Certain metabolic alterations, also referred to as
metabolic reprogramming, are commonly observed in tumor cells and
are proposed to be hallmarks of cancer (8). Given the vast differences in
metabolism between healthy and tumor cells, there is hope that
selective targeting of tumor metabolism may be achieved while
limiting toxicity to healthy tissue. The most striking and
characteristic metabolic alteration in cancer cells is anomalous
glucose metabolism and cancer cells tend to utilize glycolysis to
obtain energy even under aerobic conditions via a process called
‘aerobic glycolysis’ (9). The
implications of this finding overshadowed the importance of
mitochondria for tumor growth for a long time. However, in recent
years, there has been increasing evidence that metformin exerts its
anticancer effects through the inhibition of oxidative
phosphorylation (OXPHOS) of tumor cell mitochondria, and metabolic
pathways based on metformin targeting have only recently become the
focus of intensive research. In order to establish a systematic
literature review, the online search engine PubMed was used for the
present study. Studies published within the last 10 years were
retrieved using the key terms ‘Metformin’ and ‘Lung Cancer’. In the
present review, NSCLC metabolism was discussed with a focus on the
potential of metformin-based targeting of NSCLC metabolism and the
associated mechanisms, and the available preclinical and clinical
evidence was assessed.
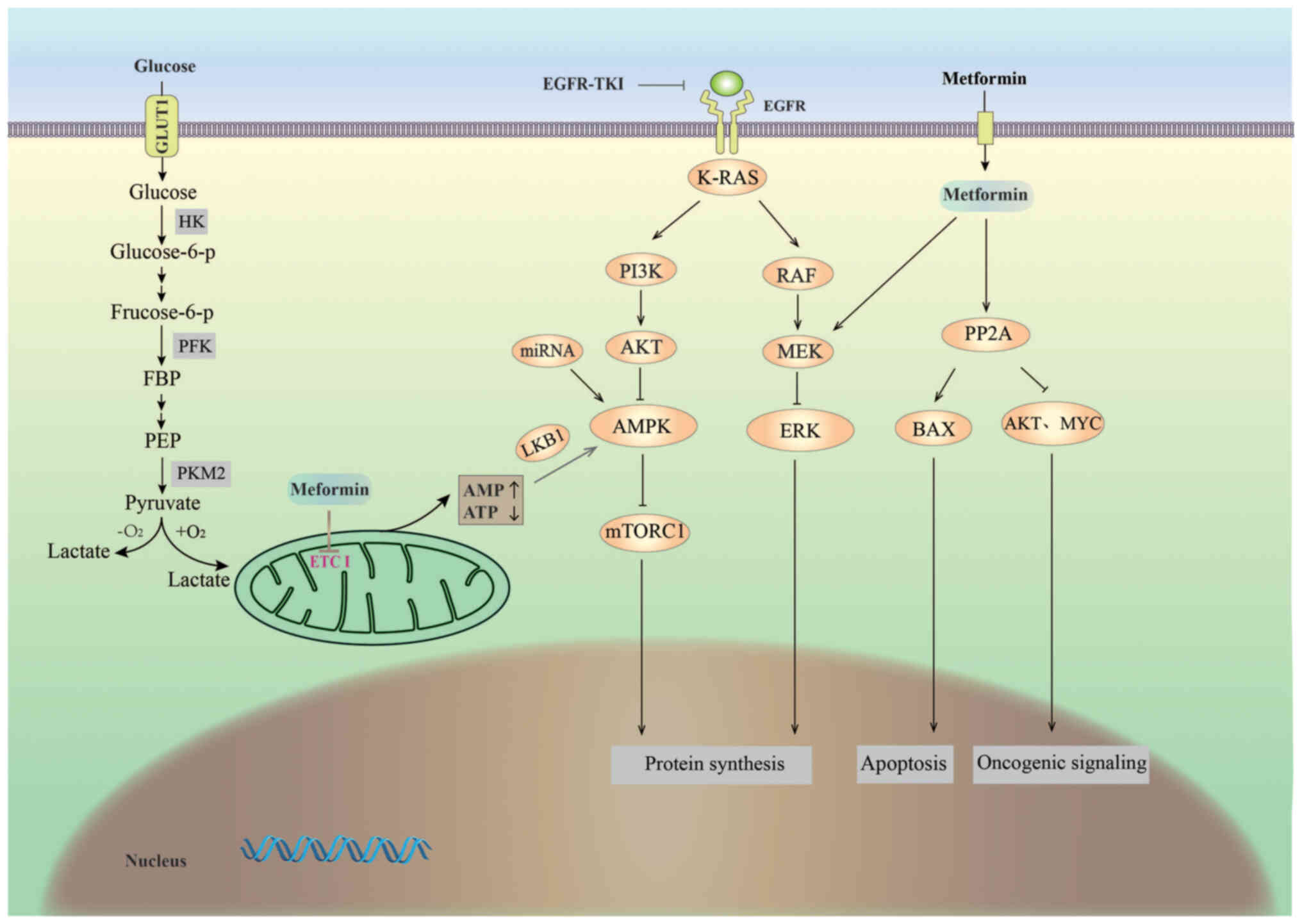
Glucose is the most abundant and important energy
source in organisms and it is metabolized in cells via two major
pathways (Fig. 1): Glycolysis,
which takes place under anaerobic conditions, and complete
oxidation, which occurs under aerobic conditions (10). In the 1920s, Otto Heinrich Warburg
discovered that cancer cells, unlike normal cells, use the
glycolytic pathway to obtain energy for growth even in the presence
of oxygen, which is a phenomenon known as ‘aerobic glycolysis’ or
the Warburg effect (9), and
aerobic glycolysis is a common metabolic phenotype in NSCLC
(11). In positron emission
tomography (PET)/CT, the high rate of glycolysis in NSCLC is
reflected by the high uptake of 18F-fluorodeoxyglucose at the
corresponding tumor sites (12).
It has been reported that lung cancer cells exhibit upregulated
expression of all key glycolytic enzymes [hexokinase 2 (HK2),
phosphofructokinase and pyruvate kinase (PK)] (13), suggesting that the essential
enzymes of the aerobic glycolytic pathway have a critical role in
the development of lung carcinoma. Therefore, various drugs that
interfere with glycolytic glucose transport proteins and key
enzymes are being studied for their potential as anticancer agents
(14).
Glucose transporter 1 (GLUT1), which drives the
intracellular transport of glucose, is the first rate-limiting
factor in glycolysis (15). Lung
cancer cells have a high rate of glycolysis and high GLUT1
expression (16), and research
focusing on GLUT1 may be important for lung cancer treatment.
WZB117 (WZB) is a synthetic small molecule that inhibits glucose
transport by downregulating GLUT1 expression (17). A study suggested that WZB may
enhance toxic effects on the NSCLC cell line H460 by limiting
glycolysis (18). In a nude mouse
tumor transplantation model of lung cancer, WZB was indicated to
inhibit tumor growth by inhibiting GLUT1 and limiting the
glycolytic flow (19,20). 2-Deoxy-D-glucose (2-DG), another
glycolysis inhibitor, restricts tumor growth by binding to HK and
preventing glucose from accessing the enzyme (5,18).
In recent years, research on microRNAs (miRNAs/miRs) has expanded
and their association with NSCLC has been explored. For instance,
Jia et al (21)
demonstrated that miR-206 levels were reduced in NSCLC cells and
tissues and overexpression of miR-206 was able to inhibit
glycolysis and cell proliferation by targeting the 3′-untranslated
region of HK2 and downregulating HK2 expression. PKM2 is essential
for tumorigenesis and An et al (22) demonstrated that small
ubiquitin-related modifier 1 (SUMO1) overexpression increased
glycolysis and promoted the growth of A549 cells in vitro by
modifying PKM2 at Lys-336. Knockdown of SUMO1 in A549 cells
resulted in a marked decrease in the protein expression of PKM2,
suggesting that SUMO1-modified PKM2 may be a potential therapeutic
target for NSCLC.
The study of aerobic glycolytic pathways and the
functions of key enzymes in tumor cells is vital for the treatment
of NSCLC. Since the Warburg effect was described, there has been an
increase in research focusing on aerobic glycolysis (14) and there have been several attempts
to limit the growth of lung cancer by cutting off its energy
supply. Although a reversal of the Warburg effect may be a broad
anticancer strategy, therapeutic approaches to limit aerobic
glycolysis in NSCLC have been only partially successful (23). The expression of PKM2 was
previously indicated to be required for aerobic glycolysis and it
was proposed that PKM2 provides a growth advantage to tumors.
However, Israelsen et al (24) excised PKM exon 10 to terminate PKM2
protein synthesis while still allowing the splicing and protein
expression of PKM1, which demonstrated that the loss of PKM2
accelerated tumor formation in a nude mouse xenograft tumor model.
Similarly, Cortés-Cros et al (25) knocked down PKM2/M1 in established
tumors and observed no significant difference in the growth of A549
lung cancer xenografts in vivo. These studies suggest the
presence of other alternative metabolic pathways.
Mitochondria are the main sites of ATP release
during oxidative phosphorylation and the original hypothesis of the
Warburg effect was that cancer cells have a defective mitochondrial
function, resulting in impaired aerobic respiration, necessitating
the reliance on glycolysis for ATP supply (26). However, later studies have
indicated that mitochondrial function is not impaired in most
cancer cells and that mitochondria have an important role in cancer
metabolism (27–29). In addition, although the ratio of
glycolysis to OXPHOS increases, in absolute terms, both glycolysis
and oxidative phosphorylation are more active in cancer cells than
in normal cells and the two processes coexist (30). Given that mitochondria are
essential for tumorigenesis and cancer cell proliferation (31–33),
targeting the mitochondrial OXPHOS metabolic pathway may be a
viable approach for inhibiting the growth of cancer cells (34).
Metformin has been the safest and most widely
prescribed drug for type 2 diabetes (T2D) (35). It downregulates cytosolic OXPHOS by
inhibiting mitochondrial electron transport chain complex I (ETC
I), thereby hampering the oxidative phosphorylation required for
tumor cell growth (36–38). Initial interest in the use of
metformin for preventing and treating lung cancer arose from a
number of clinical studies suggesting that metformin reduces the
risk of lung cancer in individuals with diabetes (39–41).
Studies have gradually revealed the mechanism of
action of metformin in the treatment of cancer (Fig. 1). Metformin has indirect
(insulin-dependent) and direct (insulin-independent) anticancer
effects (42). The indirect
anticancer effect of metformin results from the attenuation of the
stimulatory effect of hyperinsulinemia on lung cancer growth via an
increase in insulin sensitivity and decrease in circulating insulin
levels (43). By contrast, the
direct effect of metformin is caused by the activation of adenosine
monophosphate (AMP)-activated protein kinase (AMPK). Metformin
indirectly activates AMPK by disrupting mitochondrial ETC I,
leading to reduced ATP synthesis and an increased cellular AMP/ATP
ratio (44). It is generally
speculated that the AMPK activation-mediated anticancer activity of
metformin may be dependent on liver kinase B1 (LKB1). Metformin
exerts its antitumor effects mainly through the AMPK/LKB1/mammalian
target of rapamycin (mTOR) complex 1 (mTORC1) signaling pathway,
causing apoptosis of cancer cells (45–48).
LKB1 is a classical tumor suppressor (49) and mutations in this gene are
associated with Peutz-Jeghers cancer susceptibility syndrome
(50,51). Genetic mutations in LKB1 are also
observed in certain sporadic cancers, particularly squamous cell
carcinoma and lung adenocarcinoma cells (52,53).
AMPK is the direct substrate of LKB1. Metformin interferes with
cellular energy metabolism by disrupting ETC I; the low energy
states induce LKB1-mediated AMPK activation and indirectly inhibit
mTORC1 to regulate cell growth (54–56).
In addition, metformin may also have anticancer activity via AMPK
activation independent of LKB1 (57–59).
Guo et al (57) evaluated
the effects of metformin on human NSCLC H1299 (LKB1-positive) and
H460 (LKB1-deficient) cells. They indicated that metformin inhibits
NSCLC proliferation in a time- and dose-dependent manner, induces
cell cycle arrest in G0/G1 phase and increases apoptosis
independent of LKB1 protein levels. They also observed that
knockdown of LKB1 using short hairpin RNA does not affect the
anti-proliferative effect of metformin on H1299 cells.
mTORC1, a serine/threonine protein kinase belonging
to the PI3K-related kinase family, acts as a regulator of cell
growth and metabolism (60).
Activated AMPK inhibits tumor growth by inhibiting mTORC1, which
blocks protein synthesis and proliferation in cancer cells
(61,62). As mTORC1 is frequently mutated in
cancers and functions downstream of several oncogenic pathways,
various tumors, including lung cancer tumors, exhibit elevated
mTORC1 activity (63). The
RAS/PI3K/AKT/mTOR signaling pathway is an important cellular
signaling cascade in which RAS activates PI3K and AKT and
indirectly regulates mTORC1 (9,64,65).
Among the three RAS genes (H-, K- and N-RAS), the highest mutation
frequency was observed for the K-RAS gene in lung cancer (6.5%
frequency for squamous cell carcinoma and 26% for adenocarcinoma in
Western populations) (66).
Metformin induces apoptosis via the downregulation of the
downstream targets of K-RAS in human A549 lung adenocarcinoma cells
with K-RAS mutations (67). It has
also been reported that metformin inhibits mTORC1 signaling in an
AMPK-independent manner and that this inhibition of mTORC1
activation and signaling may be Rag GTPase-dependent (68).
The anticancer effects of metformin are also
speculated to be related to miRNAs in NSCLC. A recent study by Dong
et al (69) indicated that
metformin inhibits the growth, migration and invasion of A549 cells
by upregulating AMPK-mediated miR-7 expression and regulating the
AKT/mTOR and MAPK/ERK pathways. Recently, it has been reported that
high Yes-associated protein (YAP) may induce the growth and
metastasis of NSCLC. Metformin also disrupts the growth and
metastasis of NSCLC by inhibiting the activity of the
miR-381-YAP-Snail axis (70).
However, the gene knockout of AMPK does not
completely block the effects of metformin against cancer
development, suggesting the presence of alternative mechanisms
(57,59). Protein phosphatase 2 (PP2A) is
considered a tumor inhibitor in a variety of tumors (71) and the PP2A inhibitor α4 is usually
overexpressed in tumor cells. Zhou et al (72) determined that metformin increases
the apoptotic rate of A549 and H1651 lung cancer cells by
disrupting the interaction of PP2A inhibitors (α4 and MID1) with
the catalytic subunit and activating PP2A. This effect is
associated with inhibited oncogenic activity of AKT and MYC, as
well as Bax phosphorylation, suggesting that PP2A may also be a
potential metformin target in lung cancer therapy.
Progress has also been made in research on the
effects of metformin in animal models of lung cancer.
Nicotine-derived nitrosamides, also known as
4-(methylnitrosamino)1-(3-pyridyl)-1-butanone (NNK), have been
identified as inducers of lung cancer (79). In a study by Memmott et al
(80), in which A/J mice were
exposed to NNK and then received intraperitoneal injections of
metformin, metformin was observed to reduce tumorigenesis by 72%.
This study demonstrated that metformin prevents the tobacco
carcinogen-induced development of lung tumors via inhibition of
Akt, upstream of mTOR, and indirect inhibition of mTOR. In three
other xenogeneic models of A549 cell origin, treatment with
metformin significantly reduced tumor growth and metastatic
capacity in vivo, and reduced the expression of proteins
such as Ki-67, proliferating cell nuclear antigen (PCNA), Akt and
Myc (72,78,81).
In a study by Moro et al (73) on patient-derived xenografts (PDXs),
metformin (100 mg/kg/day) partially inhibited the tumor growth of
PDXs with wild-type LKB1 (maximum inhibition rate, 50.5±14.8%), but
had no significant inhibitory effect on LKB1-mutant PDXs, and with
increasing doses of metformin, p-AMPK expression was increased and
Ki67 expression was decreased, indicating that LKB1-deficient
tumors have an impaired ability to adapt to metabolic stress
induced by metformin treatment. More recently, in another study on
wild-type LKB1 PDXs, metformin only induced apoptosis in wild-type
LKB1 PDXs with high expression of miR-17, suggesting that high
miR-17 expression increased sensitivity to metformin treatment
(82).
Preclinical studies have indicated that metformin
has anticancer effects and numerous retrospective clinical studies
have demonstrated that metformin significantly improved anticancer
activity in patients with NSCLC compared to those not taking
metformin (Table II). Several
retrospective studies suggested that metformin use is associated
with a decreased risk of lung cancer (41,83,84).
Metformin use was also significantly associated with a favorable
prognosis of patients with NSCLC (85,86).
In a retrospective study assessing overall survival (OS) of
patients with T2D and metastatic lung cancer, patients treated with
metformin had 20% higher survival rates than those who did not take
metformin (87). A comprehensive
systematic evaluation and meta-analysis of 10 published
retrospective studies by Cao et al (88) determined that treatment with
metformin significantly improved survival, with corresponding
increases in OS and progression-free survival (PFS) of 23 and 47%,
respectively. In addition, analyses stratified by tissue type
indicated a significant improvement in OS and PFS in NSCLC,
suggesting that metformin may be an effective treatment option for
patients with diabetes combined with lung cancer. However, Kim
et al (89) performed a
retrospective study of 336,168 individuals regarding lung cancer
incidence with a median study duration of 12.86 years and observed
that metformin treatment did not reduce lung cancer incidence in
the diabetic population. The potential use of metformin in lung
cancer prevention should be reconsidered and requires to be further
validated in randomized controlled trials.
Another strategy to influence the aerobic glycolytic
pathway in cancer cells includes the inhibition of glucose
concentrations in culture media in vitro and diet
restrictions to lower blood glucose levels in vivo (98). Several studies have indicated that
cancer cells cultured under low glucose concentrations or in
sugar-free media are more susceptible to the cytotoxic effects of
metformin (55,91,99).
Restricted diets exhibited a strong synergistic effect on
anticancer activity in preclinical models of lung adenocarcinoma.
Elgendy et al (92) treated
mice undergoing a 24-h feeding/fasting cycle with metformin and
they observed impaired tumor growth only when the drug was
administered during fasting-induced hypoglycemia. This indicated
that metformin combined with fasting-induced hypoglycemia
synergistically inhibited the growth of transplanted tumors in nude
mice. In addition, an ongoing clinical trial aims to determine
whether the combination of metformin and fasting improves PFS in
patients with advanced lung adenocarcinoma compared with historical
data on metformin alone (100).
In another clinical trial, the investigators will assess for the
first time the efficacy of combining standard-of-care
platinum-based chemoimmunotherapy with metformin plus/minus a
fasting-mimicking diet in patients with LKB1-inactive, advanced
lung adenocarcinoma (ClinicalTrials.gov identifier no.
NCT03709147).
In recent years, under single treatment regimens
[chemotherapy, immune checkpoint inhibitors (ICIs) and targeted
therapies] patients have exhibited relapses due to the development
of acquired drug resistance (101–103). There is growing evidence that
metformin exerts its anticancer effects by inhibiting tumor
metabolism and that metformin may be a potential candidate for
combination therapy in NSCLC. A number of preclinical studies have
reported good results of metformin acting concurrently with
radiotherapy, tyrosine kinase inhibitors (TKIs) and ICIs in NSCLC
(104–107), which has encouraged the use of
combination therapies. In a meta-analysis of 14 clinical studies
comprising 3,856 patients, the combination of metformin with
standard antineoplastic drugs significantly improved OS in patients
with lung cancer (108). These
results suggest that metformin combined with radiotherapy may be an
effective regimen for the treatment of patients with NSCLC.
However, in two recent randomized clinical trials, Skinner et
al (109) and Tsakiridis
et al (110) reported
poorer outcomes for patients with NSCLC treated with metformin in
combination with radiotherapy, suggesting that the addition of
metformin to radiotherapy did not improve OS in patients with NSCLC
and increased toxicities, which contrasts the results of previous
studies. Promising results have also been reported by two recent
studies of metformin in combination with TKIs and ICIs,
respectively, which suggested that metformin was able to
significantly improve PFS and OS in patients with NSCLC by
overcoming acquired resistance to TKIs and enhancing PD-1 blockade
by anti-PD-1 antibodies, respectively (101,102). Other studies (111–114) suggested that metformin may
increase tumor response to ICI through a variety of mechanisms,
including upregulation of CD8+ tumor-infiltrating
lymphocytes and their function, downregulation of myeloid
suppressor cells with immunosuppressive effects, reduction of tumor
hypoxia, anti-angiogenic effects and shifting the composition of
the patient's gut flora to bacterial strains that may respond
better to immunotherapy (107).
Although it has been suggested that metformin treatment may exert a
synergistic antitumor effect with ICIs, the study by Jacobi et
al (107) did not obtain any
positive association between metformin and ICIs in the treatment of
patients with diabetes combined with NSCLC. More prospective
studies are required to further evaluate the effect of metformin in
combination with radiotherapy, TKIs and ICIs on the outcome of
patients with NSCLC. A search on https://clinicaltrials.gov indicated that a number of
prospective clinical trials (Table
III) are currently evaluating the preventive and therapeutic
effects of metformin alone or in combination with other treatment
options for NSCLC. One of these is an ongoing open, single-arm,
phase II clinical trial (ClinicalTrials.gov identifier no.
NCT03874000) to evaluate the safety, efficacy and pharmacokinetics
of the metformin-sintilimab combination in the treatment of NSCLC
(115).
Therapeutic methods that target the metabolic
differences between tumor cells and normal cells have potential in
cancer treatment and the restriction of aerobic glycolysis in
tumors has been somewhat effective in inducing lung cancer cell
apoptosis. There are also increasing reports confirming the
important role of mitochondria in the development and growth of
cancer. In recent years, there has been increasing evidence of the
antitumor effects of metformin as an OXPHOS inhibitor and in a
number of retrospective clinical trials, metformin has produced
beneficial effects on survival outcomes in patients with NSCLC. The
theory of the antitumor effects of metformin involves its action on
several major signaling pathways, including indirect
(insulin-dependent) and direct (activation of AMPK pathways) and
corresponding targets, such as PI3K, K-RAS, mTORC, PP2A and miRNA.
However, as with aerobic glycolysis inhibitors, metformin alone
exhibited limitations in its effectiveness in in vitro
trials. Drugs that target enzymes or metabolites of key metabolic
pathways may be highly specific and effective but must be matched
to responsive tumors that are likely to adapt rapidly. Preclinical
evidence in recent years has demonstrated synergistic effects of
metformin in combination with glycolysis inhibitors, radiotherapy,
EGFR-TKIs and ICIs in NSCLC, but it is not consistent with the
results of certain retrospective studies and clinical trials, and
more prospective studies are required to further evaluate the
influence of metformin combination effects on the outcomes for
patients with NSCLC. However, metformin inhibits mitochondria in a
dose-dependent manner and at high doses, although it is able to
impair tumor growth, it may also lead to lactic acidosis (116). The clinical application of
experimental doses of metformin may be challenging. Of note,
metformin accumulates in tissues at concentrations several times
higher than those in the blood and the positive charge on metformin
has been indicated to promote its accumulation in the mitochondrial
matrix <1,000-fold (>20 mmol/l). Hence, metformin
concentrations of 1–10 mmol/l, which have been used in preclinical
models, may also be effective during cancer treatment in clinical
settings (117). In a recent
study, Reinfeld et al (118) used PET tracers to measure glucose
uptake in specific cellular subpopulations in the tumor
microenvironment and determined that in a range of cancer models,
myeloid cells have the greatest glucose uptake capacity within the
tumor, followed by T cells and cancer cells. Furthermore, they
observed that cancer cells had higher uptake of glutamine than of
glucose. In the future, more in-depth basic research on target
metabolic pathways in lung cancer is required to provide an
improved theoretical basis for adjuvant lung cancer therapy.
Not applicable.
Funding: No funding was received.
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the current
study.
NC and JBH designed the review and edited the
manuscript. NC and JBH wrote the manuscript. NC, YSZ and LCW
collected and analyzed data. All authors read and approved the
final manuscript. Data authentication is not applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Wang W, Hao Y, Liu Y, Li R, Huang DB and
Pan YY: Nanomedicine in lung cancer: Current states of overcoming
drug resistance and improving cancer immunotherapy. Wiley
Interdiscip Rev Nanomed Nanobiotechnol. 13:e16542021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2021. CA Cancer J Clin. 71:7–33. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Duma N, Santana-Davila R and Molina JR:
Non-small cell lung cancer: Epidemiology, screening, diagnosis, and
treatment. Mayo Clin Proc. 94:1623–1640. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hai J, Zhu CQ, Bandarchi B, Wang YH, Navab
R, Shepherd FA, Jurisica I and Tsao MS: L1 cell adhesion molecule
promotes tumorigenicity and metastatic potential in non-small cell
lung cancer. Clin Cancer Res. 18:1914–1924. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Meijer TWH, Peeters WJM, Dubois LJ, van
Gisbergen MW, Biemans R, Venhuizen JH, Span PN and Bussink J:
Targeting glucose and glutamine metabolism combined with radiation
therapy in non-small cell lung cancer. Lung Cancer. 126:32–40.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yao L, Liu M, Huang Y, Wu K, Huang X, Zhao
Y, He W and Zhang R: Metformin use and lung cancer risk in diabetic
patients: A systematic review and meta-analysis. Dis Markers.
2019:62301622019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Troncone M, Cargnelli SM, Villani LA,
Isfahanian N, Broadfield LA, Zychla L, Wright J, Pond G, Steinberg
GR and Tsakiridis T: Targeting metabolism and AMP-activated kinase
with metformin to sensitize non-small cell lung cancer (NSCLC) to
cytotoxic therapy: Translational biology and rationale for current
clinical trials. Oncotarget. 8:57733–57754. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
DeBerardinis RJ and Chandel NS:
Fundamentals of cancer metabolism. Sci Adv. 2:e16002002016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vander Heiden MG, Cantley LC and Thompson
CB: Understanding the warburg effect: The metabolic requirements of
cell proliferation. Science. 324:1029–1033. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bose S and Le A: Glucose metabolism in
cancer. Adv Exp Med Biol. 1063:3–12. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu W, Yu X, Zhou L, Li J, Li M, Li W and
Gao F: Sinomenine inhibits non-small cell lung cancer via
downregulation of hexokinases II-mediated aerobic glycolysis. Onco
Targets Ther. 13:3209–3221. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Toba H, Kawakita N, Takashima M, Matsumoto
D, Takizawa H, Otsuka H and Tangoku A: Diagnosis of recurrence and
follow-up using FDG-PET/CT for postoperative non-small-cell lung
cancer patients. Gen Thorac Cardiovasc Surg. 69:311–317. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li XB, Gu JD and Zhou QH: Review of
aerobic glycolysis and its key enzymes-new targets for lung cancer
therapy. Thorac Cancer. 6:17–24. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Martinez-Outschoorn UE, Peiris-Pagés M,
Pestell RG, Sotgia F and Lisanti MP: Cancer metabolism: A
therapeutic perspective. Nat Rev Clin Oncol. 14:11–31. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang L, Ran Y, Zhu Y and Zhen Q: Effect
of addition of WZB117 as an inhibitor of glucose transporter 1 for
venous blood glucose determination. Lab Med. 52:197–201. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tiemin P, Peng X, Qingfu L, Yan W, Junlin
X, Zhefeng H, Ming Z, Desen L and Qinghui M: Dysregulation of the
miR-148a-GLUT1 axis promotes the progression and chemoresistance of
human intrahepatic cholangiocarcinoma. Oncogenesis. 9:192020.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhao F, Ming J, Zhou Y and Fan L:
Inhibition of Glut1 by WZB117 sensitizes radioresistant breast
cancer cells to irradiation. Cancer Chemother Pharmacol.
77:963–972. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yakisich JS, Azad N, Kaushik V and Iyer
AKV: The biguanides metformin and buformin in combination with
2-Deoxy-glucose or WZB-117 inhibit the viability of highly
resistant human lung cancer cells. Stem Cells Int.
2019:62542692019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ojelabi OA, Lloyd KP, Simon AH, De Zutter
JK and Carruthers A: WZB117 (2-Fluoro-6-(m-hydroxybenzoyloxy)
Phenyl m-Hydroxybenzoate) Inhibits GLUT1-mediated sugar transport
by binding reversibly at the exofacial sugar binding site. J Biol
Chem. 291:26762–26772. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu Y, Cao Y, Zhang W, Bergmeier S, Qian
Y, Akbar H, Colvin R, Ding J, Tong L, Wu S, et al: A small-molecule
inhibitor of glucose transporter 1 downregulates glycolysis,
induces cell-cycle arrest, and inhibits cancer cell growth in vitro
and in vivo. Mol Cancer Ther. 11:1672–1682. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jia KG, Feng G, Tong YS, Tao GZ and Xu L:
MiR-206 regulates non-small-cell lung cancer cell aerobic
glycolysis by targeting hexokinase 2. J Biochem. 167:365–370. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
An S, Huang L, Miao P, Shi L, Shen M, Zhao
X, Liu J and Huang G: Small ubiquitin-like modifier 1 modification
of pyruvate kinase M2 promotes aerobic glycolysis and cell
proliferation in A549 human lung cancer cells. Onco Targets Ther.
11:2097–2109. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Porporato PE, Filigheddu N, Pedro JMB,
Kroemer G and Galluzzi L: Mitochondrial metabolism and cancer. Cell
Res. 28:265–280. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Israelsen WJ, Dayton TL, Davidson SM,
Fiske BP, Hosios AM, Bellinger G, Li J, Yu Y, Sasaki M, Horner JW,
et al: PKM2 isoform-specific deletion reveals a differential
requirement for pyruvate kinase in tumor cells. Cell. 155:397–409.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cortés-Cros M, Hemmerlin C, Ferretti S,
Zhang J, Gounarides JS, Yin H, Muller A, Haberkorn A, Chene P,
Sellers WR and Hofmann F: M2 isoform of pyruvate kinase is
dispensable for tumor maintenance and growth. Proc Natl Acad Sci
USA. 110:489–494. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Warburg O: On the origin of cancer cells.
Science. 123:309–314. 1956. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Weinhouse S: The Warburg hypothesis fifty
years later. Z Krebsforsch Klin Onkol Cancer Res Clin Oncol.
87:115–126. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fantin VR, St-Pierre J and Leder P:
Attenuation of LDH-A expression uncovers a link between glycolysis,
mitochondrial physiology, and tumor maintenance. Cancer Cell.
9:425–434. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Moreno-Sánchez R, Rodríguez-Enríquez S,
Marín-Hernández A and Saavedra E: Energy metabolism in tumor cells.
FEBS J. 274:1393–1418. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zacksenhaus E, Shrestha M, Liu JC,
Vorobieva I, Chung PED, Ju Y, Nir U and Jiang Z: Mitochondrial
OXPHOS Induced by RB1 deficiency in breast cancer: Implications for
anabolic metabolism, stemness, and metastasis. Trends Cancer.
3:768–779. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Joshi S, Tolkunov D, Aviv H, Hakimi AA,
Yao M, Hsieh JJ, Ganesan S, Chan CS and White E: The genomic
landscape of renal oncocytoma identifies a metabolic barrier to
tumorigenesis. Cell Rep. 13:1895–1908. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Weinberg F, Hamanaka R, Wheaton WW,
Weinberg S, Joseph J, Lopez M, Kalyanaraman B, Mutlu GM, Budinger
GR and Chandel NS: Mitochondrial metabolism and ROS generation are
essential for Kras-mediated tumorigenicity. Proc Natl Acad Sci USA.
107:8788–8793. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Martínez-Reyes I, Diebold LP, Kong H,
Schieber M, Huang H, Hensley CT, Mehta MM, Wang T, Santos JH,
Woychik R, et al: TCA cycle and mitochondrial membrane potential
are necessary for diverse biological functions. Mol Cell.
61:199–209. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Cheng G, Zhang Q, Pan J, Lee Y, Ouari O,
Hardy M, Zielonka M, Myers CR, Zielonka J, Weh K, et al: Targeting
lonidamine to mitochondria mitigates lung tumorigenesis and brain
metastasis. Nat Commun. 10:22052019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Viollet B, Guigas B, Sanz Garcia N,
Leclerc J, Foretz M and Andreelli F: Cellular and molecular
mechanisms of metformin: An overview. Clin Sci (Lond). 122:253–270.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sanchez-Alvarez R, Martinez-Outschoorn UE,
Lamb R, Hulit J, Howell A, Gandara R, Sartini M, Rubin E, Lisanti
MP and Sotgia F: Mitochondrial dysfunction in breast cancer cells
prevents tumor growth: Understanding chemoprevention with
metformin. Cell Cycle. 12:172–182. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Brown SL, Kolozsvary A, Isrow DM, Al
Feghali K, Lapanowski K, Jenrow KA and Kim JH: A novel mechanism of
high dose radiation sensitization by metformin. Front Oncol.
9:2472019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhao Q, Zhou X, Curbo S and Karlsson A:
Metformin downregulates the mitochondrial carrier SLC25A10 in a
glucose dependent manner. Biochem Pharmacol. 156:444–450. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhang ZJ, Bi Y, Li S, Zhang Q, Zhao G, Guo
Y and Song Q: Reduced risk of lung cancer with metformin therapy in
diabetic patients: A systematic review and meta-analysis. Am J
Epidemiol. 180:11–14. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Tsai MJ, Yang CJ, Kung YT, Sheu CC, Shen
YT, Chang PY, Huang MS and Chiu HC: Metformin decreases lung cancer
risk in diabetic patients in a dose-dependent manner. Lung Cancer.
86:137–143. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kang J, Jeong SM, Shin DW, Cho M, Cho JH
and Kim J: The associations of aspirin, statins, and metformin with
lung cancer risk and related mortality: A time-dependent analysis
of population-based nationally representative data. J Thorac Oncol.
16:76–88. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Li C, Xue Y, Xi YR and Xie K: Progress in
the application and mechanism of metformin in treating non-small
cell lung cancer. Oncol Lett. 13:2873–2880. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Frasca F, Pandini G, Sciacca L, Pezzino V,
Squatrito S, Belfiore A and Vigneri R: The role of insulin
receptors and IGF-I receptors in cancer and other diseases. Arch
Physiol Biochem. 114:23–37. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mihaylova MM and Shaw RJ: The AMPK
signalling pathway coordinates cell growth, autophagy and
metabolism. Nat Cell Biol. 13:1016–1023. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kim KH, Song MJ, Yoo EJ, Choe SS, Park SD
and Kim JB: Regulatory role of glycogen synthase kinase 3 for
transcriptional activity of ADD1/SREBP1c. J Biol Chem.
279:51999–52006. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Shaw RJ, Kosmatka M, Bardeesy N, Hurley
RL, Witters LA, DePinho RA and Cantley LC: The tumor suppressor
LKB1 kinase directly activates AMP-activated kinase and regulates
apoptosis in response to energy stress. Proc Natl Acad Sci USA.
101:3329–3335. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Woods A, Johnstone SR, Dickerson K, Leiper
FC, Fryer LG, Neumann D, Schlattner U, Wallimann T, Carlson M and
Carling D: LKB1 is the upstream kinase in the AMP-activated protein
kinase cascade. Curr Biol. 13:2004–2008. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Koo SH, Flechner L, Qi L, Zhang X,
Screaton RA, Jeffries S, Hedrick S, Xu W, Boussouar F, Brindle P,
et al: The CREB coactivator TORC2 is a key regulator of fasting
glucose metabolism. Nature. 437:1109–1111. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Inoki K, Zhu T and Guan KL: TSC2 mediates
cellular energy response to control cell growth and survival. Cell.
115:577–590. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Forcet C and Billaud M: Dialogue between
LKB1 and AMPK: A hot topic at the cellular pole. Sci STKE.
2007:pe512007. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Korsse SE, Peppelenbosch MP and van Veelen
W: Targeting LKB1 signaling in cancer. Biochim Biophys Acta.
1835:194–210. 2013.PubMed/NCBI
|
|
52
|
Shackelford DB and Shaw RJ: The LKB1-AMPK
pathway: Metabolism and growth control in tumour suppression. Nat
Rev Cancer. 9:563–575. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Liu B, Fan Z, Edgerton SM, Deng XS,
Alimova IN, Lind SE and Thor AD: Metformin induces unique
biological and molecular responses in triple negative breast cancer
cells. Cell Cycle. 8:2031–2040. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Gwinn DM, Shackelford DB, Egan DF,
Mihaylova MM, Mery A, Vasquez DS, Turk BE and Shaw RJ: AMPK
phosphorylation of raptor mediates a metabolic checkpoint. Mol
Cell. 30:214–226. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Buzzai M, Jones RG, Amaravadi RK, Lum JJ,
DeBerardinis RJ, Zhao F, Viollet B and Thompson CB: Systemic
treatment with the antidiabetic drug metformin selectively impairs
p53-deficient tumor cell growth. Cancer Res. 67:6745–6752. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Bolster DR, Crozier SJ, Kimball SR and
Jefferson LS: AMP-activated protein kinase suppresses protein
synthesis in rat skeletal muscle through down-regulated mammalian
target of rapamycin (mTOR) signaling. J Biol Chem. 277:23977–23980.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Guo Q, Liu Z, Jiang L, Liu M, Ma J, Yang
C, Han L, Nan K and Liang X: Metformin inhibits growth of human
non-small cell lung cancer cells via liver kinase B-1-independent
activation of adenosine monophosphate-activated protein kinase. Mol
Med Rep. 13:2590–2596. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Xiao X, He Q, Lu C, Werle KD, Zhao RX,
Chen J, Davis BC, Cui R, Liang J and Xu ZX: Metformin impairs the
growth of liver kinase B1-intact cervical cancer cells. Gynecol
Oncol. 127:249–255. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Storozhuk Y, Hopmans SN, Sanli T, Barron
C, Tsiani E, Cutz JC, Pond G, Wright J, Singh G and Tsakiridis T:
Metformin inhibits growth and enhances radiation response of
non-small cell lung cancer (NSCLC) through ATM and AMPK. Br J
Cancer. 108:2021–2032. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Condon KJ and Sabatini DM: Nutrient
regulation of mTORC1 at a glance. J Cell Sci. 132:jcs2225702019.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Saxton RA and Sabatini DM: mTOR signaling
in growth, metabolism, and disease. Cell. 168:960–976. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Düvel K, Yecies JL, Menon S, Raman P,
Lipovsky AI, Souza AL, Triantafellow E, Ma Q, Gorski R, Cleaver S,
et al: Activation of a metabolic gene regulatory network downstream
of mTOR complex 1. Mol Cell. 39:171–183. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Howell JJ, Ricoult SJ, Ben-Sahra I and
Manning BD: A growing role for mTOR in promoting anabolic
metabolism. Biochem Soc Trans. 41:906–912. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Schneider MB, Matsuzaki H, Haorah J,
Ulrich A, Standop J, Ding XZ, Adrian TE and Pour PM: Prevention of
pancreatic cancer induction in hamsters by metformin.
Gastroenterology. 120:1263–1270. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bussink J, van der Kogel AJ and Kaanders
JH: Activation of the PI3-K/AKT pathway and implications for
radioresistance mechanisms in head and neck cancer. Lancet Oncol.
9:288–296. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Dearden S, Stevens J, Wu YL and Blowers D:
Mutation incidence and coincidence in non small-cell lung cancer:
Meta-analyses by ethnicity and histology (mutMap). Ann Oncol.
24:2371–2376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Ma Y, Guo FC, Wang W, Shi HS, Li D and
Wang YS: K-ras gene mutation as a predictor of cancer cell
responsiveness to metformin. Mol Med Rep. 8:763–768. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kalender A, Selvaraj A, Kim SY, Gulati P,
Brûlé S, Viollet B, Kemp BE, Bardeesy N, Dennis P, Schlager JJ, et
al: Metformin, independent of AMPK, inhibits mTORC1 in a rag
GTPase-dependent manner. Cell Metab. 11:390–401. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Dong J, Peng H, Yang X, Wu W, Zhao Y, Chen
D, Chen L and Liu J: Metformin mediated microRNA-7 upregulation
inhibits growth, migration, and invasion of non-small cell lung
cancer A549 cells. Anticancer Drugs. 31:345–352. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Jin D, Guo J, Wu Y, Chen W, Du J, Yang L,
Wang X, Gong K, Dai J, Miao S, et al: Metformin-repressed
miR-381-YAP-snail axis activity disrupts NSCLC growth and
metastasis. J Exp Clin Cancer Res. 39:62020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Fatehi Hassanabad A and MacQueen K:
Molecular mechanisms underlining the role of metformin as a
therapeutic agent in lung cancer. Cell Oncol (Dordr). 44:1–18.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Zhou X, Liu S, Lin X, Xu L, Mao X, Liu J,
Zhang Z, Jiang W and Zhou H: Metformin inhibit lung cancer cell
growth and invasion in vitro as well as tumor formation in vivo
partially by activating PP2A. Med Sci Monit. 25:836–846. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Moro M, Caiola E, Ganzinelli M, Zulato E,
Rulli E, Marabese M, Centonze G, Busico A, Pastorino U, de Braud
FG, et al: Metformin enhances cisplatin-induced apoptosis and
prevents resistance to cisplatin in Co-mutated KRAS/LKB1 NSCLC. J
Thorac Oncol. 13:1692–1704. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Luo Z, Zhu T, Luo W, Lv Y, Zhang L, Wang
C, Li M, Wu W and Shi S: Metformin induces apoptotic cytotoxicity
depending on AMPK/PKA/GSK-3β-mediated c-FLIPL
degradation in non-small cell lung cancer. Cancer Manag Res.
11:681–689. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Riaz MA, Sak A, Erol YB, Groneberg M,
Thomale J and Stuschke M: Metformin enhances the radiosensitizing
effect of cisplatin in non-small cell lung cancer cell lines with
different cisplatin sensitivities. Sci Rep. 9:12822019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Lee BB, Kim Y, Kim D, Cho EY, Han J, Kim
HK, Shim YM and Kim DH: Metformin and tenovin-6 synergistically
induces apoptosis through LKB1-independent SIRT1 down-regulation in
non-small cell lung cancer cells. J Cell Mol Med. 23:2872–2889.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Ko E, Baek S, Kim J, Park D and Lee Y:
Antitumor activity of combination therapy with metformin and
trametinib in non-small cell lung cancer cells. Dev Reprod.
24:113–123. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Wang JL, Lan YW, Tsai YT, Chen YC,
Staniczek T, Tsou YA, Yen CC and Chen CM: Additive
antiproliferative and antiangiogenic effects of metformin and
pemetrexed in a non-small-cell lung cancer xenograft model. Front
Cell Dev Biol. 9:6880622021. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Akopyan G and Bonavida B: Understanding
tobacco smoke carcinogen NNK and lung tumorigenesis. Int J Oncol.
29:745–752. 2006.PubMed/NCBI
|
|
80
|
Memmott RM, Mercado JR, Maier CR, Kawabata
S, Fox SD and Dennis PA: Metformin prevents tobacco
carcinogen-induced lung tumorigenesis. Cancer Prev Res (Phila).
3:1066–1076. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
De Bruycker S, Vangestel C, Van den
Wyngaert T, Pauwels P, Wyffels L, Staelens S and Stroobants S:
18F-Flortanidazole Hypoxia PET holds promise as a
prognostic and predictive imaging biomarker in a lung cancer
xenograft model treated with metformin and radiotherapy. J Nucl
Med. 60:34–40. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Borzi C, Ganzinelli M, Caiola E, Colombo
M, Centonze G, Boeri M, Signorelli D, Caleca L, Rulli E, Busico A,
et al: LKB1 down-modulation by miR-17 identifies patients with
NSCLC having worse prognosis eligible for energy-stress-based
treatments. J Thorac Oncol. 16:1298–1311. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Tseng CH: Metformin and lung cancer risk
in patients with type 2 diabetes mellitus. Oncotarget.
8:41132–41142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Xiao K, Liu F, Liu J, Xu J, Wu Q and Li X:
The effect of metformin on lung cancer risk and survival in
patients with type 2 diabetes mellitus: A meta-analysis. J Clin
Pharm Ther. 45:783–792. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Arrieta O, Varela-Santoyo E,
Soto-Perez-de-Celis E, Sánchez-Reyes R, De la Torre-Vallejo M,
Muñiz-Hernández S and Cardona AF: Metformin use and its effect on
survival in diabetic patients with advanced non-small cell lung
cancer. BMC Cancer. 16:6332016. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Xu T, Li D, He Y, Zhang F, Qiao M and Chen
Y: Prognostic value of metformin for non-small cell lung cancer
patients with diabetes. World J Surg Oncol. 16:602018. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Lin JJ, Gallagher EJ, Sigel K, Mhango G,
Galsky MD, Smith CB, LeRoith D and Wisnivesky JP: Survival of
patients with stage IV lung cancer with diabetes treated with
metformin. Am J Respir Crit Care Med. 191:448–454. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Cao X, Wen ZS, Wang XD, Li Y, Liu KY and
Wang X: The clinical effect of metformin on the survival of lung
cancer patients with diabetes: A comprehensive systematic review
and meta-analysis of retrospective studies. J Cancer. 8:2532–2541.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Kim J, Hyun HJ, Choi EA, Yoo JW, Lee S,
Jeong N, Shen JJ, You HS, Kim YS and Kang HT: Diabetes, metformin,
and lung cancer: Retrospective study of the Korean NHIS-HEALS
Database. Clin Lung Cancer. 21:e551–e559. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Cruz-Bermúdez A, Laza-Briviesca R,
Vicente-Blanco RJ, García-Grande A, Coronado MJ, Laine-Menéndez S,
Palacios-Zambrano S, Moreno-Villa MR, Ruiz-Valdepeñas AM, Lendinez
C, et al: Cisplatin resistance involves a metabolic reprogramming
through ROS and PGC-1α in NSCLC which can be overcome by OXPHOS
inhibition. Free Radic Biol Med. 135:167–181. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Menendez JA, Oliveras-Ferraros C, Cufí S,
Corominas-Faja B, Joven J, Martin-Castillo B and Vazquez-Martin A:
Metformin is synthetically lethal with glucose withdrawal in cancer
cells. Cell Cycle. 11:2782–2792. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Elgendy M, Cirò M, Hosseini A, Weiszmann
J, Mazzarella L, Ferrari E, Cazzoli R, Curigliano G, DeCensi A,
Bonanni B, et al: Combination of hypoglycemia and metformin impairs
tumor metabolic plasticity and growth by modulating the
PP2A-GSK3β-MCL-1 Axis. Cancer Cell. 35:798–815.e5. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Hao W, Chang CP, Tsao CC and Xu J:
Oligomycin-induced bioenergetic adaptation in cancer cells with
heterogeneous bioenergetic organization. J Biol Chem.
285:12647–12654. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Jose C, Bellance N and Rossignol R:
Choosing between glycolysis and oxidative phosphorylation: A
tumor's dilemma? Biochim Biophys Acta. 1807:552–561. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Birsoy K, Possemato R, Lorbeer FK,
Bayraktar EC, Thiru P, Yucel B, Wang T, Chen WW, Clish CB and
Sabatini DM: Metabolic determinants of cancer cell sensitivity to
glucose limitation and biguanides. Nature. 508:108–112. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Dykens JA, Jamieson J, Marroquin L,
Nadanaciva S, Billis PA and Will Y: Biguanide-induced mitochondrial
dysfunction yields increased lactate production and cytotoxicity of
aerobically-poised HepG2 cells and human hepatocytes in vitro.
Toxicol Appl Pharmacol. 233:203–210. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Hou XB, Li TH, Ren ZP and Liu Y:
Combination of 2-deoxy d-glucose and metformin for synergistic
inhibition of non-small cell lung cancer: A reactive oxygen species
and P-p38 mediated mechanism. Biomed Pharmacother. 84:1575–1584.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Lee C, Raffaghello L, Brandhorst S, Safdie
FM, Bianchi G, Martin-Montalvo A, Pistoia V, Wei M, Hwang S,
Merlino A, et al: Fasting cycles retard growth of tumors and
sensitize a range of cancer cell types to chemotherapy. Sci Transl
Med. 4:124ra272012. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Javeshghani S, Zakikhani M, Austin S,
Bazile M, Blouin MJ, Topisirovic I, St-Pierre J and Pollak MN:
Carbon source and myc expression influence the antiproliferative
actions of metformin. Cancer Res. 72:6257–6267. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Vernieri C, Signorelli D, Galli G,
Ganzinelli M, Moro M, Fabbri A, Tamborini E, Marabese M, Caiola E,
Broggini M, et al: Exploiting FAsting-mimicking Diet and MEtformin
to improve the efficacy of platinum-pemetrexed chemotherapy in
advanced LKB1-inactivated lung adenocarcinoma: The FAME Trial. Clin
Lung Cancer. 20:e413–e417. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Arrieta O, Barrón F, Padilla M,
Avilés-Salas A, Ramírez-Tirado L, Arguelles Jiménez M, Vergara E,
Zatarain-Barrón Z, Hernández-Pedro N, Cardona A, et al: Effect of
metformin plus tyrosine kinase inhibitors compared with tyrosine
kinase inhibitors alone in patients with epidermal growth factor
receptor-mutated lung adenocarcinoma: A phase 2 randomized clinical
trial. JAMA Oncol. 5:e1925532019. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Afzal MZ, Dragnev K, Sarwar T and Shirai
K: Clinical outcomes in non-small-cell lung cancer patients
receiving concurrent metformin and immune checkpoint inhibitors.
Lung Cancer Manag. 8:LMT112019. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Zhang J, Jiao K, Liu J and Xia Y:
Metformin reverses the resistance mechanism of lung adenocarcinoma
cells that knocks down the Nrf2 gene. Oncol Lett. 16:6071–6080.
2018.PubMed/NCBI
|
|
104
|
Wang J, Wang Y, Han J, Mei H, Yu D, Ding
Q, Zhang T, Wu G, Peng G and Lin Z: Metformin attenuates
radiation-induced pulmonary fibrosis in a murine model. Radiat Res.
188:105–113. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Huang S, He T, Yang S, Sheng H, Tang X,
Bao F, Wang Y, Lin X, Yu W, Cheng F, et al: Metformin reverses
chemoresistance in non-small cell lung cancer via accelerating
ubiquitination-mediated degradation of Nrf2. Transl Lung Cancer
Res. 9:2337–2355. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Wang X, Chen K, Yu Y, Xiang Y, Kim JH,
Gong W, Huang J, Shi G, Li Q, Zhou M, et al: Metformin sensitizes
lung cancer cells to treatment by the tyrosine kinase inhibitor
erlotinib. Oncotarget. 8:109068–109078. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Jacobi O, Landman Y, Reinhorn D, Icht O,
Sternschuss M, Rotem O, Finkel I, Allen AM, Dudnik E, Goldstein DA
and Zer A: The relationship of diabetes mellitus to efficacy of
immune checkpoint inhibitors in patients with advanced non-small
cell lung cancer. Oncology. 99:555–561. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Luo X, Chen X, Wang L, Yang B and Cai S:
Metformin adjunct with antineoplastic agents for the treatment of
lung cancer: A meta-analysis of randomized controlled trials and
observational cohort studies. Front Pharmacol. 12:6390162021.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Skinner H, Hu C, Tsakiridis T,
Santana-Davila R, Lu B, Erasmus JJ, Doemer AJ, Videtic GMM, Coster
J, Yang AX, et al: Addition of metformin to concurrent
chemoradiation in patients with locally advanced non-small cell
lung cancer: The NRG-LU001 phase 2 randomized clinical trial. JAMA
Oncol. 7:1324–1332. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Tsakiridis T, Pond GR, Wright J, Ellis PM,
Ahmed N, Abdulkarim B, Roa W, Robinson A, Swaminath A, Okawara G,
et al: Metformin in combination with chemoradiotherapy in locally
advanced non-small cell lung cancer: The OCOG-ALMERA randomized
clinical trial. JAMA Oncol. 7:1333–1341. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Eikawa S, Nishida M, Mizukami S, Yamazaki
C, Nakayama E and Udono H: Immune-mediated antitumor effect by type
2 diabetes drug, metformin. Proc Natl Acad Sci USA. 112:1809–1814.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Kim SH, Li M, Trousil S, Zhang Y, Pasca di
Magliano M, Swanson KD and Zheng B: Phenformin inhibits
myeloid-derived suppressor cells and enhances the anti-tumor
activity of PD-1 blockade in melanoma. J Invest Dermatol.
137:1740–1748. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Scharping NE, Menk AV, Whetstone RD, Zeng
X and Delgoffe GM: Efficacy of PD-1 blockade is potentiated by
metformin-induced reduction of tumor hypoxia. Cancer Immunol Res.
5:9–16. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Wang JC, Sun X, Ma Q, Fu GF, Cong LL,
Zhang H, Fan DF, Feng J, Lu SY, Liu JL, et al: Metformin's
antitumour and anti-angiogenic activities are mediated by skewing
macrophage polarization. J Cell Mol Med. 22:3825–3836. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kubo T, Ninomiya T, Hotta K, Kozuki T,
Toyooka S, Okada H, Fujiwara T, Udono H and Kiura K: Study
protocol: Phase-Ib trial of nivolumab combined with metformin for
refractory/recurrent solid tumors. Clin Lung Cancer. 19:e861–e864.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Granja S, Marchiq I, Le Floch R, Moura CS,
Baltazar F and Pouysségur J: Disruption of BASIGIN decreases lactic
acid export and sensitizes non-small cell lung cancer to biguanides
independently of the LKB1 status. Oncotarget. 6:6708–6721. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Morgillo F, Sasso FC, Della Corte CM,
Festino L, Manzo A, Martinelli E, Troiani T, Capuano A and
Ciardiello F: Metformin in lung cancer: Rationale for a combination
therapy. Expert Opin Investig Drugs. 22:1401–1409. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Reinfeld BI, Madden MZ, Wolf MM, Chytil A,
Bader JE, Patterson AR, Sugiura A, Cohen AS, Ali A, Do BT, et al:
Cell-programmed nutrient partitioning in the tumour
microenvironment. Nature. 593:282–288. 2021. View Article : Google Scholar : PubMed/NCBI
|