Introduction
RUNX1-RUNX1T1 [t(8;21)] or CBFB-MYH11 [inv(16)] fusion transcripts identify the core
binding factor (CBF) acute myeloid leukaemia (AML). Both t(8;21)
and inv(16) are characterised at
the molecular level by disruption of genes encoding different
subunits of CBF (1). CBF AML
represents 5–8% of all AML (2) and
has a relatively favourable prognosis, following treatment with
high dose cytarabine in the consolidation phase (3–5).
Mutations of c-KIT occur in 20–25% of t(8;21) and in approximately
30% of inv(16) cases (6). In CBF AML, c-KIT mutations occur
frequently within exon 17, which encodes the activation loop in the
kinase domain, and in exon 8, which encodes the extracellular
portion of the KIT receptor (7).
Older age, CD56 expression and activating c-KIT mutations are
reported to be associated with higher incidence of relapse and
lower survival (6,8,9) while
inv(16) patients with +22
secondary abnormality have a better prognosis (10,11).
However, no significant differences in overall survival (OS) rates
according to c-KIT mutation status have been reported in CBF AML
patients (12). In the present
study, we retrospectively analysed 23 patients with CBF AML in
order to investigate the incidence and prognostic value of c-KIT
mutations.
Materials and methods
Patients
Two hundred and forty-nine consecutive unselected
adult patients with newly diagnosed AML were admitted to the
Division of Haematology, Città della Salute e della Scienza,
University of Turin, Italy, from 2000 to 2011. Among these, 23
patients (12 female and 11 male) with de novo CBF AML were
retrospectively examined. The mean age was 42.7 years (range,
19–64). Diagnosis of CBF AML was performed according to the WHO
criteria (2). Inv(16) was present in 14 patients (60.8%), 9
with isolated inv(16) and 5 with
additional cytogenetic abnormalities. Nine patients (39.2%) showed
t(8;21); 7 had isolated t(8;21) and 2 t(8;21) with additional
cytogenetic aberrations. All patients received standard induction
chemotherapy with cytarabine, idarubicin and etoposide (ICE),
followed by consolidation treatment with high-dose cytarabine.
Thirteen patients with suitable HLA matched donors (related or
unrelated) underwent allogeneic stem cell transplantation in first
(10 cases) or second (3 cases) remission. To avoid confounding
effect of the transplant procedure, patients were censored at the
time of the transplantation. General informed consent was obtained
according to the local Ethics Committee guidelines. Samples were
numerically identified, maintaining patient anonymity.
Molecular analysis
c-KIT mutations in exons 8, 9, 10, 11, 13, 14 and 17
were assessed by polymerase chain reaction (PCR) amplification in
combination with direct sequencing from bone marrow (BM)
samples.
Amplification of c-KIT exons was performed by PCR
with specific oligonucleotide primers (Table I) (13–15),
and DNA sequencing was executed using the cDNA from AML BM samples.
Sequencing reactions were carried out using the BigDye Terminator
Cycle Sequencing Ready Reaction kit (Applied Biosystems, Foster
City, CA, USA), and the analysis was performed on an ABI 3130
automated capillary system. FLT3-ITD and D835 mutation status was
determined by conventional PCR and direct sequencing (16) and NPM1 mutation status was
determined by PCR-capillary electrophoresis methods (17), followed by direct sequencing for
positive sample characterization (18) (primers in Table I). The electropherograms were
compared to published germ-line sequences using basic local
alignment search tool (BLAST) on the Internet. Wilms tumour gene 1
(WT1) expression was quantified using a real-time quantitative PCR
(WT1 ELN kit, Nanogen, Buttigliera Alta, Turin, Italy).
 | Table IPrimer sequences for mutation
analysis. |
Table I
Primer sequences for mutation
analysis.
| Sequences |
|---|
| FLT3 ITD | F:
TGTCGAGCAGTACTCTAAACA |
| R:
ATCCTAGTACCTTCCCAAACTC |
| FLT3 D835 | F:
CCGCCAGGAACGGCTTG |
| R:
GCAGACGGGCATTGCCCC |
| NPM-I11f-FAM |
GTGGTAGAATGAAAAATAGAT |
| NPM-E12r |
CTTGGCAATAGAACCTGGAC |
| NPM1 | F:
TGGTTCTCTTCCCAAAGTGG |
| R:
CCTGGACAACATTTATCAAACACG |
| CK9 | F:
TCCTAGAGTAAGCCAGGGCTT |
| R:
TGGTAGACAGAGCCTAAACATCC |
| CK11 | F:
CCAGAGTGCTCTAATGACTG |
| R:
AGCCCCTGTTTCATACTGAC |
| CK13 | F:
GCTTGACATCAGTTTGCCAG |
| R:
AAAGGCAGCTTGGACACGGCTTTA |
| CK17 | F:
TGAACATCATTCAAGGCGTACTTTTG |
| R:
TTGAAACTAAAAATCCTTTGCAGGAC |
| CK14 | F:
TCTCACCTTCTTTCTAACCTTTTC |
| R:
AACCCTTATGACCCCATGAA |
| KIT10 | F:
TGCCAAAGTTTGTGATTCCA |
| R:
GTGGGGAGAAAGGGAAAAAT |
| CKIT8 | F:
GCAGCCTCAGGAAGGTTGTA |
| R:
AATTGCAGTCCTTCCCCTCT |
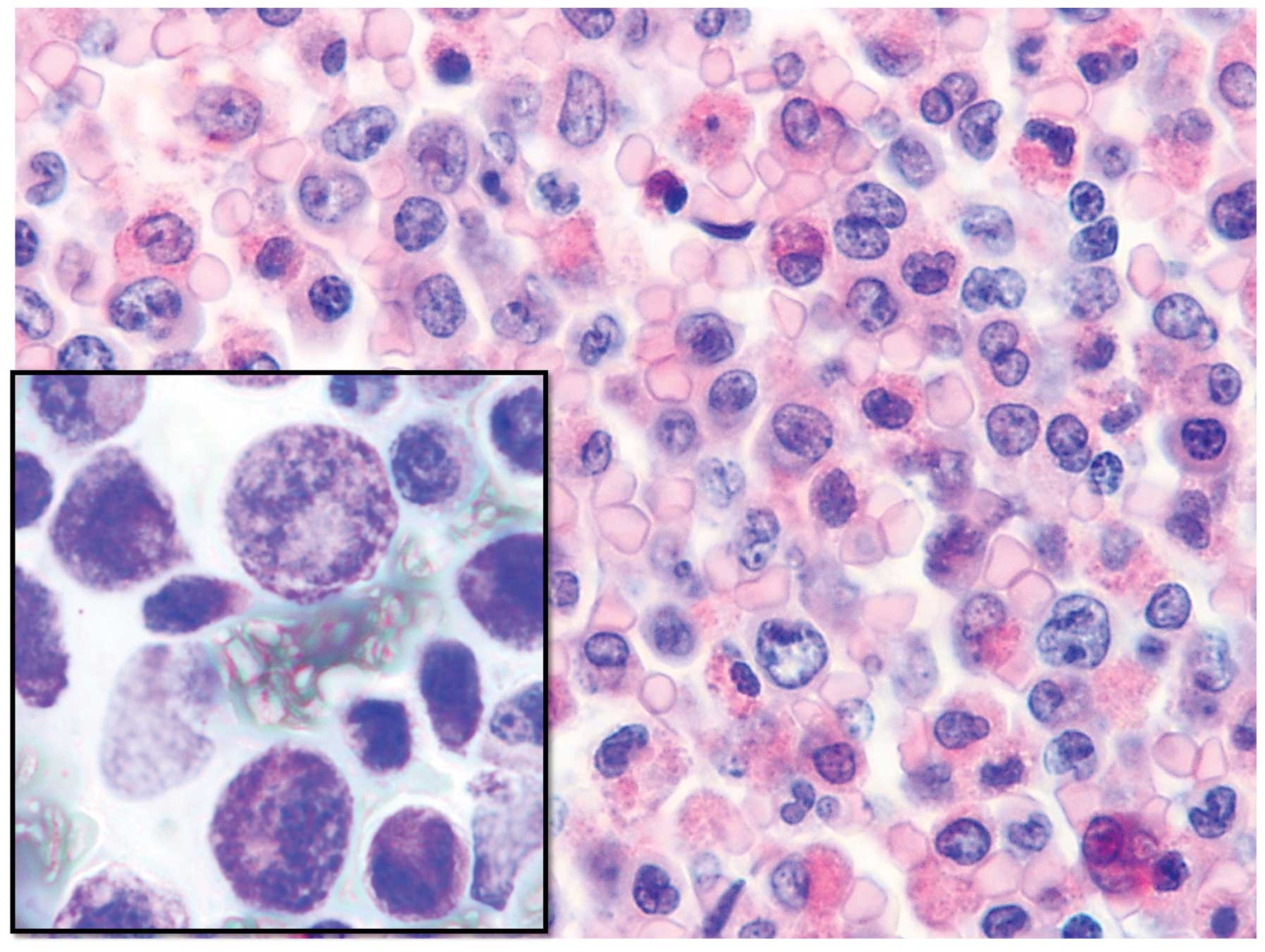
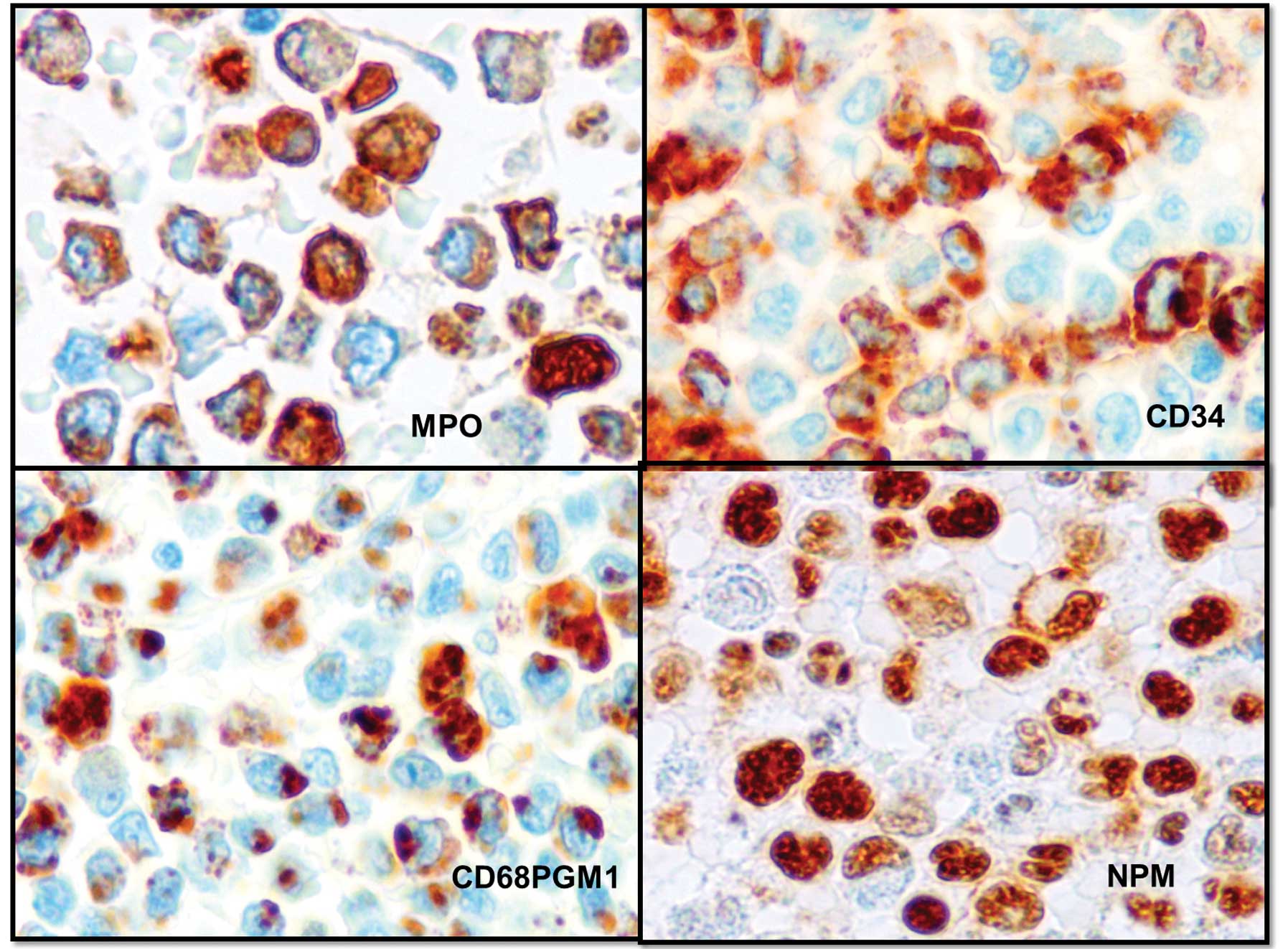
Histology
Formalin-fixed, paraffin-embedded BM biopsies were
stained with H&E, Dominici, Perls, reticulin and immunostained
with monoclonal antibodies anti-CD2, CD13, CD33, CD34, CD56 (all
from Novocastra, Newcastle, UK), anti-human nucleophosmin,
CD68PGM1, and polyclonal antibodies anti-human myeloperoxidase and
CD117 (all from Dako, Glostrup, Denmark) (Figs. 1 and 2).
Statistical analysis
The association between c-KIT mutation and clinical
or haematological parameters was assessed by the one-way analysis
of variance (ANOVA) and the Fisher’s exact test. Univariate
survival analyses were based on Kaplan-Meier product-limit
estimates of survival distribution, and differences between
survival curves were tested using the Cox-Mantel test.
Results
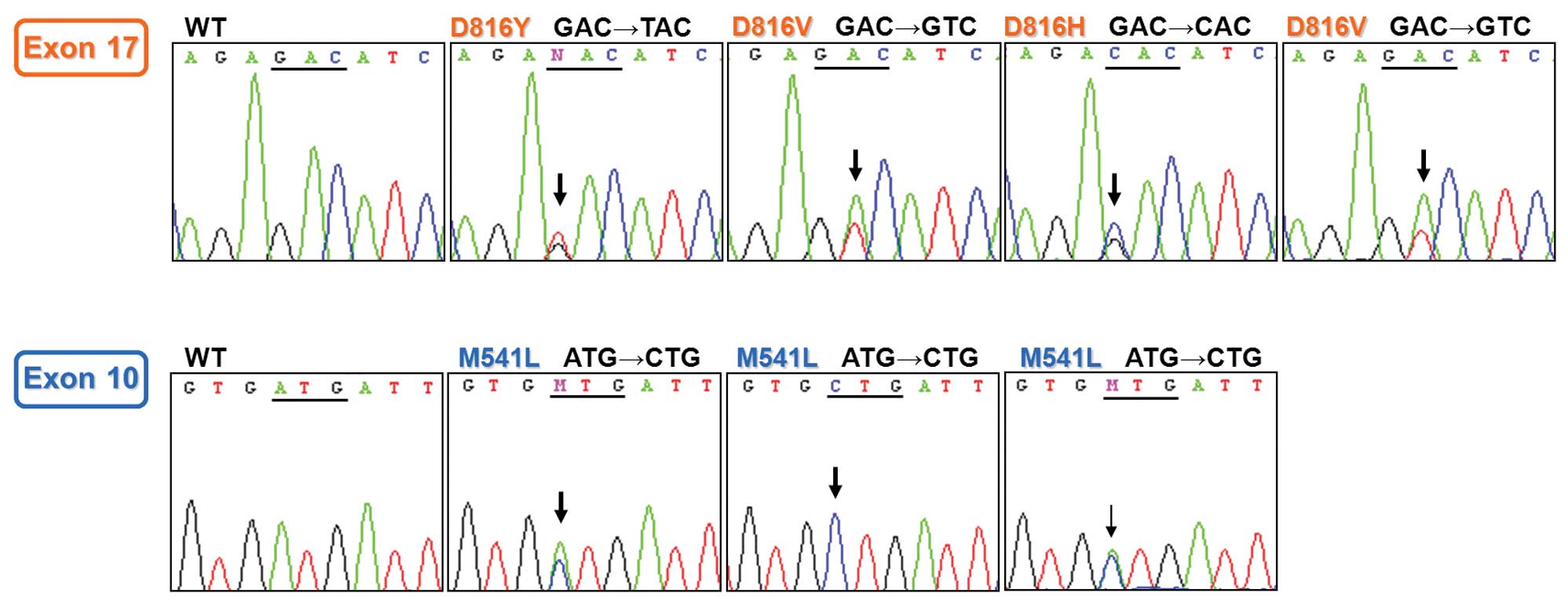
c-KIT mutations were detected in 7/23 (30.4%)
patients. M541L mutation (exon 10) was found in 3 samples and D816V
or D816H or D816Y mutation (exon 17) in 4. Two SNPs (K546K and
I798I) were detected in 6 AML samples (Table II). c-KIT mutation
electropherograms are shown in Fig.
3. FLT3 ITD, FLT3 D835 and NPM1 mutations rarely occurred (data
not shown).
 | Table IIc-KIT mutations observed in 23 CBF AML
cases. |
Table II
c-KIT mutations observed in 23 CBF AML
cases.
| No. of cases | c-KIT mutated | Mutation type | c-KIT negative
(polymorphism) | Polymorphism |
|---|
| t(8;21) | 9 | 3 | D816H (exon 17) | 6 (3) | I798I |
| | | D816V (exon 17) | | I798I |
| | | M541L (exon
10) | | I798I, K546K
(simultaneous) |
| inv(16) | 14 | 4 | D816Y (exon
17) | 10 (3) | K546K |
| | | D816V (exon
17) | | I798I |
| | | M541L (exon
10) | | K546K |
| | | M541L (exon
10) | | |
| Total | 23 | | | | |
Association between c-KIT mutation and
clinical and haematological characteristics
c-KIT mutations were detected in 3/9 (33.3%)
patients with t(8;21) and in 4/14 (28.6%) patients with
inv(16). No significant difference
in c-KIT mutation was found between cases with t(8;21) or
inv(16) alone and cases with
additional cytogenetic aberrations (Tables III and IV).
 | Table IIIAssociation between c-KIT mutations
and t(8;21) AML (N=9). |
Table III
Association between c-KIT mutations
and t(8;21) AML (N=9).
| No. of cases | t(8;21) alone | t(8;21) plus
additional cytogenetic abnormalities | P-value |
|---|
| Mutation | 3 | 2 | 1 | 0.58 |
| No mutation | 6 | 5 | 1 | |
| Total | 9 | 7 | 2 | |
 | Table IVAssociation between c-KIT mutations
and inv(16) AML (N=14). |
Table IV
Association between c-KIT mutations
and inv(16) AML (N=14).
| No. of cases | inv(16) alone | inv(16) plus
additional cytogenetic abnormalities | P-value |
|---|
| Mutation | 4 | 2 | 2 | 0.45 |
| No mutation | 10 | 7 | 3 | |
| Total | 14 | 9 | 5 | |
c-KIT mutation status was not associated with
gender, age, white blood cell and platelet count, percentage of
peripheral blood and bone marrow blasts at diagnosis, cytogenetic
risk groups and WT1 levels. Also, no association was found for the
achievement of complete remission (CR), although the two patients
who did not achieve CR were non-mutated. On the contrary, lactate
dehydrogenase (LDH) levels were higher (1386 UI/l) in c-KIT mutated
than in non-mutated patients (753 UI/l; P=0.01) (Table V).
 | Table VAssociation between c-KIT mutation
and clinical and haematological characteristics in CBF AML
(N=23). |
Table V
Association between c-KIT mutation
and clinical and haematological characteristics in CBF AML
(N=23).
| | c-KIT mutated
(n=7) | c-KIT non mutated
(n=16) | |
|---|
| |
|
| |
|---|
| Variables | No. of cases | Mean ± SD | Mean ± SD | P-value |
|---|
| Age (years) | 23 | 51±11.2 | 39±13.4 | 0.06 |
| WBC count
(x109/l) | 23 | 34.045±33.9 | 21.702±19.918 | 0.3 |
| Plt count
(x109/l) | 23 | 30.428±31.320 | 46.133±24.023 | 0.2 |
| LDH (UI/l) | 23 | 1,386±629 | 753±312 | 0.01 |
| PB blasts (%) | 23 | 48.43±23.04 | 54.92±19.67 | 0.5 |
| BM blasts (%) | 23 | 48.85±24.88 | 60.64±14.25 | 0.17 |
| WT1 (number of WT1
copies/104 ABL copies) | 15 | 17,307±22,628
(4) | 15,687±17,780
(11) | 0.8 |
| Gender |
| Male | 11 | 3/7 | 8/16 | |
| Female | 12 | 4/7 | 8/16 | 0.5 |
| Cytogenic risk |
| Low | 18 | 6/7 | 12/16 | |
| High | 5 | 1/7 | 4/16 | 0.5 |
| Remission |
| Complete
remission | 21 | 7/7 | 14/16 | |
| No remission | 2 | 0/7 | 2/16 | 0.5 |
Correlation of c-KIT mutation with
overall and disease-free survival
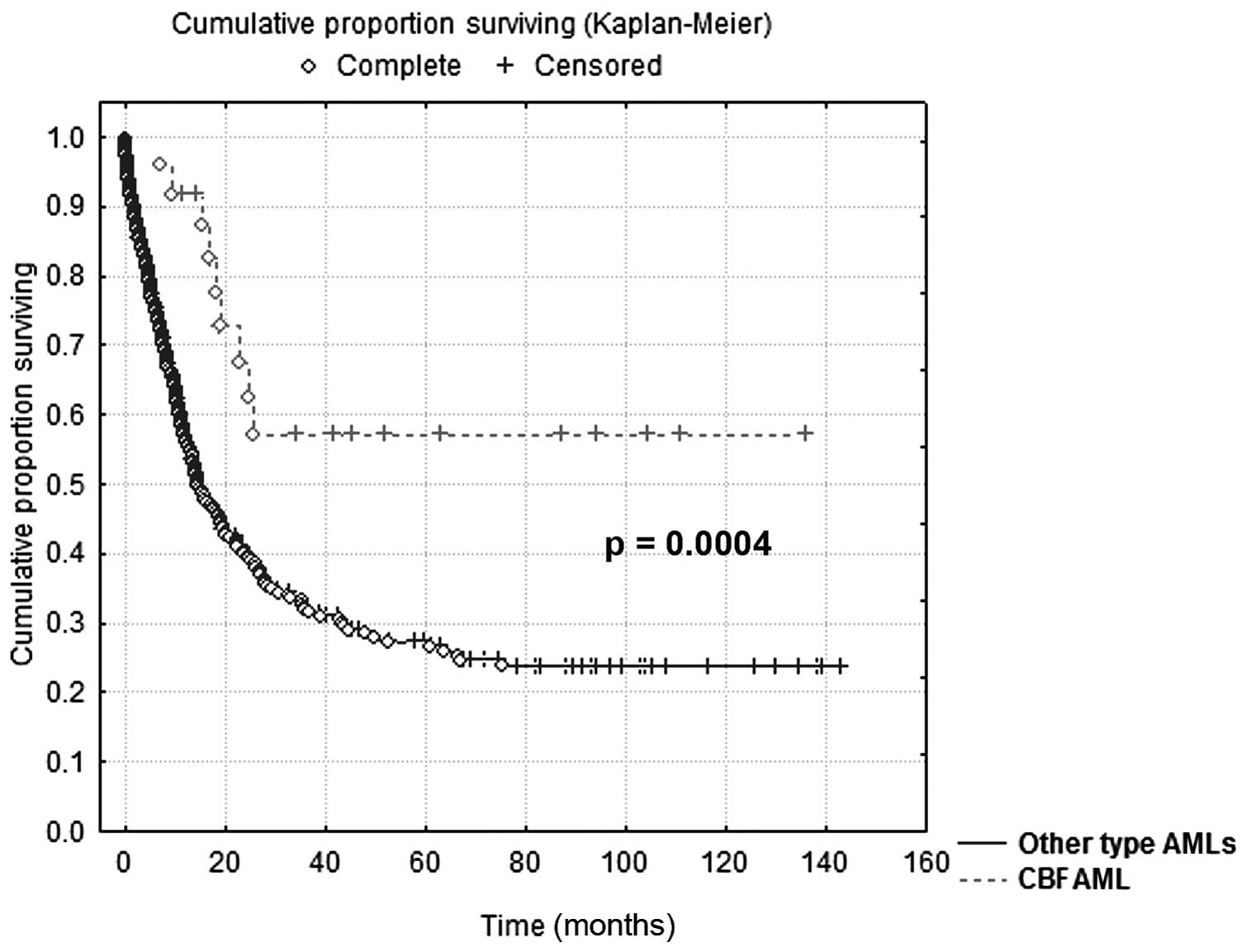
In the 23 CBF AML patients OS was significantly
longer than in the 226 patients with other types of AML treated at
the same institution during the same period; at the 10-year
follow-up, 57% of CBF AML patients were alive compared to 24% of
patients with all other AML categories (P=0.0004) (Fig. 4).
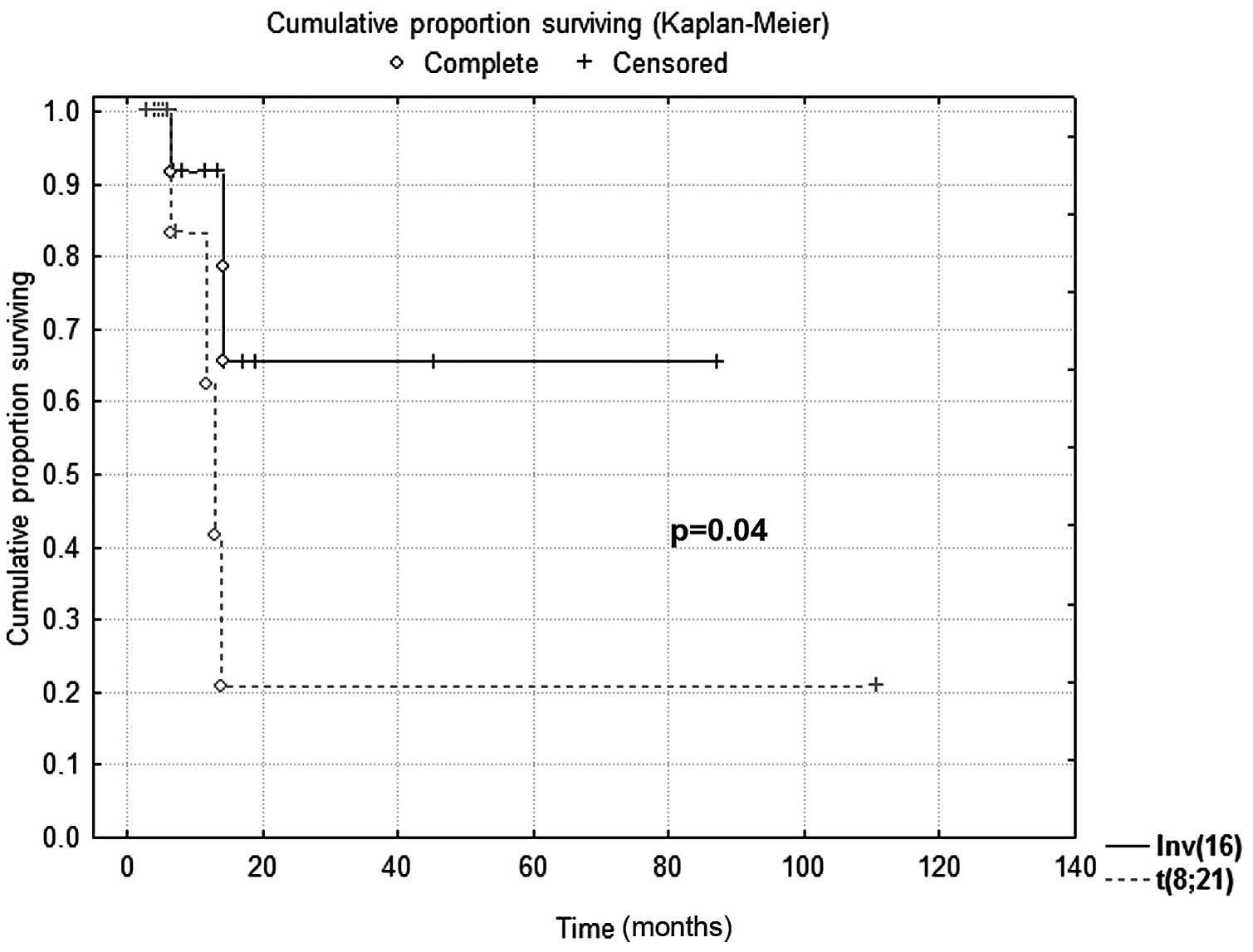
No difference in OS was found between inv(16) and t(8;21) CBF AML; after 88 months,
76% of inv(16) and 60% of t(8;21)
patients were alive, respectively (P=0.6). However, DFS for
inv(16) AML was significantly
longer than that for t(8;21) cases; after 88 months, 67% of
inv(16) patients were free of the
disease, vs. 20% of those with t(8;21) (P=0.04) (Fig. 5).
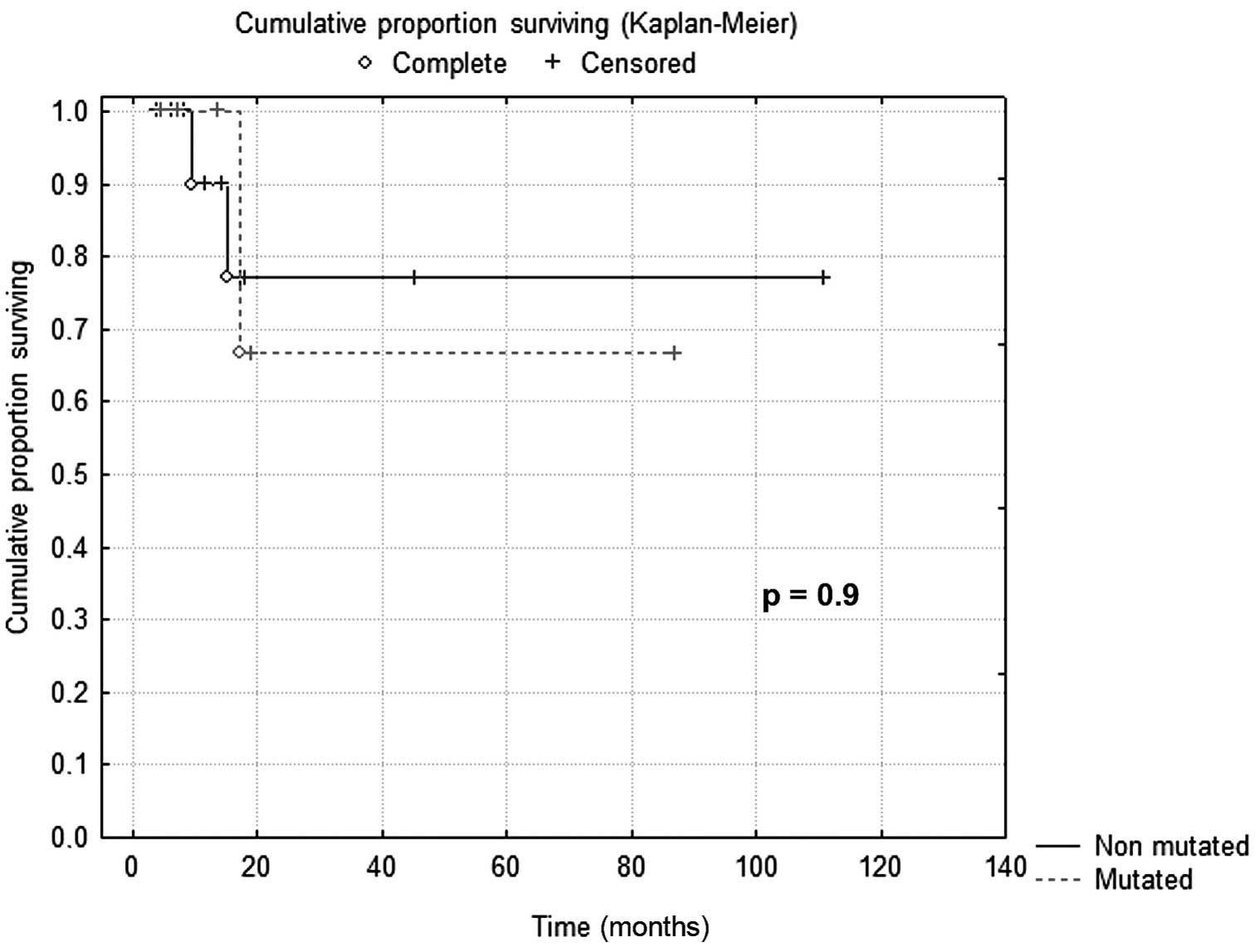
No difference in OS was found when CBF AML patients
were categorised according to c-KIT mutation; after 88 months, 78%
of c-KIT non-mutated and 68% of mutated patients were alive,
respectively (P=0.9) (Fig. 6). DFS
was similar in c-KIT mutated and non-mutated CBF AML patients
(P=0.6).
Discussion
Our results showed an overall incidence of c-KIT
mutation in 30.4% of cases, as previously reported in adult CBF AML
(6), and a better prognosis for CBF
AML than for cytogenetically normal or other subtypes of AML, which
is in agreement with previous data (19,20).
In our study, inv(16) AML had a
significantly longer DFS than t(8;21) AML, consistent with previous
reports demonstrating that patients with t(8;21) have significantly
shorter survival times after relapse than patients with
inv(16), possibly related to a
lower response to salvage treatment in patients with
t(8;21)(10,11,21).
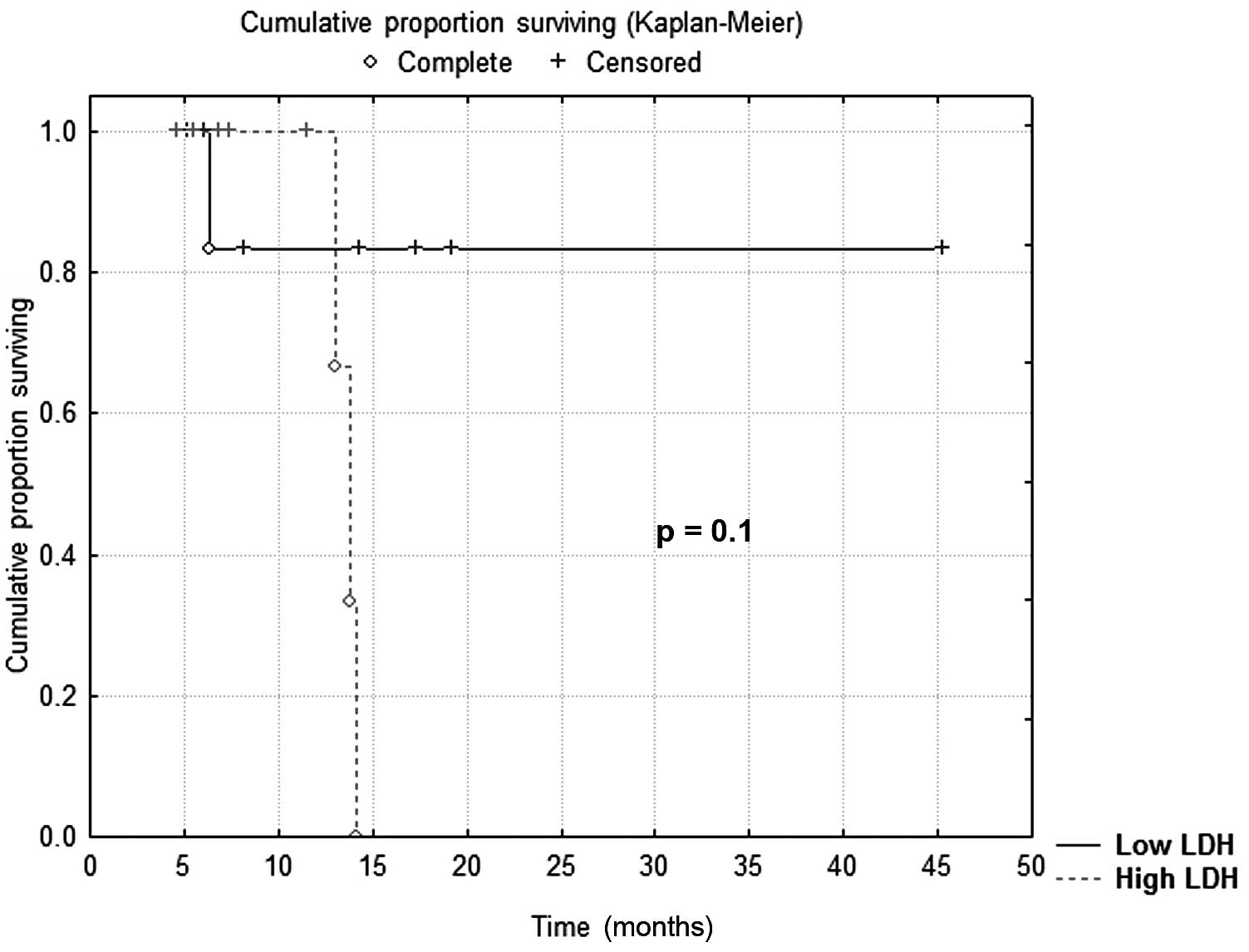
c-KIT mutations in our CBF AMLs were associated with
higher LDH levels, suggesting a possible prognostic role. It is
well known that high LDH values are associated with a poorer
outcome both in AML and myelodysplastic syndromes (MDS) (22–24).
This was observed in our study as well; when cases were categorised
according to the median LDH value (880 UI/l), all patients with
higher LDH values relapsed after 15 months, while 84% of patients
with lower LDH values were free of the disease. However, possibly
due to the small number of cases, the result is only of borderline
significance (P=0.1) (Fig. 7). The
association between c-KIT mutation and LDH levels is likely to
indicate a more active proliferation in mutated CBF AML.
Contrary to most published studies, no association
was found in our CBF AML group between c-KIT mutations and
achievement of CR, OS and DFS; this may be due to the small number
of cases and to considering CBF AML as a single group. Indeed,
previous reports showed a prognostic value of c-KIT mutations in
t(8;21) but not in inv(16) CBF AML
(7,25). Therefore, t(8;21) and inv(16) AML should be regarded as distinct
clinical entities to be stratified and reported separately, as
already suggested (11), and
possibly treated with a tailored approach (26).
Therefore, further studies are required to clarify
the prognostic value of c-KIT mutations in newly diagnosed adult
AML.
Acknowledgements
This study was supported by grants from the Italian
Ministero dell’Università e Ricerca Scientifica e Tecnologica
(MURST).
References
|
1
|
Speck NA and Gilliland DG: Core-binding
factors in haematopoiesis and leukaemia. Nat Rev Cancer. 2:502–513.
2002. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Arber DA, Brunning RD, Le Beau MM, Falini
B, Vardiman JW, Porwit A, Thiele J and Bloomfield CD: Acute myeloid
leukaemia with recurrent genetic abnormalities. WHO Classification
of Tumours of Haematopoietic and Lymphoid Tissues. Swerdlow SH,
Campo E, Harris NL, Jaffe ES, Pileri S, Stein H, Thiele J and
Vardiman JW: 4th edition. IARC Press; Lyon: pp. 110–112. 2008
|
|
3
|
Mrózek K, Heinonen K, Lawrence D, Carroll
AJ, Koduru PR, Rao KW, Strout MP, Hutchison RE, Moore JO, Mayer RJ,
Schiffer CA and Bloomfield CD: Adult patients with de novo acute
myeloid leukemia and t(9;11)(p22;q23) have a superior outcome to
patients with other translocations involving band 11q23: a Cancer
and Leukemia Group B Study. Blood. 90:4532–4538. 1997.PubMed/NCBI
|
|
4
|
Bloomfield CD, Lawrence D, Byrd JC,
Carroll A, Pettenati MJ, Tantravahi R, Patil SR, Davey FR, Berg DT,
Schiffer CA, Arthur DC and Mayer RJ: Frequency of prolonged
remission duration after high-dose cytarabine intensification in
acute myeloid leukemia varies by cytogenetic subtype. Cancer Res.
58:4173–4179. 1998.PubMed/NCBI
|
|
5
|
Grimwade D, Walker H, Oliver F, Wheatley
K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A and
Goldstone A: The importance of diagnostic cytogenetics on outcome
in AML: analysis of 1,612 patients entered into the MRC AML 10
trial. The Medical Research Council Adult and Children’s Leukaemia
Working Parties. Blood. 92:2322–2333. 1998.PubMed/NCBI
|
|
6
|
Paschka P, Marcucci G, Ruppert AS, Mrózek
K, Chen H, Kittles RA, Vukosavljevic T, Perrotti D, Vardiman JW,
Carroll AJ, Kolitz JE, Larson RA and Bloomfield CD; Cancer and
Leukemia Group B. Adverse prognostic significance of KIT mutations
in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer
and Leukemia Group B Study. J Clin Oncol. 24:3904–3911. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park SH, Chi HS, Min SK, Park BG, Jang S
and Park CJ: Prognostic impact of c-KIT mutations in core binding
factor acute myeloid leukemia. Leuk Res. 35:1376–1383. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Baer MR, Stewart CC, Lawrence D, Arthur
DC, Byrd JC, Davey FR, Schiffer CA and Bloomfield CD: Expression of
the neural cell adhesion molecule CD56 is associated with short
remission duration and survival in acute myeloid leukemia with
t(8;21)(q22;q22). Blood. 90:1643–1648. 1997.PubMed/NCBI
|
|
9
|
Delaunay J, Vey N, Leblanc T, Fenaux P,
Rigal-Huguet F, Witz F, Lamy T, Auvrignon A, Blaise D, Pigneux A,
Mugneret F, Bastard C, Dastugue N, Van den Akker J, Fière D,
Reiffers J, Castaigne S, Leverger G, Harousseau JL and Dombret H;
French Acute Myeloid Leukemia Intergroup; Groupe Ouest-Est des
Leucémies Aiguës Myéoblastiques; Leucémies Aiguës Myéoblastiques de
l’Enfant; Acute Leukemia French Association;
Bordeaux-Grenoble-Marseille-Toulouse cooperative groups. Prognosis
of inv(16)/t(16;16) acute myeloid leukemia (AML): a survey of 110
cases from the French AML Intergroup. Blood. 102:462–469. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schlenk RF, Benner A, Krauter J, Büchner
T, Sauerland C, Ehninger G, Schaich M, Mohr B, Niederwieser D,
Krahl R, Pasold R, Döhner K, Ganser A, Döhner H and Heil G:
Individual patient data-based meta-analysis of patients aged 16 to
60 years with core binding factor acute myeloid leukemia: a survey
of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol.
22:3741–3750. 2004.PubMed/NCBI
|
|
11
|
Marcucci G, Mrózek K, Ruppert AS, Maharry
K, Kolitz JE, Moore JO, Mayer RJ, Pettenati MJ, Powell BL, Edwards
CG, Sterling LJ, Vardiman JW, Schiffer CA, Carroll AJ, Larson RA
and Bloomfield CD: Prognostic factors and outcome of core binding
factor acute myeloid leukemia patients with t(8;21) differ from
those of patients with inv(16): a Cancer and Leukemia Group B
study. J Clin Oncol. 23:5705–5717. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Marková J, Marková J, Trnková Z, Michková
P, Maaloufová J, Starý J, Cetkovský P and Schwarz J: Monitoring of
minimal residual disease in patients with core binding factor acute
myeloid leukemia and the impact of C-KIT, FLT3, and JAK2 mutations
on clinical outcome. Leuk Lymphoma. 50:1448–1460. 2009.PubMed/NCBI
|
|
13
|
Lasota J, Wozniak A, Sarlomo-Rikala M, Rys
J, Kordek R, Nassar A, Sobin LH and Miettinen M: Mutations in exons
9 and 13 of KIT gene are rare events in gastrointestinal stromal
tumors. A study of 200 cases. Am J Pathol. 157:1091–1095. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rubin BP, Singer S, Tsao C, Duensing A,
Lux ML, Ruiz R, Hibbard MK, Chen CJ, Xiao S, Tuveson DA, Demetri
GD, Fletcher CD and Fletcher JA: KIT activation is a ubiquitous
feature of gastrointestinal stromal tumors. Cancer Res.
61:8118–8121. 2001.PubMed/NCBI
|
|
15
|
Miselli FC, Casieri P, Negri T, Orsenigo
M, Lagonigro MS, Gronchi A, Fiore M, Casali PG, Bertulli R, Carbone
A, Pierotti MA, Tamborini E and Pilotti S: c-Kit/PDGFRA gene status
alterations possibly related to primary imatinib resistance in
gastrointestinal stromal tumors. Clin Cancer Res. 13:2369–2377.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kottaridis PD, Gale RE and Linch DC: Flt3
mutations and leukaemia. Br J Haematol. 122:523–538. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Thiede C, Koch S, Creutzig E, Steudel C,
Illmer T, Schaich M and Ehninger G: Prevalence and prognostic
impact of NPM1 mutations in 1485 adult patients with acute myeloid
leukemia (AML). Blood. 107:4011–4020. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Verhaak RG, Goudswaard CS, van Putten W,
Bijl MA, Sanders MA, Hugens W, Uitterlinden AG, Erpelinck CA,
Delwel R, Löwenberg B and Valk PJ: Mutations in nucleophosmin
(NPM1) in acute myeloid leukemia (AML): association with other gene
abnormalities and previously established gene expression signatures
and their favorable prognostic significance. Blood. 106:3747–3754.
2005. View Article : Google Scholar
|
|
19
|
Gulley ML, Shea TC and Fedoriw Y: Genetic
tests to evaluate prognosis and predict therapeutic response in
acute myeloid leukemia (Review). J Mol Diagn. 12:3–16. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sangle NA and Perkins SL: Core-binding
factor acute myeloid leukemia. Arch Pathol Lab Med. 135:1504–1509.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Appelbaum FR, Kopecky KJ, Tallman MS,
Slovak ML, Gundacker HM, Kim HT, Dewald GW, Kantarjian HM, Pierce
SR and Estey EH: The clinical spectrum of adult acute myeloid
leukaemia associated with corebinding factor translocations. Br J
Haematol. 135:165–173. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kern W, Haferlach T, Schoch C, Loffler H,
Gassmann W, Heinecke A, Sauerland MC, Berdel W, Buchner T and
Hiddemann W: Early blast clearance by remission induction therapy
is a major independent prognostic factor for both achievement of
complete remission and long-term outcome in acute myeloid leukemia:
data from the German AML Cooperative Group (AMLCG) 1992 Trial.
Blood. 101:64–70. 2003. View Article : Google Scholar
|
|
23
|
Germing U, Hildebrandt B, Pfeilstöcker M,
Nösslinger T, Valent P, Fonatsch C, Lübbert M, Haase D, Steidl C,
Krieger O, Stauder R, Giagounidis AA, Strupp C, Kündgen A, Mueller
T, Haas R, Gattermann N and Aul C: Refinement of the international
prognostic scoring system (IPSS) by including LDH as an additional
prognostic variable to improve risk assessment in patients with
primary myelodysplastic syndromes (MDS). Leukemia. 19:2223–2231.
2005. View Article : Google Scholar
|
|
24
|
Spoo AC, Lübbert M, Wierda WG and Burger
JA: CXCR4 is a prognostic marker in acute myelogenous leukemia.
Blood. 109:786–791. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Boissel N, Leroy H, Brethon B, Philippe N,
de Botton S, Auvrignon A, Raffoux E, Leblanc T, Thomas X, Hermine
O, Quesnel B, Baruchel A, Leverger G, Dombret H and Preudhomme C;
Acute Leukemia French Association (ALFA); Leucémies Aiguës
Myéloblastiques de l’Enfant (LAME) Cooperative Groups. Incidence
and prognostic impact of c-Kit, FLT3, and Ras gene mutations in
core binding factor acute myeloid leukemia (CBF-AML). Leukemia.
20:965–970. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dombret H, Preudhomme C and Boissel N:
Core binding factor acute myeloid leukemia (CBF-AML): is high-dose
Ara-C (HDAC) consolidation as effective as you think? Curr Opin
Hematol. 16:92–97. 2009. View Article : Google Scholar : PubMed/NCBI
|