Introduction
Mantle cell lymphoma (MCL) is an uncommon yet
distinct entity accounting for approximately 3–6% of all
non-Hodgkin lymphoma cases (1–3). It
was added to the Revised European-American Classification of
Lymphoid Neoplasms in 1994, two years after the name was coined by
Banks and colleagues (4). It is
characterized by a poor patient prognosis with a reported median
overall survival (OS) of only 30–43 months (1,2,5).
In 2008, Hoster et al developed the Mantle
Cell Lymphoma International Prognostic Index (MIPI) as the first
prognostic index specific to patients with advanced stage MCL
(6). The prognostic index is based
on four independent factors: age, performance status, lactate
dehydrogenase (LDH) and leukocyte count. Cell proliferation (Ki-67)
was exploratively analyzed as an important biological marker and
showed strong additional prognostic relevance. Using data from
patients treated in clinical trials, the authors described the
simplified prognostic index, which yielded high concordance
(weighted κ=0.79) and good separation of the overall survival
curves. However, no independent study is currently available to
validate this index in routine clinical practice. We, therefore,
retrospectively applied MIPI to our MCL patients.
Materials and methods
This was a retrospective study. All consecutive MCL
patients treated in Weston Park Hospital from 1981 to 2008 were
included. The patient population was obtained from a dedicated
Lymphoma Database.
The four prognostic factors assessed were: age,
performance status, LDH and leukocyte count. Simplified MIPI was
applied to stratify patients into low- (score 0–3), intermediate-
(score 4–5) or high-risk (score 6–11) groups (Table I). Survival was calculated from the
date of diagnosis. The Kaplan-Meier survival curves were calculated
for the three risk groups and compared using the log-rank test for
trend.
 | Table IThe simplified Mantle Cell Lymphoma
International Prognostic Index was used to stratify patients into
risk groups according to the four prognostic factors. |
Table I
The simplified Mantle Cell Lymphoma
International Prognostic Index was used to stratify patients into
risk groups according to the four prognostic factors.
| Points | Age | ECOG PS | LDH (ULN) | WBC
(109/l) |
|---|
| 0 | <50 | 0–1 | <0.67 | <6.700 |
| 1 | 50–59 | - | 0.67–0.99 | 6.700–9.999 |
| 2 | 60–69 | 2–4 | 1.0–1.49 | 10.000–14.999 |
| 3 | ≥70 | - | ≥1.5 | ≥15.000 |
Results
Seventy-six patients attended from January 1981 to
July 2008. Only 50 patients had complete data for MIPI scoring. The
median age was 64 years. Thirty-eight of the patients (66%) were
males.
According to the simplified MIPI scoring system, 11
patients (22%) were in low-, 23 (46%) in intermediate- and 16
patients (32%) in high-risk groups.
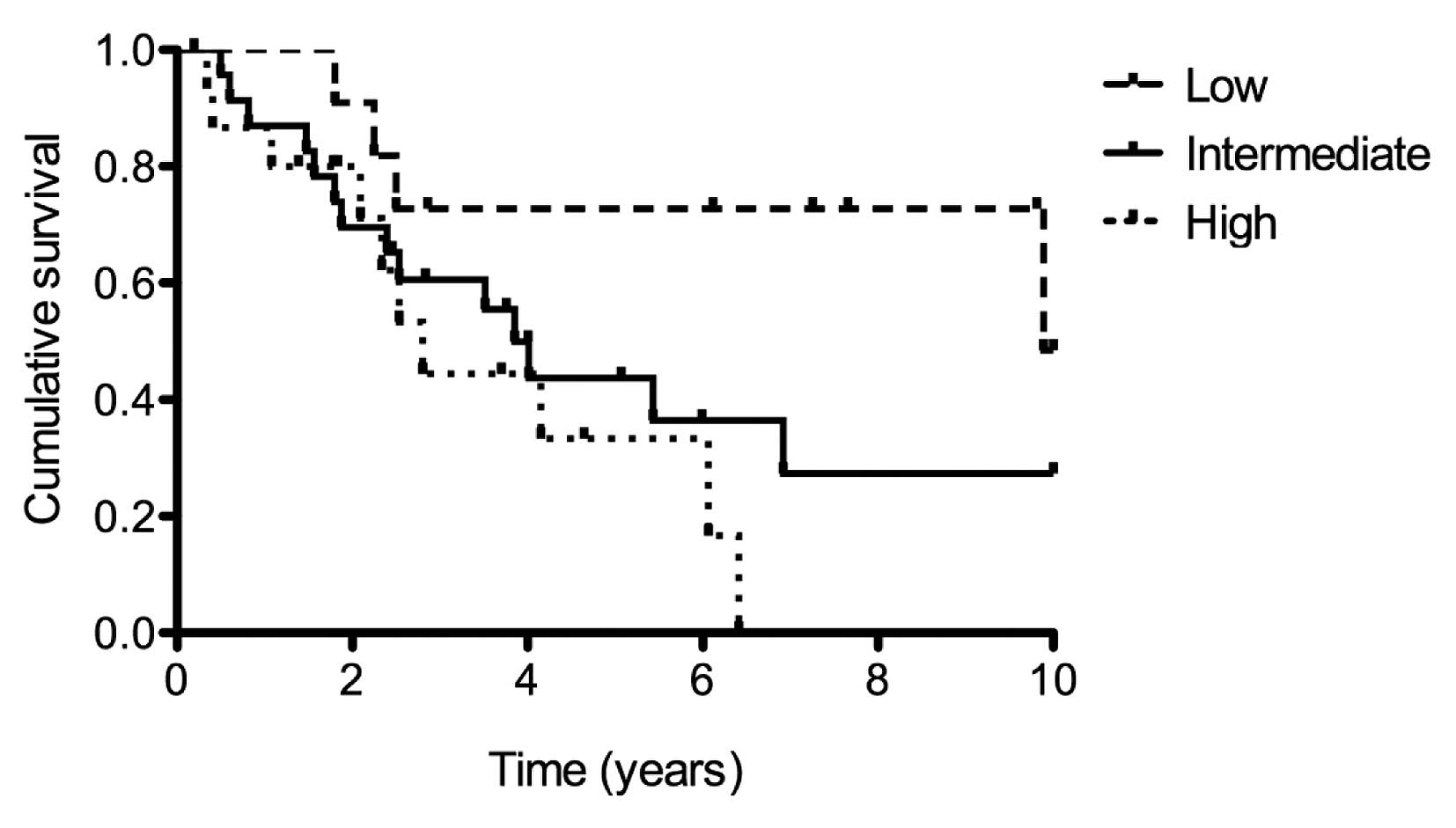
There was a statistically significant trend in
survival across the three groups (p=0.013), with median survival in
the low-, intermediate- and high-risk groups being 9.89, 3.85 and
2.81 years, respectively (Fig. 1).
Each risk group was compared with each of the other two using the
Bonferroni corrected threshold to adjust for multiple comparisons.
Survival time in the high-risk group was statistically
significantly less than in the low-risk group (p=0.0112).
Discussion
Until 2007, there was no generally established
prognostic index for patients with MCL. The International
Prognostic Index (IPI) and Follicular Lymphoma International
Prognostic Index (FLIPI) had been developed for diffuse large
B-cell (DCBCL) and follicular lymphoma patients, respectively. IPI
and FLIPI showed poor separation of survival curves for MCL
patients (6). The IPI score
classifies most patients in the two intermediate-risk groups and
does not separate the outcomes. The FLIPI score places most
patients into the high-risk group and does not separate low from
intermediate in outcome (7). MIPI,
derived using data of 455 advanced stage patients treated within
three clinical trials, proved to be a suitable index for MCL
patients (7).
We retrospectively applied the simplified MIPI to
all of the consecutive patients (for whom full data were available)
referred to our lymphoma service. MIPI proved a valuable guide to
prognosis with a significant trend for difference between low-,
intermediate- and high-risk groups, but in particular low- and
high-risk.
Conventional non-trial treatment for younger
patients with MCL is anthracycline-containing (CHOP-like)
chemotherapy, which in responding patients proceeds to
consolidative intensive chemotherapy with autologous stem cell
rescue (recently with the addition of rituximab). In our series
only 7 patients went on to have high-dose therapy. As expected, in
this selected group, survival was favorable (mean overall survival,
97 months; range, 49–132). Four patients were in the best-risk
group by MIPI. Only 1 patient was in the high-risk group and he had
the shortest survival. On the other hand, Martin et al
reported that it may be possible to select certain asymptomatic
patients with MCL for deferred initial treatment (‘watch and wait’)
(8). When we evaluated our patients
there were 3 who had little or no previous treatment and had better
than expected survival; the 3 patients had low-risk MIPIs.
Evidently there are factors at work other than those
comprising MIPI, and a search for these continues. In the interim,
the index provides us with a reasonable guide to prognosis which
works in unselected cases of mantle cell lymphoma presenting to an
orthodox lymphoma service.
References
|
1
|
Andersen NS, Jensen MK, de Nully Brown P
and Geisler CH: A Danish population-based analysis of 105 mantle
cell lymphoma patients: incidences, clinical features, response,
survival and prognostic factors. Eur J Cancer. 38:401–408. 2002.
View Article : Google Scholar
|
|
2
|
Velders GA, Kluin-Nelemans JC, de Boer CJ,
et al: Mantle cell lymphoma: a population-based clinical study. J
Clin Oncol. 14:1269–1274. 1996.PubMed/NCBI
|
|
3
|
A clinical evaluation of the International
Lymphoma Study Group Classification Project. Blood. 89:3909–3918.
1997.PubMed/NCBI
|
|
4
|
Banks PM, Chan J, Cleary ML, et al: Mantle
cell lymphoma. A proposal for unification of morphologic,
immunologic and molecular data. Am J Surg Pathol. 16:637–640. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Argatoff LH, Connors JM, Klasa RJ, et al:
Mantle cell lymphoma: a clinicopathologic study of 80 cases. Blood.
89:2067–2078. 1997.PubMed/NCBI
|
|
6
|
Hoster E, Dreyling M, Klapper W, et al: A
new prognostic index (MIPI) for patients with advanced-stage mantle
cell lymphoma. Blood. 111:558–565. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Smith MR: Mantle cell lymphoma: advances
in biology and therapy. Curr Opin Haematol. 15:415–421. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Martin P, Chadburn A, Christos P, et al:
Outcome of deferred initial therapy in mantle cell lymphoma. J Clin
Oncol. 27:1209–1213. 2009. View Article : Google Scholar : PubMed/NCBI
|