological
rationale meet clinical needs? Crit Rev Oncol Hematol. 119:30–39.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
272
|
Tagliamento M, Genova C, Rossi G, Coco S,
Rijavec E, Dal Bello MG, Boccardo S, Grossi F and Alama A:
Microtubule-targeting agents in the treatment of non-small cell
lung cancer: Insights on new combination strategies and
investigational compounds. Expert Opin Investig Drugs. 28:513–523.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
273
|
Girard N: New strategies and novel
combinations in EGFR TKI-resistant non-small cell lung cancer. Curr
Treat Options Oncol. 23:1626–1644. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
274
|
Wu YL, Guarneri V, Voon PJ, Lim BK, Yang
JJ, Wislez M, Huang C, Liam CK, Mazieres J, Tho LM, et al:
Tepotinib plus osimertinib in patients with EGFR-mutated
non-small-cell lung cancer with MET amplification following
progression on first-line osimertinib (INSIGHT 2): A multicentre,
open-label, phase 2 trial. Lancet Oncol. 25:989–1002. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
275
|
Yoshida R, Saigi M, Tani T, Springer BF,
Shibata H, Kitajima S, Mahadevan NR, Campisi M, Kim W, Kobayashi Y,
et al: MET-induced CD73 restrains STING-mediated immunogenicity of
EGFR-mutant lung cancer. Cancer Res. 82:4079–4092. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
276
|
Zhao S, Ma Y, Liu L, Fang J, Ma H, Feng G,
Xie B, Zeng S, Chang J, Ren J, et al: Ningetinib plus gefitinib in
EGFR-mutant non-small-cell lung cancer with MET and AXL
dysregulations: A phase 1b clinical trial and biomarker analysis.
Lung Cancer. 188:1074682024. View Article : Google Scholar : PubMed/NCBI
|
|
277
|
Wang S, Liu C, Yang C, Jin Y, Cui Q, Wang
D, Ge T, He G, Li W, Zhang G, et al: PI3K/AKT/mTOR and
PD-1/CTLA-4/CD28 pathways as key targets of cancer immunotherapy
(review). Oncol Lett. 28:5672024. View Article : Google Scholar : PubMed/NCBI
|
|
278
|
Fu ZY, Huang Y, Lian LS, Huang HT, Zhan
SF, Cai Y, Li JX and Liu XH: Potential of semen coicis in enhancing
the anti-tumor effects of PD-1 inhibitor on A549 cell lines by
blocking the PI3K-AKT-mTOR pathway. Clin Transl Oncol.
26:2250–2261. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
279
|
Li C, Tian C, Liu Y, Liang J, Zeng Y, Yang
Q, Liu Y, Wu D, Wu J, Wang J, et al: Comprehensive profiling
reveals distinct microenvironment and metabolism characterization
of lung adenocarcinoma. Front Genet. 12:6198212021. View Article : Google Scholar : PubMed/NCBI
|
|
280
|
Li Y, Tuerxun H and Zhao Y, Liu X, Li X,
Wen S and Zhao Y: The new era of lung cancer therapy: Combining
immunotherapy with ferroptosis. Crit Rev Oncol Hematol.
198:1043592024. View Article : Google Scholar : PubMed/NCBI
|
|
281
|
Nair NU, Greninger P, Zhang X, Friedman
AA, Amzallag A, Cortez E, Sahu AD, Lee JS, Dastur A, Egan RK, et
al: A landscape of response to drug combinations in non-small cell
lung cancer. Nat Commun. 14:38302023. View Article : Google Scholar : PubMed/NCBI
|
|
282
|
Zheng H, Zeltsman M, Zauderer MG, Eguchi
T, Vaghjiani RG and Adusumilli PS: Chemotherapy-induced
immunomodulation in non-small-cell lung cancer: A rationale for
combination chemoimmunotherapy. Immunotherapy. 9:913–927. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
283
|
Corke L and Sacher A: New strategies and
combinations to improve outcomes in immunotherapy in metastatic
non-small-cell lung cancer. Curr Oncol. 29:38–55. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
284
|
Casagrande GMS, Silva MO, Reis RM and Leal
LF: Liquid biopsy for lung cancer: Up-to-date and perspectives for
screening programs. Int J Mol Sci. 24:25052023. View Article : Google Scholar : PubMed/NCBI
|
|
285
|
Pellini B and Chaudhuri AA: ctDNA
monitoring for small cell lung cancer: Ready for prime time? Clin
Cancer Res. 29:2176–2178. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
286
|
Pan Y, Zhang JT, Gao X, Chen ZY, Yan B,
Tan PX, Yang XR, Gao W, Gong Y, Tian Z, et al: Dynamic circulating
tumor DNA during chemoradiotherapy predicts clinical outcomes for
locally advanced non-small cell lung cancer patients. Cancer Cell.
41:1763–1773 .e4. 2023.
|
|
287
|
Sun X, Abrahamson P, Ballew N, Kalilani L,
Phiri K, Bell KF, Slowley A, Zajac M, Hofstatter E, Stojadinovic A,
et al: The utility of ctDNA in lung cancer clinical research and
practice: A systematic review and meta-analysis of clinical
studies. Cancer Invest. 41:571–592. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
288
|
Ren F, Fei Q, Qiu K, Zhang Y, Zhang H and
Sun L: Liquid biopsy techniques and lung cancer: Diagnosis,
monitoring and evaluation. J Exp Clin Cancer Res. 43:962024.
View Article : Google Scholar : PubMed/NCBI
|
|
289
|
Sands J, Li Q and Hornberger J: Urine
circulating-tumor DNA (ctDNA) detection of acquired EGFR T790M
mutation in non-small-cell lung cancer: An outcomes and total
cost-of-care analysis. Lung Cancer. 110:19–25. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
290
|
Chen K, Yang F, Shen H, Wang C, Li X,
Chervova O, Wu S, Qiu F, Peng D, Zhu X, et al: Individualized
tumor-informed circulating tumor DNA analysis for postoperative
monitoring of non-small cell lung cancer. Cancer Cell.
41:1749–1762.e6. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
291
|
Yan X and Liu C: Clinical application and
prospect of MRD evaluation in lung cancer based on ctDNA level: A
review. Tumori. 109:356–362. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
292
|
Chae YK and Oh MS: Detection of minimal
residual disease using ctDNA in lung cancer: Current evidence and
future directions. J Thorac Oncol. 14:16–24. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
293
|
Reina C, Šabanović B, Lazzari C, Gregorc V
and Heeschen C: Unlocking the future of cancer diagnosis-promises
and challenges of ctDNA-based liquid biopsies in non-small cell
lung cancer. Transl Res. 272:41–53. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
294
|
Medford AJ, Moy B, Spring LM, Hurvitz SA,
Turner NC and Bardia A: Molecular residual disease in breast
cancer: Detection and therapeutic interception. Clin Cancer Res.
29:4540–4548. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
295
|
Lavacchi D, Gelmini S, Calabri A, Rossi G,
Simi L, Caliman E, Mancini I, Salvianti F, Petroni G, Guidolin A,
et al: Early changes in circulating tumor DNA (ctDNA) predict
treatment response in metastatic KRAS-mutated colorectal cancer
(mCRC) patients. Heliyon. 9:e218532023. View Article : Google Scholar : PubMed/NCBI
|
|
296
|
Pellini B and Chaudhuri AA: Circulating
tumor DNA minimal residual disease detection of non-small-cell lung
cancer treated with curative intent. J Clin Oncol. 40:567–575.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
297
|
Dong S, Wang Z, Zhang JT, Yan B, Zhang C,
Gao X, Sun H, Li YS, Yan HH, Tu HY, et al: Circulating tumor
DNA-guided de-escalation targeted therapy for advanced non-small
cell lung cancer: A nonrandomized controlled trial. JAMA Oncol.
10:932–940. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
298
|
Yao H, Wen L, Li Z and Xia C: Analysis of
diagnostic value of CTC and CTDNA in early lung cancer. Cell Mol
Biol (Noisy-le-grand). 69:57–62. 2023. View Article : Google Scholar
|
|
299
|
Xie J, Hu B, Gong Y, He S, Lin J, Huang Q
and Cheng J: A comparative study on ctDNA and tumor DNA mutations
in lung cancer and benign cases with a high number of CTCs and
CTECs. J Transl Med. 21:8732023. View Article : Google Scholar : PubMed/NCBI
|
|
300
|
Xiang Y, Liu X, Wang Y, Zheng D, Meng Q,
Jiang L, Yang S, Zhang S, Zhang X, Liu Y and Wang B: Mechanisms of
resistance to targeted therapy and immunotherapy in non-small cell
lung cancer: Promising strategies to overcoming challenges. Front
Immunol. 15:13662602024. View Article : Google Scholar : PubMed/NCBI
|
|
301
|
Zhang KR, Zhang YF, Lei HM, Tang YB, Ma
CS, Lv QM, Wang SY, Lu LM, Shen Y, Chen HZ and Zhu L: Targeting
AKR1B1 inhibits glutathione de novo synthesis to overcome acquired
resistance to EGFR-targeted therapy in lung cancer. Sci Transl Med.
13:eabg64282021. View Article : Google Scholar : PubMed/NCBI
|
|
302
|
Roys A, Chang X, Liu Y, Xu X, Wu Y and Zuo
D: Resistance mechanisms and potent-targeted therapies of
ROS1-positive lung cancer. Cancer Chemother Pharmacol. 84:679–688.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
303
|
Liu WJ, Du Y, Wen R, Yang M and Xu J: Drug
resistance to targeted therapeutic strategies in non-small cell
lung cancer. Pharmacol Ther. 206:1074382020. View Article : Google Scholar : PubMed/NCBI
|
|
304
|
Lim ZF and Ma PC: Emerging insights of
tumor heterogeneity and drug resistance mechanisms in lung cancer
targeted therapy. J Hematol Oncol. 12:1342019. View Article : Google Scholar : PubMed/NCBI
|
|
305
|
Meyer ML, Fitzgerald BG, Paz-Ares L,
Cappuzzo F, Jänne PA, Peters S and Hirsch FR: New promises and
challenges in the treatment of advanced non-small-cell lung cancer.
Lancet. 404:803–822. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
306
|
Koga T, Suda K and Mitsudomi T: Utility of
the Ba/F3 cell system for exploring on-target mechanisms of
resistance to targeted therapies for lung cancer. Cancer Sci.
113:815–827. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
307
|
Makarem M and Jänne PA: Top advances of
the year: Targeted therapy for lung cancer. Cancer. 130:3239–3250.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
308
|
Li S, Wang A, Wu Y, He S, Shuai W, Zhao M,
Zhu Y, Hu X, Luo Y and Wang G: Targeted therapy for non-small-cell
lung cancer: New insights into regulated cell death combined with
immunotherapy. Immunol Rev. 321:300–334. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
309
|
Zullo L, Dall'Olio FG, Rossi G, Dellepiane
C, Barletta G, Bennicelli E, Ingaliso M, Tagliamento M and Genova
C: Molecular and genetic advances in small cell lung cancer
landscape: From homogeneity to diversity. Int J Mol Sci.
25:2242023. View Article : Google Scholar : PubMed/NCBI
|