Introduction
Liver cancer, the third leading cause of
cancer-related death worldwide, is a primary malignant cancer
originating in the liver. There are ~60–70 million liver
cancer-related deaths each year, 50% of which occur in China. Most
patients are diagnosed at intermediate or advanced stages of the
disease (1,2). The early detection and diagnosis of
liver cancer is an important issue that must be addressed. One
study has shown that detection of liver cancer using magnetic
resonance imaging (MRI) has a high degree of accuracy, but there
are some limitations in the method in the identification of small
lesions, particularly in patients with liver lesions smaller than 1
cm, and in detecting liver cancer accompanied by liver cirrhosis
(3). In order to detect small
lesions more clearly, enhancement of the contrast agent in the
contrast ratio and improvement of the MRI resolution of soft
tissues are required. Gadolinium is effective for the imaging of
the brain, kidneys and blood system, but is poor in imaging the
hepatobiliary system. Therefore, it is necessary to investigate
other contrast agents for imaging the liver using MRI.
Superparamagnetic iron oxide (SPIO) has wide applications in the
biomedical field and can be used not only as a drug-release carrier
but also as a targeted probe carrier for monoclonal antibodies,
polypeptides, hormones and genes (4–6). SPIO
has recently garnered much attention in the field of molecular
imaging research (7,8). SPIO is a specific MRI contrast agent
for liver imaging and plays an important role in the diagnosis of
hepatocellular carcinoma, particularly small hepatocellular
carcinoma (9,10). In order to improve the targeting of
SPIO and increase the efficiency of MRI in the diagnosis of
hepatocellular carcinoma, modification of SPIO is necessary. In the
present study, we synthesized SPIO using the chemical
coprecipitation method. The nanoparticle SPIO-PEG-CTX was prepared
using SPIO as the core, coating it with polyethylene glycol (PEG),
and conjugating it with the targeting agent, chlorotoxin (CTX).
This nanoparticle was studied using in vitro and in
vivo MRI to determine its MR characteristics.
Materials and methods
Statement of ethics
The present study was reviewed and approved by the
Second Xiangya Hospital Institutional Review Board. All procedures
involving animals were reviewed and approved by the Institutional
Animal Care and Use Committee of Second Xiangya Hospital (SYXK
2012-003).
Reagents and animals
Reagents used to prepare the nanoparticle
SPIO-PEG-CTX were as follows: iron trichloride hexahydrate (99%),
ferrous chloride tetrahydrate (99%) (both from Aladdin Co.), PEG
[average molecular weight (Mw), 6,000; Sinopharm Chemical Reagent
Co. Ltd.] and CTX (98%; Sigma-Aldrich).
Experimental animals included 8 New Zealand white
rabbits of both genders weighing 2.0–3.0 kg provided by the
Experimental Animal Center of Second Xiangya Hospital. One
tumor-bearing rabbit was provided by Wuhan Union Hospital, Tongji
Medical College, Huazhong University of Science and Technology.
MRI and SPIO hydrophobic
nanoparticles
MRI was performed by Holland Philips Achieva 3.0T X
Series superconducting MRI system and 16-channel SENSE XL Torso
coil.
SPIO hydrophobic nanoparticles were prepared using
the coprecipitation method. Iron trichloride hexahydrate (1.081 g,
4 mmol) and ferrous chloride (0.397 g, 2 mmol) were mixed in a
250-ml 3-necked flask (Fig. 1).
Then, 120 ml deionized water was added into the flask. The flask
was sealed, vacuumed of oxygen, and backfilled with nitrogen 3
times to create an anaerobic environment. Next, the whole iron
solution system was stirred (mechanical agitation, faster than
1,500 rpm), and 0.2 ml oleic acid was added to the mixed solution
drop by drop. Then, 15 ml of ammonium hydroxide (28%) was added
slowly to a 3-necked flask and the mixture was heated to 80°C in an
ultrasonicator. The solution turned brown-black gradually during
the addition of ammonium hydroxide. After 30 min, the SPIO
nanoparticles were prepared, which were dried by centrifugation,
washed with anhydrous alcohol and vacuum dried at room
temperature.
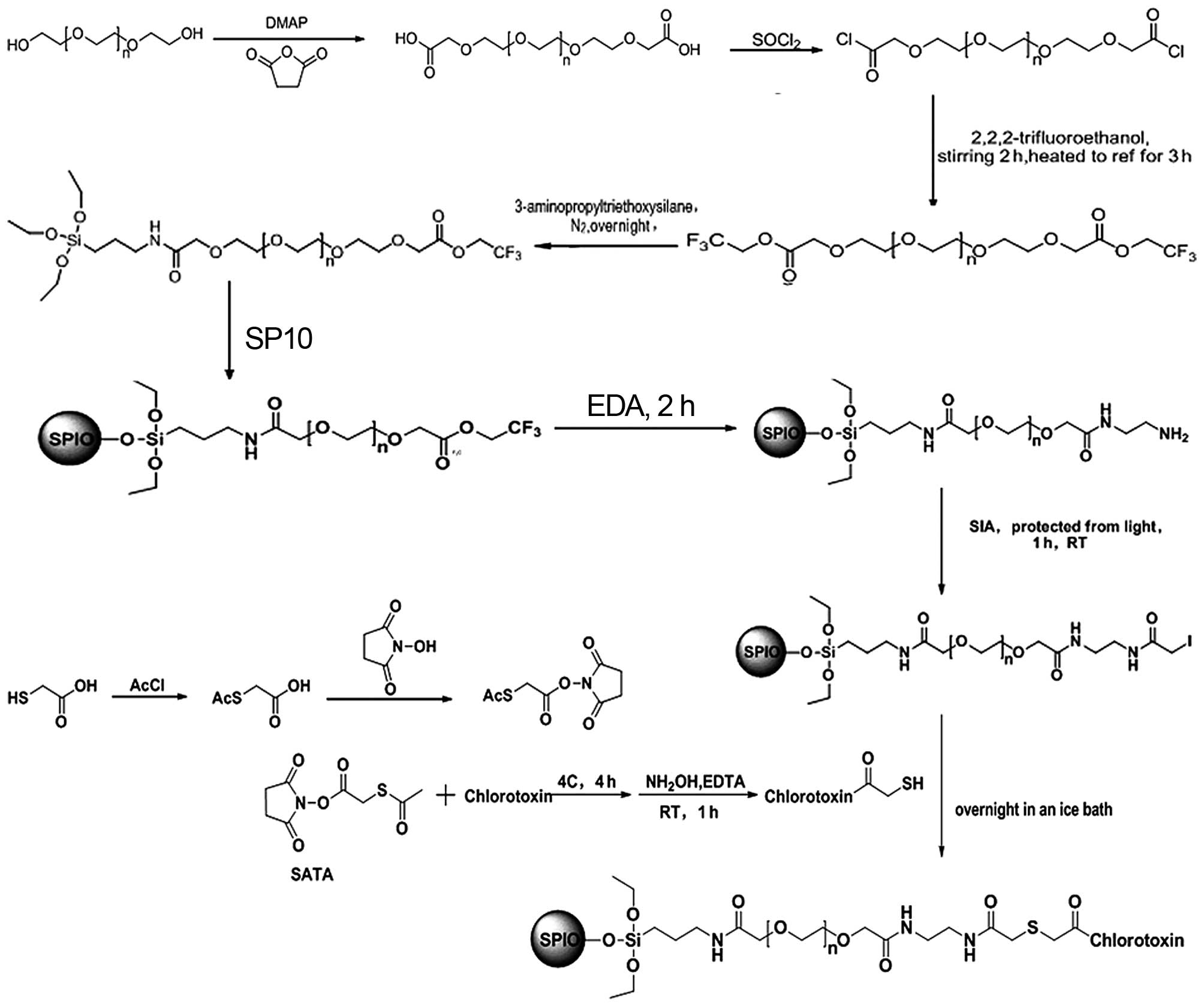
Surface modification of hydrophobic SPIO
nanoparticles
Surface modification of hydrophobic SPIO
nanoparticles was performed according to the methods of Veiseh
et al (11) and Sun et
al (12) as described below
(Fig. 1). Step 1: PEG was added to
a two-necked flask. One neck was connected to a water-separator,
which was connected with a condenser tube, and the other neck was
connected with a thermometer. Then, toluene was added to the flask
to dissolve the PEG. The toluene/water mixture was removed by
azeotroping at 110–130°C followed by cooling to room temperature to
provide the product. Step 2: Succinic anhydride, the dried PEG6000
and 4-dimethylaminopyridine (DMAP) were stirred in methylene
chloride for 24 h. Then, the white solid was precipitated after
treatment with ether. The solid was dissolved in isopropyl alcohol.
The solid byproduct was removed, and carboxyl-terminated PEG was
isolated following column chromatography and condensation. Step 3:
PEG acid chloride was prepared by treatment of the
carboxyl-terminated PEG with thionyl chloride under a nitrogen
atmosphere for 1.5 h. Step 4: Trifluoroethanol was added to the PEG
acid chloride and stirred under nitrogen for 2 h. Then, the mixture
was heated to reflux for 3 h, and the
trifluoromethyl-functionalized PEG was purified using column
chromatography. Step 5: Adenosine phosphosulfate (APS) and
trifluoromethyl-functionalized PEG in a ratio of 1:2 were added to
the solution made of PEG in dichloromethane. The solution was
stirred overnight under nitrogen, and the PEG-modified silane was
isolated following vacuum drying. Step 6: The PEG-modified silane
was added to dry SPIO dispersed in cyclohexane at 50°C under
ultrasound conditions to yield the hydrophilic SPIO modified by
PEG-silane following removal of the cyclohexane. Step 7: An excess
of ethanediamine was added to the SPIO modified by PEG-silane.
After a 2-h reaction, the aminated SPIO was isolated by
centrifugation following a wash with deionized water. Step 8: The
carboxyl-activated iodoacetic acid was prepared by stirring
iodoacetic acid, dicyclohexylcarbodiimide (DCC) and
N-hydroxysuccinimide (NHS) in ethyl acetate for 3 h. The
carboxyl-activated iodoacetic acid dissolved in dimethyl sulfoxide
(DMSO) was added to a suspension of SPIO in water. The reaction
proceeded at room temperature overnight, and the ethyl
iodoacetate-terminated SPIO was prepared following the removal of
excess iodoacetic acid by filtration through a semipermeable
membrane with a molecular weight limitation of 3,500. Step 9:
Thioglycolic acid protected by acetylated sulfhydryl was prepared
by reacting thioglycolic acid and acetyl chloride under anhydrous
conditions. Carboxy-activated N-succinimidyl-S-acetylthioacetate
(SATA) was prepared from thioglycolic acid, DCC and NHS at 0°C. The
carboxy-activated SATA was purified and then reacted with CTX
(pH=8.5 in bicarbonate buffer solution, 1 μg/μl) for
4 h to yield SATA-CTX. Purification and concentration were
performed by filtration through semipermeable membranes of a
molecular weight range of 8,000-12,000. Step 10: Hydroxylamine
hydrochloride and ethylenediaminetetraacetic acid (EDTA) was added
to SATA-CTX, which reacted at room temperature for 1 h. Then, the
acetyl group of SATA-CTX was released to expose the reactive
sulfhydryl group and the mercapto-modified CTX was formed. The
mercapto-modified CTX was purified by filtration through
semipermeable membranes with a molecular weight limitation of
3,500. The product reacted with ethyl iodoacetate-terminated SPIO
by stirring in an ice-bath overnight to form the final product. The
characterizations of the product were analyzed using infrared
spectrometer and nuclear magnetic resonance spectrometer.
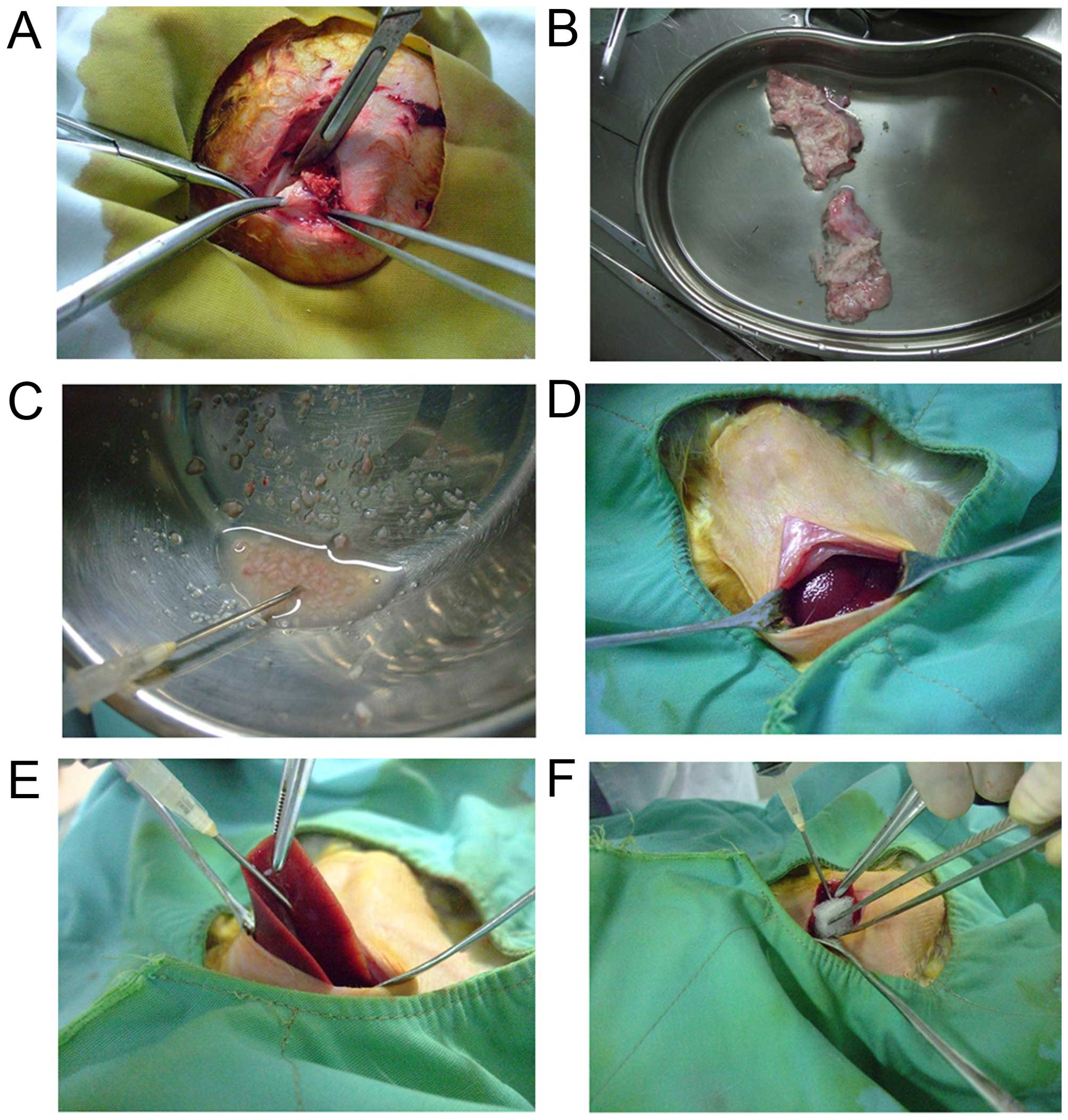
Establishment of the rabbit VX2 liver
carcinoma model
Establishment of the rabbit VX2 liver carcinoma
model was performed according to the methods of Chen et al
(13), as described below (Fig. 2). The operation was carried out
under sterile condition and anaesthesia with chloral hydrate.
Tissue at the edge of the tumor was removed from the tumor-bearing
rabbit (Fig. 2A). Necrotic tissue,
fascia and other connective tissues were removed (Fig. 2B). The remained tissue was cut into
small pieces (0.5–1 mm diameter) using scissors (Fig. 2C). A vertical incision was conducted
below the xiphoid of healthy rabbits to expose the liver (Fig. 2D). The middle lobe of the liver was
exposed using smooth forceps, and a 15-G needle was inserted
sideways and upward into the visceral surface of the liver lobe and
then 0.5-ml tumor fragments were injected with a 5 ml syringe.
During this process, we ensured that the tumor fragments were
injected into the liver parenchyma (Fig. 2E). Finally, the puncture site was
covered with gelfoam after removal of the needle, and the incision
was sutured after confirming no obvious bleeding (Fig. 2F).
MRI of SPIO and SPIO-PEG-CTX in vitro and
in vivo
The MRI of SPIO and SPIO-PEG-CTX in vitro and
in vivo were performed as follows. All scans were performed
on an MR scanner (Philips Achieva 3.0T X Series; Phillips
Healthcare, The Netherlands), using a 16-element phased array of
SENSE XL Torso coil. The imaging protocol included the following:
axial planes sense turbo spin-echo T2-weighted MRI [repetition time
(TR)/echo time (TE), 1,565/70 millisecond (msec); NSA=3; flip
angle, 90°; matrix size, 252×192; field of view (FOV), 24×24 cm;
section thickness: 4 mm, gap 0.4 mm]. Axial planes sense turbo
spin-echo T1-weighted MRI (T1WI; TR/TE, 10/2.3 msec; NSA=3, flip
angle, 15°; matrix, 252×193; FOV, 24×24 cm; section thickness: 4
mm; gap 0.4).
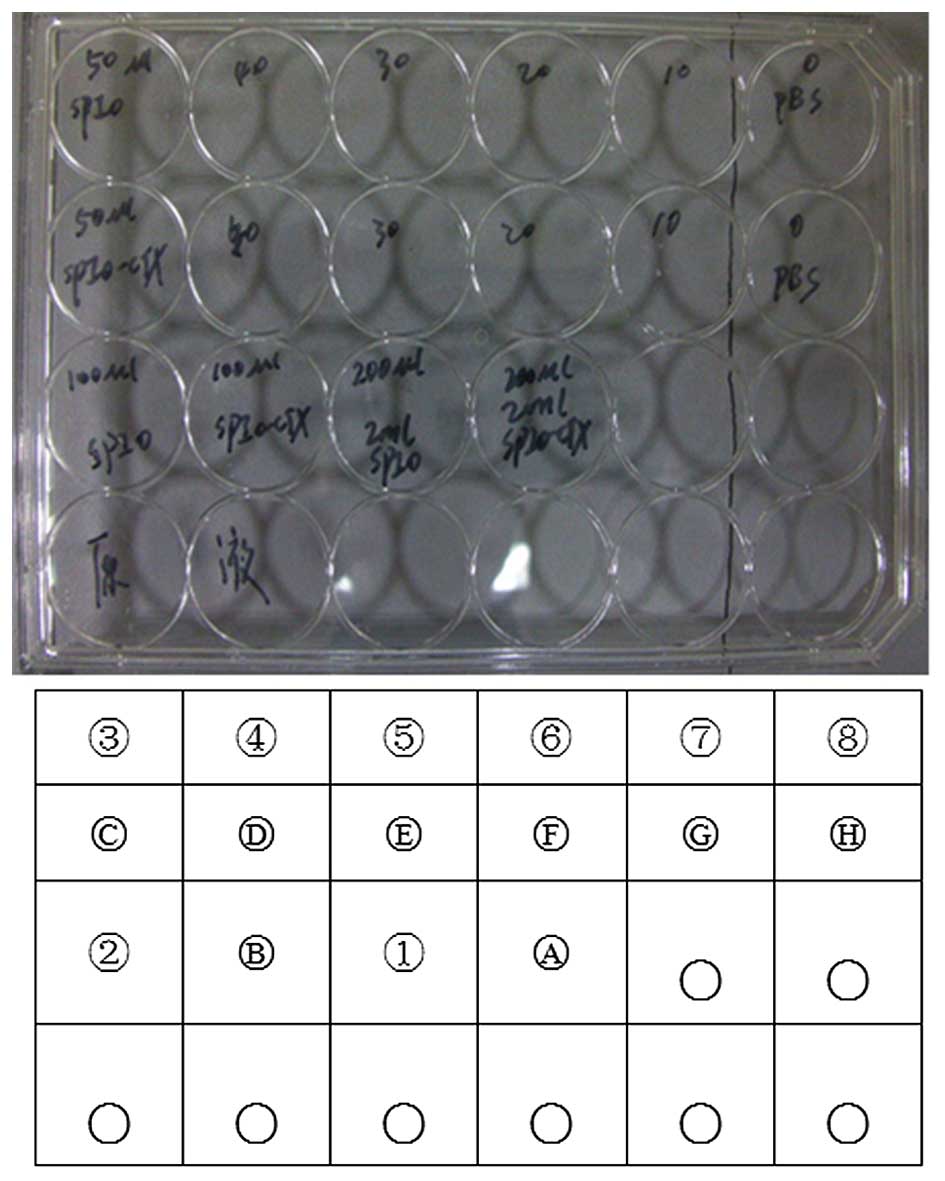
MRI scanning
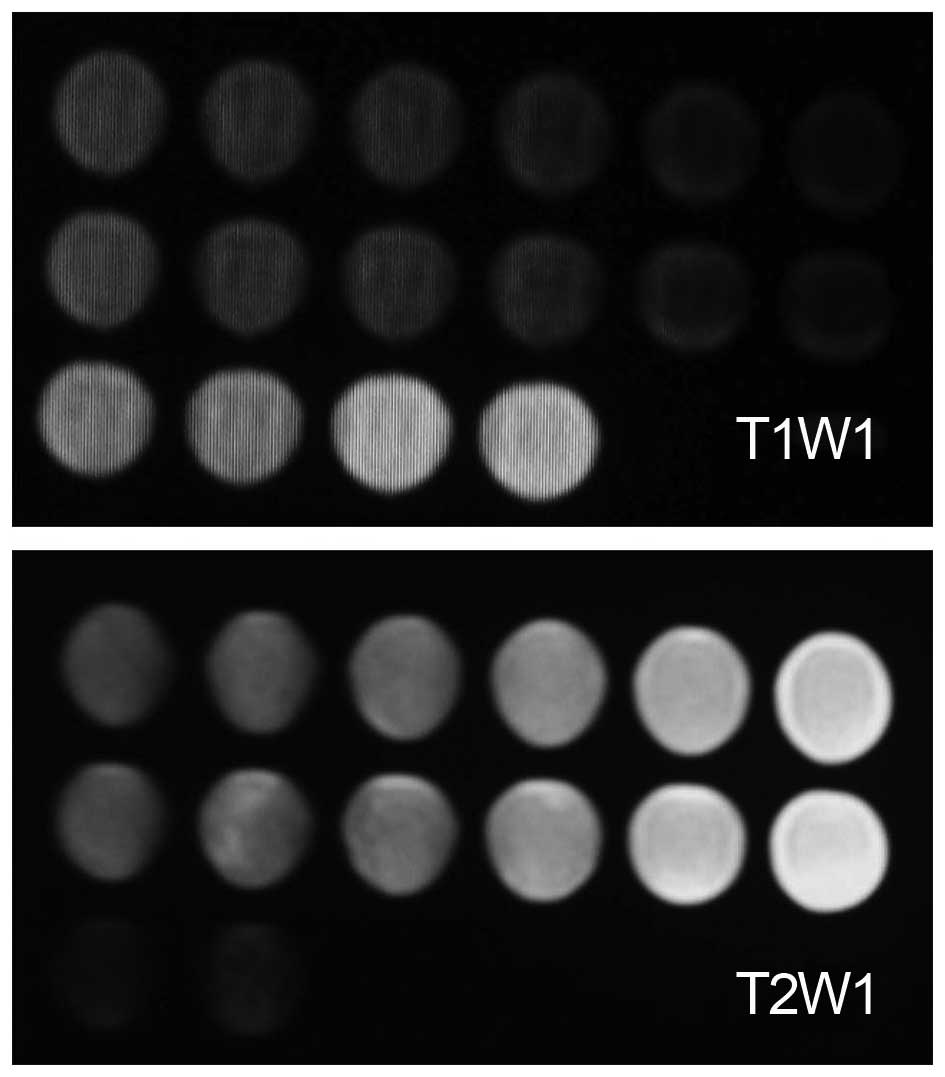
MRI scanning was performed using the SPIO and
SPIO-PEG-CTX solutions. The arrangements of the SPIO and
SPIO-PEG-CTX solutions are shown in Fig. 3. The concentrations of the SPIO and
SPIO-PEG-CTX stock solutions were both 10 mg Fe/ml. In samples no.
1-7, the solutions were prepared by adding 200, 100, 50, 40, 30, 20
and 10 μl SPIO stock solution separately and diluting to 2
ml in phosphate-buffered saline (PBS). PBS was used in sample no.
8. In the samples A-G the solutions were prepared by adding 200,
100, 50, 40, 30, 20 and 10 μl SPIO-PEG-CTX stock solution
and diluting to 2 ml with PBS. PBS was used in sample H. The
concentrations of samples no. 1-8 and A-H were: 1, 0.5, 0.25, 0.2,
0.15, 0.1, 0.05 and 0 mg Fe/ml.
MRI scanning of all 8 living rabbits was performed
before and after the injection of the SPIO-PEG-CTX solution.
Contrast enhanced T2 weighed images of the VX2 rabbits were
acquired 30 min after intravenous bolus injection of 5 ml
SPIO-PEG-CTX at 25 μg/ml.
The MR images were sent to a dedicated workstation
and analyzed by 3 experienced radiologists. The region of interest
(ROI) was 5 × 5 mm for the SPIO and SPIO-PEG-CTX solution or rabbit
liver tumor. Partial volume effect and pixels on the margin were
not taken into account.
The liver tumors were removed and fixed in formalin
after MRI scanning, and the sections were prepared for hematoxylin
and eosin (H&E) staining. The morphology and structure of the
liver tumors were observed to determine the malignancy.
Data are presented as the mean ± standard deviation
and were analyzed using the paired t-test bySPSS 17.0 software. A
difference with a P-value of <0.05 was considered to indicate a
statistically significant result.
Results
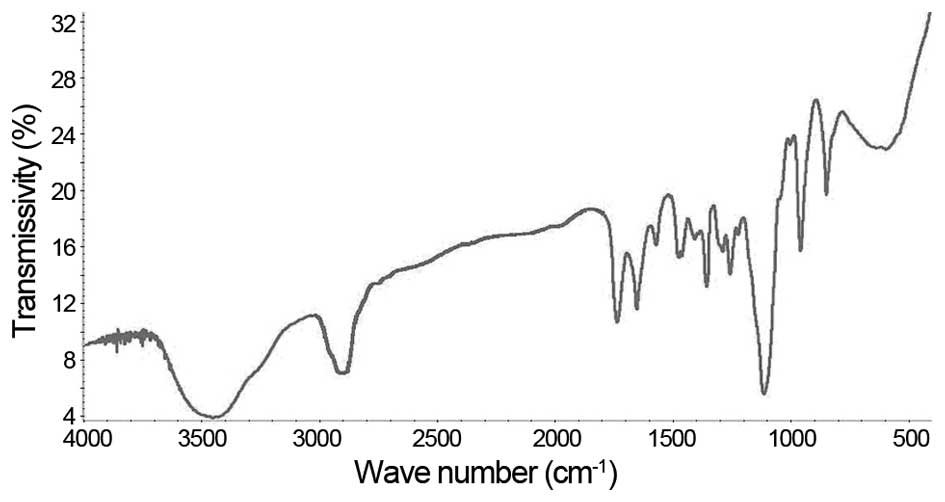
Characterizations of the product
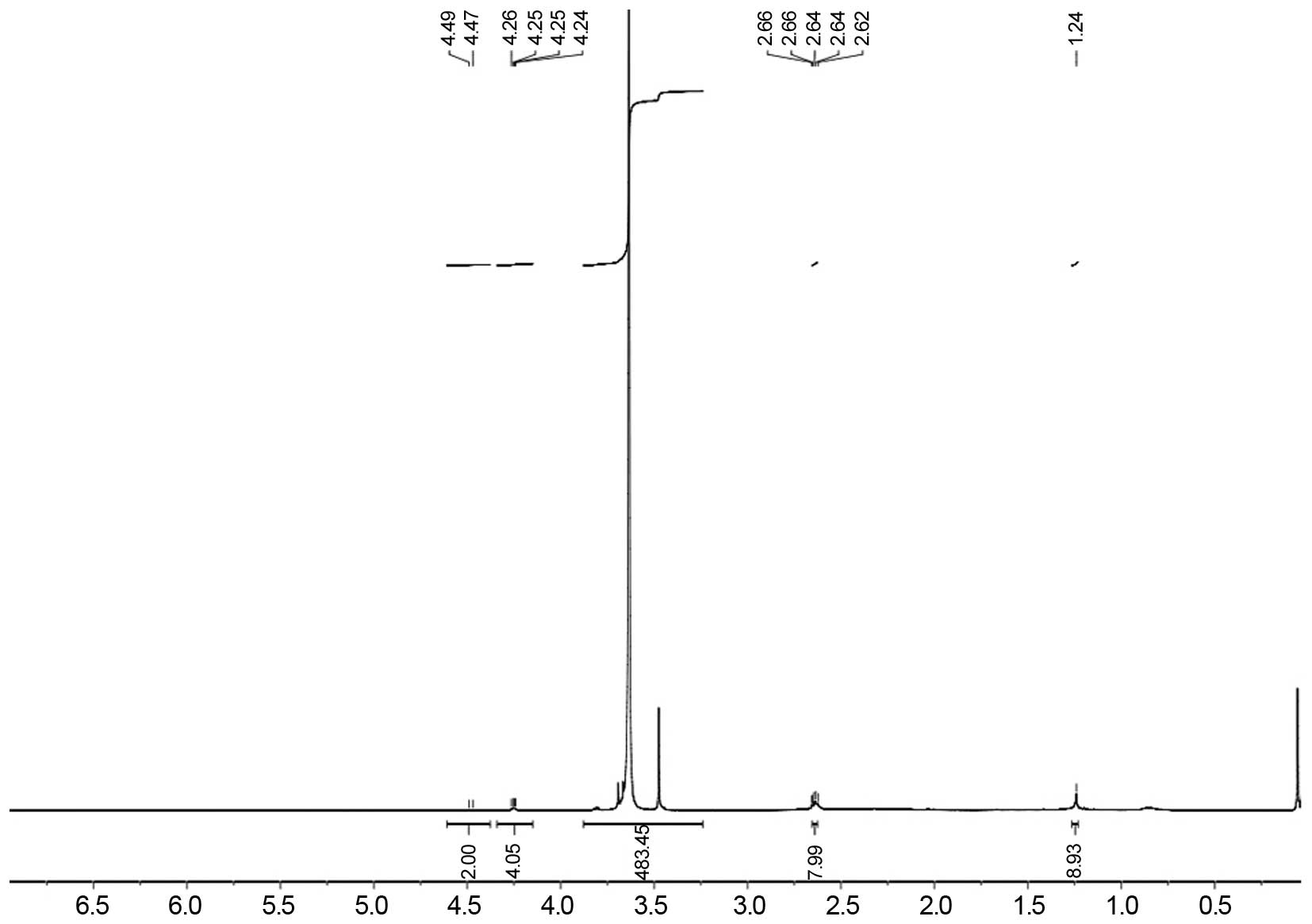
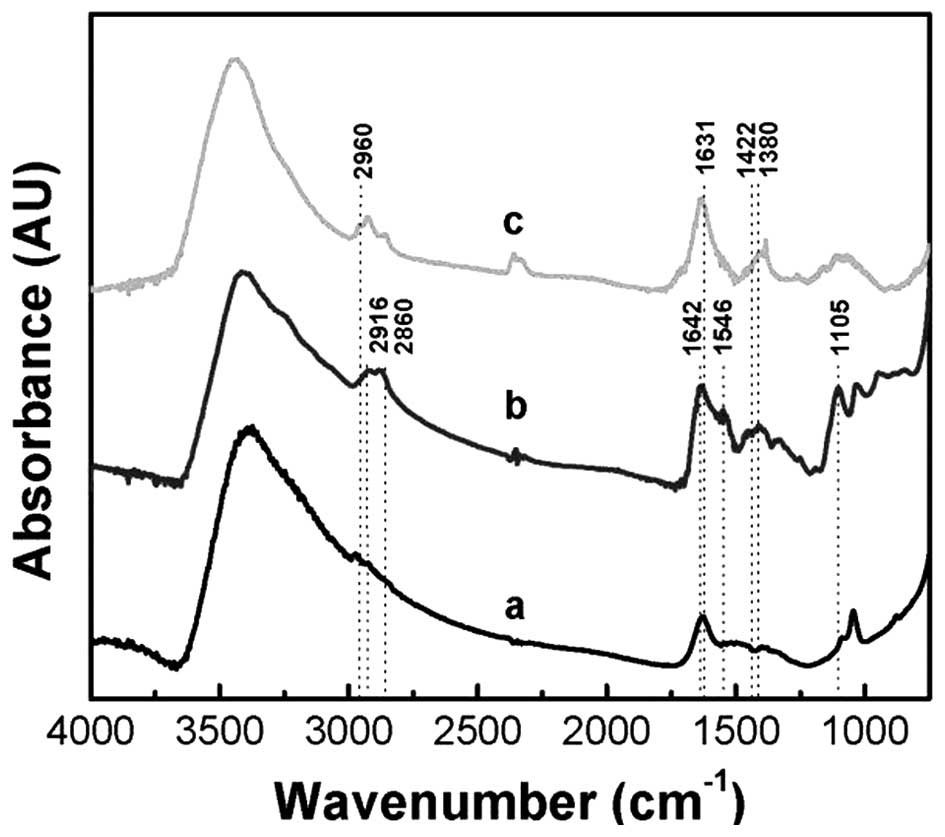
The infrared spectrum of the carboxyl-terminated PEG
is shown in Fig. 4. The 3,000
cm−1 broad peak and 1,700 cm−1 double peak
verified the success of the carboxyl modification. Nuclear magnetic
resonance spectroscopy of PEG-modified silane is shown in Fig. 5. The infrared spectrums of
Fe3O4,
Fe3O4-PEG-NH2 and
Fe3O4-PEG-CTX are shown in Fig. 6.
The MRI results of SPIO and SPIO-PEG-CTX
in vitro
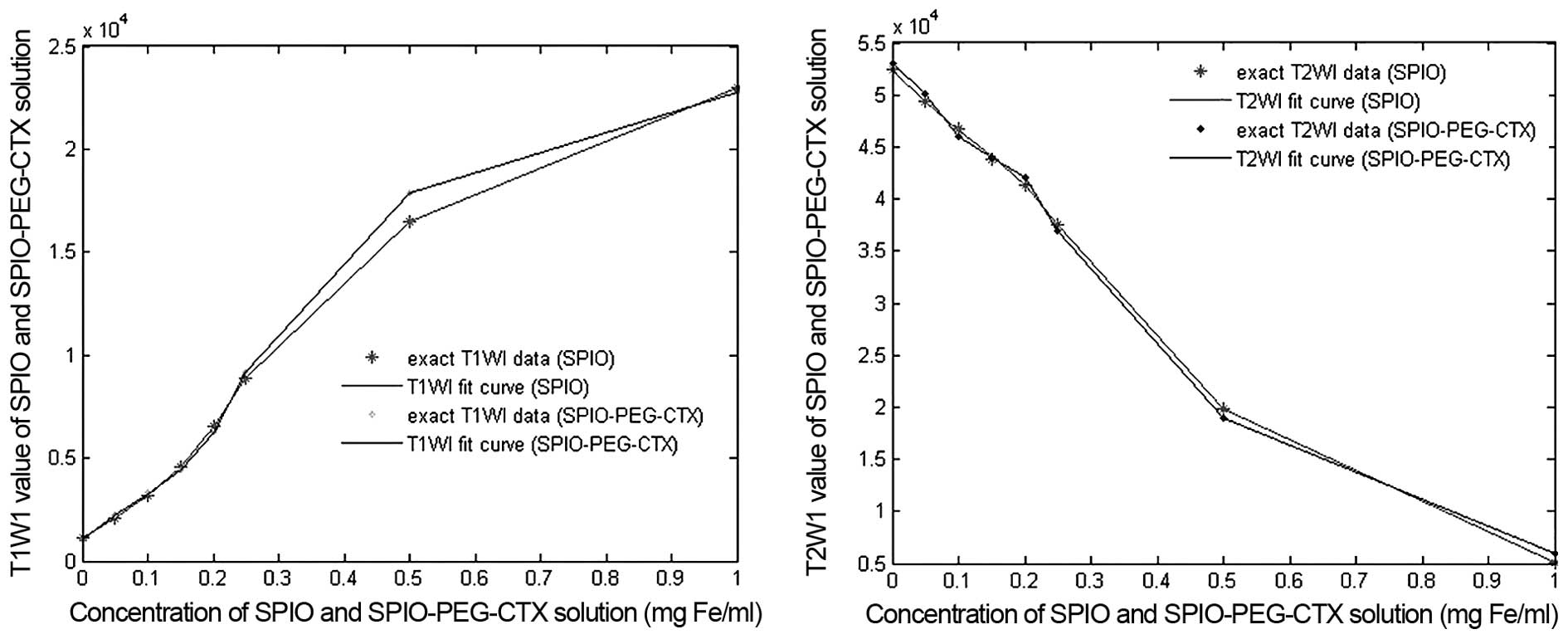
The MRI signal values of the SPIO and SPIO-PEG-CTX
solutions are shown in Table I. The
calibration curves of the concentrations and MRI signal values of
the SPIO and SPIO-PEG-CTX solutions are shown in Fig. 7. There was a linear relationship
between the concentrations and MRI values of the SPIO and
SPIO-PEG-CTX solutions. With increasing SPIO and SPIO-PEG-CTX
concentrations, the T1WI value increased, and the T2WI values
gradually decreased. The MRI value variations of the two solutions
were basically identical. The MR images of the SPIO and
SPIO-PEG-CTX solutions are shown in Fig. 8.
 | Table IMRI signal values of the SPIO and
SPIO-PEG-CTX solutions. |
Table I
MRI signal values of the SPIO and
SPIO-PEG-CTX solutions.
| No. of holes | 1/A | 2/B | 3/C | 4/D | 5/E | 6/F | 7/G | 8/H |
|---|
| Concentration of
SPIO-PEG-CTX and SPIO (mg Fe/ml) | 1 | 0.5 | 0.25 | 0.2 | 0.15 | 0.1 | 0.05 | 0 |
| T1WI value of
SPIO | 23,012 | 16,484 | 8,876 | 6,572 | 4,539 | 3,210 | 2,055 | 1,105 |
| T1WI value of
SPIO-PEG-CTX | 22,800 | 17,896 | 9,138 | 6,256 | 4,398 | 3,299 | 2,199 | 1,030 |
| T2WI value of
SPIO | 5,124 | 19,840 | 37,550 | 41,368 | 43,877 | 46,734 | 49,372 | 52,370 |
| T2WI value of
SPIO-PEG-CTX | 5,967 | 19,034 | 36,898 | 42,054 | 43,976 | 45,987 | 50,134 | 53,098 |
The MRI results of SPIO-PEG-CTX in
vivo
Thirteen hepatic tumors were dissected from 8
rabbits. The MRI values of the tumors and the adjacent normal
hepatic tissues on T2WI are shown in Table II. STumor-0 and SNormal-0,
respectively, indicate the T2 signal value of the hepatic tumor and
the normal adjacent hepatic tissue before injection of the
SPIO-PEG-CTX solution. STumor-1 and SNormal-1, respectively,
indicate the T2 signal value of the hepatic tumor and the adjacent
normal hepatic tissue after injection of the SPIO-PEG-CTX solution.
The data in Table II were analyzed
by paired samples t-test using SPSS 17.0 software to evaluate
differences between STumor-0 and STumor-1,
SNormal-0 and SNormal-1. A P<0.05 was
considered to indicate a significant difference. The T2 signal
values of VX2 liver tumors and adjacent normal hepatic tissue
before and after injection of the SPIO-PEG-CTX solution are shown
in Table III. The MR images of a
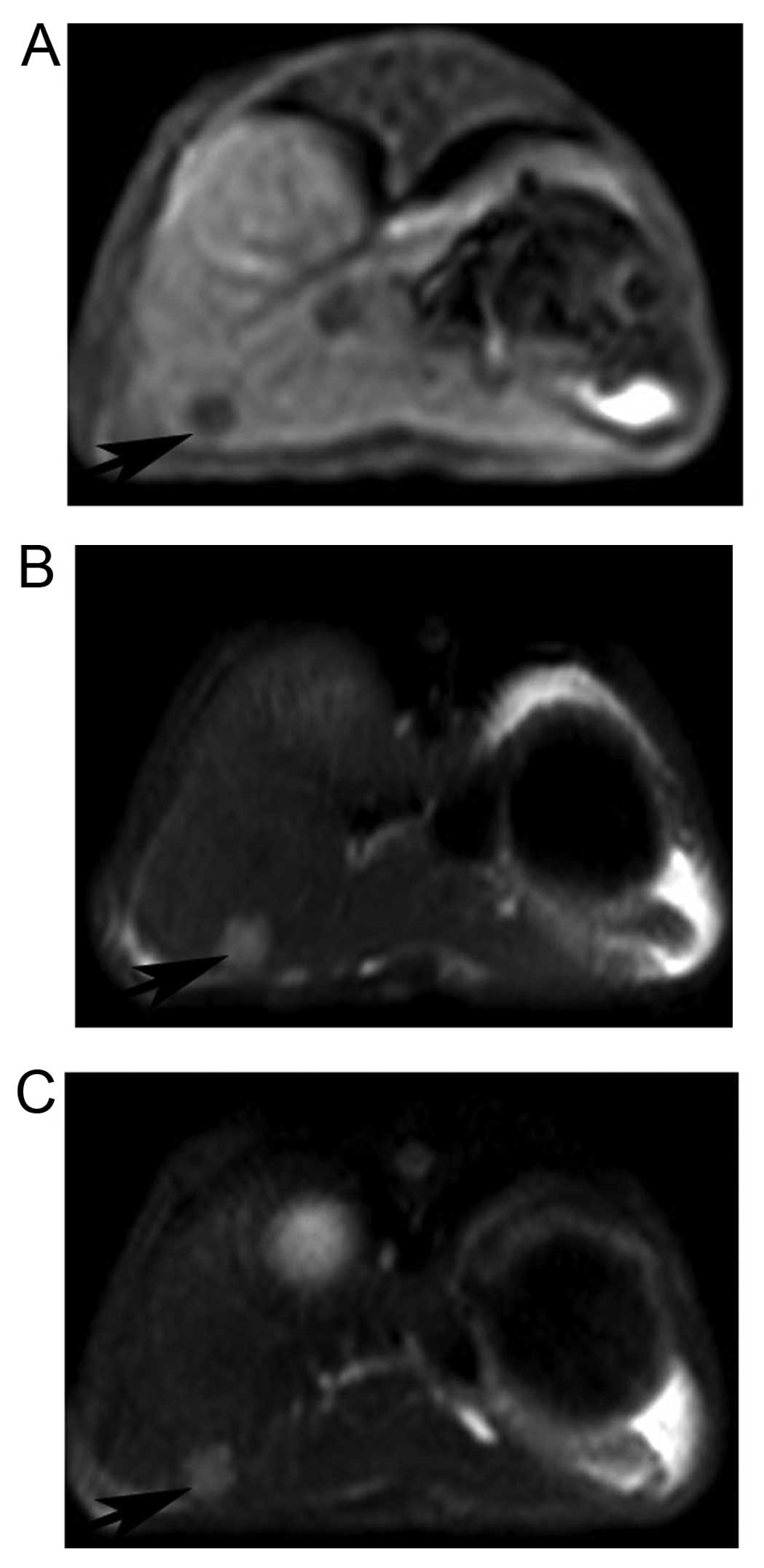
rabbit are shown in Fig. 9.
Fig. 9A is the T1WI image. Fig. 9B is the plan-scanning T2WI image.
Fig. 9C is the enhanced-scanning
T2WI image. The VX2 liver tumor is indicated by an arrow. The tumor
demonstrated hypointensity on plan-scanning T2WI, hyperintensity on
T2WI, and the T2 signal intensity increased on enhanced-scanning
T2WI.
 | Table IIThe MRI values of tumors and adjacent
normal hepatic tissue on T2WI. |
Table II
The MRI values of tumors and adjacent
normal hepatic tissue on T2WI.
| No. |
STumor-0 |
STumor-1 |
SNormal-0 |
SNormal-1 |
|---|
| 1 | 1,226 | 1,096.3 | 585.9 | 441.1 |
| 2 | 1,231 | 1,012.7 | 580.7 | 394.3 |
| 3 | 1,221 | 964.1 | 591.2 | 333.3 |
| 4 | 951.2 | 1,025.4 | 584.3 | 396.2 |
| 5 | 943.1 | 679.8 | 583.2 | 331.5 |
| 6 | 1,367.9 | 1,083.1 | 477.2 | 527.3 |
| 7 | 1,363.4 | 1,164.9 | 474.9 | 772.4 |
| 8 | 1,333.2 | 1,195.8 | 475.6 | 527.3 |
| 9 | 1,335.7 | 1,366.5 | 473.1 | 770.1 |
| 10 | 1,453.4 | 1,427.3 | 650.3 | 460.7 |
| 11 | 1,449.7 | 1,305.2 | 645.9 | 407 |
| 12 | 1,450.9 | 771.7 | 648.5 | 237.1 |
| 13 | 2,175.3 | 2,004.3 | 552.9 | 650.1 |
 | Table IIIThe T2 signal values of VX2 liver
tumors and adjacent normal hepatic tissue before and after
injection of SPIO-PEG-CTX solution. |
Table III
The T2 signal values of VX2 liver
tumors and adjacent normal hepatic tissue before and after
injection of SPIO-PEG-CTX solution.
| S0 | S1 | P-value |
|---|
| Tumors | 1,346±300.5 | 1,161±331.5 | 0.004 |
| Adjacent normal
hepatic tissues | 563.4±67.8 | 480.6±165.1 | 0.202 |
The mean T2 value of the 13 VX2 tumors from 8
rabbits before injection of the SPIO-PEG-CTX solution was
1,346±300.5, and the mean value after injection was 1,161±331.5.
Thus, the enhanced-scanning T2 value was smaller than the
plan-scanning (P=0.004<0.05). The mean T2 values of the normal
hepatic tissues near the 13 tumors before and after injection of
SPIO-PEG-CTX were 563.4±67.8 and 480.6±165.1, respectively
(P=0.202>0.05). Thus the T2 value of the normal hepatic tissue
had no obvious change after injection of SPIO-PEG-CTX.
The histological findings as shown in
Fig. 10
Fig. 10A shows the
MR image of VX2 liver carcinoma on T1WI before the injection of
SPIO-PEG-CTX (indicated by an arrow). The carcinoma was in the
front of the liver and demonstrated hypointensity. Fig. 10B shows general sample observation
of the VX2 liver carcinoma (indicated by an arrow). There was a
circumscribed whitish nodule at the edge of the liver. Fig. 10C is the pathological image of
H&E staining at a magnification, x100; and Fig. 10D is the pathological image of
H&E staining at a magnification, ×400. The tumor cells were
morphologically diverse, with obviously heterogeneous and
trachychromatic nuclei; karyokinesis was also observed (indicated
by an arrow in Fig. 10D).
Discussion
Hepatocarcinoma is able to be detected by MRI in the
clinical. However, there are some difficulties in the detection of
small lesions, particularly in patients with liver lesions smaller
than 1 cm or liver cancer accompanied by liver cirrhosis (3). The development of molecular imaging
provides a new way for the early diagnosis of hepatocarcinoma. SPIO
has a broad application in the biomedical field, and currently has
become a hot spot in the field of molecular imaging research
(7,8).
Compared to gadolinium, SPIO can heighten the proton
relaxation rate and shorten the T2 relaxation time. The
reticuloendothelial system contains Kupffer cells, which can uptake
SPIO and decrease the signal intensity of the liver. Since there
are few or no Kupffer cells in the majority of malignant tumors of
the liver, the signal intensity of malignant tumors remains
unchanged when the liver takes up SPIO. In this case, the contrast
in T2WI between the lesion and liver increases, which leads to
negative enhancement (6).
The main ingredients of SPIO are
Fe3O4 and some γ-Fe2O3
(14). Fe3O4
is black and strongly ferromagnetic, while
γ-Fe2O3 is brown and has strong magnetic
permeability. There are many methods by which to prepare magnetic
nanoparticles, such as mechanical ball mill, coprecipitation,
emulsification, sol-gel method, liquid-phase microwave dielectric
heating, vapor deposition and hydrothermal method (15,16).
Chemical coprecipitation is the most common method, which is simple
and inexpensive. Thus, stable and uniform SPIO was prepared using
this method in the present study.
Previous studies have demonstrated that matrix
metal-loproteinase-2 (MMP-2) is expressed weakly in the liver
tissues of chronic hepatitis and liver cirrhosis, but strongly in
hepatocellular carcinoma (17,18).
The expression of MMP-2 is related to the differentiation,
invasion, ability to metastasize and tendency of the tumor to recur
in liver cancer (19). Thus, MMP-2
may be a new target that can be combined with a new molecular probe
of hepatocarcinoma. CTX is a 36-amino acid peptide containing 1
tyrosine residue, 8 cysteine residues and 4 disulfide bonds. It is
purified from the venom of the giant Israeli scorpion (Leiurus
quinquestriatus). CTX can combine with MMP-2 selectively and
specifically (20), which is
strongly expressed in hepatocellular carcinomas. PEG is a cheap and
commonly used surface-modification agent with good hydrophilicity
and biocompatibility, but without immunogenicity and toxicity
(21–24). It is soluble in water and many types
of organic solvents and can be bound to nanoparticles by blocking
or grafting. The nanoparticles modified with different functional
groups display hydrophilicity and stability, can prolong the blood
circulation time and can reduce phago-cytosis. Therefore, we
combined PEG as medium with SPIO and CTX to prepare SPIO-PEG-CTX
nanoparticles. These nanoparticles can target hepatocellular
carcinoma through the combination of CTX and MMP-2.
There are many dangling bonds on the surface of SPIO
nanoparticles, which can be modified by targeted molecular probes
with different functional groups such as carboxyl or amino groups
or monoclonal antibodies. This type of modification can make
magnetic nanoparticles reach the targeted organization and then
amplify an imaging signal and improve image quality, effectively
(25,26). Surface modification is defined as
changing the physicochemical properties of particles such as
surface chemical structure, reaction characteristics, surface
hydrophobicity, or surface chemical adsorption by physical or
chemical methods. The unmodified nanoparticles have large specific
surface area, surface hydrophobicity and static electricity. They
can bring about precipitation and combine with plasma protein
easily and then be cleared by the reticuloendothelial system in
vivo, which may affect biomedical application of the particles.
Therefore, SPIO was modified using ligand exchange in the present
study. Whether the magnetic performance of SPIO could change after
modification was investigated. In the present study, MRI signals of
the SPIO and SPIO-PEG-CTX solutions had the same variations in
vitro. These results suggest that SPIO-PEG-CTX can be used as a
negative MRI contrast agent in T2WI sequence similar to SPIO.
The reticuloendothelial system contains Kupffer
cells, which can uptake SPIO and decrease T2 signal intensity of
the liver, while liver tumors do not uptake SPIO for the lack of
Kupffer cells. In the present study, MR images of VX2
hepatocarcinoma rabbits injected with the SPIO-PEG-CTX (contrast)
agent indicated an uptake of SPIO-CTX in the liver tumors which
induced a decrease in the T2 signal intensity which was not
observed in healthy regions of the liver. This suggests that CTX
can alter the targeting of SPIO, and SPIO-PEG-CTX was taken up by
the liver tumors, but not by the normal liver tissue. Thus, the
SPIO-PEG-CTX nanoparticles have potential for use in the early
diagnosis of hepatocellular carcinoma. However, there were some
limitations to the present study. The concentration of SPIO-PEG-CTX
was not changed as an MR agent, and the time of enhanced-scanning
was invariable. Thus, further investigation is warranted.
Acknowledgments
The present study was supported by the Natural
Science Foundation of Hunan Province, China (no. 14JJ2034), the
Natural Science Foundation of China (no. 81571784), the Foundation
of Hunan Province and Technology Department, China (no.
2015SF2020-4), the Industry Research and Development Projects of
the Development and Reform Commission of Hunan Province, China (no.
2060403-30499).
References
|
1
|
Kudo M: Hepatocellular carcinoma 2009 and
beyond: From the surveillance to molecular targeted therapy.
Oncology. 75(Suppl 1): S1–S12. 2008. View Article : Google Scholar
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Obuz F, Oksüzler M, Seçil M, Sağol O,
Karademir S and Astarcioğlu H: Efficiency of MR imaging in the
detection of malignant liver lesions. Diagn Interv Radiol.
12:17–21. 2006.PubMed/NCBI
|
|
4
|
Bowman K and Leong KW: Chitosan
nanoparticles for oral drug and gene delivery. Int J Nanomedicine.
1:117–128. 2006. View Article : Google Scholar
|
|
5
|
Cheng FY, Su CH, Yang YS, Yeh CS, Tsai CY,
Wu CL, Wu MT and Shieh DB: Characterization of aqueous dispersions
of Fe3O4 nanoparticles and their biomedical
applications. Biomaterials. 26:729–738. 2005. View Article : Google Scholar
|
|
6
|
Le Renard PE, Lortz R, Senatore C, Rapin
JP, Buchegger F, Petri-Fink A, Hofmann H, Doelker E and Jordan O:
Magnetic and in vitro heating properties of implants formed in situ
from injectable formulations and containing superparamagnetic iron
oxide nanoparticles (SPIONs) embedded in silica microparticles for
magnetically induced local hyperthermia. J Magn Magn Mater.
323:1054–1063. 2011. View Article : Google Scholar
|
|
7
|
Rosen JE, Chan L, Shieh DB and Gu FX: Iron
oxide nanoparticles for targeted cancer imaging and diagnostics.
Nanomedicine. 8:275–290. 2012.
|
|
8
|
Tassa C, Shaw SY and Weissleder R:
Dextran-coated iron oxide nanoparticles: A versatile platform for
targeted molecular imaging, molecular diagnostics, and therapy. Acc
Chem Res. 44:842–852. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nishie A, Tajima T, Ishigami K, Ushijima
Y, Okamoto D, Hirakawa M, Nishihara Y, Taketomi A, Hatakenaka M,
Irie H, et al: Detection of hepatocellular carcinoma (HCC) using
super paramagnetic iron oxide (SPIO)-enhanced MRI: Added value of
diffusion-weighted imaging (DWI). J Magn Reson Imaging. 31:373–382.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tanimoto A and Kuribayashi S: Application
of superparamagnetic iron oxide to imaging of hepatocellular
carcinoma. Eur J Radiol. 58:200–216. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Veiseh O, Sun C, Gunn J, Kohler N,
Gabikian P, Lee D, Bhattarai N, Ellenbogen R, Sze R, Hallahan A, et
al: Optical and MRI multifunctional nanoprobe for targeting
gliomas. Nano Lett. 5:1003–1008. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sun C, Veiseh O, Gunn J, Fang C, Hansen S,
Lee D, Sze R, Ellenbogen RG, Olson J and Zhang M: In vivo MRI
detection of gliomas by chlorotoxin-conjugated superparamagnetic
nano-probes. Small. 4:372–379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen Z, Kang Z, Xiao EH, Tong M, Xiao YD
and Li HB: Comparison of two different laparotomy methods for
modeling rabbit VX2 hepatocarcinoma. World J Gastroenterol.
21:4875–4882. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gupta AK and Gupta M: Cytotoxicity
suppression and cellular uptake enhancement of surface modified
magnetic nanoparticles. Biomaterials. 26:1565–1573. 2005.
View Article : Google Scholar
|
|
15
|
Laurent S, Forge D, Port M, Roch A, Robic
C, Vander Elst L and Muller RN: Magnetic iron oxide nanoparticles:
Synthesis, stabilization, vectorization, physicochemical
characterizations, and biological applications. Chem Rev.
108:2064–2110. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hyeon T: Chemical synthesis of magnetic
nanoparticles. Chem Commun. 21:927–934. 2003. View Article : Google Scholar
|
|
17
|
Lichtinghagen R, Helmbrecht T, Arndt B and
Böker KH: Expression pattern of matrix metalloproteinases in human
liver. Eur J Clin Chem Clin Biochem. 33:65–71. 1995.PubMed/NCBI
|
|
18
|
Jacob A, Jing J, Lee J, Schedin P, Gilbert
SM, Peden AA, Junutula JR and Prekeris R: Rab40b regulates
trafficking of MMP2 and MMP9 during invadopodia formation and
invasion of breast cancer cells. J Cell Sci. 126:4647–4658. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wong JC, Chan SK, Schaeffer DF, Sagaert X,
Lim HJ, Kennecke H, Owen DA, Suh KW, Kim YB and Tai IT: Absence of
MMP2 expression correlates with poor clinical outcomes in rectal
cancer, and is distinct from MMP1-related outcomes in colon cancer.
Clin Cancer Res. 17:4167–4176. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Deshane J, Garner CC and Sontheimer H:
Chlorotoxin inhibits glioma cell invasion via matrix
metalloproteinase-2. J Biol Chem. 278:4135–4144. 2003. View Article : Google Scholar
|
|
21
|
Gryparis EC, Hatziapostolou M,
Papadimitriou E and Avgoustakis K: Anticancer activity of
cisplatin-loaded PLGA-mPEG nanoparticles on LNCaP prostate cancer
cells. Eur J Pharm Biopharm. 67:1–8. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gref R, Minamitake Y, Peracchia MT,
Trubetskoy V, Torchilin V and Langer R: Biodegradable
long-circulating polymeric nano-spheres. Science. 263:1600–1603.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Moghimi SM and Szebeni J: Stealth
liposomes and long circulating nanoparticles: Critical issues in
pharmacokinetics, opsonization and protein-binding properties. Prog
Lipid Res. 42:463–478. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gref R, Lück M, Quellec P, Marchand M,
Dellacherie E, Harnisch S, Blunk T and Müller RH: 'Stealth'
corona-core nanoparticles surface modified by polyethylene glycol
(PEG): Influences of the corona (PEG chain length and surface
density) and of the core composition on phagocytic uptake and
plasma protein adsorption. Colloids Surf B Biointerfaces.
18:301–313. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Juang JH, Wang JJ, Shen CR, Kuo CH, Chien
YW, Kuo HY, Tsai ZT and Yen TC: Magnetic resonance imaging of
transplanted mouse islets labeled with chitosan-coated
superparamagnetic iron oxide nanoparticles. Transplant Proc.
42:2104–2108. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ahmad T, Bae H, Rhee I, Chang Y, Lee J and
Hong S: Particle size dependence of relaxivity for silica-coated
iron oxide nanoparticles. Curr Appl Phys. 12:969–974. 2012.
View Article : Google Scholar
|