Introduction
During the last decades, the development and
clinical use of anticancer drugs has become a regularity and
therefore an important way of controlling malignancies. However,
tumors can develop drug resistance to different therapeutic drugs,
making available chemotherapeutic agents ineffective in the course
of the disease. Among the proteins involved in anticancer drug
resistance are the ATP-binding cassette (ABC) transporters
(1). ABC transporters constitute
the largest superfamily of human cellular transporters. There are
currently 48 members classified in seven subfamilies termed A to G.
These transporters have the ability to actively transfer a
multitude of structurally dissimilar endogenous and exogenous
substrates and their metabolites across cell membranes (2). ABCG2 (also known as the breast cancer
resistance protein/mitoxantrone-resistance/ABC protein) consists of
655 amino acids, one transmembrane domain with six putative
transmembrane segments, and a single ATP-binding site. Deduced from
its structure, ABCG2 is a ‘semi-transporter’ (3–5)
similar to other members of the ABCG subfamily including the
Drosophila White protein ortholog (6). Overexpression of ABCG2 has been shown
to confer resistance to a variety of chemotherapeutic agents.
Affected drugs are anthracenedione mitoxantrone (7,8); the
camptothecin derivatives, topotecan (9,10) and
SN-38 (11); the anthracycline
doxorubicin (12); and the
antifolate methotrexate (13–15).
Mutations in the ABCG2 gene have been associated with high-level
anticancer drug resistance (16).
Furthermore, the effect of tyrosine kinase inhibitors on ABCG2 has
been reported (17).
Pharmacogenetic studies showed influences on pharmacokinetics of
tyrosine kinase inhibitors through mutations in the ABCG2 coding
sequence (18). The use of the
tyrosine kinase inhibitor imatinib has been shown to overcome
cancer drug resistance via ABCG2, whereas the efflux function is
inhibited by tyrosine kinase inhibitors. This functionality was
shown to be mediated through an interaction with ABCG2 at the
substrate binding site (19).
Recent structural analyses identified transmembrane domain 3
(around amino acid position 482) as the potential substrate-binding
pocket (20). In medical oncology,
tyrosine kinase inhibitors have become important drugs in the
treatment of renal cancer and therefore predictive markers for
treatment efficacy are of interest. To date, no data on mutations
in the potential substrate binding pocket of ABCG2 in tumor tissue
are available. Therefore, our aim was to investigate mutations in
the coding region for the transmembrane domain 3 and the
surrounding domains of ABCG2 in numerous renal cancer samples.
Thus, we directly sequenced the corresponding cDNA taken from 36
renal cancer tumor samples.
Materials and methods
Patient samples
Tissue samples were obtained from 36 renal cell
carcinoma patients who underwent elective surgery in the University
Hospital Heidelberg, Germany, after giving their informed consent
and following the ethics approval of the respective committees. The
sample of tumor tissue (200–500 mg) was obtained from a central
part of the respective carcinoma. Only non-necrotic tissue was
collected. All samples were snap frozen in liquid nitrogen and
stored at −80°C until further examination. Approximately 20–200 mg
of tumor sample was subjected to DNA and RNA extraction.
Extraction of RNA
For RNA extraction, tissue samples from renal cell
carcinoma patients were subjected to homogenisation and lysis using
the Qiagen RNA kit (Qiagen, Hilden, Germany). Isolated RNA was
measured by spectrophotometry.
Synthesis of cDNA from RNA
Reverse transcription was performed with the
Superscript III reverse transcriptase (Invitrogen) and random
hexamer primers (Applied Biosystems). The reaction mix was
incubated for 5 min at 25°C, 60 min at 50°C and finally at 70°C for
15 min to inactivate the reverse transcriptase.
Amplification of ABCG2 sequence fragments
and detection of ABCG2 mutations by sequencing
The following set of primers was used to amplify a
fragment of 690 bp. Forward primer sequence was
5′-tggagattccactgctgtggca and reverse primer sequence was
5′-tgacctgctgctatggccagtg, annealing temperature was 60.5°C.
Reaction volume was 25 μl, with 17.5 μl RNAse-free water, 2.5 μl
10X PCR buffer, 0.75 μl MgCl2 50 mM, 2 μl dNTP mix 10
mM, 0.5 μl of each primer (10 μM) and 0.25 μl of Taq polymerase.
cDNA (1.0 μl) was added. Thirty-five cycles were performed on an MJ
Research PCR Engine with an initial denaturation of 10 min. A cycle
consisted of 1 min denaturation of 95°C, 60.5°C annealing for 1 min
and 1 min at 72° for extension. Sequencing reactions were then
performed on the PCR products with the respective sequencing primer
and the 3′Big Dye Terminator Cycle Sequencing Ready Reaction kit
(ABI, Weiterstadt, Germany) according to the manufacturer's
instructions.
Identification of possible functional
single-nucleotide polymorphisms (SNPs) affecting the region of
interest
Annotated SNPs from dbSNP (http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=snp)
and the HapMap project (http://www.hapmap.org/) in the corresponding genomic
region of the ABCG2 gene were included in the analysis. The
following coding non-synonymous SNPs were analyzed (21,22):
rs41282401, rs9282571, rs3201997, rs3116448, rs2231142, rs1061018
and rs1061017. Coding synonymous SNPs were: rs12721640, rs3116439
and rs2231139.
Computational protein secondary structure
prediction
To evaluate the impact of an amino acid change we
used the JPRED software (http://www.compbio.dundee.ac.uk/www-jpred/) (23). This software predicts the secondary
structure using a neural network called Jnet. The prediction is the
definition of each residue into either α helix, β sheet or random
coil secondary structures (24,25).
Predictions were generated for the unaltered protein sequence and
for the corresponding mutated protein. Predictions were then
compared by visual inspection.
Additionally, a secondary structure prediction was
performed with the ESyPred3D program (26), accessible through http://www.fundp.ac.be/sciences/biologie/urbm/bioinfo/esypred/.
A secondary structure could be computed for the unaltered protein,
but no secondary structure prediction was possible for the mutated
protein.
Results
Comparative proteomics analysis
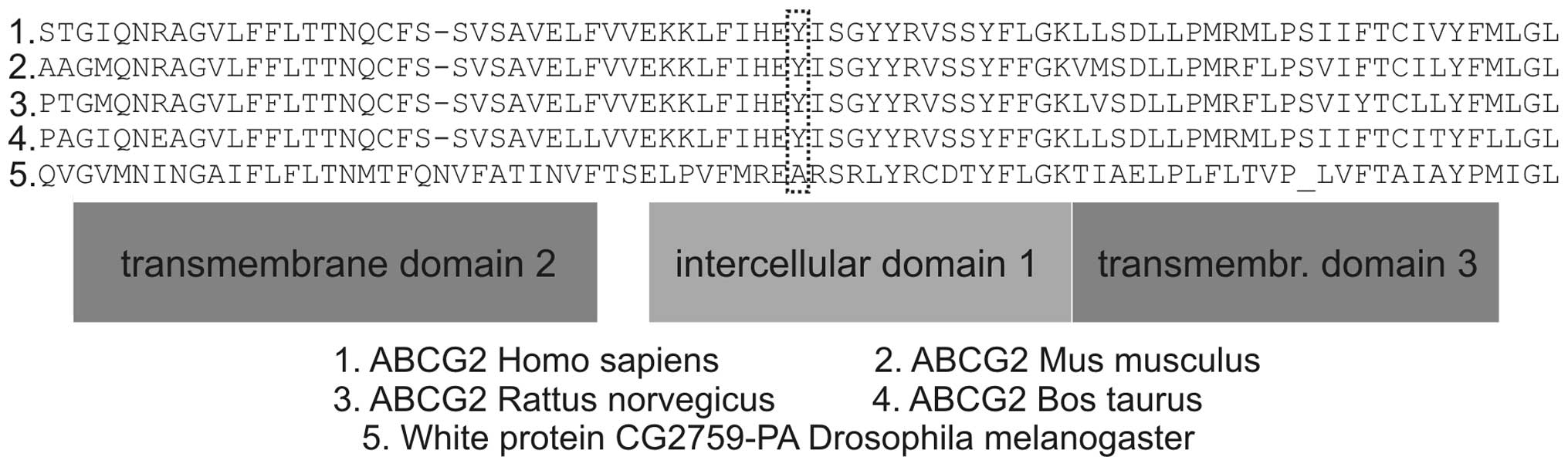
To further elucidate the structural organization of
the domains in the region of interest, a computational analysis was
performed. BLASTp searches and a PSI-BLAST against the whole
protein, the ABC_Transporter_2 domain (PS50893) and the
ABC2-membrane domain (PF01061) revealed a set of highly conserved
residues. In Fig. 1, the
position-specific conservation scores and a subset of aligned
protein sequences are shown.
Sequence analysis
Detailed examination of the raw sequences and the
automated sequences revealed a heterozygous shift from A to G at
position 1376 (Y→C at 459 aa, ICD1a, intracellular domain 1a, a
position which is highly conserved) in 3 patients. Of note, none of
the known SNPs was detected. Sequencing was repeated when the
acquired sequence data was ambiguous.
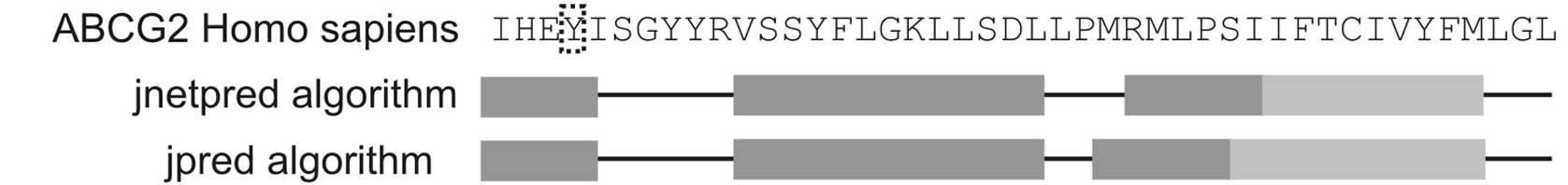
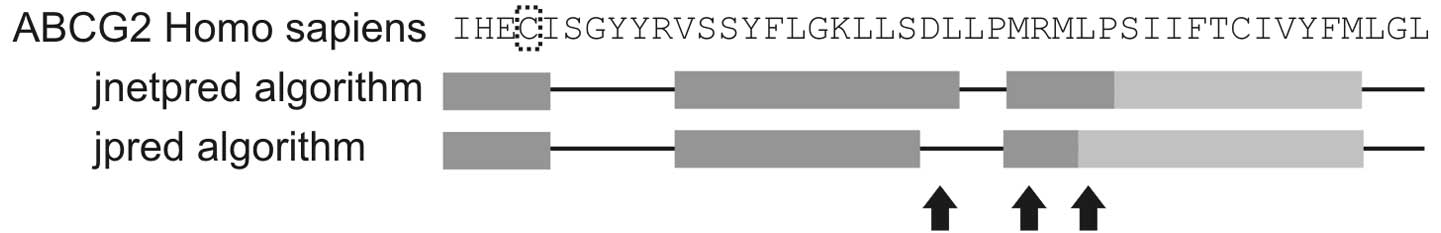
Computational protein folding
prediction
The prediction with JPRED showed a subsequent change
in the downstream folding of the protein induced by the mutation.
The structures of the intercellular domain 1b and 1c and of the
transmembrane domain 3 (TM3) were changed (Figs. 2 and 3).
Association with clinical data
Tumor samples with mutations led to evaluation of
the clinical course of the corresponding patient. All 3 patients
had surgical resection of the tumor and are in regular follow-up.
To date, no active tumor disease has been found in the 3 patients.
Therefore, no clinical data on treatment response were available
for these patients.
Discussion
Cancer drug resistance is a problem usually
encountered in prolonged chemotherapy. A significant proportion of
patients has no primary response to certain chemotherapeutic
agents. Understanding the mechanisms behind this drug resistance on
the molecular level can lead to improved therapeutic approaches. In
the case of renal carcinoma, the introduction of tyrosine kinase
inhibitors marked the beginning of a new therapeutic era. Thus far,
mechanisms for tumor drug resistance against tyrosine kinase
inhibitors in renal cancer cells have not been identified.
The ABCG2 gene was identified as a potent
‘de-toxification’ transporter for tyrosine kinase inhibitors in
cancer cells. In renal cancer cell lines, aberrant promoter
methylation of the ABCG2 gene was shown (27) and multiple SNPs have been reported
in patients with renal cancer (28), but no direct analyis of tumor tissue
samples or a direct association with resistance to tyrosine kinase
inhibitors has been reported. Herein we report an analysis of the
corresponding cDNA sequence of the probable substrate binding
pocket of ABCG2 by direct sequencing. It has been hypothesized that
residue R482 in the transmembrane domain 3 (TM3) is likely to
interact with substrates based on the effect of R482G/T mutations
(29). The aforementioned mutations
generated gain-of-function mutants, resulting in resistance to a
wider range of substrates than the wild-type transporter.
Further mutagenesis studies showed that replacement
of arginine with virtually any residue that was not positively
charged led to a similar gain-of-function or change-of-function
(30). Based on these findings, it
was speculated that R482 must be part of the substrate-binding
pocket in the structure (20). Our
data shows a mutation resulting in Y459C in the intracellular
domain 1a (ICD1a). This position was identified as highly conserved
(20) and showed heterozygous
mutations from A to G at the nucleotide position 1376 in 3 out of
36 tumor samples. Based on the actual models (20), the apparent flexibility of the ICD1
may play a role in transmitting conformational changes from the
nucleotide binding domain to the transmembrane domain or vice
versa. The prediction of JPRED regarding secondary folding showed
an alteration in the adjacent helical structure supporting the
hypothesis of a structural change associated with this
mutation.
Two mutation-bearing tumor samples were clear cell
renal carcinomas, one sample included a chromophobe renal cell
carcinoma, therefore, association of the mutation with a certain
histological tumor type was not possible.
In future studies we will investigate tumor tissue
from renal cancer patients who receive treatment with tyrosine
kinase inhibitors to determine whether this mutation is associated
with increased tumor drug resistance or good response to therapy
with tyrosine kinase inhibitors.
The estimated rate of 8.3% among all renal cancer
patients makes this mutation particularly attractive with regard to
a possible pre-estimate of (non-surgical) therapeutic efficacy.
This is the first report on the sequence analysis of the substrate
binding pocket ABCG2 from tumor tissue of renal cell carcinoma.
References
|
1
|
Sagara N and Katoh M: Mitomycin C
resistance induced by TCF-3 overexpression in gastric cancer cell
line MKN28 is associated with DT-diaphorase down-regulation. Cancer
Res. 60:5959–5962. 2000.PubMed/NCBI
|
|
2
|
Haimeur A, Conseil G, Deeley RG and Cole
SPC: The MRP-related and BCRP/ABCG2 multidrug resistance proteins:
biology, substrate specificity and regulation. Curr Drug Metab.
5:21–53. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Allikmets R, Schriml LM, Hutchinson A,
Romano-Spica V and Dean M: A human placenta-specific ATP-binding
cassette gene (ABCP) on chromosome 4q22 that is involved in
multidrug resistance. Cancer Res. 58:5337–5339. 1998.PubMed/NCBI
|
|
4
|
Doyle LA, Yang W, Abruzzo LV, Krogmann T,
Gao Y, Rishi AK and Ross DD: A multidrug resistance transporter
from human MCF-7 breast cancer cells. Proc Natl Acad Sci USA.
95:15665–15670. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miyake K, Mickley L, Litman T, et al:
Molecular cloning of cDNAs which are highly overexpressed in
mitoxantrone-resistant cells: demonstration of homology to ABC
transport genes. Cancer Res. 59:8–13. 1999.
|
|
6
|
Ewart GD and Howells AJ: ABC transporters
involved in transport of eye pigment precursors in
Drosophilamelanogaster. Methods Enzymol. 292:213–224. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Brangi M, Litman T, Ciotti M, et al:
Camptothecin resistance: role of the ATP-binding cassette (ABC),
mitoxantrone-resistance half-transporter (MXR), and potential for
glucuronidation in MXR-expressing cells. Cancer Res. 59:5938–5946.
1999.PubMed/NCBI
|
|
8
|
Litman T, Brangi M, Hudson E, et al: The
multidrug-resistant phenotype associated with overexpression of the
new ABC half-transporter, MXR (ABCG2). J Cell Sci. 113:2011–2021.
2000.PubMed/NCBI
|
|
9
|
Maliepaard M, Scheffer GL, Faneyte IF, et
al: Subcellular localization and distribution of the breast cancer
resistance protein transporter in normal human tissues. Cancer Res.
61:3458–3464. 2001.PubMed/NCBI
|
|
10
|
Yang CH, Schneider E, Kuo ML, Volk EL,
Rocchi E and Chen YC: BCRP/MXR/ABCP expression in
topotecan-resistant human breast carcinoma cells. Biochem
Pharmacol. 60:831–837. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kawabata S, Oka M, Shiozawa K, et al:
Breast cancer resistance protein directly confers SN-38 resistance
of lung cancer cells. Biochem Biophys Res Commun. 280:1216–1223.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen YN, Mickley LA, Schwartz AM, Acton
EM, Hwang JL and Fojo AT: Characterization of adriamycin-resistant
human breast cancer cells which display overexpression of a novel
resistance-related membrane protein. J Biol Chem. 265:10073–10080.
1990.
|
|
13
|
Volk EL, Rohde K, Rhee M, McGuire JJ,
Doyle LA, Ross DD and Schneider E: Methotrexate cross-resistance in
a mitoxantrone-selected multidrug-resistant MCF7 breast cancer cell
line is attributable to enhanced energy-dependent drug efflux.
Cancer Res. 60:3514–3521. 2000.
|
|
14
|
Volk EL, Farley KM, Wu Y, Li F, Robey RW
and Schneider E: Overexpression of wild-type breast cancer
resistance protein mediates methotrexate resistance. Cancer Res.
62:5035–5040. 2002.PubMed/NCBI
|
|
15
|
Ifergan I, Shafran A, Jansen G, Hooijberg
JH, Scheffer GL and Assaraf YG: Folate deprivation results in the
loss of breast cancer resistance protein (BCRP/ABCG2) expression. A
role for BCRP in cellular folate homeostasis. J Biol Chem.
279:25527–25534. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shafran A, Ifergan I, Bram E, et al: ABCG2
harboring the Gly482 mutation confers high-level resistance to
various hydrophilic antifolates. Cancer Res. 65:8414–8422. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Houghton PJ, Germain GS, Harwood FC,
Schuetz JD, Stewart CF, Buchdunger E and Traxler P: Imatinib
mesylate is a potent inhibitor of the ABCG2 (BCRP) transporter and
reverses resistance to topotecan and SN-38 in vitro. Cancer Res.
64:2333–2337. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li J, Cusatis G, Brahmer J, et al:
Association of variant ABCG2 and the pharmacokinetics of epidermal
growth factor receptor tyrosine kinase inhibitors in cancer
patients. Cancer Biol Ther. 6:432–438. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Brendel C, Scharenberg C, Dohse M, et al:
Imatinib mesylate and nilotinib (AMN107) exhibit high-affinity
interaction with ABCG2 on primitive hematopoietic stem cells.
Leukemia. 21:1267–1275. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li Y, Polgar O, Okada M, Esser L, Bates SE
and Xia D: Towards understanding the mechanism of action of the
multidrug resistance-linked half-ABC transporter ABCG2: a molecular
modeling study. J Mol Graph Model. 25:837–851. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fairbrother WG, Yeo GW, Yeh R, Goldstein
P, Mawson M, Sharp PA and Burge CB: RESCUE-ESE identifies candidate
exonic splicing enhancers in vertebrate exons. Nucleic Acids Res.
32:W187–W190. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fairbrother WG, Holste D, Burge CB and
Sharp PA: Single nucleotide polymorphism-based validation of exonic
splicing enhancers. PLoS Biol. 2:E2682004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cuff JA, Clamp ME, Siddiqui AS, Finlay M
and Barton GJ: JPred: a consensus secondary structure prediction
server. Bioinformatics. 14:892–893. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Finn RD, Mistry J, Schuster-Bockler B, et
al: Pfam: clans, web tools and services. Nucleic Acids Res.
34:D247–D251. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Letunic I, Copley RR, Pils B, Pinkert S,
Schultz J and Bork P: SMART 5: domains in the context of genomes
and networks. Nucleic Acids Res. 34:D257–D260. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lambert C, Leonard N, De Bolle X and
Depiereux E: ESyPred3D: prediction of proteins 3D structures.
Bioinformatics. 18:1250–1256. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
To KKW, Zhan Z and Bates SE: Aberrant
promoter methylation of the ABCG2 gene in renal carcinoma. Mol Cell
Biol. 26:8572–8585. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Korenaga Y, Naito K, Okayama N, et al:
Association of the BCRP C421A polymorphism with nonpapillary renal
cell carcinoma. Int J Cancer. 117:431–434. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Honjo Y, Hrycyna CA, Yan QW, et al:
Acquired mutations in the MXR/BCRP/ABCP gene alter substrate
specificity in MXR/BCRP/ABCP-overexpressing cells. Cancer Res.
61:6635–6639. 2001.PubMed/NCBI
|
|
30
|
Ejendal KFK, Diop NK, Schweiger LC and
Hrycyna CA: The nature of amino acid 482 of human ABCG2 affects
substrate transport and ATP hydrolysis but not substrate binding.
Protein Sci. 15:1597–1607. 2006. View Article : Google Scholar : PubMed/NCBI
|