Introduction
Bisphosphonates (BPs) are stable analogues of
pyrophosphate with P-C-P structure and 2 side chains attached to
the carbon atom. BPs, approved for clinical use, differ based on
structural alterations of the so called R-2 side chain, which
determines the efficiency as inhibitor of bone resorption (1,2). Drug
potency has increased with each successive generation, as the R-2
side chain was lengthened and an amino group incorporated. Until
now, osteonecrosis of the jaws (ONJ) has been described only in
patients undergoing treatment with amino-group-containing BPs,
which are much more potent than of that the non-amino group
drug.
BPs act through the inhibition of bone resorption
and are used in combination with antineoplastic chemotherapy for
treatment of hypercalcaemia associated with malignancy, lytic bone
metastasis and multiple myeloma (3). Several cases describing a correlation
between osteonecrosis of the jaws and intravenous administration of
BPs have been recently reported in literature (4,5).
Different definitions for ONJ have been proposed and
all include exposure of maxillary or mandibular bone, but a breach
in the oral mucosa is an absolute requirement. At the present time,
it is in fact, not definitively known if the ONJ lesion originates
in the bone, or whether it may initiate in the oral mucosa.
The clinical examination of patients needs to be
accompanied by a careful evaluation of the imaging features of bone
lesions to better understand their extent and features. Digital
panoramic radiography, computed tomography (CT) scan, magnetic
resonance imaging (MRI) and 99Tcm-MDP three-phase bone scan are
diagnostic tools that add value to the clinical findings by
revealing different aspects of bone involvement.
Since 2003, numerous reports of
bisphosphonate-induced osteonecrosis of the jaws have been reported
in literature (6). Several theories
have been proposed regarding the etiopathology of ONJ, e.g. that
necrosis is related to an over suppression of bone turnover by BPs
(7,8) or that BPs decrease angiogenesis
(9–11).
The jaw bones are separated from a trauma-intense
and microbiologically diverse oral environment by thin mucosa and
periosteum. Minor trauma may cause local damage to the thin
barrier, leading to bone necrosis. Besides, teeth are usually
infected by bacteria that cause caries or periodontal disease and
are separated from periodontal tissue ~2 mm. This condition allows
the access of the infection to underlying bone (12) coupled with chronic invasive dental
treatments and the thin mucosa over bone, this anatomical
concentration of BPs causes this condition to be manifested
exclusively in the jaws. Oral infections are a considerable problem
in patients with cancer treated with intensive chemotherapy
regimens, including hematopoietic stem-cell transplant procedures.
These infections are caused by the complex interaction between the
toxicity of cancer chemotherapy for oral mucosal tissue.
Thus, the aim of the present study was to evaluate
human gingival epithelium and underlying bone after BPs
administration and to analyze the structural damage of the mucosa
in ONJ patients correlated to damage of the bone. We examined the
effects of zoledronate and aledronate, nitrogen-containing BPs, on
human oral mucosa and the underlying mandibular bone.
We demonstrated that BPs induce changes in
expression of adhesion to cell-cell/cell-matrix proteins in human
oral mucosa. In addition, we demonstrated that a gradual decrease
of adhesion proteins correlate with bone damage.
Materials and methods
Samples of human gingival epithelium and bone tissue
were obtained from 12 patients, 6 affected by ONJ and treated with
alendronate orally administered (70 mg for week), and 6 affected by
cancer as well as breast or prostatic cancer treated with
zoledronate (4 mg for month) by intravenous infusion over at least
15 min. Both BPs have a light chain attached to the central carbon
atom increasing efficacy of drug but also its toxicity.
All patients showed exposing bone areas of jaw.
Biopsies were obtained during sequestrectomy intervention removing
necrotic bone and relative perilesional gingival mucosa.
In another group of subjects who had undergone oral
procedures for other reasons, not treated with BPs, intrasurgical
biopsies were obtained and then used as normal control.
The age of the patients ranged between 30 and 81
years and all gave their informed consent. The procedures followed
were in accordance with the principles outlined in the Helsinki
Declaration of 1975.
The biopsies were treated to study the bone tissue
by scanning electron microscopy and the gingival mucosa by
immunohistochemistry method.
Scanning electron microscopy
The biopsy specimens utilized for the scanning
electron microscopy were fixed for 24 h in 2.5% glutaraldehyde in
0.1 M phosphate buffer at pH 7.4 at room temperature. The specimens
were dehydrated through a gradual increase in concentrations of
ethanol and amile acetate; they were then dried at critical-point
in a Balzers critical point drier using liquid CO2. The
fractured surfaces of bone were then mounted on stub and platinum
coated with a sputtering system ‘Plasma Sciences CrC-100 Turbo
Pumped’ and observed by Phenom G2 pro scanning electron
microscope.
Immunohistochemistry
Biopsies of gingival mucosa were fixed in 3%
paraformaldehyde in 0.2 M phosphate buffer, pH 7.4, for 2 h at room
temperature. They were then washed extensively with 0.2 M phosphate
buffer, pH 7.4, and then with phosphate-buffered saline (PBS),
containing 12 and 18% sucrose. The samples were snap-frozen in
liquid nitrogen and 20 μm sections were prepared in a cryostat for
their use in a protocol for immunofluorescence. The sections were
placed on glass slides that were coated with 0.5% gelatin and
0.005% chromium potassium sulphate. To block non-specific binding
sites and to permeabilize the membranes, the sections were
preincubated with 1% bovine serum albumin (BSA), 0.3% Triton X-100
in PBS at room temperature for 15 min. Finally, the sections were
incubated with primary antibodies against sarcoglycans and
integrins in order to value adhesion zones cell-cell and
cell-extracellular matrix of gingival mucosa.
The following antibodies for double fluorescence
were used: anti-α-sarcoglycan diluted 1:100, anti-β-sarcoglycan
diluted 1:200, anti-γ-sarcoglycan diluted 1:100, anti-δ-sarcoglycan
diluted 1:50, anti-ɛ-sarcoglycan diluted 1:100 (all from Novocastra
Laboratories, Newcastle upon Tyne, UK); anti-β1-integrin diluted
1:100, and anti-α6-integrin diluted 1:100 (both from Sigma
Chemicals, St. Louis, MO, USA); anti-α2-integrin diluted 1:100
(Jackson ImmunoResearch Laboratories, West Grove, PA, USA). In all
reactions, Texas Red conjugated IgG anti-goat (red channel), and
FITCconjugated IgG anti-mouse (green channel), all from Jackson
ImmunoResearch Laboratories, were used respectively.
Slides were finally washed in PBS and sealed with
mounting medium. The sections were then analyzed and images
acquired using a Zeiss LSM 5 DUO confocal laser scanning microscope
by META module. All images were digitalized at a resolution of 8
bits into an array of 2048 × 2048 pixels. Optical sections of
fluorescent specimens were obtained using a HeNe laser (wavelength,
543 nm) and an Argon laser (wavelength, 458 nm) at a 1-min 2-sec
scanning speed with up to 8 averages; 1.50 μm-thick sections were
obtained using a pinhole of 250. Contrast and brightness were
established by examining the most brightly labeled pixels and
choosing the settings that allowed clear visualization of the
structural details while keeping the pixel intensity at its highest
(~200).
Each image was acquired within 62 sec, in order to
minimize photodegradation. Digital images were cropped and the
figure montage prepared using Adobe Photoshop 7.0.
Results
Scanning electron microscopy
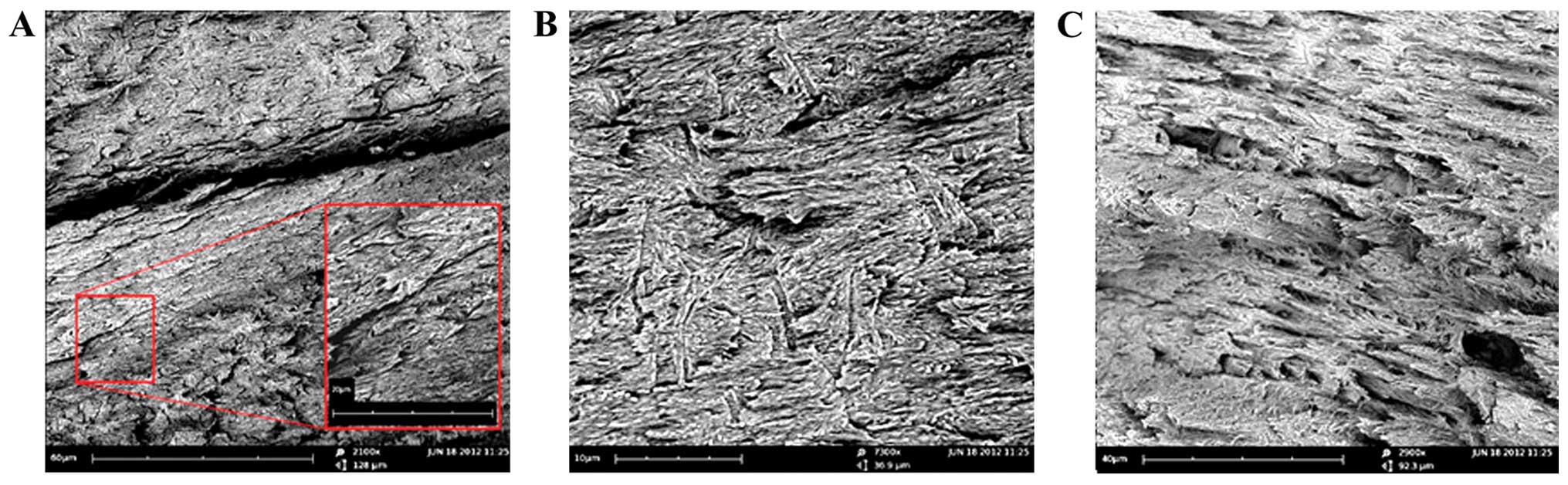
On healthy subject, the observation of the fracture
surface in biopsy of the jaw bone, show the presence of bone
lamellae parallel to each other and partially overlapping like roof
tiles, alternating to bone lamellae with the same architecture, but
with opposite orientation (Fig.
1A). A higher magnification allow to show, in each flap, bands
of fibrillar subunits with parallel arrangement to each other and
parallel to the major axis of the lamellae (insert in Fig. 1A). On a fracture in orthogonal plane
to that previously described, are several furrows transversely
oriented to the major axis of lamellae, which frequently bifurcate
to Y (Fig. 1B); at higher
magnification, the morphology of the furrows with fibrillar
subunits of the lamellae can be clearly seen (Fig. 1C).
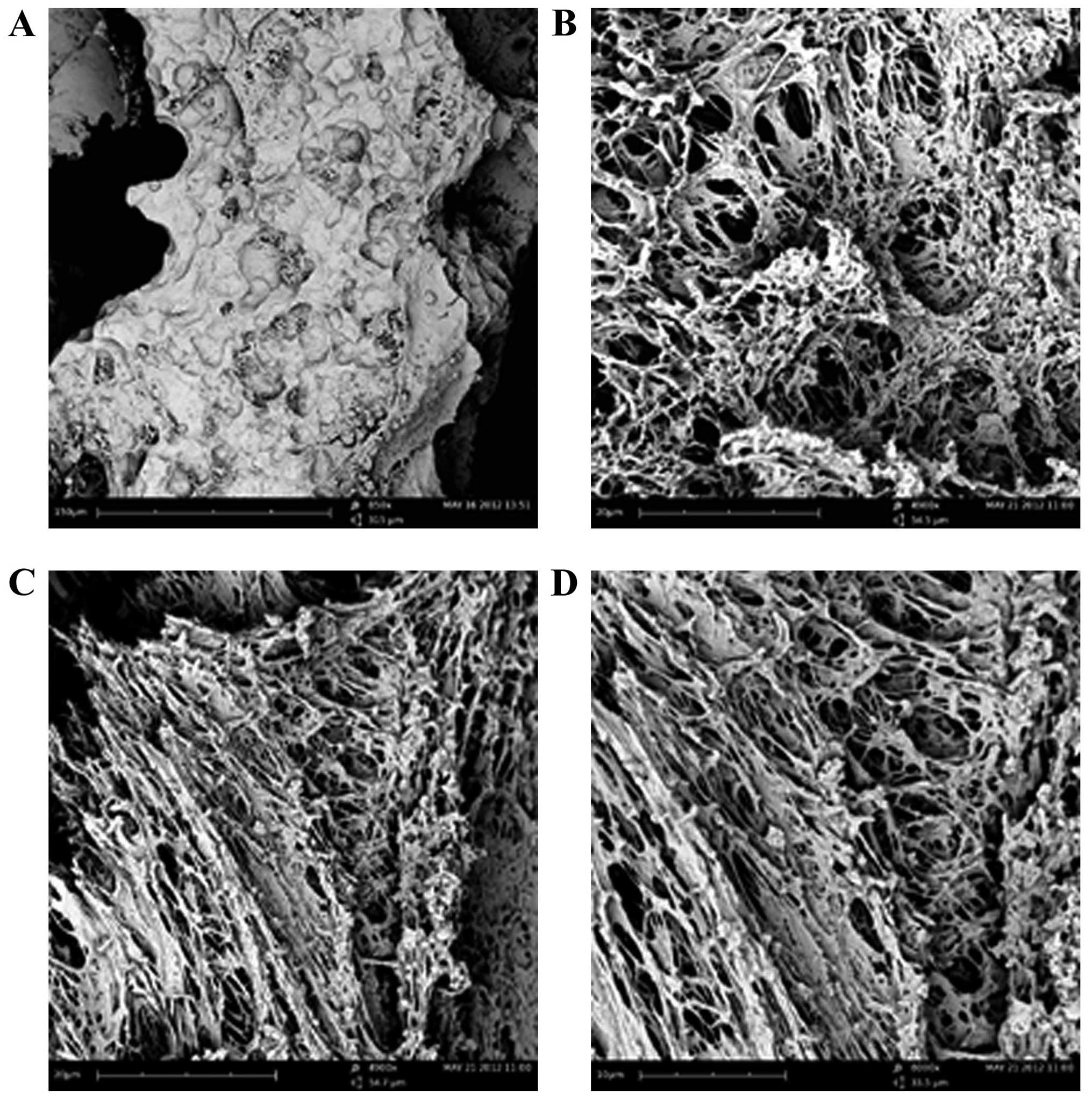
In subjects treated with BPs for 24 months, the
fracture surfaces of biopsy fragments of mandibular bone frequently
show areas with honeycomb morphology represented by half-cells
irregularly spherical or elongated and interrupted by presence of
half-cells of smaller size (Fig.
2A).
Higher magnification allows to distinguish the
fibrillar subunits irregularly arranged or (Fig. 2B) oriented parallel (Fig. 2C), constituting the surface of
half-cells. Further high magnification permits individual fibrillar
subunits to be observed, sized ~0.001 mm (Fig. 2D).
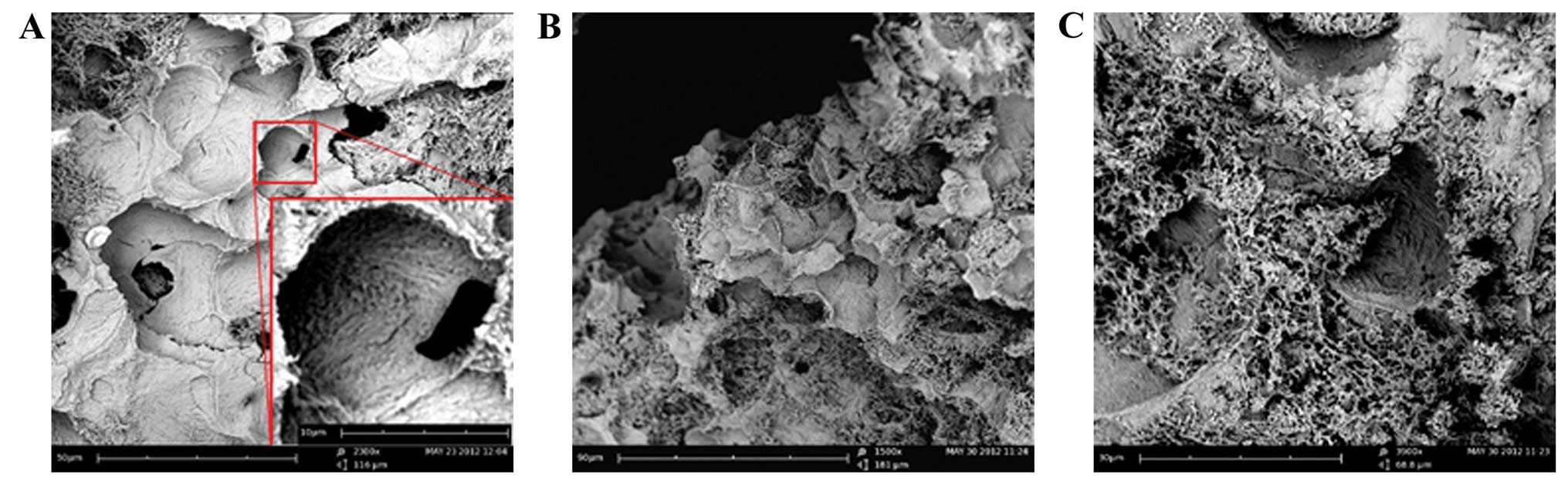
In patients treated with BPs for 36 months visible
extensive and frequent areas consisting of a honeycomb structure,
or areas with half-cells of different sizes and irregular
boundaries, occasionally, partially overlapping each other can be
seen (Fig. 3A). Sometimes, the
bottom of the half-cells appears compact, although it is possible
to recognize the presence of fibrillar bands (insert in Fig. 3A).
In other cases the bottom, as well as the outline,
appear clearly fibrillar (Fig. 3B);
in some areas, it is possible to observe a total derangement of
fibrillar component to the bottom of the half-cells (Fig. 3C).
Immunohistochemistry
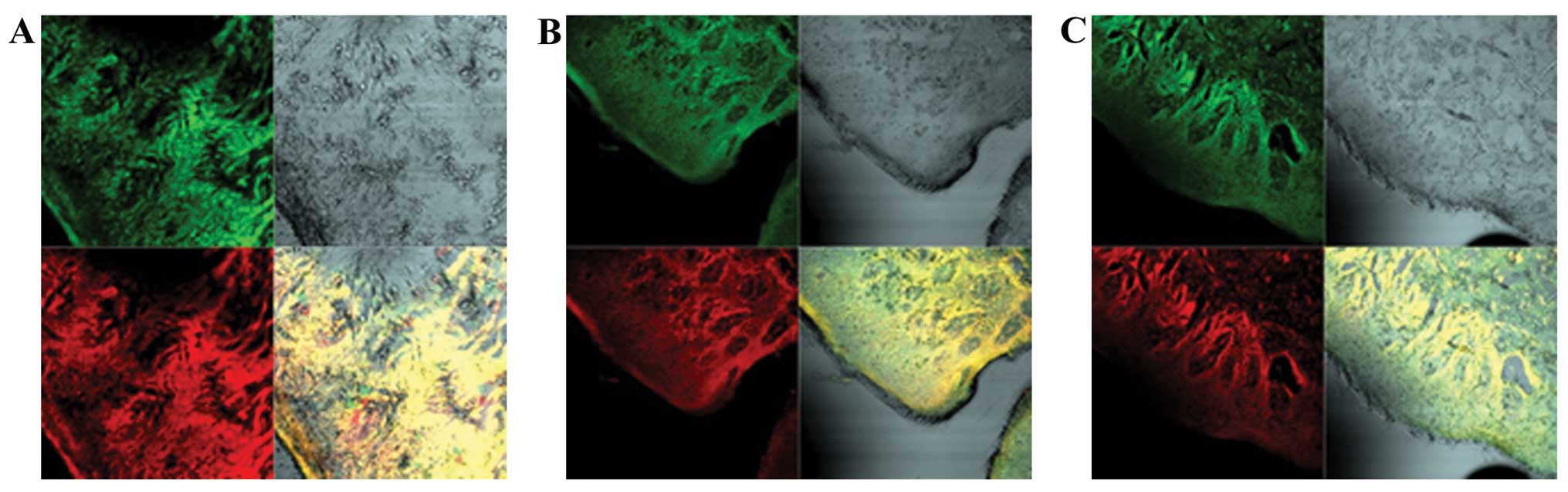
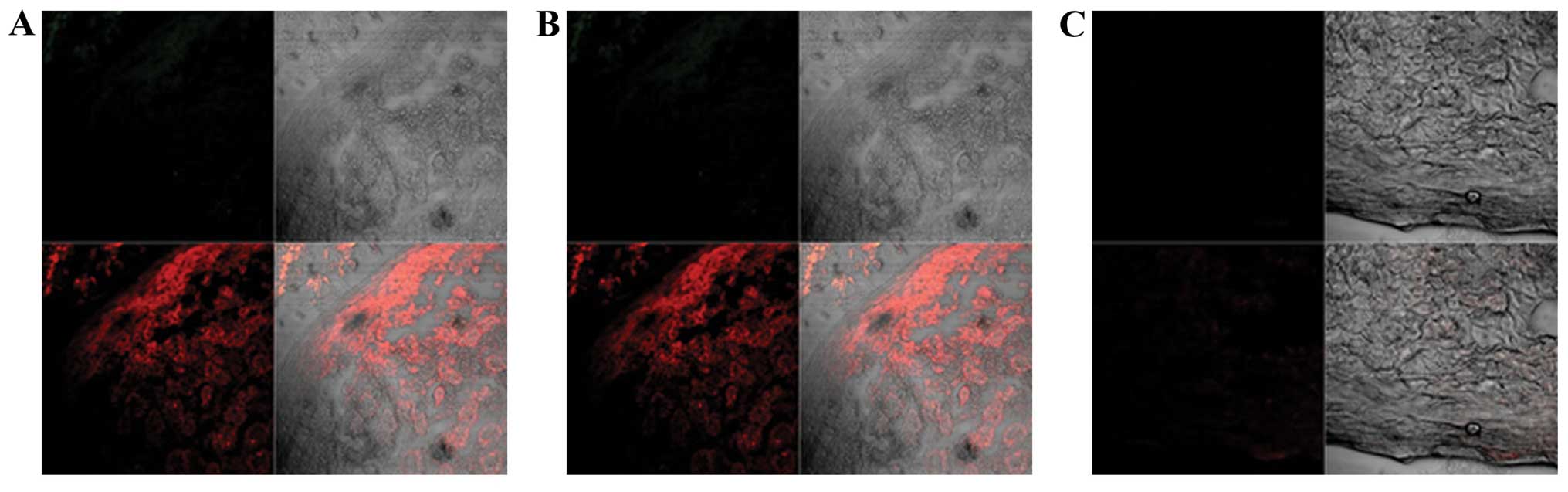
Double localization reactions between sarcoglycans
and integrins, on intraoperative biopsies of oral mucosa of
subjects not treated with BPs demonstrate a normal staining pattern
in all analyzed regions from basal keratinocytes to superficial
layers. By splitting the image it is possible to denote staining
patterns for α-sarcoglycan and β1-integrin (red and green channel
in Fig. 4A, respectively), the
merging of the channels shows a yellow fluorescence demonstrating a
colocalization between two tested proteins. Similar staining
patterns are shown for ɛ-sarcoglycan and α6-integrin (red and green
channel in Fig. 4B, respectively)
and for γ-sarcoglycan and α2-integrin (red and green channel in
Fig. 4C, respectively).
Double localization reaction between sarcoglycans
and integrin in intraoperative biopsies of the oral mucosa in
patients treated with zoledronate for 24 months, compared with
healthy subjects, generally show a decreased staining pattern for
both proteins. In detail, by splitting the image it is possible to
show decreased staining patterns for α-sarcoglycan and β1-integrin
(red and green channel in Fig. 5A,
respectively), while the merge of two channels shows a
colocalization between two tested proteins. Similarly, the staining
patterns for ɛ-sarcoglycan and α6-integrin (red and green channel
in Fig. 5B, respectively) and for
γ-sarcoglycan and α2-integrin (red and green channel in Fig. 5C, respectively), show decreased
fluorescence.
On intraoperative biopsies of the oral mucosa of
patients undergoing BPs therapy for 36 months, double localization
reaction between sarcoglycans and integrins reveals an almost
absent staining pattern for the tested proteins. By splitting of
image it is possible to denote the absence of β1-integrin (Fig. 6A) and a markedly decreased staining
pattern for α-sarcoglycan (red channel in Fig. 6A). Staining patterns for
ɛ-sarcoglycan and α6-integrin (red and green channel in Fig. 6B, respectively) and for
γ-sarcoglycan and α2-integrin (red and green channel in Fig. 6C, respectively), show absence of the
fluorescence.
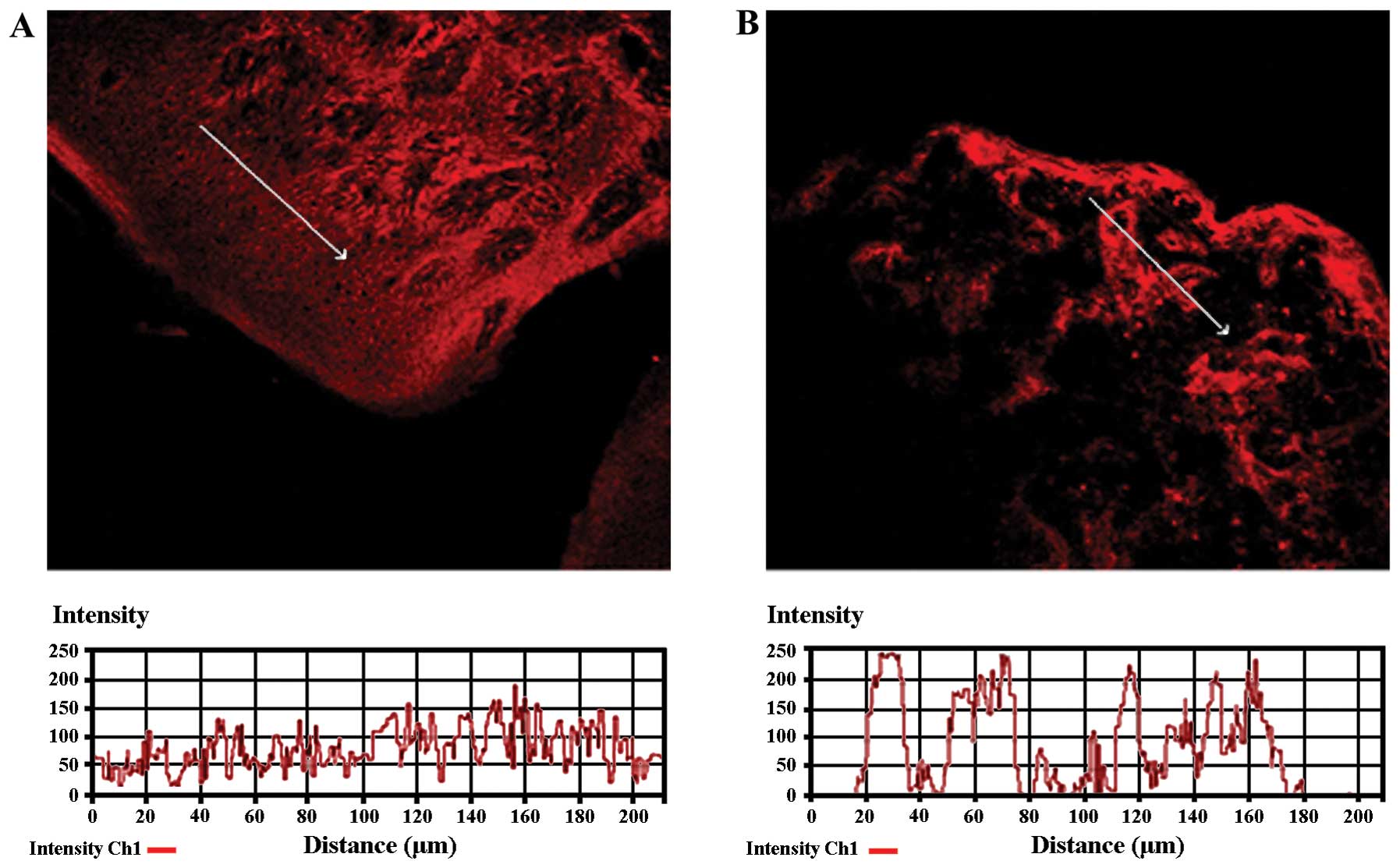
To confirm the protein staining patterns, we used
the ‘display profile’ software function of the laser scanning
microscope for selected samples. This additional analysis, which
reveals the fluorescence intensity profile across an image along a
freely selectable line, converted the immunofluorescence signal
into a graph. The display profile of the control specimens shows
clear and frequent peaks of fluorescence for ɛ-sarcoglycan
(Fig. 7A), while a biopsy of a
patient treated with BPs for 24 months, peaks of fluorescence
appear less frequently, demonstrating a decreased fluorescence
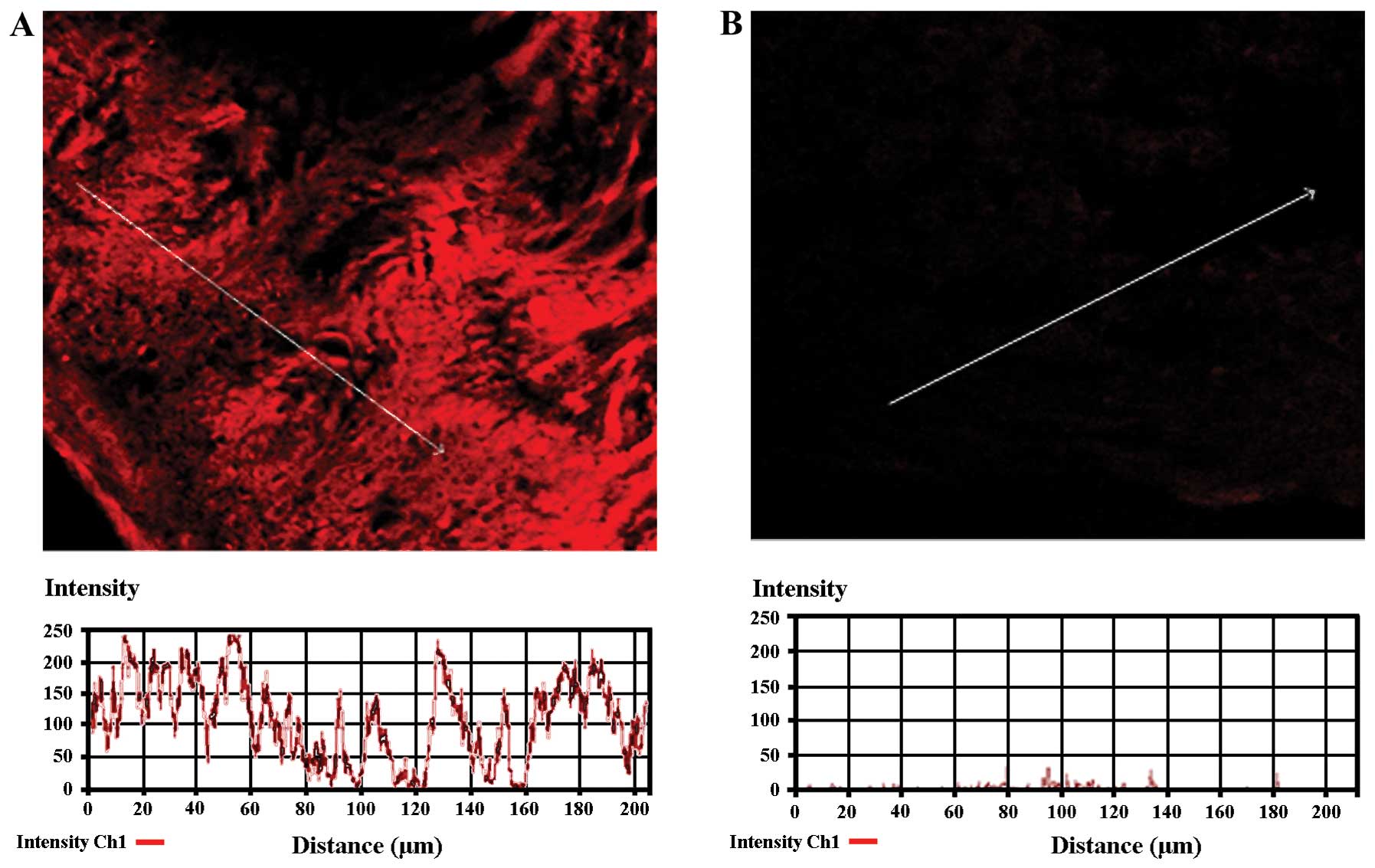
(Fig. 7B). In the same way, the
display profile for α-sarcoglycan, in a control subject, shows
normal and frequent peaks of fluorescence (Fig. 8A), while a biopsy treated with BPs
for 36 months shows an almost total absence of peaks (Fig. 8B).
Discussion
Osteonecrosis of the jaw has been identified as a
serious potential complication during prolonged therapy with BPs
(6,13). Many studies have suggested that
zoledronate and pamidronate may be directly responsible for
bisphosphonates related osteonecrosis of the jaw (14,15);
nevertheless, the exact mechanism of a predilection for the jaw
remains unclear.
Regarding bone healing it was hypothesized that BPs
have an effect on bone blood flow in rats and significantly they
also reduce circulating vascular endothelial growth factor levels;
in other words, the BPs inhibit the angiogenesis process (16,17).
In particular, anti-angiogenic properties have been
reported for nitrogen-containing BPs and decreased levels of
vascular endothelial growth factor have been observed in humans
after administration of zoledronic acid (9,10,18).
This hypothesis has been contrasted in several cases
of ONJ, reporting intact vascular channels, even in areas with
acute inflammatory infiltrates and bacterial over growth; moreover,
no-vital bone fragments without any vascular alteration were also
described (19). Recently, the
increased level of VEGF in patients with ONJ was demonstrated,
using immunohistochemistry methods (11).
An alternative hypothesis is that BPs directly
affect viability of osteocytes decreasing their lifespan and
increasing the rate of necrotic matrix formation.
In contrast, there is no evidence on the in
vivo effects of BPs on osteocytes at high doses, although
pamidronate and alendronate have been show to inhibit osteoblastic
differentiation in vitro and to suppress the activity of
osteoblasts in vivo(20–22).
It is possible that during prolonged therapy the BPs may accumulate
in the bone toxic levels for osteocytes. Particularly, the mandible
and maxillary bone have high rates of bone remodeling and are sites
of high rate BP uptake and accumulation.
It is known that the BPs inhibit the mevalonate
pathway; blocking the enzyme farnesyl-diphosphate synthase they
lead to poor cell function and apoptosis (23,24).
In this case, the osteocytes move down by howship lacunae; the
lacunae appear empty because the osteoclasts cannot produce new
bone material. In our study, at 24 months of treatment with BPs the
perilesional bone demonstrated delineated areas with micro-lacunae;
after 36 months of treatment the micro-lacunae became wide
areas.
Iwata et al(21) have valued connection between organic
matrix necrosis toxicity of BPs towards the osteocytes. Moreover,
it is not clear whether osteocytic death in the canine model occurs
through direct toxic effects of BPs or it occurs through
reduced/suppressed remodeling of regions which normally undergo
cell death. Which of these hypothesis is correct remains an open
question; in either cases, the osteocyte death without replacement
inevitably leads to bone matrix necrosis. Our reports of human
perilesional bone tissue demonstrate wide areas with absence of
matrix and the presence of fibrillar structures exclusively. At 36
months of treatment with BPs we observed many unorganized fibrils
or crushed fibrils. It was proposed that higher BP levels in
alveolar bone would result in high enough BP concentrations to be
directly toxic to oral epithelium, resulting in secondary infection
of the underlying bone (25). Our
findings demonstrate a strong correlation between gingival
epithelium alteration and bone alteration. In agreement, Reid et
al(26) suggested that seminal
event in the development of ONJ was actually bisphosphonate-induced
soft tissue injury. Indeed, it is known that the BPs as pamidronate
and aledronate have cytotoxic effects on human intestinal cells
(27,28). In particular, Twiss et
al(29) demonstrated increased
cell permeability after high doses of pamidronate and aledronate
exposure in vitro.
Landesberg et al(30) evaluated whether oral keratinocytes
undergo apoptosis following exposure to pamidronate by three
different methods. But all assays failed to show any significant
increase in oral keratinocyte apoptosis secondary to BP exposure.
However, it was demonstrated that high concentrations show a
significant decreased cellular adhesion in the keratinocytes. This
decrease in cell-cell adhesion could create cellular necrosis.
In the present study, we have demonstrated that the
subjects treated with BPs, independently by adopted drug, reveal a
gradual decrease or absence of transmembrane proteins of integrin
system and sarcoglycan complex. This decrease is highly correlated
with the treatment duration. It is known that integrins and
sarcoglycans are transmembrane proteins that can have a role in
cell-cell adhesion and in cell-matrix adhesion (32–34).
Therefore, we hypothesize that the BPs have an effect on
development of ONJ in two different ways: a direct one on the bone
and a indirect one from gingival epithelium. In the direct way on
the bone the BPs cause matrix necrosis in maxillar and mandibular
bone that have a high bone remodeling from the constant stress of
masticatory forces; turnover suppression increases the mean tissue
because mandibular bone is remodeled less frequently. In the second
way the BPs have effect on the gingival epithelium and they, at the
same time, cause absence of cell-cell adhesion and cell-matrix
adhesion that lead to cellular apoptosis; this second way
facilitates the transit of normal bacterial flora in underlying
bone of oral region that causes clinical manifestation as
osteomyelitis.
In conclusion, our data show, for the first time, a
strong temporal relationship between damage of gingival mucosa and
perilesional damage. Regardless of drug chosen and of
administration modalities, we demonstrate that both mucosal damage
and bone tissue damage increases together with advance of time of
treatment.
Primarily, we hypothesize that BPs act on jaw bone
through two mechanisms; first, directly on bone tissue, second,
indirect on gingival mucosa acting on gingival epithelial
permeability. Our results need further analyses on experimental
animal models in order to confirm these hypotheses.
References
|
1
|
Merigo E, Manfredi M, Meleti M, et al:
Bone necrosis of the jaws associated with bisphosphonate treatment:
a report of twenty-nine cases. Acta Biomed. 77:109–117.
2006.PubMed/NCBI
|
|
2
|
Gutta R and Louis PJ: Methemoglobinemia:
an unusual cause of intraoperative hypoxya. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 103:197–202. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fleisch H: The use of bisphosphonates in
osteoporosis. Br J Clin Pract. 48:323–326. 1994.PubMed/NCBI
|
|
4
|
Wang CJ, Wang JW, Weng LH, Hsu CC, Huang
CC and Chen HS: The effect of Alendronate on bone mineral density
in the distal part of the femur and the proximal part of the tibia
after total knee arthroplasty. J Bone Joint Surg Am. 85:2121–2126.
2003.PubMed/NCBI
|
|
5
|
Ficarra G, Beninati F, Rubino I, Vannucchi
A, Longo G, Tonelli P and Pini Prato G: Osteonecrosis of the jaws
in periodontal patients with a history of bisphosphonate treatment.
J Clin Periodontol. 32:1123–1128. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Marx RE: Pamidronate (Aredia) and
zoledronate (Zometa) induced avascular necrosis of the jaws: a
growing epidermic. J Oral Maxillofac Surg. 61:1115–1157. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ruggiero SL, Mehrotra B, Rosenberg TJ and
Engroff SL: Osteonecrosis of the jaws associated with the use of
bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg.
62:527–534. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marx RE, Sawatari Y, Fortin M and Broumand
V: Bisphosphonate-induced exposed bone (osteonecrosis/osteoporosis)
of the jaws: risk factors, recognition, prevention, and treatment.
J Oral Maxillofac Surg. 63:1567–1575. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wood J, Bonjean K, Ruetz S, et al: Novel
antiangiogenic effects of the bisphosphonate compound zoledronic
acid. J Pharmacol Exp Ther. 302:1055–1061. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Santini D, Vincenzi B, Dicuonzo G, et al:
Zoledronic acid induces significant and long-lasting modifications
of circulating angiogenic factors in cancer patients. Clin Cancer
Res. 9:2893–2897. 2003.PubMed/NCBI
|
|
11
|
Nastro Siniscalchi E, Cutroneo G,
Catalfamo L, et al: Immunohistochemical evaluation of sarcoglycans
and integrins in gingival epithelium of multiple myeloma patients
with bisphosphonate-induced osteonecrosis of the jaw. Oncol Rep.
24:129–134. 2010.PubMed/NCBI
|
|
12
|
Woo SB, Hellstein JW and Kalmar JR:
Narrative (corrected) review: BPs and osteonecrosis of the jaws.
Ann Intern Med. 144:753–761. 2006.PubMed/NCBI
|
|
13
|
Mehrotra B and Ruggiero S: Bisphosphonate
complications including osteonecrosis of the jaw. Hematology Am Soc
Hematol Educ Program. 515:356–360. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Migliorati CA, Casiglia J, Epsten J,
Jacobsen PL, Siegel MA and Woo SB: Managing the care of patients
with bisphosphonate-associated osteonecrosis: an American Academy
of Oral Medicine position paper. J Am Dent Assoc. 136:1658–1668.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Khosla S, Burr D, Cauley J, et al:
Bisphosphonate-associated osteonecrosis of the jaw: report of a
task force of the American Society for Bone and Mineral Research. J
Bone Miner Res. 22:1479–1489. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cheng A, Mavrokokki A, Carter G, et al:
The dental implications of bisphosphonates and bone disease. Aust
Dent J. 50:S4–S13. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kapitola J and Zák J: Effect of
pamidronate on bone blood flow in oophorectomized rats. Physiol
Res. 47:237–240. 1998.PubMed/NCBI
|
|
18
|
Allegra A, Oteri G, Nastro E, et al:
Patients with bisphosphonate-associated osteonecrosis of the jaw
have reduced circulating endothelial cells. Hematol Oncol.
25:164–169. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hellstein JW and Marek CL: Bisphosphonate
osteochemonecrosis (bis-phossy jaw): is this phossy jaw of the 21st
century? J Oral Maxillofac Surg. 63:682–689. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Idris AI: Role of cannabinoid receptors in
bone disorders: alternatives for treatment. Drug News Perspect.
21:533–540. 2008.PubMed/NCBI
|
|
21
|
Iwata K, Li J, Follet H, Phipps RJ and
Burr DB: Bisphosphonates suppress periosteal osteoblast activity
independently of resorption in rat femur and tibia. Bone.
39:1053–1058. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tobias JH, Chow JW and Chambers TJ:
3-Amino-1-hydroxypropylidine-1-bisphosphonate (AHPrBP) suppresses
not only the induction of new, but also the persistence of existing
bone-forming surfaces in rat cancellous bone. Bone. 14:619–623.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shipman CM, Rogers MJ, Apperley JF,
Russell RG and Croucher PI: Bisphosphonates induce apoptosis in
human myeloma cell lines: a novel anti-tumour activity. Br J
Haematol. 98:665–672. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
van Beek ER, Cohen LH, Leroy IM, Ebetino
FH, Löwik CW and Papapoulos SE: Differentiating the mechanisms of
antiresorptive action of nitrogen containing bisphosphonates. Bone.
33:805–811. 2003.PubMed/NCBI
|
|
25
|
Bauss F and Bergström B: Preclinical and
clinical efficacy of the bisphosphonate ibandronate in cancer
treatment. Curr Clin Pharmacol. 3:1–10. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Reid IR, Bolland MJ and Grey AB: Is
bisphosphonate-associated osteonecrosis of the jaw caused by soft
tissue toxicity? Bone. 41:318–320. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Twiss IM, de Water R, den Hartigh J, et
al: Cytotoxic effects of pamidronate on monolayers of human
intestinal epithelial (Caco-2) cells and its epithelial transport.
J Pharm Sci. 83:699–703. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Suri S, Monkkonen J, Taskinen M, Pesonen
J, Blank MA, Phipps RJ and Rogers MJ: Nitrogen-containing
bisphosphonates induce apoptosis of Caco-2 cells in vitro by
inhibiting the mevalonate pathway: a model of
bisphosphonate-induced gastrointestinal toxicity. Bone. 29:336–343.
2001. View Article : Google Scholar
|
|
29
|
Twiss IM, Pas O, Rampkoopmanscap W, den
Harigh J and Vermeij P: The effects of nitrogen-containing
bisphosphonates on human epithelial (Caco-2) cells, an in vitro
model for intestinal epithelium. J Bone Miner Res. 14:784–791.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Landesberg R, Cozin M, Cremers S, Woo V,
Koustent S and Sinba S: Inhibition of oral mucosal cell wound
healing by bisphosphonates. J Oral Maxillofac Surg. 66:839–847.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Anastasi G, Amato A, Tarone G, et al:
Distribution and localization of vinculin-talin integrin system and
dystrophin-glycoprotein complex in human skeletal muscle:
immunohistochemical study using confocal laser scanning microscopy.
Cells Tissues Organs. 175:151–164. 2003. View Article : Google Scholar
|
|
32
|
Anastasi G, Cutroneo G, Rizzo G, et al:
Sarcoglycan and integrin behavior in normal human skeletal muscle:
a CLSM (confocal laser scanning microscope) study. Eur J Histochem.
48:245–252. 2004.PubMed/NCBI
|
|
33
|
Anastasi G, Cutroneo G, Santoro G, et al:
Integrins, muscle agrin and sarcoglycans during muscular inactivity
conditions: an immunohistochemical study. Eur J Histochem.
50:327–336. 2006.PubMed/NCBI
|
|
34
|
Anastasi G, Cutroneo G, Santoro G, et al:
Costameric proteins in human skeletal muscle during muscular
inactivity. J Anat. 213:284–295. 2008. View Article : Google Scholar : PubMed/NCBI
|