Introduction
The surgical treatment for colorectal cancer has
been established, and the developed operating procedures in primary
tumor resection with lymphadenectomy including laparoscopic
technique have improved and prolonged the survival of colorectal
cancer patients, particularly in stage II and III cases. To date,
staging classification of colorectal cancers is performed by the
UICC/TNM classification system (1)
which is still used as the global gold standard for the decision in
selecting treatment of cancers or predicting parameter for
prognoses. However, we often experience in actual clinical practice
that there are considerable differences in prognoses between
patients who have the same classification particularly in stage III
cancers, even though the advanced adjuvant chemotherapy after
curative resection has been established. The adjuvant chemotherapy
for stage II cases still remains controversial, because its benefit
in survival has not been clearly defined. Therefore, the G-Project
Committee was established by the Japan Society for
Gastroenterological Carcinogenesis at the 2005 annual meeting with
an aim of investigating whether a new TNM-G classification can be
proposed to predict prognosis and recurrence by supplementing the
conventional TNM classification. Gene expression (named as
G-factors) which can transmit the molecular biological
characteristics, would be included as prognostic factors and new
classification of cancers in the TNM classification system. While
evaluating the convenience of implementing the TNM-G classification
system, it was determined that clinical application of RNA and DNA
level analysis of the candidate factors would be challenging. Thus,
analysis of protein expression levels by immunohistological
staining of resected specimens was chosen for nominating the
G-factors because of the relative ease of this method. Here, we
conducted a multicenter collaborative study with cases extracted
from several facilities.
Materials and methods
Patients
In total, 220 cases of colorectal cancer at stage II
(n=77) and stage III (n=143) were registered from four
institutions. Of 220 cases, 109 were confirmed postoperative
recurrence or death within 5 years, and 111 cases were confirmed as
5–10 year recurrence-free survival. The pathological final stages
were managed based on the UICC/TNM classification system (1). The four facilities, Department of
Surgical Oncology, Osaka City University Graduate School of
Medicine (Osaka, Japan); Department of Gastroenterological Surgery,
Kanazawa University (Kanazawa, Japan); Department of Surgery and
Science, Graduate School of Medicine, Kyushu University (Fukuoka,
Japan); Department of Gastroenterological Surgery, Saga University,
Faculty of Medicine (Saga, Japan), were selected to extract
clinical cases, and resected specimens to examine evidence based on
the correlation of staining outcomes and clinicopathologic factors.
This study was conducted after obtaining approval from the
society’s Ethics Committee at the annual meeting in 2007, and then
requesting for approval from the ethics committee of each of the
four facilities supplying resected specimens. Each facility
provided samples according to an implementation planning report.
The study protocol conformed to the ethical guidelines of the
Declaration of Helsinki (1975). Upon gaining approval from the
ethics committees, tissue samples were obtained from each specimen
of the most recent cases from each facility, along with anonymous
background data such as age, gender, occupation, operative
procedure, degree of penetration into the wall (pT), lymph node
metastasis (pN), final stage, ly and v factors, histological type,
presence or absence of adjuvant therapy and regime, recurrence
type, treatment after recurrence, postoperative disease-free
survival (DFS), and postoperative overall survival (OS) period. The
data and clinicopathological background factors were subsequently
analyzed by the Department of Oncology at the Institute of
Geriatrics and Medical Science, Graduate School of Medicine, Osaka
City University.
Selection for factor analysis and case
extraction
As a preliminary step, a literature search of
articles published between 1990 and 2005 was conducted in PubMed
using the key word ‘colorectal cancer’ and ‘independent prognostic
factors’. A total of 396 articles on colorectal cancer, were
extracted and reviewed (Table I).
The reports indicated 30 molecules as prognostic factors in
colorectal cancer. These were classified into 9 groups based on
molecular function: oncogenes, tumor suppressor genes,
microsatellite instability, cell proliferation, growth
factors/cytokines and their receptors, apoptosis signaling
pathways, cell adhesion and invasion, angiogenesis, and others.
Concerning the literature search, highly reported prognostic
factors in colorectal cancers are: p53, 11 papers; microsatellite
instability (MSI), 12; vascular endothelial growth factor (VEGF),
8; vascular density, 5; and CD44, 4. Based on these results, p53
and VEGF are the most common in colorectal cancers and supposed as
candidate molecular factors namely ‘G factors’. Therefore, three
factors, p53, VEGF-A and VEGF-C, were nominated as candidate
factors (2–9) and evaluated in stage II and III
cancers. In addition to the three factors, five molecules,
regenerating islet-derived family, member 4 (Reg IV) (10,11),
olfactomedin 4 (12), Claudin-18
(Invitrogen) (13) and matrix
metalloproteinase-7 (MMP-7) (14),
were added as candidate factors and evaluated.
 | Table IPrognostic factors in colorectal
cancer. |
Table I
Prognostic factors in colorectal
cancer.
| Category | Molecules | No. of papers by
multivariate (M) or univariate (U) analysis |
|---|
| Oncogene | k-ras | |
| c-erbB-2 | |
| Tumor suppressor
gene | P53 | M, 6a; U, 5b |
| DCC | |
| SPN | |
| MSI (MMR gene) | MSI/BAT | M, 4a; U, 8b |
| Cell
proliferation | Polyamine | |
| Growth
factor/cytokine and those receptor | VEGF | M, 2a; U, 6b |
| IL6 | |
| IGF | |
| cMet | |
| EGFR | |
| Apoptosis signal
pathway | TRAIL | |
| Cell invasion and
adhesion | MRP-1 | |
| uPA | |
| Matrilysin | |
| S100A4 | |
| Angiomodulin | |
| CD44 | M, 1a; U, 3b |
| Laminin | |
| β6-integrin | |
| α3-integrin | |
| Angiogenesis | CD105 | |
| Others | Vascular density | M, 3a; U, 2b |
| Galectin | |
| CD95 | |
| Telomerase | |
Methods of immunohistochemical staining
and evaluation
In total, 110 cases of colorectal cancer, in which
postoperative recurrence/death was confirmed within 5 years, and
similarly, 110 cases, in which 5–10 year recurrence-free survival
was confirmed, were used in a case-control study. A total of 220
patients who had undergone a R0 resection of the primary tumor and
were confirmed histologically to have colorectal cancer, were
enrolled in this study. Of the 220 cancers, 60 cases were from
Osaka City University, 40 from Kanazawa University, 40 from Kyushu
University, and 80 were from Saga University. The pathological
final stages were managed based on Japanese Classification of
Colorectal Carcinoma (7th edition) (15) which was revised based on the
UICC/TNM Classification of malignant tumors (1). The above four institutions ultimately
registered 220 cases of colorectal cancer (111 recurrence-free and
109 with recurrence), and these specimens were formalin-fixed and
paraffin-embedded. Immunohistochemical staining was performed at
the Department of Molecular Pathology at Hiroshima University
(Hiroshima, Japan) using seven primary antibodies for p53 (DO-7;
Dako), VEGF-A (Santa Cruz Biotechnologies, Inc.), and VEGF-C
(American Research Products, Inc.), Reg IV; olfactomedin 4;
Claudin-18 (Invitrogen); and MMP-7 (141-7B2; Daiichi Fine
Chemicals, Inc.). Paraffin-embedded specimens were sectioned at 4
μm, hydrophilized, and microwaved for 30 min in pH 6.0 citric acid
buffer or autoclaved in ethylenediaminetetraacetic acid buffer to
activate the antigen. Intrinsic peroxidase was deactivated by
incubation with 3% H2O2 for 10 min, and
blocking was performed using sheep serum and reacting with each
primary antibody for 1 h at room temperature. The samples were
incubated in diaminobenzidine solution for 10 min, and
counterstained with hematoxylin. The stained area was scored by the
percentage of immunopositive cells as an index of the expression of
each molecule. Cases that were not at all stained were scored as 0,
cases with <10% of stained tumor cells were 1+, cases with
10–50% of stained tumor cells were 2+, and cases with >50% of
stained tumor cells were 3+. Evaluation of immunostaining was
conducted independently by two pathologists, and any discrepancies
in assessment were discussed and reassessed by microscopy.
Data analysis and testing for significant
difference
The correlation between a clinicopathological factor
and immunostaining result was analyzed by the Chi-square test or
Fisher’s exact test. The survival duration was calculated using the
Kaplan-Meier method and analyzed by the log-rank test to compare
the cumulative survival durations in the patient groups. In all
tests, a P-value of <0.05 was considered to represent
statistical significance. SPSS statistical software (SPSS Japan
Inc., Tokyo, Japan) was used for all analyses.
Results
Positive staining rate in colorectal
cancer
Cases with >10% of stained tumor cells and
scoring 2 or 3+ were assessed to be positive by two independent
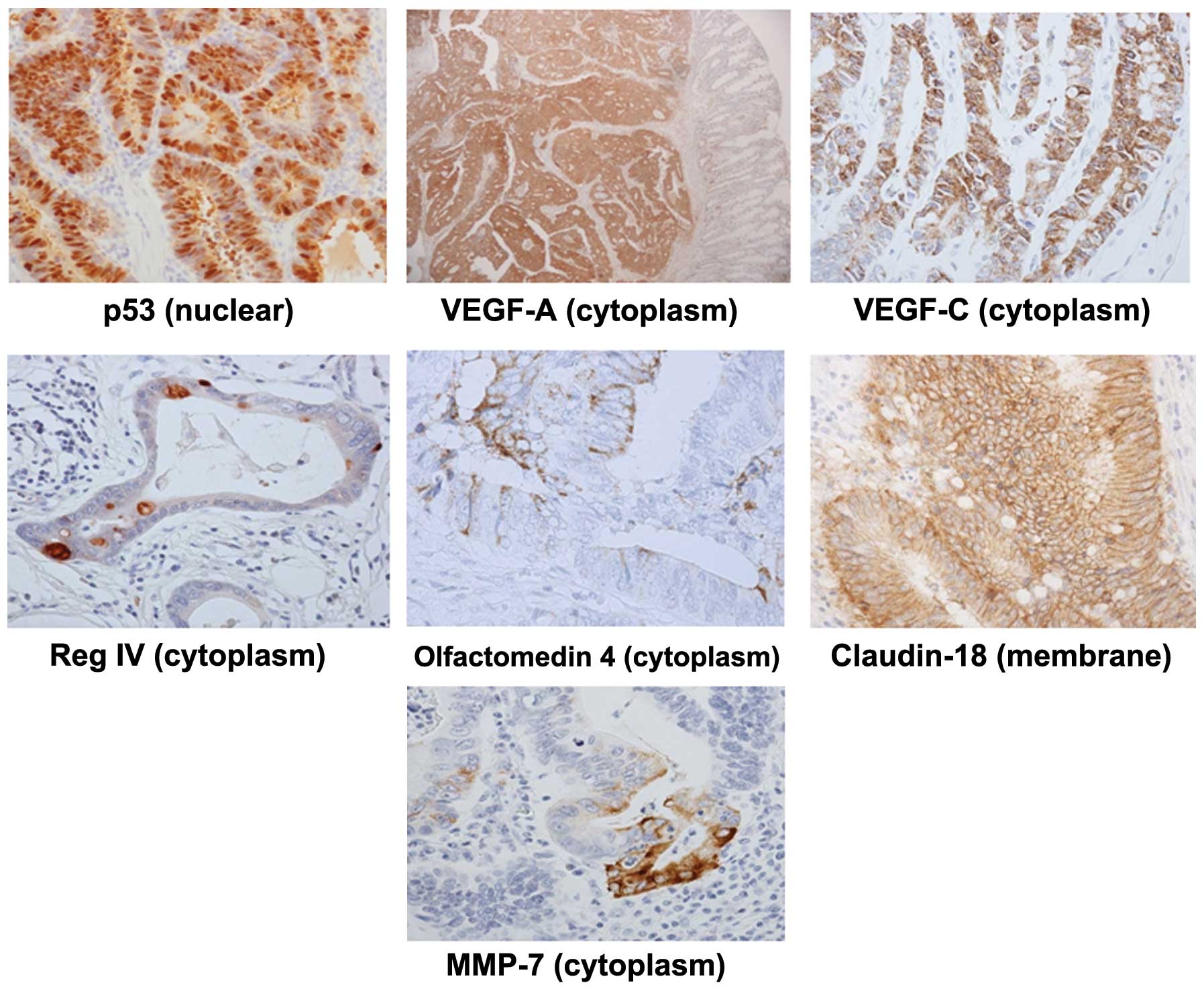
pathologists. Each representative positive expression in
histological image for colorectal cancer is depicted in Fig. 1. Concerning to the positive staining
rate of each factor, 51.8% of p53, 59.1% of VEGF-A, 60.0% of
VEGF-C, 20.9% of Reg IV, 62.3% of olfactomedin 4, 8.2% of
Claudin-18 and 45.5% of MMP-7 were positive in colorectal cancers
(Table II).
 | Table IICorrelation between postoperative
recurrence and clinicopathological features in 220 patients with
colorectal cancer. |
Table II
Correlation between postoperative
recurrence and clinicopathological features in 220 patients with
colorectal cancer.
| Recurrence | |
|---|
|
| |
|---|
| Clinicopathological
factors | Negative n=111
(50%) | Positive n=109
(50%) | P-value |
|---|
| Gender |
| Male | 59 (47) | 66 (53) | 0.268 |
| Female | 52 (55) | 43 (45) | |
| Location |
| Right | 31 (54) | 26 (46) | 0.465 |
| Left | 79 (49) | 83 (51) | |
| pT |
| 1 | 2 (100) | 0 (0) | 0.008 |
| 2 | 5 (50) | 5 (50) | |
| 3 | 96 (53) | 84 (47) | |
| 4 | 8 (29) | 20 (71) | |
| pN |
| Negative | 48 (59) | 33 (41) | 0.046 |
| Positive | 63 (45) | 76 (55) | |
| Stage |
| II | 46 (60) | 31 (40) | 0.043 |
| III | 65 (46) | 78 (54) | |
| Histologic type |
| Diffuse | 11 (38) | 18 (62) | 0.140 |
| Intestinal | 100 (53) | 90 (47) | |
| Lymphatic
invasion |
| Negative | 53 (60) | 35 (40) | 0.041 |
| Positive | 58 (44) | 73 (56) | |
| Venous
invasion |
| Negative | 74 (52) | 68 (48) | 0.509 |
| Positive | 37 (48) | 40 (52) | |
| p53 |
| Negative | 51 (48) | 55 (52) | 0.503 |
| Positive | 60 (53) | 54 (47) | |
| VEGF-A |
| Negative | 46 (51) | 44 (49) | 0.871 |
| Positive | 65 (50) | 65 (50) | |
| VEGF-C |
| Negative | 46 (52) | 42 (48) | 0.660 |
| Positive | 65 (49) | 67 (51) | |
| Reg IV |
| Negative | 91 (52) | 83 (48) | 0.287 |
| Positive | 20 (44) | 26 (56) | |
| Olfactomedin 4 |
| Negative | 43 (52) | 40 (48) | 0.755 |
| Positive | 68 (50) | 69 (50) | |
| Claudin18 |
| Negative | 104 (52) | 98 (48) | 0.306 |
| Positive | 7 (39) | 11 (61) | |
| MMP-7 |
| Negative | 58 (48) | 62 (52) | 0.491 |
| Positive | 53 (53) | 47 (47) | |
Correlation of postoperative recurrence
and clinicopathological factors or the candidate molecular factors
in colorectal cancer
Examination of the 220 colorectal cancer cases
revealed a significant correlation between the postoperative
recurrence and pT stage (P=0.008), pN stage (P=0.046), clinical
stage (P=0.043), and ly factors (P=0.041), whereas no significant
correlation was observed between the presence or absence of
expression of the seven molecular factors and recurrence (Table II). Analysis of each stage revealed
that the postoperative recurrence was significantly higher in Reg
IV positive cases (P=0.042) at stage II in compared to negative
cases, while no significant correlation was observed for any of the
factors in stage III (Table
III).
 | Table IIICorrelation between postoperative
recurrence and candidate G-factors in 220 patients with colorectal
carcinoma at stage II and III. |
Table III
Correlation between postoperative
recurrence and candidate G-factors in 220 patients with colorectal
carcinoma at stage II and III.
| Stage II
(n=77)
Recurrence | Stage III
(n=143)
Recurrence |
|---|
|
|
|
|---|
| Clinicopathological
factors | Negative
n=46 (60%) | Positive
n=31 (40%) | P-value | Negative
n=65 (45%) | Positive
n=78 (55%) | P-value |
|---|
| p53 |
| Negative | 17 (53) | 15 (47) | 0.318 | 34 (46) | 40 (54) | 0.903 |
| Positive | 29 (64) | 16 (36) | | 31 (45) | 38 (55) | |
| VEGF-A |
| Negative | 18 (60) | 12 (40) | 0.970 | 28 (47) | 32 (53) | 0.805 |
| Positive | 28 (60) | 19 (40) | | 37 (45) | 46 (55) | |
| VEGF-C |
| Negative | 21 (62) | 13 (38) | 0.747 | 25 (46) | 29 (54) | 0.875 |
| Positive | 25 (58) | 18 (42) | | 40 (45) | 49 (55) | |
| Reg IV |
| Negative | 40 (66) | 21 (34) | 0.042 | 51 (45) | 62 (55) | 0.881 |
| Positive | 6 (38) | 10 (62) | | 14 (47) | 16 (53) | |
| Olfactomedin 4 |
| Negative | 19 (68) | 9 (32) | 0.272 | 24 (44) | 31 (56) | 0.730 |
| Positive | 27 (55) | 22 (45) | | 41 (47) | 47 (53) | |
| Claudin-18 |
| Negative | 43 (61) | 28 (39) | 0.612 | 61 (47) | 70 (53) | 0.378 |
| Positive | 3 (50) | 3 (50) | | 4 (33) | 8 (67) | |
| MMP-7 |
| Negative | 23 (55) | 19 (45) | 0.329 | 35 (45) | 43 (55) | 0.878 |
| Positive | 23 (66) | 12 (34) | | 30 (46) | 35 (54) | |
Prognostic analysis of OS and DFS in
expression of the candidate molecular factors of colorectal
cancer
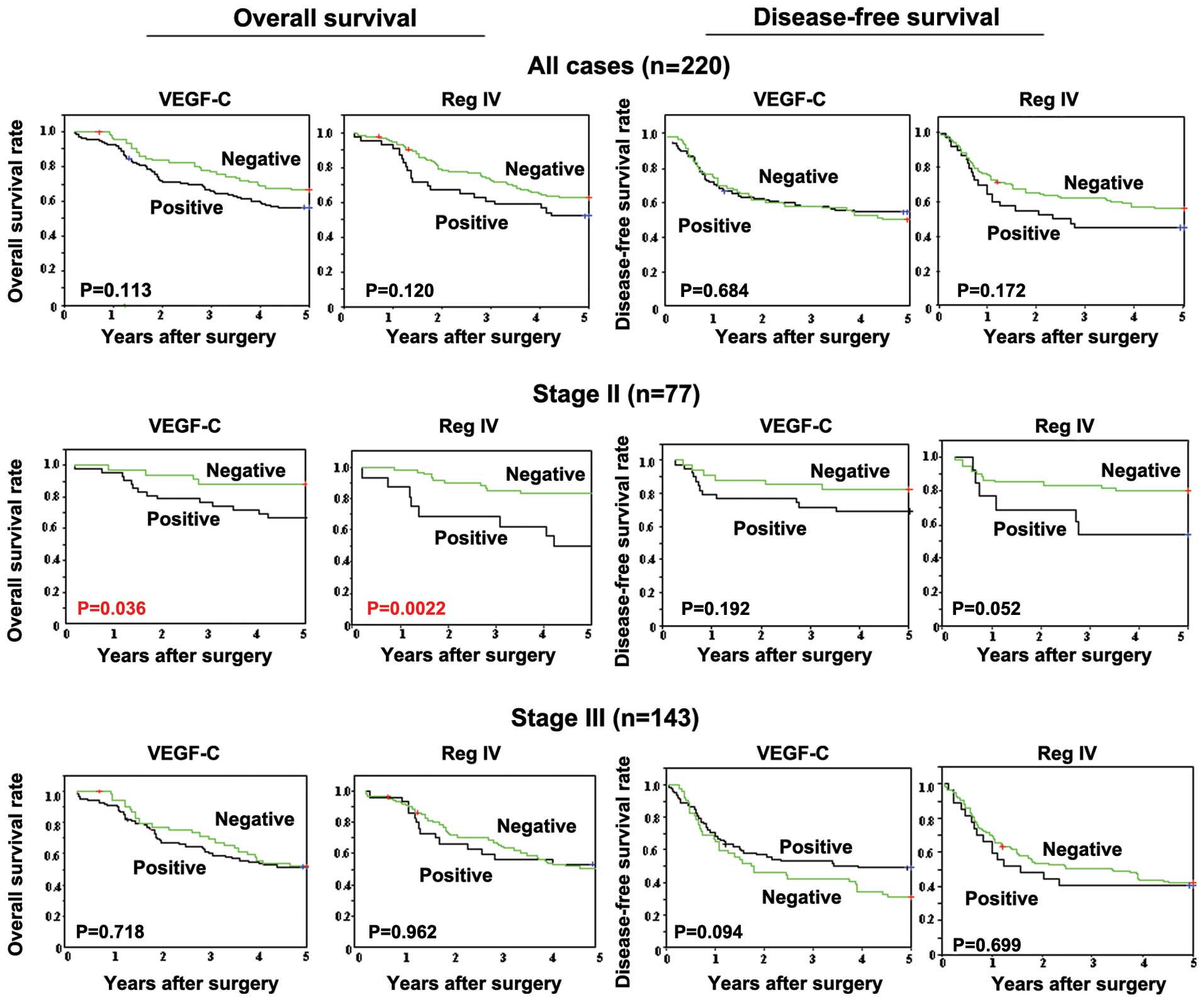
In OS of stage II and III, colorectal cancer cases
positive for VEGF-C and Reg IV tended to have poorer OS in
comparison with the negative cases, although this was not
significant. The prognosis of OS was significantly poorer (P=0.036)
in stage II cases positive for VEGF-C expression in comparison with
VEGF-C negative cases, moreover positive cases for Reg IV in stage
II demonstrated significant poorer prognosis (P=0.0022) compared to
negative cases. Reg IV positive cases at stage II and VEGF-C
positive cases at stage III tended to have poorer DFS (P=0.052 and
0.094, respectively) (Fig. 2). In
contrast, no significant difference was observed in OS between
positive and negative cases for any of the 7 factors at stage III.
Also, no significant difference of DFS was found between positive
and negative groups in stage II cases.
Feasibility of the candidate molecular
factors
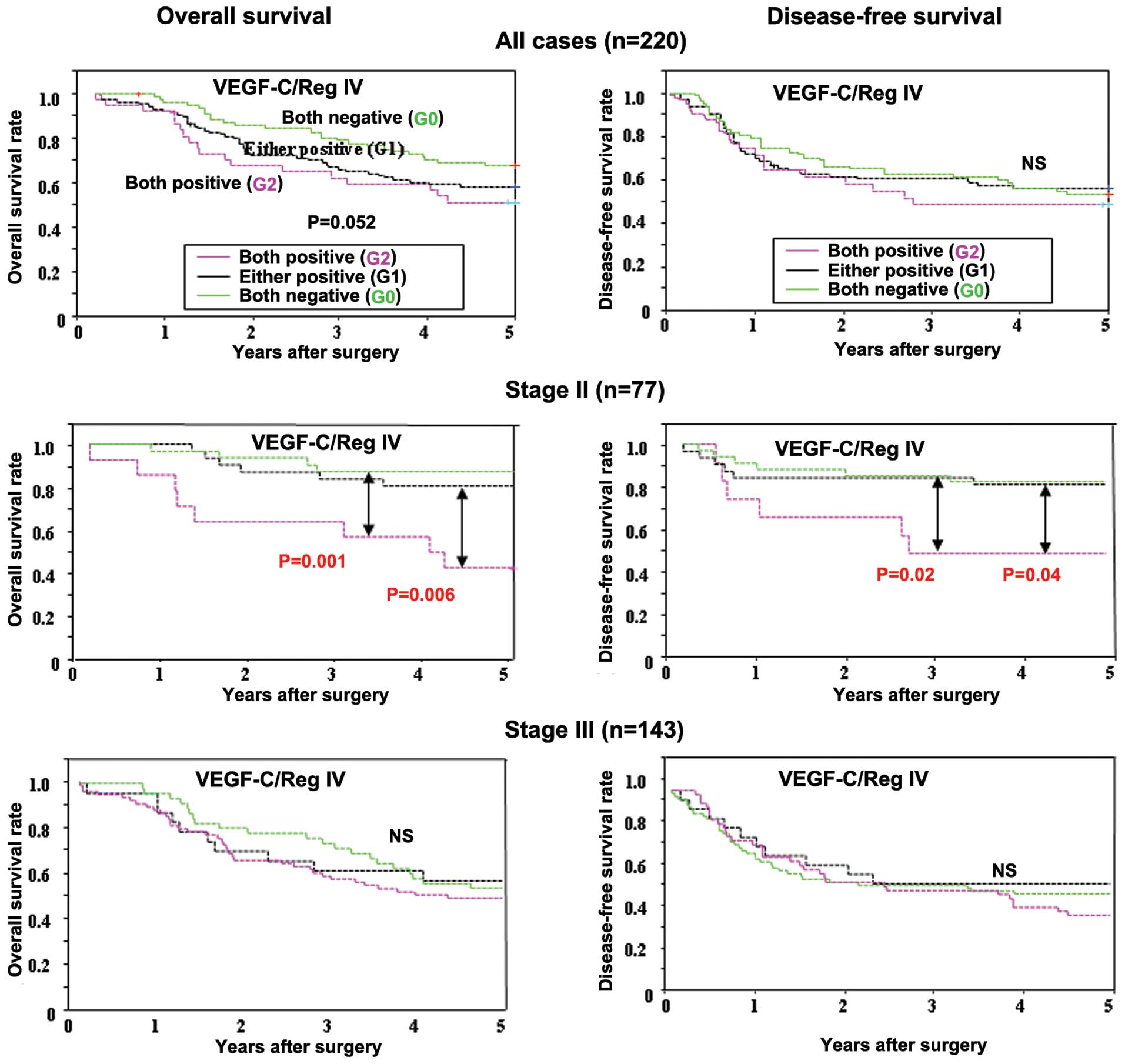
According to the above results, we selected VEGF-C
and Reg IV as nominating factors in colorectal cancer. We then
analyzed the relationship between the combination of VEGF-C and Reg
IV expression and prognosis. Then, colorectal cancer patients were
divided into three groups based on the VEGF-C and Reg IV
expression; G0 group (both negative group, n=69), G1 group (either
positive group, n=104), G2 group (both positive group, n=37).
Fig. 3 shows the relationship
between the combination of VEGF-C and Reg IV expression and
prognosis. In stage II cases, OS of G2 cases were significantly
poorer in comparison with that of G0 cases (P=0.001) and G1 cases
(P=0.006), and DFS was also poorer than that of G0 cases (P=0.02)
and G1 cases (P=0.04). In contrast, no significant difference of OS
or DFS was observed among G0, G1 and G2 groups in all of cases or
in stage III cases (Fig. 3).
Table IV shows the relationship
between the combination of VEGF-C and Reg IV expression and the
postoperative recurrence. In all 220 colorectal cancer cases, the
recurrence rate was slightly higher (59%) in G2 cases compared to
48% in G0 cases while no significant difference was observed
(P=0.413). In stage II cases, the recurrence rate of G2 cases (64%)
was high in comparison with that of G1 cases and G0 cases (32 and
37%, respectively), while the difference was not significant
(P=0.117).
 | Table IVRelationship between reccurrence and
two molecular factors. |
Table IV
Relationship between reccurrence and
two molecular factors.
| Recurrence, n
(%) | |
|---|
|
| |
|---|
| VEGF-C and Reg
IV | Negative | Positive | P-value |
|---|
| Total (n=220) | 111 (51) | 109 (49) | |
| Both negative G0
(n=79) | 41 (52) | 38 (48) | |
| Either positive G1
(n=104) | 55 (53) | 49 (47) | |
| Both positive G2
(n=37) | 15 (41) | 22 (59) | 0.413 |
| Stage II
(n=77) | 46 (60) | 31 (40) | |
| Both negative G0
(n=32) | 20 (63) | 12 (37) | |
| Either positive G1
(n=31) | 21 (68) | 10 (32) | |
| Both positive G2
(n=14) | 5 (36) | 9 (64) | 0.117 |
| Stage III
(n=143) | 65 (45) | 78 (55) | |
| Both negative G0
(n=47) | 21 (45) | 26 (55) | |
| Either positive G1
(n=73) | 34 (47) | 39 (53) | |
| Both positive G2
(n=23) | 10 (43) | 13 (57) | 0.959 |
Discussion
This study was a multicenter collaborative study
with cases extracted from four universities. The four institutions
ultimately registered 220 cases of colorectal cancer. The analysis
of protein expression levels by immunohistological staining was
selected for nominating the G-factors. The immunohistological
staining was performed in each Department of Pathology by keeping
patient infomation and clinicopathologic factors anonymous. The
relationship between protein expression levels and
clinicopathological background factors was independently analyzed
at each facility. Therefore, the objectivity of these results can
be considered to have high reliability and authenticity.
Precise clinical classification of prognosis might
be useful to select a strategy for rigorous adjuvant chemotherapy
and careful follow-up (16,17). The present study was conducted to
establish a new classification system based on the biochemical
characteristics of cancer, which would supplement the conventional
TNM staging system. As shown in Fig.
2, VEGF-C and Reg IV expression was associated with a
significantly poorer prognosis for OS of stage II colorectal
cancer. However, these factors alone could not be found in the
progressing stage to advance. Concerning these results, single use
of G-factors by supplementing TNM staging may be difficult and
limited. Because TNM staging is classified into T1-4, N0-3, and
M0-1, consequently, in regard to the feasibility of TNM-G staging,
combination of VEGF-C and Reg IV in 7 factors were selected and
analyzed for usefulness. High frequent recurrences in stage II
cases were observed in both positive cases (G2), but no
relationship of recurrence was found among the 3 groups, G0-2. In
contrast, a significant difference in OS was observed between G0/1
and G2 in stage II cases. Furthermore, the prognosis of OS and DFS
of stage II G2 cases showed a survival curve apparently similar to
that of stage III cases. This result indicated that prognosis of
VEGF-C and Reg IV both positive G2 in stage II colorectal cancer
was the same as that of stage III cases, and the advancement of one
stage up based on G-factors may be highly feasible for clinical
application. These findings suggested that TNM-G staging may have a
possibility for use as a reasonable supplement to the TNM
classification system.
Through the collaboration of many facilities and the
Japan Society for Gastroenterological Carcinogenesis, the present
study was schemed to investigate the feasibility of new molecular
staging as a G-factor to further supplement the TNM classification
system, which is the standard staging system used for colorectal
cancers. With the advancement of molecular-targeting drugs, we
investigated the possible application of G-factors, which are
derived from molecular biological characteristics of cancer, in
staging along with clinicopathological factors. However, in
accordance with previous reports from single institutions, no
correlation between recurrence/prognosis and up-staging migration
was found. Thus, the proposal of an individual single G-factor was
supposed to be challenging. However, when colorectal cancer was
limited to stage II, the present results indicated that G2 cases
both positive for VEGF-C/Reg IV were likely to advance up to stage
III, suggesting that G-factors can be used to supplement initial
staging by TNM classification. Application and effect of adjuvant
chemotherapy for stage II colorectal cancers still remains
controversial. The present results may suggest a good indication of
adjuvant chemotherapy for G2 cases in stage II. In future studies,
the highly relevant factors may be identified by the involvement of
the degree of molecular biological malignancy to establish TNM-G
staging, and application of these factors by supplementing TNM
classification may contribute to more accurate prediction of
prognosis.
In conclusion, the members of the Japan Society for
Gastroenterological Carcinogenesis, investigated the feasibility of
a new molecular factor(s) to further supplement the TNM
classification system, and found that the combination of VEGF-C and
Reg IV might be a promising factor for clinical staging to
supplement the classical TNM classification system, and it may
suggest a good indication of adjuvant chemotherapy for G2 cases in
stage II colorectal cancers.
Acknowledgements
We thank Emeritus Professor Eiichi Tahara (Hiroshima
Cancer Seminar Foundation, Hiroshima, Japan) and Emeritus Professor
Michio Kaminishi (Showa General Hospital, Tokyo, Japan) for helpful
advice. This study is partially funded by the Japan Society for
Gastroenterological Carcinogenesis.
References
|
1
|
Sobin LH: TNM, sixth edition: new
developments in general concepts and rules. Semin Surg Oncol.
21:19–22. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tanigawa N, Amaya H, Matsumura M and
Shimomatsuya T: Correlation between expression of vascular
endothelial growth factor and tumor vascularity, and patient
outcome in human gastric carcinoma. J Clin Oncol. 15:826–832.
1997.
|
|
3
|
Maeda K, Kang SM, Onoda N, et al:
Expression of p53 and vascular endothelial growth factor associated
with tumor angiogenesis and prognosis in gastric cancer. Oncology.
55:594–599. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Maehara Y, Tomoda M, Hasuda S, et al:
Prognostic value of p53 protein expression for patients with
gastric cancer - a multivariate analysis. Br J Cancer.
79:1255–1261. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kakeji Y, Koga T, Sumiyoshi Y, et al:
Clinical significance of vascular endothelial growth factor
expression in gastric cancer. J Exp Clin Cancer Res. 21:125–129.
2002.PubMed/NCBI
|
|
6
|
Fondevila C, Metges JP, Fuster J, et al:
p53 and VEGF expression are independent predictors of tumour
recurrence and survival following curative resection of gastric
cancer. Br J Cancer. 90:206–215. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Resnick MB, Routhier J, Konkin T, Sabo E
and Pricolo VE: Epidermal growth factor receptor, c-MET,
beta-catenin, and p53 expression as prognostic indicators in stage
II colon cancer: a tissue microarray study. Clin Cancer Res.
10:3069–3075. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
White JD, Hewett PW, Kosuge D, et al:
Vascular endothelial growth factor-D expression is an independent
prognostic marker for survival in colorectal carcinoma. Cancer Res.
62:1669–1675. 2002.PubMed/NCBI
|
|
9
|
Des Guetz G, Uzzan B, Nicolas P, et al:
Microvessel density and VEGF expression are prognostic factors in
colorectal cancer. Meta-analysis of the literature. Br J Cancer.
94:1823–1832. 2006.PubMed/NCBI
|
|
10
|
Oue N, Kuniyasu H, Noguchi T, et al: Serum
concentration of Reg IV in patients with colorectal cancer:
overexpression and high serum levels of Reg IV are associated with
liver metastasis. Oncology. 72:371–380. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oue N, Mitani Y, Aung PP, et al:
Expression and localization of Reg IV in human neoplastic and
non-neoplastic tissues: Reg IV expression is associated with
intestinal and neuroendocrine differentiation in gastric
adenocarcinoma. J Pathol. 207:185–198. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Oue N, Sentani K, Noguchi T, et al: Serum
olfactomedin 4 (GW112, hGC-1) in combination with Reg IV is a
highly sensitive biomarker for gastric cancer patients. Int J
Cancer. 125:2383–2392. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sanada Y, Oue N, Mitani Y, Yoshida K,
Nakayama H and Yasui W: Down-regulation of the claudin-18 gene,
identified through serial analysis of gene expression data
analysis, in gastric cancer with an intestinal phenotype. J Pathol.
208:633–642. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ajisaka H, Yonemura Y and Miwa K:
Correlation of lymph node metastases and expression of matrix
metalloproteinase-7 in patients with gastric cancer.
Hepatogastroenterology. 51:900–905. 2004.PubMed/NCBI
|
|
15
|
Japanese Society for Cancer of the Colon
and Rectum. Japanese Classification of Colorectal Carcinoma. 7th
edition. Kanehara; Tokyo: 2009
|
|
16
|
Mejia A, Schulz S, Hyslop T, Weinberg DS
and Waldman SA: Molecular staging individualizing cancer
management. J Surg Oncol. 105:468–474. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Eschrich S, Yang I, Bloom G, et al:
Molecular staging for survival prediction of colorectal cancer
patients. J Clin Oncol. 23:3526–3535. 2005. View Article : Google Scholar : PubMed/NCBI
|