|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2016. CA Cancer J Clin. 66:7–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang ZC, Birkbak NJ, Culhane AC, Drapkin
R, Fatima A, Tian R, Schwede M, Alsop K, Daniels KE, Piao H, et al:
Profiles of genomic instability in high-grade serous ovarian cancer
predict treatment outcome. Clin Cancer Res. 18:5806–5815. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
National institute for health and clinical
excellence, . Guidance on the use of paclitaxel in the treatment of
ovarian cancer. 2005.http://www.nice.org.uk/guidance/ta55
|
|
4
|
Goff BA: Advanced ovarian cancer: What
should be the standard of care? J Gynecol Oncol. 24:83–91. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pils D, Hager G, Tong D, Aust S, Heinze G,
Kohl M, Schuster E, Wolf A, Sehouli J, Braicu I, et al: Validating
the impact of a molecular subtype in ovarian cancer on outcomes: A
study of the OVCAD Consortium. Cancer Sci. 103:1334–1341. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Smith WL: Prostanoid biosynthesis and
mechanisms of action. Am J Physiol. 263:F181–F191. 1992.PubMed/NCBI
|
|
7
|
Farhat A, Philibert P, Sultan C, Poulat F
and Boizet-Bonhoure B: Hematopoietic-prostaglandin D2 synthase
through PGD2 production is involved in the adult ovarian
physiology. J Ovarian Res. 4:32011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Abdel-Halim MS, Hamberg M, Sjöquist B and
Anggård E: Identification of prostaglandin D2 as a major
prostaglandin in homogenates of rat brain. Prostaglandins.
14:633–643. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saso L, Leone MG, Sorrentino C, Giacomelli
S, Silvestrini B, Grima J, Li JC, Samy E, Mruk D and Cheng CY:
Quantification of prostaglandin D synthetase in cerebrospinal
fluid: A potential marker for brain tumor. Biochem Mol Biol Int.
46:643–656. 1998.PubMed/NCBI
|
|
10
|
Kikuchi Y, Miyauchi M, Oomori K, Kita T,
Kizawa I and Kato K: Inhibition of human ovarian cancer cell growth
in vitro and in nude mice by prostaglandin D2. Cancer Res.
46:3364–3366. 1986.PubMed/NCBI
|
|
11
|
Yoshida T, Ohki S, Kanazawa M, Mizunuma H,
Kikuchi Y, Satoh H, Andoh Y, Tsuchiya A and Abe R: Inhibitory
effects of prostaglandin D2 against the proliferation of human
colon cancer cell lines and hepatic metastasis from colorectal
cancer. Surg Today. 28:740–745. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Payne CA, Maleki S, Messina M, O'Sullivan
MG, Stone G, Hall NR, Parkinson JF, Wheeler HR, Cook RJ, Biggs MT,
et al: Loss of prostaglandin D2 synthase: A key molecular event in
the transition of a low-grade astrocytoma to an anaplastic
astrocytoma. Mol Cancer Ther. 7:3420–3428. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shyu RY, Wu CC, Wang CH, Tsai TC, Wang LK,
Chen ML, Jiang SY and Tsai FM: H-rev107 regulates prostaglandin D2
synthase-mediated suppression of cellular invasion in testicular
cancer cells. J Biomed Sci. 20:302013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tippin BL, Kwong AM, Inadomi MJ, Lee OJ,
Park JM, Materi AM, Buslon VS, Lin AM, Kudo LC, Karsten SL, et al:
Intestinal tumor suppression in ApcMin/+ mice by
prostaglandin D2 receptor PTGDR. Cancer Med.
3:1041–1051. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
du Bois A, Reuss A, Pujade-Lauraine E,
Harter P, Ray-Coquard I and Pfisterer J: Role of surgical outcome
as prognostic factor in advanced epithelial ovarian cancer: A
combined exploratory analysis of 3 prospectively randomized phase 3
multicenter trials: By the Arbeitsgemeinschaft Gynaekologische
Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe
d'Investigateurs Nationaux Pour les Etudes des Cancers de l'Ovaire
(GINECO). Cancer. 115:1234–1244. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cooke SL and Brenton JD: Evolution of
platinum resistance in high-grade serous ovarian cancer. Lancet
Oncol. 12:1169–1174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Colombo PE, Fabbro M, Theillet C, Bibeau
F, Rouanet P and Ray-Coquard I: Sensitivity and resistance to
treatment in the primary management of epithelial ovarian cancer.
Crit Rev Oncol Hematol. 89:207–216. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rustin GJ, Vergote I, Eisenhauer E,
Pujade-Lauraine E, Quinn M, Thigpen T, du Bois A, Kristensen G,
Jakobsen A, Sagae S, et al: Definitions for response and
progression in ovarian cancer clinical trials incorporating RECIST
1.1 and CA 125 agreed by the Gynecological Cancer Intergroup
(GCIG). Int J Gynecol Cancer. 21:419–423. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Alagoz T, Buller RE, Berman M, Anderson B,
Manetta A and DiSaia P: What is a normal CA125 level? Gynecol
Oncol. 53:93–97. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Taylor PT and Haverstick D: Re: New
guidelines to evaluate the response to treatment in solid tumors
(ovarian cancer). J Natl Cancer Inst. 97:151–152. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rustin GJ, Quinn M, Thigpen T, du Bois A,
Pujade-Lauraine E, Jakobsen A, Eisenhauer E, Sagae S, Greven K,
Vergote I, et al: Re: New guidelines to evaluate the response to
treatment in solid tumors (ovarian cancer). J Natl Cancer Inst.
96:487–488. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ritchie ME, Phipson B, Wu D, Hu Y, Law CW,
Shi W and Smyth GK: limma powers differential expression analyses
for RNA-sequencing and microarray studies. Nucleic Acids Res.
43:e472015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
McGuire WP, Hoskins WJ, Brady MF, Kucera
PR, Partridge EE, Look KY, Clarke-Pearson DL and Davidson M:
Cyclophosphamide and cisplatin compared with paclitaxel and
cisplatin in patients with stage III and stage IV ovarian cancer. N
Engl J Med. 334:1–6. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Neijt JP, Engelholm SA, Tuxen MK, Sorensen
PG, Hansen M, Sessa C, de Swart CA, Hirsch FR, Lund B and van
Houwelingen HC: Exploratory phase III study of paclitaxel and
cisplatin versus paclitaxel and carboplatin in advanced ovarian
cancer. J Clin Oncol. 18:3084–3092. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Xie C, Mao X, Huang J, Ding Y, Wu J, Dong
S, Kong L, Gao G, Li CY and Wei L: Kobas 2.0: A web server for
annotation and identification of enriched pathways and diseases.
Nucleic Acids Res 39 (Web Server Issue). W316–W322. 2011.
View Article : Google Scholar
|
|
26
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using realtime quantitative PCR and
the 2−ΔΔCT method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kurman RJ, Carcangiu ML, Herrington CS and
Young RH: WHO Classification of Tumours of Female Reproductive
Organs. Vol 6. 4th edition. WHO Press. 2014.
|
|
28
|
Malpica A, Deavers MT, Lu K, Bodurka DC,
Atkinson EN, Gershenson DM and Silva EG: Grading ovarian serous
carcinoma using a two-tier system. Am J Surg Pathol. 28:496–504.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Alvarenga AW, Coutinho-Camillo CM,
Rodrigues BR, Rocha RM, Torres LF, Martins VR, da Cunha IW and Hajj
GN: A comparison between manual and automated evaluations of tissue
microarray patterns of protein expression. J Histochem Cytochem.
61:272–282. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Harrell FE Jr, Lee KL and Mark DB:
Tutorial in biostatistics mul-tivariable prognostic models: Issues
in developing models, evaluating assumptions and adequacy, and
measuring and re-ducing errors. Stat Med. 15:361–387. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ozols RF, Schwartz PE and Eifel PJ:
Relapsed ovarian cancer: Challenges and management strategies for a
chronic disease. Oncologist. 7 (Suppl 5):20–28. 2002. View Article : Google Scholar
|
|
32
|
Ahmed AA, Etemadmoghadam D, Temple J,
Lynch AG, Riad M, Sharma R, Stewart C, Fereday S, Caldas C, Defazio
A, et al: Driver mutations in TP53 are ubiquitous in high
grade serous carcinoma of the ovary. J Pathol. 221:49–56. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wallstrom G, Anderson KS and LaBaer J:
Biomarker discovery for heterogeneous diseases. Cancer Epidemiol
Biomarkers Prev. 22:747–755. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Petrillo M, Nero C, Amadio G, Gallo D,
Fagotti A and Scambia G: Targeting the hallmarks of ovarian cancer:
The big picture. Gynecol Oncol. 142:176–183. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang D and Dubois RN: Prostaglandins and
cancer. Gut. 55:115–122. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang MT, Honn KV and Nie D:
Cyclooxygenases, prostanoids, and tumour progression. Cancer
Metastasis Rev. 26:525–534. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Greenhough A, Smartt HJ, Moore AE, Roberts
HR, Williams AC, Paraskeva C and Kaidi A: The COX-2/PGE2 pathway:
Key roles in the hallmarks of cancer and adaptation to the tumour
microenvironment. Carcinogenesis. 30:377–386. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kim J, Yang P, Suraokar M, Sabichi AL,
Llansa ND, Mendoza G, Subbarayan V, Logothetis CJ, Newman RA,
Lippman SM, et al: Suppression of prostate tumor cell growth by
stromal cell prostaglandin D synthase-derived products. Cancer Res.
65:6189–6198. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kinzler KW and Vogelstein B: Landscaping
the cancer terrain. Science. 280:1036–1037. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Issemann I and Green S: Activation of a
member of the steroid hormone receptor superfamily by peroxisome
proliferators. Nature. 347:645–650. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Rossi A, Kapahi P, Natoli G, Takahashi T,
Chen Y, Karin M and Santoro MG: Anti-inflammatory cyclopentenone
prostaglandins are direct inhibitors of IkappaB kinase. Nature.
403:103–108. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang C, Fu M, D'Amico M, Albanese C, Zhou
JN, Brownlee M, Lisanti MP, Chatterjee VK, Lazar MA and Pestell RG:
Inhibition of cellular proliferation through IkappaB
kinase-independent and peroxisome proliferator-activated receptor
gamma-dependent repression of cyclin D1. Mol Cell Biol.
21:3057–3070. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
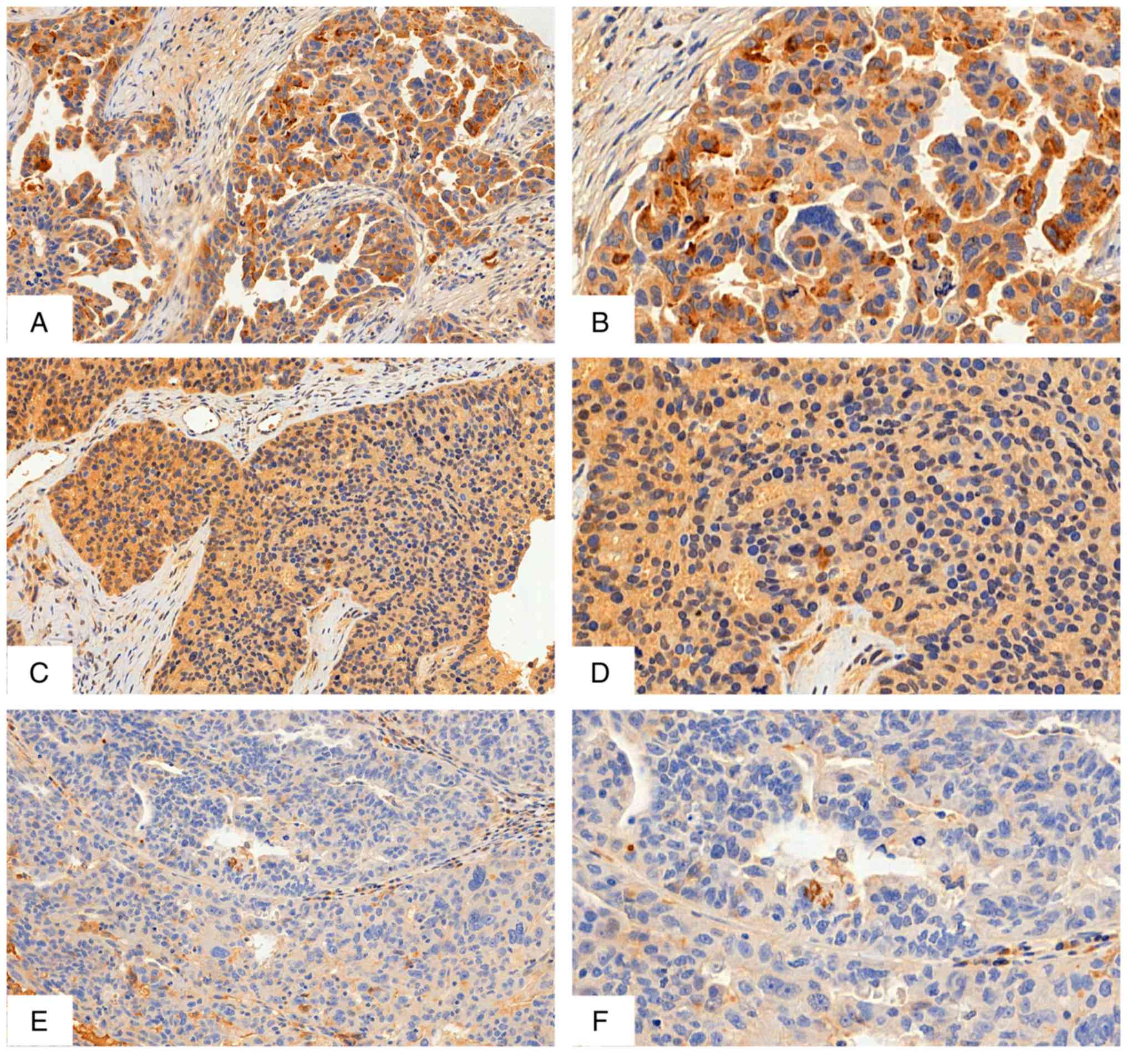
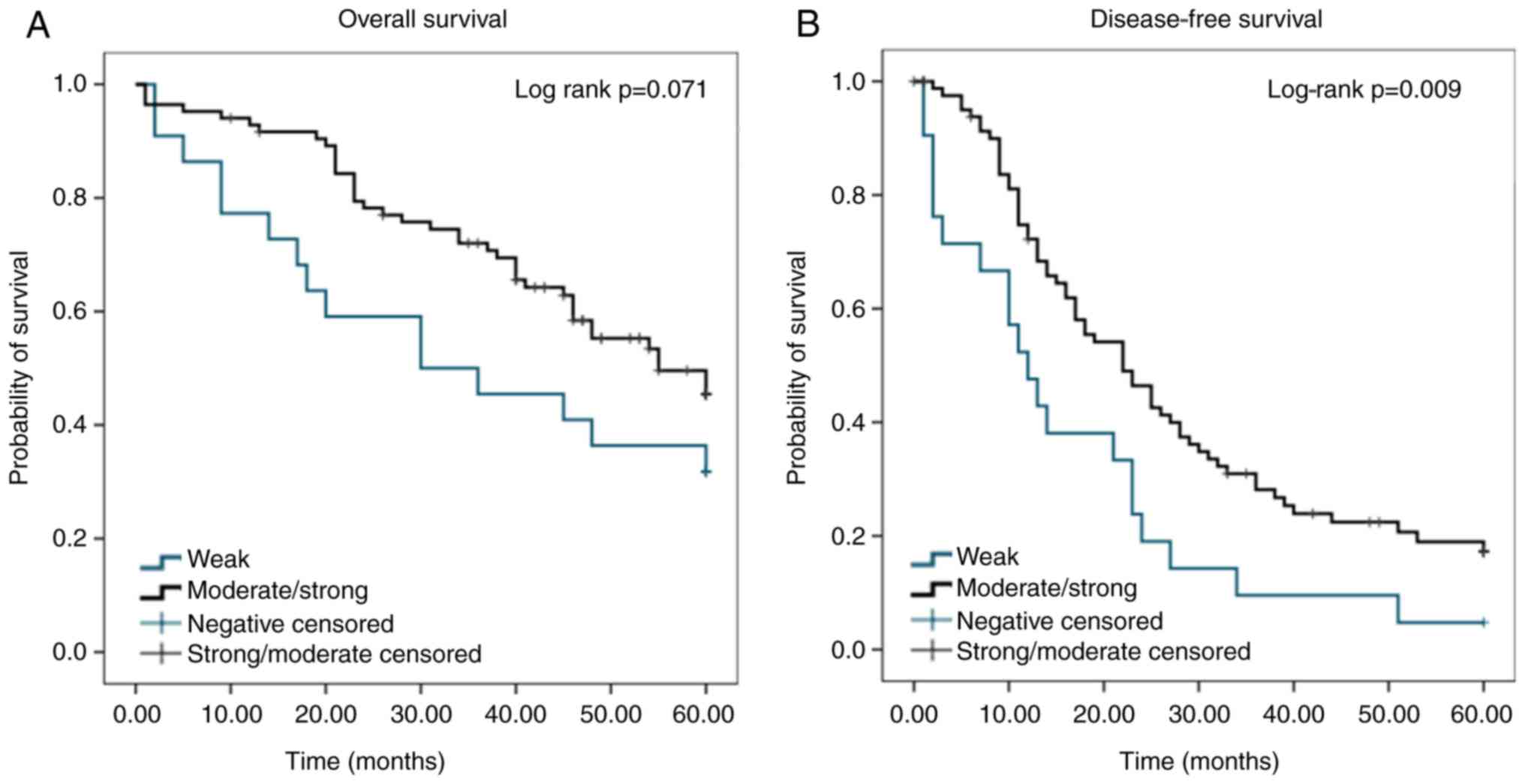
Su B, Guan M, Zhao R and Lu Y: Expression
of prostaglandin D synthase in ovarian cancer. Clin Chem Lab Med.
39:1198–1203. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
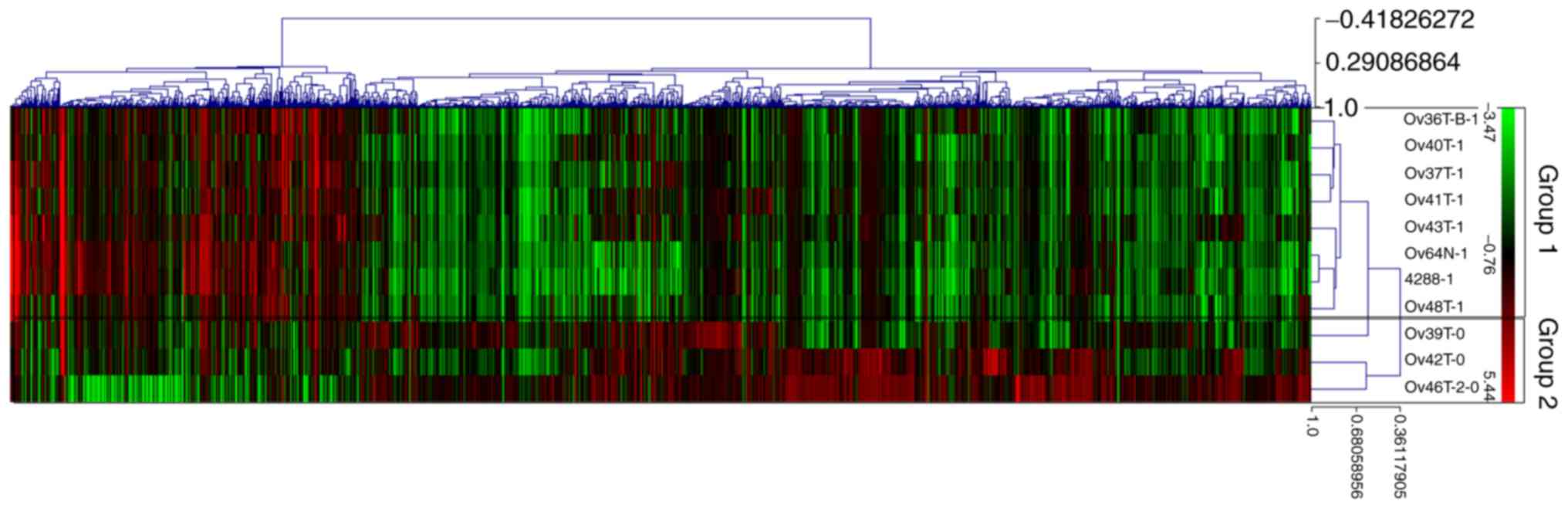
Bachvarov D, L'esperance S, Popa I,
Bachvarova M, Plante M and Têtu B: Gene expression patterns of
chemoresistant and chemosensitive serous epithelial ovarian tumors
with possible predictive value in response to initial chemotherapy.
Int J Oncol. 29:919–933. 2006.PubMed/NCBI
|
|
46
|
Vogel C and Marcotte EM: Insights into the
regulation of protein abundance from proteomic and transcriptomic
analyses. Nat Rev Genet. 13:227–232. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Yu ZW, Zhong LP, Ji T, Zhang P, Chen WT
and Zhang CP: MicroRNAs contribute to the chemoresistance of
cisplatin in tongue squamous cell carcinoma lines. Oral Oncol.
46:317–322. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
de Jong E, Winkel P, Poelstra K and
Prakash J: Anticancer effects of 15d-prostaglandin-J2 in
wild-type and doxorubicin-resistant ovarian cancer cells: Novel
actions on SIRT1 and HDAC. PLoS One. 6:e251922011. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Goossens N, Nakagawa S, Sun X and Hoshida
Y: Cancer biomarker discovery and validation. Transl Cancer Res.
4:256–269. 2015.PubMed/NCBI
|