Introduction
Bladder cancer is the fourth most common cancer and
is the ninth leading cause of cancer-related mortality among men in
the United States (1); it is also
the most common urologic cancer in China (2). An estimated 70,530 new cases were
diagnosed and 14,680 people succumbed to bladder cancer in the
United States in 2010 (3). Although
the majority of patients present with superficial bladder tumors,
50–70% will recur and 10–30% will progress to muscle-invasive
disease (1). Although
organ-confined muscle-invasive bladder cancer was subjected to
radical cystectomy according to the NCCN guidelines,
bladder-sparing tri-modality is an alternative approach (4). Bladder cancer has a tendency to recur,
and with recurrence a few number of cases progress, making the
early detection of high-risk patients urgent (1). Clinical stage and histological grade
are significant predictors of outcome (5). Tumor number and lymphovascular
invasion are also reported to be associated with recurrence after
surgery (6). However, few
biomarkers were considered as prognostic factors in cystectomy
candidates with organ-confined bladder cancer.
Non-muscle myosin II A (NM IIA), which belongs to
the myosin II subfamily, is an actin-binding protein and is
regulated by the phosphorylation of its heavy and light chains
(7). NMHC IIA is a subunit of NM
IIA which is central to the control of cell adhesion, cell
migration and tissue architecture (7,8). MYH9
gene localized to chromosome 22q11.2 and encoded NMHC IIA (9), whose mutations are responsible for a
complex disorder named MYH9-related disease, are characterized by
an association of different phenotypic features (10). Although NM IIA has a basic role in
processes that require cellular reshaping and movement, such as
cell adhesion and cell migration (7,11),
only a few studies have evaluated its role in cancer tissues. Its
expression has been accounted as a negative prognostic indicator in
stage I lung adenocarcinoma (12).
Another study of non-small cell lung cancer indicated that
overactivation of myosin II could be a factor contributing to
metastasis (13). Overexpression of
myosin IIA may promote the progression and poor prognosis of
esophageal squamous cancer, and this effect may be related to
increased cancer cell migration (14). However, there is currently no report
on the relationship between myosin IIA expression and bladder
cancer.
The purpose of the present study was to investigate
the expression level of NMHC IIA in bladder cancer and its
clinicopathological and prognostic significance. In this study,
real-time PCR and immunohistochemistry assay were performed to
examine mRNA and protein expression in a cohort of early-stage
bladder cancer cystectomy candidates.
Materials and methods
Patients and tissue specimens
For real-time PCR, 16 paired bladder cancer and
adjacent normal bladder tissues were collected from patients who
underwent surgery between March 2010 and June 2010. In addition,
167 paraffin-embedded specimens of bladder cancer from 88 patients
treated with radical cystectomy and 79 patients of bladder-sparing
treatment were collected between January 2003 and December 2009 for
immunohistochemical assay. Patients with non-urothelial tumor
ingredients, imaging of hydronephrosis, metastasis and T3b-T4
disease were excluded from the radical cystectomy group. Clinical
staging was carried out according to the American Joint Committee
on Cancer (AJCC) TNM Staging System (7th edition, 2010) and
histologic grade was according to WHO 1973. The clinicopathological
characteristics of cystectomy candidates with early-stage bladder
cancer are summarized in Table I.
Consent from the patients and approval from the Sun Yat-sen
University Cancer Center institute research ethics committee were
obtained before using these clinical materials.
 | Table IClinical characteristics of cystectomy
candidates with early-stage bladder cancer. |
Table I
Clinical characteristics of cystectomy
candidates with early-stage bladder cancer.
| Group | No. of patients
treated with radical cystectomy (%) | No. of patients
treated with bladder-sparing approach (%) | P-value |
|---|
| Age (years) |
| ≤60 | 50 (50) | 50 (50) | 0.394 |
| >60 | 38 (57) | 29 (43) | |
| Gender |
| Male | 86 (57) | 65 (43) | 0.001 |
| Female | 2 (13) | 14 (87) | |
| Size (cm) |
| >3 | 36 (35) | 67 (65) | 0.000 |
| ≤3 | 52 (81) | 12 (19) | |
| Number |
| >3 | 69 (57) | 52 (43) | 0.069 |
| ≤3 | 19 (41) | 27 (59) | |
| Clinical stage |
| Tis,T1 | 24 (45) | 29 (55) | 0.191 |
| T2 | 64 (56) | 50 (44) | |
| Grade |
| G1,G2 | 33 (54) | 28 (46) | 0.783 |
| G3 | 55 (52) | 51 (48) | |
RNA extraction and real-time PCR
analysis
Total RNA was isolated from 16 pairs of bladder
cancer tissues and their adjacent normal bladder tissues using
TRIzol reagent (Invitrogen, Carlsbad, CA, USA). RNA was
reverse-transcribed performing SuperScript First Strand cDNA System
(Invitrogen). The first strand cDNA products were then amplified
with GAPDH-specific (F: 5′-CTCCTCCTGTTCGACAGTCAGC-3′ and R:
5′-CCCAATACGACCAAATCCGTT-3′) and NMHC IIA-specific (F:
5′-CCATCACAGACACCGCCTACAG-3′ and R: 5′-CTTCTTGGTGTTCTCCGTCTTGC-3′)
primers by real-time PCR and data collection were performed on the
ABI Prism 7900HT system.
Immunohistochemistry analysis
Immunohistochemistry was performed as a modification
of the method previously described (15). Paraffin-embedded specimens were cut
into 4-μm sections and baked at 65°C for 30 min. Following
deparaffinization and hydration, endogenous peroxidase was blocked
using blocking buffer (3% hydrogen peroxide) and antigen retrieval
was implemented in a pressure sterilizer. After the sections were
incubated with 1% bovine serum albumin for 30 min at room
temperature, the rabbit polyclonal anti-NMHC-IIA antibody (Abcam,
Cambridge, UK) (1:2000) was added and set overnight in a wetting
case at 4°C. After washing, the biotinylated anti-rabbit secondary
antibody was added, followed by streptavidin-horseradish peroxidase
complex. The sections were counterstained with hematoxylin before
mounting and evaluating. Negative controls were performed using the
non-immune rabbit IgG of the same isotype instead of NMHC-IIA
antibody.
Statistical analysis
All statistical analyses were carried out with the
SPSS 16.0 statistical software package. In the real-time PCR,
Student’s t-test was used to analyze mRNA expression between
bladder cancer and adjacent normal tissues. The χ2 test
for proportion was used to analyze the relationship between NMHC
IIA protein expression and clinicopathological characteristics.
Cancer-specific survival rates, recurrence-free survival rates and
overall survival rates were calculated using the Kaplan-Meier
method and compared by the log-rank test. The clinical
characteristics of patients treated with the bladder-sparing
approach and radical cystectomy were compared by the χ2
test and the rank sum test. Prognostic factors were evaluated using
the cox regression method. P<0.05 was considered to indicate
statistically significant differences.
Results
Detection of NMHC IIA mRNA expression in
paired bladder tissues
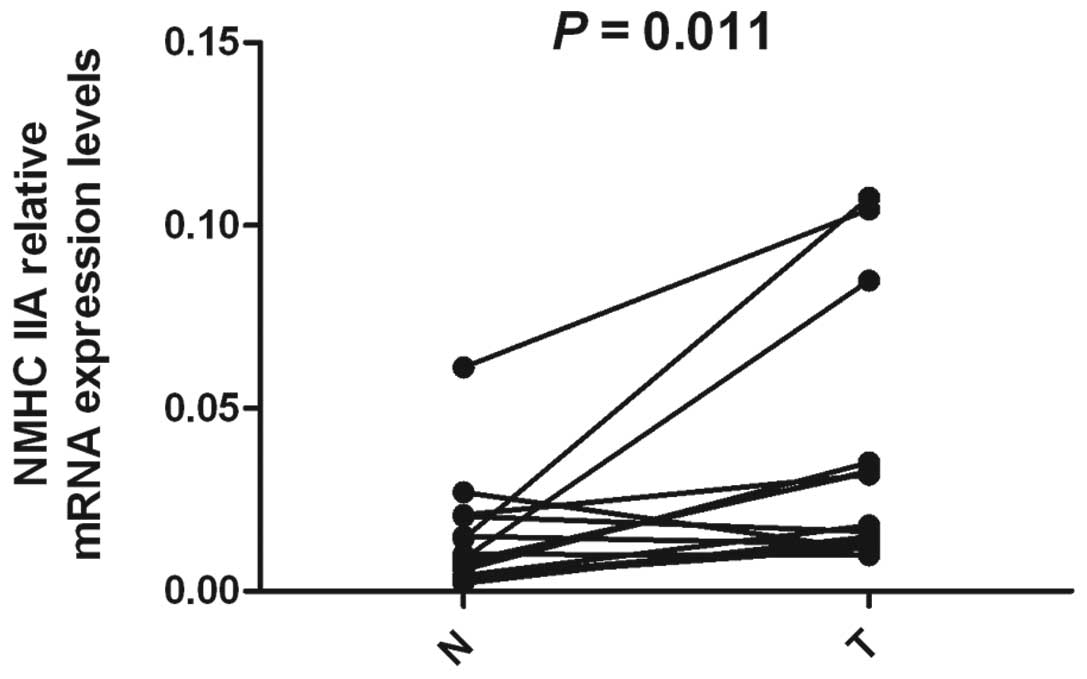
To investigate the status of transcriptional
expression of NMHC IIA in bladder cancer, real-time PCR was
performed in 16 pairs of bladder cancer and adjacent normal bladder
specimens, respectively. In the real-time PCR analysis, a total of
13 of 16 (81.3%) bladder cancer tissues showed upregulated NMHC IIA
expression, when compared with their adjacent normal bladder
tissues. Expression of mRNA was found to be higher in tumor tissues
than in the paired adjacent normal tissues (P=0.011) (Fig. 1). The relative expression levels
were determined as a ratio between NMHC IIA and the reference gene
(GAPDH) for variation in the quantity of mRNA. The ratios (bladder
cancer/normal tissue) were 4.0, 1.5, 7.3, 2.1, 7.0, 4.5, 3.0, 5.9,
9.6, 3.1, 1.7, 4.2 and 3.3, respectively. This result was in line
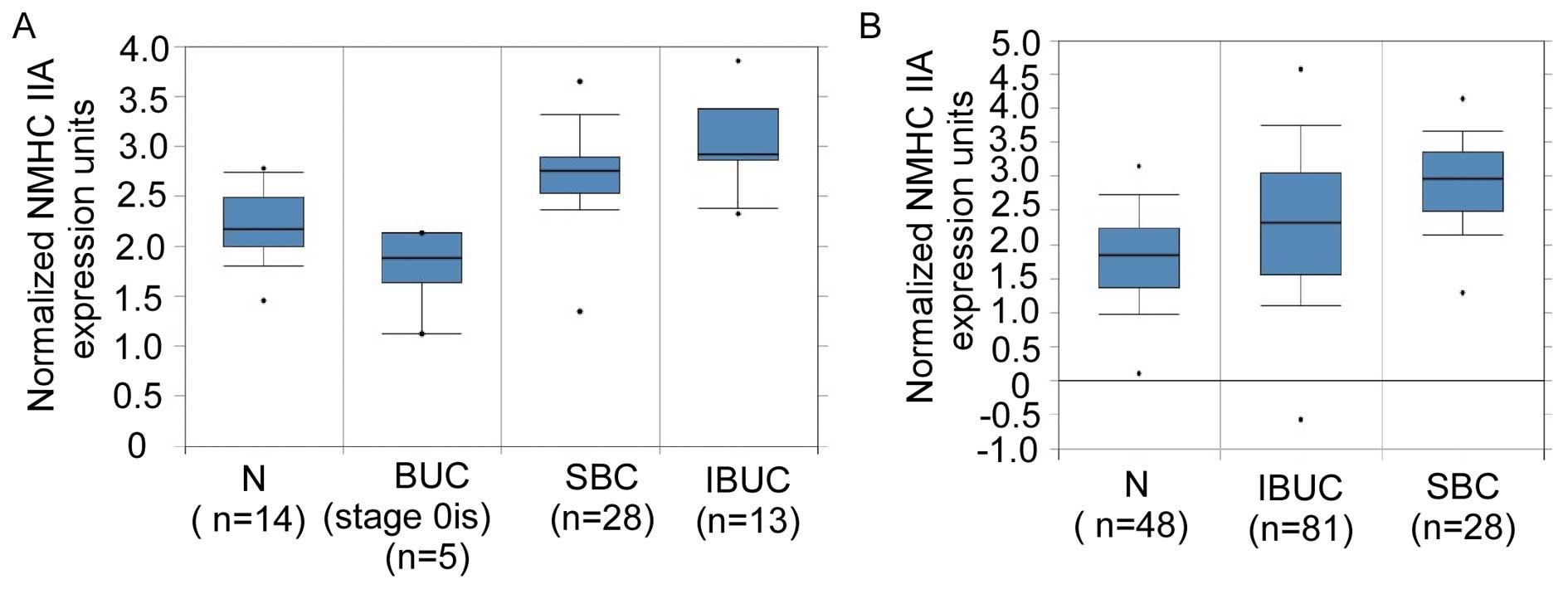
with the NMHC IIA expression data in two microarray expression
profiling reports as deposited in the Oncomine database (16,17).
Oncomine expression analysis showed consistent NMHC IIA
upregulation in human bladder cancer compared with normal bladder
tissues (Fig. 2).
Expression of NMHC IIA protein in
paraffin-embedded bladder cancer tissues
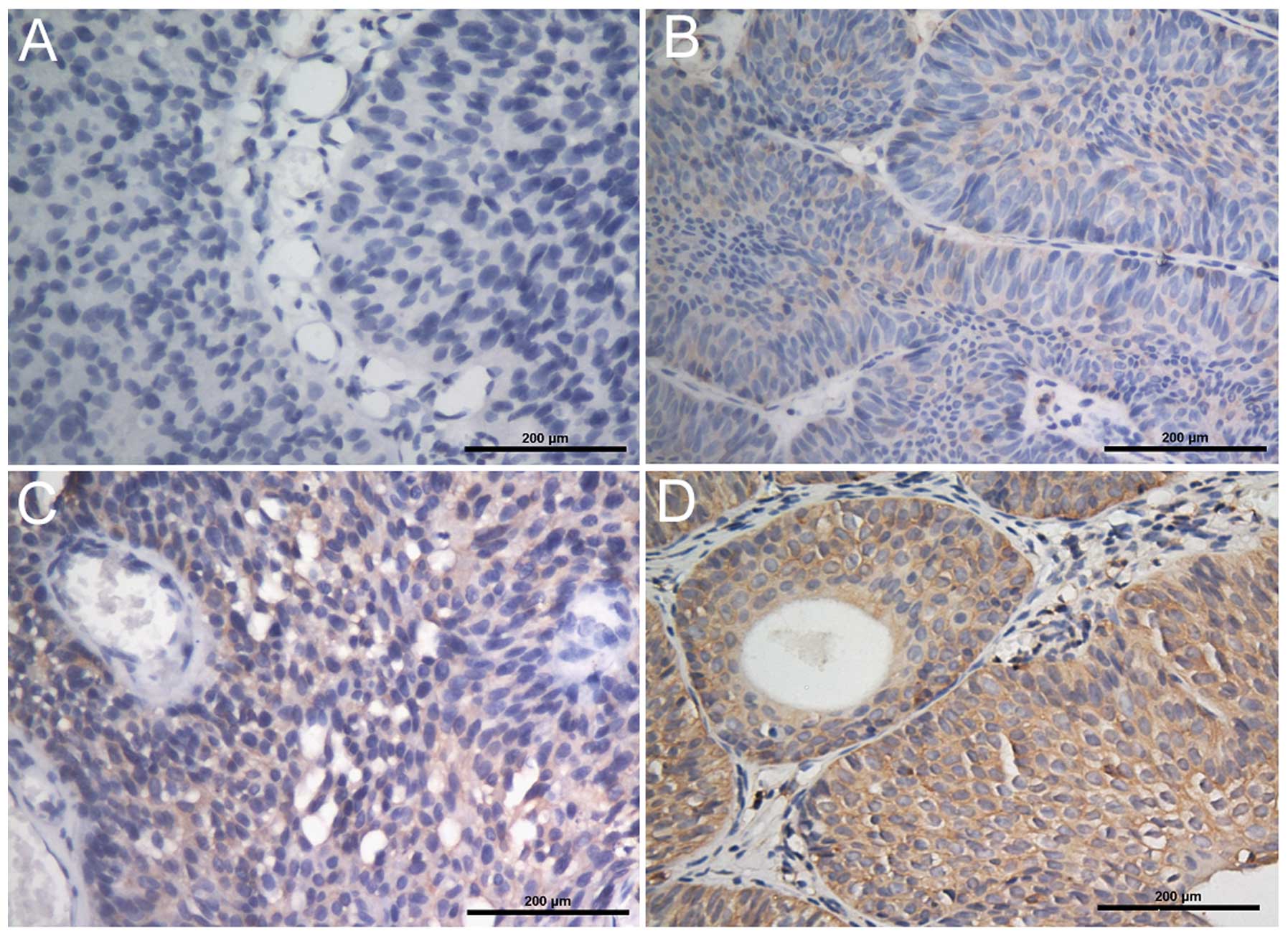
Expression and subcellular location of NMHC IIA
protein were investigated by immunohistochemistry of 167
paraffin-embedded, archival bladder cancer tissues. Representative
staining of NMHC IIA in the cancer is shown in Fig. 3. The NMHC IIA protein staining was
localized mainly in the cytoplasm of all tumor tissues and on the
cell membrane of some tumor tissues (Fig. 3). Samples with >50% of the cells
showing immunohistochemical reactivity for NMHC IIA were considered
as positive according to the criteria by Maeda et al
(12). Positive expression was
further subdivided into weakly positive (Fig. 3B), median positive (Fig. 3C) and strongly positive (Fig. 3D) based on staining intensity. The
negative NMHC IIA staining is shown in Fig. 3A. The low expression of NMHC IIA
included weakly positive and negative staining. The median positive
and strongly positive staining was considered as high expression of
NMHC IIA.
Relationship between NMHC IIA expression
and clinicopathological characteristics
The relationship between the expression of NMHC IIA
protein and clinical characteristics is shown in Table II. Intense expression of NMHC IIA
protein in bladder cancer was not significantly correlated with
gender, age, tumor number, tumor size, group or clinical stage
(P>0.05), but was significantly correlated with the
histopathological grade and lymph node metastasis (P<0.05). The
high expression of NMHC IIA protein was noted in 54 and 72% of
bladder tumors of histopathological grade (G1+G2) and G3,
respectively (P<0.05). In addition, NMHC IIA had increased
expression in lymph node metastasis positive tumors compared with
lymph node non-metastasis tumors, although the cases of lymph node
metastasis positive tumors were very few (n=7).
 | Table IICorrelation between the expression of
NMHC IIA protein and clinicopathological factors in cystectomy
candidates with early-stage bladder cancer. |
Table II
Correlation between the expression of
NMHC IIA protein and clinicopathological factors in cystectomy
candidates with early-stage bladder cancer.
| | NMHC IIA
expression | |
|---|
| |
| |
|---|
| Characteristics | N | Low (%) | High (%) | P-value |
|---|
| Gender |
| Male | 151 | 52 (34) | 99 (66) | 0.807 |
| Female | 16 | 6 (38) | 10 (62) | |
| Age (years) |
| <60 | 100 | 35 (35) | 65 (65) | 0.929 |
| ≥60 | 67 | 23 (34) | 44 (66) | |
| Tumor no. |
| ≤3 | 121 | 43 (36) | 78 (64) | 0.723 |
| >3 | 46 | 15 (33) | 31 (67) | |
| Clinical stage |
| Tis,T1 | 53 | 23 (43) | 30 (57) | 0.109 |
| T2 | 114 | 35 (31) | 79 (69) | |
| Grade |
| G1,G2 | 61 | 28 (46) | 33 (54) | 0.021 |
| G3 | 106 | 30 (28) | 76 (72) | |
| Tumor size
(cm) |
| ≤3 | 103 | 41 (40) | 62 (60) | 0.081 |
| >3 | 64 | 17 (27) | 47 (73) | |
| Group |
| BS | 79 | 24 (30) | 55 (70) | 0.263 |
| RC | 88 | 34 (39) | 54 (61) | |
| Lymph node |
| N0 | 160 | 58 (36) | 102 (64) | 0.047 |
| N1,N2 | 7 | 0 (0) | 7 (100) | |
Univariate and multivariate analyses for
prognosis of bladder cancer patients
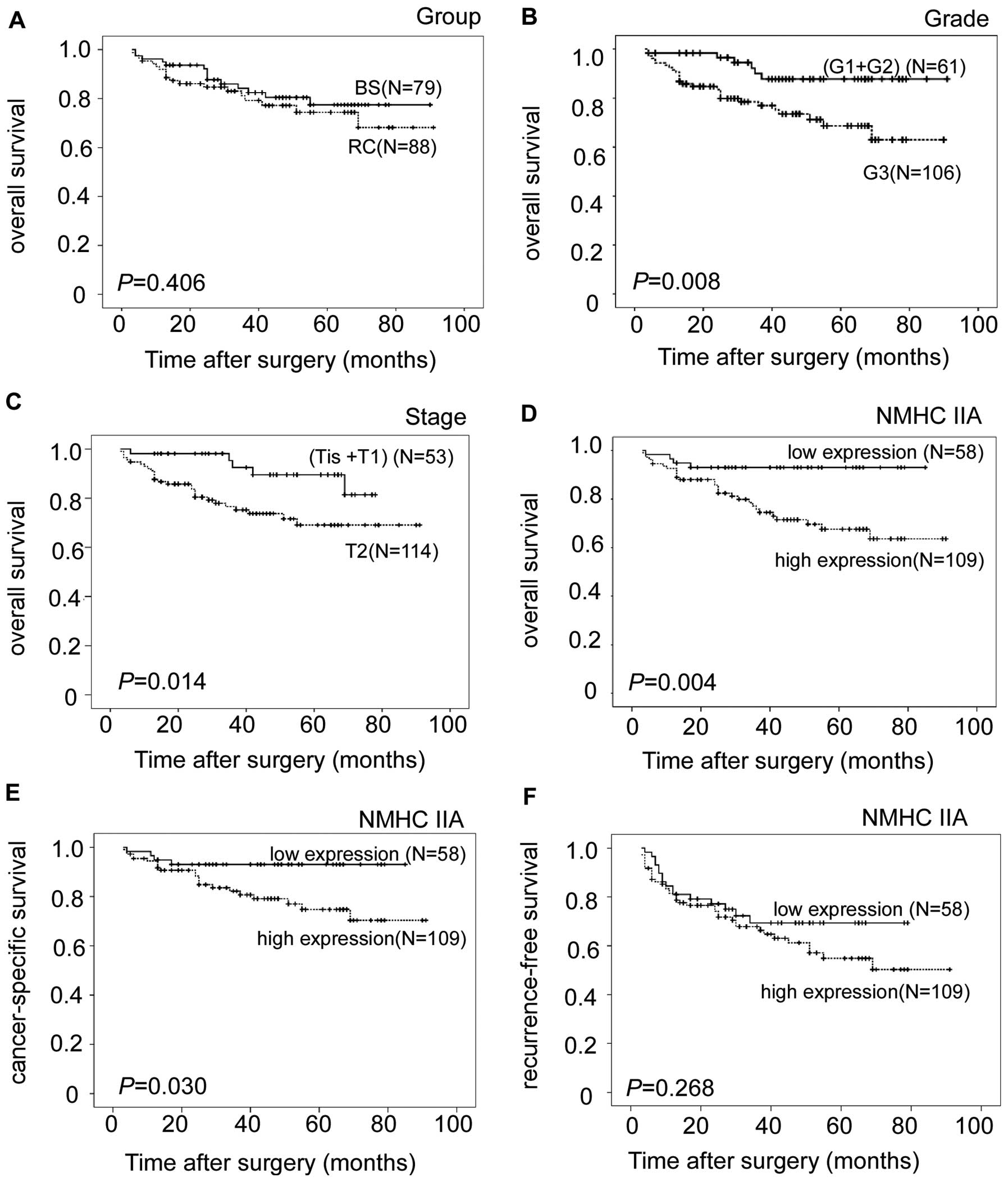
Univariate and multivariate data analyses were
carried out using the Cox proportional hazards regression model to
investigate the prognostic value of NMHC IIA expression (Table III and Fig. 4). Grade, clinical T stage and high
NMHC IIA expression were the prognostic factors to predict a poor
prognosis in univariate analysis (P=0.014, 0.008, and 0.004,
respectively), however, there was no statistical difference between
the overall survival of patients treated with bladder-sparing and
those treated with radical cystectomy (P=0.406) (Table III and Fig. 4A-D). By multivariate analysis of the
prognostic factors, we confirmed that high NMHC IIA expression was
an independent prognostic factor (95% confidence interval:
0.115–0.985; P=0.047), grade and clinical T stage were also two
independent and significant prognostic factors for overall survival
(P=0.02 and 0.049)(Table III).
The survival rate was higher in patients with lower grade and
clinical T stage (Fig. 4).
 | Table IIIUnivariate and multivariate analysis
of potential factors in cystectomy candidates with early-stage
bladder cancer. |
Table III
Univariate and multivariate analysis
of potential factors in cystectomy candidates with early-stage
bladder cancer.
| | | | 95% CI for
Exp(B) |
|---|
| | | |
|
|---|
| Factors | Category | Univariate | Multivariate | Lower | Upper |
|---|
| Group | BS/RC | 0.406 | 0.422 | 0.298 | 1.660 |
| T-Stage | T1/T2 | 0.014 | 0.049 | 0.138 | 0.994 |
| Grade | (G1+G2)/3 | 0.008 | 0.020 | 0.128 | 0.840 |
| Age (years) | ≤65/>65 | 0.275 | 0.182 | 0.798 | 3.278 |
| No. | ≤3/>3 | 0.443 | 0.660 | 0.497 | 3.020 |
| Size (cm) | ≤3/>3 | 0.161 | 0.714 | 0.496 | 2.785 |
| Gender | Male/Female | 0.767 | 0.589 | 0.198 | 2.509 |
| NMHC IIA | Low/High | 0.004 | 0.047 | 0.115 | 0.985 |
Correlation of clinicopathological
variables and NMHC IIA expression with patient survival in bladder
cancer
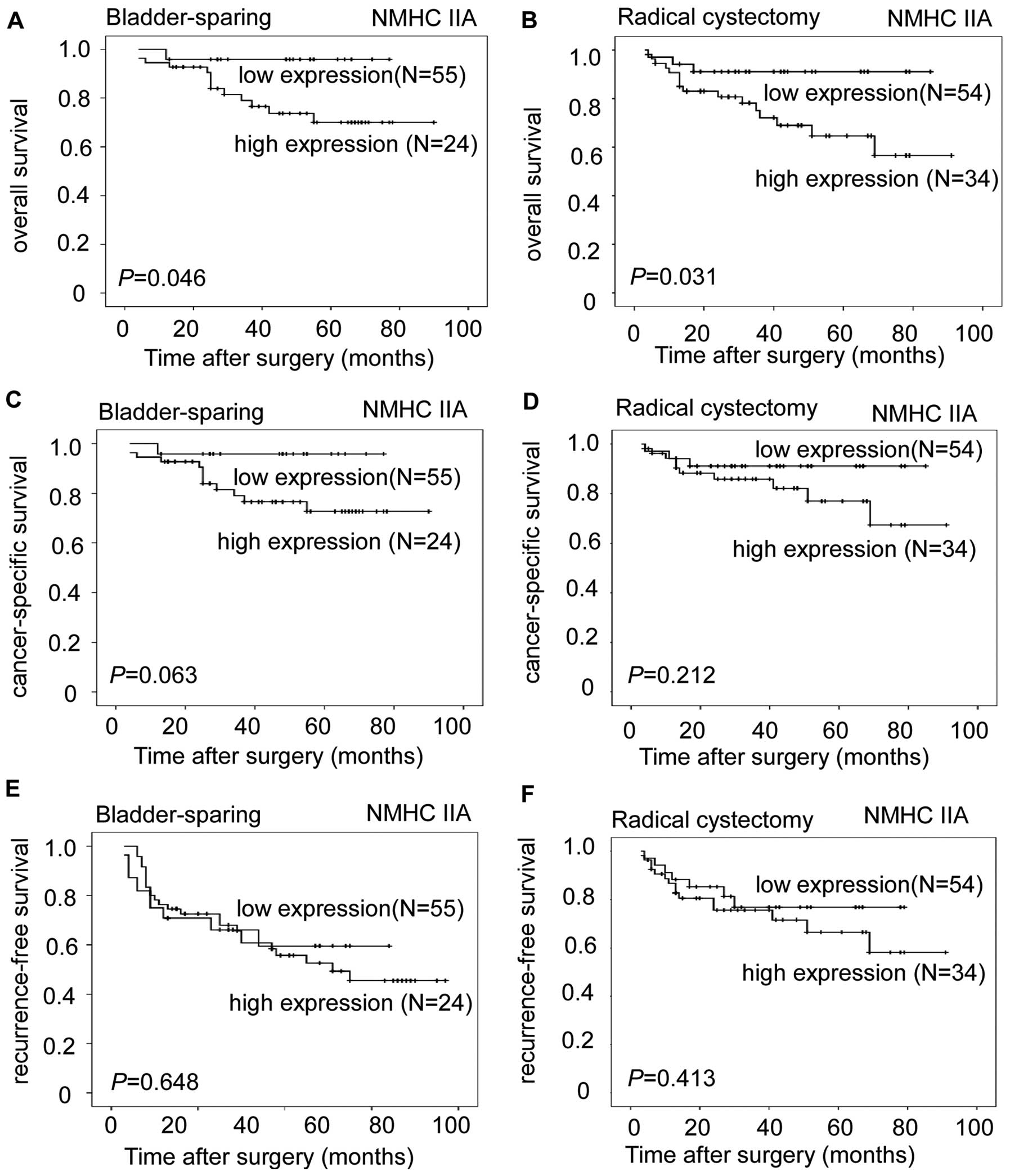
With a median follow-up of 40 months (3–91 months),
salvage cystectomy was performed in 8 patients and 2 died in 19 and
37 months after initial bladder-sparing treatment. The median time
after completing bladder-sparing treatment was 24 months (range
4–37 months). The 3- and 5-year overall survival rates of patients
who underwent bladder-sparing treatment, assessed by the
Kaplan-Meier method, were 81 and 61%, respectively; those of the
patients who completed radical cystectomy were 72 and 54%
(P=0.406). The association between overall survival and clinical
characteristics is shown in Table
III and Fig. 4. There was a
significantly higher 5-year survival rate in the NMHC IIA
protein-low group than in the NMHC IIA protein-high group (P=0.004)
(Fig. 4D). In addition, we also
analyzed the cancer-specific survival (CSS) and recurrence-free
survival (RFS) between the two NMHC IIA expression groups in
bladder cancer. The CSS of the high NMHC IIA expression group was
significantly lower than that of the low NMHC IIA expression group
(P=0.03) (Fig. 4E); there was no
significant difference between the two NMHC IIA expression groups
of the RFS in bladder cancer (P=0.268) (Fig. 4F). Furthermore, we divided the
patients into two groups according to the treatment in bladder
cancer. For patients treated with the bladder-sparing approach, the
overall survival of the NMHC IIA protein-low group was
significantly higher than that of the NMHC IIA protein-high group
(P=0.046) (Fig. 5A), and the
cancer-specific survival of the NMHC IIA protein-low group also
showed a higher trend compared to that of the NMHC IIA protein-high
group (P=0.063) (Fig. 5C).
Recurrence-free survival of the two groups was not significantly
different (P=0.648) (Fig. 5E). For
patients treated with radical cystectomy, the overall survival of
the NMHC IIA protein-high group was significantly lower than that
of the NMHC IIA protein-low group (P=0.031) (Fig. 5B), and there was no statistical
difference between the cancer-specific survival of the NMHC IIA
protein-high group and that of the NMHC IIA protein-low group
(P=0.212) (Fig. 5D).
Recurrence-free survival of the two groups showed no statistical
difference (P=0.413) (Fig. 5E).
Discussion
Bladder cancer carries among the highest costs of
all types of cancer, from diagnosis until mortality (18). Patients with the same
clinicopathological stage of bladder cancer treated with radical
cystectomy exhibit considerable variability in survival (19,20).
Particularly for cystectomy candidates with early-stage bladder
cancer, bladder-sparing treatment is a viable alternative.
Therefore, there is an urgent need for new factors that can
distinguish between patients with an unfavorable prognosis and
those with a better prognosis, and optimize individual
management.
This study demonstrated that there was a significant
increase of NMHC IIA expression at mRNA levels between bladder
cancer cells and the adjacent normal bladder tissue. This result
was similar to those of previous studies of other human cancers
(12,14). Furthermore, intense expression of
NMHC IIA in bladder cancer was correlated with its
clinicopathological features including histopathological
classification and lymph node metastasis. Our results provide a
basic concept that upregulated expression of NMHC IIA in human
bladder cancer may be important in the acquisition of a poor
prognostic phenotype. Of note, the high expression of NMHC IIA is
an independent molecular marker for shortened survival time of
patients, who were cystectomy candidates with early-stage bladder
cancer, and it might be a helpful criterion to optimize individual
therapy management.
In this study, there was a significantly lower
5-year survival rate in the NMHC IIA protein-high group than in the
NMHC IIA protein-low group (P<0.05). The CSS of the low NMHC IIA
expression group was significantly higher than that of the high
NMHC IIA expression group (P=0.03), however, there were no
significant differences between the two NMHC IIA expression groups
of the RFS in bladder cancer (P=0.268). For patients treated with
the bladder-sparing approach or radical cystectomy, the overall
survival of the NMHC IIA protein-high group was significantly lower
than that of the NMHC IIA protein-low group (P<0.05), and there
was no statistical difference between the cancer-specific survival
of the NMHC IIA protein-high group and that of the NMHC IIA
protein-low group (P>0.05). Recurrence-free survival of the two
groups was also not significantly different (P>0.05). These
results suggest that overexpression of NMHC IIA might not affect
the initiation of tumor recurrence, but might induce disease
progression after recurrence. Therefore, investigation of the
molecular and biological changes associated with NMHC IIA
expression in course to carcinogenesis and progression can provide
new insight into the pathology of the disease and may provide
biological factors as new prognostic markers.
NMHC IIA is a major subunit of the actomyosin
cytoskeleton and is generally considered to attribute to the
contraction of the cell posterior during migration (21). Previous studies have shown that NMHC
IIA plays a key role in tumor cell invasiveness, and the
EGF-dependent phosphorylation of the myosin IIA heavy chain has a
direct function in mediating motility and chemotaxis in human
breast cancer cells MDA-MB-231 (22). Also, it was reported as a target of
SRF, which contributes to invasion and metastasis in breast cancer
(23). A recent report suggested
that overexpression of let-7f in gastric cancer could inhibit
invasion and migration of gastric cancer cells through directly
targeting the tumor metastasis-associated gene MYH9/NMHC IIA
(24). NMHC IIA has been reported
as a decisive protein for cells to invade, indicating that this
molecule is a candidate for targeted anti-invasive treatment
(25). Our study demonstrated that
NMHC IIA had increased expression in lymph node metastasis positive
tumors compared with lymph node non-metastasis tumors, although the
cases of lymph node metastasis positive tumors were very few. This
molecule might reflect the cellular functions of metastasis.
Therefore, the exact function of NMHC IIA in bladder cancer, such
as metastasis, needs further exploration.
To our knowledge, this is the first report on the
overexpression of NMHC IIA in bladder cancer, and it is an
independent predictor of overall survival for cystectomy candidates
with early-stage bladder cancer. However, as the cystectomy
candidates with clinical stage T1 and T2 disease represented a
specific and small number of the patients with bladder cancer, the
correlation between NMHC IIA and bladder cancer requires more
detailed investigation. Moreover, the number of patients with lymph
node metastasis in this study was few, therefore the findings
require further investigation.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (81072101, 81025014 and
91019015).
References
|
1
|
Jacobs BL, Lee CT and Montie JE: Bladder
cancer in 2010: how far have we come? CA Cancer J Clin. 60:244–272.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gu FL and Liu YL: Changing status of
genitourinary cancer in recent 50 years. Chin J Urol. 2002:88–90.
2002.
|
|
3
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar
|
|
4
|
Montie JE, Clark PE, Eisenberger MA, et
al: Bladder cancer. J Natl Compr Canc Netw. 7:8–39. 2009.
|
|
5
|
Wasco MJ, Daignault S, Zhang Y, et al:
Urothelial carcinoma with divergent histologic differentiation
(mixed histologic features) predicts the presence of locally
advanced bladder cancer when detected at transurethral resection.
Urology. 70:69–74. 2007. View Article : Google Scholar
|
|
6
|
Zhang M, Tao R, Zhang C and Shen Z:
Lymphovascular invasion and the presence of more than three tumors
are associated with poor outcomes of muscle-invasive bladder cancer
after bladder-conserving therapies. Urology. 76:902–907. 2010.
View Article : Google Scholar
|
|
7
|
Vicente-Manzanares M, Ma X, Adelstein RS
and Horwitz AR: Non-muscle myosin II takes centre stage in cell
adhesion and migration. Nat Rev Mol Cell Biol. 10:778–790. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arii J, Goto H, Suenaga T, et al:
Non-muscle myosin IIA is a functional entry receptor for herpes
simplex virus-1. Nature. 467:859–862. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Simons M, Wang M, McBride OW, et al: Human
nonmuscle myosin heavy chains are encoded by two genes located on
different chromosomes. Circ Res. 69:530–539. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Burt RA, Joseph JE, Milliken S, Collinge
JE and Kile BT: Description of a novel mutation leading to
MYH9-related disease. Thromb Res. 122:861–863. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Conti MA and Adelstein RS: Nonmuscle
myosin II moves in new directions. J Cell Sci. 121:11–18. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Maeda J, Hirano T, Ogiwara A, et al:
Proteomic analysis of stage I primary lung adenocarcinoma aimed at
individualisation of postoperative therapy. Br J Cancer.
98:596–603. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Minamiya Y, Nakagawa T, Saito H, et al:
Increased expression of myosin light chain kinase mRNA is related
to metastasis in non-small cell lung cancer. Tumour Biol.
26:153–157. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xia ZK, Yuan YC, Yin N, Yin BL, Tan ZP and
Hu YR: Nonmuscle myosin IIA is associated with poor prognosis of
esophageal squamous cancer. Dis Esophagus. Sep 23–2011.(Epub ahead
of print). View Article : Google Scholar
|
|
15
|
Richards KL, Zhang B, Sun M, et al:
Methylation of the candidate biomarker TCF21 is very frequent
across a spectrum of early-stage nonsmall cell lung cancers.
Cancer. 117:606–617. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dyrskjøt L, Kruhøffer M, Thykjaer T, et
al: Gene expression in the urinary bladder: a common carcinoma in
situ gene expression signature exists disregarding
histopathological classification. Cancer Res. 64:4040–4048.
2004.
|
|
17
|
Sanchez-Carbayo M, Socci ND, Lozano J,
Saint F and Cordon-Cardo C: Defining molecular profiles of poor
outcome in patients with invasive bladder cancer using
oligonucleotide microarrays. J Clin Oncol. 24:778–789. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Botteman MF, Pashos CL, Redaelli A, Laskin
B and Hauser R: The health economics of bladder cancer: a
comprehensive review of the published literature.
Pharmacoeconomics. 21:1315–1330. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen W, Luo JH, Hua WF, et al:
Overexpression of EIF-5A2 is an independent predictor of outcome in
patients of urothelial carcinoma of the bladder treated with
radical cystectomy. Cancer Epidemiol Biomarkers Prev. 18:400–408.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Schrier BP, Hollander MP, van Rhijn BW,
Kiemeney LA and Witjes JA: Prognosis of muscle-invasive bladder
cancer: difference between primary and progressive tumours and
implications for therapy. Eur Urol. 45:292–296. 2004. View Article : Google Scholar
|
|
21
|
Ridley AJ, Schwartz MA, Burridge K, et al:
Cell migration: integrating signals from front to back. Science.
302:1704–1709. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dulyaninova NG, House RP, Betapudi V and
Bresnick AR: Myosin-IIA heavy-chain phosphorylation regulates the
motility of MDA-MB-231 carcinoma cells. Mol Biol Cell.
18:3144–3155. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Medjkane S, Perez-Sanchez C, Gaggioli C,
Sahai E and Treisman R: Myocardin-related transcription factors and
SRF are required for cytoskeletal dynamics and experimental
metastasis. Nat Cell Biol. 11:257–268. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liang S, He L, Zhao X, et al: MicroRNA
let-7f inhibits tumor invasion and metastasis by targeting MYH9 in
human gastric cancer. PLoS One. 6:e184092011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Derycke L, Stove C, Vercoutter-Edouart AS,
et al: The role of non-muscle myosin IIA in aggregation and
invasion of human MCF-7 breast cancer cells. Int J Dev Biol.
55:835–840. 2011. View Article : Google Scholar : PubMed/NCBI
|