Introduction
Squamous cell carcinoma (SCC) occurs most frequently
in the oral and maxillofacial region, and its metastatic ability
conveys a poor prognosis. The standard treatment for oral cancer is
a combination of surgery, radiation, and chemotherapy. Better
insight into the mechanisms of progression of this cancer, of which
one major issue is metastasis, is clearly needed, and discovery of
novel molecular targets to assist the development of new
therapeutic strategies is vital. Metastasis is a multi-step process
by which primary tumor cells invade adjacent tissues, enter the
systemic circulation (intravasate), translocate through the
vasculature, arrest in distant capillaries, extravasate into the
surrounding tissue parenchyma, and finally proliferate from a tiny
cell mass into large secondary tumors in a foreign environment
(1). In the past decade, studies
have been carried out to investigate the genes and gene products
that drive the metastatic process. Many molecules have been
identified, some of which are involved in primary tumor-specific
and target tissue-specific manners (2,3).
Determination of the molecules involved in oral SCC metastasis is
necessary.
Signal transduction by the epidermal growth factor
(EGF) family of ligands has been demonstrated to promote
tumorigenesis and metastasis (4,5).
Several studies using EGF receptor (EGFR) inhibitors have indicated
that EGF/EGFR signaling mediates osteolytic bone metastasis of
breast, prostate, and kidney cancers (6). Heparin-binding epidermal growth
factor-like growth factor (HB-EGF) contributes to cell adhesion,
invasion, and angiogenesis associated with transcoelomic metastasis
in ovarian cancer (7). In addition,
HB-EGF was identified as one of the mediators of cancer cell
passage through the blood-brain barrier during metastasis (3). These findings suggest that HB-EGF is
important in several metastatic processes.
HB-EGF is initially synthesized as a transmembrane
protein, similar to other members of the EGF family. The
membrane-anchored form of HB-EGF (pro-HB-EGF) is cleaved at the
cell surface by a protease to yield the soluble form (s-HB-EGF);
this process is known as ectodomain shedding (8,9).
s-HB-EGF has potent mitogenic and chemoattractant activities for a
number of cell types (10). In many
cases, s-HB-EGF released from cancer cells is involved in oncogenic
transformation, tumor invasion, and metastasis (11,12).
Although it is interesting whether HB-EGF affects oral SCC
metastasis, there is limited evidence supporting their
relation.
The present study examined whether HB-EGF affects
metastasis in oral SCC. The results indicate that when HB-EGF is
overexpressed in oral SCC cells, s-HB-EGF is released by shedding
and subsequently increases invasion activity through upregulation
of MMP-9 downstream of EGFR, in an autocrine manner.
Materials and methods
Reagents
Recombinant human HB-EGF was purchased from Wako
Pure Chemical Industries, Ltd. TAPI-2 and AG1478 were purchased
from Calbiochem.
Cell culture and RNA extraction
The human tongue squamous cell carcinoma cell line
HSC3 was obtained from the Human Science Research Resource Bank
(Osaka, Japan). HSC3 cells were grown as monolayers in Dulbecco’s
modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine
serum (FBS) in humidified 5% CO2 in air at 37°C in a
CO2 incubator (Sanyo, Japan). Total-RNA was isolated
using a Qiagen RNeasy mini kit (Qiagen) or TRIzol reagent
(Invitrogen, Carlsbad, CA), according to the manufacturer’s
instructions.
Real-time quantitative PCR and reverse
transcription-PCR
First-strand cDNA synthesis was performed using 2 μg
of total-RNA and TaqMan reverse transcription reagents (Roche) for
real-time PCR, and using 1 μg of total-RNA and SuperScript III for
reverse transcription-PCR, following the manufacturer’s
instructions. The TaqMan quantitative PCR reaction was carried out
using the following oligonucleotide primers: β-actin (forward
5′-AAACTGGACGGTGGAGGT-3′ and reverse 5′-AG AGAAGTGGGGTGGCTTTT-3′);
amphiregulin (forward 5′-GA GAAGCTGAGGAACGAAAGAA-3′ and reverse
5′-AGGACC GACTCATCATTTATGG-3′); epigen (forward 5′-GCCCTATA
ATGTGTCAGGCACT-3′ and reverse 5′-GAAGGCAAATTTT TACCACTCG-3′);
epiregulin (forward 5′-GAGAAGGGGGA GTAATGACTTG-3′ and reverse
5′-AAGTGCAATTACAGA GTGCAAAA-3′); HB-EGF (forward 5′-GGAACTCACTTTC
CCTTGTGTC-3′ and reverse 5′-CTCAGCCTTTTGCTTT GCTAAT-3′); TGF-α
(forward 5′-GAAGGAGGAATGACTCA AATGC-3′ and reverse
5′-AAGCCTGGTAAATCAATGG CTA-3′); betacellulin (forward
5′-GAATGTGTCTCAGGAA AAACAGC-3′ and reverse 5′-TGTTGCTACCTAACCAGT
TGCT-3′); EGF (forward 5′-TTGGGACAACAGTGCTTTG TAA-3′ and reverse
5′-CTGACCAAACCAGTGTGACTGT-3′). Experiments were performed
independently in triplicate. To examine the expression of MMP-9,
β-actin and GAPDH, reverse transcription-PCR analysis was carried
out using primers specific for MMP9 (forward 5′-GTGCTCCTGGTGC
TGGGCTG-3′ and reverse TCCAGCTCACCGGTCTCGGG); β-actin (forward
5′-GAAAATCTGGCACCACACCTT-3′ and reverse
5′-TTGAAGGTAGTTTCGTGGAT-3′); GAPDH (forward
5′-ACAGTCAGCCGCATCTTCTT-3′ and reverse
5′-TGGAAGATGGTGATGGGATT-3′).
RNA interference
HSC3 cells were transfected with HB-EGF siRNA oligos
(sense 5′-GGACCCAUGUCUUCGGAAA-3′ and antisense
5′-UUUCCGAAGACAUGGGUCC-3′) or control scrambled siRNA oligos (sense
5′-AUCCGCGCGAU AGUACGUA-3′ and antisense 5′-UACGUAGUAUCGCGCG
GAU-3′) (B-Bridge International, Mountain View, CA) using
Lipofectamine™ RNAiMAX (Invitrogen) according to the manufacturer’s
instructions, followed by incubation for 48 h at 37°C in a
humidified atmosphere of 5% CO2 in air.
Cell proliferation assay
Cell proliferation was assessed using a
3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide (MTT)
assay at three time points, Days 1, 2 and 3 after seeding. MTT
reagent (50 μl) was added to each well, and the plates were
incubated for 1 h at 37°C. After the reaction, 500 μl of
isopropanol containing 0.04 N HCl were added to each well. The
reactions were transferred to a 96-well plate, and the absorbance
was measured at a test wavelength of 570 nm and reference
wavelength of 630 nm with a microplate reader (Model 680;
Bio-Rad).
In vitro cell invasion assay
Cell invasion assays were performed according to the
manufacturer’s instructions. Briefly, cells (2×104/well)
were seeded in a 6-well BioCoat Matrigel Invasion Chamber
(Becton-Dickinson, Bedford, MA) in DMEM containing 10% (v/v)
heat-inactivated FBS. After 48 h of incubation, non-invading cells
were removed from the upper surface of the membrane by scrubbing,
and the membrane was stained using a Diff-Quik staining kit.
Invading cells were counted under a microscope, and the invasion
index (= cells migrating through Matrigel-coated membrane/cells
migrating through control insert membrane) was determined.
Zymogram
After cells had been incubated in serum-free medium
for 48 h, the conditioned medium was collected for zymography.
Samples were diluted in SDS-polyacrylamide gel electrophoresis
(SDS-PAGE) sample buffer and electrophoresed in 12.5%
polyacrylamide gels containing gelatin (0.1%), at 60 mA for 2 h at
4°C. The gels containing the separated sample proteins were
incubated overnight in 0.05 M Tris/HCl (pH 7.5) containing 10 M
CaCl2, then stained with Coomassie Blue (0.25%), and
de-stained in methanol/acetic acid/water (50:10:40).
Statistical analysis
The Mann-Whitney U test was used to assess the
statistical significance of differences between samples. P-values
<0.05 were considered to indicate statistical significance.
Results
HB-EGF is associated with the invasion
potential of oral SCC HSC3 cells
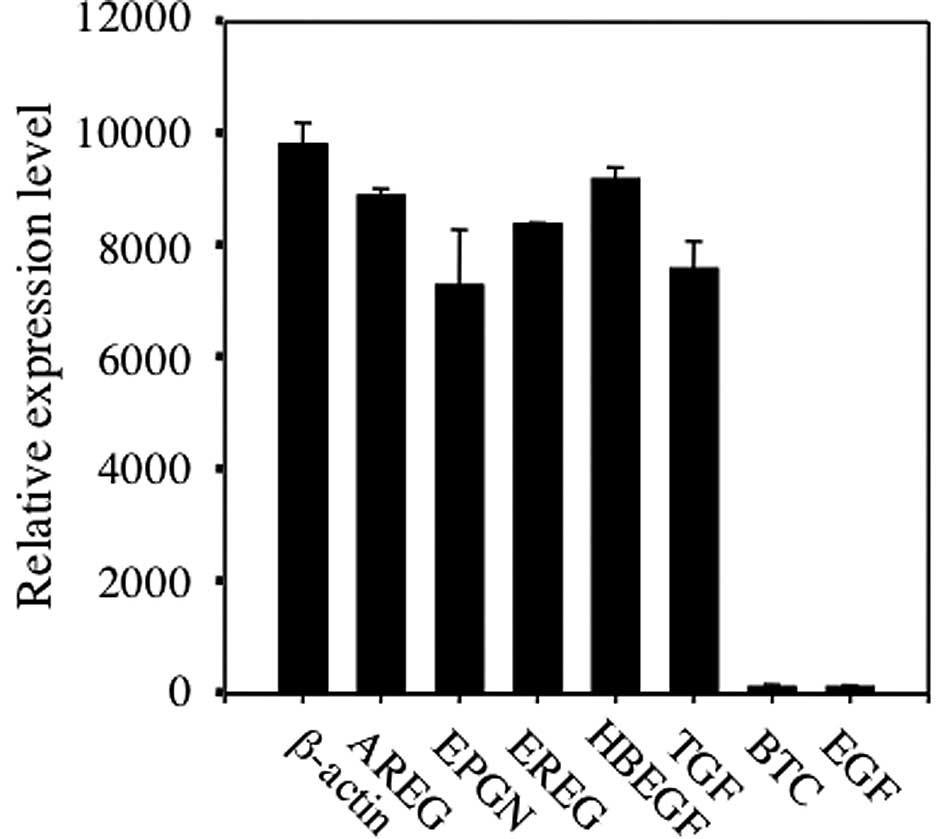
Expression of EGF family mRNA in HSC3 cells was
analyzed by real-time RT-PCR. The expression levels of HB-EGF were
high in HSC3 cells (Fig. 1). In
addition, high expression levels of amphiregulin (AREG), epigen
(EPGN), epiregulin (EREG), and TGF-α mRNA were detected, but
betacellulin (BTC) and EGF mRNA were not highly expressed (Fig. 1).
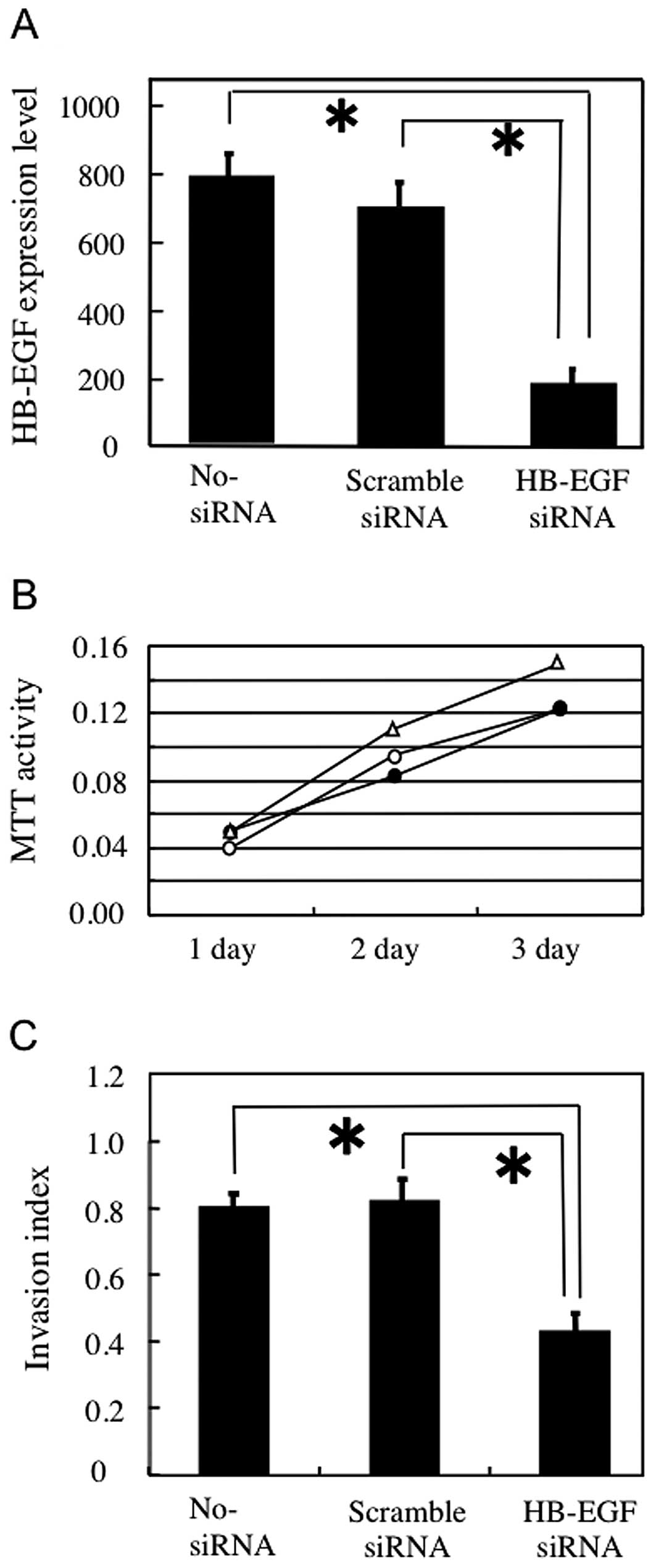
To determine the role of HB-EGF in oral SCC cells,
we performed HB-EGF knockdown using siRNA in HSC3 cells with high
HB-EGF expression. Cells treated with oligofectamine reagent only
(no-siRNA) and cells treated with scrambled siRNA were used as
controls for non-specific effects. The HB-EGF mRNA expression level
did not differ significantly between the scrambled siRNA and
no-siRNA transfectants, but HB-EGF mRNA expression was obviously
reduced in the HB-EGF siRNA transfectants (Fig. 2A). As HB-EGF has been shown to
stimulate growth in a variety of cells (13), the effect of HB-EGF siRNA treatment
on HSC3 cell proliferation was analyzed by the MTT assay. After 1,
2 and 3 days of culture, there was no difference in MTT activity
between HSC3 cells transfected with HB-EGF siRNA and cells
transfected with scrambled siRNA (Fig.
2B). Furthermore, no difference in cell density was observed
among the three treatments (data not shown). These data indicate
that HB-EGF had no effect on HSC3 cell proliferation.
The effect of HB-EGF siRNA treatment on the invasion
potential of HSC3 cells was analyzed by a Matrigel invasion assay.
Invasion activity did not differ between the no-siRNA and scrambled
siRNA transformants, whereas transfection with HB-EGF siRNA
significantly decreased the number of invasive HSC3 cells (Fig. 2C). These results suggest that HB-EGF
is associated with the invasion activity of HSC3 cells.
Secreted HB-EGF is associated with the
MMP-9 level in HSC3 cells
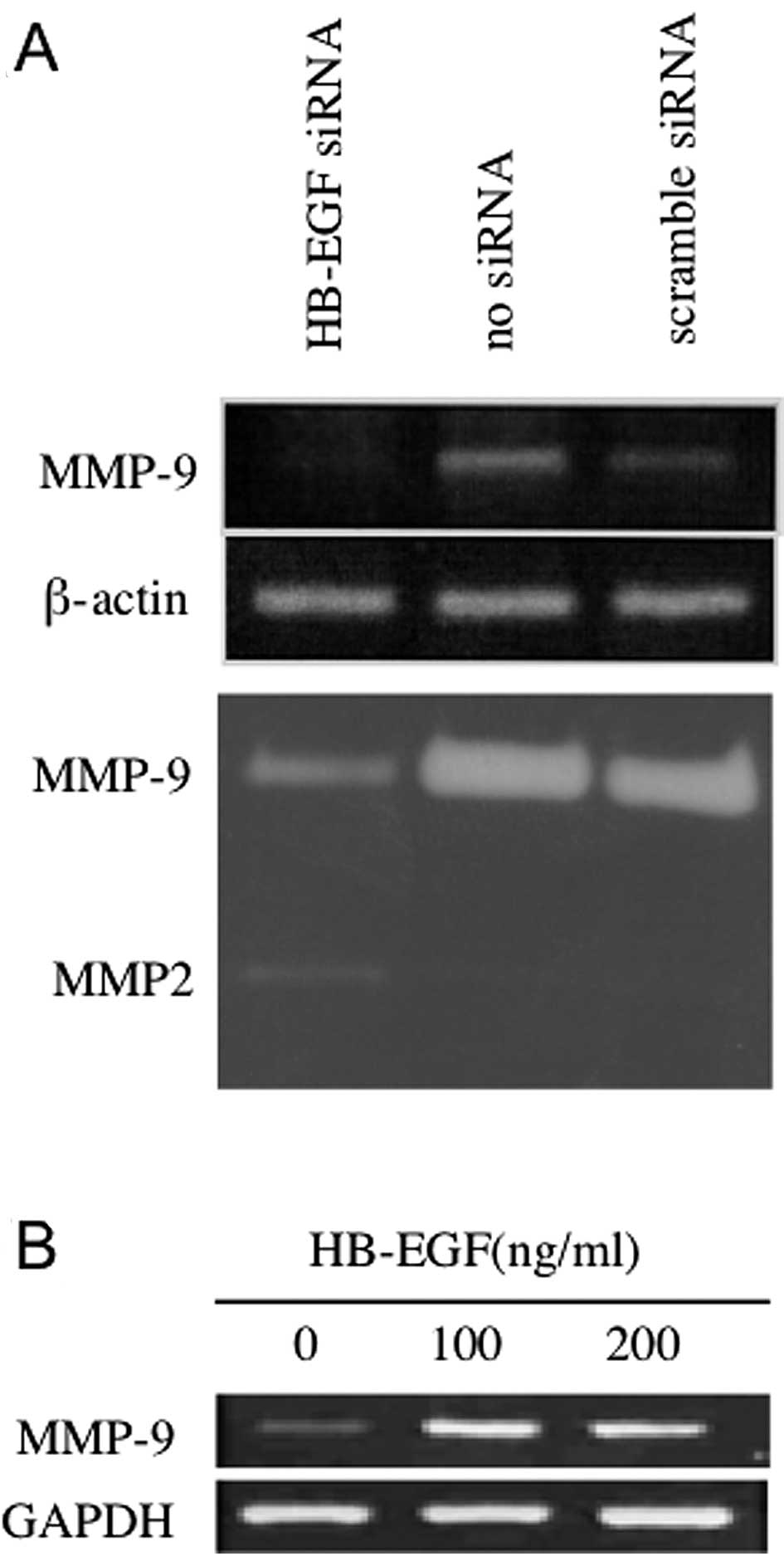
Secreted and activated MMPs, including MMP-2 and
MMP-9, degrade a variety of extracellular matrix macromolecules and
thus facilitate cell invasion (14). The effects of HB-EGF siRNA treatment
on the MMP-9 mRNA level and collagenase activity were determined by
semi-quantitative RT-PCR and zymography, respectively. The MMP-9
mRNA level and collagenase activity were lower in HSC3 cells
treated with HB-EGF siRNA compared with the control cells (Fig. 3A), suggesting that HB-EGF
synthesized in HSC3 cells upregulates MMP-9 mRNA expression. To
examine whether soluble HB-EGF upregulates MMP-9 mRNA levels in
HSC3 cells, we added soluble HB-EGF to the culture medium and
assessed the MMP-9 mRNA level by RT-PCR. The added HB-EGF induced
MMP-9 mRNA expression (Fig. 3B),
indicating that HB-EGF released from HSC3 cells upregulates MMP-9
in HSC3 cells in an autocrine manner.
HB-EGF is shed and activates EGFR on HSC3
cells
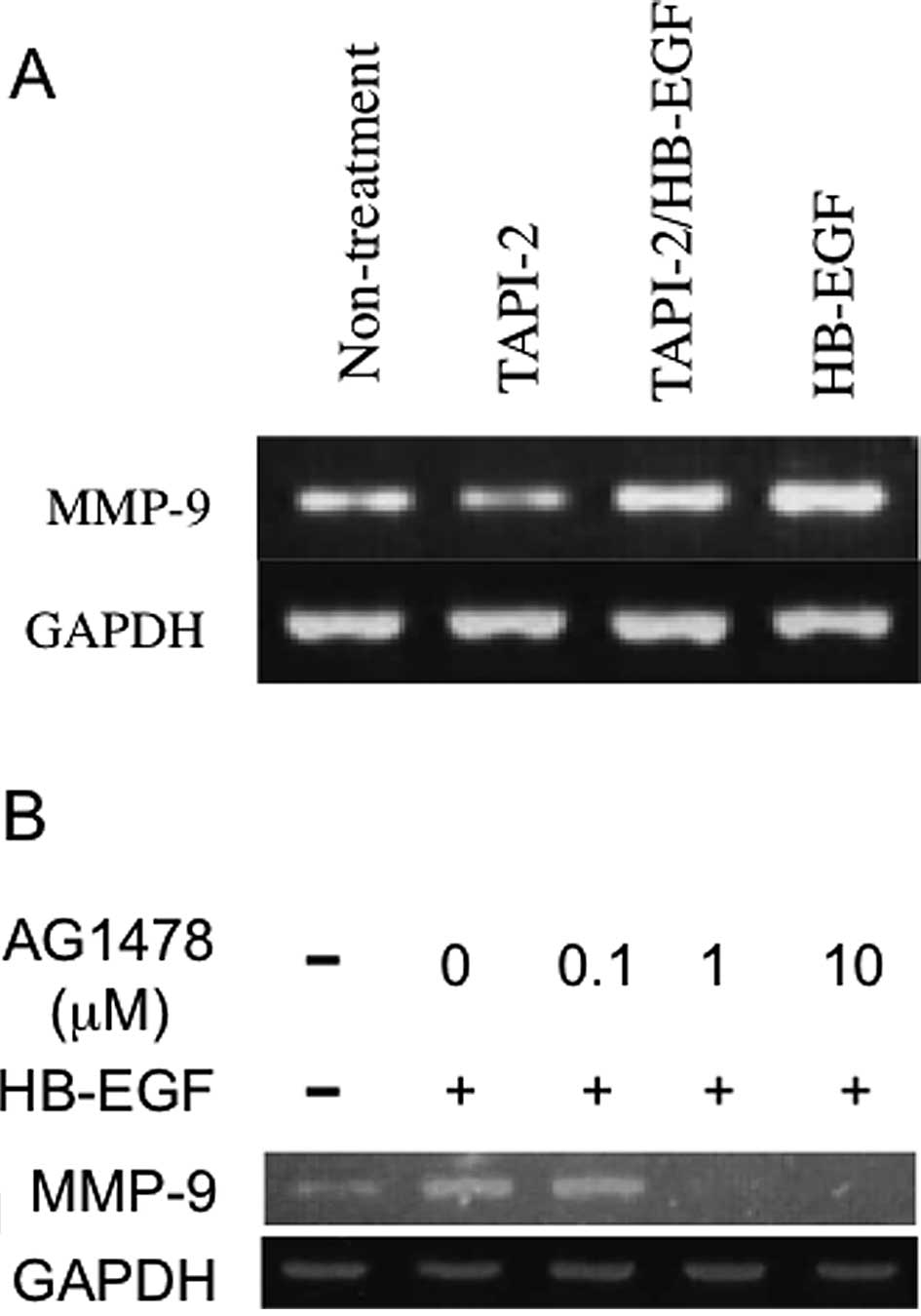
HB-EGF is initially synthesized as a membrane-bound
precursor (pro-HB-EGF), which is subsequently cleaved by a membrane
sheddase. The cleaved ectodomain plays several roles as a soluble
factor (s-HB-EGF). To assess the involvement of the candidate
sheddase ADAM17, we analyzed the MMP-9 mRNA level in HSC3 cells
treated with an ADAM17 inhibitor, TAPI-2. The MMP-9 mRNA level was
decreased in HSC3 cells treated with TAPI-2 (Fig. 4A). Furthermore, the addition of
s-HB-EGF to HSC3 cells treated with TAPI-2 resulted in increased
MMP-9 mRNA levels (Fig. 4A),
showing that TAPI-2 did not act by inhibiting s-HB-EGF. These data
suggest that pro-HB-EGF is cleaved by ADAM17 to release s-HB-EGF,
which stimulates MMP-9 mRNA upregulation in HSC3 cells.
To examine whether s-HB-EGF upregulates MMP-9 mRNA
via EGFR stimulation, we analyzed the effect of the EGFR inhibitor
AG1478 on MMP-9 mRNA levels in HSC3 cells. The addition of AG1478
at concentrations greater than 1 μM reduced the basal level of MMP9
mRNA in HSC3 cells as well as the HB-EGF-induced upregulation of
MMP-9 mRNA (Fig. 4B). Thus,
s-HB-EGF appears to upregulate MMP-9 mRNA expression through the
activation of EGFR.
Discussion
This study provides evidence that HB-EGF acts as an
autocrine EGFR ligand to augment cell invasion activity through
MMP-9 upregulation in the oral SCC cell line HSC3. Similarly, it
has been shown that the invasion ability and MMP-9 levels in
ovarian cancer cells are stimulated by HB-EGF expression (7,11). We
further showed that the EGFR ligands, AREG, EPGN, EREG and TGF-α as
well as HB-EGF are expressed at high levels in HSC3 cells, whereas
EGF and BTC are expressed at low levels. Gastrointestinal stromal
tumors express several EGFR ligands, but not EGF (15). Although EGF can elicit a variety of
biological actions, including the proliferation and differentiation
of epithelial and mesenchymal cells (16), particularly in the embryonic stage
(17), EGFR ligands other than EGF
may play crucial roles in cancer cells.
HB-EGF is initially synthesized as a pro-HB-EGF and
is cleaved at the apical plasma membrane to yield s-HB-EGF
(18–20), which transactivates EGFR in a
variety of cell types (21,22). Ectodomain shedding, the proteolytic
processing of the extracellular domain of pro-HB-EGF to release
s-HB-EGF, is mediated by several membrane-anchored enzymes,
including MMP-2, MMP-3, MMP-9, tumor necrosis factor-α-converting
enzyme/a disintegrin and metalloprotease 17 protease (TACE/ADAM17),
and ADAM10 (19,20,23–26).
In our results, TAPI-2, a specific inhibitor of TACE (27), inhibited HB-EGF activity, indicating
that s-HB-EGF, released from the cell membrane by TACE/ADAM17, is
necessary for regulation of MMP-9 levels and invasion activity of
HSC3 cells. The HB-EGF/EGFR autocrine loop via ADAM17 may play a
crucial role in the aggressive behavior of oral SCCs, although
further investigation is needed to confirm this.
The standard treatment for oral cancer is a
combination of surgery, radiation and chemotherapy. Cytotoxic
agents, including carboplatin, cisplatin, and paclitaxel, form the
cornerstone of chemotherapy for oral cancer. However, some patients
with advanced oral cancer relapse and ultimately die due to the
development of drug resistance. Alternative cancer therapies target
molecules overexpressed in cancer cells. For example, many human
tumors exhibit overexpression of the ErbB family of receptors,
including EGFR, which correlates with more aggressive tumors, poor
prognosis, and resistance to therapy (28,29).
Thus, the ErbB family has become a target of cancer therapy,
although the actual curative effects remain insufficient. A large
percentage of patients who are initially responsive to ErbB
receptor-targeted therapies later become resistant. It is possible
that therapy targeted against HB-EGF may overcome such obstacles.
It has been suggested that CRM197, a specific inhibitor of HB-EGF,
is a promising therapeutic agent for advanced ovarian cancer
(30). In addition, the shedding
machinery may be a good target for cancer therapy. Inhibition of
HB-EGF shedding results in the accumulation of pro-HB-EGF and
promotes E-cadherin expression, leading to suppression of EGFR
activity. Upregulation of E-cadherin by pro-HB-EGF not only
produces cellular morphological changes but also decreases cell
motility and enhances apoptotic sensitivity in response to
gemcitabine-erlotinib treatment (31). Thus, targeting the cleavage of
HB-EGF by ADAM17 may be effective in overcoming chemotherapy
resistance in oral cancer.
References
|
1
|
Fidler IJ: The pathogenesis of cancer
metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev
Cancer. 3:453–458. 2003.
|
|
2
|
Nguyen DX, Bos PD and Massague J:
Metastasis: from dissemination to organ-specific colonization. Nat
Rev Cancer. 9:274–284. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bos PD, Zhang XH-F, Nadal C, et al: Genes
that mediate breast cancer metastasis to the brain. Nature.
459:1005–1009. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jorissen RN, Walker F, Pouliot N, Garrett
TPJ, Ward CW and Burgess AW: Epidermal growth factor receptor:
mechanisms of activation and signaling. Exp Cell Res. 284:31–53.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hynes NE and Lane HA: ERBB receptors and
cancer: the complexity of targeted inhibitors. Nat Rev Cancer.
5:341–354. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lu X and Kang Y: Epidermal growth factor
signaling and bone metastasis. Br J Cancer. 102:457–461. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yagi H, Yotsumoto F and Miyamoto S:
Heparin-binding epidermal growth factor-like growth factor promotes
transcoelomic metastasis in ovarian cancer through
epithelial-mesenchymal transition. Mol Cancer Ther. 7:3441–3451.
2008. View Article : Google Scholar
|
|
8
|
Goishi K, Higashiyama S, Klagsbrun M, et
al: Phorbol ester induces the rapid processing of cell surface
heparin-binding EGF-like growth factor: conversion from juxtacrine
to paracrine growth factor activity. Mol Biol Cell. 6:967–980.
1995. View Article : Google Scholar
|
|
9
|
Higashiyama S, Abraham JA, Miller J,
Fiddes JC and Klagsbrun M: A heparin-binding growth factor secreted
by macrophage-like cells that is related to EGF. Science.
251:936–939. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Higashiyama S, Abraham JA and Klagsbrun M:
Heparin-binding EGF-like growth factor stimulation of smooth muscle
cell migration: dependence on interactions with cell surface
heparin sulfate. J Cell Biol. 122:933–940. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ongusaha PP, Kwak JC, Zwible AJ, et al:
HB-EGF is a potent inducer of tumor growth and angiogenesis. Cancer
Res. 64:5283–5290. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miyamoto S, Hirata M, Yamazaki A, et al:
Heparin-binding EGF-like growth factor is a promising target for
ovarian cancer therapy. Cancer Res. 64:5720–5727. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Freeman MR, Yoo JJ, Raab G, et al:
Heparin-binding EGF-like growth factor is an autocrine growth
factor for human urothelial cells and is synthesized by epithelial
and smooth muscle cells in the human bladder. J Clin Invest.
99:1028–1036. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Weaver MA: Invadopodia: specialized cell
structures of cancer invasion. Clin Exp Metastasis. 23:97–105.
2006. View Article : Google Scholar
|
|
15
|
Nakagawa M, Nabeshima K, Asano S, et al:
Up-regulated expression of ADAM17 in gastrointestinal stromal
tumors: coexpression with EGFR and EGFR ligands. Cancer Sci.
100:654–662. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cohen S: Origins of growth factors: NGF
and EGF. Ann NY Acad Sci. 1038:98–102. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Iwasaki S, Aoyagi H and Yoshizawa H:
Immunohistochemical detection of epidermal growth factor and
epidermal growth factor receptor in the lingual mucosa of rats
during the morphogenesis of fili form papileae. Acta Histochem.
109:37–44. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Iwamoto R and Mekada E: Heparin-binding
EGF-like growth factor: a juxtacrine growth factor. Cytokine Growth
Factor Rev. 11:335–344. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Izumi Y, Hirata M, Hasuwa H, et al: A
metalloprotease-disintegrin, MDC9/meltrin-gamma/ADAM9 and PKC-delta
are involved in TPA-induced ectodomain shedding of
membrane-anchored heparin-binding EGF-like growth factor. EMBO J.
17:7260–7272. 1998. View Article : Google Scholar
|
|
20
|
Suzuki M, Raab G, Moses MA, Fernandez CA
and Klagsbrun M: Matrix metalloproteinase-3 releases active
heparin-binding EGF-like growth factor by cleavage at a specific
juxtamembrane site. J Biol Chem. 272:31730–31737. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fischer OM, Hart S, Gschwind A and Ullrich
A: EGFR signal transactivation in cancer cells. Biochem Soc Trans.
31:1203–1208. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Miyamoto S, Yagi H, Yotsumoto F,
Kawarabayashi T and Mekada E: Heparin-binding epidermal growth
factor-like growth factor as a novel targeting molecule for cancer
therapy. Cancer Sci. 97:341–347. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Razandi M, Pedram A, Park ST and Levin ER:
Proximal events in signaling by plasma membrane estrogen receptors.
J Biol Chem. 278:2701–2712. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gooz M, Gooz P, Luttrell LM and Raymond
JR: 5-HT2A receptor induces ERK phosphorylation and proliferation
through ADAM-17 tumor necrosis factor-alpha-converting enzyme
(TACE) activation and heparin-bond epidermal growth factor-like
grow factor (HB-EGF) shedding in mesangial cells. J Biol Chem.
281:21004–21012. 2006. View Article : Google Scholar
|
|
25
|
Horiuchi K, Le Gall S, Schulte M, et al:
Substrate selectivity of epidermal growth factor-receptor ligand
sheddases and their regulation by phorbol esters and calcium
influx. Mol Biol Cell. 18:176–188. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sahin U, Weskamp G, Kelly K, et al:
Distinct roles for ADAM10 and ADAM17 in ectodomain shedding of six
EGFR ligands. J Cell Biol. 164:769–779. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zheng X, Jiang F, Katakowski M, Zhan ZG,
Lu QE and Chopp M: ADAM17 promotes breast cancer cell malignant
phenotype through EGFR-PI3K-AKT activation. Cancer Biol Ther.
8:1045–1054. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Liu PCC, Liu X, Li Y, et al:
Identification of ADAM10 as a major source of HER2 ectodomain
sheddase activity in HER2 overexpressing breast cancer cell. Cancer
Biol Ther. 5:657–664. 2006.PubMed/NCBI
|
|
29
|
Wikstland CJ, Reist CJ, Archer GE,
Zalutsky MR and Bigner DD: The class III variant of the epidermal
growth factor receptor (EGFRvIII): characterization and utilization
as an immunotherapeutic target. J Neurovirol. 4:148–158. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tsujioka H, Yotsumoto F, Hikita S, Ueda T,
Kuroki M and Miyamoto S: Targeting the heparin-binding epidermal
growth factor-like growth factor in ovarian cancer therapy. Curr
Opin Obstet Gynecol. 23:24–30. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang F, Sloss C, Zhang X, Lee SW and
Cusack JC: Membrane-bound heparin-binding epidermal growth
factor-like growth factor regulates E-cadherin expression in
pancreatic carcinoma cells. Cancer Res. 67:8486–8493. 2007.
View Article : Google Scholar
|