Introduction
Multiple primary malignant neoplasms (MPMNs) denote
the concurrent or sequential development of at least two distinct
primary malignant tumors within the body, which may arise from the
same organ, paired organs, different regions of the same system, or
various organs across different systems. Based on the time interval
between tumor occurrences, MPMNs are categorized into two
sub-types, namely, simultaneous MPMNs (sMPMNs), with an interval of
≤6 months, and metachronous MPMNs (mMPMNs), with an interval of
>6 months (1). The morbidity of
MPMNs is steadily increasing, with reported rates in China ranging
from 1.02 to 37.25% over the past 5 years (2). Cases with double primary tumors are
the most common, while cases with three or more primary tumors are
rare (3). Medical advancement has
led to a notable increase in the number of long-term survivors of
initial primary tumors, consequently leading to an increased number
of patients with MPMNs. The present study describes the case of a
patient diagnosed with seven primary malignant tumors that spanned
a 38-year period.
Case report
Current presentation
A 68-year-old female patient with bilateral
pulmonary nodules first identified on a routine health check-up in
July 2021, was admitted to the Department of Cardiothoracic Surgery
at the General Hospital of Central Theater Command (Wuhan, China)
in January 2024, following the detection of an enlarged nodule in
the right lung. At the request of the patient, a breast ultrasound
was conducted, revealing a solid hypoechoic nodule of ~0.5×0.5 cm
at the 8–9 o'clock position, 3–4 cm away from the right nipple,
with clear borders and uneven internal echoes. In the left breast,
a solid hypoechoic nodule of 1.2×0.8 cm was identified at the 2–3
o'clock position, 3–4 cm away from the nipple, with indistinct
borders and uneven internal echoes. Following discussions with the
patient and their family, it was decided that the breast nodules
should be removed. With reference to the Guidelines for Breast
Cancer Diagnosis and Treatment by China Anti-Cancer Association
(2024 edition) (4), the patient and
their family were informed of the survival rate and incidence of
distant metastasis in patients with early-stage breast cancer, as
these rates are comparable between those that undergo
breast-conserving therapy and those that undergo total mastectomy.
Notably, breast-conserving therapy includes both breast-conserving
surgery and post-operative adjuvant radiotherapy. Considering the
age of the patient, their history of multiple tumors and their
financial situation, the patient ultimately opted against
breast-conserving therapy. During surgery, a bilateral breast
nodulectomy was initially performed, and the intraoperative frozen
pathology indicated bilateral breast invasive carcinoma.
Consequently, a bilateral simple mastectomy and bilateral sentinel
lymph node biopsy were subsequently performed. Postoperative
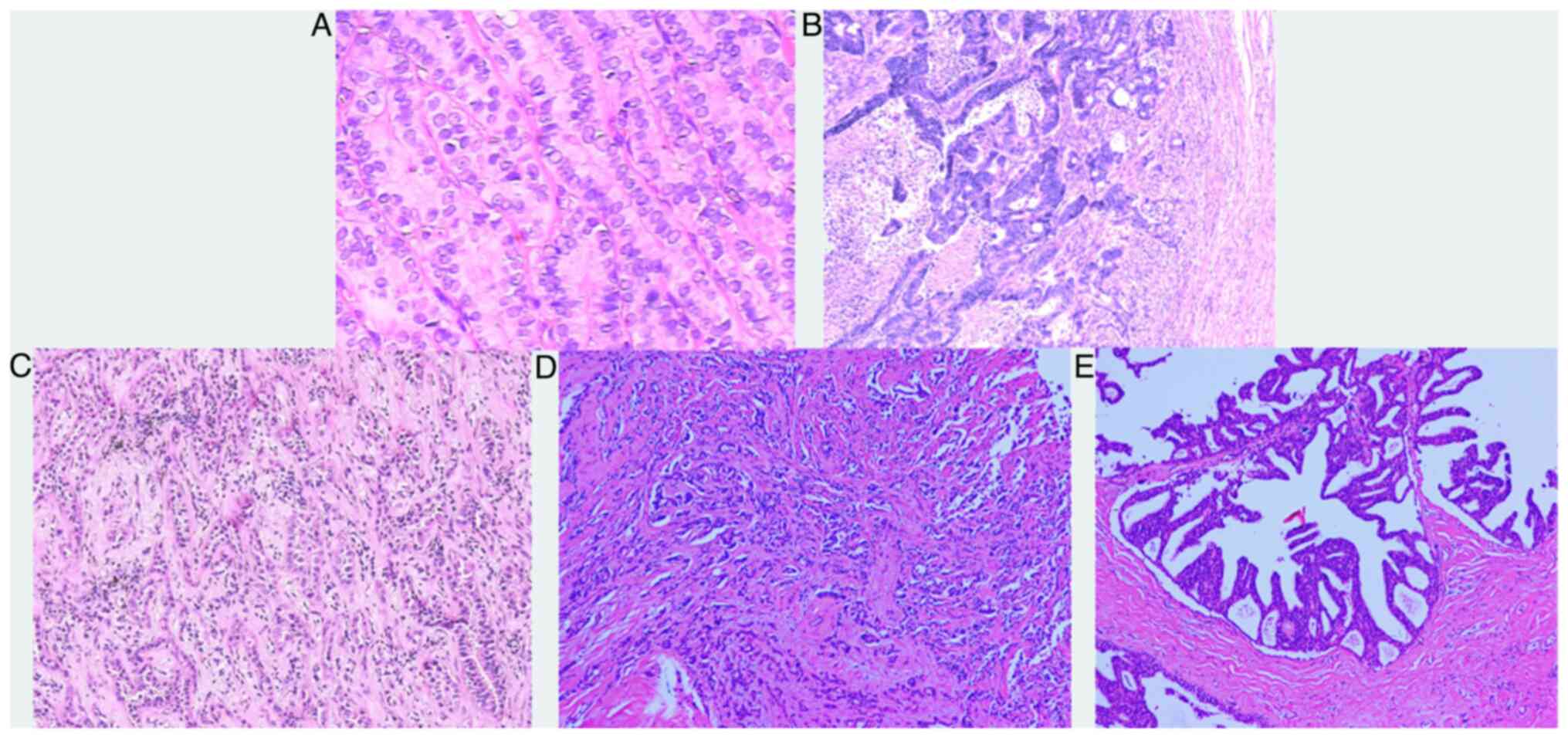
pathology (Fig. 1D and E) revealed
invasive breast cancer on the right side, with a tumor diameter of
2 mm, and without nerve invasion or intravascular cancer embolism.
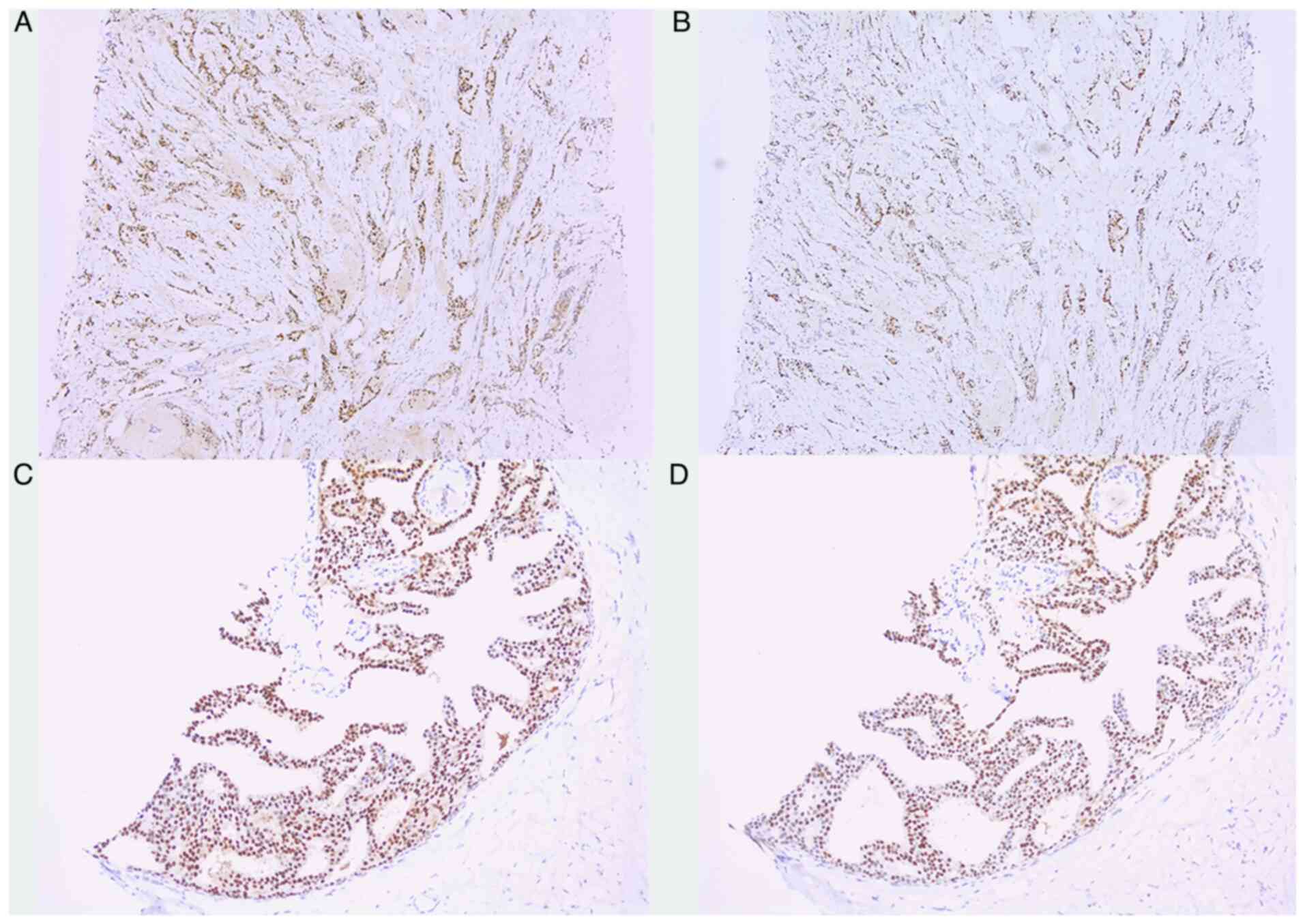
Results of the immunohistochemical analysis (Fig. 2A and B) of the right breast specimen
revealed the following expression results: Estrogen receptor
(ER)(+) (moderate to strong, 95%), progesterone receptor (PR)(+)
(moderate to strong, 80%), human epidermal growth factor receptor 2
(HER-2)(−), GATA binding protein 3 (GATA-3)(+), E-cadherin(+)
(membrane), P120(+) (membrane), cytokeratin (CK)5/6(−), tumor
protein p63 (p63)(−), transcription factor SOX-10 (SOX-10)(−),
calponin(−), gross cystic disease fluid protein-15 (GCDFP-15)(+),
mammaglobin(+), Ki-67(+) (5%) and p53 (wild-type) (data not shown).
Subsequently, the patient was diagnosed with breast carcinoma on
the left side with three foci (1, 3 and 4 mm in diameter,
respectively). Notably, there was no nerve invasion and no
intravascular cancer thrombi were observed; however, breast
carcinoma was accompanied by low-grade ductal carcinoma in
situ, including cribriform and papillary types. Results of
additional immunohistochemical analysis (Fig. 2C and D) of the left breast specimen
revealed expression levels as follows: ER(+) (moderate to strong,
80%), PR(+) (moderate to strong, 60%), HER-2(0), GATA-3(+),
E-cadherin(+) (membrane), P120(+) (membrane), CK5/6(−), p63(−),
SOX-10(−), calponin(−), GCDFP-15(+), mammaglobin(+), Ki-67(+) (10%)
and p53 (wild-type) (data not shown). Notably, no metastases were
detected in the bilateral sentinel or axillary lymph nodes.
Following surgery, the patient was discharged without any
complications and received oral letrozole for endocrine therapy.
Daily letrozole (2.5 mg) was continued for a duration of 5 years,
until the time of disease recurrence. Following 3 months of rest,
the patient was instructed to return to the hospital to address the
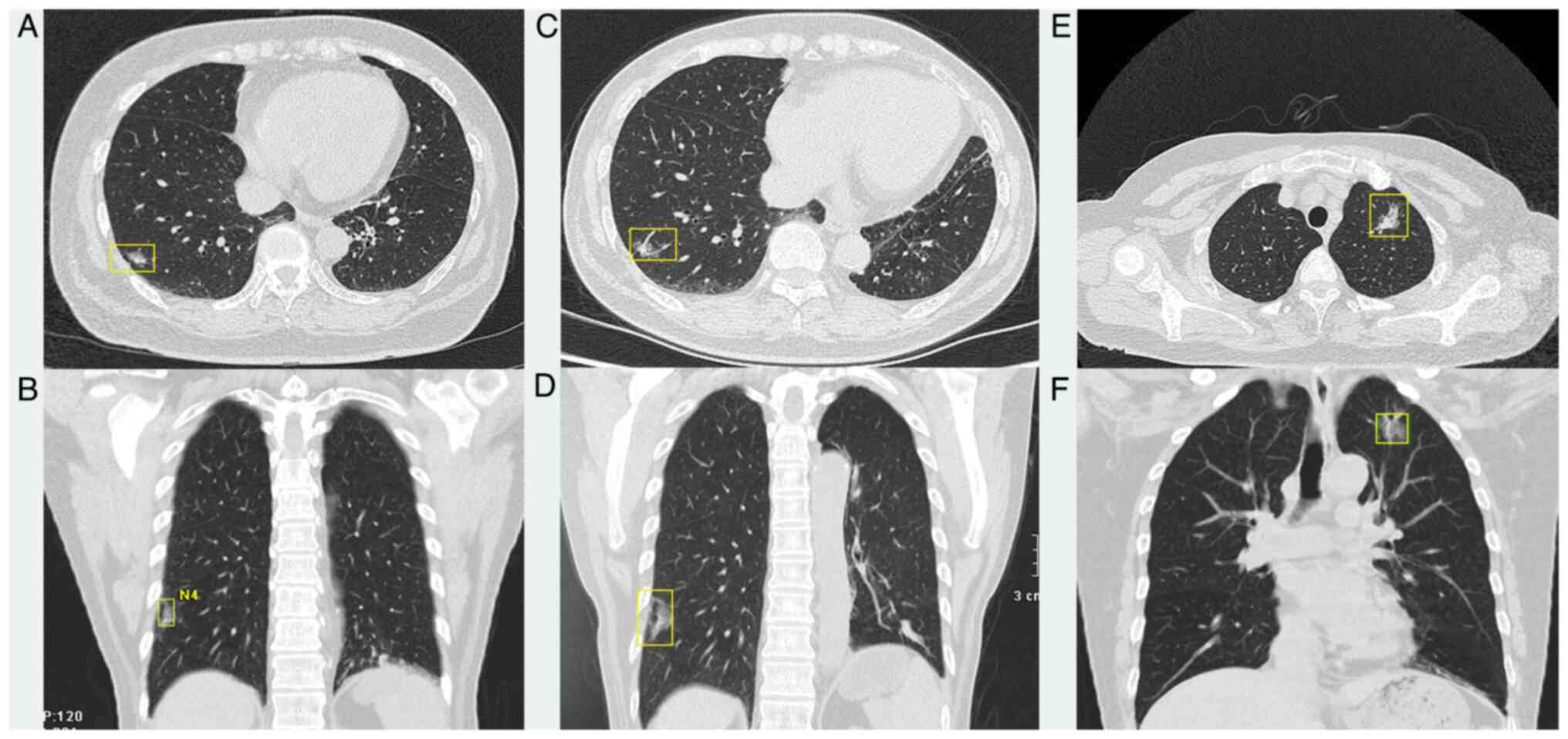
right pulmonary nodule. In April 2024, follow-up chest CT scans
(Fig. 3C and D) revealed an
increase in the size of the right lung nodule. Surgical
intervention was planned to confirm the pathological diagnosis, but
it was postponed due a recent cerebral infarction experienced by
the patient and a high surgical risk. During post-operative
follow-up, the patient, who underwent radical resection of cancer
in the right lower lung at the Tongji hospital (Wuhan, China) in
November 2024, exhibited invasive adenocarcinoma that was
moderately differentiated with an acinar growth pattern, with no
lymph node metastasis. Immunohistochemical analysis revealed the
following expression results: TTF-1(+), CD56(+), synaptophysin(+),
chromogranin A(+), insulinoma-associated protein 1(punctate +),
PCK(−), epithelial membrane antigen(−), CK8/18(−), p63(−), p40(−),
Somatostatin receptor 2(−), PR (1E2)(−), S-100(−), SOX10(−) and
Ki-67 (~1%) (data not shown).
Patient history
The patient presented with a history of hypertension
lasting >10 years. In July 2021, a coronary angiography at the
Department of Cardiothoracic Surgery at the General Hospital of
Central Theater Command revealed moderate-to-severe stenosis in the
proximal left anterior descending artery. In April 2022, the
patient experienced cerebral infarction, and in 2023, the patient
was diagnosed with type 2 diabetes. The patient reported no history
of food or drug allergies, no history of smoking or drinking, no
family history of tumors and maintained healthy lifestyle habits.
Notably, the parents of the patient died due to unknown causes.
In February 1987, the patient had presented to the
Department of General Surgery at the General Hospital of Central
Theater Command with a 10-month history of fecal occult blood. The
patient underwent radical resection of sigmoid colon cancer and
removal of rectal polyps. Postoperative pathology revealed a
papillary adenocarcinoma of the protruding type in the sigmoid
colon, which had invaded the muscular layer, with no metastasis to
the mesenteric lymph nodes. The rectal polyp was identified as an
inflammatory polyp. In 2014, the patient was again admitted to the
Department of General Surgery following the discovery of thyroid
nodules. In October 2014, the patient underwent a bilateral thyroid
and isthmus resection, in addition to a left central compartment
lymph node dissection. Postoperative pathology (Fig. 1A) revealed a left thyroid papillary
microcarcinoma measuring ~0.6 cm, an isthmus papillary
microcarcinoma measuring ~0.3 cm and one parathyroid lymph node
with an inflammatory lesion. In July 2017, the patient was
diagnosed with ileocecal adenocarcinoma at the Hubei Jianghan
Oilfield General Hospital (Qianjiang, China) and was subsequently
admitted to the Department of General Surgery at the General
Hospital of Central Theater Command. The patient underwent a right
hemicolectomy and cholecystectomy. Post-operative pathology
(Fig. 1B) revealed a poorly-to
moderately-differentiated adenocarcinoma, with some mucinous
adenocarcinoma, infiltrating the serosa. No metastasis was detected
in the ileocecal or pericolonic lymph nodes; however, one tumor
nodule was observed in the ileocecal mesentery. In addition, a
tubular adenoma was identified in the colon. Immunohistochemistry
results revealed expression levels as follows: CK7(−), CK20(+),
villin(+), Ki-67(+) (50%), DNA mismatch repair (MMR) protein Msh6
(MSH6)(+), DNA MMR protein Mlh1 (MLH1)(+), MMR endonuclease PMS2
(PMS2)(+) and MSH2(+). Following surgery, the patient received one
course of chemotherapy locally (specific drug names unspecified by
the hospital). In 2021, chest computed tomography (CT) scans
identified partially solid nodules in the upper lobe of the left
lung (Fig. 3E and F) and the lower
lobe of the right lung (Fig. 3A and
B) that were 23×15 and 10×7 mm in size, respectively,
displaying lobulation, spiculation, vacuoles and cavities. The
morphology of the nodules indicated a high likelihood of
early-stage malignant tumors in the lungs. Due to multiple
comorbidities and limited tolerance of the patient, surgery was
initially performed on the left pulmonary nodule. Post-operative
pathology (Fig. 1C) revealed
invasive adenocarcinoma of the left upper lung, comprising 70%
acinar, 25% lepidic and 5% micropapillary types, with no evidence
of nerve invasion, intravascular cancer embolism or lymph node
metastasis. Immunohistochemical analysis revealed expression levels
as follows: Pan-cytokeratin (PCK)(+), CK7(+), NapsinA(+), Thyroid
transcription factor-1 (TTF-1)(+), Ki-67 (3–5%), smooth muscle
actin(+), CK5/6(−), S-100(partially +), CD34(+) (blood vessels) and
D2-40(+) (vascular channels).
Histological examination
Frozen section histopathology
Tissue samples were embedded, frozen at −20 to
−25°C, and sectioned at 4–6 µm. Sections were mounted on glass
slides and immediately fixed in 95% ethanol for 30 sec. H&E
staining (cat. no. G1120; Beijing Solarbio Science & Technology
Co., Ltd.) was performed at room temperature with hematoxylin for
30 sec and eosin for 10 sec.
Conventional histopathology
Specimens were fixed in 10% neutral buffered
formalin at 4°C for 24 h, dehydrated through a graded ethanol
series, paraffin-embedded and sectioned at 4–5 µm. Sections were
H&E-stained at room temperature with hematoxylin for 5 min and
eosin for 10 sec. All stained sections were examined using an
Olympus BX53 light microscope (Olympus Corporation).
Immunohistochemistry
Paraffin-embedded sections (4 µm) were
deparaffinized and rehydrated. Following deparaffinization and
rehydration, antigen retrieval was conducted using citrate buffer
(95°C for 20 min). Endogenous peroxidase activity was quenched with
3% H2O2 for 10 min at room temperature.
Non-specific binding sites were blocked with normal goat serum (20
min at room temperature). Sections were then incubated overnight at
4°C with primary antibodies against ER (1:100; cat. no. RMA-1065),
PR (1:100; cat. no. RMA-0896), HER-2 (1:100; cat. no. RMA-1022),
GATA-3 (1:100; cat. no. RMA-1022), E-cad (1:100; cat. no.
MAB-0738), P120 (1:100; cat. no. MAB-1077), CK5/6 (1:100; cat. no.
RMA-1144), p63 (1:100; cat. no. RMA-1152), SOX-10 (1:100; cat. no.
RMA-1058), calponin (1:100; cat. no. MAB-0712), GCDFP-15 (1:100;
cat. no. MAB-1035), mammaglobin (1:100; cat. no. RMA-1133), Ki-67
(1:100; cat. no. RMA-0542) and p53 (1:100; cat. no. MAB-0674) (all
Fuzhou Maixin Biotech. Co., Ltd.). After washing, sections were
incubated with an HRP-conjugated goat anti-mouse secondary antibody
(1:500; cat. no. ab6789; Abcam) for 30 min at room temperature.
Signal detection was carried out using a DAB substrate (cat. no.
kit-0038; MXB Biotechnologies), followed by counterstaining with
hematoxylin. All sections were examined under an Olympus BX53 light
microscope (Olympus Corporation).
Discussion
The diagnostic criteria for MPMNs were established
by Warren (5) in 1932, requiring
each tumor to be pathologically confirmed as malignant, occur
independently without mutual metastasis and be located in different
sites. The patient described in the present case underwent six
surgeries under general anesthesia (Table I), all of which were pathologically
and immunohistochemically consistent with the diagnosis of a
primary malignant tumor. One limitation of the present study is
that the results described in the manuscript are based on pathology
reports rather than retrievable image files.
 | Table I.Summary of the tumor diagnosis and
treatment of the patient. |
Table I.
Summary of the tumor diagnosis and
treatment of the patient.
| Date | Age at diagnosis,
years | Indication | Treatment | Dosage |
|---|
| February 1987 | 31 | Papillary
adenocarcinoma of the sigmoid colon | Radical surgery for
sigmoid colon cancer | NA |
| October 2014 | 59 | Microscopic papillary
thyroid cancer | Bilateral thyroid and
isthmus resection | NA |
| July 2017 | 62 | Adenocarcinoma of the
ileocecal region | Right
hemicolectomy | No data |
| August 2021 | 66 | Invasive
adenocarcinoma of the left upper lung | Radical surgery for
left upper lung cancer | NA |
| January 2024 | 68 | Invasive carcinoma of
the left and right breasts | Bilateral simple
mastectomy + sentinel lymph node biopsy | Letrozole, 2.5 mg
daily |
| November 2024 | 69 | Invasive
adenocarcinoma of the right lower lung | Radical surgery for
left lower lung cancer | NA |
Prior research has indicated a typical 5- to 10-year
time lapse between the emergence of the initial primary tumor and
the subsequent primary tumor (6).
Other studies have revealed that the peak occurrence of secondary
primary tumors falls within 1 to 3 years following the onset of the
first primary tumor, with a notably higher morbidity observed in
the initial year (7,8). In Western countries, such as Europe
and the United States, MPMNs often manifest in organs such as the
skin, bladder, prostate and thyroid (9). By contrast, in Asian countries, such
as China and Japan, MPMNs are more prevalent in gastrointestinal
malignancies, particularly in esophageal, gastric and colorectal
cancer (10). Zhang et al
(11) conducted a study involving
557 patients, and identified colorectal, breast and thyroid cancer
as the most frequently encountered MPMNs. Notably, the patient
described in the present study was diagnosed with sigmoid carcinoma
as the primary malignancy 38 years prior to study inclusion,
aligning with the predisposition of Asian populations towards
gastrointestinal tumors as initial malignancies. However, the
discovery of the second primary malignancy occurred after a notably
prolonged interval of 27 years, highlighting relatively uncommon
circumstances.
The pathogenic factors of MPMNs remain largely
undefined. Scholars have proposed the multifactorial origin
encompassing environmental influences, lifestyle choices, such as
smoking, excessive alcohol use and obesity, endocrine factors,
genetic predispositions, cancer treatments, such as radiotherapy
and chemotherapy, and age (12).
The patient described in the present study was diagnosed with
sigmoid colon cancer in 1987 and ileocecal adenocarcinoma in 2017,
indicative of metachronous multiple primary colorectal cancer.
Genetic conditions, such as Lynch syndrome (LS) and familial
adenomatous polyposis should also be considered. LS, or hereditary
non-polyposis colorectal cancer, is an autosomal dominant disorder
caused by mutations in DNA MMR genes, namely, MLH1, MSH2, MSH6 and
PMS2, leading to microsatellite instability in the tumor and a lack
of expression. Individuals with LS exhibit a heightened risk of
various cancer types, including colorectal, gastric and endometrial
cancer. In addition, the risk of colorectal cancer may reach 80%,
making it the most prevalent hereditary familial tumor syndrome
(13,14). LS was effectively ruled out in the
present study due to the absence of colorectal cancer among the
patient's close relatives and positive immunohistochemical results
for MMR protein levels. Moreover, extracolorectal MPMNs are not
often observed in cases of colorectal cancer. Lee et al
(15) conducted a retrospective
analysis of 758 patients with colorectal cancer, including 33
patients with extracolorectal MPMNs. Of these, 36.4% presented with
gastric cancer, 15.1% presented with thyroid cancer, 15.1%
presented with prostate cancer and 6.0% presented with esophageal
cancer. The patient described in the present study presented with a
second primary tumor that was papillary microcarcinoma in the left
lobe and isthmus, while the fifth and sixth primary tumors were
invasive carcinomas of the left and right breasts, respectively.
According to the Chinese Expert Consensus on Diagnosis and
Treatment of Multiple Primary Neoplasms (2024 Edition) (16), the diagnostic criteria for bilateral
primary breast cancer stipulate that when the histopathological
types of the bilateral breast cancers are identical, the primary
tumor on the first side must not exhibit local recurrence, lymph
node metastasis or any distant metastases. In this case, the
patient demonstrated no metastasis in the sentinel lymph nodes or
the axillary lymph nodes. Coupled with immunohistochemical results
and a tumor interval time of <6 months, the patient was
diagnosed with synchronous bilateral primary breast cancer. Studies
have noted that the coexistence of breast and thyroid cancer is the
most prevalent among patients with multiple primary cancers
(17,18). A family history of breast cancer, ER
positivity, PR positivity and thyroid hormone positivity are
associated with thyroid and breast tumor development (19). The breast cancer pathology of the
present patient revealed positive ER and PR expression patterns,
indicating its suitability for endocrine therapy. Consequently,
oral letrozole was recommended to the patient for endocrine
treatment during the post-operative period.
The patient's fourth and seventh primary malignant
tumors were invasive adenocarcinomas of the left and right lungs,
respectively. Van Rens et al (20) demonstrated that p53 gene mutation
analysis may differentiate metastatic lung cancer from multiple
primary lung cancers. By comparison, Iwata et al (21) revealed that EGFR and KRAS gene
mutation analysis is conducive to distinguishing multiple primary
lung cancers from intrapulmonary metastases. Mutations in EGFR,
KRAS and TP53 genes may be associated with MPMNs. Despite a healthy
lifestyle and no history of smoking or drinking, the patient's
condition may be associated with factors such as endocrine
influences, proto-oncogene amplification, tumor suppressor gene
mutations or MMR gene defects. Due to financial constraints, the
patient in the present study did not undergo genetic testing to
verify gene mutation-related etiology, which is a limitation of the
present case report. The p53 immunohistochemical assay primarily
reflects the expression status of the p53 protein, and its various
expression patterns can indirectly infer mutations or other
abnormalities in the TP53 gene. Although further genetic testing
has not been conducted, the relatively inexpensive p53
immunohistochemical assay may still hold value.
A unified treatment protocol for MPMNs remains
elusive, largely influenced by tumor stage, underlying conditions,
patient age and complications. Personalized treatment necessitates
a multidisciplinary team approach. Surgery is crucial in managing
multiple primary solid tumors (22). Adebonojo et al (23) revealed that active surgical
intervention is generally preferable for the majority of patients
with MPMNs. The patient described in the present study underwent
six surgeries under general anesthesia since the onset of the
disease, with precise timing and successful post-operative
recovery. The patient receives follow-up phone calls every 3 months
to assess their physical condition. As of the latest submission,
they are reported to be in generally good health.
Research indicates that the prognosis for patients
with MPMNs is influenced by multiple factors, such as tumor stage,
differentiation, site distribution, interval between tumor
occurrences, treatment method and patient age (24). Amer (25) discovered that patients with multiple
primary malignant tumors exhibit a higher survival rate than those
with a single tumor, and the life expectancy of patients with three
or more primary tumors aligns with that of age- and sex-matched
healthy populations. Moreover, a prolonged interval between the
first and second primary cancers may be associated with an improved
prognosis. Oeffinger et al (26) revealed that patients with mMPMNs
exhibited an improved prognosis compared with those with sMPMNs.
Jiang et al (13) documented
the case of a male patient with LS who was diagnosed with a total
of eight primary malignant tumors and survived for >41 years.
Similarly, Zhao et al (27)
reported the case of a female patient with eight primary malignant
tumors who exhibited a lifespan of >32 years. Long-term survival
of the patient described in the present study is attributed to
early disease detection, as well as timely and effective treatment.
The majority of the tumors were diagnosed at an early clinical
stage, allowing for successful surgical intervention. In addition,
the extended intervals between tumor occurrences may contribute to
prolonged survival.
Patients with multiple primary malignant tumors
require diligent post-operative follow-up. Educating patients to
enhance their awareness is crucial for early detection, diagnosis
and treatment, thereby optimizing outcomes. The present patient
exhibited post-operative psychological stress during the follow-up
period, highlighting the requirement to address psychological
well-being. In addition, counseling to alleviate any anxiety
experienced by the patient is crucial for optimal medical
management.
In conclusion, the pathogenesis of MPMNs remains to
be fully elucidated. Immunohistochemistry and molecular genetic
testing are crucial for diagnosis and etiological identification.
Notably, the treatment and prognosis predictions for MPMNs differ
from those of metastatic and recurrent cancers. Early diagnosis and
intervention are vital, and radical surgery may be curative. For
patients who are ineligible for surgical intervention, personalized
treatment plans may be used to prolong survival and improve
prognosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
BX and KH acquired the data. BX, KH and SZ analyzed
and interpreted the data, and confirm the authenticity of all the
raw data. All authors have read and approved the final version of
the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Niu N, Zhou T, Zhao J, Ma X, Yang F and Qi
W: Sublobar reseetion versus Lobectomy in the treatment of
synchronous muhiple primary lung cancer. World J Surg Oncol.
21:1352023. View Article : Google Scholar
|
|
2
|
Amikura K, Ehara K and Kawashima Y: The
Risk of Developing Multiple Primary Cancers among Long-term
survivors five years or more after stomach carcinoma resection.
Tohoku J Exp Med. 250:31–41. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim SH, Park BS, Kim HS and Kim JH:
Synchronous quintuple primary gastrointestinal tract malignancies:
Case report. World J Gastroenterol. 23:173–177. 2017. View Article : Google Scholar
|
|
4
|
The Society of Breast Cancer China
Anti-Cancer Association, Breast Oncology Group of the Oncology
Branch of the Chinese Medical Association, . Guidelines for breast
cancer diagnosis and treatment by China Anti-cancer Association
(2024 edition). China Oncology. 33:1092–1186. 2023.
|
|
5
|
Warren S: Multiple primary malignant
tumors: A survey of the literature and statistical study. Am J
Cancer. 16:7791932.
|
|
6
|
Seegobin K, Staggs E, Khawaja R, Maharaj
S, Gautam S, Smotherman C and Rana F: Pilot study on the occurrence
of multiple cancers following cancer-related therapy at the
University of Florida, Jacksonville (2011–2016). J Investig Med.
66:1050–1054. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim BK, Oh SJ, Song JY, Lee HB, Park MH,
Jung Y, Park WC, Lee J and Sun WY; Korean Breast Cancer Society, :
Clinical characteristics and prognosis associated with multiple
primary cancers in breast cancer patients. J Breast Cancer.
21:62–69. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Berrington de Gonzalez A, Gilbert E,
Curtis R, Inskip P, Kleinerman R, Morton L, Rajaraman P and Little
MP: Second solid cancers after radiation therapy: A systematic
review of the epidemiologic studies of the radiation dose-response
relationship. Int J Radiat Oncol Biol Phys. 86:224–233. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Matsubara T, Yamada K and Nakagawa A: Risk
of second primary malignancy after esophagectomy for squamous cell
carcinoma of the thoracic esophagus. J Clin Oncol. 21:4336–4341.
2003. View Article : Google Scholar
|
|
11
|
Zhang S, Xu Z, Dong G, Li M and Xu L:
Analysis of clinical characteristics of lung cancer combined with
multiple primary malignancies in other organs. Zhongguo Fei Ai Za
Zhi. 24:7–12. 2021.(In Chinese).
|
|
12
|
Corso G, Veronesi P, Santomauro GI,
Maisonneuve P, Morigi C, Peruzzotti G, Intra M, Sacchini V and
Galimberti V: Multiple primary Non-breast tumors in breast cancer
survivors. J Cancer Res Clin Oncol. 144:979–986. 2018. View Article : Google Scholar
|
|
13
|
Jiang J, Huang T, Lin X, Zhang Y, Yang X,
Huang L, Ye Z, Ren X, Teng L, Li J, et al: Long-term survival of a
lynch syndrome patient with eight primary tumors: A case report.
Front Oncol. 12:8960242022. View Article : Google Scholar
|
|
14
|
Hornbuckle K and Fritz CDL: What is Lynch
syndrome? JAMA. 332:1782024. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lee JW, Kim JW and Kim NK: Clinical
characteristics of colorectal cancer patients with a second primary
cancer. Ann Coloproctol. 30:18–22. 2014. View Article : Google Scholar
|
|
16
|
Integrated Rehabilitation Committee for
Multiple Primary Neoplasms and Unknown Primary Tumors of Chinese
Anti-Cancer Association, . Chinese expert consensus on diagnosis
and treatment of multiple primary neoplasms (2024 edition). Chin J
Dig Surg. 23:1261–1276. 2024.
|
|
17
|
Garner CN, Ganetzky R, Brainard J, Hammel
JP, Berber E, Siperstein AE and Milas M: Increased prevalence of
breast cancer among patients with thyroid and parathyroid disease.
Surgery. 142:806–183. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Endo M, Liu JB, Dougan M and Lee JS:
Incidence of second malignancy in patients with papillary thyroid
cancer from surveillance, epidemiology, and end results 13 dataset.
J Thyroid Res. 2018:87653692018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li S and Yang J, Shen Y, Zhao X, Zhang L,
Wang B, Li P, Wang Y, Yi M and Yang J: Clinicopathological
features, survival and risk in breast cancer survivors with thyroid
cancer: An analysis of the SEER database. BMC Public Health.
19:15922019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Van Rens MT, Eijken EJ, Elbers JR, Lammers
JW, Tilanus MG and Slootweg PJ: p53 mutation analysis for definite
diagnosis of multiple primary lung carcinoma. Cancer. 94:188–196.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Iwata T, Sugio K, Uramoto H, Yamada S,
Onitsuka T, Nose N, Ono K, Takenoyama M, Oyama T, Hanagiri T and
Yasumoto K: Detection of EGFR and K-ras mutations for diagnosis of
multiple lung adenocarcinomas. Front Biosci (Landmark Ed).
16:2961–2969. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li QW, Zhu YJ, Zhang WW, Yang H, Liang Y,
Hu YH, Qiu B, Liu MZ and Liu H: Chemoradiotherapy for synchronous
multiple primary cancers with esophageal squamous cell carcinoma: A
Case-control Study. J Cancer. 8:563–569. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Adebonojo SA, Moritz DM and Danby CA: The
results of modern surgical therapy for multiple primary lung
cancers. Chest. 112:693–701. 1997. View Article : Google Scholar
|
|
24
|
Kim BK, Oh SJ, Song JY, Lee HB, Park MH,
Jung Y, Park WC, Lee J and Sun WY; Korean Breast Cancer Society, :
Clinical characteristics and prognosis associated with multiple
primary cancers in breast cancer patients. J Breast Cancer.
21:62–69. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Amer MH: Multiple neoplasms, single
primaries, and patient survival. Cancer Manag Res. 6:119–134. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Oeffinger KC, Baxi SS, Novetsky Friedman D
and Moskowitz CS: Solid tumor second primary neoplasms: Who is at
risk, what can we do? Semin Oncol. 40:676–689. 2013. View Article : Google Scholar
|
|
27
|
Zhao J, Tan Y, Wu Y, Zhao W, Wu J, Ji M,
Shi L, Jiang J and Wu C: A rare case of eight multiple primary
malignant neoplasms in a female patient: A case report and review
of the literature. Oncol Lett. 9:587–590. 2015. View Article : Google Scholar
|