Introduction
Lung cancer is the leading cause of cancer-related
mortality in the world. It is classified into two groups: non-small
cell lung cancer (NSCLC) and small cell lung cancer (1). Chemotherapy has been the mainstay of
treatment for advanced NSCLC. Of the various types of chemotherapy
regimens available, platinum-based derivatives have been shown to
improve overall survival (2).
Cisplatin was the first platinum agent to be used in the clinic in
the early 1970s and proved very effective in the treatment of
several types of cancer (3–5). It is classed as an alkylating agent,
DNA binds to it by nucleophilic substitution, and it is one of the
substances which can cause crosslinking (6). Cisplatin can react with DNA in several
ways, the most common is the reaction with guanine leading to the
formation of intrastrand crosslinks (65% of DNA modifications). It
has been shown that platinum-DNA adducts correlate with the disease
response. Thus, the capacity to repair DNA damage caused by
platinum derivatives may reflect cellular sensitivity to this agent
(7,8).
There have been many studies on patients under
treatment for cancer; the majority of investigations examine
peripheral blood lymphocytes (PBLs) for increased levels of DNA
damage, although other cells (for example, buccal cells) can also
serve as surrogates. Collection of PBLs is usually less invasive
than that of target tissue, and they are the surrogate cells of
choice in studies where target tissue is not readily attainable
(9,10). With specific regard to cancer, this
approach has been used experimentally to measure the levels of
basal DNA damage in PBLs of cancer patients, as well as to assess
the susceptibility of cells to the DNA-damaging effects of
radiotherapy or chemotherapy (9).
DNA repair is growing in popularity as a biomarker in human
biomonitoring. It seems that more useful information has come from
phenotypic assays for repair-enzyme activity than from measuring
expression of repair genes. Results thus so far tend to be
inconsistent. Studies on the effect of occupational or
environmental exposure to genotoxins have shown the full range of
positive, negative and null effects on repair and the same is true
of nutritional studies. Even the generally assumed decline in
repair capacity with age has not been confirmed in population
surveys with biomarker assays for DNA repair (11).
We performed our measurements (DNA damage and
repair) using the comet assay test. The comet assay or single-cell
gel electrophoresis (SCGE) assay is a rapid, sensitive and
relatively simple method for detecting DNA damage at the level of
individual cells (12). This assay
is now widely accepted as a standard method for assessing DNA
damage in individual cells, and is used in a broad variety of
applications including human biomonitoring, genotoxicology,
ecological monitoring and as a tool to investigate DNA damage and
repair in different cell types in response to a range of
DNA-damaging agents (13). The
comet assay would be eminently suitable for use in clinical
practice, since it is a relatively simple and inexpensive technique
which requires only a small quantity of cells, and results can be
obtained within a matter of hours. Comet assay is a method specific
for investigation of DNA damage, and is recommended for studies on
reagents that cause DNA damage. Studies have shown that results
generated by the comet assay provide important information about
the nature of a particular cancer, and could be used by oncologists
in their determination of the best possible course of intervention
(9).
Materials and methods
Chemicals and reagents
All chemicals were purchased from Sigma Aldrich.
Cell culture
HeLa cells were obtained from Professor Andrew
Collins (University of Oslo, Norway). Cells were cultivated in DMEM
supplemented with 10% fetal bovine serum, antibiotics and an
antimycotic mixture (all ingredients from PAA Laboratories,
Pasching, Austria). Cells were passaged twice a week by
trypsinization in the ratio 1:10.
Patients
Blood samples were obtained from 20 patients with
NSCLC stage 4. Patient age was between 47 and 74 years. Patients
were programmed for chemotherapy according to the following
protocol: blood samples were collected from each patient during the
1st and 3rd cycles of chemotherapy; 1 day before starting the
cycle, immediately after administration of the chemotherapy, and 1
and 7 days after completion of the chemotherapy cycle. The last
control measurement was performed 3 weeks after the final (4th
cycle) completed course of chemotherapy. All patients received
chemotherapy for the first time. They received platinum-based
derivatives (cisplatin or carboplatin) in a combination therapy.
Blood samples were also obtained from an age-corresponding control
group (10 subjects). The study was conducted according to the
guidelines of the Declaration of Helsinki and all procedures
involving human subjects were approved by the Ethics Committee of
the Charles University Medical Faculty in Hradec Kralove. Written
informed consent was obtained from all subjects.
Comet assay
Lymphocyte preparation. Peripheral blood lymphocytes
were obtained from heparinized blood and separated using LSM (PAA
Laboratories) according to the method of Boyum in 1964 (14). Peripheral blood lymphocytes were
washed and re-suspended with PBS buffer and adjusted to 1 million
cells/ml.
The comet assay modification was used as previously
described (15). Briefly, 35 μl of
cell suspension (»35,000 cells) was mixed with 85 μl low melting
point agarose, spread onto an 85 μl high melting point on normal
agarose pre-coated microscope slide and left at 4ºC to allow for
solidification. Cells were lysed for 1 h in high salt and detergent
solution. They were then exposed for 40 min to alkali to allow for
DNA unwinding and cleavage of alkali-labile sites. Electrophoresis
was applied for 30 min at 4ºC, after which the slides were
neutralized, stained with ethidium bromide and analyzed by
fluorescence microscopy. Fifty cells per slide were scored
according to % tail DNA by the Lucia G analyzing software
(Laboratory Imaging, Prague, Czech Republic).
DNA crosslinks were measured using the modified
comet assay, using styrene oxide. Briefly, cells were incubated
with styrene oxide to induce DNA breaks prior to comet assay.
Incubation of cells with styrene oxide leads to the formation of
comets containing ~80–90% of DNA in the tail. When crosslinks are
present in the DNA the alkaline unwinding is blocked and the % of
DNA in the tail is reduced accordingly (16).
DNA repair, base excision repair (BER) and
nucleotide excision repair (NER), were measured using the modified
comet assay in an extract of lymphocytes. Nucleoids of HeLa cells
containing specific lesions (8-oxoguanine or cyclobutane pyrimidine
dimers) in their DNA embedded in agarose were incubated along with
the extracts prepared from lymphocytes of the study subjects whose
excision repair activity was to be measured. The nature of the DNA
lesion in the substrate defines the repair pathway that is
measured. Substrate containing 8-oxoguanine is used to measure BER
activity, and if the substrate contains bulky adducts or
cyclobutane pyrimidine dimers NER is measured (17–20).
Statistical analysis
Statistical significance of the differences between
groups was assessed by using GraphPad Prism 5.03 software (GraphPad
Software, Inc., San Diego, CA, USA).
Results
In the present study, we investigated DNA damage and
repair in 20 NSCLC patients and in 10 subjects from the control
group as well. Patients were in the last stage of cancer and
chemotherapy was indicated as a palliative. Thirteen patients
completed the entire course of chemotherapy and seven patients died
during the chemotherapy.
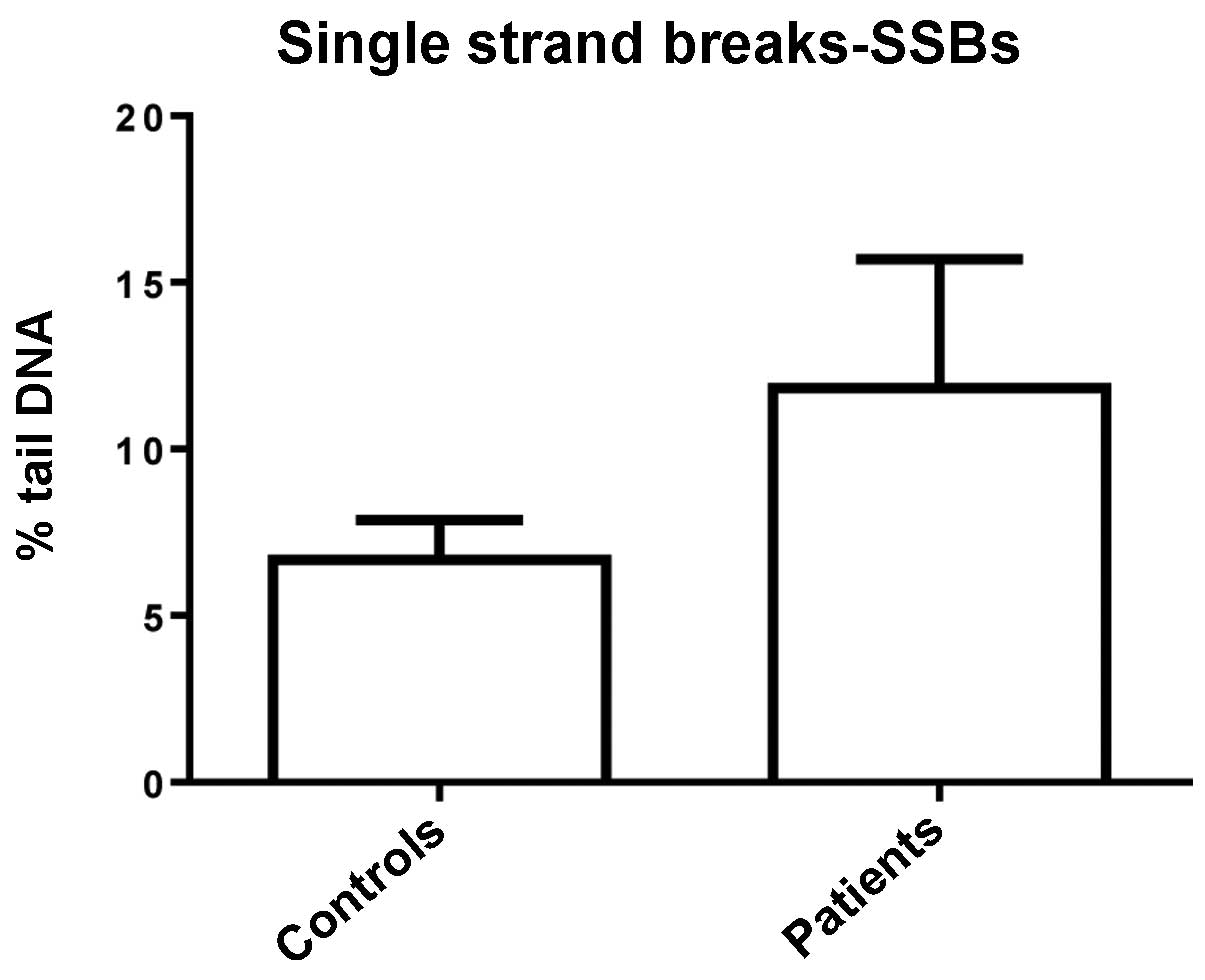
The degree of DNA damage was estimated by the comet
assay and was expressed as the percentage Tail DNA. In the healthy
controls, the percentage Tail DNA in single strand breaks (SSBs)
was 6.679±1.193. In cancer patients, percentage Tail DNA in SSBs
was 11.830±3.865. In the cancer patient group, we found high
inter-individual variability, with coefficient of variation
142.46%. Results were not statistically significantly different:
P=0.3674 in the Mann-Whitney test (Fig.
1).
We compared values of BER and NER activity in
healthy controls and in cancer patients. BER of healthy controls
was higher (P=0.0320 in the T-test) than BER of cancer patients.
NER was almost at the same level in both healthy controls and
cancer patients (P=0.9670 in the T-test). Data are shown in
Table I.
 | Table IComparison of values of BER and NER of
healthy controls and cancer patients. |
Table I
Comparison of values of BER and NER of
healthy controls and cancer patients.
| % Tail DNA ± SE | Controls | Patients | P-value |
|---|
| BER | 17.10±1.170 | 10.57±2.569 |
0.0320a |
| NER | 12.88±1.131 | 12.75±3.074 | 0.9670 |
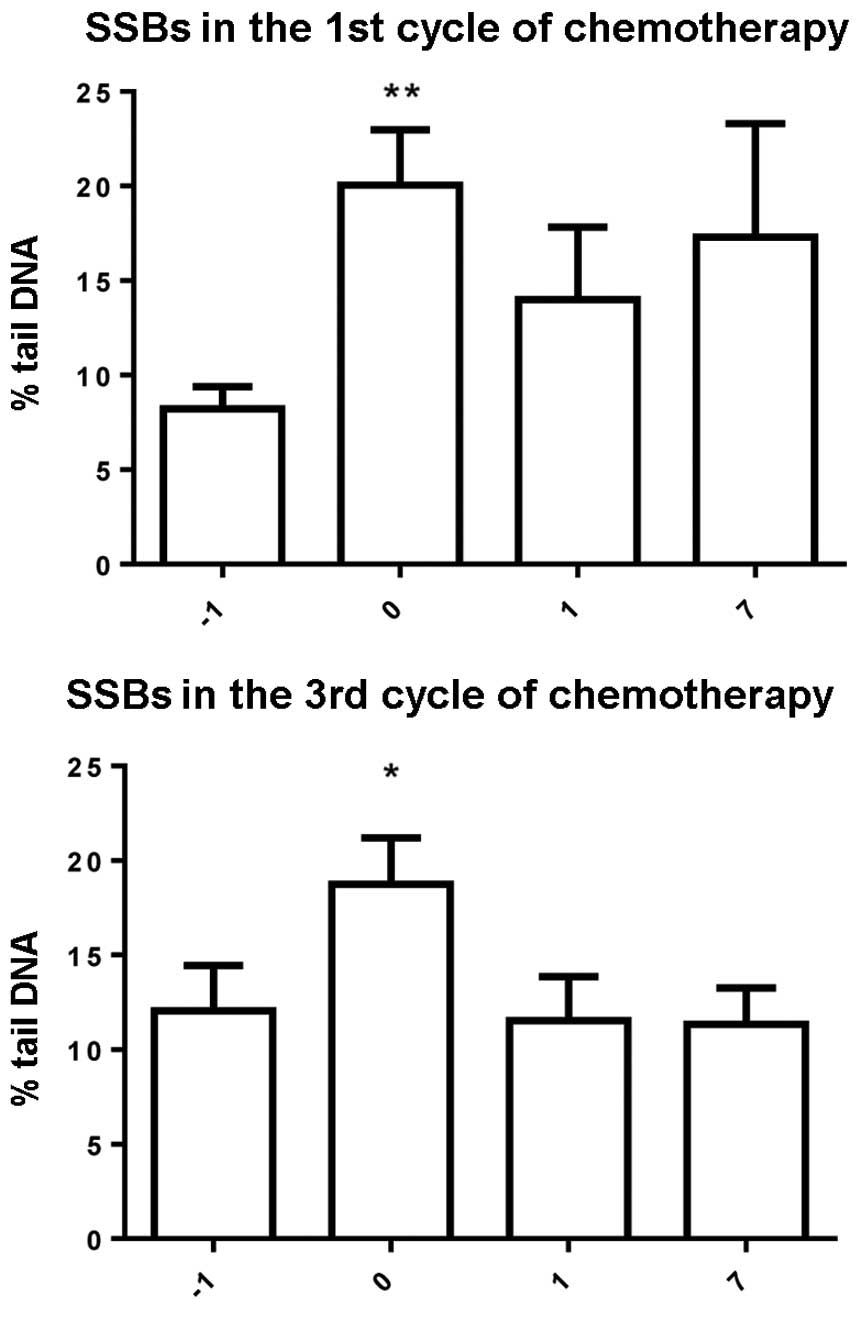
We monitored changes in SSBs in PBLs during the
entire course of chemotherapy. Samples were collected from each
patient during the 1st and 3rd cycles of chemotherapy: 1 day before
starting the cycle, immediately after administration of the
chemotherapy, and 1 and 7 days after completion of the chemotherapy
cycle. The last control measurement was performed 3 weeks after the
final (4th cycle) completed course of chemotherapy. In both cycles
(1st and 3rd), we found a significantly (Friedman test) higher
level of SSBs in measurement immediately after administration of
the chemotherapy (compared to the measurement before chemotherapy).
The level of SSBs then returned towards baseline values (Fig. 2).
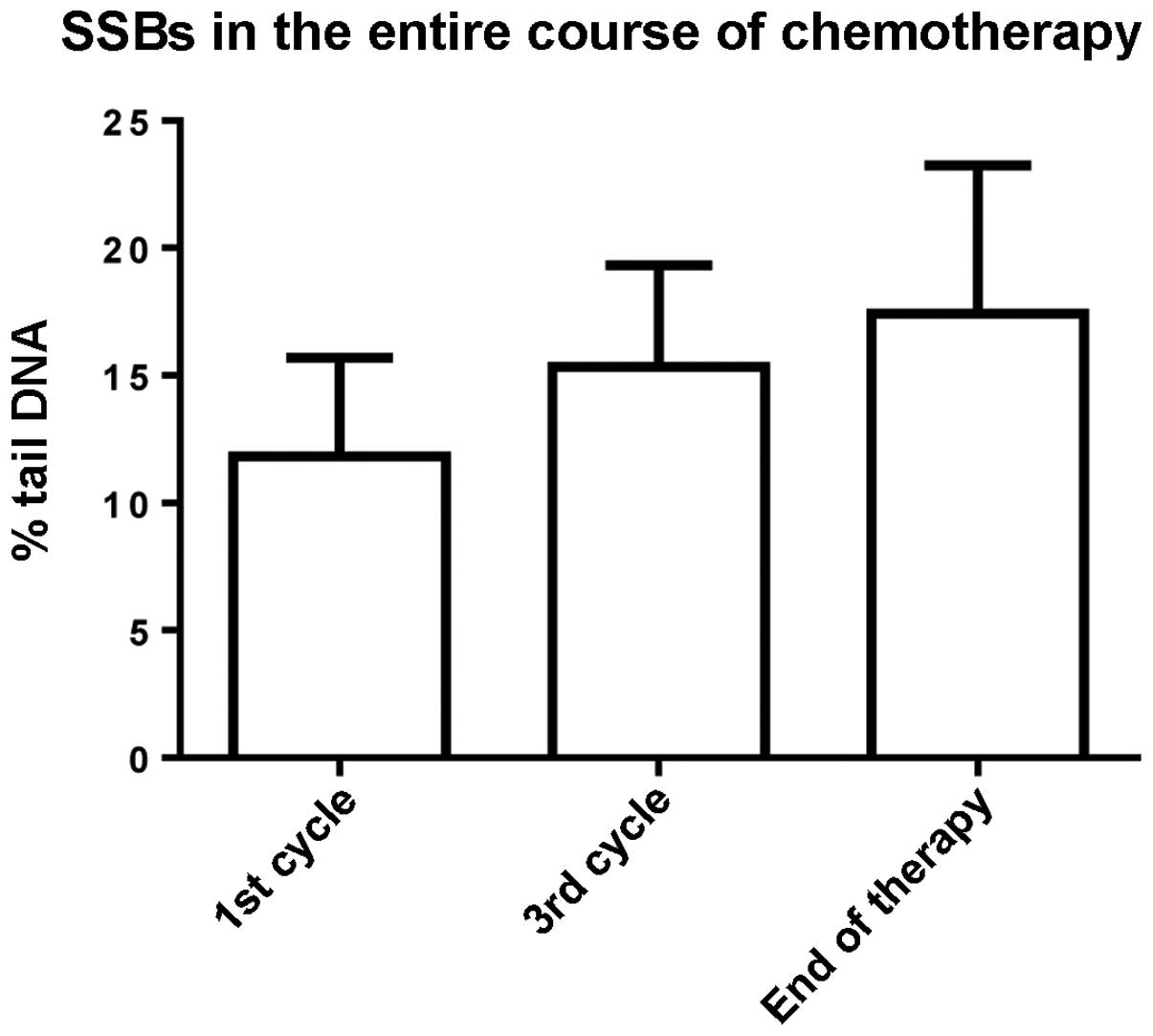
The amount of SSBs increased throughout the course
of chemotherapy, but there were no statistically significant
differences among SSBs measured before chemotherapy, in the middle
of the chemotherapy (3rd cycle) and at the end of the chemotherapy
(Fig. 3).
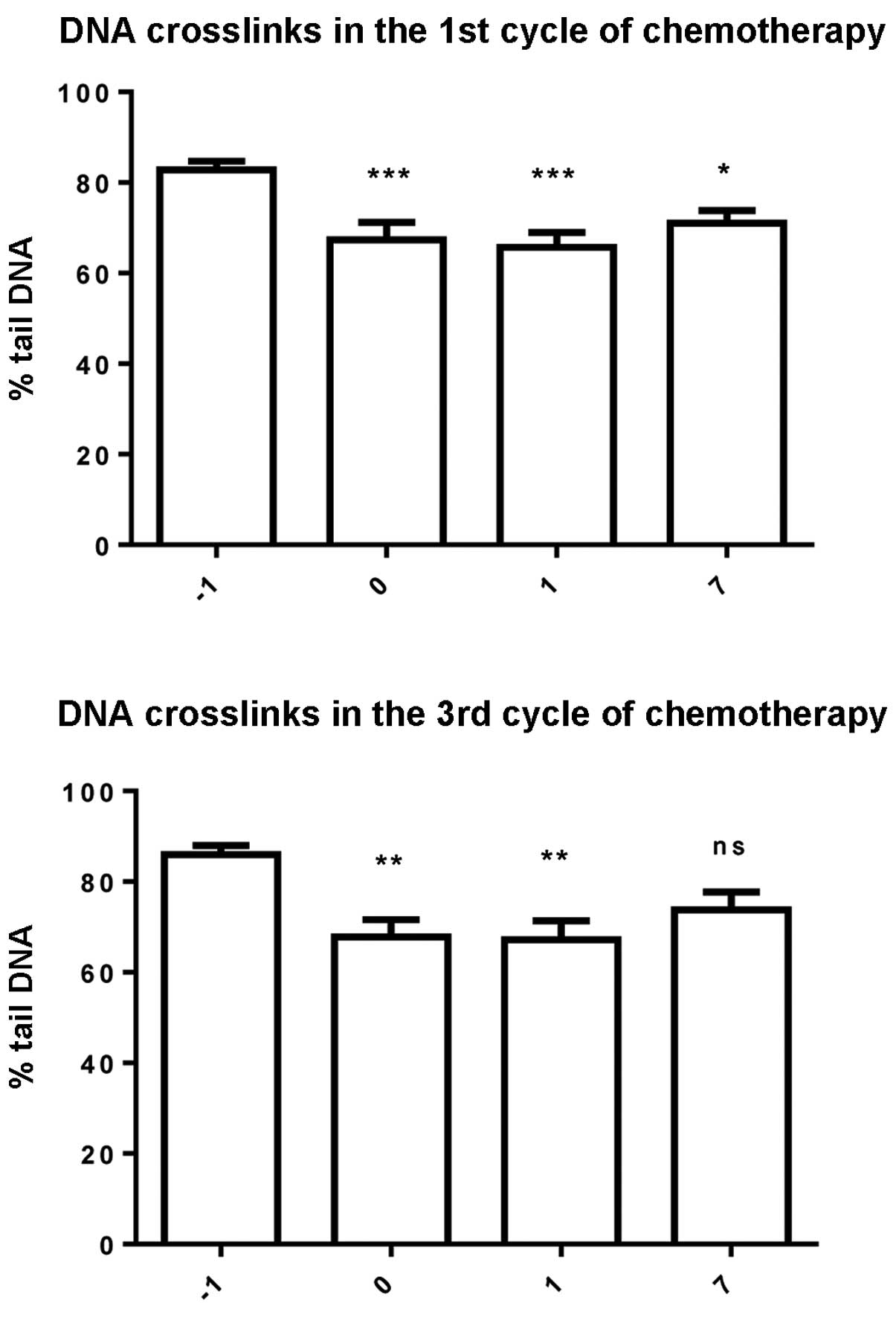
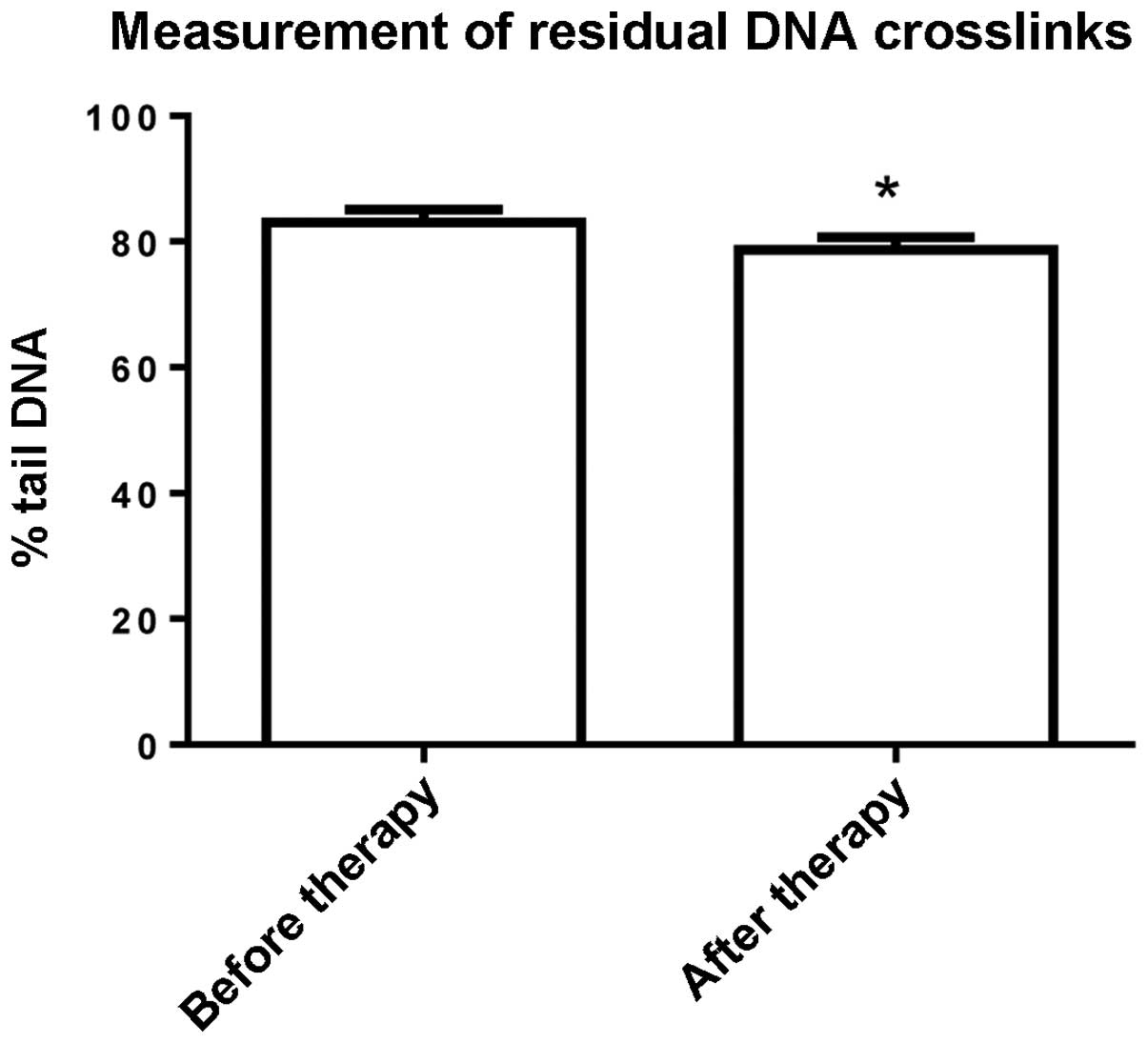
The comet assay protocol, modified for the
measurement of crosslinks (using styrene oxide treatment), was used
to measure the induction and repair of DNA crosslinks caused by
platinum-based derivatives. A significant reduction (Friedman test)
in percentage Tail DNA was found during the 1st and 3rd cycle of
the chemotherapy, indicating the presence of crosslinks (Fig. 4). The value of Tail DNA increased
again after one week although it did not reach the baseline value.
The response in patients showed a similar trend, although there
appeared to be high inter-individual variability. Percentage of
Tail DNA in the measurement at the end of the chemotherapy was
significantly lower than in the measurement before the
chemotherapy, indicating that some DNA crosslinks persist even
after the chemotherapy (P=0.0280 in the paired T-test) (Fig. 5).
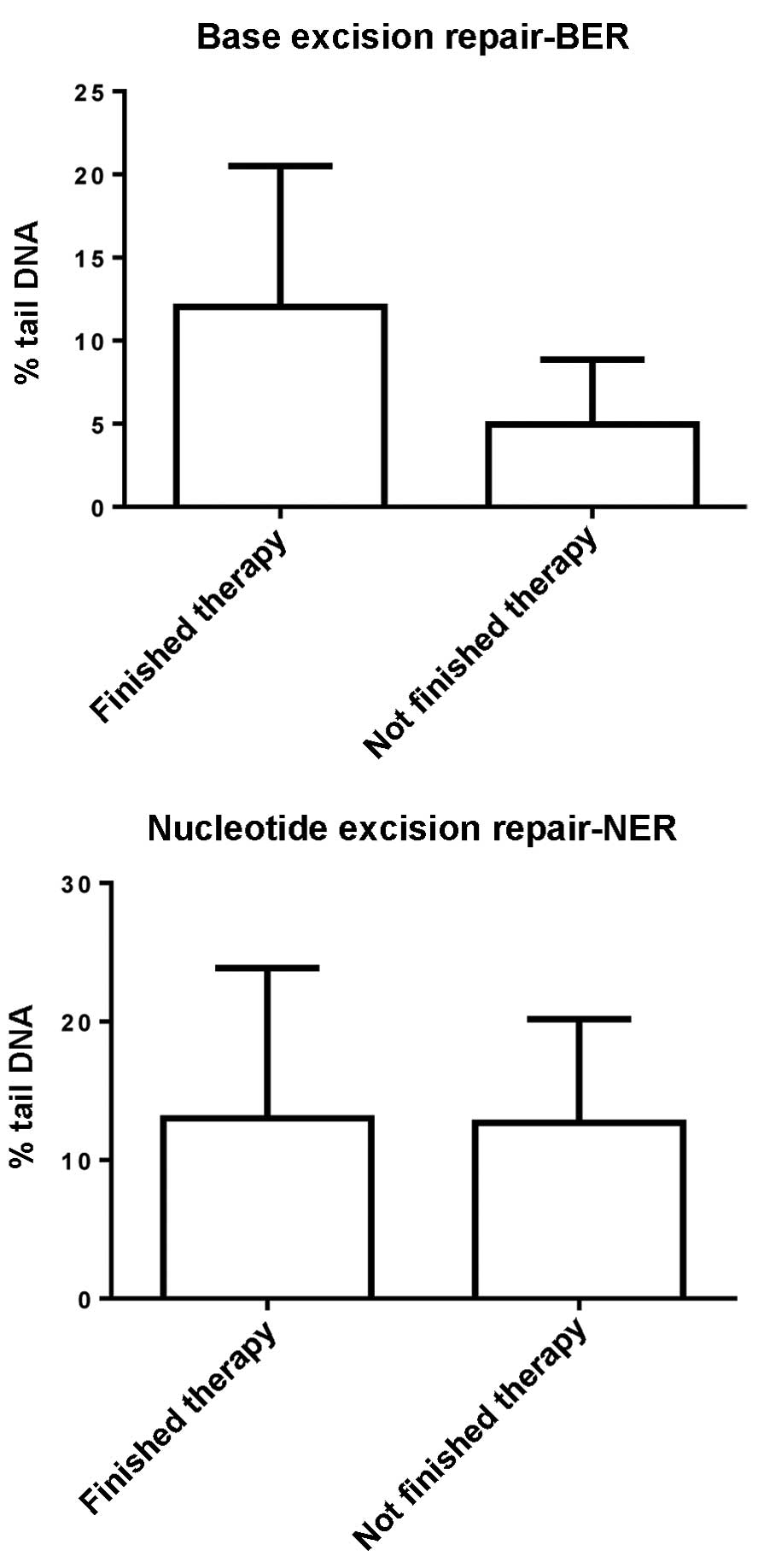
We performed tests for DNA repair, specifically
tests for BER and tests for NER, to determine whether is there any
relationship between DNA repair and patient survival in the last
stage of NSCLC. Using the paired T-test we compared BER and NER in
13 patients who finished the entire course of chemotherapy. In both
cases, we found a non-significant increase of repair at the end of
the chemotherapy compared to the status before the chemotherapy
(Table II). Moreover, we compared
input values of DNA repair (BER and NER) in patients who finished
the whole course of chemotherapy with those who died during the
chemotherapy. We found similar results as for comparison of repair
capacity between patients and controls, thus input values of BER
were non-significantly higher than input values of patients who
finished chemotherapy (P=0.0787 in the Mann-Whitney test) and input
values of NER were almost at the same level in both groups of
patients (P=0.8930 in the Mann-Whitney test) (Fig. 6).
 | Table IIComparison of values of BER and NER of
cancer patients in the course of chemotherapy. |
Table II
Comparison of values of BER and NER of
cancer patients in the course of chemotherapy.
| % Tail DNA ± zSE | Before
chemotherapy | At the end of
chemotherapy | P-value |
|---|
| BER | 12.03±2.355 | 19.62±4.191 | 0.0505 |
| NER | 13±3.015 | 22.01±5.551 | 0.2061 |
We found negative correlation between input values
of NER of cancer patients and the level of DNA crosslinks on the
1st day after administration of chemotherapy in the 3rd cycle of
chemotherapy. We found a negative correlation between NER measured
before the 3rd cycle and persistent DNA crosslinks (measurement at
the end of the chemotherapy).
Discussion
In the present study, we monitored the induction and
repair of DNA breaks and interstrand crosslinks in the DNA of
peripheral lymphocytes isolated from patients with non-small cell
lung carcinoma (NSCLC) during chemotherapy with platinum-based
derivatives. The level of single strand breaks (SSBs) in cancer
patients was compared to SSBs in controls, and also the repair
capacity [base excision repair (BER) and nucleotide excision repair
(NER)] of these patients was compared to that of control subjects.
We found that the number of SSBs was higher in cancer patients
relative to controls, but not significantly. Thus, our findings are
in accordance with published studies showing that the level of
basal DNA damage in peripheral blood lymphocytes (PBLs) of patients
suffering from a variety of cancers is higher than that of controls
(9,21–27).
DNA BER in PBLs of healthy controls was higher
(P=0.0320) compared to that of cancer patients, and DNA NER was
almost at the same level in both controls and patients. Our results
may indicate a link between the process of carcinogenesis and BER,
but not between carcinogenesis and NER. Functional assays performed
in blood leukocytes of cancer patients and matched controls show
that specific BER pathways are less efficient in cancer patients,
which suggests that BER capability may represent a risk factor
(28). Another study which examined
whether reduced DNA repair is associated with lung cancer suggested
that reduced activity of various DNA repair mechanisms causes lung
cancer predisposition (29).
We observed changes in DNA damage (SSBs) in the
course of chemotherapy. In both measured cycles, we found a
significantly higher level of SSBs immediately after administration
of chemotherapy (compared to measurement before chemotherapy). The
level of SSBs increased throughout the entire course of
chemotherapy, but non-significantly. Other studies have confirmed
an increase of SSBs in PBLs of cancer patients after different
combined chemotherapies; in some studies the increase was
significant (30,31), but it was non-significant elsewhere
(32).
We also measured the induction and repair of DNA
crosslinks caused by platinum-based derivatives. In both cycles
(1st and 3rd), we found the highest degree of crosslinking
immediately or 1 day after chemotherapy. Seven days after
chemotherapy the level of crosslinks gradually decreases and
returns to pre- chemotherapy values. We found that some crosslinks
persist in the DNA even after the entire 4 cycles of chemotherapy
and that there is great inter-individual variability among patients
as well. Similar studies demonstrating the formation and repair of
DNA crosslinks have also demonstrated great inter-individual
variability among patients but, in general, the trend for repair of
DNA crosslinks can be monitored (3,33).
DNA repair (BER and NER) was monitored throughout
the whole course of chemotherapy. In patients who survived the
chemotherapy, DNA repair (both BER and NER) increased during the
course of chemotherapy. This increase (at least in the case of BER)
was on the border of statistical significance. Moreover, we
compared levels of DNA repair in patients who survived chemotherapy
with those in patients who died in the course of chemotherapy. We
found similar results as in the comparison of cancer patients with
healthy controls: values of BER were higher in the case of
surviving patients, while levels of NER were essentially the same.
The removal of cisplatin-DNA adducts is mediated by the NER
pathway, in which ERCC1 is one of the key enzymes. The present
study confirmed this, since we found negative correlation between
NER and the level of DNA crosslinks in the course of chemotherapy.
Other studies showed that high expression of ERCC1 had an adverse
effect on survival following the administration of cisplatin-based
chemotherapy in patients with NSCLC (34). There is a hypothesis that lung
cancer patients with lower ERCC1 levels and, thus, lower NER DNA
repair capacity, may have an enhanced response and survival with
cisplatin-based chemotherapy. In an experimental model, elevated
DNA repair capacity was associated with resistance to cisplatin in
lung cancer cell lines (35).
However, no correlation between NER, formation and repair of DNA
crosslinks, or survival of patients was found.
Results from the present study confirm those of
other studies dealing with DNA damage and repair in cancer patients
treated with chemotherapy. Moreover, our results indicated that
despite the fact that cisplatin-DNA adducts are removed by the NER
pathway, BER also plays a role in the clinical status of patients
and their survival. For confirmation of these conclusions, a study
on a larger number of patients is required.
Acknowledgements
The present study was supported by MH CZ-DRO (UHHK,
00179906) and the Faculty of Pharmacy (project no. SVV/267 003).
The authors thank Ian McColl for assisting with the language of the
manuscript.
References
|
1
|
Crohns M, Liippo K, Erhola M, Kankaanranta
H, Moilanen E, Alho H and Kellokumpu-Lehtinen P: Concurrent decline
of several antioxidants and markers of oxidative stress during
combination chemotherapy for small cell lung cancer. Clin Biochem.
12:1236–1245. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gurubhagavatula S, Liu G, Park S, Zhou W,
Su L, Wain JC, Lynch TJ, Neuberg DS, David C and Christiani DC: XPD
and XRCC1 genetic polymorphisms are prognostic factors in advanced
non-small-cell lung cancer patients treated with platinum
chemotherapy. J Clin Oncol. 22:2594–2601. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Almeida GM, Duarte TL, Steward WP and
Jones GD: Detection of oxaliplatin-induced DNA crosslinks in vitro
and in cancer patients using the alkaline comet assay. DNA Repair.
5:219–225. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rosenberg B: Fundamental studies with
cisplatin. Cancer. 55:2303–2316. 1985. View Article : Google Scholar
|
|
5
|
Lebwohl D and Canetta R: Clinical
development of platinum complexes in cancer therapy: an historical
perspective and an update. Eur J Cancer. 34:1522–1534. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dronkert ML and Kannar R: Repair of DNA
interstrand cross-links. Mutat Res. 486:217–247. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Unger FT, Klasen HA, Tchartchian G, de
Wilde RL and Witte I: DNA damage induced by cis- and carboplatin as
indicator for in vitro sensitivity of ovarian carcinoma cells. BMC
Cancer. 9:3592009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rabik CA and Dolan ME: Molecular
mechanisms of resistance and toxicity associated with platinating
agents. Cancer Treat Rev. 33:9–23. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McKenna DJ, McKeown SR and McKelvey-Martin
VJ: Potential use of the comet assay in the clinical management of
cancer. Mutagenesis. 23:183–190. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Faust F, Kassie F, Knasmuller S, Boedecker
RH, Mann M and Mersch-Sundermann V: The use of the alkaline comet
assay with lymphocytes in human biomonitoring studies. Mutat Res.
566:209–229. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Collins AR and Ferguson LR: DNA repair as
a biomarker. Mutat Res. 736:2–4. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Singh NP, McCoy MT, Tice RR and Schneider
EL: A simple technique for the quantitation of low levels of DNA
damage in individual cells. Exp Cell Res. 175:184–191. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Collins AR: The comet assay for DNA damage
and repair: principles, applications, and limitations. Mol
Biotechnol. 26:249–261. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Boyum A: Separation of white blood cells.
Nature. 204:793–794. 1964. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Collins AR, Dobson VL, Dusinská M, Kennedy
G and Stětina R: The comet assay: what can it really tell us? Mutat
Res. 375:183–193. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fikrova P, Stetina R, Hrnciarik M, Rehacek
V, Jost P, Hronek M and Zadak Z: Detection of DNA crosslinks in
peripheral lymphocytes isolated from patients treated with platinum
derivates using modified comet assay. Neoplasma. 60:413–418. 2013.
View Article : Google Scholar
|
|
17
|
Collins AR, Dušinská M, Horváthová E,
Munro E, Savio M and Stětina R: Inter-individual differences in
repair of DNA base oxidation, measured in vitro with the comet
assay. Mutagenesis. 16:297–301. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gaivão I, Piasek A, Brevik A, Shaposhnikov
S and Collins AR: Comet assay based methods for measuring DNA
repair in vitro; estimates of inter- and intraindividual variation.
Cell Biol Toxicol. 25:45–52. 2009.PubMed/NCBI
|
|
19
|
Langie SA, Knaapen AM, Brauers KJJ, van
Berlo D, van Schooten FJ and Godschalk RWL: Development and
validation of a modified comet assay to phenotypically assess
nucleotide excision repair. Mutagenesis. 21:153–158. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Azqueta A, Shaposhnikov S and Collins AR:
DNA repair measured by the comet assay. DNA Repair. Kruman I:
InTech; Croatia: 2011, View
Article : Google Scholar : 2011, Available
from: http://www.intechopen.com/books/dna-repair/dna-repair-measured-by-the-comet-assay.
|
|
21
|
Palyvoda O, Polanska J, Wygoda A and
Rzeszowska-Wolny J: DNA damage and repair in lymphocytes of normal
individuals and cancer patients: studies by the comet assay and
micronucleus tests. Acta Biochim Pol. 50:181–190. 2003.PubMed/NCBI
|
|
22
|
Smith TR, Miller MS, Lohman KK, Case LD
and Hu JJ: DNA damage and breast cancer risk. Carcinogenesis.
24:883–889. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rajeswari N, Ahuja YR, Malini U,
Chandrashekar S, Balakrishna N, Rao KV and Khar A: Risk assessment
in first degree female relatives of breast cancer patients using
the alkaline comet assay. Carcinogenesis. 21:557–561. 2000.
View Article : Google Scholar
|
|
24
|
Sanchez C, Clementi M, Benitez D,
Contreras H, Huidobro C and Castellon E: Effect of GnRH analogs on
the expression of TrkA and p75 neurotrophin receptors in primary
cell cultures from human prostate adenocarcinoma. Prostate.
65:195–202. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lin X, Wood CG, Shao L, Huang M, Yang H,
Dinney CP and Wu X: Risk assessment of renal cell carcinoma using
alkaline comet assay. Cancer. 110:282–288. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schabath MB, Grossman HB, Delclos GL,
Hernandez LM, Day RS, Davis BR, Lerner SP, Spitz MR and Wu X:
Dietary carotenoids and genetic instability modify bladder cancer
risk. J Nutr. 134:3362–3369. 2004.PubMed/NCBI
|
|
27
|
Lou J, He J, Zheng W, Jin L, Chen Z, Chen
S, Lin Y and Xu S: Investigating the genetic instability in the
peripheral lymphocytes of 36 untreated lung cancer patients with
comet assay and micronucleus assay. Mutat Res. 617:104–110. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tudek B: Base excision repair modulation
as a risk factor for human cancers. Mol Aspects Med. 28:258–275.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Paz-Elizur T, Krupsky M, Elinger D,
Schechtman E and Livneh Z: Repair of the oxidative DNA damage
8-oxoguanine as a biomarker for lung cancer risk. Cancer Biomark.
1:201–205. 2005.PubMed/NCBI
|
|
30
|
Sánchez-Suárez P, Ostrosky-Wegman P,
Gallegos-Hernández F, Peñarroja-Flores R, Toledo-García J, Bravo
JL, Del Castillo ER and Benítez-Bribiesca L: DNA damage in
peripheral blood lymphocytes in patients during combined
chemotherapy for breast cancer. Mutat Res. 640:8–15.
2008.PubMed/NCBI
|
|
31
|
Kopjar N, Garaj-Vrhovac V and Milas I:
Assessment of chemotherapy-induced DNA damage in peripheral blood
leukocytes of cancer patients using the alkaline comet assay.
Teratog Carcinog Mutagen. 22:13–30. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Plummer ER, Middleton MR, Jones C, Olsen
A, Hickson I, McHugh P, Margison GP, McGown G, Thorncroft M, Watson
AJ, Boddy AV, Calvert AH, Harris AL, Newell DR and Curtin NJ:
Temozolomide pharmacodynamics in patients with metastatic melanoma:
DNA damage and activity of repair enzymes
O6-alkylguanine alkyltransferase and
poly(ADP-ribose) polymerase-1. Clin Cancer Res. 11:3402–3409. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wynne P, Newton C, Ledermann JA, Olaitan
A, Mould TA and Hartley JA: Enhanced repair of DNA interstrand
crosslinking in ovarian cancer cells from patients following
treatment with platinum-based chemotherapy. Br J Cancer.
97:927–933. 2007.PubMed/NCBI
|
|
34
|
Li XQ, Li J, Shi SB, Chen P, Yu LC and Bao
QL: Expression of MRP1, BCRP, LRP and ERCC1 as prognostic factors
in non-small cell lung cancer patients receiving postoperative
cisplatin-based chemotherapy. Int J Biol Markers. 24:230–237.
2009.PubMed/NCBI
|
|
35
|
Rosell R, Lord RV, Taron M and Reguart N:
DNA repair and cisplatin resistance in non-small-cell lung cancer.
Lung Cancer. 38:217–227. 2002. View Article : Google Scholar : PubMed/NCBI
|