Introduction
Glioma is a malignant brain tumor associated with
poor prognosis and a median survival period of only 12–15 months
(1,2). Unfortunately, gliomas can be resistant
to irradiation and chemotherapy, and surgical resection is
sometimes difficult. Thus, more effective treatment strategies are
required to manage this malignancy and improve the survival rate of
patients.
It is well known that ataxia-telangiectasia mutated
(ATM) is a proximal component of DNA damage-induced cell cycle
checkpoint pathways (3–5). It is believed that the ATM gene plays
a role in blocking the cell cycle in order to protect cells from
damage caused by irradiation and provide enough time for
self-repair (2,6,7). Many
laboratories have verified that overexpression of the ATM gene in
gliomas is linked with the radioresistance of these tumors
(1,8–10).
Therefore, strategies that suppress ATM gene expression may improve
the radio-sensitivity of malignant gliomas. At present,
pharmacological and genetic methods are used to repress the
expression of ATM. For example, Guha et al (11) found that attenuated ATM protein
expression via antisense-ATM could increase radiosensitivity in U87
cells. Chuah et al (12)
employed and compared three different viral vectors (retrovirus,
adenovirus, and lentivirus) to deliver the siRNA-ATM plasmid, and
found that radiosensitivity of the glioma cell line was obviously
enhanced after suppression of ATM expression. Furthermore, they
reported that the lentivirus system was the most efficient with
regard to transfection and suppression of the ATM gene. Nadkarni
et al (13) reported that
after inhibition of the ATM kinase KU55933 in glioma cells,
expression levels of the genes related to radiosensitization (ATM
and p53) and the cell cycle (p21) were significantly decreased, and
proliferation of cells in the G2 phase was blocked. In recent
years, KU60019, a new ATM kinase inhibitor, was found to have good
potential with regard to increase in tumor cell apoptosis and
repression of tumor growth in gliomas (1,7).
However, the optimal dose and mode of administration of ATM kinase
inhibitors are not clear (7).
Moreover, inhibitors are usually short acting and therefore cannot
permanently and stably repress ATM gene expression. Therefore,
there is a need for more effective inhibitors and gene interference
strategies that can ensure long-term stable ATM silencing.
To date, few studies have been conducted on the
radiosensitivity of glioma cells after ATM gene interference or
silencing. Some scholars have reported that siRNA against ATM could
improve the effect of radiotherapy in glioma cell lines (11,12).
These were in vitro studies conducted on different cell
lines and under different experimental conditions, thus the siRNA
strategy needs to be explored under in vivo conditions.
In our study, we induced silencing of the ATM gene
using the siRNA technique and then explored its effect on the in
vivo and in vitro radiosensitivity of gliomas. To the
best of our knowledge, there is less research on in vivo
silencing of the ATM gene. We therefore believe that the
contributions of this study will be extremely valuable with regard
to establishing treatment strategies for this tumor.
Materials and methods
Cell line and culture
The human glioma cell line U251 was used; it was
gifted by the Central Laboratory of the Oncology Department of
Xinqiao Hospital of the Third Military Medical University. The cell
line was cultured in RPMI-1640 medium supplemented with 10% fetal
calf serum (FCS) (both from Gibco, Grand Island, NY, USA), 100 U/ml
penicillin, 100 µg/ml streptomycin, 2 mM glutamine, and 1 mM
sodium pyruvate. The cells were cultured in humidified incubators
at 37°C in an atmosphere containing 5% CO2. The cells
were maintained as a monolayer by serial passaging after
trypsinization with 0.1% trypsin (Gibco).
Animals
Four-week-old male Balb/c-nu/nu mice weighing 20–23
g were purchased from the Shanghai Experimental Animal Center of
the Chinese Academy of Medical Sciences, China. They were kept in
cages and supplied with food and water ad libitum in a
pathogen-free environment at a temperature of 25–27°C and humidity
of 45–50%. All the animals received humane care according to the
institutional policies on Human Care and Use of Laboratory Animals
and with the approval of the Ethics Committee of Chongqing Cancer
Institute.
Cell transfection and in vitro radiation
treatment
The cell line was seeded at a density of
2×105 cells/well in 6-well plates and cultured
overnight. After 48 h of incubation, 40 µl (MOI=2) of
siRNA-ATMPuro or siRNA-HKPuro lentivirus
(Hanheng Bio Co., Ltd., Shanghai, China) was added to the wells
when the cells had reached a confluency of 30–40%. Then, serum-free
medium was added to 6-well plates for 24 h of co-culture. The
efficiency of transfection into tumor cells was observed under an
inverted fluorescence microscope, and resistant target cells were
selected by treatment with puromycin until a stable cell line
transfected with the lentivirus was successfully established.
Three groups were created for the in vitro
experiments: the blank control group C (U251 cells were not
transfected with siRNA), the negative control group N (U251 cells
were transfected with siRNA-HKPuro), and the
experimental group A (U251 cells were transfected with
siRNA-ATMPuro). The cells from the three groups were
irradiated using a 6-MV X Rad source (SN4474, Varian) to deliver
doses of 2, 4, 5, 6 and 8 Gy. The dose rate was 300 cGy/min. The
cells were harvested after irradiation for different time periods:
cells for RT-qPCR and western blotting were harvested 24 h after
irradiation; cells for the comet assay were harvested after 4 h;
and cells for flow cytometric analysis were harvested after 24
h.
Animal model and in vivo radiation
treatment
U251 cells transfected with siRNA-ATMPuro
or siRNA-HKPuro were collected at the log phase and
injected into each side of the same mouse's haunch. Two weeks
later, the tumor reached a volume of 2.0×1.8×1.0 cm, which
indicated that the model was successfully established.
The mice from each group (siRNA-ATMPuro
and siRNA-HKPuro) were divided into two subgroups of
three animals each after subcutaneous implantation: the irradiation
group and the radiation-free group. The model mice from the two
radiation subgroups (n=6) were administered ketamine (10 ml/kg) and
fixed in the ventricumbent position. The subcutaneous tumor was
thereafter irradiated locally with ionizing radiation under a 6-MV
linear accelerator. The parameters for radiotherapy were as
follows: target range, 100 cm; dose rate, 300 MU/min; total dose
(TD), 1,500 cGy. Changes in tumor volume were examined within one
to four weeks after irradiation, and the corresponding growth curve
was drawn. All the mice were sacrificed after 4 weeks to harvest
the tumor for histopathological examination. The samples were fixed
in 10% formalin to create paraffin sections, and stained with
hematoxylin and eosin for microscopic examination.
RNA isolation and reverse
transcription
Total RNA of the U251 cell line was extracted using
TRIzol (Sigma, Milwaukee, WI, USA). Concentration and purity were
assessed using an ultraviolet spectrophotometer at a wavelength of
260 and 280 nm. RNA was reverse transcribed into cDNA using the
reverse transcription kit (Takara Bio, Dalian, China). A master mix
(20 µl in total) containing 2X RT buffer (10 µl), RT
mix (1 µl), 6N random primers (1 µl), total RNA
(5µl), and nuclease-free water (3 µl) was prepared on
ice. The reaction was performed at 25°C for 10 min, 42°C for 50
min, and finally at 85°C for 5 min.
RT-qPCR
cDNA from the U251 glioma cell line was subjected to
RT-qPCR, which was performed using the IQ5 PCR instrument and the
SYBR Green real-time PCR Master Mix kit (Takara Bio). For
amplification of ATM, a Master Mix (50 µl) was prepared on
ice with 25.5 µl SYBR Green I Master Mix, 1 µl of
each primer, 2 µl cDNA, and 20.5 µl nuclease-free
water. The cDNA was initially denatured at 94°C for 4 min followed
by 35 cycles of denaturation at 94°C for 20 sec, annealing at 60°C
for 30 sec, and extension at 72°C for 30 sec. For amplification of
p53, PCNA and survivin, a Master Mix (25 µl) containing 10
µl SYBR Green I Master Mix, 1 µl of each primer, 5
µl of cDNA, and 8 µl nuclease-free water was prepared
on ice. After the cDNA was denatured at 94°C for 4 min, 40 cycles
of denaturation at 95°C for 5 sec, annealing at 60°C for 30 sec,
and extension at 72°C for 40 sec were performed. Primer sequences
were designed using the software Primer 5.0, and the sequences used
are listed in Table I. Actin was
used as an endogenous control. All the experiments were performed
in triplicate. The specificity of the amplification instructions
and absence of primer dimers were confirmed through a melting curve
analysis for each run. Relative quantification of the expression of
all genes was performed using the 2−ΔΔCt method.
 | Table ISequences of the primers used for
RT-qPCR. |
Table I
Sequences of the primers used for
RT-qPCR.
| Gene | Primer
sequences | Annealing
temperature (°C) | Product length
(bp) |
|---|
| Actin | F:
5′-TGACGTGGACATCCGCAAAG-3′ | R:
5′-CTGGAAGGTGGACAGCGAGG-3′ | 60 | 205 |
| ATM | F:
5′-GCACAGAAGTGCCTCCAATTC-3′ | R:
5′-ACATTCTGGCACGCTTTGG-3′ | 60 | 125 |
| P53 | F:
5′-CAGTCTACCTCCCGCCATAA-3′ | R:
5′-GTTCAAAGACCCAAAACCCA-3′ | 57 | 144 |
| PCNA | F:
5′-GGGACACTGCTGGTGGTATT-3′ | R:
5′-ACTGGTGGAGGGTAAACGGA-3′ | 59 | 102 |
| Survivin | F:
5′-TGTGATGAGGACAAAACGAAGC-3′ | R:
5′-CAGCCTGAGCAACAGAGCAA-3′ | 59 | 100 |
Western blotting
U251 cells were harvested on ice, and the total
protein extraction kit containing protease inhibitor was used.
Total protein from U251 cells was extracted after homogenization.
The protein concentration was determined using Coomassie brilliant
blue staining. Subsequently, 10% SDS-PAGE was performed to separate
the proteins (50 mg of protein per sample), and the extracted
proteins were transferred onto a polyvinylidene fluoride (PVDF)
membrane. The membrane was incubated overnight with the primary
antibodies diluted to 1:1,000 (5% w/v-BSA/TBST), and then incubated
with the secondary antibodies diluted to 1:1,000 (Zhongshan
Biotechnology). Next, the treated membrane was used for film
development and further analysis. The primary antibodies used were
anti-ATM and anti-phos-ATM (S1981) antibodies (Santa Cruz
Biotechnology Inc., Santa Cruz, CA, USA).
Cell counting
After irradiation, the ability for cell
proliferation was determined in triplicate using the CCK-8 assay
(Dojindo, Japan). Malignant cells, including those transfected with
siRNA-ATMPuro or siRNA-HKPuro, were plated
onto 96-well plates at a concentration of 3,000 per well and
cultured at 37°C overnight. Thereafter, the cells were incubated
with 10 µl CCK-8 for 4 h without removal of the medium. The
plates were shaken for 15 min, and absorbance was detected within
the range 490–630 nm on an ELISA reader (ELX800, Bio-Tek
Instruments Inc.).
Clonogenic survival assay
The cell survival fraction was determined by a
standard colony-forming efficiency assay. Briefly, U251 glioma
cells or transfected cells were disaggregated into a single-cell
suspension and diluted to a final concentration of 1×103
cells/ml. The cells were then plated onto 6-well plates and
cultured overnight. Then, the cells were subjected to irradiation
at doses of 2, 4, 6 and 8 Gy. After irradiation, the plates were
incubated at 37°C in a 5% CO2 atmosphere for ~2 weeks.
Prior to colony counting, the cells were washed with PBS, fixed
with formalin, stained with crystal violet (0.1% w/v), rinsed with
dH2O, and finally dried. Under a microscope, colonies
that contained more than 50 cells were considered to represent
survival colonies. The formula used was as follows: colony
formation rate (PE) = colony number/cell plating number × 100%;
survival fraction (SF) = number of colonies formed in response to a
certain dose/cell plating number × PE. Data were analyzed, and the
cell survival curve was drawn using the GraphPad Prism 5.0
software. Survival assays were repeated in triplicate.
Single-cell gel electrophoresis (neutral
comet assay)
The single-cell gel electrophoresis assay was
carried out with the CometAssay kit (Trevigen, USA) according to
the manufacturer's instructions. Briefly, 4 h after irra diation
with 5 Gy of X-rays, U251 single-cell suspensions were washed with
PBS and mixed with low-melting agarose (1:10). Next, the
cell-agarose mixtures were pipetted onto the comet assay slides.
Cell lysis was induced by incubating the mixture at 4°C for 3 h,
and the treated cells were then electrophoresed for 20 min at 4°C.
Subsequently, the resolved samples were fixed, and the DNA was
visualized by staining with 5 µg/ml Goldview (SBS Genetech,
Co., Ltd). Finally, the slides were observed under a confocal laser
microscope. Digital fluorescence images were obtained to calculate
the percentage of comet tails per 100 cells.
Cell cycle phase and cell apoptosis
analysis by flow cytometry
The percentage of cell distribution in the various
phases of the cell cycle was detected by flow cytometry.
Single-cell suspensions of U251 glioma cells (1×105
cells/ml) were washed twice with PBS and fixed with 75% alcohol.
After treatment with 500 µl of 1 g/l RNase at 37°C for 30
min, the cells were collected and fixed again, followed by staining
with propidium iodide (PI) for flow cytometric analysis. The
percentage of cells that underwent cell apoptosis was also
determined by flow cytometry. Single-cell suspensions of the glioma
cells (1×105 cells/ml, 100 µl) were added into
microcentrifuge tubes and mixed with 5 µl of Annexin IV-FITC
and 20 µg/ml PI. After 15 min of incubation at room
temperature, the percentage of apoptotic cells was determined by
flow cytometry.
Detection of caspase-3, -8, and -9
Malignant cells were plated onto 96-well plates at a
concentration of 3,000 cells/well and cultured at 37°C overnight.
After 24 h of irradiation, caspase-3, -8, and -9 (100
µl/well) were added to the plate. The plates were then
shaken for 15 min at 37°C, and absorbance was detected at a
wavelength range of 490–630 nm using an ELISA reader (ELX800,
Bio-Tek Instruments Inc.).
Statistical analysis
SAS 8.1 was used to analyze the experimental data,
which are presented as mean ± SD. The RT-qPCR, CCK-8, caspase
expression, comet tail percentage, and flow cytometry data were
analyzed by ANOVA. The data from the clonogenic survival assay were
analyzed using GraphPad Prism 5.0. Changes in tumor volume were
analyzed using the Student's t-test. Statistical significance was
set at a P-value of <0.05.
Results
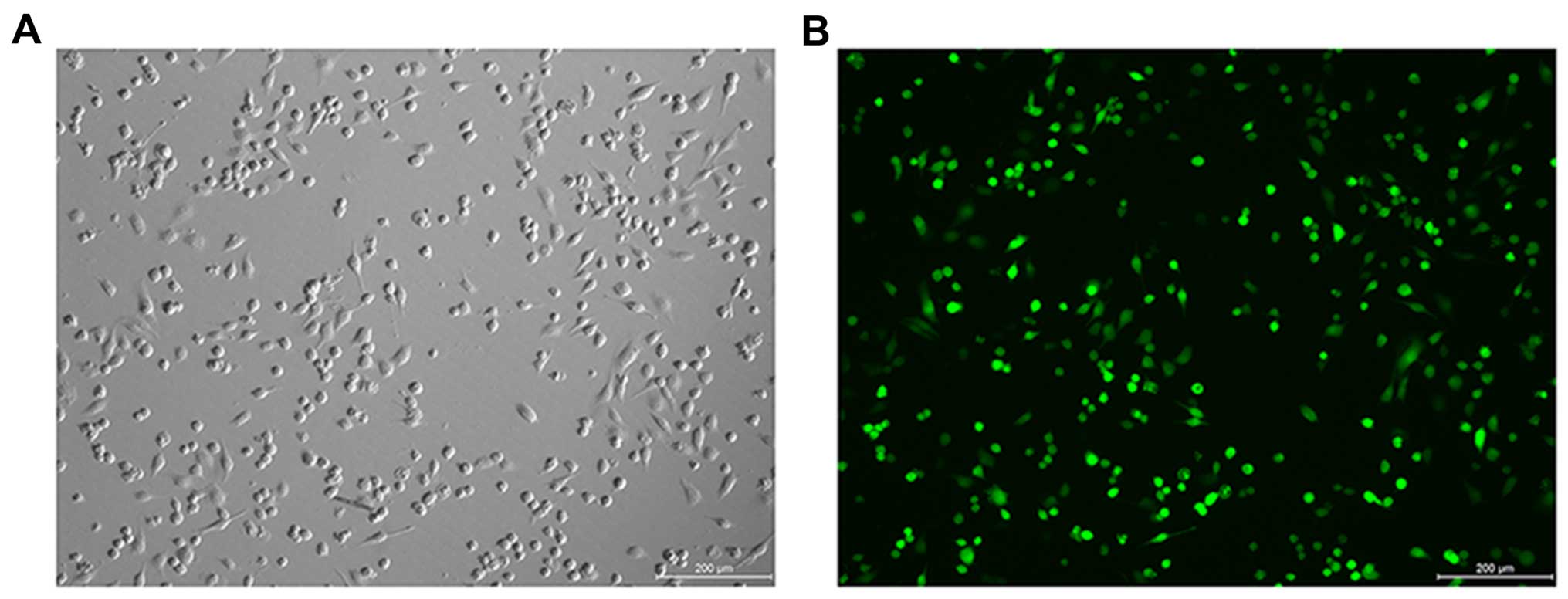
Efficiency of cell transfection
siRNA-ATMPuro and siRNA-HKPuro
lentiviruses were transfected into glioma U251 cells. Under an
inverted fluorescence microscope, green fluorescence protein (GFP)
was observed to be obviously expressed in the tumor cells,
indicating that the efficiency of transfection was nearly 99%
(Fig. 1A and B). Moreover, no
obvious dead cells were observed in the medium after resistance
selection using puromycin, which also demonstrated the high
efficiency of the lentivirus transfection.
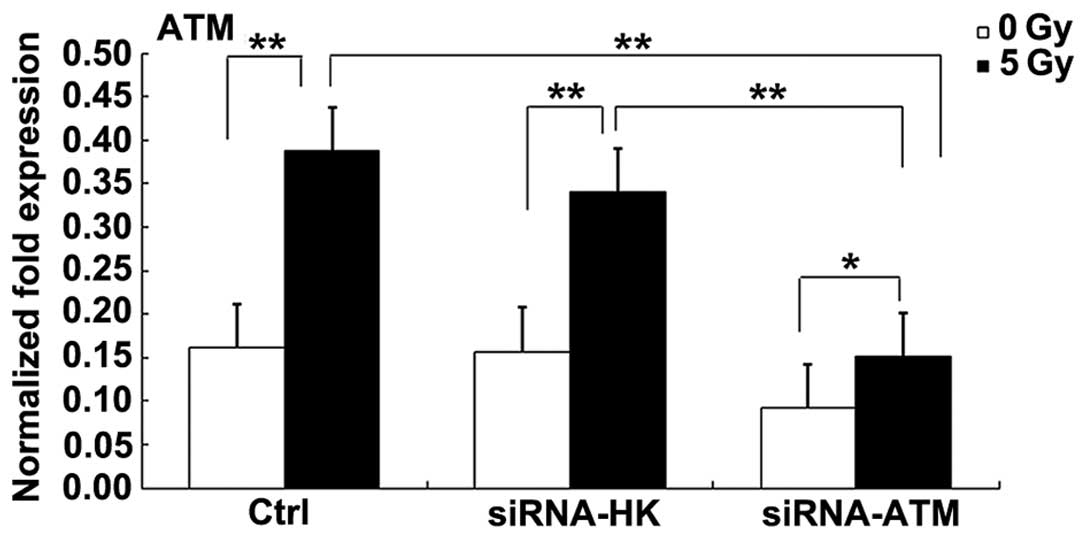
Changes in in vitro ATM expression after
siRNA treatment
To assess the effect of siRNA-ATM, we examined ATM
gene and protein expression in the glioblastoma cells by RT-qPCR
and western blotting. In the U251 cells, ATM expression was
obviously downregulated after transfection with the lentivirus
vector expressing siRNA-ATM. PCR results showed that after exposure
to radiation, ATM expression in the C and N groups was obviously
increased (P<0.01). However, there was little increase in ATM
expression in the A group after irradiation (P<0.05). Moreover,
ATM gene expression was considerably lower in the A group than that
noted in the C or N group (P<0.01) (Fig. 2).
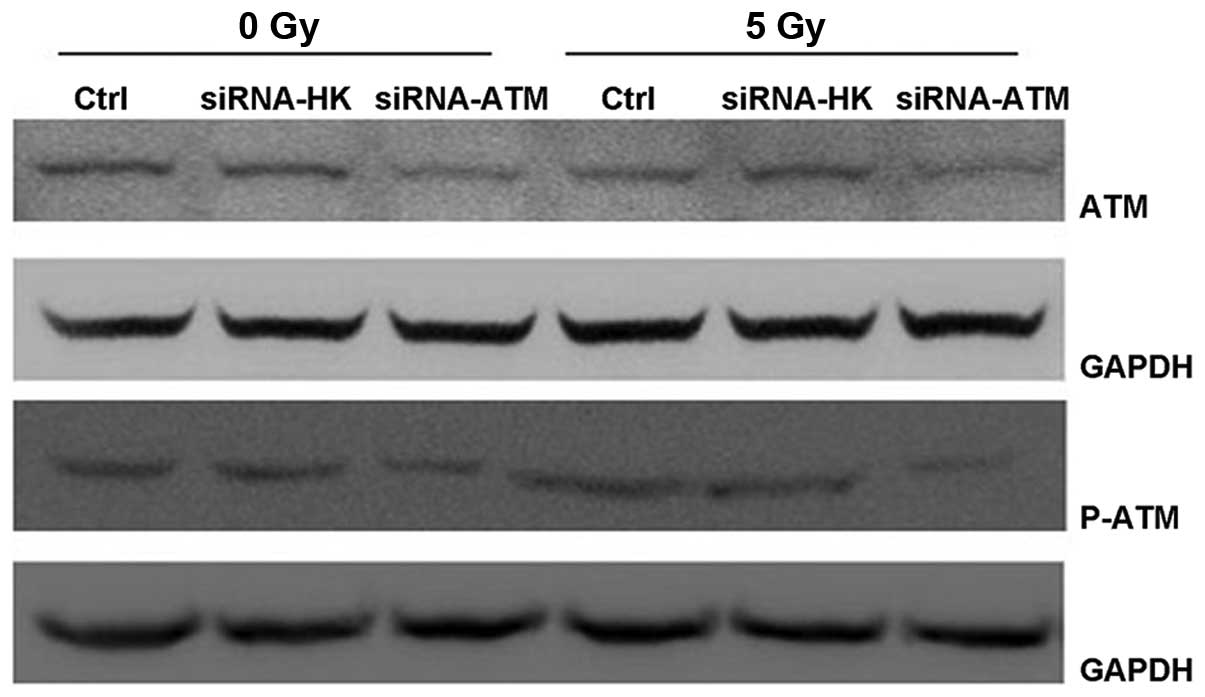
Western blotting revealed similar results in the
U251 cell line. In both the C and N groups, the total level of ATM
protein was similar before and after irradiation. p-ATM protein was
expressed slightly before irradiation, while its expression was
considerably higher after irradiation. In the A group, the amount
of total ATM protein was obviously lower after irradiation, but
expression of the p-ATM protein was not obviously observed before
or after irradiation (Fig. 3).
After radiation treatment, the levels of total ATM and p-ATM
proteins in group A were lower than levels in the C and N groups
(Fig. 3).
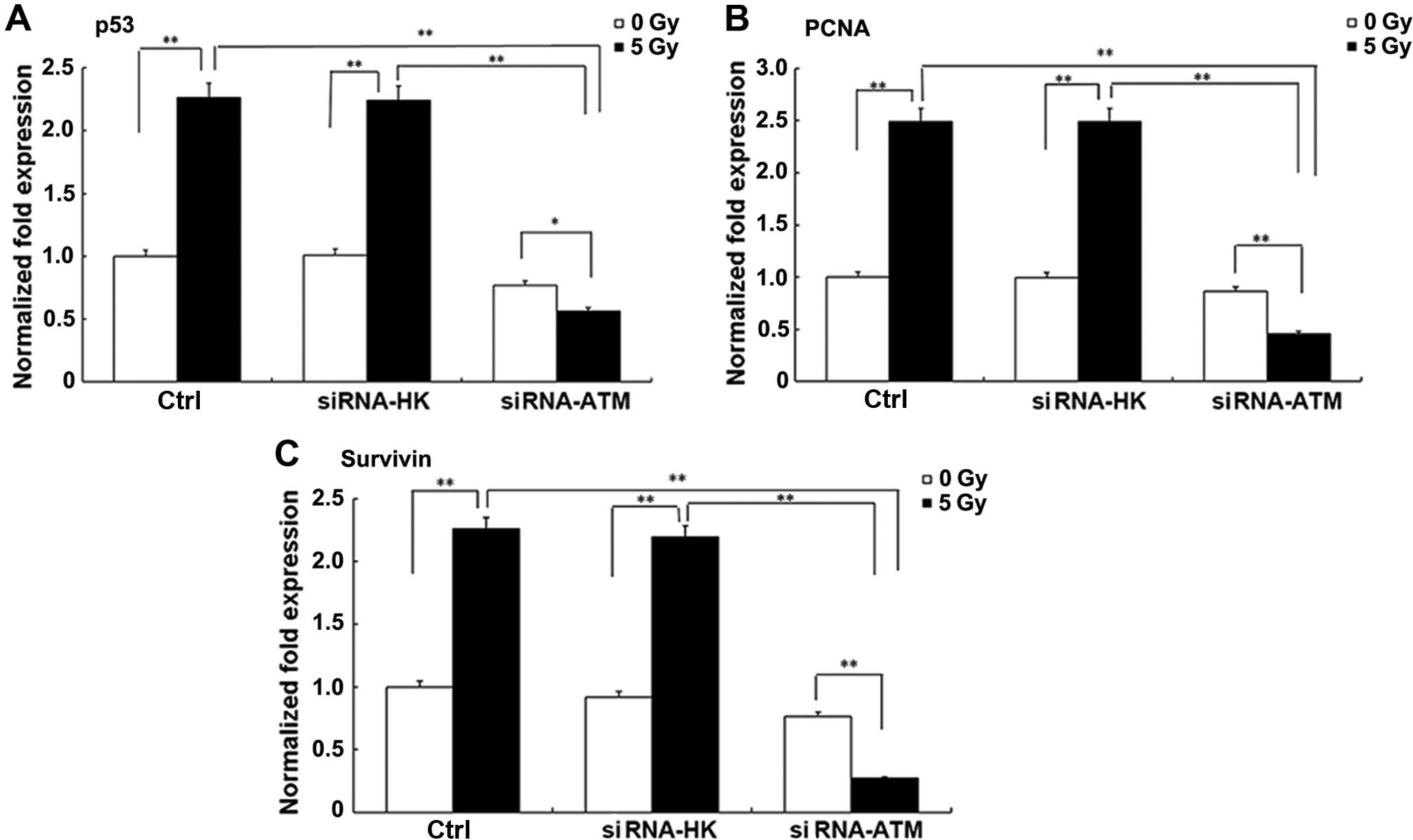
Changes in the expression of other
radiosensitivity-related genes after transfection of siRNA-ATM
lentivirus into glioma cell lines
The expression of other radiosensitivity-related
genes, including P53, PCNA and survivin, was also examined by
RTq-PCR. After irradiation, the expression of the three genes (P53,
PCNA, and survivin) increased to some degree in the C and N groups,
but their expression was decreased in the A group (P<0.01).
After irradiation, the lower expression of these genes in the A
group was more obvious (P<0.01) (Fig. 4A–C).
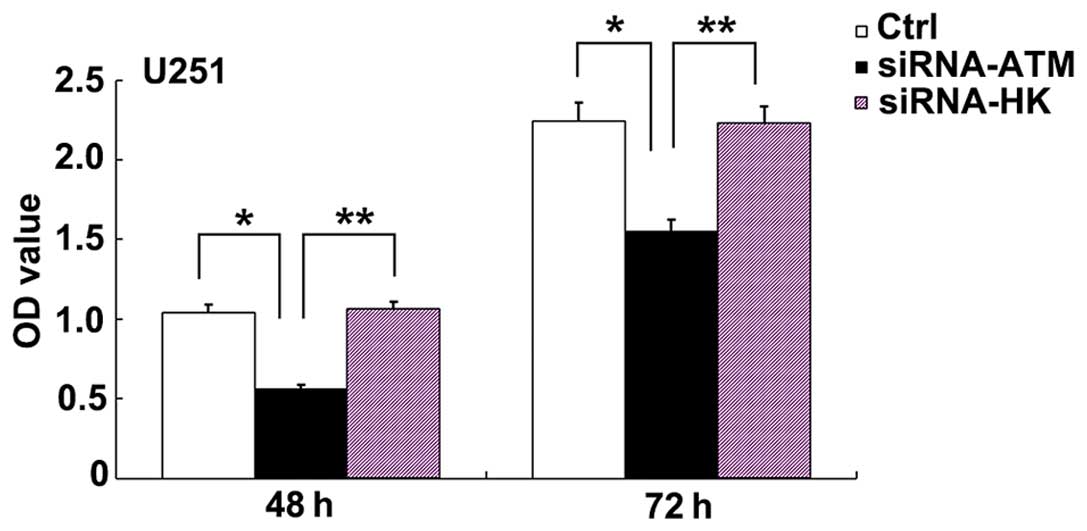
Inhibition of cell proliferation after
siRNA-ATM treatment
At 48 and 72 h after irradiation, cell proliferation
in the A group was significantly less than that in the C and N
groups (Fig. 5) (P<0.01, A group
vs. N group; P<0.05, A group vs. C group). Between the two
time-points, there was no obvious increase in cell proliferation in
the A group. However, cell proliferation in the C and N groups
showed a mild increase from 48 to 72 h (P>0.05).
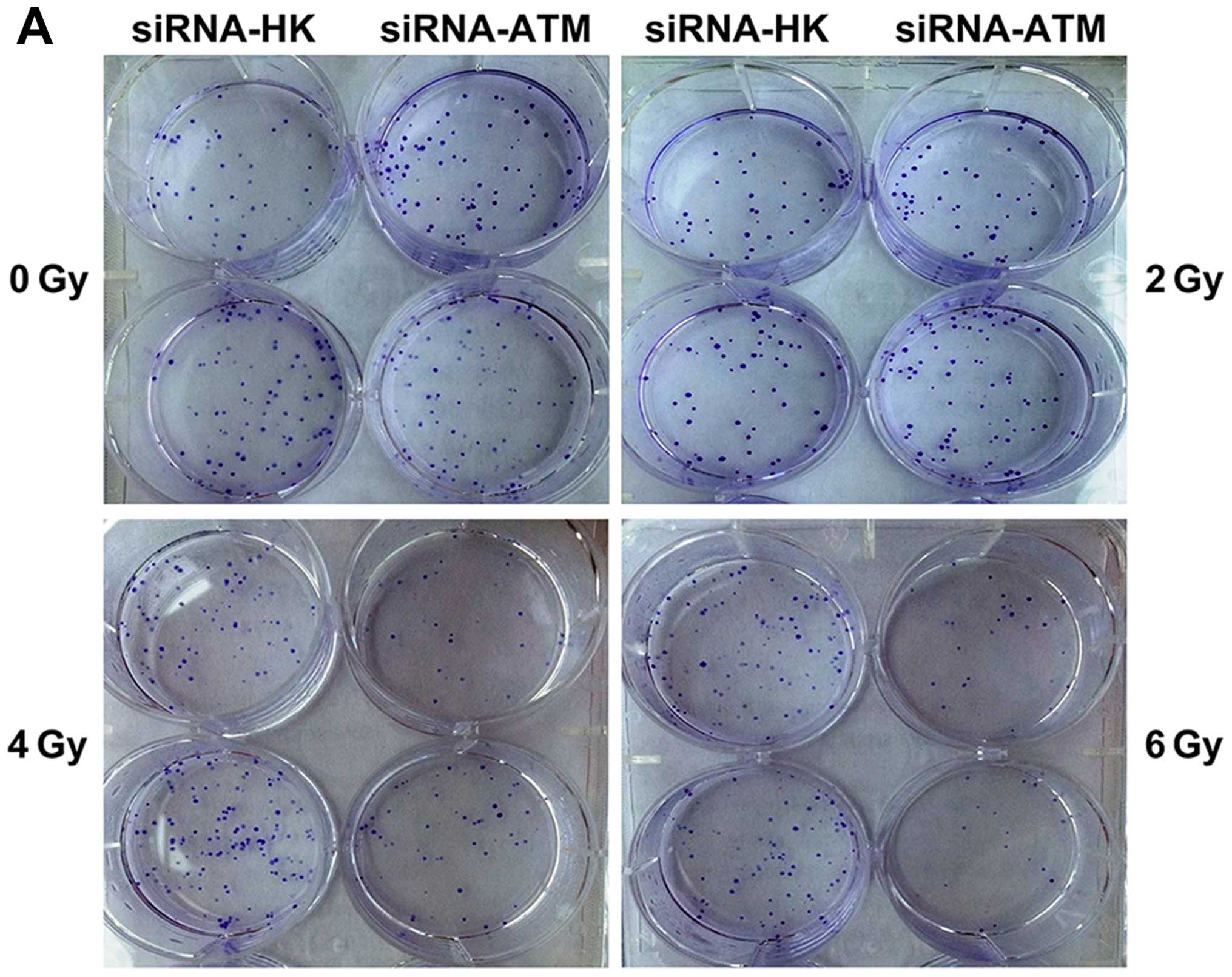
Clonogenic survival assay of the
siRNA-ATM-transfected cell line after irradiation
The number of colonies formed decreased with an
increase in the radiation dose in groups A and N, which indicated a
dose-dependent relationship (Fig.
6A). At the same dose, the number of colonies in the A group
was less than that in the C and N groups, while the number was
similar in the N group (Fig. 6B).
Microscopic observation after crystal violet staining showed that
the colonies formed by cells of the A group were smaller and lesser
in number (Fig. 6C), and they
further decreased in size and number with an increase in the
radiation dose.
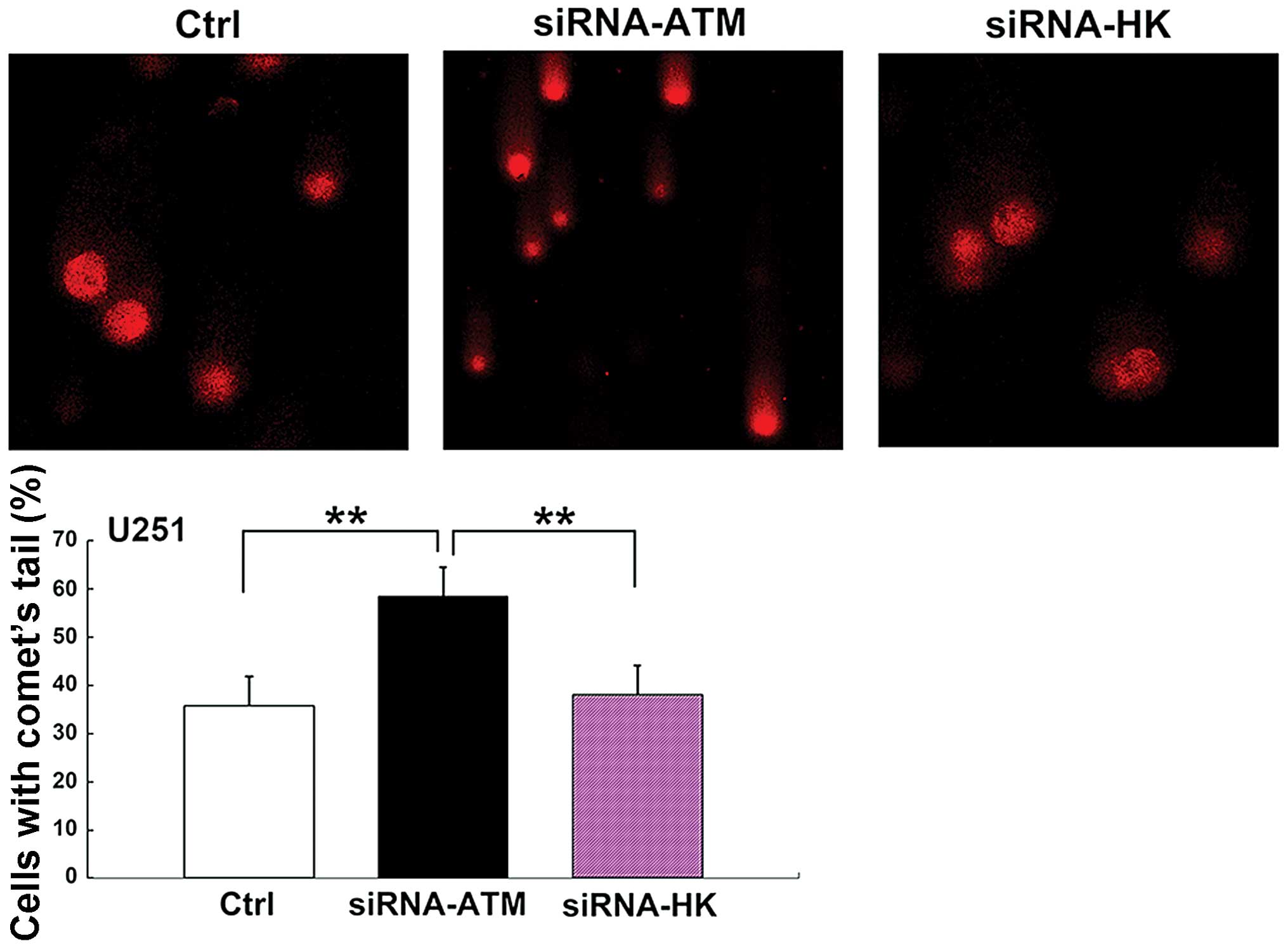
Single-cell gel electrophoresis (neutral
comet assay)
Before irradiation, comet tail formation was not
observed in any of the three groups. However, the proportion of
comet tails in the A group was elevated after irradiation with 5 Gy
X-ray, as compared with that in the C and N groups (P<0.01)
(Fig. 7). The results in the C
group were similar to those in the N group.
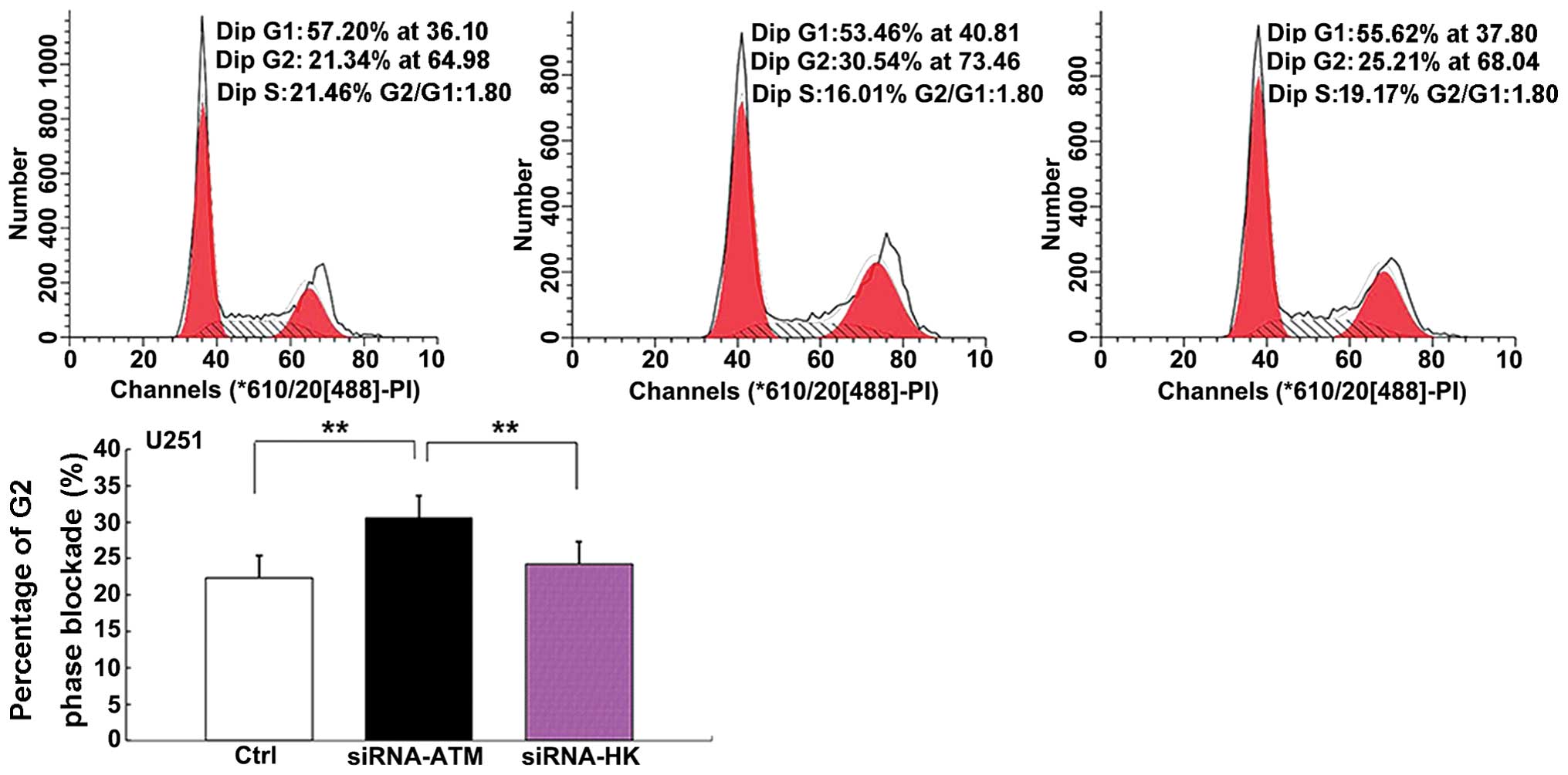
Effect of irradiation on cell cycle
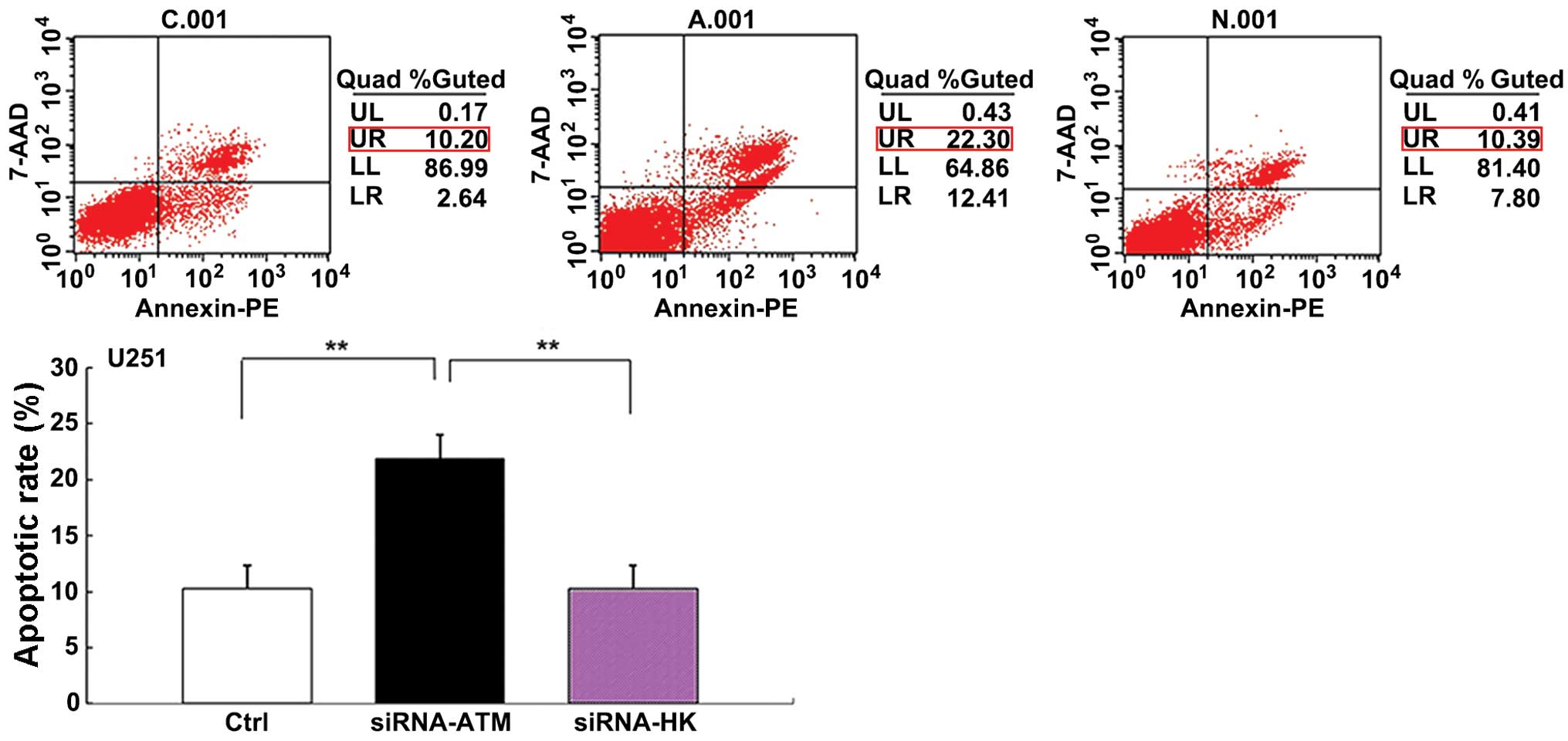
distribution and cell apoptosis
The percentage of apoptotic cells in group A,
particularly those in the later cell cycle stages, was greater than
that in groups C and N (P<0.01) (Fig. 8). There was no significant
difference in the apoptosis rate between group C and group N.
Similarly, the percentage of cells in the G2 phase in group A
showed an obvious increase compared with groups C and N (P<0.01)
(Fig. 9).
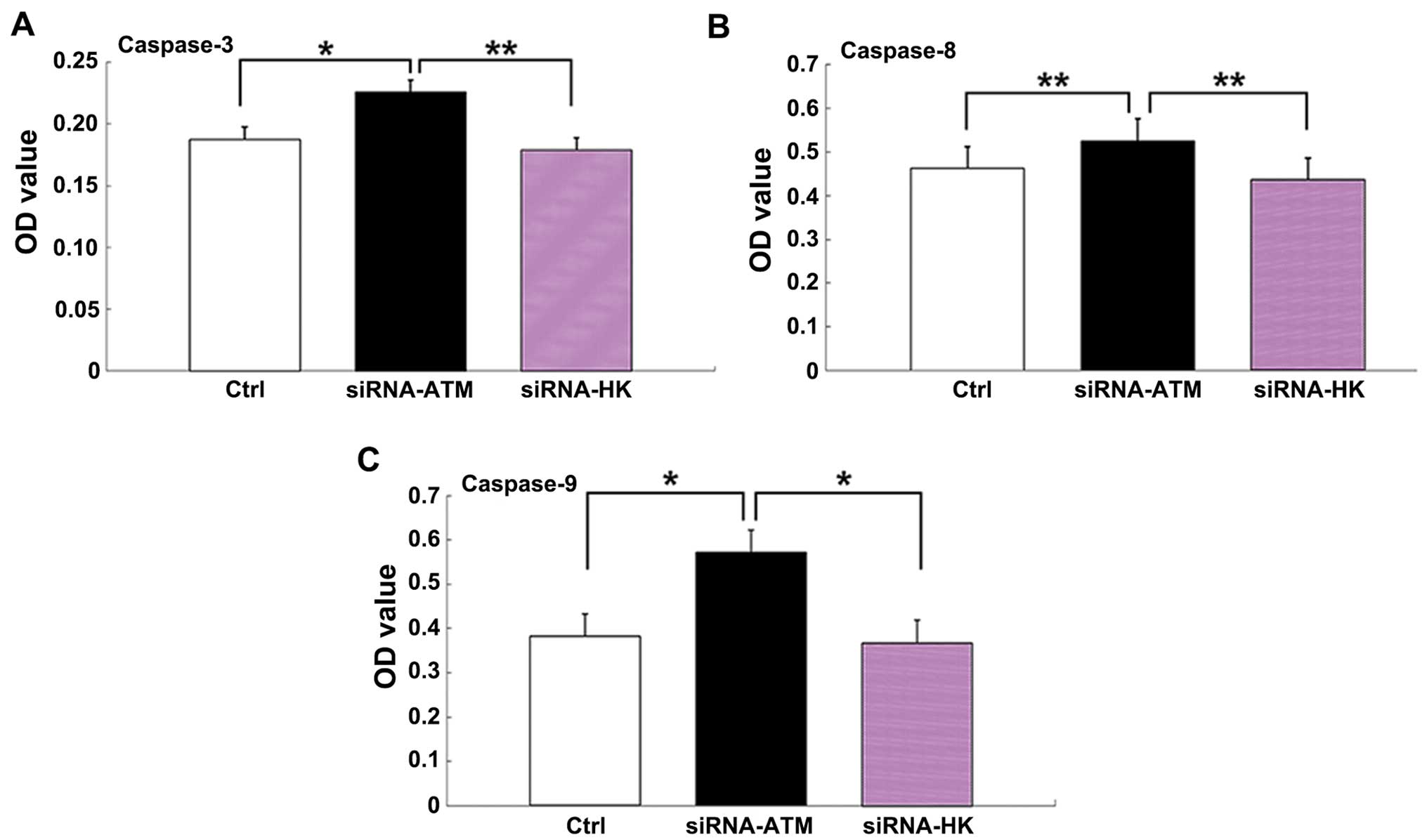
Detection of caspase-3, -8 and -9
The expression levels of caspase-3, -8 and -9, which
are linked to the apoptosis pathway, were higher in group A than in
group C and N (caspase-3: P<0.05, group A vs. group C;
P<0.01, group A vs. group N; caspase-8: P<0.01, group A vs.
group C/N; caspase-9: P<0.05, group A vs. group C/N). No
significant difference was found between group C and N (Fig. 10A–C).
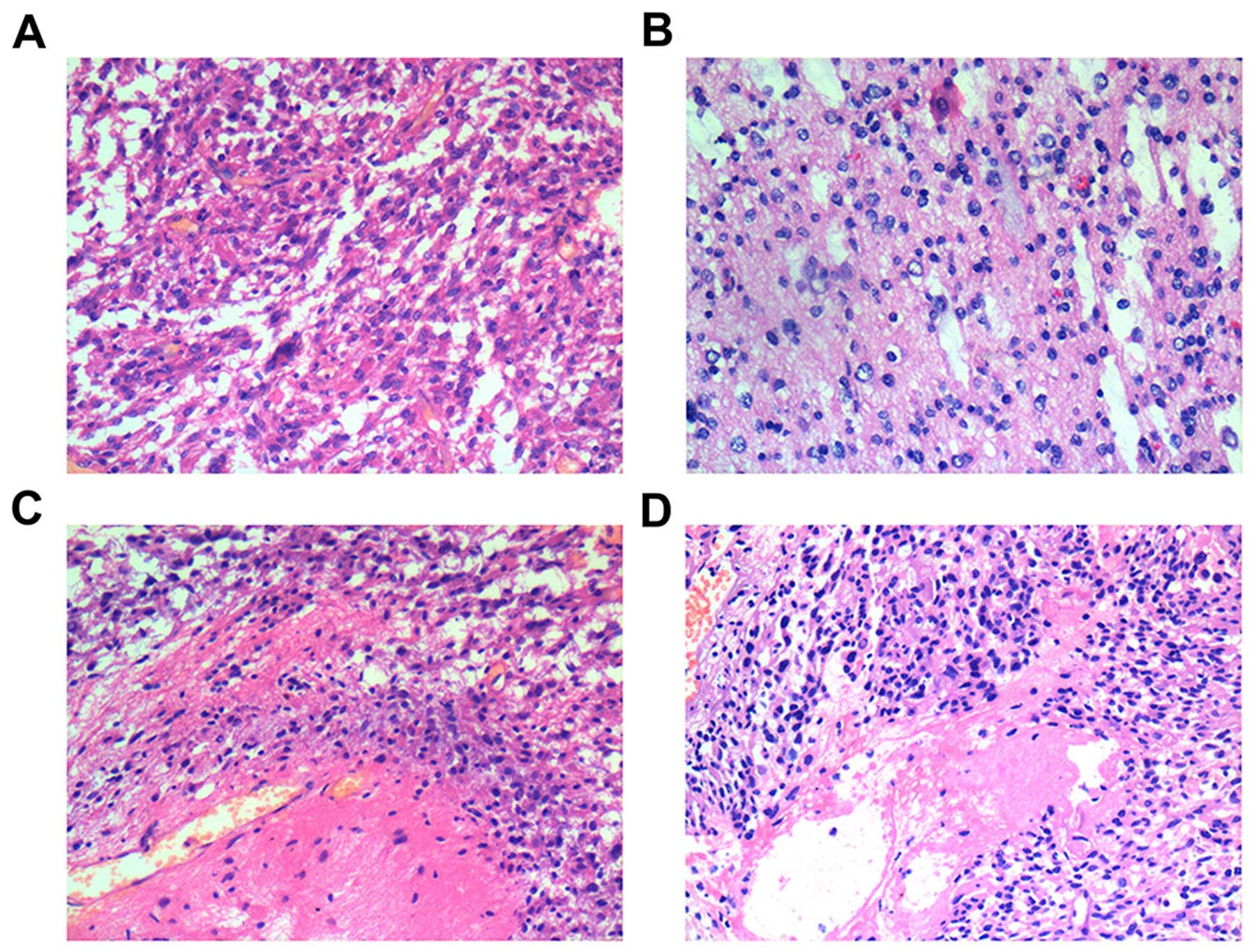
Histopathalogical findings
The histopathological findings in the animal models
differed before and after irradiation. Prior to irradiation, the
histological features of group A (Fig.
11A) were similar to those of group N (Fig. 11B), and were characterized by
nuclear polymorphism, nuclear hyperchromatism, and considerable
karyokinesis. However, after irradiation, necrosis and hemorrhage
of tumor cells in group A (Fig.
11C) were more obvious than that in group N (Fig. 11D).
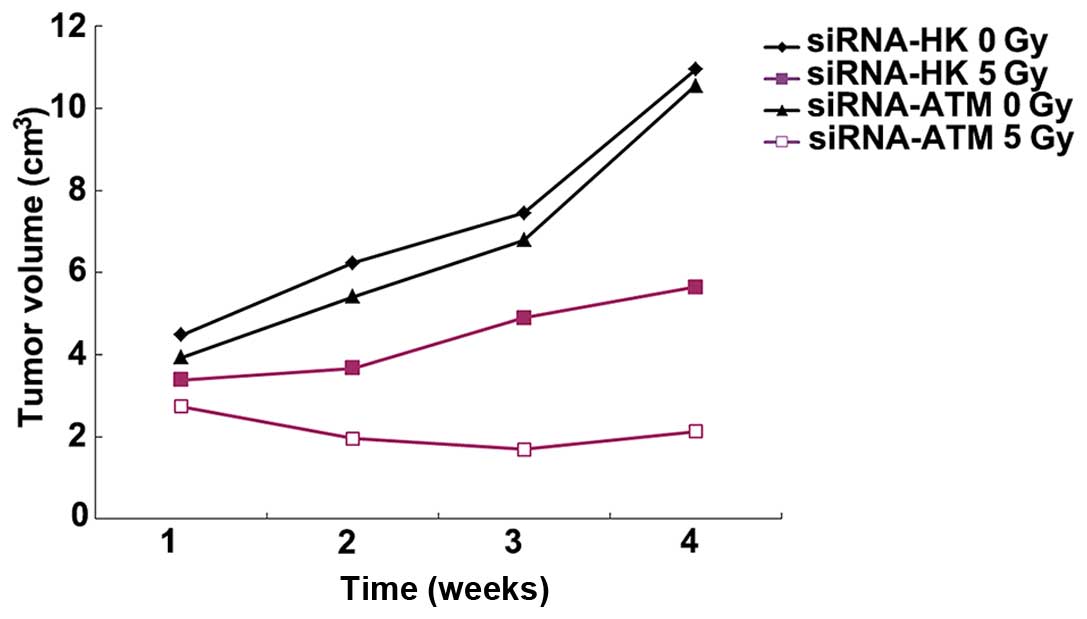
Changes in tumor volume
Within the first to fourth week after implantation,
there was no obvious difference in tumor volume between groups A
and N before treatment with ionizing radiation. The tumor volume
was found to be time-dependent: that is, it increased with time.
After radiation treatment, the tumor volume in group A decreased
while that in group N remained more or less stable from the first
to the fourth week (Fig. 12). The
tumor volume in group A was significantly lower than that in group
N (P<0.05, 2 and 3 weeks; P<0.01, 1 and 4 weeks).
Discussion
Glioma is a malignant brain tumor that continues to
have a poor median survival of about one year. Several researchers
have reported that the ATM gene is linked with resistance against
radiotherapy, which is associated with the poor prognosis of glioma
(2,8,9). For
example, Tribius et al (14)
reported that ATM was highly expressed after radiation treatment of
a glioma cell line. Similarly, in tumors such as cervical cancer
and breast cancer, expression of the ATM gene is greatly increased
after radiation treatment in tumor cells (15,16).
Based on these findings, we hypothesized that lentivirus-mediated
silencing of ATM gene expression via the siRNA technique may
enhance the radiosensitivity of malignant glioma.
Although gene interference suppressed ATM gene
expression, it was not completely effective, and failed to result
in the control of the downstream pathway by ATM imperfect
retardant. Therefore, in order to ensure effective gene silencing,
gene knockdown should be considered to further repress the related
signal pathway, as it may enhance the radiosensitivity of gliomas.
For instance, some scholars found that ATM−/−mice had
better survival than ATM−/+ mice, which indicates that
ATM is responsible for therapy resistance (6).
ATM kinase inhibitors have been the subject of
research on gliomas during recent years (1,7,13).
However, there are still many limitations: there is no effective
delivery system for administration in cephalic regions; the
pharmacological dose for effective in vivo therapy is not
clear; and possible harmful effects on the brain are also not clear
(7).
In our study, genes related to radiosensitivity
(P53, survivin, and PCNA) identified as downstream genes of ATM
(17–19), were analyzed by RT-qPCR. The results
indicated that P53, survivin, and PCNA were indeed involved in the
repair pathway and play a role in the radiosensitivity of glioma
cells. These findings are consistent with those of the CCK-8 and
clone formation assay, in which proliferation was also found to be
decreased in response to ATM silencing.
Our study found that damage to glioma tumor cells
was obviously enhanced by ionizing radiation after the ATM gene was
silenced by the siRNA technique. Compared to the control group, the
survival curve of group A showed a significant decline, and the
number of damaged cells, i.e. the cleavage of double-stranded DNA,
in the comet tail assay was obviously increased. All these results
verify that the tumor responded to radiation and that
radiosensitivity was enhanced after silencing of the ATM gene. The
CCK-8 findings showed high expression of ATM after radiation
treatment in the control cells, which was considered to be
responsible for the repair of damaged cells and maintaining cell
proliferation. However, suppression of the ATM gene resulted in a
decrease in cell proliferation as a result of slowing down of the
cell repair mechanism. However, changes in cell proliferation in
relation to time need to be explored in the future. Intriguingly,
Moschos et al (20) reported
contrasting results when malignant melanoma cells were transfected
with siRNA against ATM. According to them, the hyperpigmentation
gene may play an important role in the radiosensitivity of
melanoma, which could explain their findings.
In our study, a higher percentage of apoptosed cells
were in the late stage than in the early stage. Therefore, another
mechanism related to the repair of damaged cells may play an
important role after suppression of the ATM gene. After
irradiation, expression of the ATM gene increased with time and
resulted in a corresponding decline in the amount of repaired cells
and increase in the amount of damaged cells. This also explains why
a higher number of cells were in the late apoptotic stage than in
the early apoptotic stage. The percentage of cells in the G2 phase
of the cell cycle was higher in the siRNA-ATM treated group than in
the control group, which implies that irradiated tumor cells which
were treated with siRNA-ATM performed slow self-repairing.
In addition, we investigated changes in the
apoptosis pathway. It is well known that the caspase family plays a
role in apoptosis, and that caspase-8 and caspase-9 in particular
are involved in the initiation of apoptosis while caspase 3 plays a
key role in apoptosis (21). We
found that the expression of caspase-3, caspase-8, and caspase-9
increased in radiation-treated siRNA-ATM tumor cells. The results
demonstrated that silencing of ATM could activate the apoptosis
pathway, followed by the enhancement of cell apoptosis and
radiosensitivity. On the contrary, Liu et al (22) reported that siRNA against ATM not
only directly inhibits caspase-3 activity but also inhibits
caspase-8 activity during TNF-α-induced apoptosis in HeLa cells. We
think that the findings may differ according to the type of
tumor.
To the best of our knowledge, there is less reported
in vivo research on the role of ATM. Here, we verified the
in vitro findings under in vivo conditions. After
irradiation, the tumor volume decreased and the growth curve was
slower than before in the siRNA-ATM-transfected animal models. The
results are consistent with the histopathological findings; in
other words, hemorrhage and necrosis of tumor cells in the
siRNA-ATM-transfected group were greater and resulted in a decrease
in tumor volume. However, there was no significant difference in
the animal models, which may be related to the short observation
period and inefficient elimination of the irradiated tumor.
Therefore, the treatment effect needs to be assessed over a longer
observation period. Moreover, there are certain limitations with
regard to establishment of the glioma model and the side effect of
radiation on adjacent tissues. We need to further explore the
optimal experimental conditions.
In conclusion, siRNA-ATM transfection in glioma
cells resulted in a decline in cell proliferation, colony formation
rate and survival and an increase in cell apoptosis, the number of
cells in the G2 phase, and the proportion of comet tails.
Therefore, we inferred that silencing of the ATM gene via the siRNA
technique could enhance the radiosensitivity of glioma cells, which
could improve the therapeutic effect of radiation and prolong
patient survival. Most of the research in this field has provided
similar evidence (1,2,9).
Acknowledgements
We would like to thank the State Key Laboratory of
Ultrasound Engineering in Medicine Co-founded by Chongqing and the
Ministry of Science and Technology for providing the lab. We
acknowledge grant support from the National Natural Science
Foundation of China (no. 81172387) and the Natural Science
Foundation of Chongqing (CSTC2011BB5119).
References
|
1
|
Biddlestone-Thorpe L, Sajjad M, Rosenberg
E, Beckta JM, Valerie NC, Tokarz M, Adams BR, Wagner AF, Khalil A,
Gilfor D, et al: ATM kinase inhibition preferentially sensitizes
p53-mutant glioma to ionizing radiation. Clin Cancer Res.
19:3189–3200. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang SC, Wu CC, Wei YY, Hong JH and Chiang
CS: Inactivation of ataxia telangiectasia mutated gene can increase
intracellular reactive oxygen species levels and alter
radiation-induced cell death pathways in human glioma cells. Int J
Radiat Biol. 87:432–442. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee JH and Paull TT: ATM activation by DNA
double-strand breaks through the Mre11-Rad50-Nbs1 complex. Science.
308:551–554. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shiloh Y: ATM and related protein kinases:
safeguarding genome integrity. Nat Rev Cancer. 3:155–168. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jackson SP: Sensing and repairing DNA
double-strand breaks. Carcinogenesis. 23:687–696. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Squatrito M, Brennan CW, Helmy K, Huse JT,
Petrini JH and Holland EC: Loss of ATM/Chk2/p53 pathway components
accelerates tumor development and contributes to radiation
resistance in gliomas. Cancer Cell. 18:619–629. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vecchio D, Daga A, Carra E, Marubbi D,
Baio G, Neumaier CE, Vagge S, Corvò R, Pia Brisigotti M, Louis
Ravetti J, et al: Predictability, efficacy and safety of
radiosensitization of glioblastoma-initiating cells by the ATM
inhibitor KU-60019. Int J Cancer. 15:479–491. 2014. View Article : Google Scholar
|
|
8
|
Golding SE, Rosenberg E, Adams BR,
Wignarajah S, Beckta JM, O'Connor MJ and Valerie K: Dynamic
inhibition of ATM kinase provides a strategy for glioblastoma
multiforme radiosensitization and growth control. Cell Cycle.
11:1167–1173. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gil del Alcazar CR, Hardebeck MC,
Mukherjee B, Tomimatsu N, Gao X, Yan J, Xie XJ, Bachoo R, Li L,
Habib AA, et al: Inhibition of DNA double-strand break repair by
the dual PI3K/mTOR inhibitor NVP-BEZ235 as a strategy for
radiosensitization of glioblastoma. Clin Cancer Res. 20:1235–1248.
2014. View Article : Google Scholar
|
|
10
|
Zhou W, Sun M, Li GH, Wu YZ, Wang Y, Jin
F, Zhang YY, Yang L and Wang DL: Activation of the phosphorylation
of ATM contributes to radioresistance of glioma stem cells. Oncol
Rep. 30:1793–1801. 2013.PubMed/NCBI
|
|
11
|
Guha C, Guha U, Tribius S, Alfieri A,
Casper D, Chakravarty P, Mellado W, Pandita TK and Vikram B:
Antisense ATM gene therapy: a strategy to increase the
radiosensitivity of human tumors. Gene Ther. 7:852–858. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chuah TL, Walker DG, Wei M, Scott S and
Lavin MF: Approaches to sensitizing glioblastoma to radiotherapy:
use of lentiviral vectors. Int J Oncol. 40:1963–1969.
2012.PubMed/NCBI
|
|
13
|
Nadkarni A, Shrivastav M, Mladek AC,
Schwingler PM, Grogan PT, Chen J and Sarkaria JN: ATM inhibitor
KU-55933 increases the TMZ responsiveness of only inherently TMZ
sensitive GBM cells. J Neurooncol. 110:349–357. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tribius S, Pidel A and Casper D: ATM
protein expression correlates with radioresistance in primary
glioblastoma cells in culture. Int J Radiat Oncol Biol Phys.
50:511–523. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li W, Jian W, Xiaoping X, Yingfeng L, Tao
X and Xiaoyan X: Enhanced radiation-mediated cell killing of human
cervical cancer cells by small interference RNA silencing of ataxia
telangiectasia-mutated protein. Int J Gynecol Cancer. 16:1620–1630.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bernstein JL, Haile RW, Stovall M, Boice
JD Jr, Shore RE, Langholz B, Thomas DC, Bernstein L, Lynch CF,
Olsen JH, et al WECARE Study Collaborative Group: Radiation
exposure, the ATM Gene, and contralateral breast cancer in the
women's environmental cancer and radiation epidemiology study. J
Natl Cancer Inst. 102:475–483. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Poosarla C, Ramesh M, Ramesh K, Gudiseva
S, Bala S and Sundar M: Proliferating cell nuclear antigen in
premalignancy and oral squamous cell carcinoma. J Clin Diagn Res.
9:ZC39–ZC41. 2015.PubMed/NCBI
|
|
18
|
Yang M, Zhai X, Xia B, Wang Y and Lou G:
Long noncoding RNA CCHE1 promotes cervical cancer cell
proliferation via upregulating PCNA. Tumour Biol. 36:7615–7622.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tamm I, Wang Y, Sausville E, Scudiero DA,
Vigna N, Oltersdorf T and Reed JC: IAP-family protein survivin
inhibits caspase activity and apoptosis induced by Fas (CD95), Bax,
caspases, and anticancer drugs. Cancer Res. 58:5315–5320.
1998.PubMed/NCBI
|
|
20
|
Moschos SJ, Dodd NR, Jukic DM, Fayewicz
SL, Wang X and Becker D: Suppressing the high-level expression and
function of ATM in advanced-stage melanomas does not sensitize the
cells to ionizing radiation. Cancer Biol Ther. 8:1815–1825. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sahu U, Sidhar H, Ghate PS, Advirao GM,
Raghavan SC and Giri RK: A novel anticancer agent,
8-methoxypyrimido[4′,5′:4,5] thieno(2,3-b) quinoline-4(3h)-one
induces neuro 2a neuroblastoma cell death through p53-dependent,
caspase-dependent and -independent apoptotic pathways. PLoS One.
8:e664302013. View Article : Google Scholar
|
|
22
|
Liu L, Yim H, Choi JH, Kim ST, Jin Y and
Lee SK: ATM kinase promotes both caspase-8 and caspase-9 activation
during TNF-α-induced apoptosis of HeLa cells. FEBS Lett.
588:929–935. 2014. View Article : Google Scholar : PubMed/NCBI
|