Introduction
Human epidermal growth factor receptor 2 (HER2, also
known as ERBB2) is a cell surface type I transmembrane glycoprotein
that is highly expressed on various solid tumors and enable a broad
repertoire of oncogenic signaling upon homo- and heterodimerization
with HER/ERBB families. HER2 overexpression is observed in ~20-30%
of human breast cancers, which are associated with poor prognosis
and higher rates of recurrence (1). In 1998, trastuzumab became the first
monoclonal antibody (mAb), which U.S. Food and Drug Administration
(FDA) approved for treatment of HER2-positive breast cancers
(2) and later in HER2-positive
gastric cancers (3).
Trastuzumab was initially considered to inhibit HER2
signaling (4,5). Numerous studies have confirmed the
inhibition of downstream phosphatidylinositol-3 kinase (PI3K)/Akt
pathway, and the suppression of tumor cell proliferation (6–8).
Concurrently, the HER2-selective tyrosine kinase inhibitors (TKIs)
such as lapatinib, neratinib and tucatinib, were developed and
exhibited a superior activity to suppress HER2 signaling (6,9,10).
However, regardless of a weaker inhibitory activity to HER2
signaling, trastuzumab has exhibited greater clinical efficacy than
TKIs. Trastuzumab has been the most effective therapy for
HER2-positive breast cancer for more than 20 years (11). Clinically, this difference in
efficacy suggests the involvement of immunologic engagement of
antibody therapy, hardly observed in TKIs (12).
Trastuzumab possesses an Fc domain which allows for
the direct engagement with Fcγ receptors (FcγRs) on various types
of immune cells. The FcγR engagement allows for phagocytic
engulfment of antibody-bound pathogens or cells, termed
antibody-dependent cellular phagocytosis. The FcγR-mediated
signaling activates dendritic cells, macrophages and neutrophils,
which can alter adaptive immune responses through antigen
presentation, cytokine production and chemotaxis. Furthermore, the
FcγR engagement can stimulate natural killer (NK) cells which
attack and lyse the target cells, termed antibody-dependent
cellular cytotoxicity (ADCC) (13). Margetuximab contains several
optimization mutations and exhibits improved FcγRIIIA engagement
and ADCC activity compared with the parental Ab trastuzumab
(14). Margetuximab was recently
approved by FDA in heavily pretreated patients based on modest but
significant improvement in progression-free survival (15,16).
Moreover, the Fc domain can trigger the activation of complement
family, and exert the complement-dependent cytotoxicity (CDC)
(17,18).
With the increase in lifespan of both humans and
dogs, the increased cancer incidence has been observed as well.
Mammary neoplasia is the most frequently observed in dog tumors
(19). Among them, ~50% are
malignant. These spontaneous canine mammary tumors (CMT) share
biological and histological characteristics with human breast
carcinoma (20). Compared with
murine model, CMT models have advantages as a naturally occurring
models of human cancers (21). In
canine tumors, the overexpression of dog HER2 (dHER2) has been
reported not only in mammary carcinoma (22) but also osteosarcoma (23), bladder carcinoma (24), and anal sac gland carcinoma
(25). Furthermore, in accordance
with the American Society of Clinical Oncology and the College of
American Pathologists guidelines for HER2 immunostaining, dHER2 has
been revealed to be overexpressed in 32% of CMT (26), 81% of intestinal tumor, 42% of
rectal carcinomas, and 28% of cutaneous squamous cell carcinomas
(27). Additionally, a
HER2-expressed recombinant Listeria vaccine administration resulted
in the induction of anti-dHER2 immunity, which resulted in the
reduced incidences of metastasis, and prolonged survival in a phase
I study for canine osteosarcoma (28). These clinical outcomes promoted the
evaluation of anti-dHER2 mAbs as a therapeutic modality for canine
cancers.
Previously, an anti-HER2 mAb, H2Mab-77
(mouse IgG1, kappa), was developed (29). In the present study, a
defucosylated mouse-dog chimeric anti-HER2 mAb (H77Bf) was
produced. The present study aimed to investigate the ability of
H77Bf to induce ADCC, CDC and antitumor efficacy in
dHER2-expressing cells.
Materials and methods
Cell lines
A canine mammary gland tumor cell line, SNP, was
purchased from the Cell Resource Center for Biomedical Research
Institute of Development, Aging and Cancer at Tohoku University
(Miyagi, Japan) (30). CHO-K1
cells were purchased from the American Type Culture Collection. Dog
HER2 (accession no. NM_001003217)-overexpressed CHO-K1 (CHO/dHER2)
was established by transfection of pCAG/3×RIEDL-dHER2 into CHO-K1
cells as previously described (31). 3×RIEDL sequence represented three
repeat of RIEDL amino acid sequence (32). RIEDL tag is an affinity tag that is
used for the one-step membrane protein purification (32–36).
CHO-K1, CHO/dHER2, and SNP were cultured in RPMI-1640 medium
(Nacalai Tesque, Inc.), supplemented with 10% heat-inactivated
fetal bovine serum (FBS; Thermo Fisher Scientific, Inc.), 100 µg/ml
streptomycin, 100 units/ml of penicillin, and 0.25 µg/ml
amphotericin B (Nacalai Tesque, Inc.). The cell lines were
maintained at 37°C in a humidified atmosphere under 5%
CO2.
Animals
Animal experiments were performed following
regulations and guidelines to minimize animal distress and
suffering in the laboratory. Animal experiments for antitumor
activity of H77Bf were approved (approval no. 2021-056) by the
Institutional Committee for Experiments of the Institute of
Microbial Chemistry (Numazu, Japan). Mice were maintained on an 11
h light/13 h dark cycle with food and water supplied ad
libitum in a specific pathogen-free environment across the
experimental period. Mice were monitored for weight and health
every 2–5 days during the experiments. The loss of original body
weight was determined to a point >25% and/or a maximum tumor
size >3,000 mm3 as humane endpoints for
euthanasia.
Antibodies
Anti-HER2 mAb H2Mab-77 was established as
previously described (29). To
generate H77B, we subcloned VH cDNA of
H2Mab-77 and CH of dog IgGB into the pCAG-Ble
vector (FUJIFILM Wako Pure Chemical Corporation). VL
cDNA of H2Mab-77 and CL cDNA of dog kappa
light chain were also subcloned into the pCAG-Neo vector (FUJIFILM
Wako Pure Chemical Corporation). The vector of H77B was transduced
into BINDS-09 (FUT8-deficient ExpiCHO-S) cells using the ExpiCHO
Expression System (Thermo Fisher Scientific, Inc.) (37–41).
H77Bf was purified using Ab-Capcher (ProteNova Co., Ltd.). Dog IgG
was purchased from Jackson ImmunoResearch Laboratories, Inc.
Flow cytometry
CHO-K1, CHO/dHER2, and SNP were harvested by 0.25%
trypsin/1 mM ethylenediamine tetraacetic acid (EDTA; Nacalai
Tesque, Inc.) treatment. After washing with blocking buffer [0.1%
bovine serum albumin (BSA; Nacalai Tesque, Inc.) in
phosphate-buffered saline (PBS)], cells were treated with H77Bf, or
blocking buffer (control) for 30 min at 4°C. Then, cells were
incubated in FITC-conjugated anti-dog IgG (cat. no. A18764;
1:1,000; Thermo Fisher Scientific, Inc.) for 30 min at 4°C.
Fluorescence data were collected by the Cell Analyzer EC800 and
analyzed by EC800 software ver. 1.3.6 (Sony Corp.).
Determination of binding affinity
CHO/dHER2 and SNP were suspended in serially diluted
H77Bf (0.006–25 µg/ml) followed by FITC-conjugated anti-dog IgG
(1:200). Fluorescence data were collected using the Cell Analyzer
EC800. The dissociation constant (KD) was
calculated by fitting binding isotherms to built-in one-site
binding models in GraphPad Prism 8 (GraphPad Software, Inc.).
Immunocytochemistry
Cells were fixed with 4% paraformaldehyde-PBS for 10
min and quenched with 50 mM NH4Cl in PBS with 0.2 mM
Ca2+ and 2 mM Mg2+. The cells were blocked
with blocking buffer (PBS containing 0.2 mM Ca2+, 2 mM
Mg2+ and 0.5% BSA) for 30 min and incubated with 10
µg/ml of H77Bf or blocking buffer for 1 h. The cells were further
incubated with Alexa Fluor 488-conjugated anti-dog IgG (1:400;
Jackson ImmunoResearch Laboratories, Inc.) and 0.3 µM of
4′,6-diamidino-2-phenylindole (DAPI; Thermo Fisher Scientific,
Inc.) for 45 min. The whole processes were performed at room
temperature. Fluorescence images were acquired with a 40× objective
on a BZ-X800 digital fluorescence microscope (Keyence
Corporation).
ADCC of H77Bf
Canine mononuclear cells (MNCs) obtained from
Yamaguchi University were resuspended in DMEM (Nacalai Tesque,
Inc.) with 10% FBS and were used as effector cells (37,38,42).
Target cells (CHO-K1, CHO/dHER2, and SNP) were labeled with 10
µg/ml Calcein AM (Thermo Fisher Scientific, Inc.) (31,39–41,43–53).
The target cells (2×104 cells) were plated in 96-well
plates and mixed with effector canine MNCs (effector/target cells
ratio, 50), 100 µg/ml of H77Bf or control dog IgG. Following
incubation for 4.5 h at 37°C, the Calcein release into the medium
was analyzed using a microplate reader (Power Scan HT; BioTek
Instruments, Inc.,) with an excitation wavelength (485 nm) and an
emission wavelength (538 nm).
Cytolyticity (% lysis) was calculated as follows: %
lysis=(E-S)/(M-S) ×100, where ‘E’ is the fluorescence in cultures
of both effector and target cells, ‘S’ is the spontaneous
fluorescence of only target cells, and ‘M’ is the maximum
fluorescence following the treatment with a lysis buffer (10 mM
Tris-HCl (pH 7.4), 10 mM of EDTA, and 0.5% Triton X-100).
CDC of H77Bf
Target cells (CHO-K1, CHO/dHER2, and SNP) were
labeled with 10 µg/ml Calcein AM (31,39–41,
43–53). The target cells (2×104
cells) were plated in 96-well plates and mixed with rabbit
complement (final dilution 1:10; Low-Tox-M Rabbit Complement;
Cedarlane Laboratories,) and 100 µg/ml of control dog IgG or H77Bf.
Following incubation for 4.5 h at 37°C, Calcein release into the
medium was measured.
Antitumor activity of H77Bf in
xenografts of CHO-K1, CHO/dHER2 and SNP cells
BALB/c nude mice (female, 5 weeks old, weighing
14–17 g) were purchased from Charles River Laboratories, Inc.
CHO-K1, CHO/dHER2, or SNP cells (5×106 cells) were
resuspended in DMEM and mixed with BD Matrigel Matrix Growth Factor
Reduced (BD Biosciences) were subcutaneously injected into the left
flank of mice.
On day 8 post-inoculation, 100 µg of H77Bf (n=8) or
control dog IgG (n=8) in 100 µl PBS were intraperitoneally
injected. On days 14 and 21, additional antibody inoculations were
performed. Furthermore, on days 8, 14 and 21, canine MNCs were
injected surrounding the tumors. The tumor volume was measured on
days 7, 10, 14, 17, 21, 24 and 28 after the injection of cells.
Tumor volumes were determined as previously described (31,37,39–41,50,54).
Statistical analyses
All data are expressed as mean ± standard error of
the mean (SEM). Statistical analysis was conducted with Welch's t
test for ADCC, CDC, and tumor weight. ANOVA with Sidak's post hoc
test were conducted for tumor volume and mouse weight. All
calculations were performed using GraphPad Prism 8 (GraphPad
Software, Inc.). P<0.05 was considered to indicate a
statistically significant difference.
Results
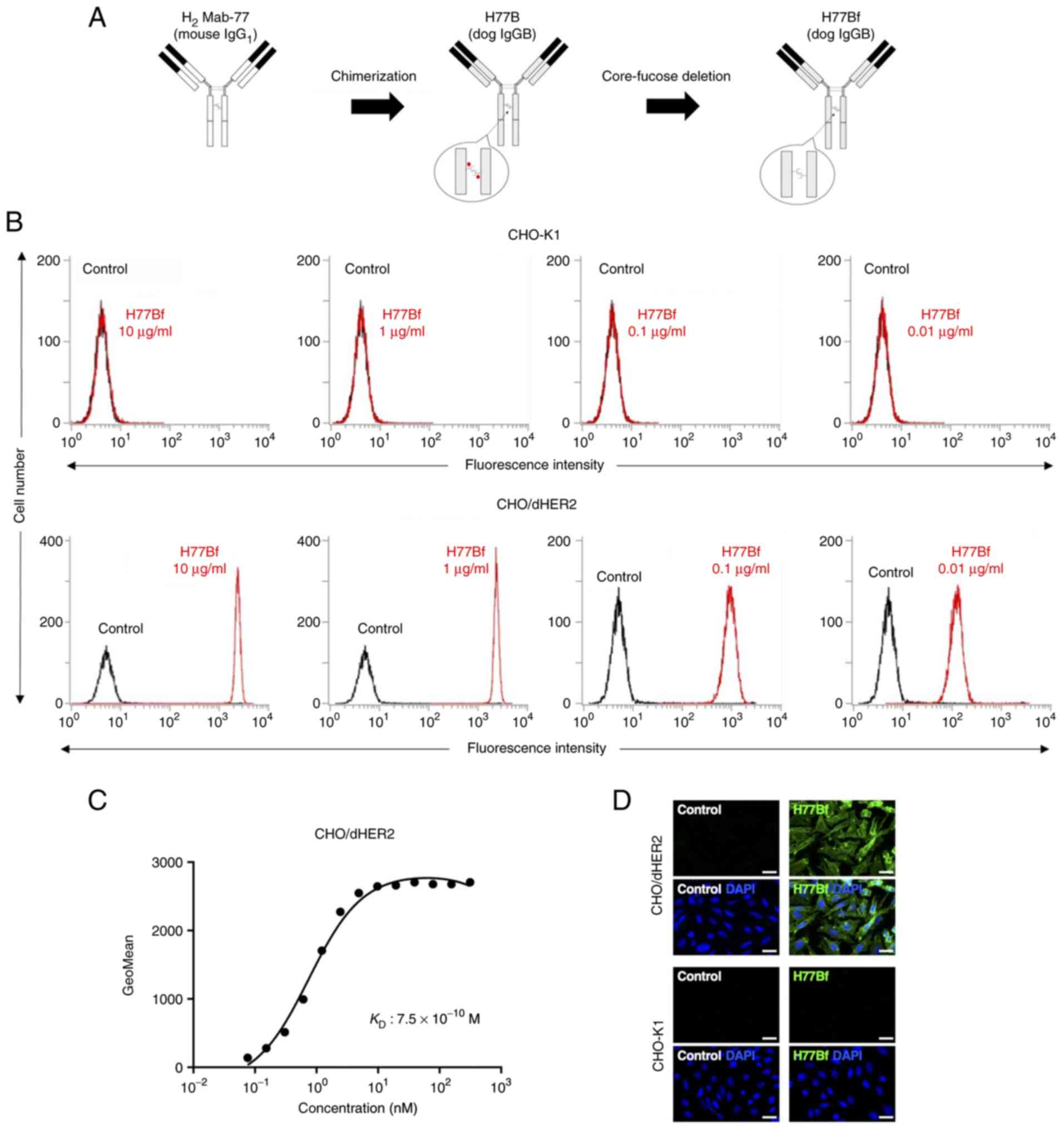
Flow cytometric analysis against
CHO/dHER2 cells using H77Bf
In our previous study, an anti-HER2 mAb
(H2Mab-77) was established using cancer-specific mAb
(CasMab) method (29).
H2Mab-77 was revealed to be very useful for flow
cytometry, western blotting and immunohistochemistry (IHC)
(29). In the present study, a
defucosylated mouse-dog chimeric anti-HER2 mAb (H77Bf) was produced
by combining VH and VL of H2Mab-77
with CH and CL of dog IgG, respectively
(Fig. 1A). H77Bf detected
CHO/dHER2 cells dose-dependently, not parental CHO-K1 cells
(Fig. 1B), indicating that H77Bf
cross-reacted with dHER2.
A kinetic analysis of the interactions of H77Bf with
CHO/dHER2 cells was performed via flow cytometry. As revealed in
Fig. 1C, the KD
for the interaction of H77Bf with CHO/dHER2 cells was
7.5×10−10 M, suggesting that H77Bf exhibits high
affinity for CHO/dHER2 cells.
Immunocytochemical analysis against
CHO/dHER2 cells using H77Bf
It was examined whether H77Bf is applicable for
immunocytochemistry. The H77Bf specificity was evaluated by using
CHO/dHER2 and CHO-K1 cells. As revealed in Fig. 1D, H77Bf detected dHER2 on CHO/dHER2
cells, but not CHO-K1 cells. Buffer control showed no signal on
both CHO/dHER2 and CHO-K1 cells. These results suggested that H77Bf
recognizes exogenous dHER2 in immunocytochemistry.
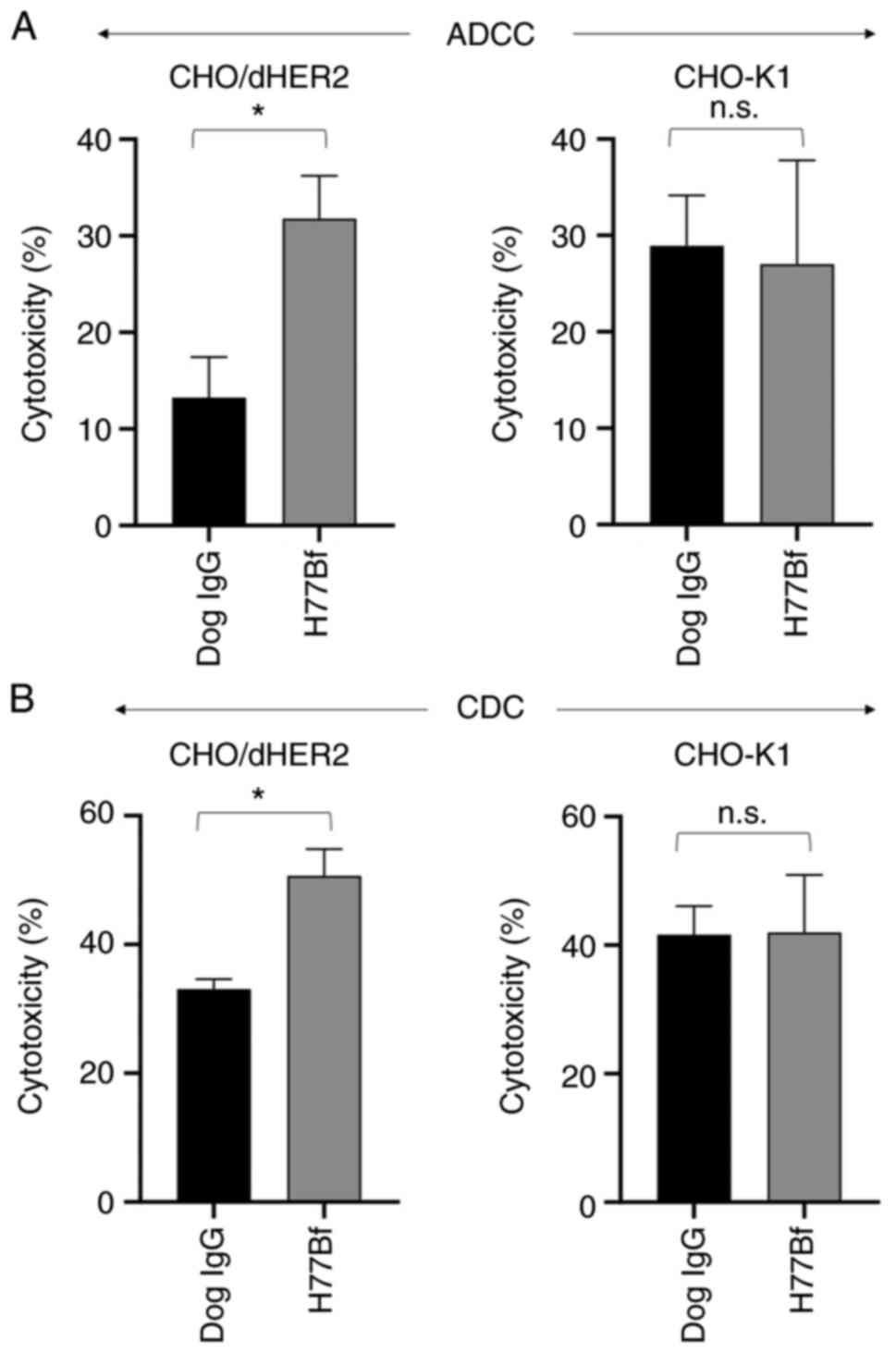
H77Bf-mediated ADCC and CDC in
CHO/dHER2 cells
It was investigated whether H77Bf was capable of
mediating ADCC against CHO/dHER2 cells. H77Bf showed ADCC (31.8%
cytotoxicity) against CHO/dHER2 cells more effectively than the
control dog IgG (13.2% cytotoxicity; P<0.05). There was no
difference between H77Bf and control dog IgG about ADCC against
CHO-K1 (Fig. 2A).
It was then examined whether H77Bf could exert CDC
against CHO/dHER2 cells. As revealed in Fig. 2B, H77Bf elicited a higher degree of
CDC (50.7% cytotoxicity) in CHO/dHER2 cells compared with that
elicited by control dog IgG (33.1% cytotoxicity; P<0.05). There
was no difference between H77Bf and control dog IgG about CDC
against CHO-K1 (Fig. 2B). These
results demonstrated that H77Bf exhibited higher levels of ADCC and
CDC against CHO/dHER2 cells.
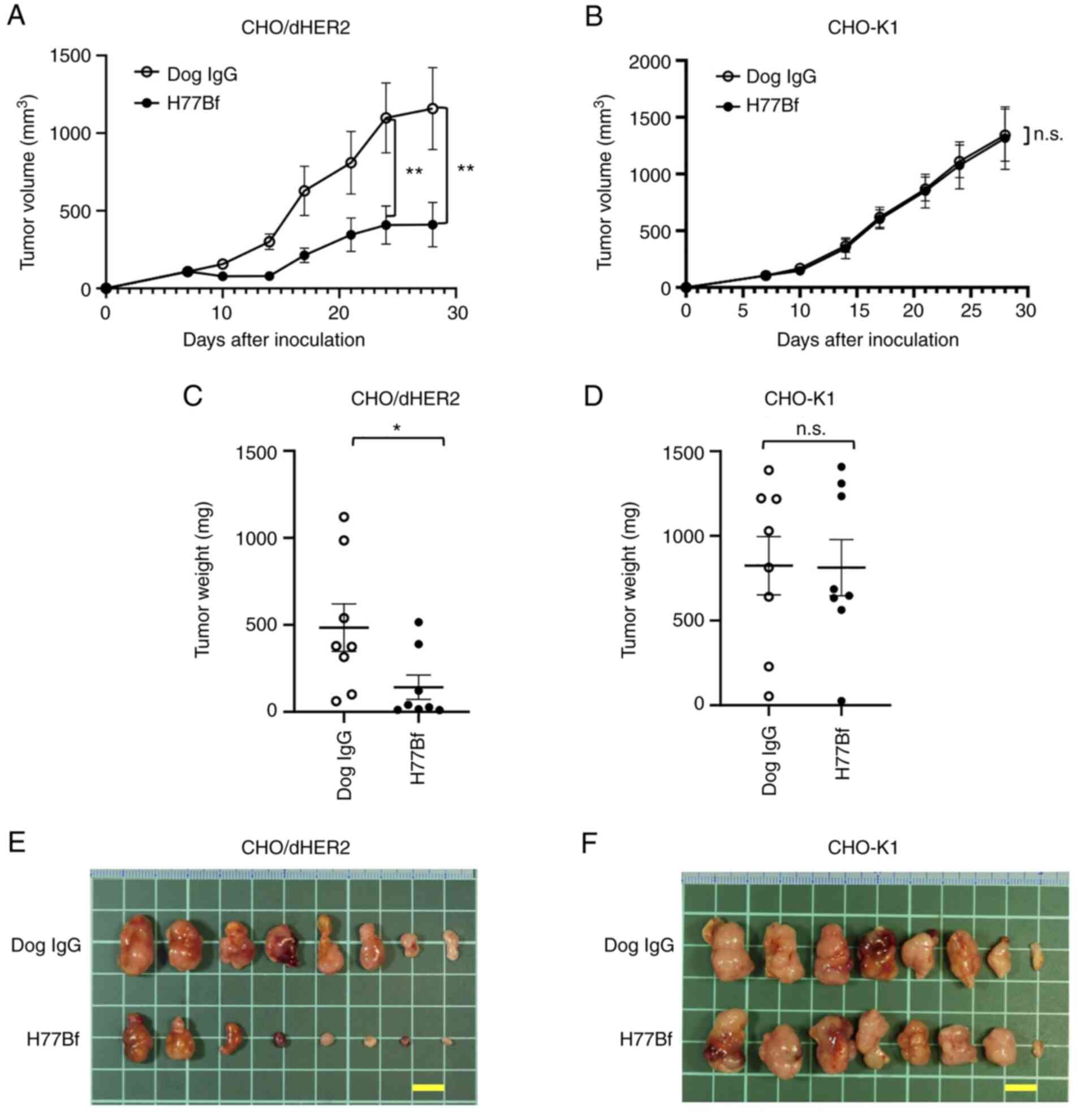
Antitumor effects of H77Bf in the
mouse xenografts of CHO/dHER2 cells
In the CHO/dHER2 ×enograft tumor, H77Bf and control
dog IgG were intraperitoneally injected into mice on days 8, 14 and
21, following the CHO/dHER2 cells injection. On days 7, 10, 14, 17,
21, 24 and 28 after the injection, the tumor volume was measured.
The H77Bf administration resulted in a significant reduction of
tumors on days 24 (P<0.01) and 28 (P<0.01) compared with that
of the control dog IgG (Fig. 3A).
The H77Bf administration resulted in a 65% reduction of the volume
compared with that of the control dog IgG on day 28
post-injection.
The weight of CHO/dHER2 tumors treated with H77Bf
was significantly lower than that treated with control dog IgG (71%
reduction; P<0.05; Fig. 3C).
CHO/dHER2 tumors that were resected from mice on day 28 are
demonstrated in Fig. 3E.
In the CHO-K1 ×enograft models, H77Bf and control
dog IgG were injected intraperitoneally into mice on days 8, 14 and
21 after the injection of CHO-K1 cells. The tumor volume was
measured on days 7, 10, 14, 17, 21, 24 and 28 after the injection
of cells. No difference was observed between H77Bf and control dog
IgG about CHO-K1 tumor volume (Fig.
3B) and CHO-K1 tumor weight (Fig.
3D). CHO-K1 tumors that were resected from mice on day 28 are
demonstrated in Fig. 3F.
The body weights loss and skin disorder were not
observed in CHO/dHER2 (Fig. 4A)
and CHO-K1 (Fig. 4B) tumor-bearing
mice. The mice on day 28 about CHO/dHER2 and CHO-K1 were shown in
Fig. 4C and D, respectively.
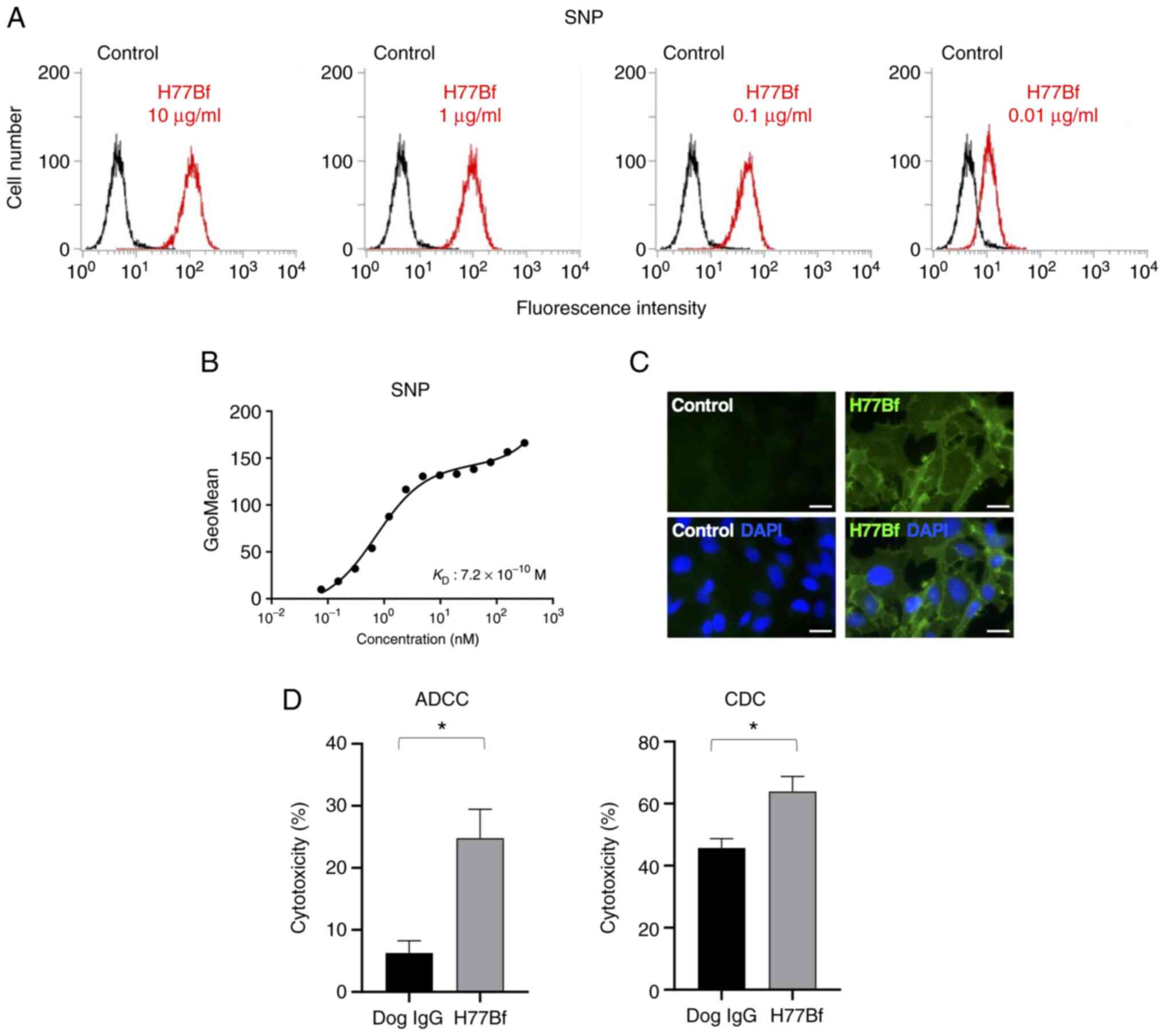
Flow cytometry and immunocytochemical
analysis against SNP cells using H77Bf
As demonstrated in Fig.
5A, H77Bf detected SNP cells dose-dependently. A kinetic
analysis of the binding of H77Bf to SNP cells was performed via
flow cytometry. The KD for the interaction of
H77Bf with SNP cells was 7.2×10−10 M (Fig. 5B), suggesting that H77Bf shows high
affinity for SNP cells.
Immunocytochemical analysis was then performed using
H77Bf for SNP cells. As a result, H77Bf detected dHER2 on SNP cells
(Fig. 5C). Buffer control detected
no signal on SNP cells. These results indicated that H77Bf
recognizes endogenous dHER2 in immunocytochemistry.
H77Bf-mediated ADCC and CDC in SNP
cells
It was investigated whether H77Bf was capable of
mediating ADCC against SNP cells. As revealed in Fig. 5D, H77Bf showed ADCC (24.8%
cytotoxicity) against SNP cells more potently than did the control
dog IgG (6.3% cytotoxicity; P<0.05). It was next investigated
whether H77Bf exhibited CDC against SNP cells. H77Bf induced a
higher degree of CDC (63.9% cytotoxicity) in SNP cells compared
with that induced by control dog IgG (45.7% cytotoxicity;
P<0.05) (Fig. 5D). These
results demonstrated that H77Bf exhibited higher levels of ADCC and
CDC against SNP cells.
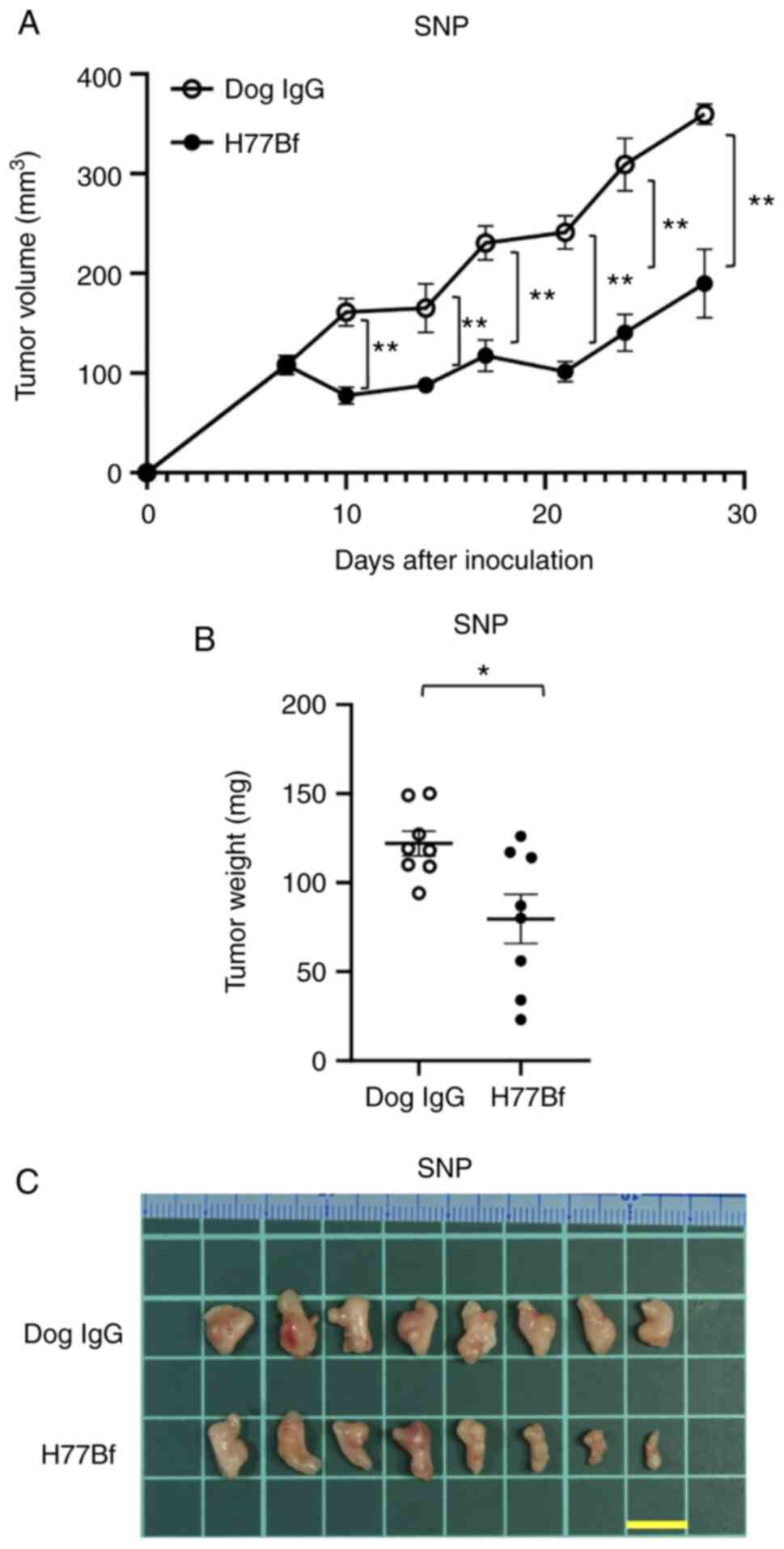
Antitumor effects of H77Bf on SNP
xenografts
In the SNP xenograft models, H77Bf and control dog
IgG were injected intraperitoneally on days 8, 14 and 21, after the
injection of SNP cells. The tumor volume was measured on days 7,
10, 14, 17, 21, 24 and 28 after the injection. The H77Bf
administration resulted in a significant reduction in tumor growth
on days 10 (P<0.01), 14 (P<0.01), 17 (P<0.01), 21
(P<0.01), 24 (P<0.01) and 28 (P<0.01) compared with that
of the control dog IgG (Fig. 6A).
The H77Bf administration resulted in a 47% reduction of tumor
volume compared with that of the control dog IgG on day 28.
Tumors from the H77Bf-treated mice weighed
significantly less than those from the control dog IgG-treated mice
(35% reduction; P<0.05, Fig.
6B). Tumors that were resected from mice on day 28 are
demonstrated in Fig. 6C.
The body weights loss and skin disorder were not
observed in SNP tumor-bearing mice (Fig. 7A). The mice on day 28 about SNP
xenograft were demonstrated in Fig.
7B.
Discussion
Human mAbs that exhibit cross-reactivity to dog have
been investigated. It has been suggested that cetuximab (anti-EGFR)
and trastuzumab (anti-HER2) can bind to certain canine cancer cell
lines (55). The clinical
relevance though is limited considering that those antibodies, such
as trastuzumab, mostly work through ADCC (56). Furthermore, there is a problem that
the humanized mAbs will induce an anti-human immune response in
dogs. Therefore, the caninization of mAbs (only the complementarity
determining regions are non-canine) is essential to develop
antibody therapy for dog. Some caninized mAbs have received
conditional approval by the United States Department of Agriculture
for lymphoma (for example Blontress, targeting CD20; and Tactress,
targeting CD52). However, no peer-reviewed clinical evidence of
efficacy for the mAb has been published (57). In the present study, caninized mAb,
H77Bf was developed from anti-HER2 mAb H2Mab-77. Among
IgG subclasses (A, B, C and D) in dogs, the B and D subclasses were
reported to be involved in ADCC (58). Therefore, B type dog IgG was
converted and a defucosylated mAb was produced, which has been
shown to exhibit more potent ADCC activity through binding to
FcγRIIIa on NK cells (59). The
cross-reactivity and binding affinity of H77Bf to CHO/dHER2 and SNP
cells were first confirmed, and it was found that H77Bf possesses
comparable high binding affinity to CHO/dHER2 (7.5×10−10
M) and SNP (7.2×10−10 M) cells, compared with human
cancer A431 (2.1×10−9 M by H2Mab-77) and
SK-BR-3 (7.3×10−9 M by H2Mab-77) cells, as
previously reported (29). The
quantitative analysis is considered to be essential to apply a
human antibody to dog.
In vivo administration of H77Bf and canine
MNC resulted in significant growth inhibition for CHO/dHER2 and SNP
cells. These results provided evidences to support the suitability
of H77Bf as a promising antibody therapy against canine cancers.
The ADCC activity was also confirmed in vitro using canine
MNCs, suggesting that ADCC activity could contribute to the
antitumor activity of H77Bf. ADCC in humans is executed
predominantly by NK cells through the FcγR that binds to the
IgG1 or IgG3 subclass (60). The FcγR-like receptors have not
been described on canine NK cells. Recently, a cell line-based
assay to measure the ADCC of a canine therapeutic antibody was
reported (61). The aforementioned
study established a human NK cell line, NK-92 cells expressed with
canine FcγR which can be used as effector cells. This system will
contribute to the understanding of NK cell-mediated target cell
lysis by canine therapeutic antibodies. Since the knowledge about
canine NK cells is incomplete, further studies are needed to reveal
the contribution of NK cells to ADCC in dogs. Furthermore, direct
cytotoxic mechanisms by the complement system in dogs is also to be
determined.
Drug-conjugated mAbs rely on direct cytotoxicity of
the payloads through endocytosis of receptor-bound mAbs-drug
conjugate (62,63). Trastuzumab deruxtecan (T-DXd,
DS-8201) is a HER2-targeting antibody conjugated with a novel DNA
topoisomerase I inhibitor (64).
T-DXd showed promising clinical outcomes in patients with
metastatic breast cancer, who had received multiple
anti-HER2-targeting regimens (65). Currently, the clinical efficacy and
safety of T-DXd have been evaluated in various clinical trials.
T-DXd have been approved in not only HER2-positive breast cancer
(65–67), but also HER2-mutant lung cancer
(66). A mouse-canine chimeric mAb
against dog podoplanin (68–70)
(P38B) conjugated with emtansine as the payload (P38B-DM1) was
previously generated and challenged for tumor therapy. P38B-DM1
showed cytotoxicity to podoplanin-expressing cells and exhibited
higher antitumor activity than P38B in the xenograft model
(71). Therefore, H77B-drug
conjugate is one more option to treat dHER2-positive CMT. Recently,
FDA-approved human immune checkpoint inhibitor against PD-1 and
PD-L1 are used in canine tumor treatment (72–74);
the combination of immune checkpoint inhibitors with other
antibody-drugs is expected to be more effective. H77Bf could
contribute to the development of canine cancer treatment, which can
be feedback for human cancer treatment.
IHC has played a critical role as a diagnostic tool
for the identification of neoplasms with conventional
histopathology. In human breast cancer pathology, IHC is routinely
used to assist with the prognosis and to determine the specific
treatment (e.g. trastuzumab) for patients. Although IHC is not
routinely used in CMTs, an increasing number of studies have been
looking for reliable diagnostic and/or prognostic IHC biomarkers
including dHER2 (21). A positive
correlation between dHER2 in serum and tissue expression (by IHC)
was reported (26). There is also
a positive correlation between dHER2 expression and tumor mitotic
index, high histological grade and size (75). However, not all studies have
confirmed this, and no difference between dHER2 expression in
non-neoplastic and neoplastic lesions was observed (76). Furthermore, in contrast to
HER2-positive breast cancer in human, dHER2 amplification and
HER2-enrichment subtype are not observed through whole-exome and
transcriptome analyses of 191 spontaneous CMTs (77). Therefore, the standardization of
dHER2 IHC is essential since those IHC analyses were performed by
different Abs. Our established H2Mab-77 mAb is available
for IHC (29), and its caninized
mAb H77Bf exerts the antitumor activity against dHER2 positive
cells, which could contribute to both diagnosis and therapy for
dHER2-positive canine tumors.
Acknowledgements
The authors would like to thank Ms. Miyuki Yanaka,
Mr. Takuro Nakamura, Mr. Yu Komatsu and Ms. Saori Handa (Department
of Antibody Drug Development, Tohoku University Graduate School of
Medicine) for technical assistance of in vitro experiments,
and Mr. Shun-ichi Ohba and Ms. Akiko Harakawa [Institute of
Microbial Chemistry (BIKAKEN), Numazu, Microbial Chemistry Research
Foundation] for technical assistance of animal experiments.
Funding
The present study was supported in part by Japan Agency for
Medical Research and Development (AMED; grant nos: JP22ama121008,
JP21am0401013, JP22bm1004001, JP22ck0106730 and JP21am0101078).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TO, TT, MS and TA performed the experiments. MKK, MK
and YK designed the experiments. TM prepared canine MNCs. TA, HS,
TY and YK analyzed the data. HS and YK wrote the manuscript. All
authors read and approved the final manuscript and agree to be
accountable for all aspects of the research in ensuring that the
accuracy or integrity of any part of the work are appropriately
investigated and resolved.
Ethics approval and consent to
participate
The animal study protocol was approved (approval no.
2021-056) by the Institutional Committee for Experiments of the
Institute of Microbial Chemistry (Numazu, Japan).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
HER2
|
human epidermal growth factor receptor
2
|
|
mAb
|
monoclonal antibody
|
|
ADCC
|
antibody-dependent cellular
cytotoxicity
|
|
CDC
|
complement-dependent cytotoxicity
|
|
FDA
|
Food and Drug Administration
|
|
PI3K
|
phosphatidylinositol-3 kinase
|
|
TKI
|
tyrosine kinase inhibitor
|
|
FcγR
|
Fcγ, receptor
|
|
NK
|
natural killer
|
|
CMT
|
canine mammary tumor
|
|
RPMI
|
Roswell Park Memorial Institute
|
|
PBS
|
phosphate-buffered saline
|
|
KD
|
dissociation constant
|
|
DAPI
|
4′,6-diamidino-2-phenylindole
|
|
MNC
|
mononuclear cell
|
|
SEM
|
standard error of the mean
|
|
IHC
|
immunohistochemistry
|
|
T-DXd
|
Trastuzumab deruxtecan
|
References
|
1
|
Slamon DJ, Clark GM, Wong SG, Levin WJ,
Ullrich A and McGuire WL: Human breast cancer: Correlation of
relapse and survival with amplification of the HER-2/neu oncogene.
Science. 235:177–182. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Slamon DJ, Leyland-Jones B, Shak S, Fuchs
H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M,
et al: Use of chemotherapy plus a monoclonal antibody against HER2
for metastatic breast cancer that overexpresses HER2. N Engl J Med.
344:783–792. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bang YJ, Van Cutsem E, Feyereislova A,
Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T,
et al: Trastuzumab in combination with chemotherapy versus
chemotherapy alone for treatment of HER2-positive advanced gastric
or gastro-oesophageal junction cancer (ToGA): A phase 3,
open-label, randomised controlled trial. Lancet. 376:687–697. 2010.
View Article : Google Scholar
|
|
4
|
Moasser MM and Krop IE: The evolving
landscape of HER2 targeting in breast cancer. JAMA Oncol.
1:1154–1161. 2015. View Article : Google Scholar
|
|
5
|
Moasser MM: Two dimensions in targeting
HER2. J Clin Oncol. 32:2074–2077. 2014. View Article : Google Scholar
|
|
6
|
Weigelt B, Lo AT, Park CC, Gray JW and
Bissell MJ: HER2 signaling pathway activation and response of
breast cancer cells to HER2-targeting agents is dependent strongly
on the 3D microenvironment. Breast Cancer Res Treat. 122:35–43.
2010. View Article : Google Scholar
|
|
7
|
Le XF, Pruefer F and Bast RC Jr:
HER2-targeting antibodies modulate the cyclin-dependent kinase
inhibitor p27Kip1 via multiple signaling pathways. Cell Cycle.
4:87–95. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yakes FM, Chinratanalab W, Ritter CA, King
W, Seelig S and Arteaga CL: Herceptin-induced inhibition of
phosphatidylinositol-3 kinase and Akt Is required for
antibody-mediated effects on p27, cyclin D1, and antitumor action.
Cancer Res. 62:4132–4141. 2002.PubMed/NCBI
|
|
9
|
Konecny GE, Pegram MD, Venkatesan N, Finn
R, Yang G, Rahmeh M, Untch M, Rusnak DW, Spehar G, Mullin RJ, et
al: Activity of the dual kinase inhibitor lapatinib (GW572016)
against HER-2-overexpressing and trastuzumab-treated breast cancer
cells. Cancer Res. 66:1630–1639. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rusnak DW, Lackey K, Affleck K, Wood ER,
Alligood KJ, Rhodes N, Keith BR, Murray DM, Knight WB, Mullin RJ
and Gilmer TM: The effects of the novel, reversible epidermal
growth factor receptor/ErbB-2 tyrosine kinase inhibitor, GW2016, on
the growth of human normal and tumor-derived cell lines in vitro
and in vivo. Mol Cancer Ther. 1:85–94. 2001.PubMed/NCBI
|
|
11
|
Maadi H, Soheilifar MH, Choi WS,
Moshtaghian A and Wang Z: Trastuzumab mechanism of action; 20 years
of research to unravel a dilemma. Cancers (Basel). 13:35402021.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tsao LC, Force J and Hartman ZC:
Mechanisms of therapeutic antitumor monoclonal antibodies. Cancer
Res. 81:4641–4651. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Musolino A, Gradishar WJ, Rugo HS,
Nordstrom JL, Rock EP, Arnaldez F and Pegram MD: Role of Fcγ
receptors in HER2-targeted breast cancer therapy. J Immunother
Cancer. 10:e0031712022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nordstrom JL, Gorlatov S, Zhang W, Yang Y,
Huang L, Burke S, Li H, Ciccarone V, Zhang T, Stavenhagen J, et al:
Anti-tumor activity and toxicokinetics analysis of MGAH22, an
anti-HER2 monoclonal antibody with enhanced Fcγ receptor binding
properties. Breast Cancer Res. 13:R1232011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
McAndrew NP: Updates on targeting human
epidermal growth factor receptor 2-positive breast cancer: What's
to know in 2021. Curr Opin Obstet Gynecol. 34:41–45. 2022.
View Article : Google Scholar
|
|
16
|
Rugo HS, Im SA, Cardoso F, Cortés J,
Curigliano G, Musolino A, Pegram MD, Wright GS, Saura C,
Escrivá-de-Romaní S, et al: Efficacy of margetuximab vs trastuzumab
in patients with pretreated ERBB2-Positive advanced breast cancer:
A phase 3 randomized clinical trial. JAMA Oncol. 7:573–584. 2021.
View Article : Google Scholar
|
|
17
|
Golay J and Taylor RP: The role of
complement in the mechanism of action of therapeutic anti-cancer
mAbs. Antibodies (Basel). 9:582020. View Article : Google Scholar
|
|
18
|
Reis ES, Mastellos DC, Ricklin D,
Mantovani A and Lambris JD: Complement in cancer: Untangling an
intricate relationship. Nat Rev Immunol. 18:5–18. 2018. View Article : Google Scholar
|
|
19
|
Salas Y, Márquez A, Diaz D and Romero L:
Epidemiological study of mammary tumors in female dogs diagnosed
during the period 2002–2012: A growing animal health problem. PLoS
One. 10:e01273812015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gray M, Meehan J, Martínez-Pérez C, Kay C,
Turnbull AK, Morrison LR, Pang LY and Argyle D: Naturally-occurring
canine mammary tumors as a translational model for human breast
cancer. Front Oncol. 10:6172020. View Article : Google Scholar
|
|
21
|
Kaszak I, Ruszczak A, Kanafa S, Kacprzak
K, Król M and Jurka P: Current biomarkers of canine mammary tumors.
Acta Vet Scand. 60:662018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gama A, Alves A and Schmitt F:
Identification of molecular phenotypes in canine mammary carcinomas
with clinical implications: Application of the human
classification. Virchows Arch. 453:123–132. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Flint AF, U'Ren L, Legare ME, Withrow SJ,
Dernell W and Hanneman WH: Overexpression of the erbB-2
proto-oncogene in canine osteosarcoma cell lines and tumors. Vet
Pathol. 41:291–296. 2004. View Article : Google Scholar
|
|
24
|
Millanta F, Impellizeri J, McSherry L,
Rocchigiani G, Aurisicchio L and Lubas G: Overexpression of HER-2
via immunohistochemistry in canine urinary bladder transitional
cell carcinoma-A marker of malignancy and possible therapeutic
target. Vet Comp Oncol. 16:297–300. 2018. View Article : Google Scholar
|
|
25
|
Yoshimoto S, Kato D, Kamoto S, Yamamoto K,
Tsuboi M, Shinada M, Ikeda N, Tanaka Y, Yoshitake R, Eto S, et al:
Detection of human epidermal growth factor receptor 2
overexpression in canine anal sac gland carcinoma. J Vet Med Sci.
81:1034–1039. 2019. View Article : Google Scholar
|
|
26
|
Campos LC, Silva JO, Santos FS, Araújo MR,
Lavalle GE, Ferreira E and Cassali GD: Prognostic significance of
tissue and serum HER2 and MUC1 in canine mammary cancer. J Vet
Diagn Invest. 27:531–535. 2015. View Article : Google Scholar
|
|
27
|
Brunetti B, Bacci B, Sarli G, Pancioni E
and Muscatello LV: Immunohistochemical screening of HER2 in canine
carcinomas: A preliminary study. Animals (Basel). 11:10062021.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mason NJ, Gnanandarajah JS, Engiles JB,
Gray F, Laughlin D, Gaurnier-Hausser A, Wallecha A, Huebner M and
Paterson Y: Immunotherapy with a HER2-targeting listeria induces
HER2-Specific immunity and demonstrates potential therapeutic
effects in a phase I trial in canine osteosarcoma. Clin Cancer Res.
22:4380–4390. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Itai S, Fujii Y, Kaneko MK, Yamada S,
Nakamura T, Yanaka M, Saidoh N, Chang YW, Handa S, Takahashi M, et
al: H2Mab-77 is a sensitive and specific Anti-HER2 monoclonal
antibody against breast cancer. Monoclon Antib Immunodiagn
Immunother. 36:143–148. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Osaki T, Sunden Y, Sugiyama A, Azuma K,
Murahata Y, Tsuka T, Ito N, Imagawa T and Okamoto Y: Establishment
of a canine mammary gland tumor cell line and characterization of
its miRNA expression. J Vet Sci. 17:385–390. 2016. View Article : Google Scholar
|
|
31
|
Tateyama N, Asano T, Ohishi T, Takei J,
Hosono H, Nanamiya R, Tanaka T, Sano M, Saito M, Kawada M, et al:
An Anti-HER2 monoclonal antibody H2Mab-41 exerts antitumor
activities in mouse xenograft model using dog HER2-overexpressed
cells. Monoclon Antib Immunodiagn Immunother. 40:184–190. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Asano T, Kaneko MK and Kato Y: RIEDL tag:
A novel pentapeptide tagging system for transmembrane protein
purification. Biochem Biophys Rep. 23:1007802020.PubMed/NCBI
|
|
33
|
Asano T, Kaneko MK and Kato Y: Development
of a novel epitope mapping system: RIEDL insertion for epitope
mapping method. Monoclon Antib Immunodiagn Immunother. 40:162–167.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Asano T, Kaneko MK, Takei J, Tateyama N
and Kato Y: Epitope mapping of the Anti-CD44 monoclonal antibody
(C44Mab-46) using the REMAP Method. Monoclon Antib Immunodiagn
Immunother. 40:156–161. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nanamiya R, Sano M, Asano T, Yanaka M,
Nakamura T, Saito M, Tanaka T, Hosono H, Tateyama N, Kaneko MK and
Kato Y: Epitope mapping of an anti-human epidermal growth factor
receptor monoclonal antibody (EMab-51) using the RIEDL insertion
for epitope mapping method. Monoclon Antib Immunodiagn Immunother.
40:149–155. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sano M, Kaneko MK, Aasano T and Kato Y:
Epitope mapping of an antihuman EGFR monoclonal antibody (EMab-134)
Using the REMAP method. Monoclon Antib Immunodiagn Immunother.
40:191–195. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li G, Ohishi T, Kaneko MK, Takei J, Mizuno
T, Kawada M, Saito M, Suzuki H and Kato Y: Defucosylated mouse-dog
chimeric Anti-EGFR antibody exerts antitumor activities in mouse
xenograft models of canine tumors. Cells. 10:35992021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mizuno T, Kato Y, Kaneko MK, Sakai Y,
Shiga T, Kato M, Tsukui T, Takemoto H, Tokimasa A, Baba K, et al:
Generation of a canine anti-canine CD20 antibody for canine
lymphoma treatment. Sci Rep. 10:114762020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Takei J, Kaneko MK, Ohishi T, Hosono H,
Nakamura T, Yanaka M, Sano M, Asano T, Sayama Y, Kawada M, et al: A
defucosylated anti-CD44 monoclonal antibody 5-mG2a-f exerts
antitumor effects in mouse xenograft models of oral squamous cell
carcinoma. Oncol Rep. 44:1949–1960. 2020.PubMed/NCBI
|
|
40
|
Takei J, Ohishi T, Kaneko MK, Harada H,
Kawada M and Kato Y: A defucosylated anti-PD-L1 monoclonal antibody
13-mG2a-f exerts antitumor effects in mouse xenograft models of
oral squamous cell carcinoma. Biochem Biophys Rep.
24:1008012020.PubMed/NCBI
|
|
41
|
Tateyama N, Nanamiya R, Ohishi T, Takei J,
Nakamura T, Yanaka M, Hosono H, Saito M, Asano T, Tanaka T, et al:
Defucosylated anti-epidermal growth factor receptor monoclonal
antibody 134-mG2a-f exerts antitumor activities in mouse
xenograft models of dog epidermal growth factor
receptor-overexpressed cells. Monoclon Antib Immunodiagn
Immunother. 40:177–183. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kato Y, Mizuno T, Yamada S, Nakamura T,
Itai S, Yanaka M, Sano M and Kaneko MK: Establishment of P38Bf, a
core-fucose-deficient mouse-canine chimeric antibody against dog
podoplanin. Monoclon Antib Immunodiagn Immunother. 37:218–223.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Asano T, Ohishi T, Takei J, Nakamura T,
Nanamiya R, Hosono H, Tanaka T, Sano M, Harada H, Kawada M, et al:
AntiHER3 monoclonal antibody exerts antitumor activity in a mouse
model of colorectal adenocarcinoma. Oncol Rep. 46:1732021.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tanaka T, Ohishi T, Asano T, Takei J,
Nanamiya R, Hosono H, Sano M, Harada H, Kawada M, Kaneko MK and
Kato Y: An antiTROP2 monoclonal antibody TrMab6 exerts antitumor
activity in breast cancer mouse xenograft models. Oncol Rep.
46:1322021. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Hosono H, Ohishi T, Takei J, Asano T,
Sayama Y, Kawada M, Kaneko MK and Kato Y: The anti-epithelial cell
adhesion molecule (EpCAM) monoclonal antibody EpMab-16 exerts
antitumor activity in a mouse model of colorectal adenocarcinoma.
Oncol Lett. 20:3832020. View Article : Google Scholar
|
|
46
|
Kaneko MK, Ohishi T, Takei J, Sano M,
Nakamura T, Hosono H, Yanaka M, Asano T, Sayama Y, Harada H, et al:
AntiEpCAM monoclonal antibody exerts antitumor activity against
oral squamous cell carcinomas. Oncol Rep. 44:2517–2526. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kaneko MK, Ohishi T, Nakamura T, Inoue H,
Takei J, Sano M, Asano T, Sayama Y, Hosono H, Suzuki H, et al:
Development of core-fucose-deficient humanized and chimeric
anti-human podoplanin antibodies. Monoclon Antib Immunodiagn
Immunother. 39:167–174. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Hosono H, Takei J, Ohishi T, Sano M, Asano
T, Sayama Y, Nakamura T, Yanaka M, Kawada M, Harada H, et al:
AntiEGFR monoclonal antibody 134mG2a exerts antitumor effects in
mouse xenograft models of oral squamous cell carcinoma. Int J Mol
Med. 46:1443–1452. 2020.PubMed/NCBI
|
|
49
|
Ohishi T, Kato Y, Kaneko MK, Ohba SI,
Inoue H, Harakawa A and Kawada M: Anti-metastatic activity of an
anti-EGFR monoclonal antibody against metastatic colorectal cancer
with KRAS p.G13D mutation. Int J Mol Sci. 21:60372020. View Article : Google Scholar
|
|
50
|
Takei J, Kaneko MK, Ohishi T, Kawada M,
Harada H and Kato Y: H2Mab-19, an anti-human epidermal growth
factor receptor 2 monoclonal antibody exerts antitumor activity in
mouse oral cancer xenografts. Exp Ther Med. 20:846–853. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kato Y, Ohishi T, Takei J, Nakamura T,
Sano M, Asano T, Sayama Y, Hosono H, Kawada M and Kaneko MK: An
anti-human epidermal growth factor receptor 2 monoclonal antibody
H2Mab-19 exerts antitumor activity in mouse colon cancer
xenografts. Monoclon Antib Immunodiagn Immunother. 39:123–128.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Takei J, Kaneko MK, Ohishi T, Kawada M,
Harada H and Kato Y: A novel anti-EGFR monoclonal antibody
(EMab-17) exerts antitumor activity against oral squamous cell
carcinomas via antibody-dependent cellular cytotoxicity and
complement-dependent cytotoxicity. Oncol Lett. 19:2809–2816.
2020.
|
|
53
|
Itai S, Ohishi T, Kaneko MK, Yamada S, Abe
S, Nakamura T, Yanaka M, Chang YW, Ohba SI, Nishioka Y, et al:
Anti-podocalyxin antibody exerts antitumor effects via
antibody-dependent cellular cytotoxicity in mouse xenograft models
of oral squamous cell carcinoma. Oncotarget. 9:22480–22497. 2018.
View Article : Google Scholar
|
|
54
|
Kato Y, Ohishi T, Yamada S, Itai S, Takei
J, Sano M, Nakamura T, Harada H, Kawada M and Kaneko MK: Anti-Human
epidermal growth factor receptor 2 monoclonal antibody H2Mab-41
exerts antitumor activity in a mouse xenograft model of colon
cancer. Monoclon Antib Immunodiagn Immunother. 38:157–161. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Singer J, Weichselbaumer M, Stockner T,
Mechtcheriakova D, Sobanov Y, Bajna E, Wrba F, Horvat R, Thalhammer
JG, Willmann M and Jensen-Jarolim E: Comparative oncology: ErbB-1
and ErbB-2 homologues in canine cancer are susceptible to cetuximab
and trastuzumab targeting. Mol Immunol. 50:200–209. 2012.
View Article : Google Scholar
|
|
56
|
Collins DM, O'Donovan N, McGowan PM,
O'Sullivan F, Duffy MJ and Crown J: Trastuzumab induces
antibody-dependent cell-mediated cytotoxicity (ADCC) in
HER-2-non-amplified breast cancer cell lines. Ann Oncol.
23:1788–1795. 2012. View Article : Google Scholar
|
|
57
|
Klingemann H: Immunotherapy for dogs:
Still running behind humans. Front Immunol. 12:6657842021.
View Article : Google Scholar
|
|
58
|
Bergeron LM, McCandless EE, Dunham S,
Dunkle B, Zhu Y, Shelly J, Lightle S, Gonzales A and Bainbridge G:
Comparative functional characterization of canine IgG subclasses.
Vet Immunol Immunopathol. 157:31–41. 2014. View Article : Google Scholar
|
|
59
|
Shinkawa T, Nakamura K, Yamane N,
Shoji-Hosaka E, Kanda Y, Sakurada M, Uchida K, Anazawa H, Satoh M,
Yamasaki M, et al: The absence of fucose but not the presence of
galactose or bisecting N-acetylglucosamine of human IgG1
complex-type oligosaccharides shows the critical role of enhancing
antibody-dependent cellular cytotoxicity. J Biol Chem.
278:3466–3473. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Kubota T, Niwa R, Satoh M, Akinaga S,
Shitara K and Hanai N: Engineered therapeutic antibodies with
improved effector functions. Cancer Sci. 100:1566–1572. 2009.
View Article : Google Scholar
|
|
61
|
Mizuno T, Takeda Y, Tsukui T and Igase M:
Development of a cell line-based assay to measure the
antibody-dependent cellular cytotoxicity of a canine therapeutic
antibody. Vet Immunol Immunopathol. 240:1103152021. View Article : Google Scholar
|
|
62
|
Scott AM, Wolchok JD and Old LJ: Antibody
therapy of cancer. Nat Rev Cancer. 12:278–287. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Zahavi D and Weiner L: Monoclonal
antibodies in cancer therapy. Antibodies (Basel). 9:342020.
View Article : Google Scholar
|
|
64
|
Takegawa N, Nonagase Y, Yonesaka K, Sakai
K, Maenishi O, Ogitani Y, Tamura T, Nishio K, Nakagawa K and
Tsurutani J: DS-8201a, a new HER2-targeting antibody-drug conjugate
incorporating a novel DNA topoisomerase I inhibitor, overcomes
HER2-positive gastric cancer T-DM1 resistance. Int J Cancer.
141:1682–1689. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Modi S, Saura C, Yamashita T, Park YH, Kim
SB, Tamura K, Andre F, Iwata H, Ito Y, Tsurutani J, et al:
Trastuzumab deruxtecan in previously treated HER2-Positive Breast
Cancer. N Engl J Med. 382:610–621. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Li BT, Smit EF, Goto Y, Nakagawa K,
Udagawa H, Mazières J, Nagasaka M, Bazhenova L, Saltos AN, Felip E,
et al: Trastuzumab Deruxtecan in HER2-Mutant Non-Small-Cell Lung
Cancer. N Engl J Med. 386:241–251. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Shitara K, Bang YJ, Iwasa S, Sugimoto N,
Ryu MH, Sakai D, Chung HC, Kawakami H, Yabusaki H, Lee J, et al:
Trastuzumab deruxtecan in previously treated HER2-positive gastric
cancer. N Engl J Med. 382:2419–2430. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kaneko MK, Honma R, Ogasawara S, Fujii Y,
Nakamura T, Saidoh N, Takagi M, Kagawa Y, Konnai S and Kato Y:
PMab-38 recognizes canine podoplanin of squamous cell carcinomas.
Monoclon Antib Immunodiagn Immunother. 35:263–266. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Ito A, Ohta M, Kato Y, Inada S, Kato T,
Nakata S, Yatabe Y, Goto M, Kaneda N, Kurita K, et al: A real-time
near-infrared fluorescence imaging method for the detection of oral
cancers in mice using an indocyanine green-labeled podoplanin
antibody. Technol Cancer Res Treat. 17:15330338187679362018.
View Article : Google Scholar
|
|
70
|
Kato Y, Ohishi T, Kawada M, Maekawa N,
Konnai S, Itai S, Yamada S and Kaneko MK: The mouse-canine chimeric
anti-dog podoplanin antibody P38B exerts antitumor activity in
mouse xenograft models. Biochem Biophys Rep. 17:23–26.
2019.PubMed/NCBI
|
|
71
|
Kato Y, Ito Y, Ohishi T, Kawada M,
Nakamura T, Sayama Y, Sano M, Asano T, Yanaka M, Okamoto S, et al:
Antibody-drug conjugates using mouse-canine chimeric anti-dog
podoplanin antibody exerts antitumor activity in a mouse xenograft
model. Monoclon Antib Immunodiagn Immunother. 39:37–44. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Pantelyushin S, Ranninger E, Guerrera D,
Hutter G, Maake C, Markkanen E, Bettschart-Wolfensberger R, Rohrer
Bley C, Läubli H and Vom Berg J: Cross-reactivity and functionality
of approved human immune checkpoint blockers in dogs. Cancers
(Basel). 13:7852021. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Maekawa N, Konnai S, Nishimura M, Kagawa
Y, Takagi S, Hosoya K, Ohta H, Kim S, Okagawa T, Izumi Y, et al:
PD-L1 immunohistochemistry for canine cancers and clinical benefit
of anti-PD-L1 antibody in dogs with pulmonary metastatic oral
malignant melanoma. NPJ Precis Oncol. 5:102021. View Article : Google Scholar
|
|
74
|
Klingemann H: Immunotherapy for dogs:
Running behind humans. Front Immunol. 9:1332018. View Article : Google Scholar
|
|
75
|
Muhammadnejad A, Keyhani E, Mortazavi P,
Behjati F and Haghdoost IS: Overexpression of her-2/neu in
malignant mammary tumors; translation of clinicopathological
features from dog to human. Asian Pac J Cancer Prev. 13:6415–6421.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Ressel L, Puleio R, Loria GR, Vannozzi I,
Millanta F, Caracappa S and Poli A: HER-2 expression in canine
morphologically normal, hyperplastic and neoplastic mammary tissues
and its correlation with the clinical outcome. Res Vet Sci.
94:299–305. 2013. View Article : Google Scholar
|
|
77
|
Kim TM, Yang IS, Seung BJ, Lee S, Kim D,
Ha YJ, Seo MK, Kim KK, Kim HS, Cheong JH, et al: Cross-species
oncogenic signatures of breast cancer in canine mammary tumors. Nat
Commun. 11:36162020. View Article : Google Scholar : PubMed/NCBI
|