Introduction
Serous microcystic adenomas are rare and account for
1–2% of all the exocrine pancreatic tumors and 25% of all
pancreatic cystic neoplasms. Due to advances in imaging techniques,
these adenomas have been identified at an increasing frequency. The
tumors usually occur in the elderly in the seventh to eighth decade
of life (range 34–91 years; mean age 66) (1,2). A
female preponderance has been noted (70% of the tumors occur in
women). According to the literature, these tumors range in size
from 1–26 cm, with an average of 6–10 cm (1,2,3). Since
serous cystic adenomas are considered to be benign tumors with
almost no potential for malignant transformation, surgery is
usually not recommended. However, recent reports have suggested a
small but finite risk of malignancy for serous cystic neoplasms of
the pancreas (4). In this case,
assessment of the relationship between the tumor and adjacent
vascular structures, such as the massive drainage veins on the
surface or tumor flow into the portal and superior mesenteric vein
(SMV) as well as the celiac and superior mesenteric arteries (SMA),
was considered to be critical for the preoperative determination of
tumor resectability. The risk of massive intraoperative hemorrhage
was felt to be considerable, given the extent of the veins on the
surface of the tumor, as well as the size and location of the
primary pancreatic mass.
In this study a case of large and hypervascular
serous microcystic adenoma of the pancreatic head was successfully
resected with the preoperative embolization of the feeding
arteries.
Case report
A 63-year-old woman visited her general practitioner
in 1999 owing to a gastric deformity detected by routine upper
gastrointestinal endoscopy. An abdominal computed tomography scan
revealed a cystic lesion measuring 6.0 cm in diameter, and the
tumor was diagnosed as a serous microcystic adenoma of the
pancreatic head. During the follow-up, the tumor increased steadily
in size, measuring 6.0 cm in diameter in 1999 and 13.0 cm in 2008,
while remaining asymptomatic throughout this time period. The risk
of malignant transformation is believed to be low even in the
long-term (5). However, some cases
of malignant transformation to serous cystadenocarcinoma have been
reported (4). Since the tumor was
large, the patient was considered to be at risk of developing
obstructive jaundice, duodenal stenosis, portal thrombosis or
rupture of the tumor, and a tumor resection was performed. On
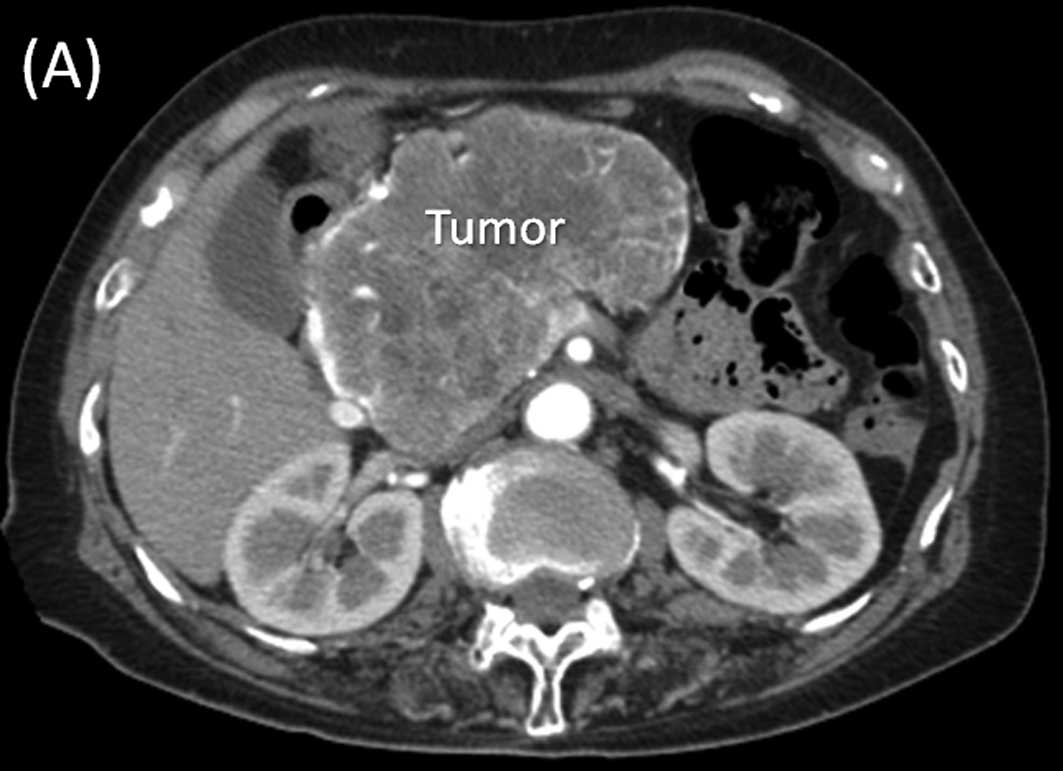
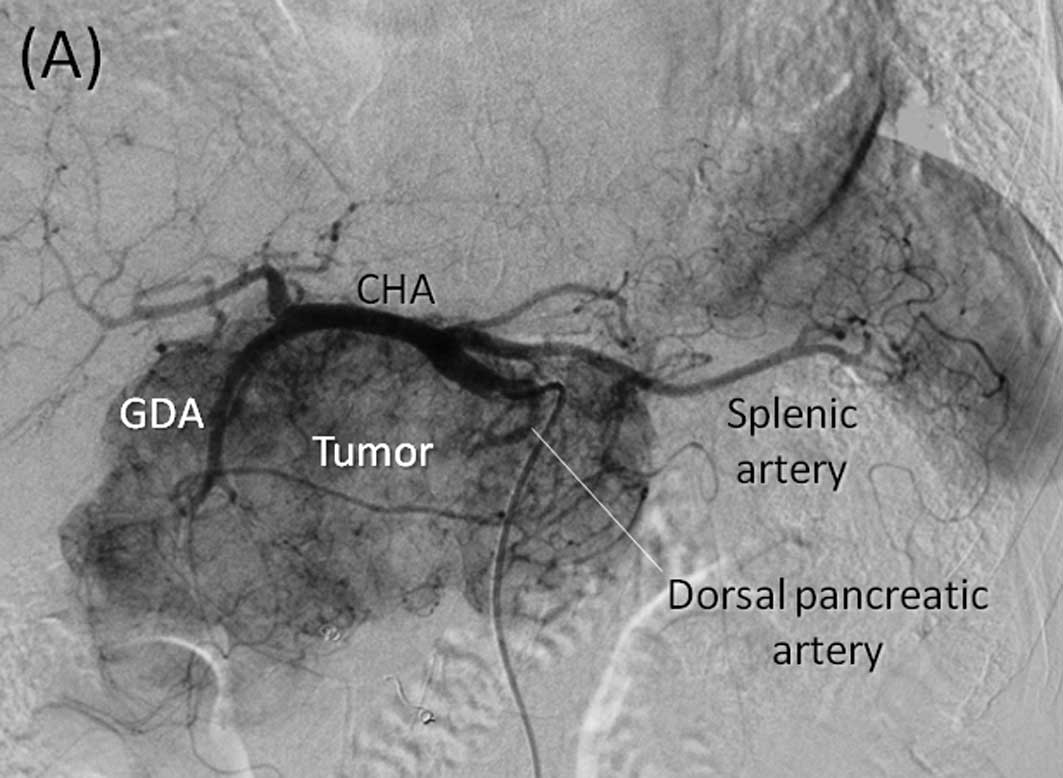
multi-detector row (MD) computed tomography scan (Fig. 1) and angiography (Fig. 2), numerous feeding arteries
(including gastroduodenal, right gastric, splenic, dorsal
pancreatic and inferior pancreatoduodenal arteries) were found to
supply blood to the tumor, and the common hepatic artery was
stretched widely across the upper surface of the tumor. Moreover,
several enlarged draining veins were found on the surface of the
tumor, and drainage of these veins into the portal vein (PV) and
SMV was observed. In the current case, although resection was
deemed to be feasible, the risk of massive intraoperative
hemorrhage was felt to be considerable. Therefore, preoperative
embolization of the tumor-feeding arteries from the celiac axis
(gastroduodenal, splenic and dorsal pancreatic arteries) was
performed, with the tumor resection performed on the following
day.
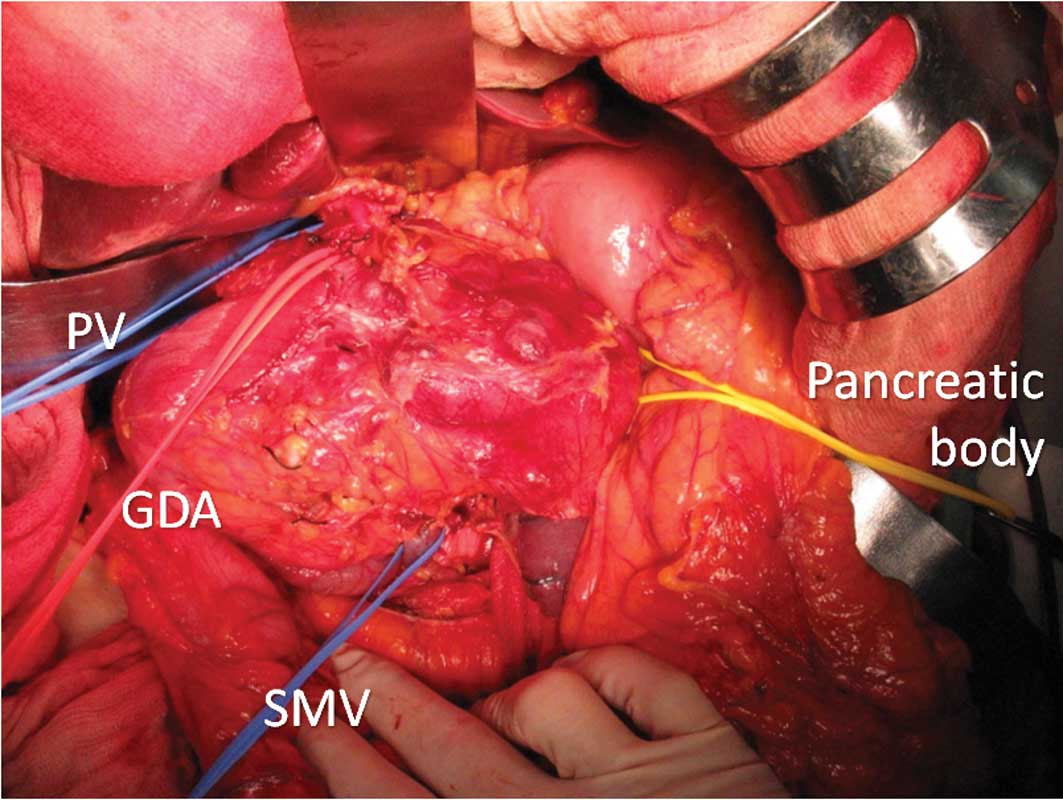
Laparotomy (Fig. 3)
showed a large multicystic tumor arising from the pancreatic head,
with numerous vessels on its surface. The distal duodenum or
proximal jejunum at the ligament of Treitz was torn from the
retroperitoneum, and the SMA was identified. The root of the
inferior pancreatoduonenal (IPDA) was detected and the vessel was
resected. The right gastric and gastroepiploic arteries were then
resected. At this point, owing to preoperative embolization, the
blood supply to the tumor was completely arrested and the tumor had
a slightly deflated appearance. As a result, the common and proper
hepatic arteries that had been in tight contact with the superior
surface of the tumor were detached and the gastroduodenal artery
was resected. The pancreatic body was cut at the left side of the
tumor with the requisite surgical margin. While we attempted to
preserve the PV, splenic vein (SpV) and SMV, several drainage veins
on the surface of the tumor were found to drain into the SMV and
PV, and the tumor was tightly adherent to the SMV and PV.
Therefore, the SMV-PV was resected and reconstructed by end-to-end
anastomosis. The estimated blood loss was 570 ml. The tumor surgery
with pancreaticoduodenectomy was performed without a blood
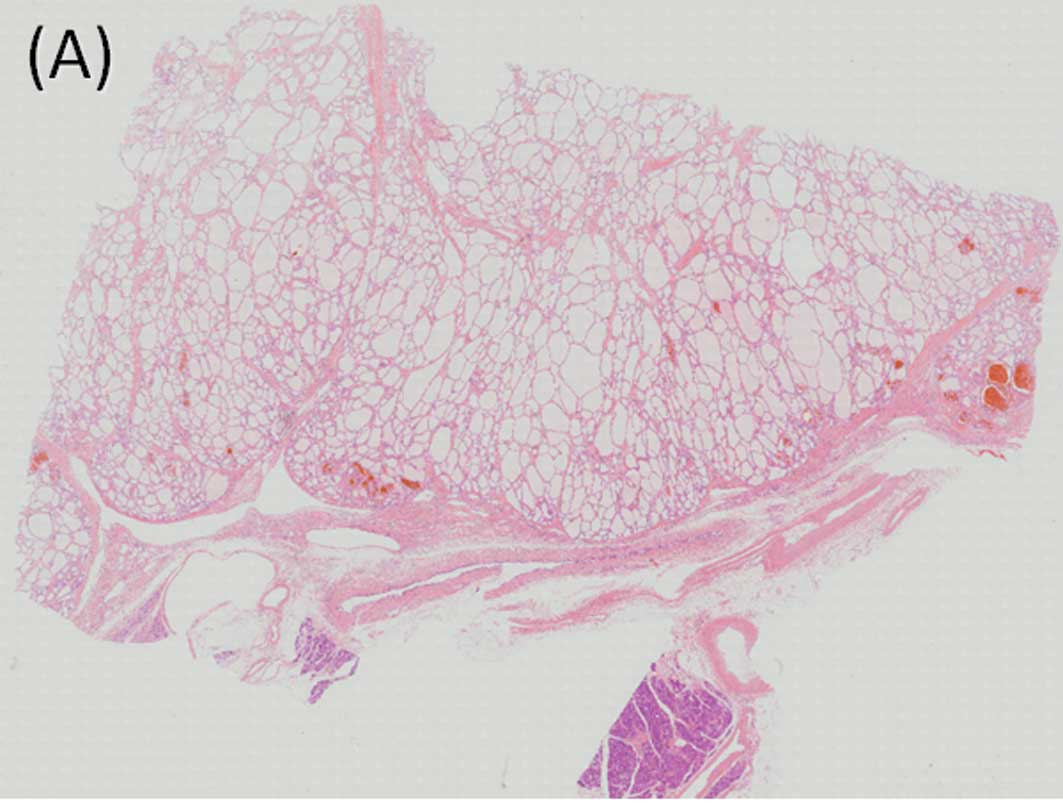
transfusion. The final pathology confirmed the diagnosis of serous
microcystic adenoma (Fig. 4).
Pathological examination of the resected specimen revealed arterial
thrombosis due to the preoperative tumor embolization. However, no
ischemic or necrotic changes occurred in the tumor. The
postoperative course was uneventful, and the patient is currently
alive and disease-free. The patient gave her informed consent, and
consent and approval for the study was obtained by the Ethics
committee.
Discussion
Cystic pancreatic neoplasms are uncommon.
Differentiation between serous cystic tumors and mucinous neoplasms
is crucial, due to the radically different biological
characteristics of the two types of neoplasms (6,7).
Mucinous cystic neoplasms should always be resected due to their
premalignant nature and strong tendency towards malignant
transformation (7). Management of
serous tumors is more controversial since serous microcystic
adenomas are considered to be tumors with almost no potential for
malignant transformation. Thus, surgery is usually not recommended.
However, during the follow-up of our case, the tumor increased
steadily in size, from 6.0 cm to 13.0 cm in diameter from 1999 to
2008. The risk of malignant transformation has been reported to be
low, even in the long-term. However, some cases of malignant
transformation to serous cystadenocarcinoma were recently reported
(4). A case of serous cystic
adenoma that increased in size, over a follow-up period of more
than 20 years, eventually producing duodenal and colonic stenosis
and portal hypertension was reported in 2007 (5). If these symptoms were to appear and
surgery was to become necessary in the future, the patient would be
much older. Therefore, tumor resection was performed.
In the current case, although resection was deemed
to be feasible, the risk of massive intraoperative hemorrhage was
felt to be considerable given the extent of the feeding arteries
and massive drainage veins, as well as the size and location of the
primary pancreatic mass. Preoperative arterial embolization was
previously shown to be a safe and efficacious tumor decompression
technique (8,9,10). On
the other hand, embolization of the feeding arteries has also been
reported to cause ischemia, necrosis, inflammation and angiogenesis
of the tumor. Therefore, arterial embolization was performed on the
day prior to surgery for some of the arteries that were located
behind the tumor and were potentially difficult to approach during
surgery.
To improve prognosis, radical
pancreaticoduodenectomy is usually performed and involves wide
lymph node dissection and complete removal of the extrapancreatic
nerve plexus of the SMA for patients with carcinoma of the
pancreatic head (11,12,13).
Additionally, SMA is approached from the distal duodenum to
proximal jejunum at the ligament of Treitz in front of the vena
cava, behind the anterior renal (subperitoneal) fissure. We
approached the SMA and resected the IPDA using the same technique
as that during surgery for cancer of the pancreatic head. This
paraduodenal approach allowed for early evaluation of the SMA.
Preoperative partial embolization of the tumor-feeding arteries and
intraoperative resection of the IPDA and right gastric artery
resulted in the arrest of the tumor blood supply without
preoperative tumor necrosis. Thus, blood loss was reduced.
Advances in imaging techniques have led to the
identification of serous microcystic adenomas of the pancreas. The
excellent prognosis associated with serous microcystic adenoma
justifies an aggressive approach to surgical resection, even in
older patients, especially since major pancreatic resections are
now performed with very low mortality and morbidity rates at
leading centers around the world. In conclusion, preoperative
partial embolization of the feeding arteries is useful for
resection of hypervascular large tumors of the pancreas. Only by
utilizing multi-modality imaging, interventional radiology
techniques and surgery can these complex patients be managed
successfully.
References
|
1
|
Tampi C, Mullerpatan P, Shah R, Jagannath
P and Zimmermann A: Microcystic serous cystadenoma of the pancreas:
a case report of two cases with one of diffuse presentation.
Pancreatology. 6:248–253. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Vernadakis S, Kaiser GM, Christodoulou E,
Mathe Z, Troullinakis M, Bankfalvi A and Paul A: Enormous serous
microcystic adenoma of the pancreas. J Pancreas. 10:332–334.
2009.PubMed/NCBI
|
|
3
|
Omeroglu A, Paner GP, Ciesla MC and Harman
G: Serous microcystic adenoma of the pancreas. Arch Pathol Lab Med.
125:1613–1614. 2001.PubMed/NCBI
|
|
4
|
King JC, Ng TT, White SC, Cortina G, Reber
HA and Hines OJ: Pancreatic serous cystadenocarcinoma: a case
report and review of the literature. J Gastrointest Surg.
13:1864–1868. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schulz HU, Kellner U, Kahl S, Effenberger
O, Asperger W, Lippert H and Röcken C: A giant pancreatic serous
microcystic adenoma with 20 years follow-up. Langenbecks Arch Surg.
392:209–213. 2007.PubMed/NCBI
|
|
6
|
Box JC and Douglas HO: Management of
cystic neoplasms of the pancreas. Am Surgeon. 66:495–501.
2000.PubMed/NCBI
|
|
7
|
Sarr MG, Kendrick ML, Nagomey DM, Thompson
GB, Farley DR and Farnell MB: Cystic neoplasms of the pancreas:
benign to malignant epithelial neoplasms. Surg Clin North Am.
81:497–509. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Adams DB, Mauterer DJ, Vujic IJ and
Anderson MC: Preoperative control of splenic artery inflow in
patients with splenic venous occlusion. South Med J. 83:1021–1024.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Umeda Y, Yagi T, Sadamori H, et al:
Preoperative proximal splenic artery embolization: a safe and
efficacious portal decompression technique that improves the
outcome of liver donor liver transplantation. Transpl Int.
20:947–955. 2007. View Article : Google Scholar
|
|
10
|
Joyce DL, Hong K, Fishman EK, Wisell J and
Pawlik TM: Multi-visceral resection of pancreatic VIPoma in a
patient with sinistral portal vein hypertension. World J Surg
Oncol. 6:80–86. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nagakawa T, Kurachi M, Konishi K, et al:
Translateral retroperitoneal approach in radical surgery for
pancreatic carcinoma. Jpn J Surg. 12:229–233. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nagakawa T, Nagamori M, Futakami F, et al:
Result of extensive surgery for pancreatic carcinoma. Cancer.
77:640–645. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Noto M, Miwa K, Kitagawa H, et al:
Pancreas head carcinoma. Frequency of invasion to soft tissue
adherent to the superior mesenteric artery. Am J Surg Pathol.
29:1056–1061. 2005.PubMed/NCBI
|