Introduction
Hepatocellular carcinoma (HCC) is the fifth most
common malignancy worldwide and the third most frequent cause of
global cancer-associated mortality (1–3).
Curative therapies for HCC include surgical resection and liver
transplantation; however, <30% of patients are candidates for
curative surgery (4,5). HCC is a highly aggressive tumor that
is characterized by high-grade malignancy, early metastasis,
infiltrating growth and a poor prognosis, even following liver
transplantation (6–8). Furthermore, treatment options using
systemic therapies are very limited. In general, HCC does not
respond to classical chemotherapeutics. Due to the extensive
molecular and genotypic heterogeneity of HCC, suitable biomarkers
for surveillance, diagnosis and prediction of prognosis in patients
with HCC remain to be identified, and are currently not ready for
introduction into clinical practice. Therefore, novel markers and
therapeutic targets are urgently required to develop effective
methods for early detection and prognosis of HCC, as well as for
therapies to treat advanced HCC.
Transarterial chemoembolization (TACE) is a
non-curative, but useful, palliative treatment option for
nonsurgical patients with preserved liver function and large or
multinodular non-invasive HCC (9).
It is also used as a bridging strategy to limit tumor growth during
the waiting times for liver transplantation (10,11).
Intra-arterial infusion of a chemotherapeutic substance with a
viscous emulsion, followed by the embolization of blood vessels
with an embolic agent, results in a cytotoxic effect with ischemia
(12). TACE has been reported to be
effective in downstaging of cancer, leading to improved overall and
recurrence-free survival following liver transplantation (13–16).
Repeatedly performed TACE has been reported to be capable of
selecting biologically favorable tumors and appears to reflect
biological properties, such as tumor aggressiveness (17). At present, little is known regarding
the molecular mechanisms that are induced during TACE treatment,
and TACE-induced prognostic markers may influence the prognosis of
HCC following liver transplantation. The identification of useful
predictive markers for the prognosis of TACE therapy may be helpful
in improving local tumor control, in order to better select
patients suitable for liver transplantation, to reduce recurrence,
and to prolong survival and quality of life for patients who remain
unsuitable for resection (12).
The insulin-like growth factor (IGF) system is
physiologically involved in the regulation of cellular
proliferation and apoptosis, and is associated with tissue growth
(18). The IGF axis is dysregulated
in numerous types of cancer and is considered a key driver in
hepatocarcinogenesis (19). Whereas
the role of the ligands IGF1 and IGF2, as well as the IGF1 receptor
(IGF1R) signaling pathway in hepatocarcinogenesis, has been the
focus of numerous studies (20–26),
few data exist regarding the specific role of the mannose
6-phosphate/IGF2 receptor (IGF2R, CD222). Many types of human
cancer, including colorectal carcinoma (27), breast cancer (28) or HCC (29), are associated with a reduced IGF2R
function. IGF2R is a transmembrane protein, which is predominantly
located in the Golgi apparatus and pre-endosomal compartments
(90%), and to a lesser extent at the cell surface (10%). It is
ubiquitously expressed in tissues, but also present in the
circulation (30,31). IGF2R binds IGF2, as well as proteins
bearing mannose 6-phosphate residues (e.g. lysosomal proteins) at
distinct sites on the receptor (32). The receptor participates in the
internalization and lysosomal degradation of IGF2, a mitogen that
normally acts through IGF1R to stimulate cell proliferation
(33). As a cell surface protein,
IGF2R lacks a tyrosine kinase domain, and was therefore originally
assumed to solely act as a scavenger receptor lacking intrinsic
signaling (34). Nonetheless, a few
studies concerning cardiac pathophysiology (35–37)
have indicated that IGF2R contains a putative G-protein binding
site within its cytoplasmic domain. Therefore, IGF2R may not only
function in degradation of IGF2, but may also trigger an
intracellular signaling pathway through coupling with
G-protein-coupled receptors. IGF2R also activates the latent
precursor of transforming growth factor-β1 (TGF-β1), which is a
potent growth inhibitor for several cell types (38,39).
The IGF2R gene is located on chromosome 6q26
in a large 140 kb locus, and is comprised of 48 exons and introns.
There is considerable evidence supporting the importance of a
genetic predisposition in patients with HCC (40). Numerous single nucleotide
polymorphisms (SNPs) have been identified; however, their impact on
HCC has yet to be fully elucidated (41). Notably, the SNP rs629849 (transition
G → A at position +1,619) in exon 34, which is localized in the
IGF2-binding domain, has been reported to be implicated in
IGF2-dependent growth (42).
Furthermore, the present study analyzed the role of the SNP
rs642588 (transition C → T), which is located in the CTCF-binding
site of the IGF2R promoter.
These previous findings have suggested that IGF2R
possesses various growth inhibitory functions and is therefore
considered a candidate tumor suppressor (43). The present study aimed to elucidate
the effects of IGF2R expression on survival and tumor
recurrence in patients with HCC. The expression levels of
IGF2R were measured in HCC and corresponding non-neoplastic
tumor-surrounding tissue (TST), and its association with
clinicopathological parameters and outcomes was determined. To the
best our knowledge, it is currently unknown as to whether the
expression and regulation of IGF2R is altered following
TACE. Therefore, the effects of TACE pretreatment on IGF2R
mRNA expression were investigated. The possible effects of
IGF2R gene polymorphisms (rs629849 and rs642588), and their
combination, on susceptibility and on the clinicopathological
features of HCC were also analyzed.
Materials and methods
Patient tissue samples
HCC tumor samples and corresponding TST were
obtained from 92 patients undergoing tumor resection (n=66) or
liver transplantation (n=26) between March 2007 and December 2013
at the Department of Hepatobiliary and Transplantation Surgery and
the Department of General and Abdominal Surgery (Johannes Gutenberg
University Mainz, Mainz, Germany). A total of 26 patients underwent
TACE prior to surgery. TACE was performed at 6-week intervals using
mitomycin and lipiodol. Written informed consent was obtained from
each patient, according to the agreement on transfer and scientific
use of excess material of the University Medicine of the Johannes
Gutenberg University Mainz. The present study followed the ethical
guidelines of the Declaration of Helsinki and was approved by the
Ethics Committee of the State of Rhineland-Palatinate Medical Board
[Number 847.243.17 (11077)]. Liver tissues were immediately flash
frozen following resection and were stored in liquid nitrogen prior
to analysis. All cases of HCC were diagnosed or confirmed by
histology. Healthy normal and non-cirrhotic control liver tissues
(n=31) were obtained from patients undergoing liver surgery for
hepatic metastases following colon or breast carcinoma (male, n=21;
female, n=10). The median age of the control patients was 63 years
old (range, 47–85 years) at the time of surgery.
Tissue homogenization, RNA isolation
and reverse transcription-polymerase chain reaction (RT-PCR)
analysis
Prior to RNA extraction, 20 mg tissue samples were
homogenized using a Precellys 24 homogenizer (Bertin Instruments,
Montigny-le-Bretonneux, France) in CK14 tubes at 5,100 rpm for 2×20
sec. RNA was extracted from tissue samples using the PeqGOLD Total
RNA kit (VWR International GmbH, Darmstadt, Germany). cDNA was
prepared from 1 µg total RNA (20 µl total volume) using the
qScript™ XLT cDNA SuperMix (Quantabio, Beverly, MA, USA). All
aforementioned kits were used according to the manufacturers'
protocols. Semi-quantitative analysis of IGF2R transcripts
was performed by RT-PCR. The Absolute Blue QPCR SYBR-Green Mix kit
(Thermo Fisher Scientific, Inc., Waltham MA, USA) and the following
primers were used: GAPDH, forward 5′-TTTTGCGTCGCCAGCCGAG-3′,
reverse 5′-ACCAGGCGCCCAATACGACC-3′; and IGF2R, HS_IGF2R_1_SG
Quantitect Primer Assay (Qiagen GmbH, Hilden, Germany). Cycling
conditions were as follows: Initial denaturation at 15 min for
95°C, followed by 45 cycles of denaturation at 95°C for 10 sec,
annealing at 66°C for GAPDH and 55°C for IGF2R for 30
sec, and elongation at 72°C for 30 sec. Samples were run on a
LightCycler® 480 Real-Time PCR system (Roche Diagnostics
GmbH, Mannheim, Germany). PCR products were analyzed using the
QIAxcel capillary gel electrophoresis system (Qiagen GmbH). The
relative expression levels of IGF2R mRNA in HCC and TST
samples were calculated by normalization to GAPDH gene
expression using LightCycler® 480 Software Release 1.5.0
(Roche Diagnostics GmbH). For examination of IGF2R mRNA
regulation, relative IGF2R mRNA expression in HCC tissues
was compared with relative IGF2R mRNA expression in the
corresponding TST.
Immunohistochemistry
Immunohistochemical staining was performed on
formalin-fixed, paraffin-embedded tissue sections (size, 4 µm). For
fixation, the tissue sections were incubated with 4% formalin at
room temperature for 48 h. Following deparaffinization and
rehydration, endogenous peroxidase activity was inhibited with 4%
hydrogen peroxide in methanol for 30 min at room temperature. For
antigen retrieval, tissue sections were incubated with 10 mM
citrate buffer (pH 6.0) for 20 min in a steamer. Cells were
permeabilized with 2% saponin (cat. no. 47036; Sigma-Aldrich; Merck
KGaA, Darmstadt, Germany) in PBS for 20 min at room temperature.
For blocking of non-specific antibody binding, tissues were
incubated for 30 min with protein blocking buffer [5% normal goat
serum (Dako; Agilent Technologies, Inc., Santa Clara, CA, USA),
0.2% Triton X-100, 2% bovine serum albumin (BSA; SERVA
Electrophoresis GmbH, Heidelberg, Germany)]. The following primary
antibody was used for immunohistochemistry: Rabbit polyclonal
anti-human IGF2R antibody (cat. no. NBP1-19465; Novus Biologicals,
LLC, Littleton, CO, USA), which was used at a dilution of 1:100,
was used to incubate the sections overnight at 4°C in PBS (2%
saponin, 5% BSA, 5% normal serum). For control sections, the
specific primary antibody was omitted. The following day, sections
were washed three times with Tris-buffered saline-0.5% Tween-20 and
incubated for 20 min with Pierce Peroxidase Suppressor (Thermo
Fisher Scientific, Inc.). After washing, sections were incubated
for 1 h at room temperature with a secondary biotinylated goat
anti-rabbit antibody (cat. no. E043201-8; Dako; Agilent
Technologies, Inc.) at a dilution of 1:100, and were then treated
with the avidin-biotin-peroxidase complex-based Vectastain Elite
ABC kit (Vector Laboratories, Inc., Burlingame, CA, USA). Following
incubation with horseradish peroxidase-conjugated streptavidin
(cat. no. P039701-2; Dako; Agilent Technologies, Inc.) at a
dilution of 1:300, tissues were stained at room temperature for 10
min with the liquid DAB+ Substrate Chromogen system (cat. no.
K346711-2; Dako; Agilent Technologies, Inc.), according to the
manufacturer's protocol. Counterstaining was performed with Gill's
hematoxylin solution (Polysciences Inc., Warrington, PA, USA) at
room temperature for 7 min and slides were mounted for examination
under a light microscope.
Tissue homogenization and DNA
extraction
Homogenization of 5–9 mg fresh frozen tissue blocks
was conducted using a Precellys 24 homogenizer (Bertin Instruments)
in CK14 tubes at 5,100 rpm for 2×20 sec following Proteinase K
(Qiagen GmbH) digestion at 56°C for 3 h. Genomic DNA was extracted
using the QIAamp DNA Micro kit (Qiagen GmbH), according to the
manufacturer's protocol, and was quantified by UV absorption via
NanoVue (GE Healthcare Life Sciences, Little Chalfont, UK).
PCR and pyrosequencing (PSQ)
Primer sets with one 5′-biotinylated primer were
used for the amplification of SNP regions. All primers used for PCR
and sequencing were generated using PyroMark Assay Design Software
2.0 (Qiagen GmbH). PCR was performed using the PyroMark PCR kit
(Qiagen GmbH), according to the manufacturer's protocol. The
following primers were used: rs629849, forward
5′-biotin-AAATCCGGCCTGAGCTATAAG-3′, reverse
5′-AGCATGAGTCTTGAGCAATTACTG-3′; and rs642588, forward
5′-biotin-CACATGGGGATTATGGGAACT-3′ and reverse
5′-AGCATGAGTCTTGAGCAATTACTG-3′. PCR reactions were run with 0.15 µM
primer under the following thermal cycling conditions: 95°C for 15
min, followed by 45 cycles at 94°C for 30 sec, at the optimized
primer-specific annealing temperature (60°C) for 30 sec and at 72°C
for 30 sec, followed by a final extension step at 72°C for 10 min.
Amplification of the correct DNA product was confirmed by
high-resolution capillary electrophoresis using a QIAxcel Advanced
system (Qiagen GmbH). Subsequently, a standard PSQ sample
preparation protocol was applied: Streptavidin beads (1.5 µl; GE
Healthcare Life Sciences), 40 µl PyroMark binding buffer (Qiagen
GmbH), 20 µl PCR product and 18.5 µl water were mixed and incubated
for 10 min at room temperature with agitation (1,200 rpm).
According to the manufacturer's recommendations, amplicons were
denaturated using PyroMark denaturation solution (Qiagen GmbH),
washed with PyroMark Wash buffer (Qiagen GmbH) and added to 20 µl
annealing buffer containing 0.375 µM sequencing primer (rs629849:
5′-TGGGCCTATTGGTTG-3′; rs642588: 5′-AGCAATTACTGATTAATATG-3′) using
the PyroMark Q24 Vacuum Workstation (Qiagen GmbH) at room
temperature. Primer annealing was performed by incubating the
samples at 80°C for 5 min and then cooling to room temperature
prior to PSQ. PyroMark Q24 Advanced Reagents (Qiagen GmbH) were
used for the PSQ reaction, and the signal was analyzed using the
Pyromark Q24 system (Qiagen GmbH). Genotype analysis of SNPs was
conducted using PyroMark Q24 Advanced Software version 3.0.0
(Qiagen GmbH).
Statistical analysis
Data management and all statistical analyses were
performed using SPSS program (version 23.0; IBM Corp., Armonk, NY,
USA). For categorical variables, between-group differences were
analyzed by χ2 test or Fisher's exact test. Continuous
data were expressed as the median and range. Two independent groups
were compared using the Mann-Whitney U test with subsequent
Bonferroni correction. For the comparison of multiple independent
samples, the Kruskal-Wallis test and Bonferroni correction was
performed. Overall survival rates were calculated using the
Kaplan-Meier method and were compared using the log-rank test. The
distributions of genotypic frequencies between cases and controls
were analyzed by χ2 test or Fisher's exact test. Odds
ratio (ORs) and 95% confidence intervals (CIs) were calculated.
Univariate analysis was performed to assess the association between
genotype frequencies and the clinicopathological features of HCC.
P≤0.05 (two-sided) was considered to indicate a statistically
significant difference.
Results
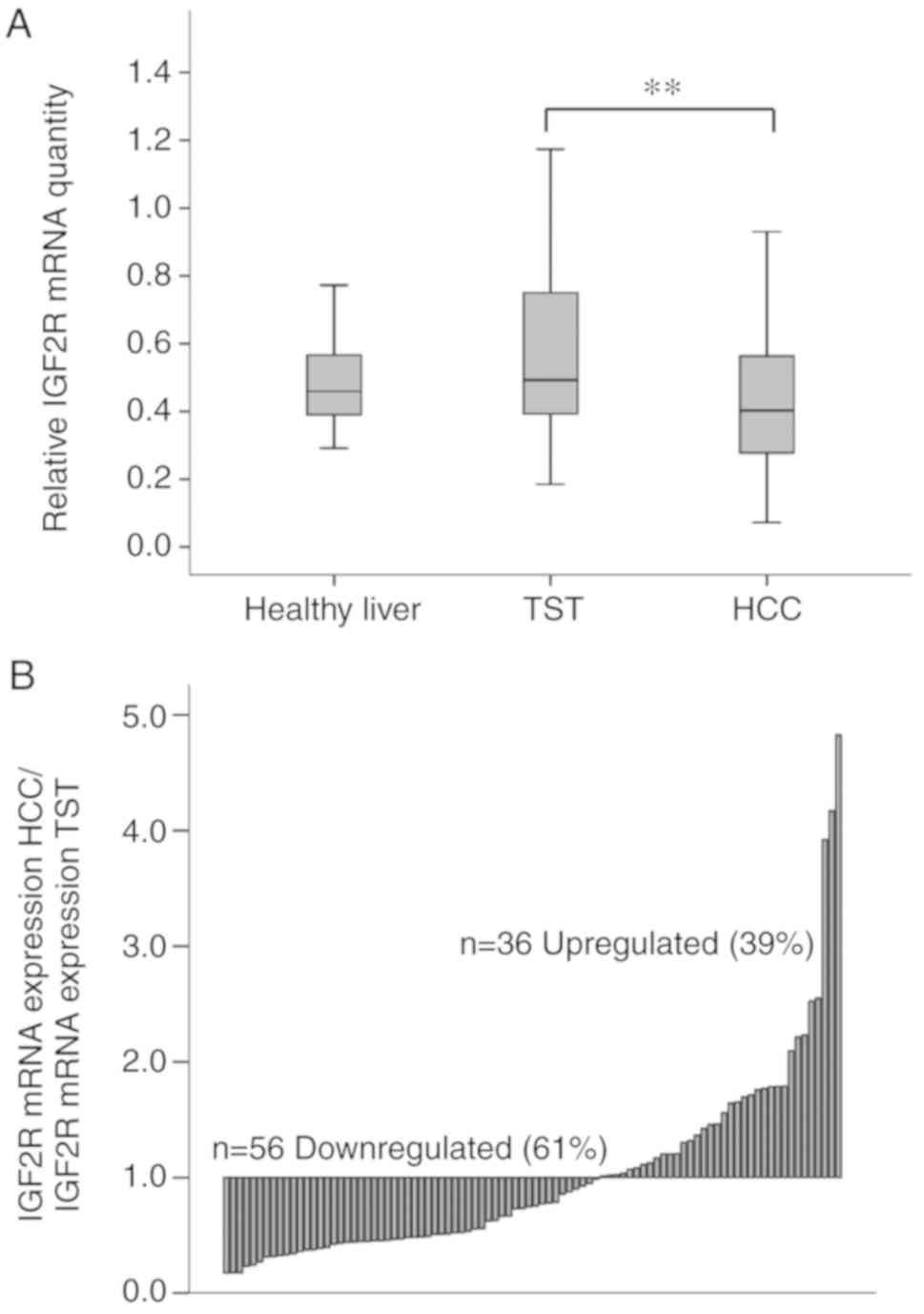
IGF2R mRNA expression in HCC
To analyze the role of IGF2R in HCC, the
present study detected the mRNA expression levels of IGF2R
in HCC tissue and corresponding non-neoplastic TST (n=92).
Semi-quantitative RT-PCR results demonstrated significant
differences in IGF2R mRNA expression between HCC and TST
(Fig. 1A). IGF2R mRNA was
highly expressed in TST and was significantly downregulated in
cancerous tissues (P=0.004). In HCC tissues, median IGF2R
mRNA expression was reduced by 20.4% compared to that in the
corresponding TST. Normal liver served as a control for the
expression of IGF2R mRNA. TST exhibited comparable
IGF2R mRNA expression to normal healthy liver tissue (n=31;
P=1.000). In the present cohort, IGF2R mRNA was
downregulated in 61% of HCC samples (n=56), whereas IGF2R
mRNA expression was upregulated in 39% (n=36) (Fig. 1B). Details of clinical and
pathological characteristics of patients and tumors are summarized
in Table I, according to World
Health Organization specifications (44).
 | Table I.Patients and tumor
characteristics. |
Table I.
Patients and tumor
characteristics.
|
Characteristics | Value |
|---|
| Total number,
n | 92 |
| Median follow-up,
days (range) | 796 (4–2,615) |
| Median
recurrence-free survival, days (range) | 529 (4–2,615) |
| Male/female, n | 79/13 |
| Median age, years
(range) | 68 (35–86) |
| Nodules
(1–3/multiple), n | 75/17 |
| Tumor diameter
(<3 cm/≥3 cm), n | 19/73 |
| Median tumor
diameter, cm (range) | 5.0 (1.0–30) |
| T-classification
(T1/T2/T3/T4), n | 42/28/21/1 |
| Grading
(G1/G2/G3/Gxa), n | 14/60/13/5 |
| AFP
(>100/<100), nb | 15/71 |
| Angioinvasion
(yes/no), nc | 24/67 |
| Cirrhosis (yes/no),
n | 54/38 |
| Child-Pugh grade
(A/B/C), n | 42/6/6 |
| Cirrhosis
(viral/non-viral), n | 27/27 |
| Pretreatment with
chemoembolization, n | 26 |
| Liver
transplantation/resection, n | 26/66 |
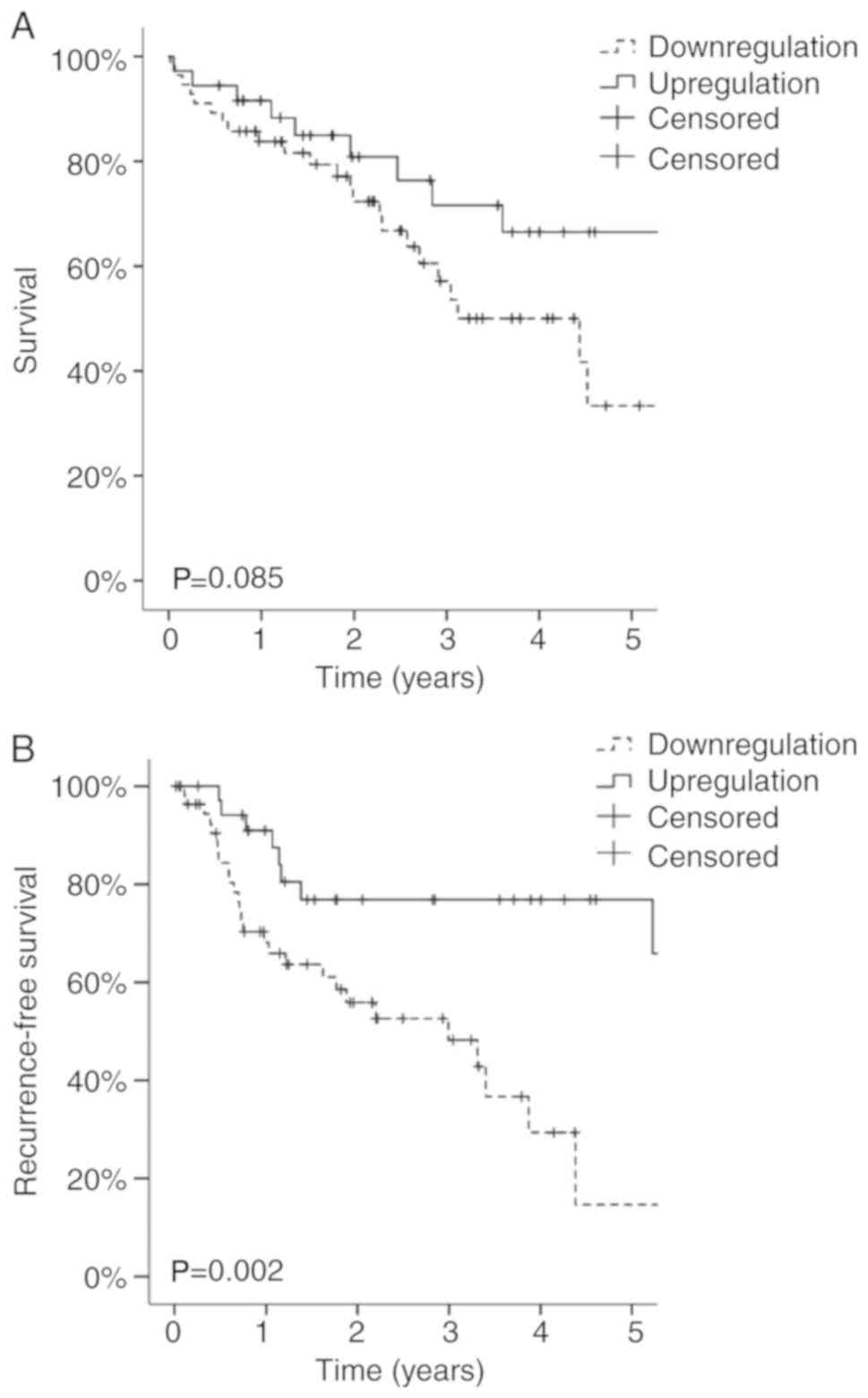
Patient survival and tumor recurrence
in patients
According to the RT-PCR results, the patients were
divided into two groups: i) Patients with HCC that exhibited
downregulated IGF2R mRNA expression (IGF2R mRNA
expression in HCC/IGF2R mRNA expression in TST <1; n=56),
and ii) patients with HCC that exhibited upregulated IGF2R
mRNA expression in HCC (IGF2R mRNA expression in
HCC/IGF2R mRNA expression in TST ≥1; n=36).
Overall 5-year survival of the patients with
downregulated IGF2R mRNA tumor expression was 34%;
conversely, it was 66% for patients with upregulated IGF2R
mRNA tumor expression. Despite this pronounced difference,
statistical significance could not be achieved (P=0.085; Fig. 2A). Significant downregulation of
IGF2R mRNA expression markedly affected the risk of tumor
recurrence within 5 years following surgery (Fig. 2B). Recurrence-free 5-year survival
was 16% in patients with downregulated IGF2R mRNA
expression, whereas it was 76% in patients with upregulated
IGF2R mRNA expression (P=0.002).
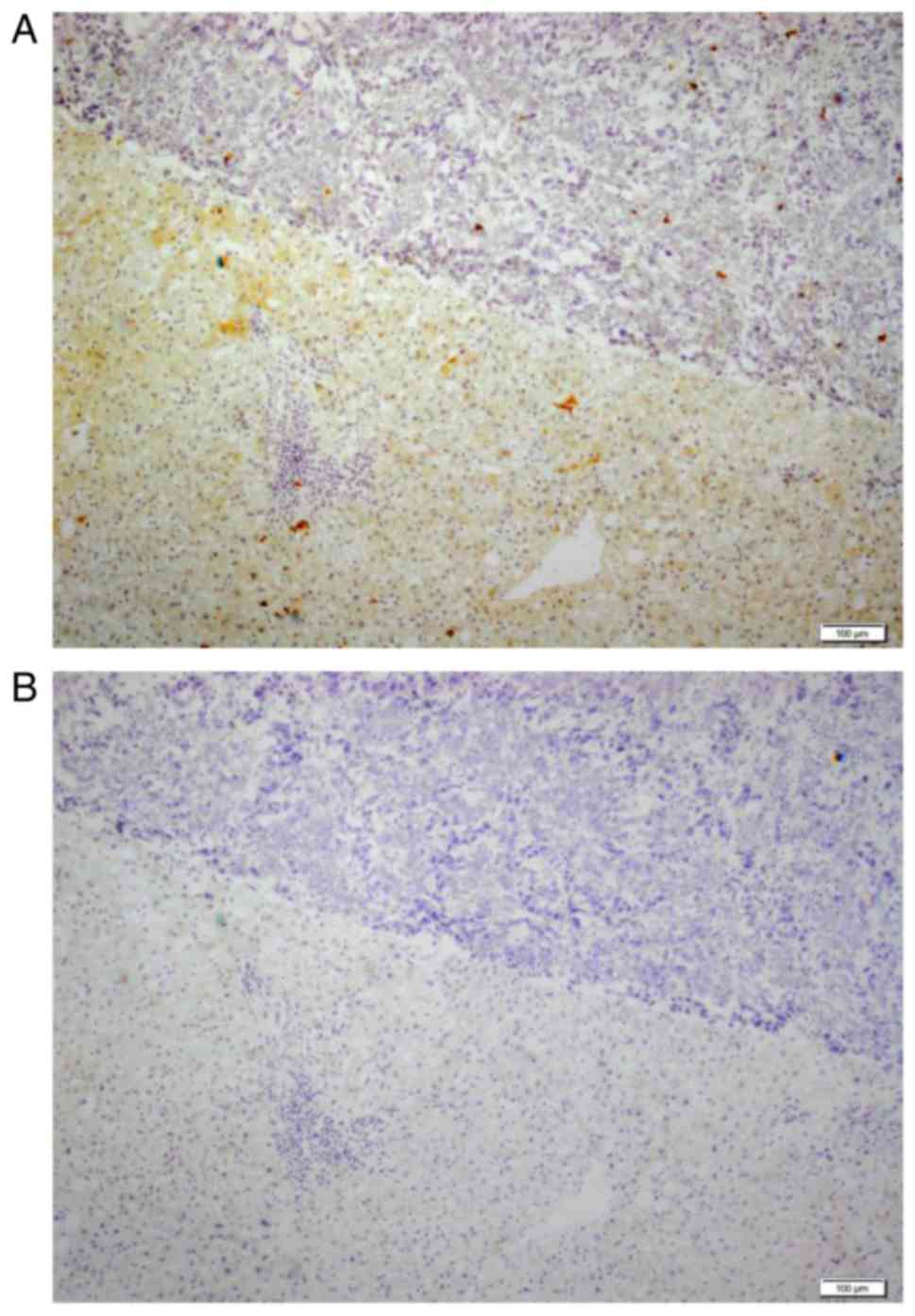
Protein expression of IGF2R, as
determined by immunohistochemistry
To identify the localization of IGF2R expression in
tumor tissue, protein expression was assessed by
immunohistochemistry. As shown in Fig.
3A, IGF2R staining was detected at the tumor border in HCC
tissues with downregulated IGF2R mRNA expression. In
addition, predominant IGF2R staining in hepatocytes was detected in
the non-neoplastic TST, whereas IGF2R staining was almost
completely absent in tumor tissue.
Patient and tumor characteristics in
association with IGF2R mRNA expression
Upregulation of IGF2R mRNA expression in HCC
was associated with a better recurrence-free survival (P=0.017), a
lower median age (P=0.013) and a higher occurrence of liver
cirrhosis (P=0.05) (Table II).
TACE pretreatment prior to resection or liver transplantation was
carried out more often in the group with upregulated IGF2R
mRNA tumor expression (P=0.032). IGF2R mRNA expression was
not associated with any other tumor characteristics.
 | Table II.Patient and tumor characteristics
associated with intratumoral IGF2R mRNA expression. |
Table II.
Patient and tumor characteristics
associated with intratumoral IGF2R mRNA expression.
|
| IGF2R
mRNA |
|
|---|
|
|
|
|
|---|
|
Characteristics | Downregulation
(HCC/TST <1) | Upregulation
(HCC/TST ≥1) | P-value |
|---|
| Number of patients,
n | 56 | 36 |
|
| Median follow-up,
(range) | 796 (5–2,316) | 826 (19–2,615) | 0.247 (n.s.) |
| Median
recurrence-free survival, days (range) | 445 (5–2,316) | 645 (19–2,615) | 0.017 |
| Male/female, n | 48/8 | 31/5 | 1.000 (n.s.) |
| Median age, years
(range) | 69 (35–86) | 66 (46–78) | 0.013 |
| 1–3
nodules/multiple nodules, n | 45/11 | 30/6 | n.s. (0.789) |
| Tumor diameter
(<3 cm/≥3 cm), n | 9/47 | 10/26 | n.s. (0.196) |
| Median tumor
diameter, cm (range) | 5.4 (1.0–20) | 4.5 (2.0–30) | n.s. (0.203) |
| T-classification
(T1/T2/T3/T4), n | 22/18/16/0 | 20/10/5/1 | n.s. (0.169) |
| Grading
(G1/G2/G3/Gxa), n | 9/39/7/1 | 5/21/6/4 | n.s. (0.233) |
| AFP
(>100/<100), nb | 10/41 | 5/30 | n.s. (0.577) |
| Angioinvasion
(yes/no), nc | 17/38 | 7/29 | n.s. (0.331) |
| Cirrhosis (yes/no),
n | 28/28 | 26/10 | 0.050 |
| Child-Pugh grade
(A/B/C), n | 23/2/3 | 19/4/3 | n.s. (0.614) |
| Cirrhosis
(viral/non-viral), n | 10/18 | 13/13 | n.s. (0.409) |
| Pretreatment with
chemoembolization (yes/no), no | 11/45 | 15/21 | 0.032 |
| Liver
transplantation/resection, n | 11/45 | 15/21 | 0.032 |
Patient and tumor characteristics in
association with TACE pretreatment
As shown in Table I,
26 patients in the present cohort were pretreated with TACE prior
to liver transplantation or resection, whereas 66 patients did not
receive any TACE pretreatment prior to surgery.
The present study analyzed the associations between
patient and tumor characteristics, and preoperative TACE treatment;
significant differences are presented in Table III. Notably, TACE-pretreated
patients exhibited a significantly longer median follow-up time
following surgery (P=0.023) and a prolonged median recurrence-free
survival time (P=0.002). Furthermore, patients receiving TACE prior
to surgery displayed less advanced HCC stages, since
TACE-pretreated HCCs presented with smaller tumor diameters
(P<0.001), with less advanced T-stage tumors (P=0.034) and with
more well differentiated tumors (P<0.001). These findings
coincided with a significantly higher expression of IGF2R
mRNA expression in the tumor tissues of TACE-pretreated patients
(P=0.028; Table III).
 | Table III.Patient and tumor characteristics
associated with preoperative TACE pretreatment. |
Table III.
Patient and tumor characteristics
associated with preoperative TACE pretreatment.
| Characteristic | No TACE | TACE | P-value |
|---|
| Number of patients,
n | 66 | 26 |
|
| Median follow-up,
days (range) | 724 (5–2,588) | 1,198
(85–2,615) | 0.023 |
| Median
recurrence-free survival, days (range) | 418 (5–25,88) | 1,127
(85–2,615) | 0.002 |
| Male/female, n | 55/11 | 24/2 | n.s. (0.337) |
| Median age, years
(range) | 71 (35–86) | 60 (47–71) |
<0.001 |
| 1–3
nodules/multiple nodules, n | 56/10 | 19/7 | n.s. (0.235) |
| Tumor diameter
(<3 cm/≥3 cm), n | 6/60 | 13/13 |
<0.001 |
| Median tumor
diameter, cm (range) | 6.2 (2.0–30) | 2.4 (1.0–18) |
<0.001 |
| T-classification
(T1/T2/T3/T4), n | 31/15/19/1 | 11/13/2/0 | 0.034 |
| Grading
(G1/G2/G3/Gxa), n | 8/46/12/0 | 6/14/1/5 |
<0.001 |
| AFP
(>100/<100), nb | 47/13 | 24/2 | n.s. (0.137) |
| Angioinvasion
(yes/no), nc | 45/20 | 22/4 | n.s. (0.189) |
| Cirrhosis (yes/no),
n | 29/37 | 25/1 |
<0.001 |
| Child-Pugh grade
(A/B/C), n | 27/1/1 | 15/5/5 |
<0.001 |
| Cirrhosis
(viral/non-viral), n | 8/21 | 15/10 | n.s. (0.027) |
| Liver
transplantation/resection, n | 2/64 | 24/2 |
<0.001 |
| IGF2R mRNA
(down-/upregulated), n | 45/21 | 11/15 | 0.032 |
| Median IGF2R mRNA
expression TST | 0.53
(0.19–4.3) | 0.48
(0.22–2.7) | n.s. (0.233) |
| Median IGF2R mRNA
expression HCC | 0.36
(0.71–3.5) | 0.49
(0.14–1.1) | 0.028 |
| Median IGF2R mRNA
expression HCC/TST | 0.59
(0.17–4.8) | 1.1 (0.27–2.2) | 0.019 |
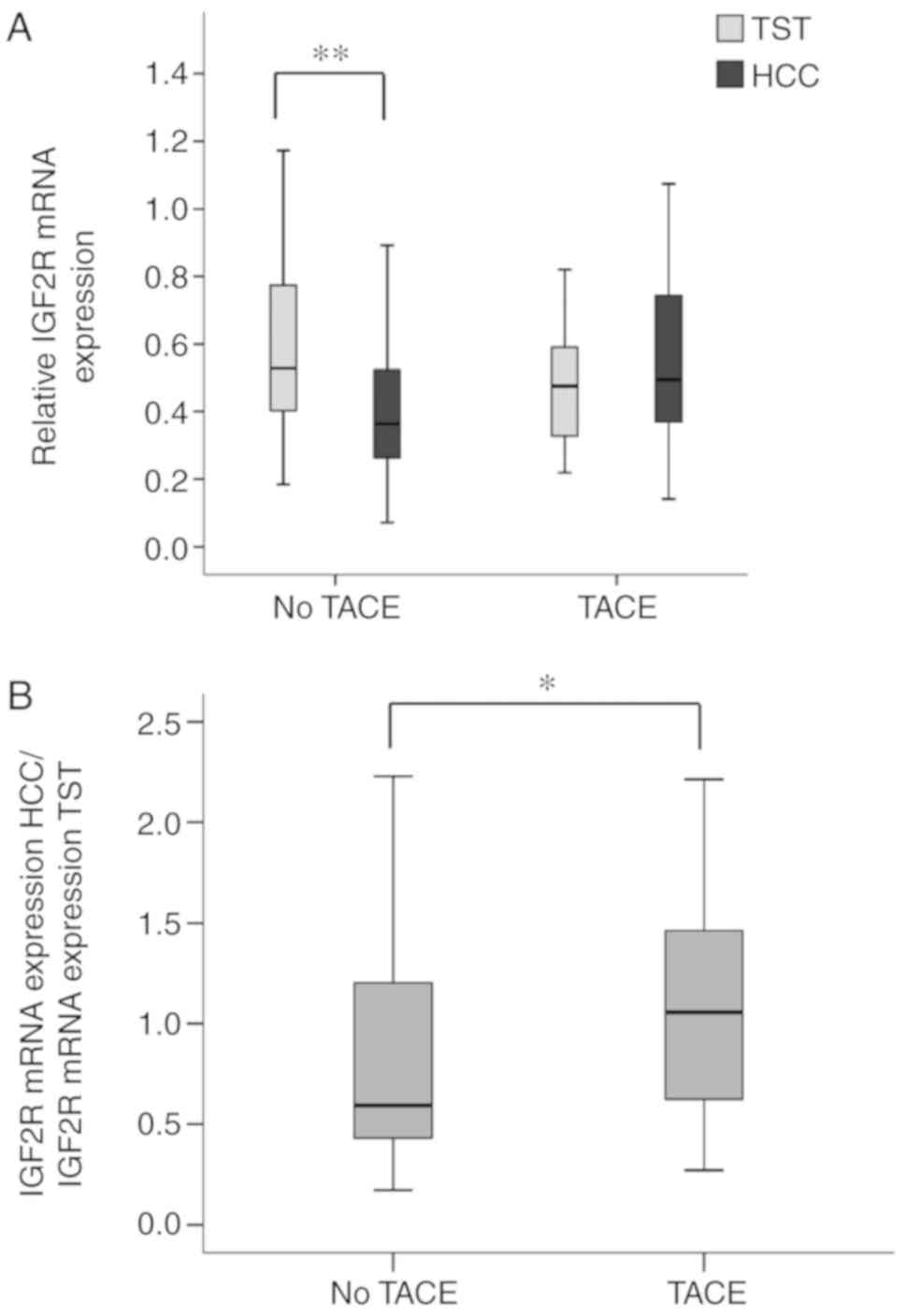
Notably, significant downregulation of IGF2R
mRNA expression in HCC tissue compared with in TST could only be
detected in the group of patients that did not receive TACE
pretreatment (P=0.004; Fig. 4A).
There was no difference between IGF2R mRNA expression in TST
and HCC samples from TACE-pretreated patients (P=1.000).
Furthermore, tumor tissues of TACE-pretreated patients exhibited a
significantly higher median IGF2R mRNA compared with
non-treated patients (P=0.019; Fig.
4B). A higher proportion of tumors in the TACE-pretreated
patient group exhibited upregulation of IGF2R mRNA
expression (P=0.032). Notably, 58% of TACE-pretreated patients
exhibited upregulated IGF2R mRNA expression in HCC compared
with only 32% of patients that did not receive TACE prior to
surgery (P=0.032; Fisher's exact test; Table IV).
 | Table IV.Association of IGF2R mRNA
expression in HCC with TACE pretreatment. |
Table IV.
Association of IGF2R mRNA
expression in HCC with TACE pretreatment.
|
| IGF2R mRNA
expression in HCC |
|
|---|
|
|
|
|
|---|
| Group | Downregulated, n
(%) | Upregulated, n
(%) | P-value |
|---|
| No TACE | 45 (68) | 21 (32) | 0.032 |
| TACE | 11 (42) | 15 (58) |
|
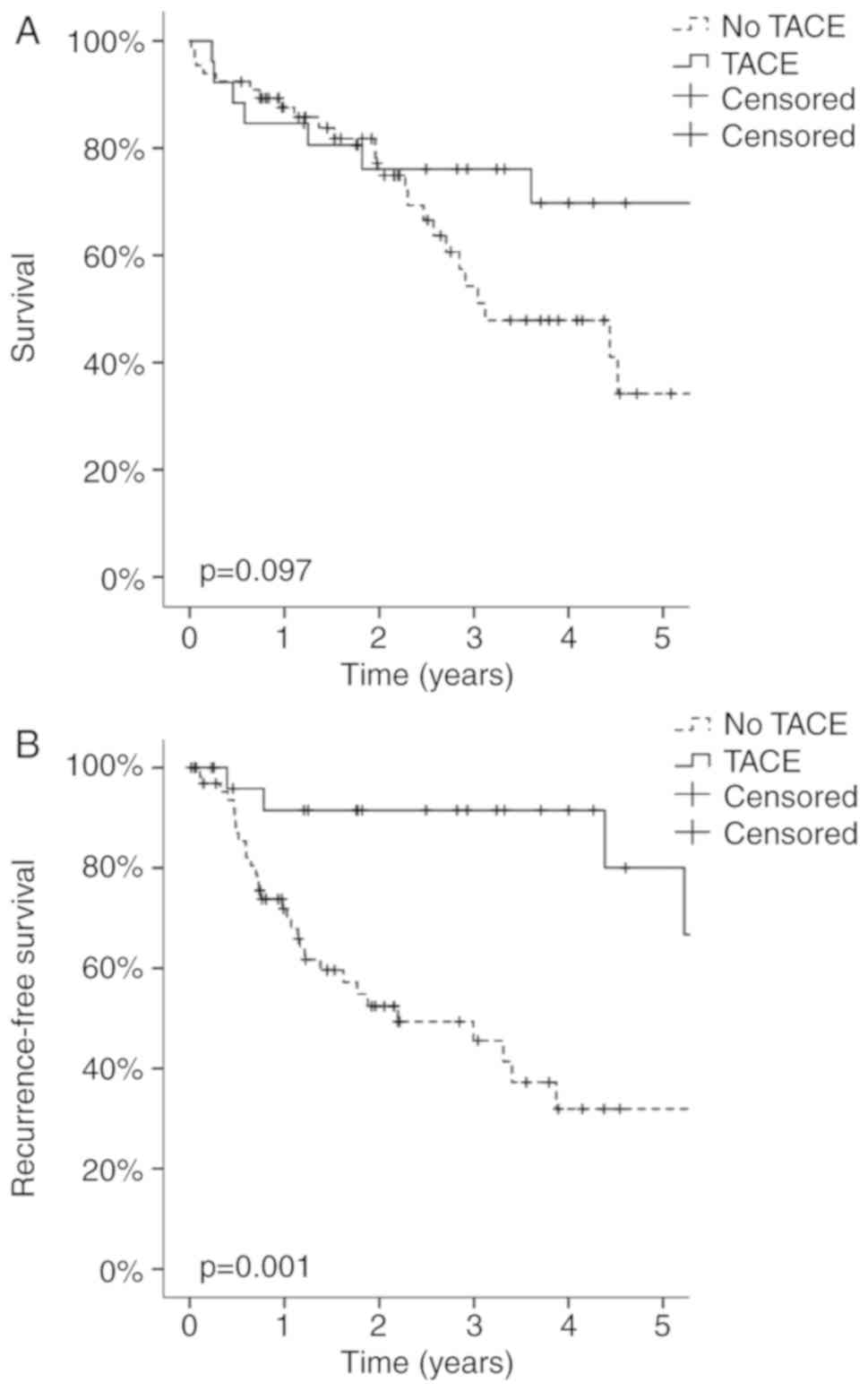
Association of TACE pretreatment with
patient survival and tumor recurrence
Patients with HCC that received TACE therapy prior
to surgery did not exhibit a significantly better overall 5-year
survival compared with non-TACE-treated patients (P=0.097; Fig. 5A). Conversely, TACE pretreatment
induced a significantly increased recurrence-free 5-year survival
in patients with HCC (P=0.001; Fig.
5B). In the TACE group, 80% of TACE-pretreated patients
exhibited recurrence-free survival 5 years after surgery, whereas
only 32% of patients who were not treated with TACE exhibited no
recurrence after 5 years.
IGF2R SNPs as a mechanism for IGF2R
mRNA expression
Two SNPs of the IGF2R gene, rs629849 and
rs642588, were investigated to analyze their association with HCC
pathological characteristics. Frequency distributions were studied
in 83 patients with HCC and were compared with those of 100 healthy
controls; 12 patients with HCC could not be analyzed due to
insufficient HCC tissue for DNA extraction. The alleles with the
highest distribution frequency for rs629849 and rs642588 were GG
(76.5%) and CC (64.5%), respectively. Differences in the
frequencies of IGF2R genotypes were not statistically
significant between patients with HCC and healthy controls (P=0.145
and P=0.068, respectively; Table
V).
 | Table V.Distribution frequency of
IGF2R genotypes in 100 healthy controls and 83 patients with
HCC. |
Table V.
Distribution frequency of
IGF2R genotypes in 100 healthy controls and 83 patients with
HCC.
| Characteristic | Control, n=100
(%) | HCC, n=83 (%) | Total, n=183
(%) | P-value |
|---|
| IGF2R
rs629849 |
| GG | 79 (79.0) | 61 (73.5) | 140 (76.5) | 0.145a |
| AG | 21 (21.0) | 19 (22.9) | 40 (21.9) |
|
| AA | 0 | 3 (3.6) | 3 (1.6) |
|
| GG | 79 (79.0) | 61 (73.5) | 140 (76.5) | 0.388b |
|
AG/AA | 21 (21.0) | 22 (26.5) | 43 (23.5) |
|
| IGF2R
rs642588 |
| CC | 60 (60.0) | 58 (69.9) | 118 (64.5) | 0.068c |
| CT | 38(38.0) | 20 (24.1) | 58 (31.7) |
|
| TT | 2 (2.0) | 5 (6.0) | 7 (3.8) |
|
| CC | 60 (60.0) | 58 (69.9) | 118 (64.5) | 0.214d |
|
CT/TT | 40 (40.0) | 25 (30.1) | 65 (35.5) |
|
To estimate the ORs and 95% CIs of each IGF2R
SNP in HCC, patients with HCC and healthy controls were classified
into two subgroups: Those with at least one mutated allele and
those with homozygous wild-type alleles. Results indicated no
significant difference in any allele frequency distribution between
patients with HCC and healthy controls (Table V). ORs with 95% CIs were estimated
for each gene polymorphism for pathological characteristics,
including T classification, grading and disease history of liver
cirrhosis. The results revealed that at least one mutated A allele
in rs629849 IGF2R gene polymorphism had a significantly
lower risk for developing non-viral liver cirrhosis (OR=0.25, 95%
CI=0.06–0.98) (Table VI).
Nevertheless, no significant difference between the IGF2R
genotype frequencies tested and any other clinicopathological
variables was observed.
 | Table VI.ORs and 95% CIs of clinical status
and IGF2R genotype frequencies in patients with
hepatocellular carcinoma (n=83). |
Table VI.
ORs and 95% CIs of clinical status
and IGF2R genotype frequencies in patients with
hepatocellular carcinoma (n=83).
|
| rs629849 | rs642588 |
|---|
|
|
|
|
|---|
|
Characteristics | GG n (%) | AG or AA n (%) | OR (95% CI) | P-value | CC n (%) | CT or TT n (%) | OR (95% CI) | P-value |
|---|
| Number of patients,
n | 61 | 22 |
|
| 58 | 25 |
| 0.21 |
| T
classification |
|
T1/T2 | 45 (73.8) | 18 (81.8) | 0.63
(0.18–2.13) | 0.57 | 43 (74.1) | 20 (80.0) | 0.72
(0.23–2.25) | 0.78 |
|
T3/T4 | 16 (26.2) | 4 (18.2) |
|
| 15 (25.9) | 5 (20.0) |
|
|
|
Gradinga |
|
G1/G2 | 51 (85.0) | 16 (84.2) | 1.06
(0.26–4.40) | 1.00 | 44 (81.5) | 23 (92.0) | 0.38
(0.08–1.90) | 0.32 |
| G3 | 9 (15.0) | 3 (15.8) |
|
| 10 (18.5) | 2 (8.0) |
|
|
| Cirrhosis |
|
Negative | 25 (41.0) | 9 (40.9) | 1.00
(0.37–2.70) | 1.00 | 25 (43.1) | 9 (36.0) | 1.35
(0.51–3.55) | 0.63 |
|
Positive | 36 (59.0) | 13 (59.1) |
|
| 33 (56.9) | 16 (64.0) |
|
|
| Cirrhosis |
|
Viral | 13 (36.1) | 9 (69.2) | 0.25
(0.06–0.98) | 0.05 | 16 (48.5) | 6 (37.5) | 1.57
(0.46–5.32) | 0.55 |
|
Non-viral | 23 (63.9) | 4 (30.8) |
|
| 17 (51.5) | 10 (62.5) |
|
|
| Child-Pugh
grade |
| A | 28 (77.8) | 11 (84.6) | 0.64
(0.12–3.48) | 0.71 | 25 (75.8) | 14 (87.5) | 0.45
(0.08–2.40) | 0.46 |
| B or
C | 8 (22.2) | 2 (15.4) |
|
| 8 (24.2) | 2 (12.5) |
|
|
| Tumor diameter
(cm) |
|
<3 | 10 (16.4) | 6 (27.3) | 0.52
(0.16–1.66) | 0.35 | 11 (19.0) | 5 (20.0) | 0.94
(0.29–3.05) | 1.00 |
| ≥3 | 51 (83.6) | 16 (72.7) |
|
| 47 (81.0) | 20 (80.0) |
|
|
| Nodules |
|
1-3 | 49 (80.3) | 19 (86.4) | 0.65
(0.16–2.54) | 0.75 | 48 (82.8) | 20 (80.0) | 1.20
(0.36–3.96) | 0.76 |
|
Multiple | 12 (19.7) | 3 (13.6) |
|
| 10 (17.2) | 5 (20.0) |
|
|
|
Angioinvasionb |
|
Negative | 46 (75.4) | 13 (61.9) | 1.89
(0.66–5.43) | 0.27 | 39 (68.4) | 20 (80.0) | 0.54
(0.18–1.67) | 0.42 |
|
Positive | 15 (24.6) | 8 (38.1) |
|
| 18 (31.6) | 5 (20.0) |
|
|
| AFPc |
|
<100 | 44 (81.5) | 18 (81.8) | 0.98
(0.27–3.53) | 1.00 | 43 (81.1) | 19 (82.6) | 0.91
(0.25–3.25) | 1.00 |
|
>100 | 10 (18.5) | 4 (18.2) |
|
| 10 (18.9) | 4 (17.4) |
|
|
| Surgery |
| Liver
transplantation | 16 (26.2) | 6 (27.3) | 0.95
(0.32–2.84) | 1.00 | 16 (27.6) | 6 (24.0) | 1.21
(0.41–3.57) | 0.79 |
|
Resection | 45 (73.8) | 16 (72.7) |
|
| 42 (72.4) | 19 (76.0) |
|
|
| Pretreatment |
| No
TACE | 46 (75.4) | 14 (63.6) | 1.75
(0.62–4.99) | 0.41 | 42 (72.4) | 18 (72.0) | 1.02
(0.36–2.91) | 1.00 |
|
TACE | 15 (24.6) | 8 (36.4) |
|
| 16 (27.6) | 7 (28.0) |
|
|
The present study also estimated the association of
various combinations of these IGF2R SNPs with HCC
susceptibility. As shown in Table VIII, no significant difference
was observed in SNPs between healthy controls and HCC patients.
Discussion
It has been suggested that IGF2R may act as a tumor
suppressor; therefore, the present study evaluated its role as a
biomarker in the pathology of HCC. To the best of our knowledge,
the present study is the first to analyze the expression profile of
IGF2R in a large series of human HCC samples, and to
investigate its association with clinical and tumor-specific data.
In the human HCC samples analyzed in the present study, the mRNA
expression levels of IGF2R were significantly downregulated
in cancerous tissue compared with in the corresponding
non-neoplastic TST. In addition, downregulation of IGF2R protein
was detected in HCC tissues from one patient, which indicated that
the results of RT-PCR were concordant with the protein expression
experiment. The present study predominantly focused on the role of
IGF2R mRNA expression as a potential marker in the
pathogenesis of HCC; therefore, solely HCC tissue and TST samples
were collected. One of the limitations of the present study is that
tissue samples containing a tumor border, which would have been
required for complete immunohistochemical analysis and subsequent
statistical analysis, were not available. Further experiments are
required to confirm the downregulation of IGF2R protein in HCC. The
loss of IGF2R has already been described in some tumor types and
its expression is associated with tumor suppression (28,45–47).
Chen et al revealed that a decreased expression of
IGF2R in human breast cancer cells, via infection with an
adenovirus carrying a ribozyme targeted against IGF2R mRNA,
enhances IGF2-induced proliferation and reduces susceptibility to
tumor necrosis factor-induced apoptosis (28). In addition, radioimmunotherapy
targeted to IGF2R in osteosarcoma cells suppresses tumor
growth in a murine osteosarcoma xenograft model (45). Transfection experiments using breast
cancer cells and choriocarcinoma cells demonstrated that
overexpression of IGF2R decreases cellular growth rates
in vitro and decreases tumor growth in nude mice (46,47).
Whether the reduction of IGF2R levels in HCC may provide HCC
cells with an important selective growth advantage should be
investigated further and has not been reported in the present
study. Furthermore, this study demonstrated that patients with
upregulated IGF2R mRNA expression were younger than those
with downregulated expression; currently, we do not have any
explanation for this. Therefore, it requires confirmation in
further studies using a different and larger cohort. Nevertheless,
the present study demonstrated a strong association between
IGF2R mRNA expression and the risk of tumor recurrence
within 5 years following surgery, indicating a functional
consequence of IGF2R expression for patients with HCC.
However, whether IGF2R serves a direct role in tumor suppression,
or merely an indirect role as a transporter for ligands designated
for degradation in the lysosomes, remains to be further
elucidated.
In order to increase the number of informative
cases, both resected and transplanted livers were included for
analysis, and approximately one-third of patients in the present
cohort were pretreated with TACE prior to surgery. These patients
most likely exhibited a good response to TACE, leading to
subsequent liver transplantation in the majority of cases. The
present study demonstrated that the TACE-pretreated patients
possessed significantly higher mRNA expression levels of
IGF2R compared with non-treated patients. To the best of our
knowledge, this study is the first to describe this relationship;
however, at present, it cannot answer whether IGF2R mRNA
expression is directly influenced by the TACE procedure, because
IGF2R mRNA expression was solely analyzed in liver tumor
explants following TACE. It may be speculated that during TACE some
factor could be induced, which may be responsible for disease
stability. IGF2R may be considered a good candidate gene to
further analyze in this context, as this study revealed that
TACE-pretreated patients with HCC had a significantly higher
expression of IGF2R mRNA compared with non-pretreated
patients. It would be interesting to know whether tumors that
respond to TACE therapy possess an overexpression of IGF2R
mRNA already prior to TACE therapy or whether IGF2R mRNA
expression is induced by TACE, e.g. by hypoxia- and/or
chemotherapy-induced mechanisms. To analyze that, the expression of
IGF2R mRNA in TACE-treated HCC samples has to be compared
with pre-TACE biopsies taken at the time of diagnosis. This
approach could determine whether IGF2R mRNA is induced by
the TACE procedure or not.
Otto et al (48) proposed that TACE pretreatment may
select patients with biologically less aggressive tumors. In this
previous study, patients who experienced tumor response to TACE had
a significantly prolonged disease-free survival compared to those
with tumor progression during TACE. These findings are in
accordance with the present study, which demonstrated that the
TACE-pretreated patient cohort exhibited a significantly increased
recurrence-free 5 year survival. Furthermore, Otto et al
reported that the freedom of recurrence was not influenced by
classification of the patient according to the Milan criteria or by
downstaging, but rather by the stability of the disease during
pretreatment with TACE (48). At
present, it has not yet been analyzed as to whether IGF2R
mRNA expression is associated with the prognosis of HCC following
TACE pretreatment. Further investigations are required to address
whether IGF2R mRNA expression before or after TACE is
associated with the prognosis of HCC.
The molecular mechanisms that are induced through
TACE therapy remain to be completely elucidated. It is well known
that cells under stress, such as hypoxia, promote IGF2R
expression (49). Whether
IGF2R expression in HCC is affected by TACE-induced hypoxia
remains to be analyzed. Nevertheless, the present data indicated
that IGF2R may be a promising candidate marker, which may serve a
role in TACE-induced hypoxia, as well as in tumor response. Most
hypoxia-induced pathways not only promote tumor growth, but also
induce apoptosis (50). Since IGF2R
induces apoptosis, this is an interesting aspect to consider. If it
could be shown that IGF2R is induced through hypoxia, and
that IGF2R expression is associated with the prognosis of
HCC following TACE pretreatment, this would be a further goal in
improving TACE treatment by potentially increasing the proportion
of patients able to undergo liver resection, reduce recurrence, and
prolong survival and quality of life of patients who remain
unsuitable for resection (12).
The genotypes of the SNPs rs629849 (located in the
binding site for IGF2) and rs642588 (located in the
CTCF-binding site of the IGF2R promoter) were not
significantly associated with HCC risk in the present study. Weng
et al (41) and Rashad et
al (51) reported that the
combination of IGF2 rs10840452 (AA) and IGF2R
rs629849 (GG) homozygosity exhibited a significant protective
effect against HCC occurrence. The authors concluded that
IGF2 and IGF2R polymorphisms are significant
IGF-system-associated factors in HCC development. The present
findings concerning the SNP rs629849 are supported by Rezgui et
al (42); this previous study
analyzed the structure and function of the human SNP rs629849 and
revealed that it fails to alter gene expression, protein half-life
and cell membrane distribution of IGF2R, thus suggesting that the
polymorphism has no direct effect on receptor function.
Furthermore, the comparison of binding kinetics of ‘wild-type’ and
‘mutated’ (rs629849) IGF2R to IGF2 revealed no
differences in ‘on’ and ‘off’ rates, concluding that the rs629849
polymorphism is non-functional.
Notably, Rashad et al (51) demonstrated that the homozygous
IGF2R rs629849 GG genotype is significantly associated with
worse Child-Pugh grades. In the present study, no significant
association was detected between the SNPs tested and the Child-Pugh
classification grade. However, patients with a homozygous
IGF2R rs629849 GG genotype were associated with a
significantly elevated risk of non-viral liver cirrhosis (P=0.05).
Furthermore, upregulation of IGF2R mRNA expression was
associated with a higher occurrence of cirrhosis in patients with
HCC (P=0.05) de Bleser et al (52) revealed that IGF2R is
upregulated during liver fibrosis, which may be caused by the
overexpression of IGF2R in hepatic stellate cells, which are
the major cell type involved in liver fibrosis (53). Fibrogenesis is stimulated by TGF-β1,
which is known to be activated by IGF2R (38). Activated stellate cells are also
responsible for secreting collagen scar tissue, which can lead to
cirrhosis (53). These findings
support the role of IGF2R in fibrogenesis and the development of
cirrhosis. However, data reporting the influence of rs642588 on the
functionality of the CTFC-binding site in the IGF2R promoter
region are currently not available.
The present study suggested an important role for
IGF2R expression in HCC, particularly with regards to TACE
pretreatment. These findings indicated that IGF2R may be
considered a good candidate for further investigation of TACE
inducibility and as a marker for improved recurrence-free patient
survival. Furthermore, this study suggested a pivotal role for
IGF2R in the development of liver cirrhosis. Further studies
are required to investigate the precise mechanisms underlying the
effects of IGF2R on the progression of HCC, and to evaluate
possible diagnostic and therapeutic consequences.
Acknowledgements
The authors would like to thank Mrs. Larissa Herbel
(1st Department of Internal Medicine, University Medicine of the
Johanes Gutenberg University Mainz) and Mrs. Ulrike Suessdorf
(Department of General, Visceral and Transplantation Surgery,
University Medicine of the Johannes Gutenberg University Mainz),
for excellent technical assistance.
Funding
Research funding from the University Medicine of the
Johannes Gutenberg University Mainz for AL, FS and TZ was used for
this study.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
AL, FS and TZ made major contributions to the
conception, analysis and interpretation of the data, and were major
contributors in writing, drafting and revising the manuscript. HL,
GO, JM, CD and PRG collected the clinical samples and the
corresponding clinical data. AL, FS, JV and MHL performed the
experiments and analyzed data. MHL conducted the clinical data
collection and performed the statistical analysis. AS performed the
histological evaluation. HL, TZ, GO, PRG and CD critically revised
the manuscript. All authors read and approved the final version of
the manuscript, and agree to be accountable for all aspects of the
research in ensuring that the accuracy or integrity of any part of
the work are appropriately investigated and resolved.
Ethics approval and consent to
participate
The present study followed the ethical guidelines of
the Declaration of Helsinki and was approved by the Ethics
Committee of the State of Rhineland-Palatinate Medical Board
[Number 847.243.17 (11077)]. All patients provide written informed
consent, according to the agreement on transfer and scientific use
of excess material of the University Medicine of the Johannes
Gutenberg University Mainz prior to data or specimen
collection.
Patient consent for publication
Not applicable.
Competing interest
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
HCC
|
hepatocellular carcinoma
|
|
IGF2R
|
insulin-like growth factor-2
receptor
|
|
TACE
|
transarterial chemoembolization
|
|
TST
|
tumor-surrounding tissue
|
|
IGF1
|
insulin-like growth factor-1
|
|
IGF2
|
insulin-like growth factor-2
|
|
IGF1R
|
insulin-like growth factor-1
receptor
|
|
TGF-β1
|
transforming growth factor-β1
|
|
PSQ
|
pyrosequencing
|
|
OR
|
odds ratio
|
References
|
1
|
El-Serag HB: Hepatocellular carcinoma. N
Engl J Med. 365:1118–1127. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Breuhahn K: Molecular mechanisms of
progression in human hepatocarcinogenesis. Pathologe (31.
(Suppl):2:S170–S176. 2010.(In German). View Article : Google Scholar
|
|
5
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dhanasekaran R, Limaye A and Cabrera R:
Hepatocellular carcinoma: Current trends in worldwide epidemiology,
risk factors, diagnosis, and therapeutics. Hepat Med. 4:19–37.
2012.PubMed/NCBI
|
|
7
|
Nguyen VT, Law MG and Dore GJ: Hepatitis
B-related hepatocellular carcinoma: Epidemiological characteristics
and disease burden. J Viral Hepat. 16:453–463. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schwartz M: Liver transplantation for
hepatocellular carcinoma. Gastroenterology. 127:S268–S276. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lencioni R: Chemoembolization in patients
with hepatocellular carcinoma. Liver Cancer. 1:41–50. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Decaens T, Roudot-Thoraval F,
Bresson-Hadni S, Meyer C, Gugenheim J, Durand F, Bernard PH,
Boillot O, Boudjema K, Calmus Y, et al: Impact of
pretransplantation transarterial chemoembolization on survival and
recurrence after liver transplantation for hepatocellular
carcinoma. Liver Transpl. 11:767–775. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yao FY, Kinkhabwala M, LaBerge JM, Bass
NM, Brown R Jr, Kerlan R, Venook A, Ascher NL, Emond JC and Roberts
JP: The impact of pre-operative loco-regional therapy on outcome
after liver transplantation for hepatocellular carcinoma. Am J
Transplant. 5:795–804. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang YX, De Baere T, Idee JM and Ballet S:
Transcatheter embolization therapy in liver cancer: An update of
clinical evidences. Chin J Cancer Res. 27:96–121. 2015.PubMed/NCBI
|
|
13
|
Bouchard-Fortier A, Lapointe R, Perreault
P, Bouchard L and Pomier-Layrargues G: Transcatheter arterial
chemoembolization of hepatocellular carcinoma as a bridge to liver
transplantation: A retrospective study. Int J Hepatol.
2011:9745142011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gordon-Weeks AN, Snaith A, Petrinic T,
Friend PJ, Burls A and Silva MA: Systematic review of outcome of
downstaging hepatocellular cancer before liver transplantation in
patients outside the Milan criteria. Br J Surg. 98:1201–1208. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Millonig G, Graziadei IW, Freund MC,
Jaschke W, Stadlmann S, Ladurner R, Margreiter R and Vogel W:
Response to preoperative chemoembolization correlates with outcome
after liver transplantation in patients with hepatocellular
carcinoma. Liver Transpl. 13:272–279. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang Z, Liu Q, He J, Yang J, Yang G and
Wu M: The effect of preoperative transcatheter hepatic arterial
chemoembolization on disease-free survival after hepatectomy for
hepatocellular carcinoma. Cancer. 89:2606–2612. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Otto G, Herber S, Heise M, Lohse AW, Mönch
C, Bittinger F, Hoppe-Lotichius M, Schuchmann M, Victor A and
Pitton M: Response to transarterial chemoembolization as a
biological selection criterion for liver transplantation in
hepatocellular carcinoma. Liver Transpl. 12:1260–1267. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kasprzak A, Kwasniewski W, Adamek A and
Gozdzicka- Jozefiak A: Insulin-like growth factor (IGF) axis in
cancerogenesis. Mutat Res Rev Mutat Res. 772:78–104. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wu J and Zhu AX: Targeting insulin-like
growth factor axis in hepatocellular carcinoma. J Hematol Oncol.
4:302011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Elmashad N, Ibrahim WS, Mayah WW, Farouk
M, Ali LA, Taha A and Elmashad W: Predictive value of serum
insulin-like growth factor-1 in hepatocellular carcinoma. Asian Pac
J Cancer Prev. 16:613–619. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Espelund U, Gronbaek H, Villadsen GE,
Simonsen K, Vestergaard PF, Jørgensen JO, Flyvbjerg A, Vilstrup H
and Frystyk J: The circulating IGF system in hepatocellular
carcinoma: The impact of liver status and treatment. Growth Horm
IGF Res. 25:174–181. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mazziotti G, Sorvillo F, Morisco F,
Carbone A, Rotondi M, Stornaiuolo G, Precone DF, Cioffi M, Gaeta
GB, Caporaso N and Carella C: Serum insulin-like growth factor I
evaluation as a useful tool for predicting the risk of developing
hepatocellular carcinoma in patients with hepatitis C virus-related
cirrhosis: A prospective study. Cancer. 95:2539–2545. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rehem RN and El-Shikh WM: Serum IGF-1,
IGF-2 and IGFBP-3 as parameters in the assessment of liver
dysfunction in patients with hepatic cirrhosis and in the diagnosis
of hepatocellular carcinoma. Hepatogastroenterology. 58:949–954.
2011.PubMed/NCBI
|
|
24
|
Su WW, Lee KT, Yeh YT, Soon MS, Wang CL,
Yu ML and Wang SN: Association of circulating insulin-like growth
factor 1 with hepatocellular carcinoma: One cross-sectional
correlation study. J Clin Lab Anal. 24:195–200. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chun YS, Huang M, Rink L and Von Mehren M:
Expression levels of insulin-like growth factors and receptors in
hepatocellular carcinoma: A retrospective study. World J Surg
Oncol. 12:2312014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dong Z, Yao M, Wang L, Yan X, Gu X, Shi Y,
Yao N, Qiu L, Wu W and Yao D: Abnormal expression of insulin-like
growth factor-I receptor in hepatoma tissue and its inhibition to
promote apoptosis of tumor cells. Tumour Biol. 34:3397–3405. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Souza RF, Wang S, Thakar M, Smolinski KN,
Yin J, Zou TT, Kong D, Abraham JM, Toretsky JA and Meltzer SJ:
Expression of the wild-type insulin-like growth factor II receptor
gene suppresses growth and causes death in colorectal carcinoma
cells. Oncogene. 18:4063–4068. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen Z, Ge Y, Landman N and Kang JX:
Decreased expression of the mannose 6-phosphate/insulin-like growth
factor-II receptor promotes growth of human breast cancer cells.
BMC Cancer. 2:182002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lu ZL, Luo DZ and Wen JM: Expression and
significance of tumor-related genes in HCC. World J Gastroenterol.
11:3850–3854. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Causin C, Waheed A, Braulke T, Junghans U,
Maly P, Humbel RE and von Figura K: Mannose
6-phosphate/insulin-like growth factor II-binding proteins in human
serum and urine. Their relation to the mannose
6-phosphate/insulin-like growth factor II receptor. Biochem J.
252:795–799. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jirtle RL, Hankins GR, Reisenbichler H and
Boyer IJ: Regulation of mannose 6-phosphate/insulin-like growth
factor-II receptors and transforming growth factor beta during
liver tumor promotion with phenobarbital. Carcinogenesis.
15:1473–1478. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kornfeld S: Structure and function of the
mannose 6-phosphate/insulinlike growth factor II receptors. Annu
Rev Biochem. 61:307–330. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Denley A, Cosgrove LJ, Booker GW, Wallace
JC and Forbes BE: Molecular interactions of the IGF system.
Cytokine Growth Factor Rev. 16:421–439. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Enguita-German M and Fortes P: Targeting
the insulin-like growth factor pathway in hepatocellular carcinoma.
World J Hepatol. 6:716–737. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chu CH, Huang CY, Lu MC, Lin JA, Tsai FJ,
Tsai CH, Chu CY, Kuo WH, Chen LM and Chen LY: Enhancement of
AG1024-induced H9c2 cardiomyoblast cell apoptosis via the
interaction of IGF2R with Galpha proteins and its downstream PKA
and PLC-beta modulators by IGF-II. Chin J Physiol. 52:31–37. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chu CH, Tzang BS, Chen LM, Kuo CH, Cheng
YC, Chen LY, Tsai FJ, Tsai CH, Kuo WW and Huang CY:
IGF-II/mannose-6-phosphate receptor signaling induced cell
hypertrophy and atrial natriuretic peptide/BNP expression via
Galphaq interaction and protein kinase C-alpha/CaMKII activation in
H9c2 cardiomyoblast cells. J Endocrinol. 197:381–390. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang KC, Brooks DA, Botting KJ and
Morrison JL: IGF-2R-mediated signaling results in hypertrophy of
cultured cardiomyocytes from fetal sheep. Biol Reprod. 86:1832012.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Dennis PA and Rifkin DB: Cellular
activation of latent transforming growth factor beta requires
binding to the cation-independent mannose 6-phosphate/insulin-like
growth factor type II receptor. Proc Natl Acad Sci USA. 88:580–584.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ghosh P, Dahms NM and Kornfeld S: Mannose
6-phosphate receptors: New twists in the tale. Nat Rev Mol Cell
Biol. 4:202–212. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Nahon P and Zucman-Rossi J: Single
nucleotide polymorphisms and risk of hepatocellular carcinoma in
cirrhosis. J Hepatol. 57:663–674. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Weng CJ, Hsieh YH, Tsai CM, Chu YH, Ueng
KC, Liu YF, Yeh YH, Su SC, Chen YC, Chen MK, et al: Relationship of
insulin-like growth factors system gene polymorphisms with the
susceptibility and pathological development of hepatocellular
carcinoma. Ann Surg Oncol. 17:1808–1815. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Rezgui D, Williams C, Savage SA, Prince
SN, Zaccheo OJ, Jones EY, Crump MP and Hassan AB: Structure and
function of the human Gly1619Arg polymorphism of M6P/IGF2R domain
11 implicated in IGF2 dependent growth. J Mol Endocrinol.
42:341–356. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
DaCosta SA, Schumaker LM and Ellis MJ:
Mannose 6-phosphate/insulin-like growth factor 2 receptor, a bona
fide tumor suppressor gene or just a promising candidate? J Mammary
Gland Biol Neoplasia. 5:85–94. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
EASL Clinical Practice Guidelines:
Management of hepatocellular carcinoma. J Hepatol. 69:182–236.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Geller DS, Morris J, Revskaya E, Kahn M,
Zhang W, Piperdi S, Park A, Koirala P, Guzik H, Hall C, et al:
Targeted therapy of osteosarcoma with radiolabeled monoclonal
antibody to an insulin-like growth factor-2 receptor (IGF2R). Nucl
Med Biol. 43:812–817. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lee JS, Weiss J, Martin JL and Scott CD:
Increased expression of the mannose 6-phosphate/insulin-like growth
factor-II receptor in breast cancer cells alters tumorigenic
properties in vitro and in vivo. Int J Cancer. 107:564–570. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
O'Gorman DB, Weiss J, Hettiaratchi A,
Firth SM and Scott CD: Insulin-like growth factor-II/mannose
6-phosphate receptor overexpression reduces growth of
choriocarcinoma cells in vitro and in vivo. Endocrinology.
143:4287–4294. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Otto G, Heise M, Moench C, Herber S,
Bittinger F, Schuchmann M, Hoppe-Lotichius M and Pitton M:
Transarterial chemoembolization before liver transplantation in 60
patients with hepatocellular carcinoma. Transplant Proc.
39:537–539. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Shneor D, Folberg R, Pe'er J, Honigman A
and Frenkel S: Stable knockdown of CREB, HIF-1 and HIF-2 by
replication-competent retroviruses abrogates the responses to
hypoxia in hepatocellular carcinoma. Cancer Gene Ther. 24:64–74.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Harris AL: Hypoxia-A key regulatory factor
in tumour growth. Nat Rev Cancer. 2:38–47. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Rashad NM, El-Shal AS, Abd Elbary EH, Abo
Warda MH and Hegazy O: Impact of insulin-like growth factor 2,
insulin-like growth factor receptor 2, insulin receptor substrate 2
genes polymorphisms on susceptibility and clinicopathological
features of hepatocellular carcinoma. Cytokine. 68:50–58. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
de Bleser PJ, Jannes P, van Buul-Offers
SC, Hoogerbrugge CM, van Schravendijk CF, Niki T, Rogiers V, van
den Brande JL, Wisse E and Geerts A: Insulinlike growth
factor-II/mannose 6-phosphate receptor is expressed on
CCl4-exposed rat fat-storing cells and facilitates
activation of latent transforming growth factor-beta in cocultures
with sinusoidal endothelial cells. Hepatology. 21:1429–1437. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Brandao DF, Ramalho LN, Ramalho FS,
Zucoloto S, Martinelli Ade L and Silva Ode C: Liver cirrhosis and
hepatic stellate cells. Acta Cir Bras. 1:54–57. 2006. View Article : Google Scholar
|