Introduction
Adenoid cystic carcinoma (ACC) is a malignant basal
cell-like tumor originating from the ducts of secretory glands, the
pathological features of which are the biphasic differentiation of
glandular epithelium and myoepithelial cells. The incidence of ACC
accounts for ~1% of malignant tumors in the head and neck region
(1–3). Notably, ACC is more common in people
aged 40–60 years and there is no notable difference in sex
distribution (4). Although disease
progression for ACC is relatively slow and the histological grade
is often low, ACC has a high tendency of neural invasion and
long-term recurrence, thus resulting in a 10-year survival rate of
~40% (5).
At present, surgical resection remains the
first-line treatment option for ACC, but it faces three major
clinical challenges (6): i) Due to
the infiltration and growth of the tumor along the perineural area,
it often leads to a high positive rate of the surgical margin; ii)
the local recurrence rate after surgery is >50%, and it is often
accompanied by symptoms related to nerve invasion; and iii) ACC is
poorly responsive to conventional radiotherapy and chemotherapy, as
evidenced by an objective response rate of <20%. The present
study describes the case of a patient with ACC in the middle and
upper trachea who experienced recurrence 2 months after undergoing
standard partial tracheal resection. The adoption of a
comprehensive intervention strategy combining photodynamic therapy
(PDT) with local targeted drug perfusion may provide a novel
treatment option with notable survival benefits for patients with
advanced ACC who are no longer eligible for surgery.
Case report
The patient was a 45-year-old woman who first
experienced intermittent dyspnea in November 2013, which worsened
after physical activity. The patient initially sought care at a
secondary general hospital in Beijing, China, where they were
diagnosed with and treated for bronchial asthma. The received
pharmacotherapy included standard bronchodilators, such as
β2-adrenergic agonists and theophylline. After 6 months of
treatment, the symptoms exhibited by the patient did not display
notable improvement. Subsequently, the patient was referred to a
tertiary hospital (Beijing, China) for further investigation. In
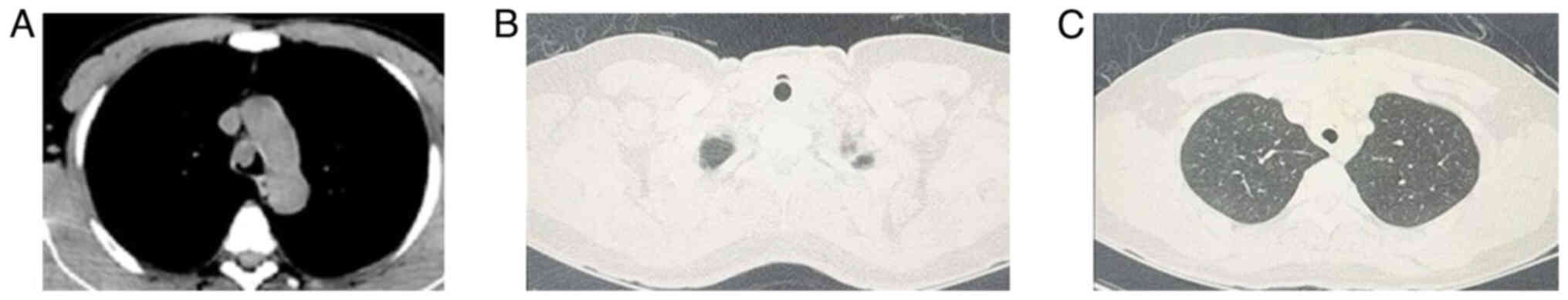
April 2014, a chest CT scan performed at the tertiary hospital
showed diffuse circumferential thickening of the airway walls, with
infiltrative growth along the long axis of the trachea and a
space-occupying lesion detected in the upper segment of the trachea
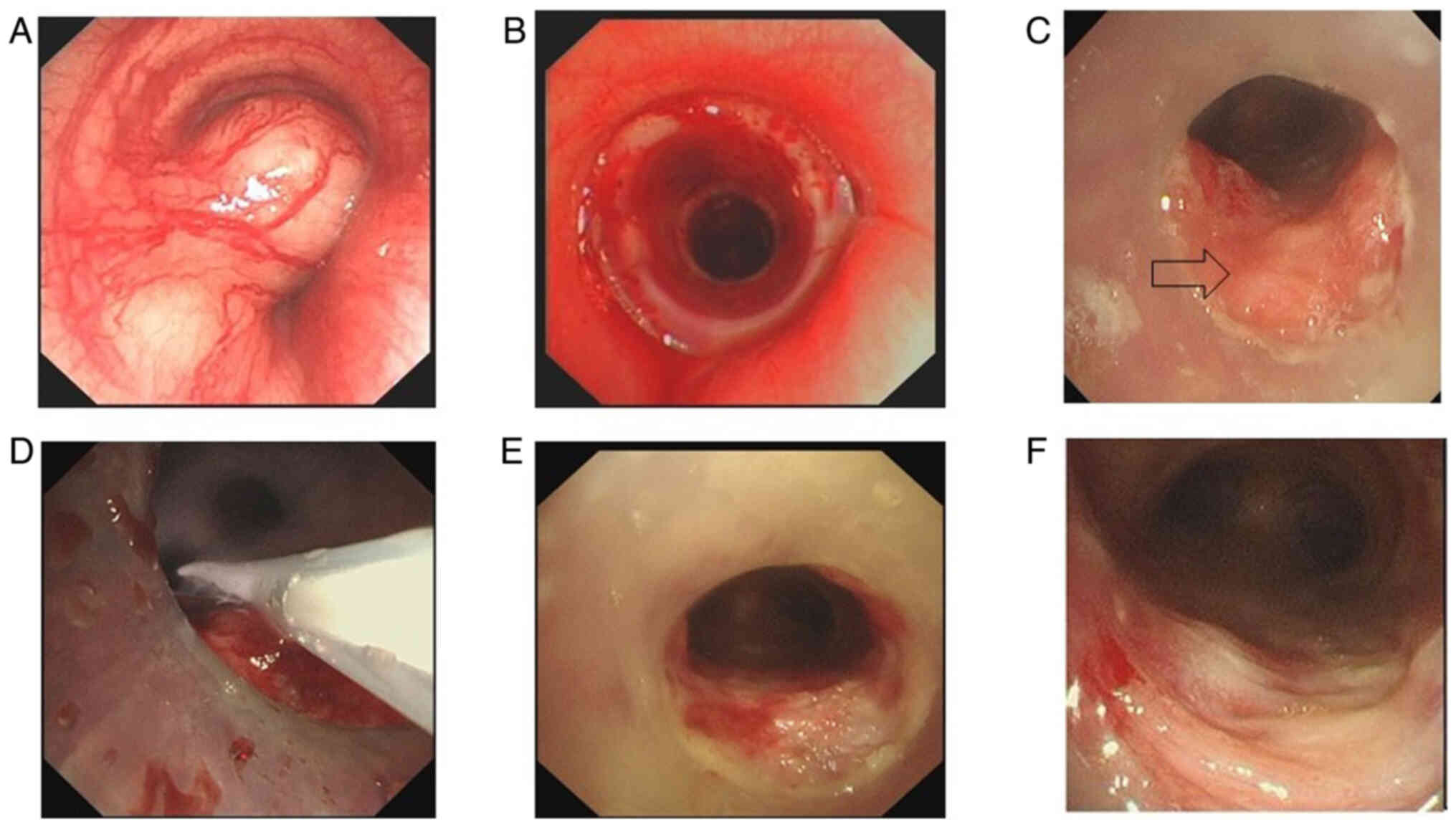
(Fig. 1A). Bronchoscopy revealed a
large, broad-based mass in area II, blocking 90% of the lumen
(Fig. 2A). Physical examination
exhibited coarse breath sounds in both lungs, with audible dry and
wet rales, and wheezing in the anterior chest area. The functional
status of the patient was assessed as follows: Modified Medical
Research Council (mMRC) (7) dyspnea
grade, 3; quality of life (QOL) score (8), 30/60; Karnofsky Performance Status
(KPS) (9), 60. Bronchial artery
embolization and electroresection of the endotracheal tumor were
performed later in April 2014, and the postoperative histopathology
reported tracheal ACC (TACC).
In July 2014, the patient underwent partial tracheal
resection and artificial airway implantation at an external
tertiary hospital (Beijing, China). The specimens of the resected
trachea showed that the entire trachea was involved, the entire
layer of the trachea wall was invaded, nerve invasion was visible,
and tumor components could be seen at both resection margins. After
discharge, the patient was admitted to Dongzhimen Hospital
Affiliated to Beijing University of Chinese Medicine (Beijing,
China) for subsequent management. After 2 months, the patient
experienced recurrent shortness of breath after activity,
accompanied by wheezing. Bronchoscopy revealed circumferential
stenosis at the lower anastomosis of the artificial trachea.
Electrocautery and dilation attempts failed to resolve this
obstruction. In January 2015, an hourglass-shaped tracheal silicone
stent (diameter 14-12-14 mm; length 15-20-15 mm) was placed in
areas I–II (Figs. 1B and C, and
2B and C). The patient reported
that the symptoms had improved following treatment.
Over the following 7 years, the patient's condition
remained stable. In March 2022, due to progressive dyspnea, a
bronchoscopy was performed, revealing a new growth at the lower
edge of the stent. Pathological examination suggested ACC, which
was considered a recurrence (Fig.
2C). After comprehensive consideration, the patient received
three sessions of PDT using HiPorfin (a hematoporphyrin
derivative), which was administered intravenously at 2 mg/kg. Light
activation was performed 48 h post-infusion using a 630-nm
semiconductor laser delivered through 3-cm cylindrical-diffuser
fibers at 100 mW/cm2 (total energy, 1,428 J over 1,380
sec), achieving a fluence of 168 J/cm2 per treatment.
Procedures were conducted under dual-channel bronchoscopic guidance
(Fig. 2D). In April 2022, a
bronchoscopy and biopsy showed no tumor cells (Fig. 2E). In May 2022, the lesion area was
notably reduced compared with before (Fig. 2F). From June to November 2023, the
patient received eight cycles of bronchoscopy-guided
submucosal-injection therapy. Each treatment session utilized a
combination of Endostar® (15 mg, 3 ml) and cisplatin (10
mg, 3 ml), administered via a disposable endoscopic injection
needle (total length, 120 cm; exposed needle tip, 6 mm; outer
diameter, 2.4 mm). During the procedure, the injection needle was
fully extended (6 mm) under direct visualization to penetrate the
mucosal layer. Quadrant injections were performed at the 3, 6, 9
and 12 o'clock positions around the lesion margins, with 0.5–1 ml
of the Endostar and cisplatin solution administered per injection
point (total dose, 6 ml per cycle). The functional outcomes were:
mMRC dyspnea, 1; KPS, 90; QOL score, 55/60. Quantitative analysis
revealed >50% improvement in key functional parameters post-PDT.
The patient was maintained under strict monitoring throughout the
entire hospitalization and treatment period. The most recent
assessment conducted in March 2025 showed a good treatment
response; it was observed that the inflammatory reaction at the
upper edge of the stent was 0 points, granulation hyperplasia was 0
points and the retention of secretions within the stent was grade 1
under bronchoscopy (10,11). The inflammatory reaction at the
lower left edge of the stent was 1 point. A tissue biopsy was
obtained via bronchoscopy, and pathological examination diagnosed
the inflammatory reaction as mucosal inflammatory granulation
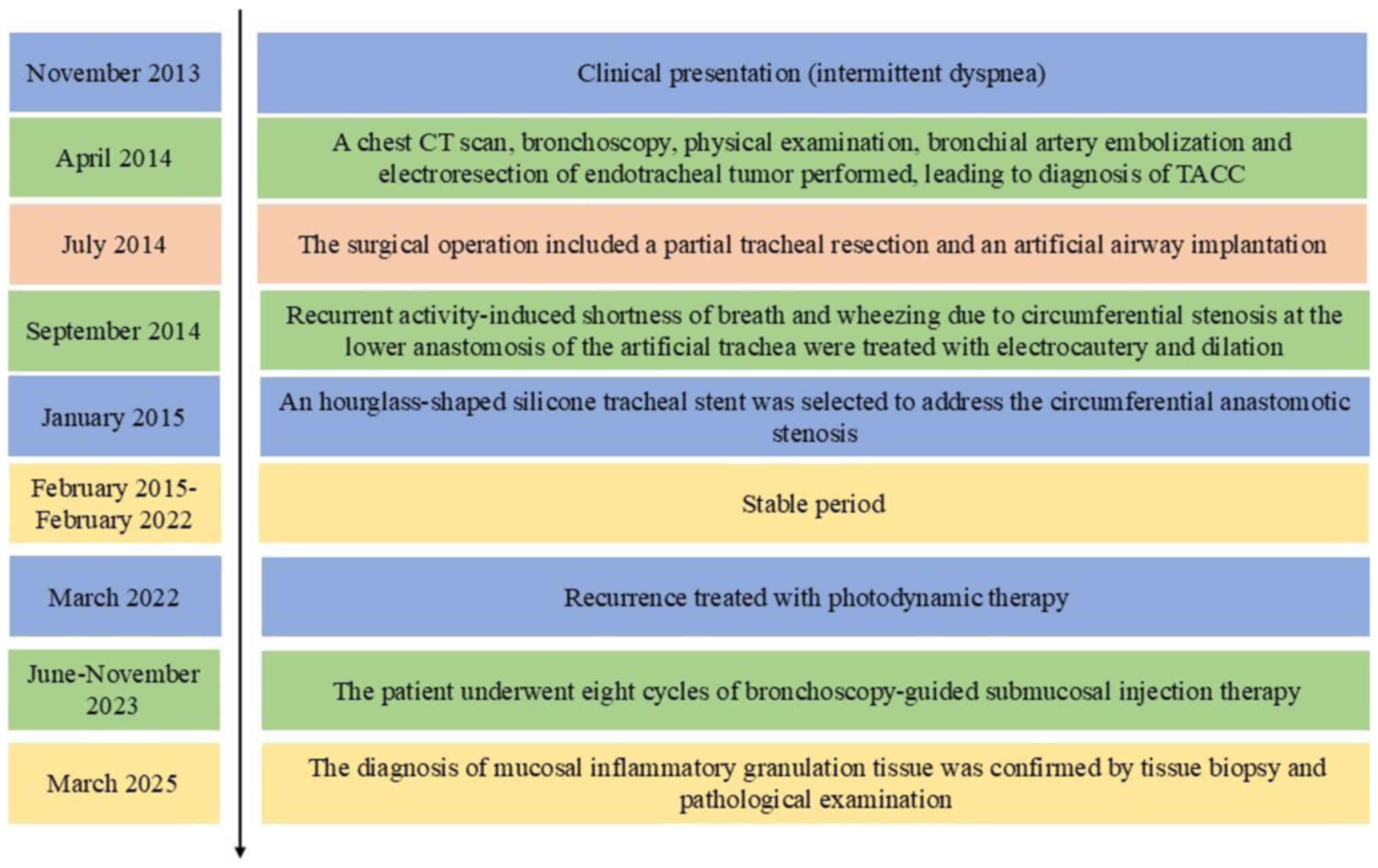
tissue (data not shown). The comprehensive 12-year treatment
schedule for the patient is shown in Fig. 3.
Discussion
The primary sites of ACC are most commonly the
parotid gland, palate and sublingual gland, although it can also
occur in the trachea and bronchi, as well as in the breast, cervix
and other sites (12). Among these
occurrences, primary ACC of the trachea is particularly rare, with
an annual incidence rate of only 0.04–0.2% (6). Furthermore, the early symptoms of
primary ACC of the trachea lack specificity, and often manifest as
progressive dyspnea, cough and expectoration, accompanied by
wheezing (13,14). Such manifestations are confused with
benign airway diseases (such as asthma or chronic bronchitis),
resulting in a delayed diagnosis. The neuroendocrine-driven
infiltration and longitudinal spread along the tracheal wall can
mimic the appearance of benign inflammatory or infectious
processes, often leading to misdiagnosis (15). The present case depicts this typical
misdiagnosis. The patient had wheezing and shortness of breath
after activity; leading to an initial misdiagnosis of bronchial
asthma. Unfortunately, no CT or bronchoscopy was performed, making
it impossible to assess airway lesions at the onset of the disease.
It was not until the asthma medication proved ineffective that CT
showed diffuse ring-shaped thickening of the tracheal wall,
accompanied by a space-occupying lesion in the upper segment of
~2.3 cm, thus confirming the diagnosis of ACC.
Due to the characteristics of slow growth, local
invasion, distant metastasis, nerve invasion and recurrence of ACC,
the tumor range far exceeds the visible and palpable range and the
surgical margin is difficult to determine. These factors result in
a poor local control rate (14).
For salivary gland tumors, in addition to as much resection as
possible, total or subtotal resection of the maxilla is also
required (16). For large tumors
involving the base and movable tongue, traction or mandibular
resection is required. If there is extensive nerve infiltration,
even if a thorough assessment and expanded resection are conducted
before the operation, it is still difficult to ensure that the
resection margin of ACC is negative (17). For tumors at stage T3-T4, complete
resection is impossible and palliative resection is performed
instead (18). The difficulty of
palliative resection lies in weighing the functional and aesthetic
damage caused by surgical trauma and the negative impact of these
factors on patients. Radiotherapy can overcome the surgical
constraints associated with the unique anatomical location of the
tumor, kill tumor cells that have invaded the surroundings of the
tumor or spread along nerves and blood vessels, and treat the areas
with lymphatic drainage. High-energy X-rays can activate the p65
signaling pathway in ACC and control the local recurrence rate
(19). However, ACC is a malignant
tumor with poor sensitivity to radiotherapy and enhancing the
radiotherapy dose poses the risk of radioactive damage. A report on
ACC of the jaw by Li et al (20) proposed that a postoperative
radiotherapy dose of ≥60 Gy had no effect on survival rate, whereas
a postoperative radiotherapy dose of <60 Gy reduced the survival
rate of the patient. A study by Huang et al (21) reported that the local tumor control
rates of patients with head and neck tumors at 2, 5 and 10 years
after brachytherapy were 86.3, 59.0 and 31.5%, respectively. The
overall survival rates at 2, 5 and 10 years were 92.1, 65.0 and
34.1% respectively. Despite active surgery and radiotherapy on ACC,
multiple local relapses are common, and the long-term prognosis is
poor. The focus of clinical treatment for ACC is to identify
effective postoperative adjuvant treatment regimens.
The recurrence of ACC in the patient described in
the present case 2 months after surgical resection highlights the
treatment dilemmas of TACC: i) The biological characteristics of
perineural infiltration, where tumor cells grow invasively along
the nerve bundle membrane space, thus making it difficult to
evaluate the postoperative resection margin. ii) Irreversible
damage to the anatomical structure. Artificial airway
reconstruction was performed during the first operation in the
present case, and the recurrent lesion was located at the distal
end of the stent-tracheal anastomosis. Notably, the second
operation may cause airway collapse or anastomotic fistula. iii)
Resistance to radiotherapy and chemotherapy. ACC tumors have low
sensitivity to traditional radiotherapy and chemotherapy, and
traditional systemic treatment is limited. As a result, PDT has
become a key alternative due to its dual selectivity mechanism
(22).
PDT achieves selective tumor destruction through
well-defined biological processes (23,24).
Firstly, photosensitizers specifically accumulate in malignant
tissues through the high permeability and retention effect of tumor
tissues, and the upregulation of low-density lipoprotein receptors
on the surface of cancer cells. Their concentration can reach 5–10
times that of normal tissues, and they have no systemic toxicity at
therapeutic doses (25). The
important stage of action begins with laser activation: When a
specific wavelength light source (such as 630 nm red light)
activates the photosensitizers, a type II photochemical reaction
occurs, converting ground-state oxygen (3O2)
into highly cytotoxic singlet oxygen (1O2).
The reactive oxygen species 1O2 has an
extremely short diffusion radius (<0.02 µm), and directly
induces the apoptosis and necrosis of cancer cells by oxidizing and
damaging lipid membranes, proteins and mitochondrial DNA. It is
worth noting that this process precisely targets the diseased
cells, and the basement membrane structure is completely preserved
due to the strong resistance of collagen components to oxidative
damage, which is important for maintaining the stability of the
airway structure (25,26). In addition, the efficacy of PDT
stems from the multimodal antitumor mechanism:
1O2 causes vascular endothelial damage,
leading to platelet aggregation and microthrombosis. These outcomes
not only inhibit tumor blood supply and hinder regeneration, but
also markedly reduce the risk of bleeding from the lesion. When
tumor cells die, they release damage-associated molecular patterns,
such as calreticulin and HMGB1, to recruit dendritic cells and
enhance cytotoxic T-lymphocyte responses, generating systemic
antitumor immunity (27).
Particularly in cases of central lung cancer, the systemic
antitumor immune response can notably preserve the normal
ventilation function of the lungs (28,29).
The combined application of PDT with submucosal injection forms a
synergistic effect. Local injection of Endostar can increase the
permeability of tumor cell membranes and promote the intracellular
enrichment of cisplatin. Subsequently, enriched cisplatin
effectively inhibits micrometastasis by binding to DNA and
interfering with its replication, and Endostar blocks the vascular
endothelial growth factor pathway to prevent angiogenesis. The
plasma concentration of cisplatin after mucosal injection is only
1/10 of the dose during intravenous administration, avoiding
systemic toxicity such as bone marrow suppression (30). This minimally invasive sequential
treatment mode achieves a dual reduction in tumor burden, notably
improves airway function and continuously benefits the QOL of
patients.
The present case supported the concept that for
inoperable advanced central ACC, PDT combined with mucosal targeted
injection of cisplatin and Endostar can not only prolong
progression-free survival, but also markedly improve the QOL by
enhancing airway function. It is worth noting that PDT has limited
control over deep tumor invasion and needs to be combined with
local drug injection to remove residual lesions. The present case
emphasizes that PDT may be regarded as a palliative treatment
option for advanced central lung cancer, and its combination with
mucosal drug injections also displays potential benefits for those
patients who are not suitable for surgery. However, it should be
noted that the current study is a single case report. The present
protocol provides a new minimally invasive treatment paradigm for
advanced TACC, but two limitations should be noted: i) The
accumulation of photosensitizers in the skin requires light
protection for 4–6 weeks; and ii) local injection requires precise
bronchoscopy.
Acknowledgements
Not applicable.
Funding
The present case report was funded by the Pilot Project for
Enhancing Clinical Research and Technology Transfer Capacity of
Dongzhimen Hospital, Beijing University of Chinese Medicine (grant
no. DZMG-TZZX-24019).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
LY, HZ and HW conceptualized the study. LW, LY and
HZ designed the study, and collected and analyzed the data. LY, LW,
HZ and HW wrote and edited the manuscript. HZ and HW confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present case report has been approved by the
Ethics Committee of Dongzhimen Hospital affiliated to Beijing
University of Chinese Medicine (approval no. 2024DZMEC-039;
Beijing, China). Ethics approval was required for this case report
because it involves the use and publication of confidential patient
data, including treatment-period photographs.
Patient consent for publication
The patient provided written informed consent for
the publication of the medical data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yao Z, Qiu T, Li C, Kong W, Li G, Song P,
Wang G and Jiao W: Primary pulmonary adenoid cystic carcinoma: A
study of clinicopathological features and molecular alterations in
twenty-one cases. Lung Cancer. 201:1084142025. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ji J, Zhang F, Duan F, Yang H, Hou J, Liu
Y, Dai J, Liao Q, Chen X and Liu Q: Distinct clinicopathological
and genomic features in solid and basaloid adenoid cystic carcinoma
of the breast. Sci Rep. 12:85042022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fang Y, Peng Z, Wang Y, Gao K, Liu Y, Fan
R, Zhang H, Xie Z and Jiang W: Current opinions on diagnosis and
treatment of adenoid cystic carcinoma. Oral Oncol. 130:1059452022.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ko JJ, Siever JE, Hao D, Simpson R and Lau
HY: Adenoid cystic carcinoma of head and neck: Clinical predictors
of outcome from a Canadian centre. Curr Oncol. 23:26–33. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen CH, Reva B, Katabi N, Wizel A, Xu H,
Ho AL, Morris LGT, Bakst RL, Parikh AS, Drier Y, et al: Sympathetic
axonogenesis promotes adenoid cystic carcinoma progression. J Exp
Med. 222:e202422502025. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen Z, Jiang J, Fan Y and Lu H: Pulmonary
adenoid cystic carcinoma: Molecular characteristics and literature
review. Diagn Pathol. 18:652023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sunjaya A, Poulos L, Reddel H and Jenkins
C: Qualitative validation of the modified Medical Research Council
(mMRC) dyspnoea scale as a patient-reported measure of
breathlessness severity. Respir Med. 203:1069842022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Licu M, Ionescu CG and Paun S: Quality of
life in cancer patients: The modern psycho-oncologic approach for
Romania-a review. Curr Oncol. 30:6964–6975. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Blum M, Zeng L and Gelfman LP: Prognostic
performance of the Karnofsky Performance Status for predicting
in-hospital mortality among unselected patients who receive
palliative care consultations. Palliat Med. 38:279–280. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li Z, Tian C, Jiao D, Li J, Li Y, Zhou X,
Zhao H, Zhao Y and Han X: Synergistic effects of silver
nanoparticles and cisplatin in combating inflammation and
hyperplasia of airway stents. Bioact Mater. 9:266–280.
2022.PubMed/NCBI
|
|
11
|
Gao E, Wang P, Chen F, Xu Y, Wang Q, Chen
H, Jiang G, Zhou G, Li D, Liu Y and Duan L: Skin-derived epithelial
lining facilitates orthotopic tracheal transplantation by
protecting the tracheal cartilage and inhibiting granulation
hyperplasia. Biomater Adv. 139:2130372022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang Y, Li X, Xue Y, Huang X, An F and
Tan M: Solid subtype of adenoid cystic carcinoma of the breast with
multiple distant metastases: A case report and literature review.
Front Oncol. 15:15651752025. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Uppal SM, Fatima S, Dandekar PR, Jadhav A
and Pathan S: Efficacy of online adaptive radiotherapy using
surface guidance in treatment of tracheal adenoid cystic carcinoma.
Cureus. 16:e676912024.PubMed/NCBI
|
|
14
|
Högerle BA, Lasitschka F, Muley T, Bougatf
N, Herfarth K, Adeberg S, Eichhorn M, Debus J, Winter H, Rieken S
and Uhl M: Primary adenoid cystic carcinoma of the trachea:
clinical outcome of 38 patients after interdisciplinary treatment
in a single institution. Radiat Oncol. 14:1172019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang SC, Yin LK, Zhang Y, Xue LM, Ye JD,
Tao GY, Yu H and Qiang JW: CT diagnosis and prognosis prediction of
tracheal adenoid cystic carcinoma. Eur J Radiol. 140:1097462021.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Saleh E and Ukwas A: Adenoid cystic
carcinoma of salivary glands: A ten-year review and an assessment
of the current management, surgery, radiotherapy, and chemotherapy.
Int J Otolaryngol. 2023:74014582023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lavareze L, Kimura TC, Cacita N, de
Lima-Souza RA, Cattan MES, Egal ESA, Altemani A and Mariano FV:
Survival outcomes in adenoid cystic carcinoma of the head and neck:
A systematic review of 17 497 cases and meta-analysis. Head Neck.
47:1541–1553. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dou S and Zhu G: Adenoid cystic carcinoma
in the trachea: When surgery is not feasible. Int J Radiat Oncol
Biol Phys. 119:1333–1334. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ran J, Qu G, Chen X and Zhao D: Clinical
features, treatment and outcomes in patients with tracheal adenoid
cystic carcinoma: A systematic literature review. Radiat Oncol.
16:382021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li Q, Xu T, Gao JM, Ye WJ, Gu MF, Hu WH,
Wang F and Cai XY: Surgery alone provides long-term survival rates
comparable to those of surgery plus postoperative radiotherapy for
patients with adenoid cystic carcinoma of the palate. Oral Oncol.
47:170–173. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Huang MW, Zheng L, Liu SM, Shi Y, Zhang J,
Yu GY and Zhang JG: 125I brachytherapy alone for recurrent or
locally advanced adenoid cystic carcinoma of the oral and
maxillofacial region. Strahlenther Onkol. 189:502–507. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sun W, Zhang Q, Wang X, Jin Z, Cheng Y and
Wang G: Clinical practice of photodynamic therapy for non-small
cell lung cancer in different scenarios: Who is the better
candidate? Respiration. 103:193–204. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Moloudi K, Abrahamse H and George BP:
Photodynamic therapy-induced inflammation and adverse effects: An
updated review. Biomed J. July 15–2025.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chang Y, Lim YG and Park K: Synergistic
photodynamic and chemodynamic therapy using hypoxia-adaptive Ce6@Co
nanoparticles for enhanced tumor suppression. Int J Pharm X.
10:1003482025.PubMed/NCBI
|
|
25
|
Ivanova-Radkevich VI: Biochemical basis of
selective accumulation and targeted delivery of photosensitizers to
tumor tissues. Biochemistry (Mosc). 87:1226–1242. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yu H, Chen B, Huang H, He Z, Sun J, Wang
G, Gu X and Tang BZ: AIE-active photosensitizers: Manipulation of
reactive oxygen species generation and applications in photodynamic
therapy. Biosensors (Basel). 12:3482022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhi YS, Chen T, Liang BF, Jiang S, Yao DH,
He ZD, Li CY, He L and Pan ZY: Endoplasmic reticulum-targeted
iridium(III) photosensitizer induces pyroptosis for augmented tumor
immunotherapy. J Inorg Biochem. 260:1126952024. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Howington JA, Blum MG, Chang AC, Balekian
AA and Murthy SC: Treatment of stage I and II non-small cell lung
cancer diagnosis and management of lung cancer, 3rd ed: American
College of Chest Physicians evidence-based clinical practice
guidelines. Chest. 143 (5 Suppl):e278S–e313S. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Alvarez N and Sevilla A: Current advances
in photodynamic therapy (PDT) and the future potential of
PDT-combinatorial cancer therapies. Int J Mol Sci. 25:10232024.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jiang W, Yang X, Wang X, Li Y, Yang X,
Wang N and Yin B: Bronchoscopic intratumoral injections of
cisplatin and endostar as concomitants of standard chemotherapy to
treat malignant central airway obstruction. Postgrad Med J.
98:104–112. 2022. View Article : Google Scholar : PubMed/NCBI
|