|
1
|
Sun H, Liu J, Hu F, Xu M, Leng A, Jiang F
and Chen K: Current research and management of undifferentiated
pleomorphic sarcoma/myofibrosarcoma. Front Genet. 14:11094912023.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wu JT, Nowak E, Imamura J, Leng J, Shepard
D, Campbell SR, Scott J, Nystrom L, Mesko N, Schwartz GK and Burke
ZDC: Immunotherapy in the treatment of undifferentiated pleomorphic
sarcoma and myxofibrosarcoma. Curr Treat Options Oncol. 26:891–909.
2025. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang J and Wu L: First-line immunotherapy
for advanced non-small cell lung cancer: Current progress and
future prospects. Cancer Biol Med. 21:117–124. 2023.PubMed/NCBI
|
|
4
|
Reardon S: First cell therapy for solid
tumours heads to the clinic: What it means for cancer treatment.
Nature. Mar 11–2024.doi: 10.1038/d41586-024-00673-w (Epub ahead of
print).
|
|
5
|
Huang Y, Zhou H, Zhao G, Wang M, Luo J and
Liu J: Immune checkpoint inhibitors serve as the First-line
treatment for advanced head and neck cancer. Laryngoscope.
134:749–761. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lamba N, Ott PA and Iorgulescu JB: Use of
First-line immune checkpoint inhibitors and association with
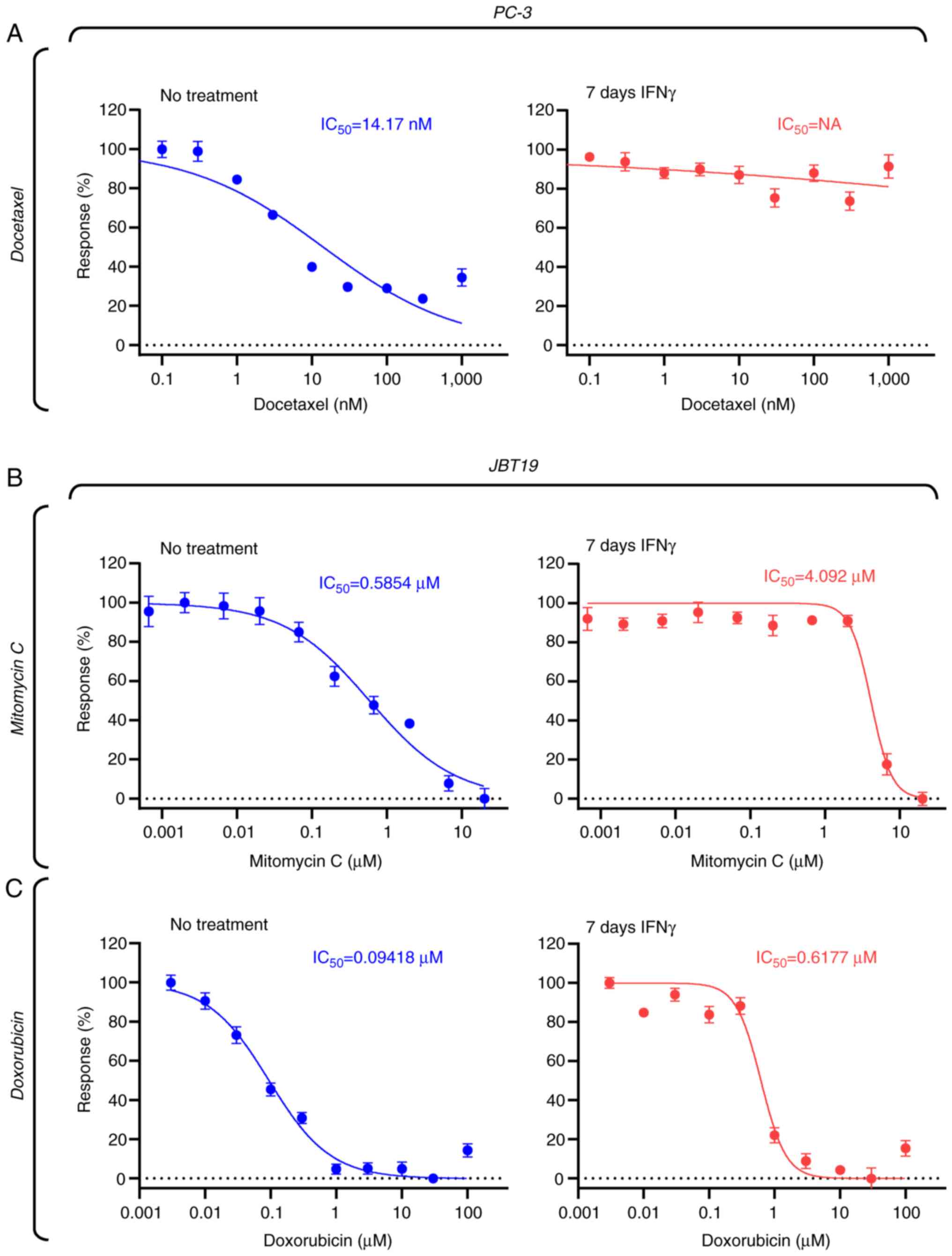
overall survival among patients with metastatic melanoma in the
Anti-PD-1 Era. JAMA Netw Open. 5:e22254592022. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yau T, Galle PR, Decaens T, Sangro B, Qin
S, da Fonseca LG, Karachiwala H, Blanc JF, Park JW, Gane E, et al:
Nivolumab plus ipilimumab versus lenvatinib or sorafenib as
first-line treatment for unresectable hepatocellular carcinoma
(CheckMate 9DW): An Open-label, randomised, phase 3 trial. Lancet.
405:1851–1864. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Diker O and Olgun P: Salvage chemotherapy
in patients with nonsmall cell lung cancer after prior
immunotherapy: Aa retrospective, real-life experience study.
Anticancer Drugs. 33:752–757. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Assi HI, Zerdan MB, Hodroj M, Khoury M,
Naji NS, Amhaz G, Zeidane RA and El Karak F: Value of chemotherapy
post immunotherapy in stage IV non-small cell lung cancer (NSCLC).
Oncotarget. 14:517–525. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sordo-Bahamonde C, Lorenzo-Herrero S,
Gonzalez-Rodriguez AP, Martínez-Pérez A, Rodrigo JP, García-Pedrero
JM and Gonzalez S: Chemo-immunotherapy: A new trend in cancer
treatment. Cancers (Basel). 15:29122023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang Z, Liu X, Chen D and Yu J:
Radiotherapy combined with immunotherapy: The dawn of cancer
treatment. Signal Transduct Target Ther. 7:2582022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ni L and Lu J: Interferon gamma in cancer
immunotherapy. Cancer Med. 7:4509–4516. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Castro F, Cardoso AP, Goncalves RM, Serre
K and Oliveira MJ: Interferon-gamma at the crossroads of tumor
immune surveillance or evasion. Front Immunol. 9:8472018.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Martinez-Lostao L, Anel A and Pardo J: How
do cytotoxic lymphocytes kill cancer cells? Clin Cancer Res.
21:5047–5056. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bhat P, Leggatt G, Waterhouse N and Frazer
IH: Interferon-γ derived from cytotoxic lymphocytes directly
enhances their motility and cytotoxicity. Cell Death Dis.
8:e28362017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mazet JM, Mahale JN, Tong O, Watson RA,
Lechuga-Vieco AV, Pirgova G, Lau VWC, Attar M, Koneva LA, Sansom
SN, et al: IFNgamma signaling in cytotoxic T cells restricts
anti-tumor responses by inhibiting the maintenance and diversity of
intra-tumoral stem-like T cells. Nat Commun. 14:3212023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jorgovanovic D, Song M, Wang L and Zhang
Y: Roles of IFN-γ in tumor progression and regression: A review.
Biomark Res. 8:492020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jing ZL, Liu GL, Zhou N, Xu DY, Feng N,
Lei Y, Ma LL, Tang MS, Tong GH, Tang N and Deng YJ: Interferon-γ in
the tumor microenvironment promotes the expression of B7H4 in
colorectal cancer cells, thereby inhibiting cytotoxic T cells. Sci
Rep. 14:60532024. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Abiko K, Matsumura N, Hamanishi J,
Horikawa N, Murakami R, Yamaguchi K, Yoshioka Y, Baba T, Konishi I
and Mandai M: IFN-γ from lymphocytes induces PD-L1 expression and
promotes progression of ovarian cancer. Br J Cancer. 112:1501–1509.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wong CW, Huang YY and Hurlstone A: The
role of IFN-γ-signalling in response to immune checkpoint blockade
therapy. Essays Biochem. 67:991–1002. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Reijers ILM, Rao D, Versluis JM, Menzies
AM, Dimitriadis P, Wouters MW, Spillane AJ, Klop WMC, Broeks A,
Bosch LJW, et al: IFN-γ signature enables selection of neoadjuvant
treatment in patients with stage III melanoma. J Exp Med.
220:e202219522023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Casadei B, Argnani L, Morigi A, Lolli G,
Broccoli A, Pellegrini C, Nanni L, Stefoni V, Coppola PE, Carella
M, et al: Effectiveness of chemotherapy after anti-PD-1 blockade
failure for relapsed and refractory Hodgkin lymphoma. Cancer Med.
9:7830–7836. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Saleh K, Daste A, Martin N, Pons-Tostivint
E, Auperin A, Herrera-Gomez RG, Baste-Rotllan N, Bidault F, Guigay
J, Le Tourneau C, et al: Response to salvage chemotherapy after
progression on immune checkpoint inhibitors in patients with
recurrent and/or metastatic squamous cell carcinoma of the head and
neck. Eur J Cancer. 121:123–129. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Goldinger SM, Buder-Bakhaya K, Lo SN,
Forschner A, McKean M, Zimmer L, Khoo C, Dummer R, Eroglu Z,
Buchbinder EI, et al: Chemotherapy after immune checkpoint
inhibitor failure in metastatic melanoma: A retrospective
multicentre analysis. Eur J Cancer. 162:22–33. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Black M, Barsoum IB, Truesdell P,
Cotechini T, Macdonald-Goodfellow SK, Petroff M, Siemens DR, Koti
M, Craig AW and Graham CH: Activation of the PD-1/PD-L1 immune
checkpoint confers tumor cell chemoresistance associated with
increased metastasis. Oncotarget. 7:10557–10567. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lazcano R, Barreto CM, Salazar R, Carapeto
F, Traweek RS, Leung CH, Gite S, Mehta J, Ingram DR, Wani KM, et
al: The immune landscape of undifferentiated pleomorphic sarcoma.
Front Oncol. 12:10084842022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wei X, Ruan H, Zhang Y, Qin T, Zhang Y,
Qin Y and Li W: Pan-cancer analysis of IFN-gamma with possible
immunotherapeutic significance: A verification of single-cell
sequencing and bulk omics research. Front Immunol. 14:12021502023.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Taborska P, Lukac P, Stakheev D,
Rajsiglova L, Kalkusova K, Strnadova K, Lacina L, Dvorankova B,
Novotny J, Kolar M, et al: Novel PD-L1- and collagen-expressing
patient-derived cell line of undifferentiated pleomorphic sarcoma
(JBT19) as a model for cancer immunotherapy. Sci Rep. 13:190792023.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kaighn ME, Narayan KS, Ohnuki Y, Lechner
JF and Jones LW: Establishment and characterization of a human
prostatic carcinoma cell line (PC-3). Invest Urol. 17:16–23.
1979.PubMed/NCBI
|
|
30
|
Taborska P, Stakheev D, Svobodova H,
Strizova Z, Bartunkova J and Smrz D: Acute conditioning of
Antigen-expanded CD8+ T cells via the GSK3β-mTORC axis
differentially dictates their immediate and distal responses after
antigen rechallenge. Cancers (Basel). 12:37662020. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Smrž D, Kim MS, Zhang S, Mock BA, Smrzová
S, DuBois W, Simakova O, Maric I, Wilson TM, Metcalfe DD and
Gilfillan AM: mTORC1 and mTORC2 differentially regulate homeostasis
of neoplastic and non-neoplastic human mast cells. Blood.
118:6803–6813. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Smrž D, Dráberová L and Dráber P:
Non-apoptotic phosphatidylserine externalization induced by
engagement of glycosylphosphatidylinositol-anchored proteins. J
Biol Chem. 282:10487–10497. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Taborska P, Bartunkova J and Smrz D:
Simultaneous in vitro generation of human CD34+-derived dendritic
cells and mast cells from non-mobilized peripheral blood
mononuclear cells. J Immunol Methods. 458:63–73. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Taborska P, Lastovicka J, Stakheev D,
Strizova Z, Bartunkova J and Smrz D: SARS-CoV-2 spike
glycoprotein-reactive T cells can be readily expanded from COVID-19
vaccinated donors. Immun Inflamm Dis. 9:1452–1467. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Stakheev D, Taborska P, Kalkusova K,
Bartunkova J and Smrz D: LL-37 as a powerful molecular tool for
boosting the performance of ex vivo-Produced human dendritic cells
for cancer immunotherapy. Pharmaceutics. 14:27472022. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Stakheev D, Taborska P, Strizova Z,
Podrazil M, Bartunkova J and Smrz D: The WNT/β-catenin signaling
inhibitor XAV939 enhances the elimination of LNCaP and PC-3
prostate cancer cells by prostate cancer patient lymphocytes in
vitro. Sci Rep. 9:47612019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Molgora M, Cortez VS and Colonna M:
Killing the invaders: NK cell impact in tumors and Anti-tumor
therapy. Cancers (Basel). 13:5952021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhang S, Liu W, Hu B, Wang P, Lv X, Chen S
and Shao Z: Prognostic significance of Tumor-infiltrating natural
killer cells in solid tumors: A systematic review and
Meta-analysis. Front Immunol. 11:12422020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sun YP, Ke YL and Li X: Prognostic value
of CD8+ tumor-infiltrating T cells in patients with breast cancer:
A systematic review and meta-analysis. Oncol Lett. 25:392023.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yaghobi Z, Movassaghpour A, Talebi M,
Abdoli Shadbad M, Hajiasgharzadeh K, Pourvahdani S and Baradaran B:
The role of CD44 in cancer chemoresistance: A concise review. Eur J
Pharmacol. 903:1741472021. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wang H, Tan M, Zhang S, Li X, Gao J, Zhang
D, Hao Y, Gao S, Liu J and Lin B: Expression and significance of
CD44, CD47 and c-met in ovarian clear cell carcinoma. Int J Mol
Sci. 16:3391–3404. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Yoshida K, Tsujimoto H, Matsumura K,
Kinoshita M, Takahata R, Matsumoto Y, Hiraki S, Ono S, Seki S,
Yamamoto J and Hase K: CD47 is an adverse prognostic factor and a
therapeutic target in gastric cancer. Cancer Med. 4:1322–1333.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Peter ME, Hadji A, Murmann AE, Brockway S,
Putzbach W, Pattanayak A and Ceppi P: The role of CD95 and CD95
ligand in cancer. Cell Death Differ. 22:549–559. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tilsed CM, Fisher SA, Nowak AK, Lake RA
and Lesterhuis WJ: Cancer chemotherapy: Insights into cellular and
tumor microenvironmental mechanisms of action. Front Oncol.
12:9603172022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Montero A, Fossella F, Hortobagyi G and
Valero V: Docetaxel for treatment of solid tumours: A systematic
review of clinical data. Lancet Oncol. 6:229–239. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Imran M, Saleem S, Chaudhuri A, Ali J and
Baboota S: Docetaxel: An update on its molecular mechanisms,
therapeutic trajectory and nanotechnology in the treatment of
breast, lung and prostate cancer. J Drug Delivery Sci Technol.
602020.
|
|
47
|
Sangfelt O, Erickson S and Grander D:
Mechanisms of interferon-induced cell cycle arrest. Front Biosci.
5:D479–D487. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kulkarni A, Scully TJ and O'Donnell LA:
The antiviral cytokine interferon-gamma restricts neural
stem/progenitor cell proliferation through activation of STAT1 and
modulation of retinoblastoma protein phosphorylation. J Neurosci
Res. 95:1582–1601. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Xaus J, Cardo M, Valledor AF, Soler C,
Lloberas J and Celada A: Interferon gamma induces the expression of
p21waf-1 and arrests macrophage cell cycle, preventing induction of
apoptosis. Immunity. 11:103–113. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bossennec M, Di Roio A, Caux C and
Menetrier-Caux C: MDR1 in immunity: Friend or foe? Oncoimmunology.
7:e14993882018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Cao ZH, Zheng QY, Li GQ, Hu XB, Feng SL,
Xu GL and Zhang KQ: STAT1-mediated down-regulation of Bcl-2
expression is involved in IFN-γ/TNF-α-induced apoptosis in NIT-1
cells. PLoS One. 10:e01209212015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Cheon H and Stark GR: Unphosphorylated
STAT1 prolongs the expression of Interferon-induced immune
regulatory genes. Proc Natl Acad Sci USA. 106:9373–9378. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Morrow AN, Schmeisser H, Tsuno T and Zoon
KC: A novel role for IFN-stimulated gene factor 3II in IFN-γ
signaling and induction of antiviral activity in human cells. J
Immunol. 186:1685–1693. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Clark DN, O'Neil SM, Xu L, Steppe JT,
Savage JT, Raghunathan K and Filiano AJ: Prolonged STAT1 activation
in neurons drives a pathological transcriptional response. J
Neuroimmunol. 382:5781682023. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yuasa K, Masubuchi A, Okada T, Shinya M,
Inomata Y, Kida H, Shyouji S, Ichikawa H, Takahashi T, Muroi M and
Hijikata T: Interferon-dependent expression of the human STAT1 gene
requires a distal regulatory region located approximately 6 kb
upstream for its autoregulatory system. Genes Cells. 30:e131882025.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Lastovicka J, Rataj M and Bartunkova J:
Assessment of lymphocyte proliferation for diagnostic purpose:
Comparison of CFSE staining, Ki-67 expression and 3H-thymidine
incorporation. Hum Immunol. 77:1215–1222. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zhou F: Molecular mechanisms of IFN-gamma
to up-regulate MHC class I antigen processing and presentation. Int
Rev Immunol. 28:239–260. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Steimle V, Siegrist CA, Mottet A,
Lisowska-Grospierre B and Mach B: Regulation of MHC class II
expression by interferon-gamma mediated by the transactivator gene
CIITA. Science. 265:106–109. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Benesova I, Kalkusova K, Kwon YS, Taborska
P, Stakheev D, Krausova K, Smetanova J, Ozaniak A, Bartunkova J,
Smrž D and Strizova ZO: Cancer-associated fibroblasts in human
malignancies, with a particular emphasis on sarcomas (review). Int
J Oncol. 67:792025. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hennequin C, Giocanti N and Favaudon V:
S-phase specificity of cell killing by docetaxel (Taxotere) in
synchronised HeLa cells. Br J Cancer. 71:1194–1198. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Mosca L, Ilari A, Fazi F, Assaraf YG and
Colotti G: Taxanes in cancer treatment: Activity, chemoresistance
and its overcoming. Drug Resist Updat. 54:1007422021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Tomasz M: Mitomycin C: Small, fast and
deadly (but very selective). Chem Biol. 2:575–579. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Paz MM, Zhang X, Lu J and Holmgren A: A
new mechanism of action for the anticancer drug mitomycin C:
Mechanism-based inhibition of thioredoxin reductase. Chem Res
Toxicol. 25:1502–1511. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Sritharan S and Sivalingam N: A
comprehensive review on Time-tested anticancer drug doxorubicin.
Life Sci. 278:1195272021. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yosri M, Dokhan M, Aboagye E, Al Moussawy
M and Abdelsamed HA: Mechanisms governing bystander activation of T
cells. Front Immunol. 15:14658892024. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wilczynski B, Dabrowska A, Kulbacka J and
Baczynska D: Chemoresistance and the tumor microenvironment: The
critical role of cell-cell communication. Cell Commun Signal.
22:4862024. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Alsaafeen BH, Ali BR and Elkord E:
Resistance mechanisms to immune checkpoint inhibitors: Updated
insights. Mol Cancer. 24:202025. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Ito T, Smrž D, Jung MY, Bandara G, Desai
A, Smržová Š, Kuehn HS, Beaven MA, Metcalfe DD and Gilfillan AM:
Stem cell factor programs the mast cell activation phenotype. J
Immunol. 188:5428–5437. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Jung MY, Smrž D, Desai A, Bandara G, Ito
T, Iwaki S, Kang JH, Andrade MV, Hilderbrand SC, Brown JM, et al:
IL-33 induces a hyporesponsive phenotype in human and mouse mast
cells. J Immunol. 190:531–538. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Desai A, Jung MY, Olivera A, Gilfillan AM,
Prussin C, Kirshenbaum AS, Beaven MA and Metcalfe DD: IL-6 promotes
an increase in human mast cell numbers and reactivity through
suppression of suppressor of cytokine signaling 3. J Allergy Clin
Immunol. 137:1863–1871. e18662016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Chang TH and Ho PC: Interferon-driven
metabolic reprogramming and tumor microenvironment remodeling.
Immune Netw. 25:e82025. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Wawrzyniak P and Hartman ML: Dual role of
interferon-gamma in the response of melanoma patients to
immunotherapy with immune checkpoint inhibitors. Mol Cancer.
24:892025. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Nigam M, Mishra AP, Deb VK, Dimri DB,
Tiwari V, Bungau SG, Bungau AF and Radu AF: Evaluation of the
association of chronic inflammation and cancer: Insights and
implications. Biomed Pharmacother. 164:1150152023. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Zemek RM, Chin WL, Nowak AK, Millward MJ,
Lake RA and Lesterhuis WJ: Sensitizing the tumor microenvironment
to immune checkpoint therapy. Front Immunol. 11:2232020. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Gillet JP, Efferth T and Remacle J:
Chemotherapy-induced resistance by ATP-binding cassette transporter
genes. Biochim Biophys Acta. 1775:237–262. 2007.PubMed/NCBI
|
|
76
|
Wang X, Long M, Dong K, Lin F, Weng Y,
Ouyang Y, Liu L, Wei J, Chen X, He T and Zhang HZ: Chemotherapy
agents-induced immunoresistance in lung cancer cells could be
reversed by trop-2 inhibition in vitro and in vivo by interaction
with MAPK signaling pathway. Cancer Biol Ther. 14:1123–1132. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Alizadeh D, Wong RA, Gholamin S, Maker M,
Aftabizadeh M, Yang X, Pecoraro JR, Jeppson JD, Wang D, Aguilar B,
et al: IFNγ is critical for CAR T Cell-mediated myeloid activation
and induction of endogenous immunity. Cancer Discov. 11:2248–2265.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Xu H, Niu M, Yuan X, Wu K and Liu A: CD44
as a tumor biomarker and therapeutic target. Exp Hematol Oncol.
9:362020. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Qu S, Jiao Z, Lu G, Xu J, Yao B, Wang T,
Wang J, Yao Y, Yan X, Wang T, et al: Human lung adenocarcinoma CD47
is upregulated by interferon-γ and promotes tumor metastasis. Mol
Ther Oncol. 25:276–287. 2022. View Article : Google Scholar
|
|
80
|
Zhao Y, Shi F, Zhou Q, Li Y, Wu J, Wang R
and Song Q: Prognostic significance of PD-L1 in advanced non-small
cell lung carcinoma. Medicine (Baltimore). 99:e231722020.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Lin YM, Sung WW, Hsieh MJ, Tsai SC, Lai
HW, Yang SM, Shen KH, Chen MK, Lee H, Yeh KT and Chen CJ: High
PD-L1 expression correlates with metastasis and poor prognosis in
oral squamous cell carcinoma. PLoS One. 10:e01426562015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Klement JD, Redd PS, Lu C, Merting AD,
Poschel DB, Yang D, Savage NM, Zhou G, Munn DH, Fallon PG and Liu
K: Tumor PD-L1 engages myeloid PD-1 to suppress type I interferon
to impair cytotoxic T lymphocyte recruitment. Cancer Cell.
41:620–636.e9. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Qadir AS, Ceppi P, Brockway S, Law C, Mu
L, Khodarev NN, Kim J, Zhao JC, Putzbach W, Murmann AE, et al:
CD95/Fas increases stemness in cancer cells by inducing a
STAT1-dependent type I interferon response. Cell Rep. 18:2373–2386.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Risso V, Lafont E and Le Gallo M:
Therapeutic approaches targeting CD95L/CD95 signaling in cancer and
autoimmune diseases. Cell Death Dis. 13:2482022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Dart A: Presenting fibroblasts. Nat Rev
Cancer. 22:1932022. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Mortara L, Castellani P, Meazza R, Tosi G,
De Lerma Barbaro A, Procopio FA, Comes A, Zardi L, Ferrini S and
Accolla RS: CIITA-induced MHC class II expression in mammary
adenocarcinoma leads to a Th1 polarization of the tumor
microenvironment, tumor rejection, and specific antitumor memory.
Clin Cancer Res. 12:3435–3443. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Panelli MC, Wang E, Shen S, Schluter SF,
Bernstein RM, Hersh EM, Stopeck A, Gangavalli R, Barber J, Jolly D
and Akporiaye ET: Interferon gamma (IFNgamma) gene transfer of an
EMT6 tumor that is poorly responsive to IFNgamma stimulation:
Increase in tumor immunogenicity is accompanied by induction of a
mouse class II transactivator and class II MHC. Cancer Immunol
Immunother. 42:99–107. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Forero A, Li Y, Chen D, Grizzle WE, Updike
KL, Merz ND, Downs-Kelly E, Burwell TC, Vaklavas C, Buchsbaum DJ,
et al: Expression of the MHC Class II pathway in Triple-negative
breast cancer tumor cells is associated with a good prognosis and
infiltrating lymphocytes. Cancer Immunol Res. 4:390–399. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Roemer MGM, Redd RA, Cader FZ, Pak CJ,
Abdelrahman S, Ouyang J, Sasse S, Younes A, Fanale M, Santoro A, et
al: Major histocompatibility complex class ii and programmed death
ligand 1 expression predict outcome after programmed death 1
blockade in classic hodgkin lymphoma. J Clin Oncol. 36:942–950.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Axelrod ML, Cook RS, Johnson DB and Balko
JM: Biological consequences of MHC-II Expression by tumor cells in
cancer. Clin Cancer Res. 25:2392–2402. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Macy AM, Herrmann LM, Adams AC and
Hastings KT: Major histocompatibility complex class II in the tumor
microenvironment: Functions of nonprofessional antigen-presenting
cells. Curr Opin Immunol. 83:1023302023. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Johnson DB, Nixon MJ, Wang Y, Wang DY,
Castellanos E, Estrada MV, Ericsson-Gonzalez PI, Cote CH, Salgado
R, Sanchez V, et al: Tumor-specific MHC-II expression drives a
unique pattern of resistance to immunotherapy via LAG-3/FCRL6
engagement. JCI Insight. 3:e1203602018. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Lei PJ, Pereira ER, Andersson P, Amoozgar
Z, Van Wijnbergen JW, O'Melia MJ, Zhou H, Chatterjee S, Ho WW,
Posada JM, et al: Cancer cell plasticity and MHC-II-mediated immune
tolerance promote breast cancer metastasis to lymph nodes. J Exp
Med. 220:e202218472023. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Shen J, Choi YL, Lee T, Kim H, Chae YK,
Dulken BW, Bogdan S, Huang M, Fisher GA, Park S, et al: Inflamed
immune phenotype predicts favorable clinical outcomes of immune
checkpoint inhibitor therapy across multiple cancer types. J
Immunother Cancer. 12:e0083392024. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Chen S, Crabill GA, Pritchard TS, McMiller
TL, Wei P, Pardoll DM, Pan F and Topalian SL: Mechanisms regulating
PD-L1 expression on tumor and immune cells. J Immunother Cancer.
7:3052019. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Mimura K, Teh JL, Okayama H, Shiraishi K,
Kua LF, Koh V, Smoot DT, Ashktorab H, Oike T, Suzuki Y, et al:
PD-L1 expression is mainly regulated by interferon gamma associated
with JAK-STAT pathway in gastric cancer. Cancer Sci. 109:43–53.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Landsberg J, Kohlmeyer J, Renn M, Bald T,
Rogava M, Cron M, Fatho M, Lennerz V, Wölfel T, Hölzel M and Tüting
T: Melanomas resist T-cell therapy through Inflammation-induced
reversible dedifferentiation. Nature. 490:412–416. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Wang B, Han Y, Zhang Y, Zhao Q, Wang H,
Wei J, Meng L, Xin Y and Jiang X: Overcoming acquired resistance to
cancer immune checkpoint therapy: Potential strategies based on
molecular mechanisms. Cell Biosci. 13:1202023. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Goddard ET, Linde MH, Srivastava S, Klug
G, Shabaneh TB, Iannone S, Grzelak CA, Marsh S, Riggio AI, Shor RE,
et al: Immune evasion of dormant disseminated tumor cells is due to
their scarcity and can be overcome by T cell immunotherapies.
Cancer Cell. 42:119–134.e12. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Yu M, Peng Z, Qin M, Liu Y, Wang J, Zhang
C, Lin J, Dong T, Wang L, Li S, et al: Interferon-gamma induces
tumor resistance to anti-PD-1 immunotherapy by promoting YAP phase
separation. Mol Cell. 81:1216–1230.e9. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Mandai M, Hamanishi J, Abiko K, Matsumura
N, Baba T and Konishi I: Dual faces of IFNγ in cancer progression:
A role of PD-L1 induction in the determination of Pro- and
antitumor immunity. Clin Cancer Res. 22:2329–2334. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Beziaud L, Young CM, Alonso AM, Norkin M,
Minafra AR and Huelsken J: IFNγ-induced stem-like state of cancer
cells as a driver of metastatic progression following
immunotherapy. Cell Stem Cell. 30:818–831.e6. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Gocher AM, Workman CJ and Vignali DAA:
Interferon-gamma: Teammate or opponent in the tumour
microenvironment? Nat Rev Immunol. 22:158–172. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Korentzelos D, Wells A and Clark AM:
Interferon-γ increases sensitivity to chemotherapy and provides
immunotherapy targets in models of metastatic Castration-resistant
prostate cancer. Sci Rep. 12:66572022. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Gupta J, Abed HS, Uthirapathy S, Kyada A,
Rab SO, Shit D, Janney B, Nathiya D, Kadhim AJ and Mustafa YF:
Beyond TRAIL resistance: Novel strategies for potentiating
TRAIL-induced apoptosis in cancer. Exp Cell Res. 450:1146192025.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Merchant MS, Yang X, Melchionda F, Romero
M, Klein R, Thiele CJ, Tsokos M, Kontny HU and Mackall CL:
Interferon gamma enhances the effectiveness of tumor necrosis
factor-related apoptosis-inducing ligand receptor agonists in a
xenograft model of Ewing's sarcoma. Cancer Res. 64:8349–8356. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Johnsen JI, Pettersen I, Ponthan F,
Sveinbjornsson B, Flaegstad T and Kogner P: Synergistic induction
of apoptosis in neuroblastoma cells using a combination of
cytostatic drugs with interferon-gamma and TRAIL. Int J Oncol.
25:1849–1857. 2004.PubMed/NCBI
|
|
108
|
Gawrylak A, Brodaczewska K,
Iwanicka-Nowicka R, Koblowska M, Synowiec A, Bodnar L, Szczylik C,
Lesyng B, Stec R and Kieda C: Hypoxia alters the response of
ovarian cancer cells to the mitomycin C drug. Front Cell Dev Biol.
13:15751342025. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Strese S, Fryknas M, Larsson R and Gullbo
J: Effects of hypoxia on human cancer cell line chemosensitivity.
BMC Cancer. 13:3312013. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Hultman I, Haeggblom L, Rognmo I, Jansson
Edqvist J, Blomberg E, Ali R, Phillips L, Sandstedt B, Kogner P,
Shirazi Fard S and Ährlund-Richter L: Doxorubicin-provoked increase
of mitotic activity and concomitant drain of G0-pool in
therapy-resistant BE(2)-C neuroblastoma. PLoS One. 13:e01909702018.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Lyu YL, Kerrigan JE, Lin CP, Azarova AM,
Tsai YC, Ban Y and Liu LF: Topoisomerase IIbeta mediated DNA
double-strand breaks: Implications in doxorubicin cardiotoxicity
and prevention by dexrazoxane. Cancer Res. 67:8839–8846. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Stronach EA, Alfraidi A, Rama N, Datler C,
Studd JB, Agarwal R, Guney TG, Gourley C, Hennessy BT, Mills GB, et
al: HDAC4-regulated STAT1 activation mediates platinum resistance
in ovarian cancer. Cancer Res. 71:4412–4422. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Patterson SG, Wei S, Chen X, Sallman DA,
Gilvary DL, Zhong B, Pow-Sang J, Yeatman T and Djeu JY: Novel role
of Stat1 in the development of docetaxel resistance in prostate
tumor cells. Oncogene. 25:6113–6122. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Zhu H, Wang Z, Xu Q, Zhang Y, Zhai Y, Bai
J, Liu M, Hui Z and Xu N: Inhibition of STAT1 sensitizes renal cell
carcinoma cells to radiotherapy and chemotherapy. Cancer Biol Ther.
13:401–407. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Suzuki K, Yokoi A, Yoshida K, Suzuki H,
Kitagawa M, Asano-Inami E, Matsuo S, Yoshihara M, Tamauchi S,
Yoshikawa N, et al: Overcoming platinum-resistant ovarian cancer
targeting the activated JAK-STAT pathways via extracellular
vesicles. Commun Biol. 8:13052025. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Damen MPF, van Rheenen J and Scheele C:
Targeting dormant tumor cells to prevent cancer recurrence. FEBS J.
288:6286–6303. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
DeMichele A, Clark AS, Shea E, Bayne LJ,
Sterner CJ, Rohn K, Dwyer S, Pan TC, Nivar I, Chen Y, et al:
Targeting dormant tumor cells to prevent recurrent breast cancer: A
randomized phase 2 trial. Nat Med. 31:3464–3474. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Li X, Lu F, Zhou J, Li X, Li Y, Ye W, Li
J, Yang L, Tang S, Zhou Y, et al: IFNγ augments TKI efficacy by
alleviating protein unfolding stress to promote GSDME-mediated
pyroptosis in hepatocellular carcinoma. Cell Death Dis. 16:5122025.
View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Cui C, Xu C, Yang W, Chi Z, Sheng X, Si L,
Xie Y, Yu J, Wang S, Yu R, et al: Ratio of the interferon-γ
signature to the immunosuppression signature predicts anti-PD-1
therapy response in melanoma. NPJ Genom Med. 6:72021. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Llop S, Plana M, Tous S, Ferrando-Díez A,
Brenes J, Juarez M, Vidales Z, Vilajosana E, Linares I, Arribas L,
et al: Salvage chemotherapy after progression on immunotherapy in
recurrent/metastatic squamous cell head and neck carcinoma. Front
Oncol. 14:14584792024. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Reverdy T, Varnier R, de Talhouet S,
Duplomb S and Bruyas A: Analysis of the benefit of salvage
chemotherapy after progression on nivolumab in patients with
squamous cell carcinoma of the head and neck. Oral Oncol.
145:1065332023. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Gaughan EM and Horton BJ: Outcomes from
cytotoxic chemotherapy following progression on immunotherapy in
metastatic melanoma: An institutional Case-series. Front Oncol.
12:8557822022. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Abdelhamid MS, Wadan AS, Saad HA,
El-Dakroury WA, Hageen AW, Mohammed DH, Mourad S, Mohammed OA,
Abdel-Reheim MA and Doghish AS: Nanoparticle innovations in
targeted cancer therapy: Advancements in Antibody-drug conjugates.
Naunyn Schmiedebergs Arch Pharmacol. 398:6369–6389. 2025.
View Article : Google Scholar : PubMed/NCBI
|