|
1
|
Medzhitov R: Origin and physiological
roles of inflammation. Nature. 454:428–435. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Engblom C, Pfirschke C and Pittet MJ: The
role of myeloid cells in cancer therapies. Nat Rev Cancer.
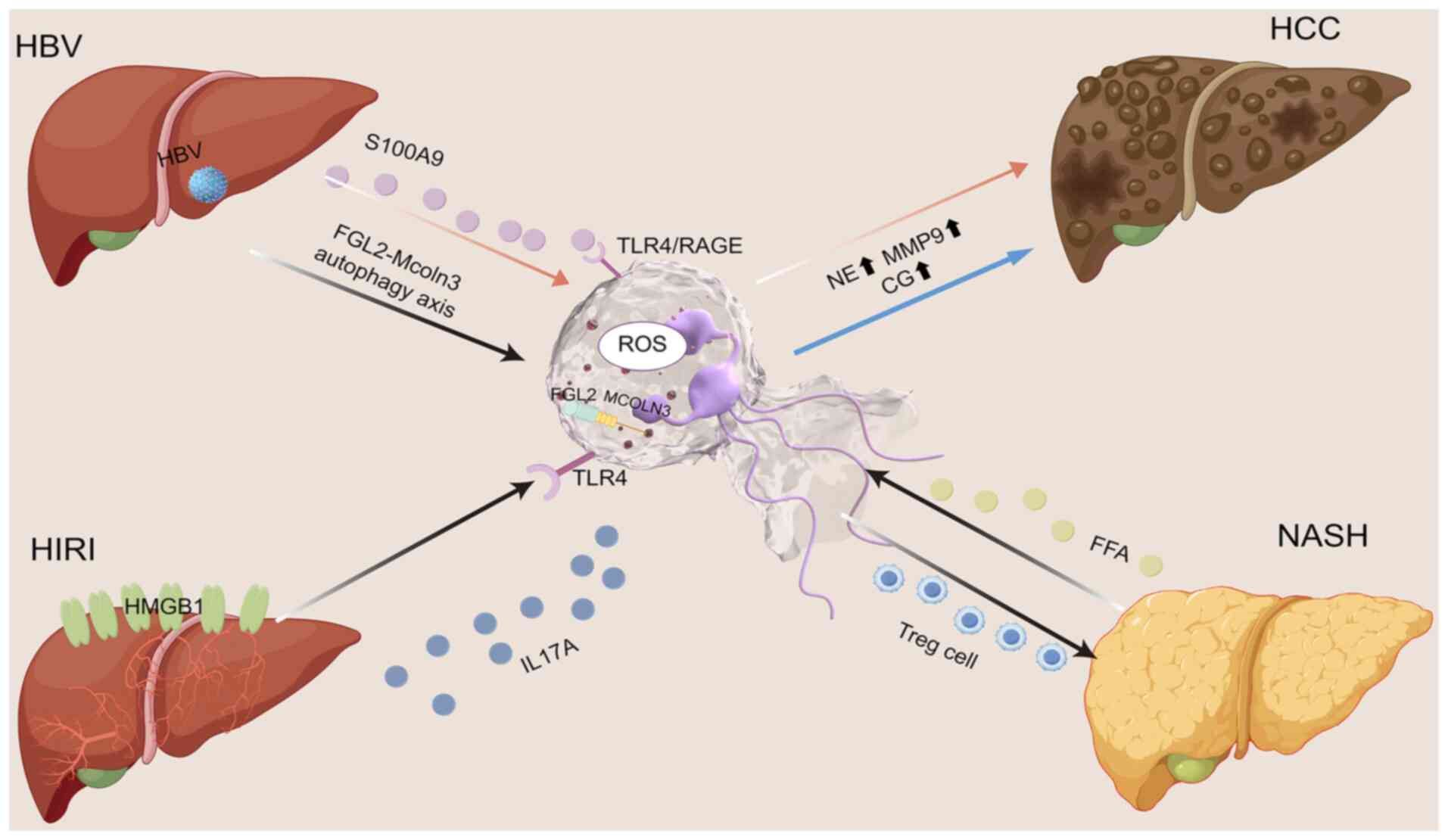
16:447–462. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444. 2008.
View Article : Google Scholar : PubMed/NCBI
|
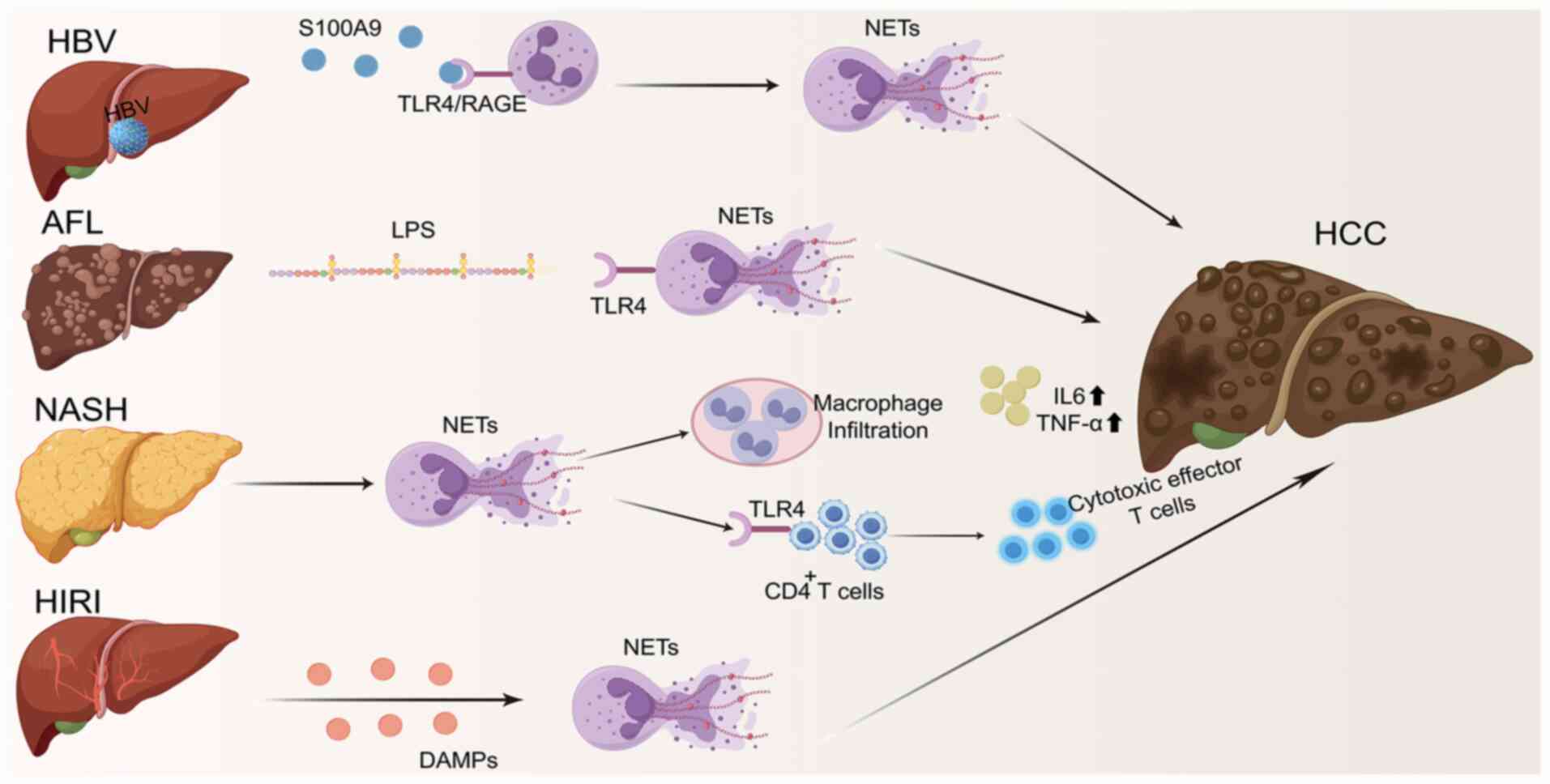
|
4
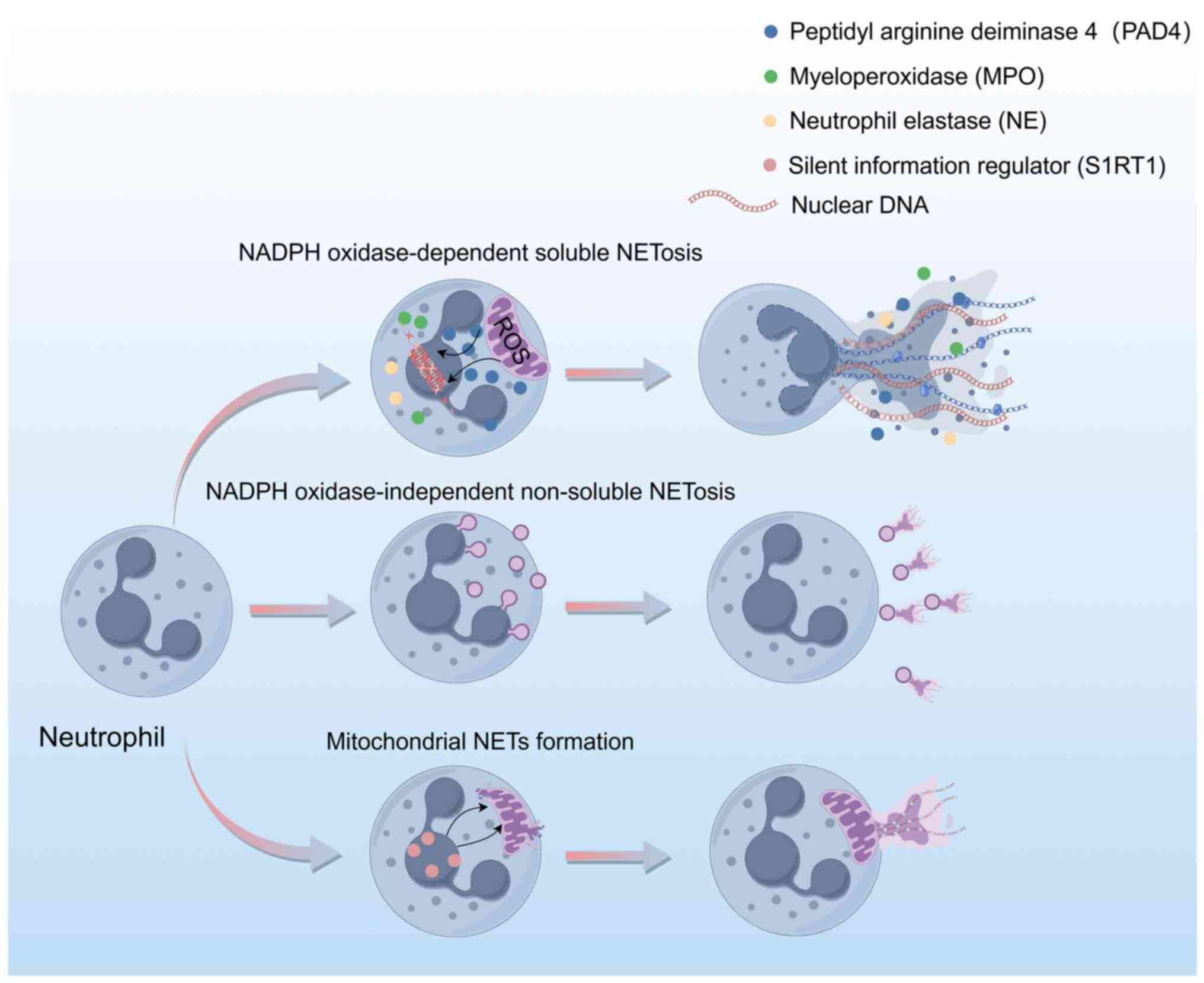
|
Liu Y, Liu L, Zhou Y, Zhou P, Yan Q, Chen
X, Ding S and Zhu F: CKLF1 enhances inflammation-mediated
carcinogenesis and prevents doxorubicin-induced apoptosis via
IL6/STAT3 signaling in HCC. Clin Cancer Res. 25:4141–4154. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wen Y, Zhu Y, Zhang C, Yang X, Gao Y, Li
M, Yang H, Liu T and Tang H: Chronic inflammation, cancer
development and immunotherapy. Front Pharmacol. 13:10401632022.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miao WG, Zhou JY and Han RQ: Analysis of
global liver cancer statistics. Zhonghua Liu Xing Bing Xue Za Zhi.
45:865–869. 2024.(In Chinese). PubMed/NCBI
|
|
7
|
Nakagawa H and Maeda S: Inflammation- and
stress-related signaling pathways in hepatocarcinogenesis. World J
Gastroenterol. 18:4071–4081. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liew PX and Kubes P: The neutrophil's role
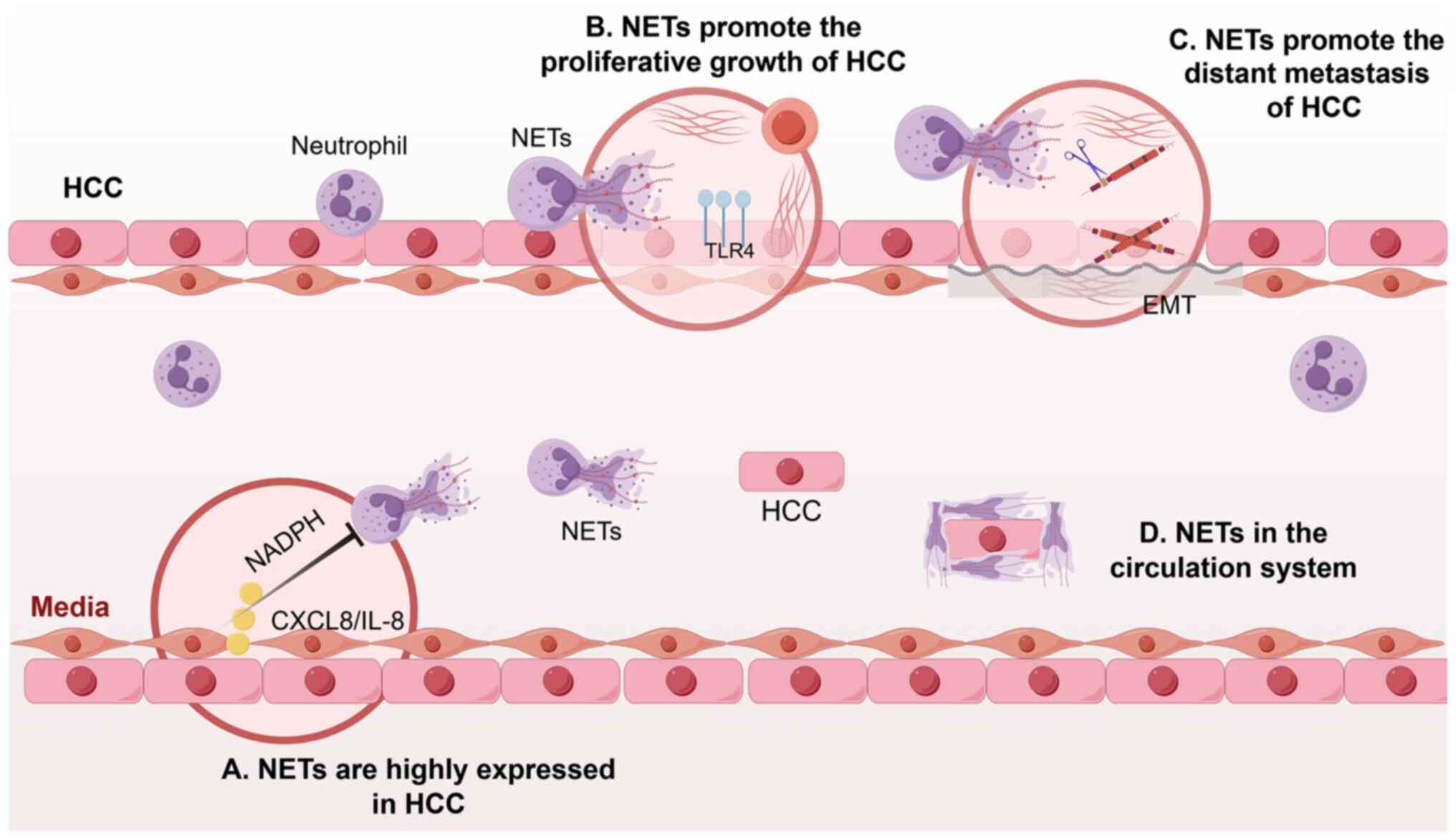
during health and disease. Physiol Rev. 99:1223–1248. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Brinkmann V, Reichard U, Goosmann C,
Fauler B, Uhlemann Y, Weiss DS, Weinrauch Y and Zychlinsky A:
Neutrophil extracellular traps kill bacteria. Science.
303:1532–1535. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hickey MJ and Kubes P: Intravascular
immunity: The host-pathogen encounter in blood vessels. Nat Rev
Immunol. 9:364–375. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li X, Gao Q, Wu W, Hai S, Hu J, You J,
Huang D, Wang H, Wu D, Han M, et al: FGL2-MCOLN3-autophagy
axis-triggered neutrophil extracellular traps exacerbate liver
injury in fulminant viral hepatitis. Cell Mol Gastroenterol
Hepatol. 14:1077–1101. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ackermann M, Anders HJ, Bilyy R, Bowlin
GL, Daniel C, De Lorenzo R, Egeblad M, Henneck T, Hidalgo A,
Hoffmann M, et al: Patients with COVID-19: In the dark-NETs of
neutrophils. Cell Death Differ. 28:3125–3139. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Corsiero E, Pratesi F, Prediletto E,
Bombardieri M and Migliorini P: NETosis as source of autoantigens
in rheumatoid arthritis. Front Immunol. 7:4852016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tohme S, Yazdani HO, Al-Khafaji AB, Chidi
AP, Loughran P, Mowen K, Wang Y, Simmons RL, Huang H and Tsung A:
Neutrophil extracellular traps promote the development and
progression of liver metastases after surgical stress. Cancer Res.
76:1367–1380. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang Y, Liu F, Chen L, Fang C, Li S, Yuan
S, Qian X, Yin Y, Yu B, Fu B, et al: Neutrophil extracellular traps
(NETs) promote non-small cell lung cancer metastasis by suppressing
lncRNA MIR503HG to activate the NF-κB/NLRP3 inflammasome pathway.
Front Immunol. 13:8675162022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fu Y, Tao J, Gu Y, Liu Y, Qiu J, Su D,
Wang R, Luo W, Liu T, Zhang F, et al: Multiomics integration
reveals NETosis heterogeneity and TLR2 as a prognostic biomarker in
pancreatic cancer. NPJ Precis Onc. 8:1092024. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Herranz R, Oto J, Hueso M, Plana E, Cana
F, Castaño M, Cordón L, Ramos-Soler D, Bonanad S, Vera-Donoso CD,
et al: Bladder cancer patients have increased NETosis and impaired
DNaseI-mediated NET degradation that can be therapeutically
restored in vitro. Front Immunol. 14:11710652023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhu W, Fan C, Dong S, Li X, Chen H and
Zhou W: Neutrophil extracellular traps regulating tumorimmunity in
hepatocellular carcinoma. Front Immunol. 14:12539642023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li Y, Wu S, Zhao Y, Dinh T, Jiang D,
Selfridge JE, Myers G, Wang Y, Zhao X, Tomchuck S, et al:
Neutrophil extracellular traps induced by chemotherapy inhibit
tumor growth in murine models of colorectal cancer. J Clin Invest.
134:e1750312024. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang Y, Wu R, Zhan X, Wang XY, Xiang LW,
Duan YQ, You Y, Zhang JB, Wu R, Zhang YY and Duan L: Neutrophil
extracellular traps facilitate liver inflammation/fibrosis
progression by entering macrophages and triggering AIM2
inflammasome-dependent pyroptosis. Cell Commun Signal. 22:5562024.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Varricchi G, Modestino L, Poto R,
Cristinziano L, Gentile L, Postiglione L, Spadaro G and Galdiero
MR: Neutrophil extracellular traps and neutrophil-derived mediators
as possible biomarkers in bronchial asthma. Clin Exp Med.
22:285–300. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vorobjeva NV and Chernyak BV: NETosis:
Molecular mechanisms, role in physiology and pathology.
Biochemistry (Mosc). 85:1178–1190. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Eghbalzadeh K, Georgi L, Louis T, Zhao H,
Keser U, Weber C, Mollenhauer M, Conforti A, Wahlers T and
Paunel-Görgülü A: Compromised anti-inflammatory action of
neutrophil extracellular traps in PAD4-deficient mice contributes
to aggravated acute inflammation after myocardial infarction. Front
Immunol. 10:23132019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sofoluwe A, Bacchetta M, Badaoui M, Kwak
BR and Chanson M: ATP amplifies NADPH-dependent and -independent
neutrophil extracellular trap formation. Sci Rep. 9:165562019.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Leshner M, Wang S, Lewis C, Zheng H, Chen
XA, Santy L and Wang Y: PAD4 mediated histone hypercitrullination
induces heterochromatin decondensation and chromatin unfolding to
form neutrophil extracellular trap-like structures. Front Immun.
3:3072012. View Article : Google Scholar
|
|
26
|
Tokuhiro T, Ishikawa A, Sato H, Takita S,
Yoshikawa A, Anzai R, Sato S, Aoyagi R, Arita M, Shibuya T, et al:
Oxidized phospholipids and neutrophil elastase coordinately play
critical roles in NET formation. Front Cell Dev Biol. 9:7185862021.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yousefi S, Mihalache C, Kozlowski E,
Schmid I and Simon HU: Viable neutrophils release mitochondrial DNA
to form neutrophil extracellular traps. Cell Death Differ.
16:1438–1444. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yang C, Wang Z, Li L, Zhang Z, Jin X, Wu
P, Sun S, Pan J, Su K, Jia F, et al: Aged neutrophils form
mitochondria-dependent vital NETs to promote breast cancer lung
metastasis. J Immunother Cancer. 9:e0028752021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Van Der Windt DJ, Sud V, Zhang H, Varley
PR, Goswami J, Yazdani HO, Tohme S, Loughran P, O'Doherty RM,
Minervini MI, et al: Neutrophil extracellular traps promote
inflammation and development of hepatocellular carcinoma in
nonalcoholic steatohepatitis. Hepatology. 68:1347–1360. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tohme S, Yazdani HO, Sud V, Loughran P,
Huang H, Zamora R, Simmons RL, Vodovotz Y and Tsung A:
Computational analysis supports IL-17A as a central driver of
neutrophil extracellular trap-mediated injury in liver ischemia
reperfusion. J Immunol. 202:268–277. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen Q, Zhang L, Li X and Zhuo W:
Neutrophil extracellular traps in tumor metastasis: Pathological
functions and clinical applications. Cancers (Basel). 13:28322021.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Burki T: WHO's 2024 global hepatitis
report. Lancet Infect Dis. 24:e362–e363. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wu W, Sun S, Wang Y, Zhao R, Ren H, Li Z,
Zhao H, Zhang Y, Sheng J, Chen Z and Shi Y: Circulating neutrophil
dysfunction in HBV-related acute-on-chronic liver failure. Front
Immunol. 12:6203652021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhang Y, Shi K, Zhu B, Feng Y, Liu Y and
Wang X: Neutrophil extracellular trap scores predict 90-day
mortality in hepatitis B-related acute-on-chronic liver failure.
Biomedicines. 12:20482024. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hu S, Liu X, Gao Y, Zhou R, Wei M, Dong J,
Yan H and Zhao Y: Hepatitis B virus inhibits neutrophil
extracellular trap release by modulating reactive oxygen species
production and autophagy. J Immunol. 202:805–815. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhao Q, Chen DP, Chen HD, Wang YZ, Shi W,
Lu YT, Ren YZ, Wu YK, Pang YH, Deng H, et al: NK-cell-elicited
gasdermin-D-dependent hepatocyte pyroptosis induces neutrophil
extracellular traps that facilitate HBV-related acute-on-chronic
liver failure. Hepatology. 81:917–931. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chalasani N, Younossi Z, Lavine JE,
Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM and Sanyal AJ:
The diagnosis and management of nonalcoholic fatty liver disease:
Practice guidance from the American association for the study of
liver diseases. Hepatology. 67:328–357. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kanda T, Goto T, Hirotsu Y, Masuzaki R,
Moriyama M and Omata M: Molecular mechanisms: Connections between
nonalcoholic fatty liver disease, steatohepatitis and
hepatocellular carcinoma. Int J Mol Sci. 21:15252020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wu L, Gao X, Guo Q, Li J, Yao J, Yan K, Xu
Y, Jiang X, Ye D and Guo J: The role of neutrophils in innate
immunity-driven nonalcoholic steatohepatitis: Lessons learned and
future promise. Hepatol Int. 14:652–666. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hwang S, Yun H, Moon S, Cho YE and Gao B:
Role of neutrophils in the pathogenesis of nonalcoholic
steatohepatitis. Front Endocrinol (Lausanne). 12:7518022021.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Rensen SS, Bieghs V, Xanthoulea S,
Arfianti E, Bakker JA, Shiri-Sverdlov R, Hofker MH, Greve JW and
Buurman WA: Neutrophil-derived myeloperoxidase aggravates
non-alcoholic steatohepatitis in low-density lipoprotein
receptor-deficient mice. PLoS One. 7:e524112012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chen J, Liang B, Bian D, Luo Y, Yang J, Li
Z, Zhuang Z, Zang S and Shi J: Knockout of neutrophil elastase
protects against western diet induced nonalcoholic steatohepatitis
in mice by regulating hepatic ceramides metabolism. Biochem Biophys
Res Commun. 518:691–697. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Xu L, Liu X, Jia T, Sun Y, Du Y, Wei S,
Wang W, Zhang Y, Chen W and Zhang S: Tanshinone IIA ameliorates
nonalcoholic steatohepatitis in mice by modulating neutrophil
extracellular traps and hepatocyte apoptosis. Evid Based Complement
Alternat Med. 2022:57693502022.PubMed/NCBI
|
|
44
|
Xu M, Xu H, Ling YW, Liu JJ, Song P, Fang
ZQ, Yue ZS, Duan JL, He F and Wang L: Neutrophil extracellular
traps-triggered hepatocellular senescence exacerbates lipotoxicity
in non-alcoholic steatohepatitis. J Adv Res. Mar 9–2025.(Epub ahead
of print). View Article : Google Scholar
|
|
45
|
Jiménez-Castro MB, Cornide-Petronio ME,
Gracia-Sancho J and Peralta C: Inflammasome-mediated inflammation
in liver ischemia-reperfusion injury. Cells. 8:11312019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Zhang S, Zhang Q, Wang F, Guo X, Liu T,
Zhao Y, Gu B, Chen H and Li Y: Hydroxychloroquine inhibiting
neutrophil extracellular trap formation alleviates hepatic
ischemia/reperfusion injury by blocking TLR9 in mice. Clin Immunol.
216:1084612020. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Arumugam S, Girish Subbiah K, Kemparaju K
and Thirunavukkarasu C: Neutrophil extracellular traps in acrolein
promoted hepatic ischemia reperfusion injury: Therapeutic potential
of NOX2 and p38MAPK inhibitors. J Cell Physiol. 233:3244–3261.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wu X, Yang Z, Wang H, Zhao Y, Gao X and
Zang B: High-mobility group box protein-1 induces acute
pancreatitis through activation of neutrophil extracellular trap
and subsequent production of IL-1β. Life Sci. 286:1192312021.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yazdani HO, Chen HW, Tohme S, Tai S, van
der Windt DJ, Loughran P, Rosborough BR, Sud V, Beer-Stolz D,
Turnquist HR, et al: IL-33 exacerbates liver sterile inflammation
by amplifying neutrophil extracellular trap formation. J Hepatol.
68:130–139. 2018. View Article : Google Scholar
|
|
50
|
Huang H, Tohme S, Al-Khafaji AB, Tai S,
Loughran P, Chen L, Wang S, Kim J, Billiar T, Wang Y and Tsung A:
Damage-associated molecular pattern-activated neutrophil
extracellular trap exacerbates sterile inflammatory liver injury.
Hepatology. 62:600–614. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang CL, Wang Y, Jiang QL, Zeng Y, Yao QP,
Liu X, Li T and Jiang J: DNase I and sivelestat ameliorate
experimental hindlimb ischemia-reperfusion injury by eliminating
neutrophil extracellular traps. J Inflamm Res. 16:707–721. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wang HT, Tong ZJ, Lin YR, Wei KC, Huang
CY, Chen PY, Chen KT, Lin YJ and Tsai HC: Acrolein-induced PKM2
modification drives NETosis and glioma progression. Free Radic Biol
Med. 241:567–581. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Burcham PC: Acrolein and human disease:
Untangling the knotty exposure scenarios accompanying several
diverse disorders. Chem Res Toxicol. 30:145–161. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Xie M, He Z, Bin B, Wen N, Wu J, Cai X and
Sun X: Bulk and single-cell RNA sequencing analysis with 101
machine learning combinations reveal neutrophil extracellular trap
involvement in hepatic ischemia-reperfusion injury and early
allograft dysfunction. Int Immunopharmacol. 131:1118742024.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yang LY, Luo Q, Lu L, Zhu WW, Sun HT, Wei
R, Lin ZF, Wang XY, Wang CQ, Lu M, et al: Increased neutrophil
extracellular traps promote metastasis potential of hepatocellular
carcinoma via provoking tumorous inflammatory response. J Hematol
Oncol. 13:32020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kaltenmeier CT, Yazdani H, Van der Windt
D, Molinari M, Geller D, Tsung A and Tohme S: Neutrophil
extracellular traps as a novel biomarker to predict recurrence-free
and overall survival in patients with primary hepatic malignancies.
HPB (Oxford). 23:309–320. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Guan X, Lu Y, Zhu H, Yu S, Zhao W, Chi X,
Xie C and Yin Z: The crosstalk between cancer cells and neutrophils
enhances hepatocellular carcinoma metastasis via neutrophil
extracellular traps-associated cathepsin G component: A potential
therapeutic target. J Hepatocell Carcinoma. 8:451–465. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Yang L, Liu Q, Zhang X, Liu X, Zhou B,
Chen J, Huang D, Li J, Li H, Chen F, et al: DNA of neutrophil
extracellular traps promotes cancer metastasis via CCDC25. Nature.
583:133–138. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Wang L, Liu Y, Dai Y, Tang X, Yin T, Wang
C, Wang T, Dong L, Shi M, Qin J, et al: Single-cell RNA-seq
analysis reveals BHLHE40-driven pro-tumour neutrophils with
hyperactivated glycolysis in pancreatic tumour microenvironment.
Gut. 72:958–971. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Awasthi D, Nagarkoti S, Sadaf S, Chandra
T, Kumar S and Dikshit M: Glycolysis dependent lactate formation in
neutrophils: A metabolic link between NOX-dependent and independent
NETosis. Biochim Biophys Acta Mol Basis Dis. 1865:1655422019.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Yang LY, Shen XT, Sun HT, Zhu WW, Zhang JB
and Lu L: Neutrophil extracellular traps in hepatocellular
carcinoma are enriched in oxidized mitochondrial DNA which is
highly pro-inflammatory and pro-metastatic. J Cancer. 13:1261–1271.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Yazdani HO, Roy E, Comerci AJ, van der
Windt DJ, Zhang H, Huang H, Loughran P, Shiva S, Geller DA,
Bartlett DL, et al: Neutrophil extracellular traps drive
mitochondrial homeostasis in tumors to augment growth. Cancer Res.
79:5626–5639. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Srirajaskanthan R, Dancey G, Hackshaw A,
Luong T, Caplin ME and Meyer T: Circulating angiopoietin-2 is
elevated in patients with neuroendocrine tumours and correlates
with disease burden and prognosis. Endocr Relat Cancer. 16:967–976.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Chen Y, Hu H, Tan S, Dong Q, Fan X, Wang
Y, Zhang H and He J: The role of neutrophil extracellular traps in
cancer progression, metastasis and therapy. Exp Hematol Oncol.
11:992022. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zhan X, Wu R, Kong X, You Y, He K, Sun XY,
Huang Y, Chen WX and Duan L: Elevated neutrophil extracellular
traps by HBV-mediated S100A9-TLR4/RAGE-ROS cascade facilitate the
growth and metastasis of hepatocellular carcinoma. Cancer Commun
(Lond). 43:225–245. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Jiang ZZ, Peng ZP, Liu XC, Guo HF, Zhou
MM, Jiang D, Ning WR, Huang YF, Zheng L and Wu Y: Neutrophil
extracellular traps induce tumor metastasis through dual effects on
cancer and endothelial cells. OncoImmunology. 11:20524182022.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Ren J, He J, Zhang H, Xia Y, Hu Z,
Loughran P, Billiar T, Huang H and Tsung A: Platelet TLR4-ERK5 axis
facilitates NET-mediated capturing of circulating tumor cells and
distant metastasis after surgical stress. Cancer Res. 81:2373–2385.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Cools-Lartigue J, Spicer J, McDonald B,
Gowing S, Chow S, Giannias B, Bourdeau F, Kubes P and Ferri L:
Neutrophil extracellular traps sequester circulating tumor cells
and promote metastasis. J Clin Invest. 123:3446–3458. 2013.(Epub
ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Wang JL, Ma JB and Wang WX: Role and
mechanisms of neutrophil extracellular traps in hepatocellular
carcinoma metastasis. CJCB. 46:502–514. 2024.
|
|
70
|
Deng Z, Mei S, Ouyang Z, Wang R, Wang L,
Zou B, Dai J, Mao K, Li Q, Guo Q, et al: Dysregulation of gut
microbiota stimulates NETs-driven HCC intrahepatic metastasis:
Therapeutic implications of healthy faecal microbiota
transplantation. Gut Microbes. 17:24765612025. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Holleczek B, Schöttker B and Brenner H:
Helicobacter pylori infection, chronic atrophic gastritis
and risk of stomach and esophagus cancer: Results from the
prospective population-based ESTHER cohort study. Int J Cancer.
146:2773–2783. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Gandhi S, de la Fuente J, Murad MH and
Majumder S: Chronic pancreatitis is a risk factor for pancreatic
cancer, and incidence increases with duration of disease: A
systematic review and meta-analysis. Clin Transl Gastroenterol.
13:e004632022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Castanheira FVS and Kubes P: Neutrophils
and NETs in modulating acute and chronic inflammation. Blood.
133:2178–2185. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Li C, Li M and Wang Z: There is a linear
negative correlation between lipoprotein(a) and non-alcoholic fatty
liver disease. Sci Rep. 15:85382025. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Wang H, Zhang H, Wang Y, Brown ZJ, Xia Y,
Huang Z, Shen C, Hu Z, Beane J, Ansa-Addo EA, et al: Regulatory
T-cell and neutrophil extracellular trap interaction contributes to
carcinogenesis in non-alcoholic steatohepatitis. J Hepatol.
75:1271–1283. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Roh JS and Sohn DH: Damage-associated
molecular patterns in inflammatory diseases. Immune Netw.
18:e272018. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Kaltenmeier C, Yazdani HO, Handu S, Popp
B, Geller D and Tohme S: The role of neutrophils as a driver in
hepatic ischemia-reperfusion injury and cancer growth. Front
Immunol. 13:8875652022. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Zhang Y, Wang Z, Lu Y, Sanchez DJ, Li J,
Wang L, Meng X, Chen J, Kien TT, Zhong M, et al: Region-specific
CD16+ neutrophils promote colorectal cancer progression
by inhibiting natural killer cells. Adv Sci (Weinh).
11:24034142024. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Gao J, Liu J, Lu J, Zhang X, Zhang W, Li
Q, Cai J, Li M, Gan Y, Tang Y and Wu S: SKAP1 expression in cancer
cells enhances colon tumor growth and impairs cytotoxic immunity by
promoting neutrophil extracellular trap formation via the
NFATc1/CXCL8 axis. Adv Sci (Weinh). 11:e24034302024. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Poto R, Cristinziano L, Modestino L, de
Paulis A, Marone G, Loffredo S, Galdiero MR and Varricchi G:
Neutrophil extracellular traps, angiogenesis and cancer.
Biomedicines. 10:4312022. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Spiegel A, Brooks MW, Houshyar S,
Reinhardt F, Ardolino M, Fessler E, Chen MB, Krall JA, DeCock J,
Zervantonakis IK, et al: Neutrophils suppress intraluminal NK
Cell-mediated tumor cell clearance and enhance extravasation of
disseminated carcinoma cells. Cancer Discov. 6:630–649. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Masucci MT, Minopoli M, Del Vecchio S and
Carriero MV: The emerging role of neutrophil extracellular traps
(NETs) in tumor progression and metastasis. Front Immunol.
11:17492020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Liu X, Arfman T, Wichapong K,
Reutelingsperger CPM, Voorberg J and Nicolaes GAF: PAD4 takes
charge during neutrophil activation: Impact of PAD4 mediated NET
formation on immune-mediated disease. J Thromb Haemost.
19:1607–1617. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Okeke EB, Louttit C, Fry C, Najafabadi AH,
Han K, Nemzek J and Moon JJ: Inhibition of neutrophil elastase
prevents neutrophil extracellular trap formation and rescues mice
from endotoxic shock. Biomaterials. 238:1198362020. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Han F, Chen H, Chen L, Yuan C, Shen Q, Lu
G, Chen W, Gong W, Ding Y, Gu A and Tao L: Inhibition of gasdermin
D blocks the formation of NETs and protects acute pancreatitis in
mice. Biochem Biophys Res Commun. 654:26–33. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
He XY, Gao Y, Ng D, Michalopoulou E,
George S, Adrover JM, Sun L, Albrengues J, Daßler-Plenker J, Han X,
et al: Chronic stress increases metastasis via neutrophil-mediated
changes to the microenvironment. Cancer Cell. 42:474–486.e12. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Papayannopoulos V: Neutrophil
extracellular traps in immunity and disease. Nat Rev Immunol.
18:134–147. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Mestas J and Hughes CCW: Of mice and not
men: Differences between mouse and human immunology. J Immunol.
172:2731–2738. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Mousset A, Lecorgne E, Bourget I, Lopez P,
Jenovai K, Cherfils-Vicini J, Dominici C, Rios G, Girard-Riboulleau
C, Liu B, et al: Neutrophil extracellular traps formed during
chemotherapy confer treatment resistance via TGF-β activation.
Cancer Cell. 41:757–775.e10. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Canè S, Barouni RM, Fabbi M, Cuozzo J,
Fracasso G, Adamo A, Ugel S, Trovato R, De Sanctis F, Giacca M, et
al: Neutralization of NET-associated human ARG1 enhances cancer
immunotherapy. Sci Transl Med. 15:eabq62212023. View Article : Google Scholar : PubMed/NCBI
|