Introduction
Gastric cancer (GC) constitutes the second major
cause of cancer-related mortality worldwide (1). The poor prognosis of this disease,
including its high relapse rate even after curative resection and a
high disease related mortality, has not been substantially improved
in recent decades.
Complete surgical resection is still the standard
treatment for all patients with resectable GC; however, regional
and less common systemic recurrence remain highly problematic.
Although the role of extended lymphadenectomy remains
controversial, it is still accepted that a modified
D2-lymphadenectomy is reasonable, due to its beneficial role for a
subgroup of patients (2–4). Yet, even among patients undergoing
gastrectomy with curative intent, the 5-year survival rates are
disappointingly low at 25 to 30% due to locoregional relapse and
distant metastases (5).
These circumstances have led to various adjuvant and
neoadjuvant protocols. Although a beneficial role is attributed to
adjuvant therapies, these are associated with severe side-effects
often resulting in premature termination of a protocol (6,7).
In contrast to these established procedures, the
idea of tumour-specific therapy is captivating. Major advances have
been achieved in the field of biological-based cancer therapies in
the last decades. Some of the recently approved targeted
therapeutics are currently being evaluated for the treatment of GC
(8,9).
The PAT-SC1 antibody described here was isolated
with the aid of human hybridoma technology from a GC patient
(10). This fully human IgM
antibody reacts with a cancer-specific isoform of CD55
decay-accelerating factor (DAF), subsequently named
CD55PAT-SC1 (11). In
previous studies the antigen was reported to be expressed in ~70%
of diffuse-type gastric carcinoma and in 25% of intestinal-type
according to the Lauren classification (12). More recent studies have demonstrated
the expression of CD55PAT-SC1 in ~80% of patients across
different ethnic groups (unpublished data). Therefore, PAT-SC1 has
a much broader potential than other targeted therapies which are
currently under evaluation for the treatment of GC. One such
therapy, trastuzumab, was found to react with only 22.9% of
advanced GCs (13). PAT-SC1 shows
no cross-reactivity with adult normal tissues, but some
cross-reactivity with embryonal tissue, indicating that the antigen
may be of oncofetal origin (10,14).
Upon binding to CD55PAT-SC1, the antibody
was found to induce apoptosis of stomach carcinoma cells in
vitro (14) and in vivo
and showed tumour-suppressing activity in xenograft animal models
(15). The apoptotic effect was not
only noted in the primary tumour but in disseminated tumour cells
as well (16). Disseminated tumour
cells in the blood of patients with GC are an independent
predictive marker of poor prognosis (17).
Based on these promising results, an academic
single-dose clinical study in patients with primary GC was
initiated in 1997 with the primary aim to establish the safety of
PAT-SC1 in humans and to confirm the ability of the PAT-SC1
antibody to induce tumour-specific apoptosis in a neoadjuvant
setting. The study was conducted in 51 patients with positively
proven expression of the CD55PAT-SC1 antigen. In
addition to the safety and the histopathological effect of the
antibody, the 10-year survival of the R0-resected patients was
investigated and compared to a historical control group.
In addition, in a historical patient group, we
analysed whether the expression of the PAT-SC1 antigen
CD55PAT-SC1 is a prognostic factor for cancer-related
survival.
Patients and methods
Antibody production and purification
The antibody was produced in miniPERM bioreactors
and purified by a two-step purification scheme as outlined
previously (18).
Clinical protocol
In a prospective series from July 1997 to January
2001, patients with primary GC were tested for expression of
CD55PAT-SC1. Preoperative biopsies (obtained
endoscopically) from the cancer were stained immunohistochemically
with the PAT-SC1 antibody according to the protocol published by
Vollmers et al (12). In
case of a positive reaction of the antibody with the tumour, the
patient was defined as being CD55PAT-SC1-positive.
Forty-eight hours prior to the surgical treatment, the patients
were administered intravenously a single dose of 20 mg PAT-SC1
diluted in 500 ml infusion solution over 4 h. During the infusion,
patients were placed on the intermediate care unit for the
monitoring of vital parameters. All patients provided written
informed consent for the preoperative antibody treatment. The study
protocol was approved by the Ethics Committee of the University of
Würzburg.
Surgical procedure
For radical resection (R0) according to the Union
Internationale Contre le Cancer (UICC) 1997, a total gastrectomy
with a modified D2-lymphadenectomy according to the site of the
tumour was performed. Lymphadenectomy included compartment I (lymph
nodes along the greater and lesser curvature) and compartment II
dependent on the site of the tumour. The lymph nodes on the upper
margin of the pancreas and within the hilus of the spleen were
removed only when the primary tumour affected the corpus or left
sided margin of the stomach. If the tumour was located in the
distal part of the stomach, lymph nodes within the hepatoduodenal
ligament and paraaortic were dissected as well (compartment
III/IV). The tail of the pancreas and the spleen were resected only
when directly involved by the tumour.
Study population
Fifty-one patients with primary carcinoma of the
stomach expressing CD55PAT-SC1 were included in the
study and were consecutively treated with the human monoclonal
antibody PAT-SC1. The details of the patient population are
summarized in Table I (group
3).
 | Table IDemographic features and clinical
staging of the groups used for the evaluation of PAT-SC1 effect and
PAT-SC1 antigen expression as a diagnostic/prognostic marker. |
Table I
Demographic features and clinical
staging of the groups used for the evaluation of PAT-SC1 effect and
PAT-SC1 antigen expression as a diagnostic/prognostic marker.
| Group 1
CD55PAT-SC1-positive (prior to 1997) (n=93) | Group 2
CD55PAT-SC1-negative (prior to 1997) (n=33) | Group 3
CD55PAT-SC1-positive (after 1997) (n=51) |
|---|
| Age (years) mean ±
SD | 63.7±11.5 | 64.4±12.0 | 62.6±12.6 |
| Gender n (%) |
| Female | 32 (34.4) | 11 (33,3) | 26 (51,0) |
| Male | 61 (65.6) | 22 (66.7) | 25 (49.0) |
| Histological stage
(%) |
| Adenocarcinoma
(intestinal type) | 47 (50.5) | 18 (54.5) | 9 (17.6) |
| Signet ring cell
carcinoma (diffuse type) | 43 (46.2) | 15 (45.5) | 36 (70.6) |
| Other | 3 (3.2) | | 6 (11.8) |
| UICC staging
(%) |
| 1A | 9 (9.7) | 5 (15.2) | 10 (19.6) |
| 1B | 8 (8.6) | 5 (15.2) | 10 (19.6) |
| 2 | 15 (16.1) | 7 (21.2) | 11 (21.6) |
| 3A | 20 (21.5) | 8 (24.2) | 3 (5.9) |
| 3B | 10 (10.8) | 2 (6.1) | 4 (7.8) |
| 4 29 | (31.2) | 5 (15.2) | 12 (23.5) |
| X | 2 (2.2) | 1 (3.0) | 1 (2.0) |
| Residual tumour
classification (%) |
| R0 | 53 (57.0) | 26 (78.8) | 35 (70.0) |
| R1 | 11 (11.8) | 3 (9.1) | 2 (4.0) |
| R2 | 29 (31.2) | 4 (12.1) | 13 (26.0) |
Historical data collection for the
patients with GC for retrospective analysis of the expression of
the PAT-SC1 antigen as a prognostic marker
To prove if the expression of CD55PAT-SC1
is of prognostic value, historical patient data from the University
Hospital Würzburg were evaluated. For this comparison, data were
included from patients who underwent radical gastrectomy and
lymphadenectomy due to GC prior to 1997. Surgery was performed
using the same methodology as in the study group (group 3/Table I). No adjuvant or neoadjuvant
treatment was performed. Antigen expression of these patients was
determined from paraffin-embedded tumour material, retrospectively.
One hundred twenty-six patients were included: 93 were positive
(group 1/Table I) and 33 were
negative (group 2/Table I) for
CD55PAT-SC1 expression. Both groups
(CD55PAT-SC1-positive and
CD55PAT-SC1-negative) were comparable in regards to UICC
stage (p=0.8121 Chi-square test).
Tumour regression
A semi-quantitative analysis was performed by two
independent experts, who microscopically evaluated three fields
from each tumour specimen and graded them on a scale of 1 to 3: 1,
low; 2, frequent; 3, high.
The values for the three fields were added together,
and then subtracted from the total score obtained from the three
fields of the biopsies taken before PAT-SC1 treatment. If the
difference was <2, tumour regression was graded as 0; if the
difference was between 2 and 3, tumour regression was graded as
(+); if the difference was ≥4, tumour regression was rated as
(++).
A consensus value was found between the experts as
the final scoring of tumour regression.
Analysis of apoptosis
Staining for apoptosis was performed as described
previously (18). A
semi-quantitative analysis was performed by two independent
experts, who evaluated via microscopy three fields from the tumour
specimens and graded them in comparison to the biopsy taken before
the treatment. The scoring range from no apoptosis (−) to (+++)
using a Tunel assay: (−), negative, similar to biopsy taken prior
to PAT-SC1 treatment; (+), up to 30% more apoptotic cells; (++), up
to 60% more apoptotic cells and (+++), 60 to 100% apoptotic cells.
As a reference, DNase-induced apoptosis was determined to be
100%.
Follow-up
All patient data were followed up with the tumour
registry of the University of Würzburg. Patients with curative
resection were followed up within the first and second year after
surgery every three months in our outpatient department or at the
general practitioner’s office to perform follow-up evaluation. The
follow-up included patient history, a physical examination and
blood tests (full blood count, electrolyte values, blood urea
nitrogen, liver function tests and tumour markers). Endoscopy of
the upper GI-tract was performed 12 months after surgery. After the
second year, the patients were followed up once each year for
routine examination. Further examinations were performed according
to changes in the clinical status of the patient. The follow-up
after palliative resection was performed according to the clinical
status of each patient individually.
Data evaluation and statistical
analysis
Patient data, side-effects, response to antibody
treatment (apoptosis of tumour cells, regression of tumour),
postoperative course, histopathological evaluation (staging and
grading according to TNM and UICC) and follow-up were recorded.
Comparison of UICC stages in the study group and the comparison
group was performed with the two group Chi-square test. The
survival rate was determined by Kaplan-Meier analysis. Differences
between survival curves were calculated with the log-rank test.
p<0.05 was considered to indicate a statistically significant
result.
Results
Patient characteristics
There was no 30-day mortality. The follow-up period
was carried out for a minimum of 120 months. The evaluation
described here was focused on the patient group undergoing curative
(R0) resection. Of this group, 16 patients died of tumour-related
causes, 18 patients were alive at the time of evaluation and there
was one non-tumour-related death.
Side-effects due to the antibody
therapy
The infusion with the PAT-SC1 antibody was generally
well-tolerated. Nineteen (37.3%) patients exhibited a total of 35
adverse events, 32 of grade 1, and 3 of grade 2 (Table II). More severe side-effects of
grade 3 or 4 were not observed. One patient had a short period of
shaking chill, which led to the termination of the PAT-SC1 infusion
after injection of 15 mg. One patient had an early termination of
the infusion due to an anaphylactic reaction and hypotension. All
other patients received the scheduled amount with a median dose of
20 mg (2 patients 10 mg, 44 patients 20 mg, 3 patients 30 mg).
 | Table IISide-effects observed during PAT-SC1
treatment. |
Table II
Side-effects observed during PAT-SC1
treatment.
| System Organ
Class | Grade 1 | Grade 2 | Grade 3 | Grade 4 | All grades |
|---|
| Preferred Term | n (%) | n (%) | n (%) | n (%) | n (%) |
|---|
| Cardiac
disorders | 4 (7.8) | | | | 4 (7.8) |
| Bradycardia
NOS | 2 (3.9) | | | | 2 (3.9) |
| Tachycardia
NOS | 2 (3.9) | | | | 2 (3.9) |
| Gastrointestinal
disorders | 1 (2.0) | | | | 1 (2.0) |
| Nausea | 1 (2.0) | | | | 1 (2.0) |
| General disorders
and administration side conditions | 13 (25.5) | 1 (2.0) | | | 14 (27.5) |
| Application site
cold feeling | 4 (7.8) | 1 (2.0) | | | 4 (7.8) |
| Pyrexia | 7 (13.7) | | | | 8 (15.7) |
| Rigors | 2 (3.9) | | | | 2 (3.9) |
| Immune system
disorders | 1 (2.0) | 1 (2.0) | | | 2 (3.9) |
| Anaphylactic
reaction | 1 (2.0) | 1 (2.0) | | | 2 (3.9) |
| Musculoskeletal and
connective tissue disorders | 3 (5.9) | | | | 3 (5.9) |
| Arthralgia | 1 (2.0) | | | | 1 (2.0) |
| Back pain | 1 (2.0) | | | | 1 (2.0) |
| Groin pain | 1 (2.0) | | | | 1 (2.0) |
| Nervous system
disorders | 4 (7.8) | | | | 4 (7.8) |
| Dizziness | 1 (2.0) | | | | 1 (2.0) |
| Headache | 3 (5.9) | | | | 3 (5.9) |
| Vascular
disorders | 6 (11.8) | 1 (2.0) | | | 7 (13.7) |
| Cyanosis
peripheral | 1 (2.0) | | | | 1 (2.0) |
| Hypertension
NOS | 2 (3.9) | | | | 2 (3.9) |
| Hypotension
NOS | 3 (5.9) | 1 (2.0) | | | 4 (7.8) |
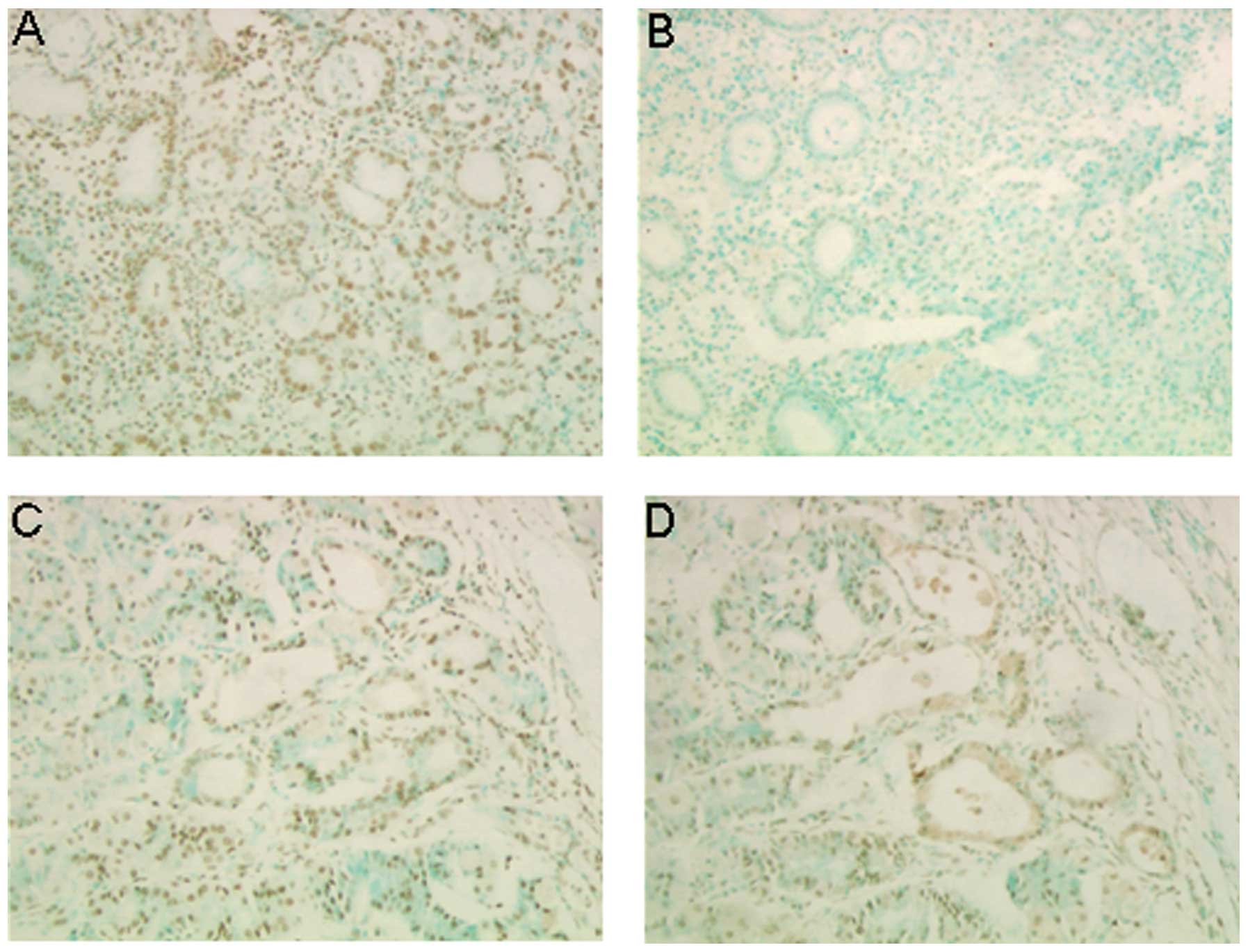
Apoptosis and regression
The primary endpoint was the measurement and
comparison of apoptosis in the resected tumour compared to the
pre-treatment biopsy by a Klenow nicked-end DNA labeling IHC assay
on paraffin-embedded tissue sections. In Fig. 1 an example of analysis of apoptosis
is shown. The pre-treatment biopsy showed no apoptotic cells
whereas an increase in the amount of apoptotic cells was
demonstrated in the post-treatment tumour sample. A high (++)
(n=21) or moderate (+) (n=18) increase in apoptosis after antibody
treatment was noted in 39 out of 51 (78%) patients, and in 9 (18%)
patients no increase in apoptosis (−) was noted (Table III). In 2 (4%) patients, the
analysis could not be performed due to the small amount of tumour
cells in the samples, and 1 (2%) patient was not included due to
another tumour resection prior to the gastrectomy. There was no
statistically significant difference in the degree of apoptosis and
patient survival (p=0.49).
 | Table IIIResidual tumour classification and
histological examination of the primary tumours for occurrence of
apoptosis and tumour regression after PAT-SC1 treatment and
gastrectomy. |
Table III
Residual tumour classification and
histological examination of the primary tumours for occurrence of
apoptosis and tumour regression after PAT-SC1 treatment and
gastrectomy.
| R0
patients
n=35
n (%) | R1–R2
patients
n=15
n (%) | ITT
population
n=51
n (%) |
|---|
| Residual tumour
classification | | | |
| R0 | | | 35 (68.6) |
| R1 | | | 2 (3.9) |
| R2 | | | 13 (25.5) |
| Missing tumour
classification | | | 1 (2.0) |
| Apoptosis
(consensus) | | | |
| Patients
evaluated | 34 | 14 | 48 |
| − | 6 (17.6) | 3 (21.4) | 9 (18.8) |
| + | 11 (32.4) | 6 (42.9) | 17 (35.4) |
| ++ | 17 (50.0) | 5 (35.7) | 22 (45.8) |
| Tumour regression
(consensus) | | | |
| Patients
evaluated | 31 | 13 | 44 |
| 0 | 11 (35.5) | 7 (53.8) | 18 (40.9) |
| + | 6 (19.3) | 5 (38.5) | 11 (25.0) |
| ++ | 14 (45.2) | 1 (7.7) | 15 (34.1) |
Twenty-six patients (52%) showed a high (++) (n=15)
or moderate (+) (n=11) increase in tumour regression after antibody
treatment and 18 (36%) patients showed no regression (−) after
PAT-SC1 therapy (Table III). In 6
(12%) patients, the analysis was not performed due to technical
problems. Patients with a high degree (++) of regression had a
statistically significant better survival (p=0.0214) compared to
the survival of patients with moderate or no tumour regression.
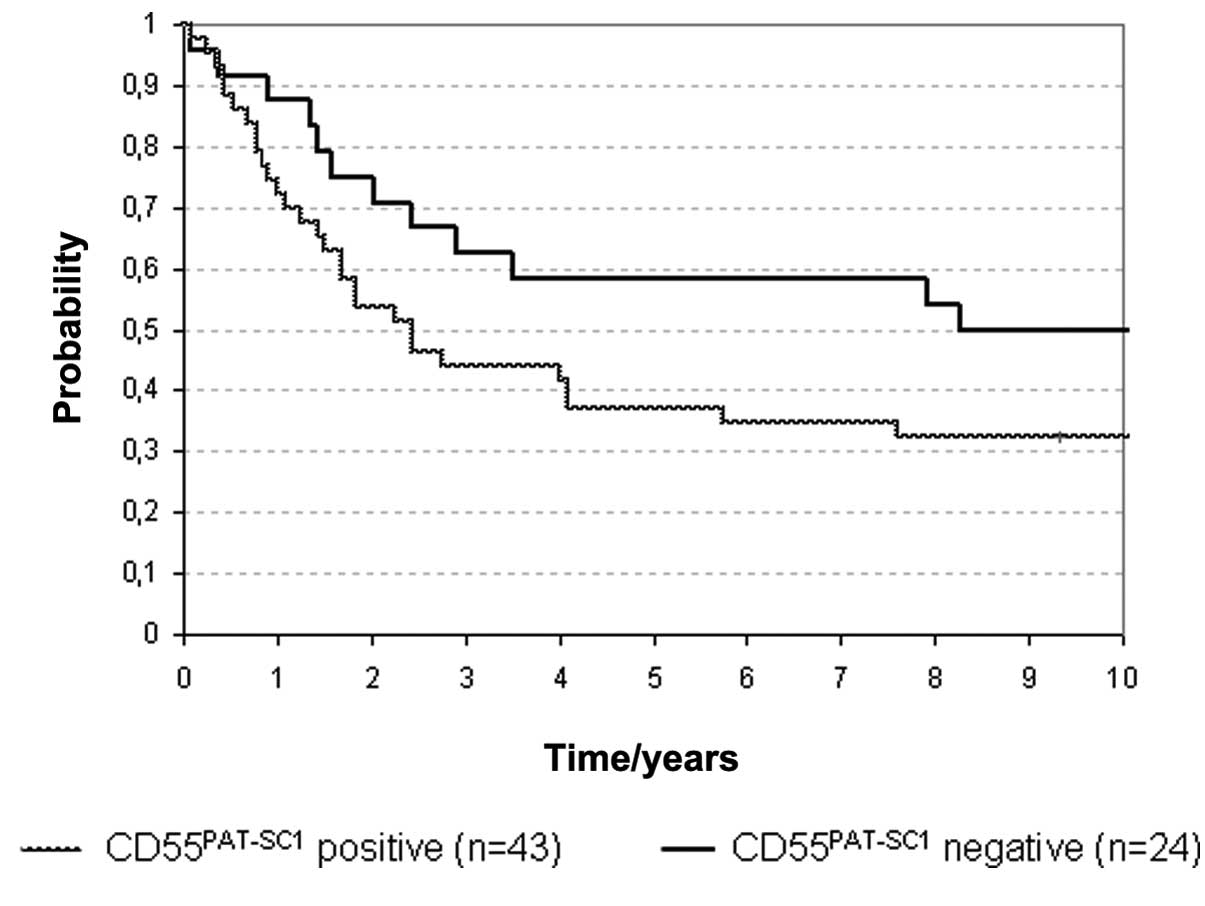
CD55PAT-SC1 expression as a
diagnostic marker
To investigate whether the expression of
CD55PAT-SC1 has any influence on the prognosis of GC
patients, a historical patient population (prior to 1997) was
tested for the expression of the CD55PAT-SC1 by
immunohistochemistry, and the correlation with the survival of the
R0 resected patients was assessed (Fig.
2). The survival rates of the 10-year follow-up were determined
for 43 CD55PAT-SC1-positive patients (group 1) and 24
CD55PAT-SC1-negative patients (group 2).
The data indicate that the expression of
CD55PAT-SC1 had a trend toward a correlation with poorer
survival but did not reach statistical significance with the number
of patients studied (p=0.227).
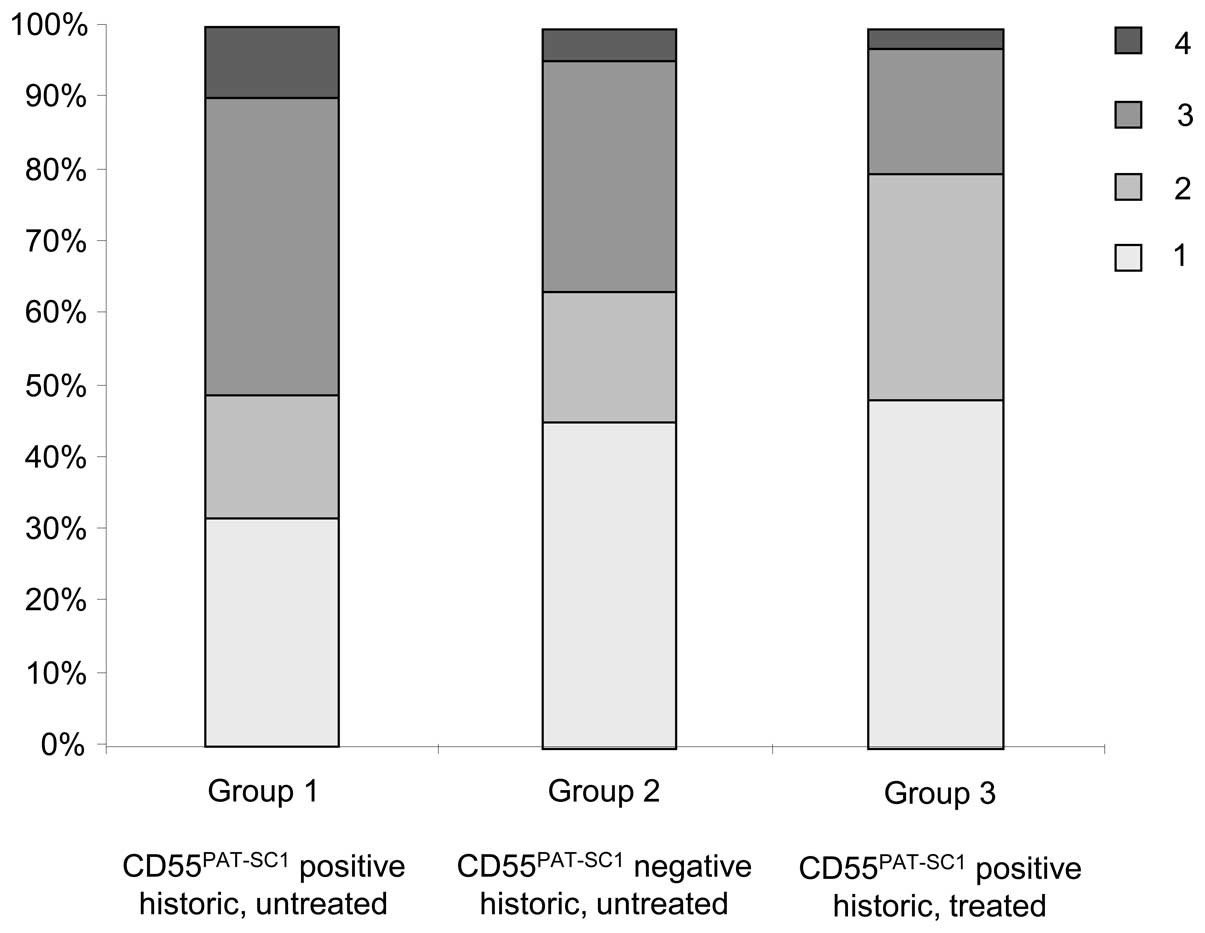
Distribution of the tumour stages
To verify the comparability of the study groups, the
distribution of the tumour stages was evaluated (Fig. 3). The staging was available for 41
of the 43 (95.3%) CD55PAT-SC1-positive and untreated
patients (group 1), 22 of the 24 (91.6%)
CD55PAT-SC1-negative and untreated patients (group 2)
and all (n=35, 100%) of the CD55PAT-SC1-positive treated
patients (group 3).
The data indicated that the tumour stages in the
CD55PAT-SC1-positive untreated patients were
significantly higher (51% stage 3 and 4) than the stages in the
CD55PAT-SC1-positive but treated patient group (20%
stage 3 and 4). There were no other inclusion criteria other than
operability for inclusion into the PAT-SC1-treated group.
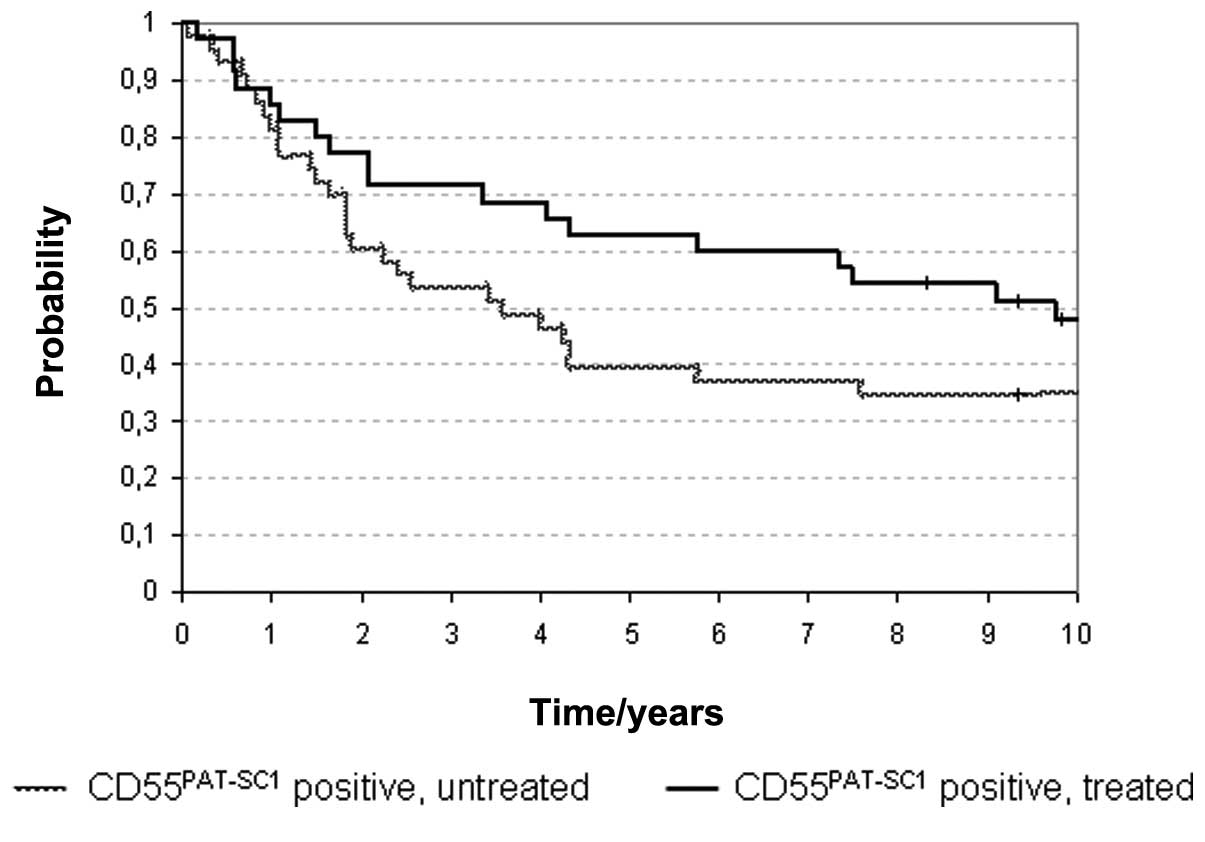
Results of retrospective analysis
Retrospective analysis of the 10-year survival of
CD55PAT-SC1-positive, untreated patients (group 1) vs.
the CD55PAT-SC1-positive, treated group revealed a
survival benefit (Fig. 4). While in
the group 1 only 15 out of 43 (34.9%) patients were alive, and in
group 3 (CD55PAT-SC1-positive, treated), 16 out of 35
(45.7%) patients were alive 10 years after antibody treatment and
curative tumour resection.
Discussion
This is the first long-term follow-up of a clinical
trial assessing an additive treatment for stomach cancer consisting
of a fully human IgM antibody directed specifically against the
tumour-specific CD55PAT-SC1 variant of CD55. In
comparison to radiation or chemotherapy, the effect of PAT-SC1 is
highly specific for susceptible tumour cells that express the
CD55PAT-SC1. PAT-SC1 also has broader reactivity for GCs
than other targeted therapeutics currently under investigation.
The present study showed three main results. i) The
previously described effects of the PAT-SC1 antibody in
vitro and in vivo, which included induction of apoptosis
in tumour cells and tumour regression, were confirmed in the
majority of PAT-SC1-treated patients. ii) The safety and
tolerability of the human antibody PAT-SC1 was excellent with no
major side-effects following antibody treatment. iii) The survival
rate of R0-resected, CD55PAT-SC1-positive, PAT-SC1
antibody-treated patients after 10 years was prolonged compared to
a historical control group of CD55PAT-SC1-positive
patients with R0-resection not treated with the PAT-SC1
antibody.
Apoptosis and tumour regression due to
PAT-SC1 antibody treatment
PAT-SC1 is a natural human IgM antibody with high
specificity to tumour cells of GC. Following the binding of the
antibody to the CD55PAT-SC1 antigen on tumour cells
in vitro, the antibody triggers highly specific apoptosis
(14). GC xenograft models with
PAT-SC1 showed that tumour cell-specific apoptosis can also be
induced in vivo, and a tumour reduction of up to 80% was
achieved (15,16).
The present study demonstrated that even with low
doses of the antibody, an induction of tumour regression and
apoptosis of gastric tumour cells in patients, prior to standard
surgical resection, were induced. We compared preoperative biopsies
from the CD55PAT-SC1-positive tumours before antibody
therapy and after antibody therapy and tumour resection. Despite
the small dose of the antibody (mean, 20 mg/patient) an increase in
apoptosis was observed in 39 of the 48 (81%) patients evaluated.
Tumour regression was observed in 26 of the 44 (59.1%) patients,
thus confirming the previously described effects in vitro
and in vivo animal models. Tumour regression studies have
shown PAT-SC1 to be of prognostic value (19), and the finding of increased tumour
regression after antibody treatment and increased 10-year survival
rate indicates the effectiveness of the antibody.
Tolerability of PAT-SC1
In the present study the treatment with the PAT-SC1
antibody did not cause severe side-effects. The observed
side-effects were all of a minor nature not exceeding grade II
(according to the WHO, Common Toxicity Criteria). While the
relatively low dose of the PAT-SC1 antibody tested in this trial
may be one reason for this finding, one can speculate that the
human origin and germline configuration of the PAT-SC1 antibody
contributes to the good tolerability of the antibody. Furthermore,
the antigen, CD55PAT-SC1, to date, has been only
detected on cancer tissues, therefore decreasing the chance of
unwanted side-effects on healthy tissues as noted for other
targeted therapeutics. Recent studies with approved antibodies for
GC showed more severe side-effects such as gastric perforation or
thromboembolic events as observed in therapy with bevacizumab
(20) Additional analysis revealed
that the application of apoptosis-inducing antibody PAT-SC1 prior
to surgery of gastric tumours had a mild if any effect on the
immune system. Therefore, from an immunological point of view, the
treatment with this monoclonal antibody is extremely safe (21).
Survival analysis and role of minimal
residual disease
Although overall survival was not an endpoint of our
study, we evaluated the 10-year survival of the PAT-SC1-treated
patients vs. a historical control group. The data revealed that
despite the low dose of PAT-SC1, a benefit in the 10-year survival
rate was observed. We found that the survival of
CD55PAT-SC1-expressing GC patients was increased after
neoadjuvant treatment with PAT-SC1 compared to a historic control
group of CD55PAT-SC1-positive patients (49 vs. 35%) even
after an observation period of 10 years. This may be regarded as
further evidence that neoadjuvant or additive therapies may improve
patient survival after radical resection of GC. In a recent
meta-analysis, a slight benefit in postoperative survival was
described for patients with additional chemotherapy. The intergroup
study reported a significant 15% survival benefit for patients
receiving postoperative radiochemotherapy compared to those in a
surgery only group (22).
Despite the fact that in the present study the
patients of the different groups were not randomized but selected
solely on the basis of CD55PAT-SC1 expression and
despite the small number of patients included, the biological
effect of the PAT-SC1 treatment cannot be ignored. Notably, in our
treatment group only minor side-effects were observed whereas in
the intergroup study, the toxicity of the adjuvant protocol was
high (WHO grade III in 6% of patients). An influence of the
CD55PAT-SC1 status on the prolonged survival of our
patients can be ruled out as our data indicate that the expression
of CD55PAT-SC1 is a negative prognostic factor. In our
retrospective data analysis, patients with tumours not expressing
the CD55PAT-SC1 had a better survival rate than those
with tumours expressing the antigen and not receiving antibody
therapy. Our favoured hypothesis for the therapeutical effect of
PAT-SC1 as additive therapy in addition to radical surgery is a
reduction in disseminated tumour cells (DTCs). DTCs are a sign of
minimal residual disease (MRD), and confirmation of DTCs is
discussed as a reason for relapse and occurrence of peritoneal or
distant metastases (23,24). DTCs have been detected in many
patients with different types of solid tumours (25). The presence of DTCs and MRD in
cancer patients is predictive of a poor clinical outcome (24). The effective elimination of DTCs was
found to result in a better prognosis in breast cancer patients
(24). In a study by our group we
identified DTCs in the venous blood of GC patients as an
independent marker of poor prognosis (17).
As long as DTCs are in a non-proliferating status of
dormancy, most adjuvant agents fail to eliminate DTCs (26). Antibodies such as PAT-SC1 which
induce apoptosis in cancer cells irrespective of their status of
proliferation may represent a much more effective tool for reducing
MRD and thus improving patient prognosis if local clearance of the
tumour has been achieved by radical surgery. Furthermore, we showed
that DTCs can be detected in an animal model with GC (27) and that therapy of the animals with
PAT-SC1 reduced the DTCs (16).
Expression of CD55PAT-SC1 was detectable in positive
lymph nodes, distant metastases and tumour cells of the peritoneal
cavity in patients with GC (18).
For this reason, the PAT-SC1 antibody may be highly effective for
all forms of MRD.
In conclusion, the human IgM antibody PAT-SC1
induces highly specific apoptosis in tumour cells expressing the
tumour-specific variant of CD55. In contrast to other therapeutic
antibodies against solid tumours, the PAT-SC1 antibody is well
tolerated by patients. The expression of CD55PAT-SC1 can
easily be determined in preoperative biopsies, which offers a novel
patient- and tumour-specific neoadjuvant therapy for GC. Together
with radical surgical treatment, a single preoperatively
administered dose of PAT-SC1 may improve patient survival possibly
through reduction of MRD. However, given the disparity of the
stages between the treatment and the historical control groups it
is not possible to draw definitive conclusions in respect to the
survival benefit. To verify this, a randomized trial is necessary
which is justified based on the survival difference observed along
with the histopathological data. Given that there is an increasing
amount of data indicating that IgM antibodies are suitable
therapeutic agents, further research is needed in order to advance
this class of antibodies for use in the clinic.
Acknowledgements
The authors thank Ewa Wozniak and Tina Grieb for the
excellent technical assistance. We would also like to thank Dr
Peter Jones, consultant to Patrys Ltd. for the helpful comments
concerning the manuscript. We thank Professor Matthias Eck for the
histopathological analysis. We thank Dr Uwe Mäder for the
statistical analysis of the data. We thank Professor Arnulf Thiede
and Professor Müller-Hermelink for the support and realization of
the study. This study was supported by the Dr Mildred Scheel
Stiftung, Deutsche Krebshilfe e.V., Bonn, Germany. F.H. is Vice
President, Research and Development of Patrys GmbH, Würzburg,
Germany. S.B. has a consultancy aggreement with Patrys Ltd.,
Australia, and receives, in part, research funding from Patrys
Ltd., Australia. All other authors have nothing to disclose. This
study is in memoriam of Professor H. Peter Vollmers.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2
|
Siewert JR, Böttcher K, Stein HJ and Roder
JD: Relevant prognostic factors in gastric cancer: ten-year results
of the German Gastric Cancer Study. Ann Surg. 228:449–461.
1998.PubMed/NCBI
|
|
3
|
Hartgrink HH and van de Velde CJ: Status
of extended lymph node dissection: locoregional control is the only
way to survive gastric cancer. J Surg Oncol. 90:153–165. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
McCulloch P, Niita ME, Kazi H and
Gama-Rodrigues JJ: Gastrectomy with extended lymphadenectomy for
primary treatment of gastric cancer. Br J Surg. 92:5–13. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
De Vita F, Vecchione L, Galizia G, et al:
Perspectives in adjuvant therapy of gastric cancer. Oncology.
77(Suppl 1): 38–42. 2009.PubMed/NCBI
|
|
6
|
Macdonald JS, Smalley SR, Benedetti J, et
al: Chemoradiotherapy after surgery compared with surgery alone for
adenocarcinoma of the stomach or gastroesophageal junction. N Engl
J Med. 345:725–730. 2001. View Article : Google Scholar
|
|
7
|
Cunningham D, Allum WH, Stenning SP, et
al: Perioperative chemotherapy versus surgery alone for resectable
gastroesophageal cancer. N Engl J Med. 355:11–20. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yoong J, Michael M and Leong T: Targeted
therapies for gastric cancer: current status. Drugs. 71:1367–1384.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Meza-Junco J and Sawyer MB: Metastatic
gastric cancer - focus on targeted therapies. Biologics. 6:137–146.
2012.PubMed/NCBI
|
|
10
|
Vollmers HP, O’Connor R, Müller J,
Kirchner T and Müller-Hermelink HK: SC-1, a functional human
monoclonal antibody against autologous stomach carcinoma cells.
Cancer Res. 49:2471–2476. 1989.PubMed/NCBI
|
|
11
|
Hensel F, Hermann R, Schubert C, et al:
Characterization of glycosylphosphatidylinositol-linked molecule
CD55/decay-accelerating factor as the receptor for antibody
SC-1-induced apoptosis. Cancer Res. 59:5299–5306. 1999.PubMed/NCBI
|
|
12
|
Vollmers HP, Dämmrich J, Hensel F, et al:
Differential expression of apoptosis receptors on diffuse and
intestinal type stomach carcinoma. Cancer. 79:433–440. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fornaro L, Lucchesi M, Caparello C, et al:
Anti-HER agents in gastric cancer: from bench to bedside. Nat Rev
Gastroenterol Hepatol. 8:369–383. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vollmers HP, Dämmrich J, Ribbert H,
Wozniak E and Müller-Hermelink HK: Apoptosis of stomach carcinoma
cells induced by a human monoclonal antibody. Cancer. 76:550–558.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vollmers HP, Hensel F, Hermann R, et al:
Tumor-specific apoptosis induced by the human monoclonal antibody
SC-1: A new therapeutical approach for stomach cancer. Oncol Rep.
5:35–40. 1998.PubMed/NCBI
|
|
16
|
Illert B, Otto C, Vollmers HP, Hensel F,
Thiede A and Timmermann W: Human antibody SC-1 reduces disseminated
tumor cells in nude mice with human gastric cancer. Oncol Rep.
13:765–770. 2005.PubMed/NCBI
|
|
17
|
Illert B, Fein M, Otto C, et al:
Disseminated tumor cells in the blood of patients with gastric
cancer are an independent predictive marker of poor prognosis.
Scand J Gastroenterol. 40:843–849. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Vollmers HP, Zimmermann U, Krenn V, et al:
Adjuvant therapy for gastric adenocarcinoma with the
apoptosis-inducing human monoclonal antibody SC-1: First clinical
and histopathological results. Oncol Rep. 5:549–552.
1998.PubMed/NCBI
|
|
19
|
Becker K, Langer R, Reim D, et al:
Significance of histopathological tumor regression after
neoadjuvant chemotherapy in gastric adenocarcinomas: a summary of
480 cases. Ann Surg. 253:934–939. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shah MA, Ramanathan RK, Ilson DH, et al:
Multicenter phase II study of irinotecan, cisplatin, and
bevacizumab in patients with metastatic gastric or gastroesophageal
junction adenocarcinoma. J Clin Oncol. 24:5201–5206. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Beutner U, Lorenz U, Illert B, et al:
Neoadjuvant therapy of gastric cancer with the human monoclonal IgM
antibody SC-1: Impact on the immune system. Oncol Rep. 19:761–769.
2008.PubMed/NCBI
|
|
22
|
Smalley SR, Benedetti JK, Haller DG, et
al: Updated analysis of SWOG-directed intergroup study 0116: a
phase III trial of adjuvant radiochemotherapy versus observation
after curative gastric cancer resection. J Clin Oncol.
30:2327–2333. 2012. View Article : Google Scholar
|
|
23
|
Heiss MM, Simon EH, Beyer BC, et al:
Minimal residual disease in gastric cancer: evidence of an
independent prognostic relevance of urokinase receptor expression
by disseminated tumor cells in the bone marrow. J Clin Oncol.
20:2005–2016. 2002. View Article : Google Scholar
|
|
24
|
Braun S, Vogl FD, Naume B, et al: A pooled
analysis of bone marrow micrometastasis in breast cancer. N Engl J
Med. 353:793–802. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Allard WJ, Matera J, Miller MC, et al:
Tumor cells circulate in the peripheral blood of all major
carcinomas but not in healthy subjects or patients with
nonmalignant diseases. Clin Cancer Res. 10:6897–6904. 2004.
View Article : Google Scholar
|
|
26
|
Braun S, Pantel K, Müller P, et al:
Cytokeratin-positive cells in the bone marrow and survival of
patients with stage I, II, or III breast cancer. N Engl J Med.
342:525–533. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Illert B, Otto C, Braendlein S, Thiede A
and Timmermann W: Optimization of a metastasizing human gastric
cancer model in nude mice. Microsurgery. 23:508–512. 2003.
View Article : Google Scholar : PubMed/NCBI
|