Introduction
As the most common cause of cancer-related deaths in
the world, lung cancer causes ~1.8 million deaths every year
(1), of which non-small-cell lung
cancer (NSCLC) accounts for ~80% of lung cancer cases and its
incidence rate is increasing yearly (2). Early diagnosis of lung cancer is
challenging, and a number of patients are already in the advanced
stage of cancer when diagnosed, which markedly reduces the
effectiveness of treatment. Meanwhile, the therapeutic effects of
some traditional chemotherapy drugs, such as cisplatin, paclitaxel
and carboplatin, remain very limited and exhibit high toxicity,
leading to serious side effects (3). Accordingly, exploring the pathogenesis
of NSCLC and discovering new effective treatment methods remain the
main obstacles that need to be addressed.
Natural products derived from plants have been
widely used since ancient times to prevent and treat various
diseases. Low-toxicity, low-cost natural products with anticancer
properties have always been of great concern (4,5).
Quinones are an interesting class of compounds developed for the
treatment of cancer, such as purpurin, lapachine and emodin
(6–8), which are expected to be used in
clinical adjuvant anticancer therapy to improve anticancer efficacy
and reduce the toxic side effects of chemotherapy alone.
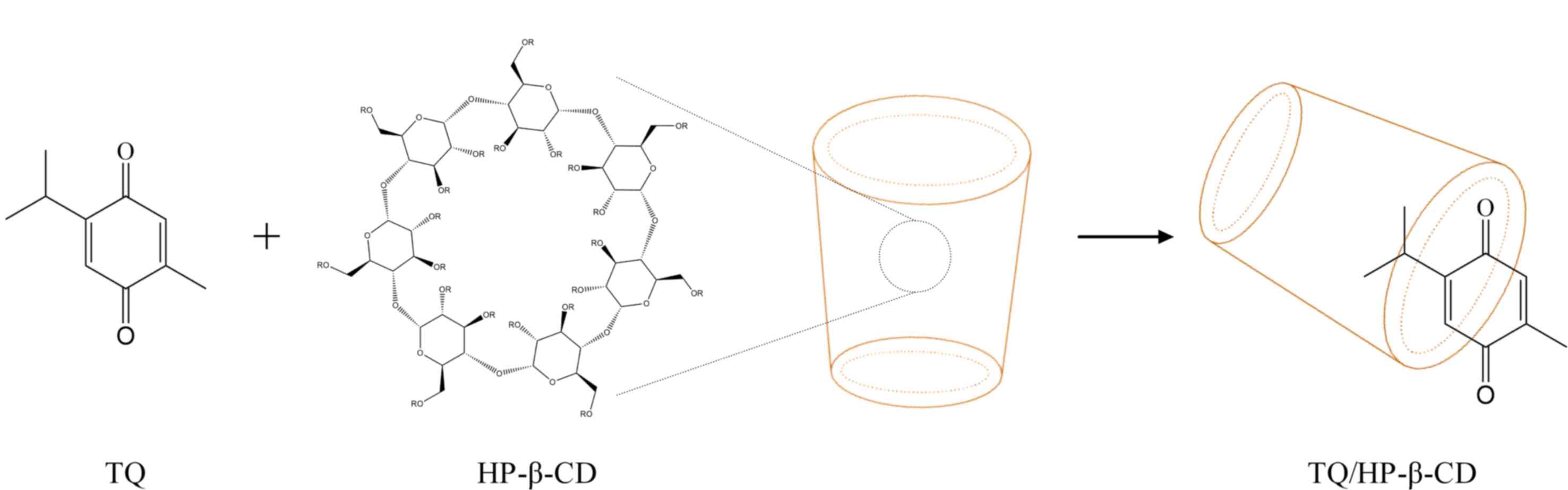
Thymoquinone (TQ) (Fig. 1) is the
primary substance that exerts biological effects in the volatile
oil of the black seed (Nigella sativa) and has been widely
used as an antibacterial, antiviral and hypoglycemic medicine for
over two centuries (9,10). In addition, TQ has shown promising
antitumor properties on several types of cancer cells. Zhao et
al (11) discovered that TQ
reduces the survival, migration and invasion of pancreatic cancer
cells by regulating the PI3K/AKT/mTOR pathway. Taiyab et al
(12) also reported the role of TQ
in breast cancer, indicating that it inhibits cell proliferation
and induces cell apoptosis. Recently, it has been proven that TQ
markedly inhibited the proliferation of NSCLC (13). A significant feature is that TQ can
induce cytotoxicity and apoptosis in cancer cells while being
relatively non-toxic to normal cells (9,10).
Based on the aforementioned research, it is not difficult to find
that TQ may have broad-spectrum anticancer properties. However, due
to its low bioavailability, TQ's poor aqueous solubility and
photosensitivity severely restrict its biomedical application.
Therefore, various solubilizers and drug carriers
are employed to promote the efficacy of hydrophobic drugs by
increasing solubility and bioavailability (14,15).
Among all solubility enhancement preparation methods, cyclodextrins
(CDs) complexation to form drug-inclusion complexes has markedly
improved the water solubility of lipophilic drugs, making it widely
used in the pharmaceutical field (16). In addition, the CD inclusion process
can also improve the pharmacological properties of these compounds,
such as eliminating unpleasant odors and flavors (17). CDs are a class of cyclic
oligosaccharides obtained from starch through enzymatic reactions,
which are non-toxic and biodegradable under certain conditions. The
microstructure of CDs presents a unique truncated cone shape
consisting of a hydrophilic exterior surface and a hydrophobic
interior cavity. When hydrophobic organic molecules enter the
internal cavity of CDs, they form inclusion complexes. CDs are
divided into three natural forms based on the number of pyranose
glucose units: α-CD, β-CD and γ-CD (18). Among different CD family members,
β-CD is widely used due to its easy availability and low cost.
Hydroxypropyl-β-cyclodextrin (HP-β-CD), as a derivative of β-CD
(Fig. 1), has been included in the
GRAS list since 1998 as a fragrance carrier and protectant due to
its higher solubility and more excellent biocompatibility (19). Subsequently, with the development of
supramolecular functional materials, HP-β-CD has become a highly
valuable and attractive nano-delivery carrier, widely used in
anticancer agents. Previous research demonstrated that the
encapsulation of paclitaxel by HP-β-CD can increase its dissolution
rate, cytotoxicity and intracellular accumulation (20). Saha et al (21) reported that trans-resveratrol
(RES) embedded in HP-β-CD exhibits more potent antitumor activity
than free RES and its effect on preventing tumor growth in
vivo is more significant. Early literature reported on the
formation of inclusion complexes between TQ and different types of
CDs (22–24), such as TQ/SBE-β-CD exhibiting
enhanced water solubility and growth inhibitory effects on leukemia
cells (24). However, to the best
of the authors' knowledge, there is currently no literature on the
growth inhibitory effect of this complex on tumors in vivo,
let alone the specific mechanism by which TQ/CD complexes exert
anticancer effects.
The present study comprehensively characterized the
inclusion complex between TQ and HP-β-CD. The authors also analyzed
the effects of pure TQ and the TQ/HP-β-CD inclusion complex on the
growth and ferroptosis of NSCLC cells both in vitro and
in vivo, as well as the possible signaling pathways involved
(NF-κB pathway), which is a novel domain.
Materials and methods
Reagents
HP-β-CD (MW 1396), TQ (MW 164), ferroptosis
inhibitor (Ferrostatin-1) and NF-κB activator (PMA) were purchased
from Shanghai Aladdin Biochemical Technology Co., Ltd. Cell
Counting Kit-8 (CCK-8) reagent (cat. no. AB0101), BeyoClick™
EdU-594 Kit (cat. no. C0071S), Hochest 33258 staining Kit (cat. no.
C1011), DCFH-DA (cat. no. S0036S), dimethyl sulfoxide (DMSO) (cat.
no. ST038), MDA Assay Kit (cat. no. S0131S), hematoxylin-eosin
(H&E) staining Kit (cat. no. C02-04004), normal goat serum
blocking solution (cat. no. P0260), HRP-labeled goat anti-rabbit
secondary antibody (cat. no. A0181) and reduced glutathione (GSH)
Assay Kit (cat. no. S0053) were obtained from Beyotime Institute of
Biotechnology. C11-BODIPY 581/591 kit (cat. no. D3861) was obtained
from Invitrogen; Thermo Fisher Scientific, Inc.. Anti-p-NF-κB (cat.
no. ab207297) and anti-Ki-67 (cat. no. ab15580) were purchased from
Abcam.
Preparation and characterization of
TQ/HP-β-CD inclusion complex
TQ/HP-β-CD was prepared by the freeze-drying method
following the protocol previously reported (22,23).
TQ/HP-β-CD inclusion complex was characterized by Fourier transform
infrared (FT-IR) spectrophotometry (Avatar 370, Thermo-Nicolet;
Thermo Fisher Scientific, Inc.), Powder X-ray diffraction (XRD)
(Shimadzu Corporation), differential scanning calorimetry (DSC)
(3500 Sirius, NETZSCH Group), and scanning electron microscopy
(SEM) (Nova Nano SEM 230; Thermo Fisher Scientific, Inc.) as
previously reported (22–24).
Determination of phase solubility
The phase solubility study was conducted according
to the methods described in previous literature (22). Briefly, excess TQ or TQ/HP-β-CD
inclusion complex is added to distilled water with a pH of 7.0 and
stirred continuously at 500 × g for 24 h at 37°C. After filtering
the suspension, the phase solubility is detected using an
ultraviolet (UV)-visible spectrometer. The apparent stability
constant (K) and complexation efficiency (CE) are calculated from
the solubility diagram using the following equations:
K=Slope/S0. (1-Slope) and CE=Slope/(1-Slope).
S0 is the solubility of TQ in the absence of HP-β-CD,
and Slope is the corresponding slope of the phase solubility
diagram.
Determination of drug release rate in
vitro
A total of 0.1 g of TQ and 0.94 g of TQ/HP-β-CD
inclusion complex (containing 0.1 g of TQ) were added each to 50 ml
of PBS (pH=7.4) and then stirred continuously at a speed of 100 × g
for 24 h at 37°C. At the predetermined time, 1 ml of the
supernatant solution was removed and replaced with an equal volume
of fresh medium. The drug release rate was determined by a
UV-visible spectrometer and calculated using the following
equation: Drug release rate (%)=D1/D2 ×100%.
D1 is the amount of released drug within a certain
period and D2 is the total amount of drug.
Hemolytic compatibility assay
Heparin sodium was added to the collected fresh
blood samples to prevent coagulation. The venous blood was divided
into three layers after centrifuging at 2,000 × g for 5 min. The
red blood cells were separated from plasma and the remaining red
blood cells were washed three times with normal saline to remove
residual white blood cells. After that, the red blood cells were
diluted with normal saline to prepare a 4% red blood cell
solution.
A total of 300 µl of TQ/HP-β-CD solution with
different concentrations (50, 100, 200, 400, 800, 1,500, 3,000
µmol/l), 1.2 ml of erythrocyte solution, and 1.2 ml of saline were
added to 5-ml centrifuge tubes. A total of 1.5 ml of 4% red blood
cell solution and 1.5 ml of deionized water were added to the test
tube of the positive control group. In total, 1.5 ml of 4% red
blood cell solution and 1.5 ml of normal saline were added to the
test tube of the negative control group. The test tube was
incubated in a 37°C constant-temperature incubator for 1 and 24 h,
respectively. The tubes were centrifuged at a speed of 2,000 × g
for 5 min to precipitate red blood cells. The absorbance value of
the supernatant at 450 nm was detected with a microplate
reader.
The hemolysis rate of the positive control group was
set as 100%, and the hemolysis rate of the TQ/HP-β-CD group was
calculated according to the following equation: Hemolysis rate
(%)=(A1/A0) ×100%. A1 is the
absorbance value of the TQ/HP-β-CD group, and A0 is the
absorbance value of the positive control group.
Cell culture
Two immortalized NSCLC cell lines (A549 and HCC827)
were obtained from the American Type Culture Collection and were
incubated as previously described (11).
Cell uptake assessment
A549 cells were plated at a density of
5×104 cells per well onto transparent microporous
membrane inserts (Thincerts™; 1 µm pore size, 1.13 cm2
surface area) within 12-well culture plates. Growth medium was
introduced into the basolateral (1.0 ml) and apical (0.5 ml)
compartments and refreshed at two-day intervals throughout a 21-day
differentiation phase. Cultures were incubated at 37°C with 90%
humidity. Monolayers achieved experimental readiness when
transepithelial electrical resistance stabilized within the 200–300
Ω·cm2 range.
Both TQ solution and the TQ/HP-β-CD inclusion
complex were diluted in Hanks' solution to yield equivalent final
TQ concentrations of 25 µmol/l. These test formulations were
apically administered to the differentiated monolayers.
Permeability assessments commenced by adding 0.5 ml of test
solution to the apical chamber and 1.0 ml of Hanks' solution to the
basolateral chamber. Aliquots were periodically collected from the
basolateral compartment for quantitative analysis via high
performance liquid chromatography.
The apparent permeability coefficient (Papp, cm/s)
was derived using the equation: Papp=dQ/(dt × A × C0).
dQ/dt is the steady-state permeation rate (mass/time),
C0 is the initial apical drug concentration, and A is
the monolayer surface area (cm2).
Cell viability assay
The increasing concentrations of TQ, HP-β-CD, and
TQ/HP-β-CD in the treatment group were 12.5, 25, 50, 100, 200, 300,
and 400 µmol/l. TQ was dissolved in DMSO to prepare a 50 mmol/l
mother solution.
Different concentrations of TQ samples were obtained
by diluting the mother liquor with a DMEM medium and labeling it as
the TQ/DMSO group. TQ was dissolved in a DMEM medium to obtain TQ
samples of different concentrations labeled as TQ/H2O
group. HP-β-CD was dissolved in a DMEM medium to obtain different
concentrations of HP-β-CD samples, which were labeled as the
HP-β-CD group. TQ/HP-β-CD inclusion complex was dissolved in DMEM
medium to obtain TQ/HP-β-CD samples of different concentrations,
labeled as TQ/HP-β-CD group.
A total of 1×104 A549 or HCC827 cells
were cultivated in 96-well plates with different concentrations of
TQ, HP-β-CD, and TQ/HP-β-CD as aforementioned for 24 h. A total of
10 µl of CCK-8 reagent was added to each well of a 96-well plate,
followed by incubation at 37°C for 1 h, and the absorbance value
was detected at 570 nm with a microplate reader. The value of
IC50 was analyzed using GraphPad software 8.0 software
(Dotmatics). The growth inhibitory rate was calculated according to
the following equation: Growth inhibitory rate
(%)=(1-A1/A0) ×100%. A1 is the
absorbance value of the treatment group, and A0 is the
absorbance value of the negative control group.
5-Ethynyl-2′-deoxyuridine (EdU)
assay
A549 or HCC827 cells at logarithmic growth phase
were inoculated into a 96-well plate and treated with different
drugs for 24 h. EdU working solution was added and cells remained
for 2 h in a 37°C incubator. Pre-cooled 4% paraformaldehyde was
added, and cells were incubated at room temperature for 30 min. A
total of 0.5% Triton X-100 was used to permeate the membrane for 20
min and react with Hoechst 33342 reaction solution in the dark for
30 min. Finally, the image was analyzed using ImageJ software
(version 1.51j8; National Institutes of Health).
Collagen sprout outgrowth assay
The proliferation and migration activities were
measured in A549 or HCC827 cells by the collagen sprout outgrowth
assay as previously described (25).
Reactive oxygen species (ROS)
detection
A549 or HCC827 cells at logarithmic growth phase
were inoculated into a 6-well plate, treated with different drugs
for 24 h at 37°C, and then washed three times with PBS. Then, ROS
was measured using fluorescence microscopy and flow cytometry,
respectively. DCFH-DA was used to detect the ROS levels according
to the manufacturer's protocol. In brief, A549 or HCC827 cells at
logarithmic growth phase were seeded in 6-well plates and cultured
with different drugs for 24 h at 37°C. After treatment, cells were
harvested and washed three times with PBS and labeled with 20
µmol/l DCFH-DA under 37°C for 30 min in the dark. The cells were
then washed with PBS, followed by fluorescence microscopy imaging
(Zeiss LSM800; Zeiss GmbH). ROS levels were detected using BD
FACS-Calibur flow cytometer (BD Biosciences), and the fluorescence
intensity of ROS was analyzed with FlowJo software (FlowJo
LLC).
Detection of lipid peroxidation
The level of lipid peroxidation in
1.0×105 A549 or HCC827 cells was measured using the
C11-BODIPY 581/591 kit according to the manufacturer's
protocol.
Measurement of malondialdehyde (MDA)
and GSH/ oxidized glutathione (GSSG) ratio
After 2.0×105 A549 or HCC827 cells were
treated with different drugs for 24 h, the content of MDA and
GSH/GSSG ratio were determined according to the manufacturer's
protocol.
Electrophoretic mobility shift assay
(EMSA)
Nuclear extracts were extracted from A549 cells and
incubated with IRDye-700-labeled NF-κb oligonucleotides for
electrophoretic mobility shift assay, as previously described
(26).
Mouse xenograft model
A total of 15 female BALB/c nude mice (6 weeks old,
~22 g) were purchased from Beijing Weitong Lihua Company. Animals
were housed under specific pathogen-free conditions at a controlled
temperature of 22±2°C, 50±10% relative humidity, and a 12/12-h
light-dark cycle with ad libitum access to autoclaved water and
standard rodent chow. Environmental enrichment (for example,
nesting material and shelters) was provided. All animal experiments
followed the ARRIVE guidelines and were approved (approval no.
20240215001) by the Animal Care and Ethics Committee of Ma'anshan
People's Hospital (Ma'anshan, China) conducted in strict accordance
with the UK Animals (Scientific Procedures) Act 1986 and relevant
institutional guidelines.
Each mouse was subcutaneously injected with
5×106 A549 cells under brief isoflurane anesthesia (4%
induction, 2% maintenance in oxygen). Tumor size was measured daily
using digital calipers with volume calculated as (Length ×
Width2)/2. Animal health and behavior (posture,
mobility, grooming, spontaneous activity, and signs of
pain/distress) were assessed twice daily throughout the study.
Pre-defined humane endpoints requiring immediate euthanasia
included: Tumor volume >1,500 mm3, tumor ulceration
or necrosis >15% surface area, body weight loss >20% from
baseline, inability to access food/water, or severe
lethargy/distress.
When tumors reached ~100 mm3, mice were
randomly assigned to treatment groups (n=5/group): untreated
control, TQ group, or TQ/HP-β-CD group. The experimental duration
post-grouping was 28 days. The TQ group received intraperitoneal
injections of 100 µl solution containing 3 mg TQ every other day.
The TQ/HP-β-CD group received intraperitoneal injections of 100 µl
solution containing 28.2 mg TQ/HP-β-CD (equivalent to 3 mg TQ)
every other day. The control group received no treatment. All mice
survived to the scheduled endpoint. On day 28, mice were euthanized
by cervical dislocation under deep isoflurane anesthesia (5%
induction in oxygen). Death was confirmed by absence of detectable
heartbeat (cardiac palpation), absence of respiratory movements for
>5 min, and fixed dilated pupils. Liver, kidney and tumor
tissues were immediately collected post-mortem for analysis.
Welfare considerations included: i) Anesthesia for tumor
implantation and euthanasia (isoflurane: 4% induction/2%
maintenance for implantation; 5% for euthanasia) ii) strict humane
endpoints iii) twice-daily health monitoring iv) environmental
enrichment and v) minimized injection volumes. No analgesics were
administered during treatment as injections caused only transient
discomfort without observable distress. No animals required early
euthanasia or were found dead during the study.
Histopathology and
immunohistochemistry (IHC)
The liver, kidney, and tumor tissues were placed in
4% paraformaldehyde for 48 h. Then, the tissues were embedded in
paraffin and cut into thin slices (4 µm). Routine H&E and Perl
staining were then performed on the slices. IHC for Ki-67 and NF-κb
as also performed on paraffin-embedded tissue sections.
Paraffin-embedded tissue sections were baked at 65°C, dewaxed,
hydrated, and subjected to antigen retrieval using citrate sodium
buffer. Endogenous peroxidase activity was blocked with 3%
H2O2. Sections were blocked with normal goat
serum blocking solution at room temperature for 30 min. Primary
antibodies were then applied: Ki-67 (1:200) or NF-κB p65 (1:100),
and incubated at 4°C overnight. After washing with PBS, HRP-labeled
goat anti-rabbit secondary antibody (1:200) was added and incubated
at room temperature for 1 h. DAB was used for color development,
followed by counterstaining with hematoxylin. Finally, the sections
were dehydrated, cleared, and mounted. Slices were observed and
images were captured using an Olympus BX41 optical microscope
(Olympus Corporation).
Statistical analysis
Three independent experiments were conducted, with
data presented as the mean ± SD of absolute values or control
percentages. Statistical analysis was conducted using GraphPad
Prism 8.0 software (Dotmatics). The differences between two or more
groups were confirmed through one-way ANOVA followed by Tukey's
post hoc test. P-<0.05 (on both sides) was considered to
indicate a statistically significant difference.
Results
Physicochemical characterization of
TQ/HP-β-CD
Based on previous studies (22,23),
the freeze-drying method was employed in the present study to
prepare TQ/HP-β-CD inclusion complexes in a 1:1 molar ratio and
characterize and biologically validate them.
FT-IR
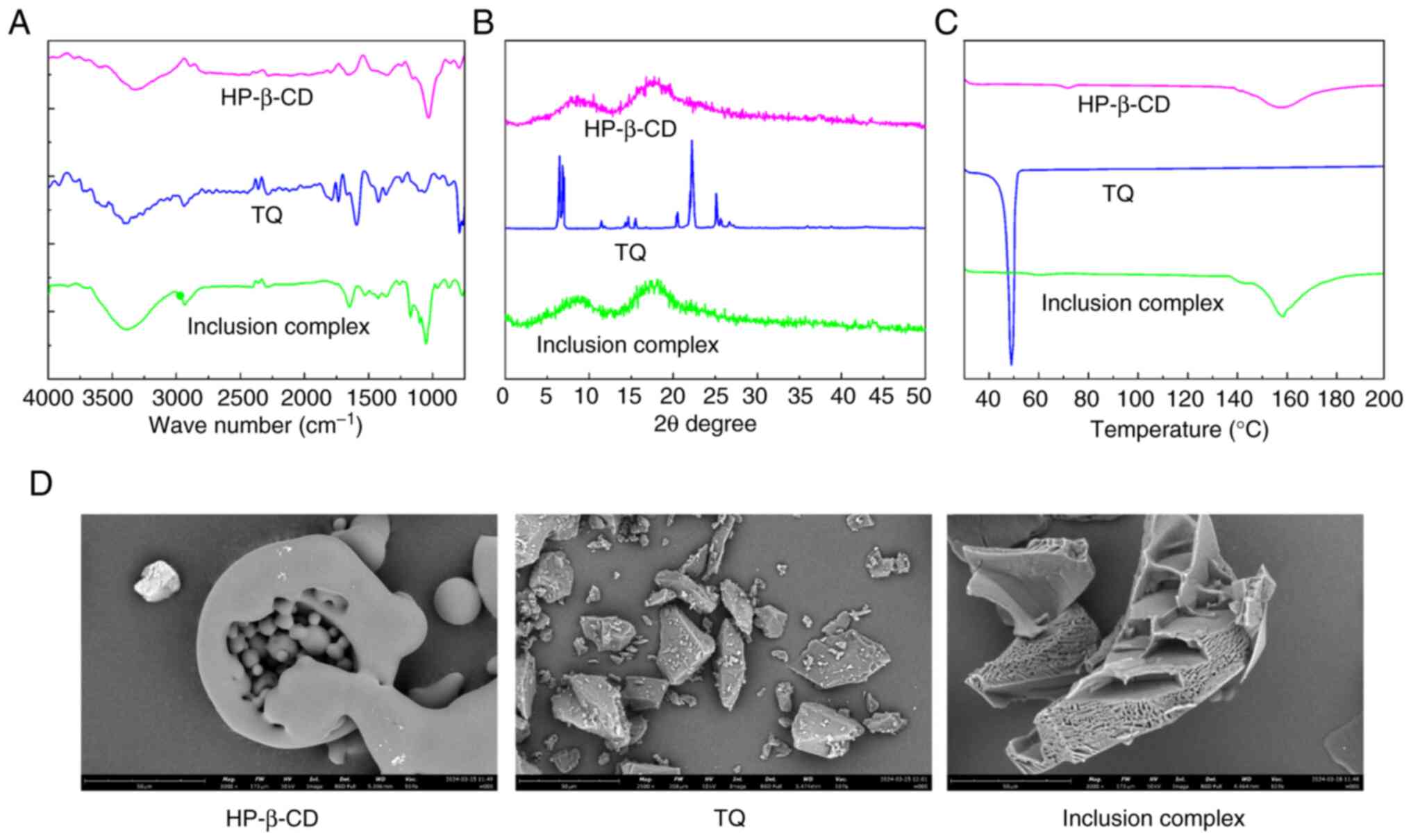
In previous studies, FTIR was used to investigate
the interaction between guest molecules and CDs in inclusion
complexes (22–24). The FTIR spectra of TQ, HP-β-CD and
TQ/HP-β-CD are demonstrated in Fig.
2A. HP-β-CD spectrum has unique absorption signals at ~3,318
cm−1 and 1,020 cm−1, representing OH group
and C-O-C glucose unit bending, respectively. Pure TQ exhibits an
intense sharp band at 1,647 cm−1, corresponding to the
stretching of carbonyl groups. CH2 produces stretching
vibration displayed at 2,970 cm−1. The spectral band of
1,450-1,020 cm−1 represents C=C bending vibration
(aliphatic) and C-O-C stretching vibration. After the formation of
the TQ/HP-β-CD inclusion complex, it can be observed that the
carbonyl group of TQ located at 1,520 cm−1 disappears
from the spectrum of the inclusion complex due to stretching.
Meanwhile, the characteristic broad band of the OH groups in
HP-β-CD shifted from 3,318 cm−1 to 3,401
cm−1. The signal changes related to the polar functional
groups of TQ and HP-β-CD can indicate the partial embedding of TQ
into the HP-β-CD cavity, thereby confirming the successful
formation of the inclusion complex (Fig. 1).
XRD
As revealed in Fig.
2B, XRD was used further to investigate the inclusion complex
of TQ and HP-β-CD. No diffraction peaks in the X-ray spectrum of
HP-β-CD indicate that it is amorphous. The XRD pattern of TQ showed
a series of strong and sharp diffraction peaks, indicating that the
compound is essentially crystalline. However, the inclusion complex
of TQ with HP-β-CD exhibited a well-differentiated diffusion X-ray
pattern similar to HP-β-CD, indicating that TQ no longer exists in
crystalline form and its inclusion complex with HP-β-CD exists in
an amorphous state. The transformation into an amorphous form is
important evidence for TQ to be embedded in the HP-β-CD cavity in a
molecular state (20,21).
DSC
The DSC curves of TQ, HP-β-CD and TQ/HP-β-CD
inclusion complex are shown in Fig.
2C. The DSC spectrum of HP-β-CD showed two peaks at 72 and
158°C, corresponding to the glass transition (Tg) and melting point
(Tm) temperatures, respectively. TQ has a sharp endothermic peak at
48.44°C, which is the Tm of the crystal. The DSC spectrum of the
TQ/HP-β-CD inclusion complex is highly similar to the HP-β-CD, but
the difference is that the TQ/HP-β-CD inclusion complex has lower
Tg and Tm. In addition, the endothermic peak of TQ disappeared in
the DSC curve of the inclusion complex, which is attributed to the
transition of crystalline TQ to an amorphous state. The
aforementioned results indicated that the TQ/HP-β-CD inclusion
complex exhibits reduced thermal stability and crystallization
trend, consistent with the XRD results.
SEM
Under a scanning electron microscope (Fig. 2D), HP-β-CD exhibits an amorphous
spherical structure with cavities. TQ presents an irregularly sized
rectangular crystal structure, and inclusion complexes exhibited
irregularly shaped aggregates or clumps. The change in the
morphology of the inclusion complex is mainly attributed to the
embedding of partial TQ molecules into the cavity of HP-β-CD, which
confirms the formation of the inclusion complex morphologically,
similar to previous literature (21).
Solubility detection
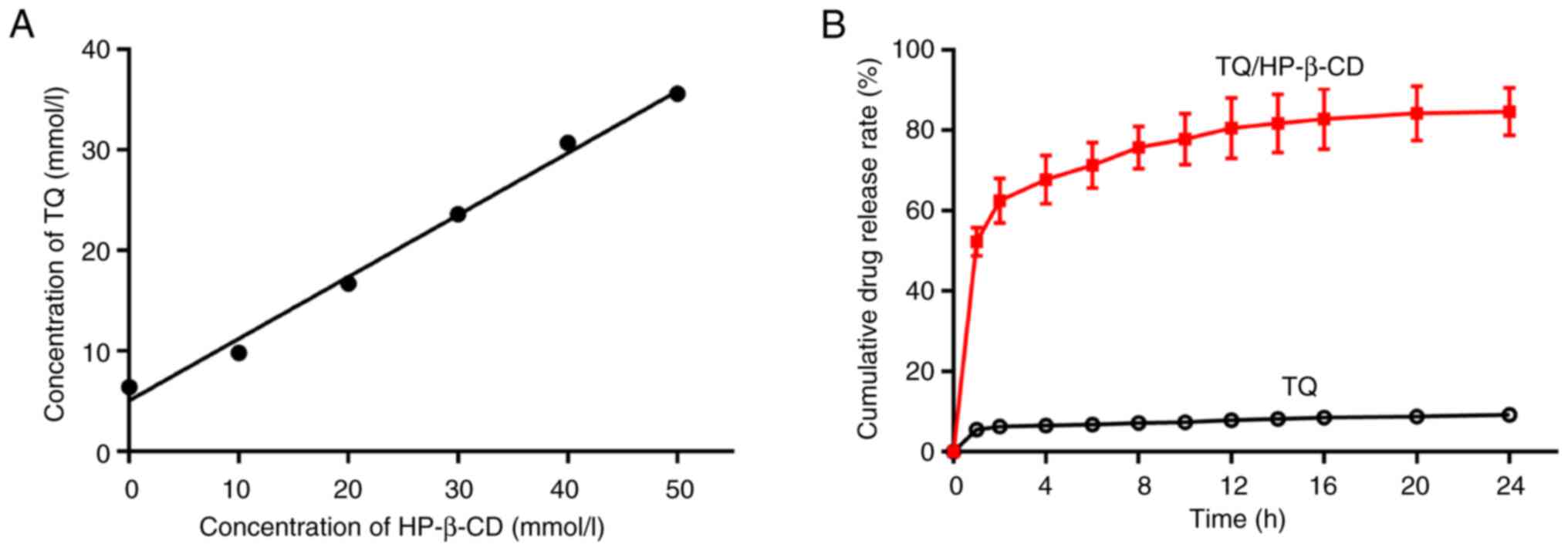
The phase solubility diagram of TQ encapsulated into
HP-β-CD was depicted in Fig. 3A,
indicating that the water solubility of TQ increases proportionally
with the increase of HP-β-CD molar concentration. The correlation
coefficient (R2) of the linear regression equation is
0.98, showing that the system follows an AL-type
solubility plot. The apparent stability constant (K1:1)
of the inclusion complex is related to its stability. The
K1:1 value increases proportionally to the stability of
the inclusion complex (24). The
K1:1 value of the TQ/HP-β-CD inclusion complex is 562.34
l/mol, demonstrating the preparation of a stable inclusion complex
between HP-β-CD and TQ. The detection of solubility at room
temperature (26°C) demonstrated that the solubility of TQ and
TQ/HP-β-CD inclusion complex in aqueous solution were 0.024 and
37.42 mmol/l, respectively. The solubility of TQ/HP-β-CD was
1,559-fold that of TQ. The CE displays the ratio of dissolved
complex concentration to dissolved free CD concentration and was
employed to evaluate the solubility of hydrophobic molecules in CDs
(27). According to the phase
solubility diagram, the CE value of the inclusion complex is 1.942,
indicating HP-β-CD is suitable for preparing TQ.
In vitro release behavior of TQ
To investigate whether the surface modifier HP-β-CD
can enhance the hydrophilicity of TQ as well as improve the release
characteristics of TQ. Then, the in vitro release experiment
of TQ was performed. The in vitro drug release curves of
free TQ and TQ/HP-β-CD inclusion complex in PBS (pH=7.4) at 37°C
for ~24 h were displayed in Fig.
3B. Specifically, the cumulative amount of TQ released from the
TQ/HP-β-CD inclusion complex increased rapidly in the first h of
the experiment, gradually increasing and reaching a plateau. A
total of >52.5% of TQ was released from the inclusion complex
within the first h, while free TQ was only released at 5.5%. After
24 h, the drug release rate in inclusion complex and free TQ were
84.3 and 9.3%, respectively. The aforementioned data confirmed the
ability of the new formula (TQ/HP-β-CD) to improve the
hydrophilicity and release characteristics of TQ.
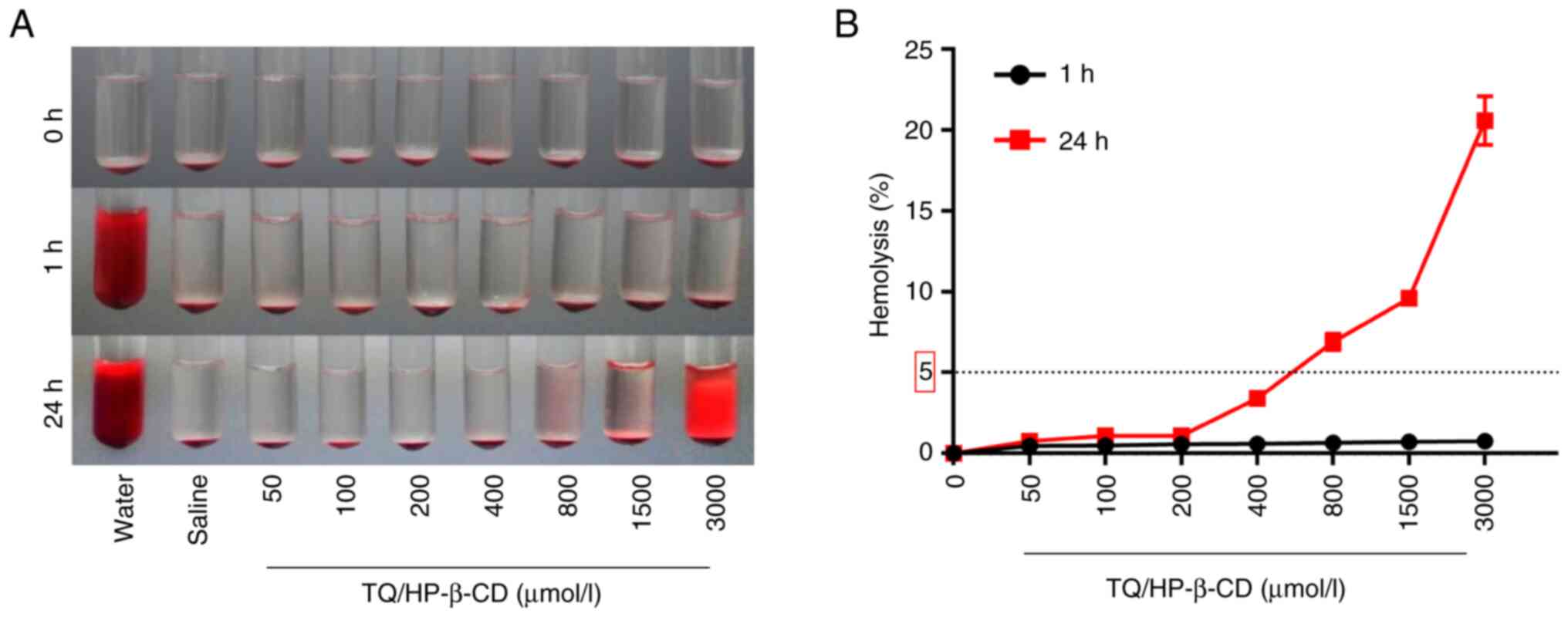
Blood hemolysis evaluation of
TQ/HP-β-CD
According to the national evaluation standard
(GB/T16886.4-2003), the hemolysis rate of medical biomaterials used
in clinical applications should be <5% to meet the safety
requirements of biomaterials (28).
As demonstrated in Fig. 4A, the
upper liquid of the test tube in the negative control group is
clear and transparent, and erythrocytes precipitate at the bottom,
indicating that hemolysis has not occurred. After 1 h of reaction,
the upper liquid of the test tube in the positive control group was
uniformly red, and there was no red blood cell precipitation at the
bottom, indicating that all red blood cells had undergone
hemolysis. After treatment with different concentrations of
TQ/HP-β-CD inclusion complex (50–3,000 µmol/l) for 1 h, the test
tube solution remained relatively clear. When the processing time
of the inclusion complex was extended to 24 h, the test tube liquid
of the low concentration TQ/HP-β-CD inclusion complex (50–400
µmol/l) group remained clear, while the upper liquid of the test
tube of the high concentration TQ/HP-β-CD inclusion complex
(800–3,000 µmol/l) group appeared red, indicating that the low
concentration TQ/HP-β-CD inclusion complex (50–400 µmol/l) used in
the present study had favorable blood compatibility.
In addition, the hemolysis degree of each group was
quantitatively measured using spectrophotometry (Fig. 4B). The results showed that after 1 h
of treatment, the hemolysis rate of the TQ/HP-β-CD groups with
different concentrations was <1%. When the action time of the
TQ/HP-β-CD is extended to 24 h, the red blood cell hemolysis rate
of the low concentration TQ/HP-β-CD groups (50–400 µmol/l) is
<5%. When the concentration of the TQ/HP-β-CD exceeds 400
µmol/l, the red blood cell hemolysis rate exceeds the threshold of
5%, indicating that the low-concentration inclusion complex
inflicts damage to red blood cells and meets the safety
requirements of national standards. The concentration of TQ/HP-β-CD
inclusion complex used in subsequent experiments is within the safe
range.
In vitro permeability study
To investigate the potential of HP-β-CD to enhance
the permeability and subsequent cellular uptake of TQ in A549
cells, permeability studies were conducted comparing free TQ to the
TQ/HP-β-CD inclusion complex. The Papp values determined were
1.04×10−7 cm/s for free TQ and 5.2×10−7 cm/s
for the TQ/HP-β-CD complex. This 5-fold increase in Papp
demonstrates that complexation with HP-β-CD significantly enhances
the transepithelial transport and cellular uptake of TQ in the A549
monolayer model. These findings indicate that HP-β-CD serves as an
effective carrier system, facilitating the delivery of a greater
amount of TQ into tumor cells.
TQ/HP-β-CD suppressed cell
proliferation and migration in NSCLC cells
Previous studies have confirmed that TQ
significantly inhibits the proliferation, migration and invasion of
various human cancer cells, including lung cancer (11–13).
Meanwhile, compared with free TQ, the nano-emulsion loaded with TQ
has higher cellular uptake and more potent anticancer activity
(27). The present study compared
the inhibitory effects of TQ/H2O, TQ/DMSO, HP-β-CD and
TQ/HP-β-CD inclusion complex on the proliferation of NSCLC cell
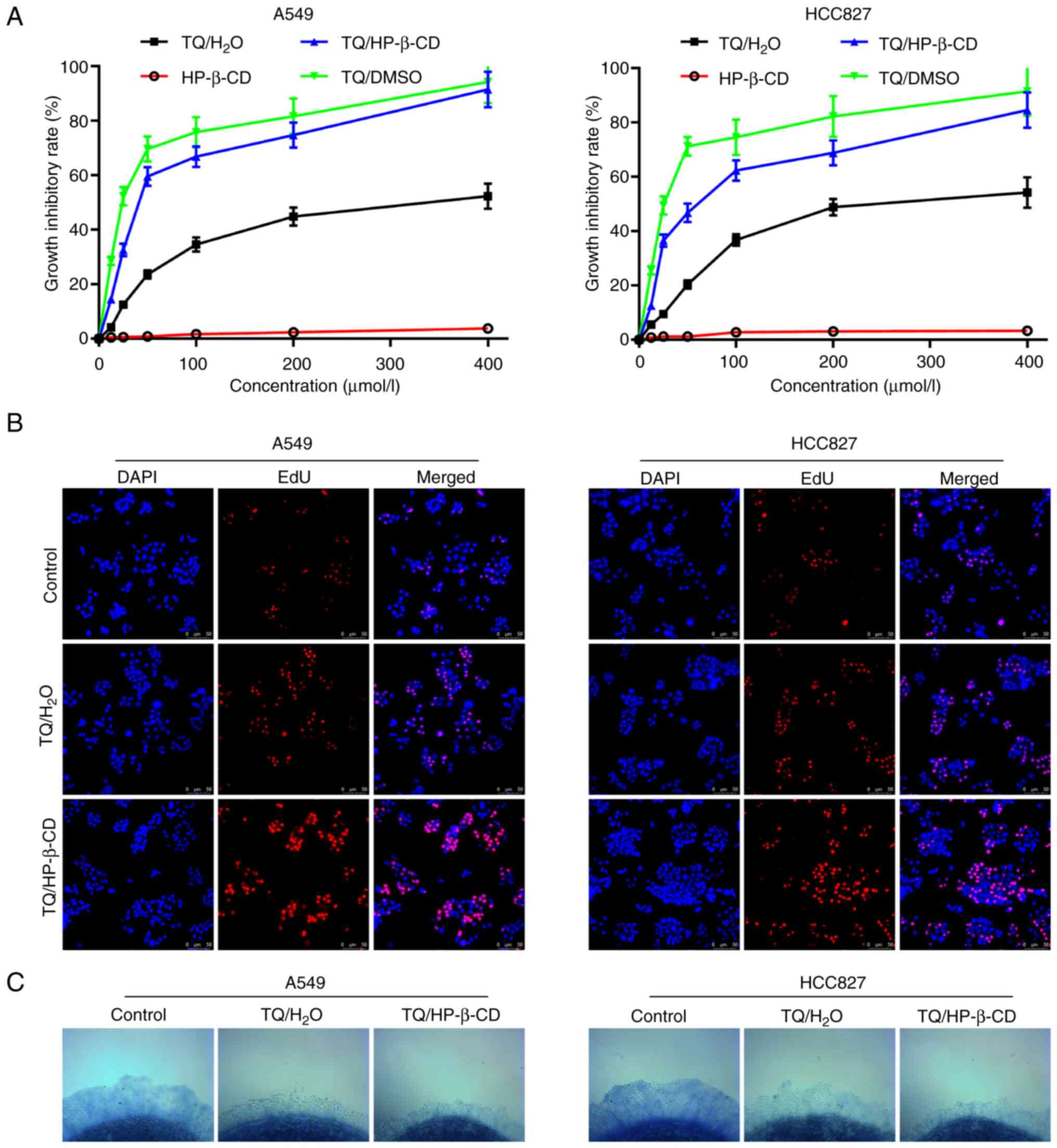
lines, specifically A549 and HCC827 cells. As shown in Fig. 5A, TQ/DMSO exerted a strong
inhibitory effect on the proliferation of A549 and HCC827 cells,
with IC50 values of 26.1 and 28.2 µmol/l, respectively,
which are similar to previous findings (13). TQ/H2O revealed a weaker
inhibitory effect on the proliferation of A549 and HCC827 cells,
with IC50 values of 290.6 and 252.2 µmol/l,
respectively. The inhibition rate of HP-β-CD on the proliferation
of NSCLC cells was <3%, indicating that HP-β-CD was almost
non-toxic. Combining TQ with HP-β-CD to form an inclusion complex
had a stronger inhibitory effect on the proliferation of NSCLC
cells than TQ/H2O, with IC50 values reduced
to 48.2 and 61.7 µmol/l, respectively. This enhanced inhibitory
activity aligns with the significantly improved permeability and
cellular uptake of TQ/HP-β-CD observed in the A549 monolayer model,
where its apparent permeability coefficient (Papp) was 5-fold
higher than that of free TQ.
The EdU assay results showed that TQ/H2O
could effectively inhibit the proliferation of A549 and HCC827
cells (Fig. 5B), and the inhibitory
effect of TQ/HP-β-CD at the same concentration on NSCLC cell
proliferation was further enhanced. In addition, the collagen
sprout outgrowth assay is an effective method for evaluating cell
proliferation and migration, with longer buds indicating more
vigorous cell proliferation and migration abilities (29). As shown in Fig. 5C, TQ/H2O significantly
inhibited the sprout outgrowth of A549 and HCC827 cells after 24 h
of treatment. Compared with TQ/H2O, the sprout length of
A549 and HCC827 cells treated with TQ/HP-β-CD was further
shortened.
The aforementioned results indicate that HP-β-CD can
enhance the inhibitory effect of TQ on the proliferation and
migration of NSCLC cells. Considering the excellent
biocompatibility of TQ/HP-β-CD in the experimental concentration
range, TQ/HP-β-CD can potentially become an anti-tumor agent for
treating NSCLC.
TQ/HP-β-CD induces ferroptosis in
NSCLC cells
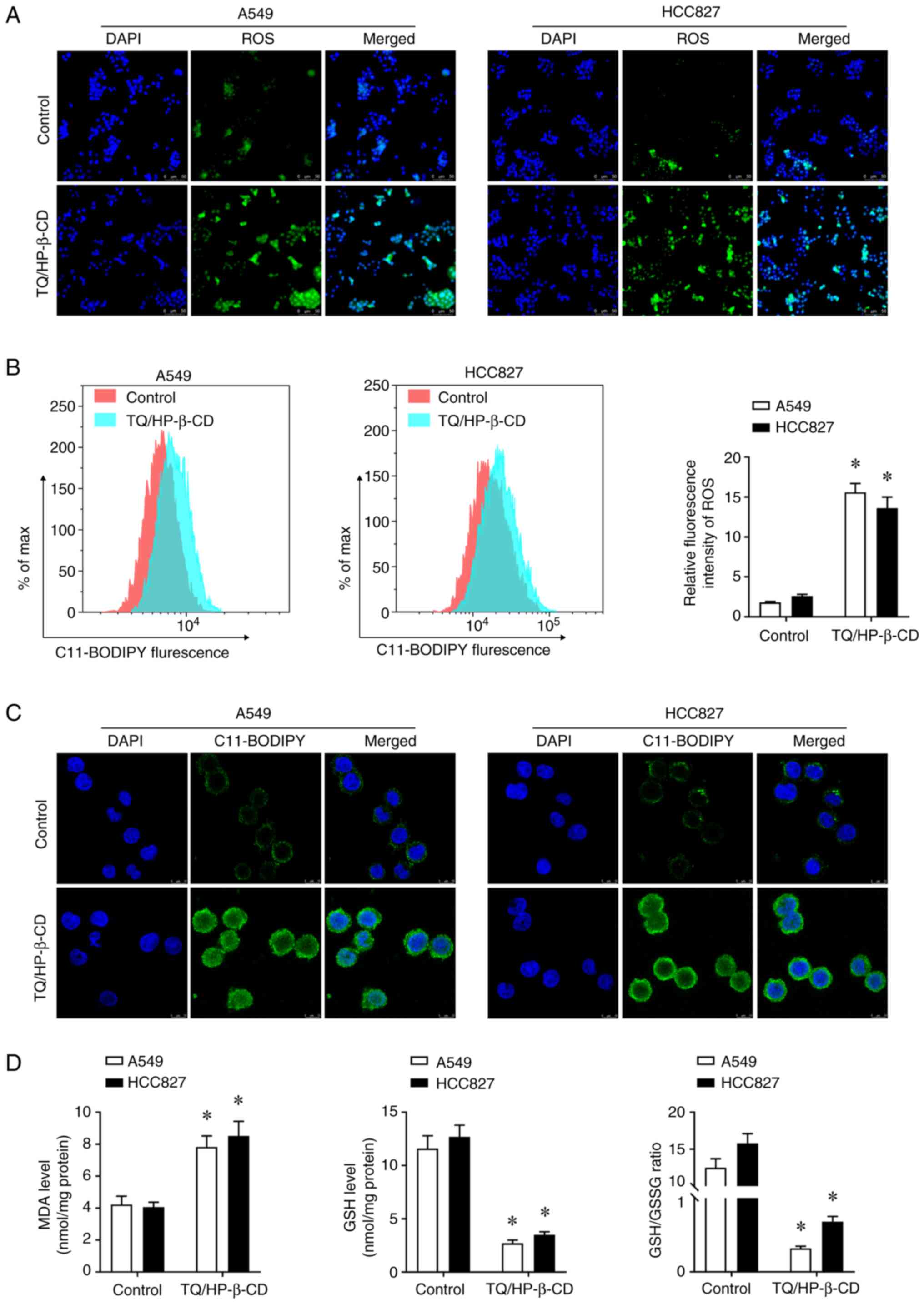
To confirm whether TQ/HP-β-CD can induce ferroptosis
in NSCLC cells, DHCA staining was first used to detect the
generation of ROS. The results showed that TQ/HP-β-CD treatment
increased ROS generation in A549 and HCC827 cells (Fig. 6A). Flow cytometry further showed
that TQ/HP-β-CD increases the expression of ROS in NSCLC cells
(Fig. 6B).
In addition, the present study further detected the
hallmark of ferroptosis - lipid peroxidation level-in NSCLC cells.
The dye C11-BODIPY 581/591 was used, which is sensitive to lipid
peroxidation, for laser confocal scanning microscopy observation.
The intensity of green fluorescence (oxidized C11-BODIPY) under the
microscope was used to evaluate the level of lipid peroxidation.
The results revealed that TQ/HP-β-CD treatment increased lipid
peroxidation levels in A549 and HCC827 cells (Fig. 6C). Meanwhile, the level of lipid
peroxidation product MDA in A549 and HCC827 cells was increased
after TQ/HP-β-CD treatment. The present study found that TQ/HP-β-CD
can significantly downregulate the level of GSH and the ratio of
GSH/GSSG in NSCLC cells (Fig. 6D).
These data indicated that TQ/HP-β-CD can induce ferroptosis in A549
and HCC827 cells.
Ferroptosis-dependent effect of
TQ/HP-β-CD against NSCLC cells
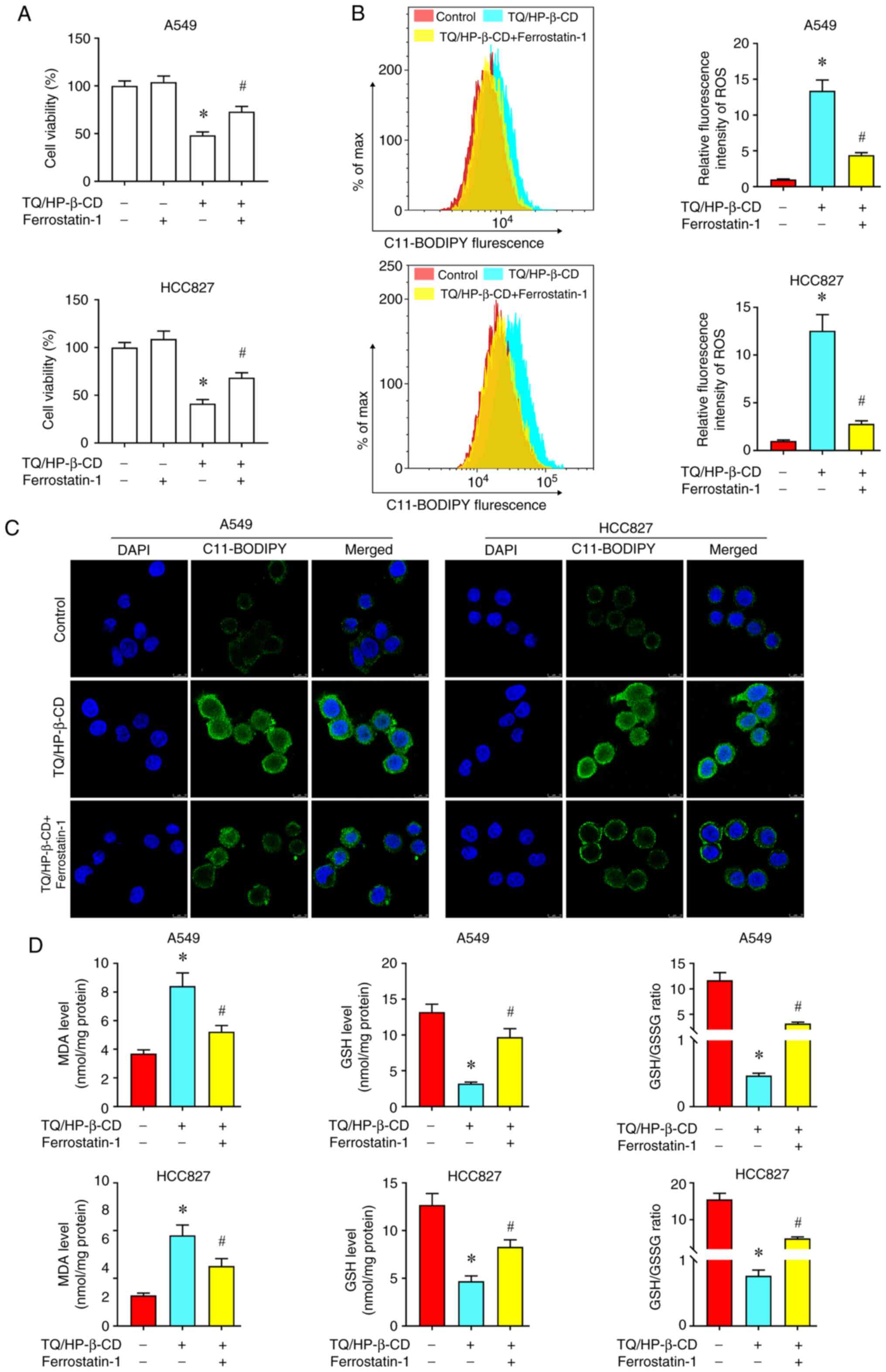
To further verify that ferroptosis is the main form
of TQ/HP-β-CD induced NSCLC cell death, rescue experiments were
conducted by Ferrostatin-1, a widely used ferroptosis inhibitor. It
was found that Ferrostatin-1 can effectively alleviate the
inhibitory effect of TQ/HP-β-CD on the proliferation of A549 and
HCC827 cells (Fig. 7A). Meanwhile,
pretreatment with Ferrostatin-1 can also reverse the accumulation
of ROS mediated by TQ/HP-β-CD in the cytoplasm (Fig. 7B) and the increase in lipid
peroxidation level (Fig. 7C). In
addition, ELISA experiments identified that Ferrostatin-1 can
effectively restore the elevated MDA level and decreased GSH level
induced by TQ/HP-β-CD in A549 and HCC827 cells (Fig. 7D).
NF-κb is a key regulatory factor in
TQ/HP-β-CD mediated ferroptosis
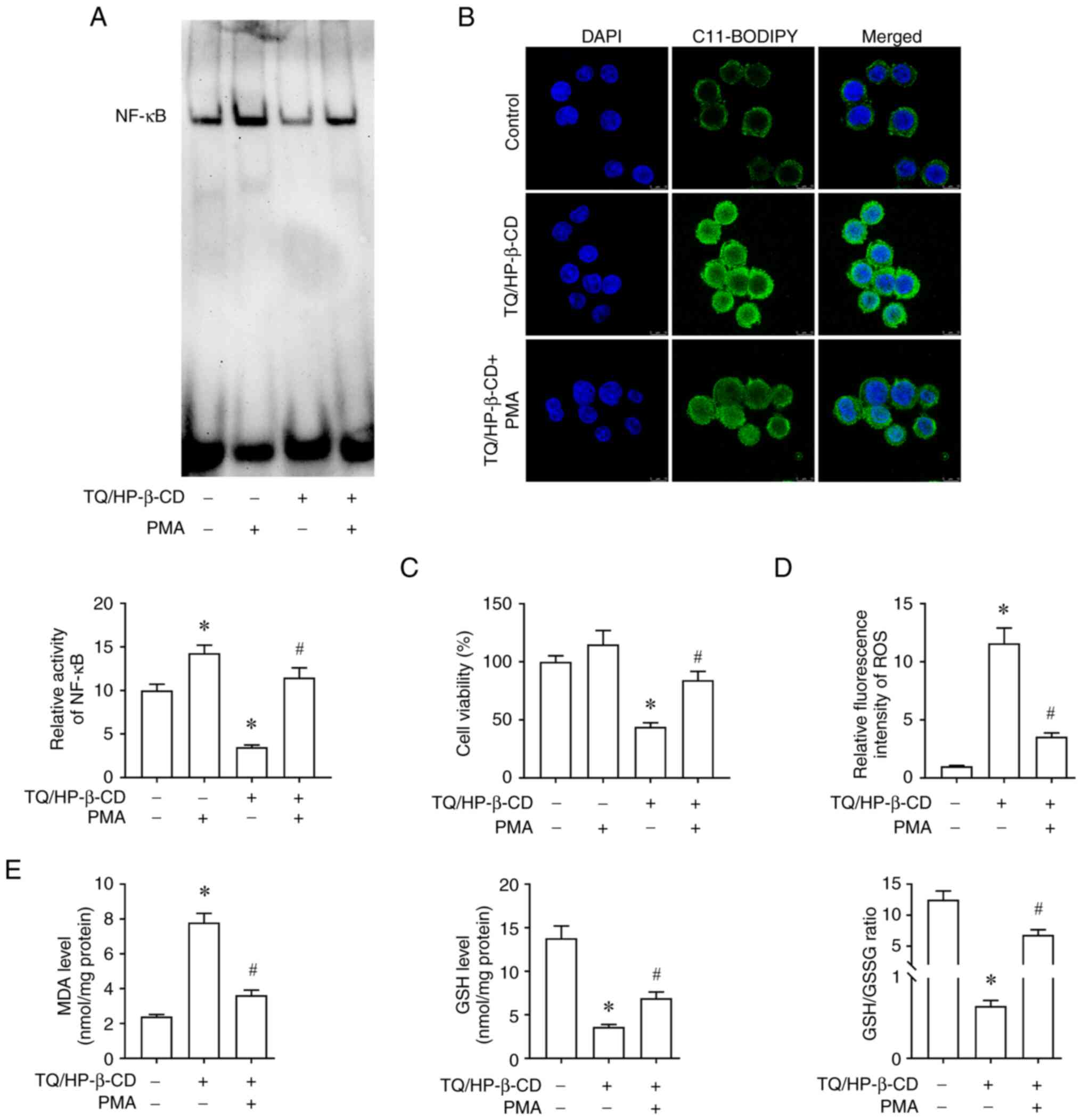
To elucidate the underlying mechanism by which
TQ/HP-β-CD induces ferroptosis, NF-κB DNA binding activity was
measured using EMSA (Fig. 8A). The
results showed that treatment with TQ/HP-β-CD alone for 24 h
effectively suppressed NF-κB DNA binding activity. To further
investigate the dependence of TQ/HP-β-CD-induced ferroptosis on
NF-κB, A549 cells were pretreated with the NF-κB activator PMA
followed by TQ/HP-β-CD treatment. Notably, PMA pretreatment rescued
the inhibitory effect of TQ/HP-β-CD on NF-κB activity.
Subsequently, the CCK-8 assay results indicated that
PMA can partially reverse the inhibitory effect of TQ on A549 cell
proliferation (Fig. 8C). Meanwhile,
after TQ/HP-β-CD treatment, lipid peroxidation level and ROS
generation increased in A549 cells. At the same time, PMA
successfully weakened the effect of TQ/HP-β-CD on lipid
peroxidation and ROS generation (Fig.
8B and D). In addition, PMA also alleviated the regulatory
effect of TQ/HP-β-CD on the expression of MDA and GSH in A549 cells
(Fig. 8E). The aforementioned
results indicated that TQ/HP-β-CD may first inhibit the basal level
of NF-κB DNA binding activity previously present in NSCLC cells,
leading to the inactivation of downstream genes and ultimately
inducing ferroptosis in NSCLC cells. However, the exact mechanism
by which TQ/HP-β-CD regulates the NF-κB pathway in NSCLC cells
remains unclear, and further research is needed to determine
whether other molecular mechanisms are involved.
In vivo antitumor efficacy and safety
of TQ/HP-β-CD
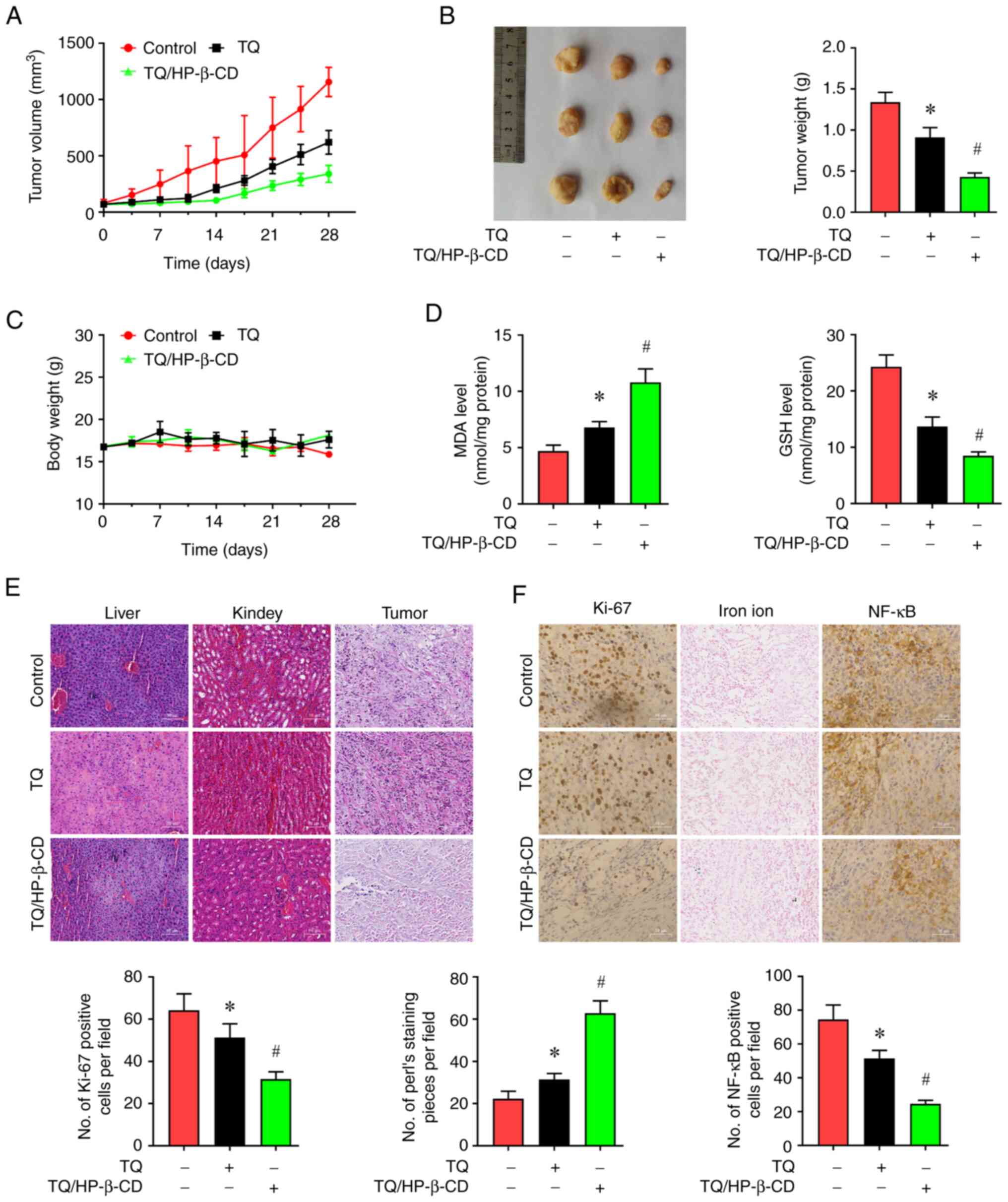
In the A549 ×enograft mouse model, both TQ and
TQ/HP-β-CD significantly inhibited tumor growth compared with the
control group. The tumor growth inhibition rates were 32.1% for TQ
and 67.9% for TQ/HP-β-CD (Fig. 9A and
B). H&E staining of tumor tissues revealed more extensive
necrotic features (nuclear fragmentation, contraction and
dissolution) in the TQ/HP-β-CD group compared with TQ and control
groups (Fig. 9E). IIHC showed a
significant reduction in Ki-67 positive cells (indicating
proliferation) in TQ/HP-β-CD treated tumors compared with both
control and TQ groups (Fig.
9F).
Furthermore, mice treated with TQ or TQ/HP-β-CD
showed no significant adverse symptoms (vomiting, convulsions or
bloating) and maintained stable body weights (Fig. 9C). H&E staining of liver and
kidney tissues from all groups revealed normal architecture without
significant pathological changes (Fig.
9E).
Induction of ferroptosis in vivo
Analysis of subcutaneous tumors showed that both TQ
and TQ/HP-β-CD treatment significantly decreased GSH levels and
increased MDA levels compared with the control group, with
TQ/HP-β-CD showing a stronger effect (Fig. 9D). Prussian blue staining revealed
significantly increased free iron deposition in tumor tissues from
both TQ and TQ/HP-β-CD treated mice compared with controls, again
more pronounced in the complex group (Fig. 9F). IHC analysis showed significantly
reduced positive expression of NF-κB in tumor tissues from TQ and
TQ/HP-β-CD groups compared with control, with TQ/HP-β-CD exhibiting
a stronger suppressive effect (Fig.
9F).
In summary, in vivo research results
indicated that TQ/HP-β-CD has favorable biocompatibility and a
stronger inhibitory effect on NSCLC growth than TQ, and
NF-κB-mediated ferroptosis induction may be its primary mechanism
of action, which is consistent with in vitro experimental
results.
Discussion
The present study established a novel TQ/HP-β-CD
inclusion complex (TQ/HP-β-CD) via freeze-drying. Structural
characterization by FT-IR, XRD, DSC and SEM confirmed successful TQ
encapsulation within the HP-β-CD cavity. The complex significantly
enhanced TQ's aqueous solubility (1,559-fold) and bioavailability,
translating to potent anti-NSCLC activity both in vitro and
in vivo. This directly addresses TQ's primary clinical
limitation: Free TQ's poor water solubility fundamentally restricts
its contact with cancer cells, explaining the weak growth
inhibition observed in aqueous formulations. While DMSO improves TQ
solubility and cytotoxicity by facilitating molecular contact, its
solvent properties preclude clinical translation and fail to
reflect physiological drug behavior.
By contrast, the TQ/HP-β-CD complex achieves
superior anticancer efficacy through dual mechanisms: i)
exceptional water solubility delivers more bioactive TQ molecules
to tumor cells, and ii) cyclodextrin-mediated transport enhances
membrane permeability-synergistically overcoming pharmaceutical
barriers constraining natural products (22). As a nano-scale delivery system,
HP-β-CD leverages critical advantages: Reduced particle size
facilitates cellular internalization, enables higher therapeutic
dosing without solvent toxicity, and minimizes drug loss from
first-pass metabolism and P-glycoprotein efflux (30). These properties potentiate TQ's
bioactivity and align with evidence that nanoparticle formulations
can trigger ferroptosis, an iron-dependent cell death pathway
driven by lipid peroxidation (31,32).
The data of the present study confirmed TQ/HP-β-CD induces
canonical ferroptosis markers (ROS accumulation, GSH depletion and
MDA elevation), positioning it alongside natural inducers such as
cantharidin (33) while offering
superior tumor selectivity (34).
Critically, the complex outperformed aqueous TQ (TQ/H2O)
in suppressing NSCLC proliferation and migration due to enhanced
intracellular delivery. It was noted that HP-β-CD alone exhibited
negligible cytotoxicity and TQ/H2O also displayed very
weak cytotoxic effects due to the inherently poor water solubility
of TQ. In light of this, a direct comparison of the cytotoxic
differences between TQ/H2O and HP-β-CD may not yield
significant insights relevant to the primary objective of the
present study, concerning the efficacy of the complex and thus such
a comparison was not performed.
A key mechanistic breakthrough is the demonstration
that TQ/HP-β-CD induces ferroptosis via NF-κB inhibition. While
NF-κB regulates tumor survival/proliferation (35) and modulates ferroptosis (36) and TQ is known to suppress NF-κB
(37), the present study was the
first to link this pathway to TQ-induced ferroptosis. Ferroptotic
cell death (evidenced by ROS, lipid peroxidation and GSH/MDA
dysregulation) was consistently triggered in NSCLC cells and
rescued by ferroptosis inhibitors. Crucially, TQ/HP-β-CD suppressed
NF-κB DNA binding, while NF-κB activation reversed
ferroptosis-establishing NF-κB inactivation as a critical mediator
of iron-dependent oxidative damage. This expands TQ's known
anticancer mechanisms beyond apoptosis (10) or PI3K/AKT modulation (11). Compared with other CDs [for example,
TQ/SBE-β-CD (27)], TQ/HP-β-CD
demonstrated superior translational potential, evidenced by robust
in vivo tumor suppression (67.9% inhibition) and minimal
toxicity. Its efficacy surpassed conventional chemotherapeutics
including cisplatin, which induce severe side effects via
apoptosis. While the present study aligned ferroptosis induction
with NSCLC vulnerability, limitations remain: the molecular link
between NF-κB suppression and ferroptosis execution (for example,
GPX4/SLC7A11 regulation) warrants deeper investigation. Future
studies should explore active targeting strategies (for example,
ligand-modified HP-β-CD) to enhance tumor selectivity and evaluate
synergy with immune checkpoint inhibitors.
In conclusion, TQ/HP-β-CD represents a promising
NSCLC therapeutic candidate that overcomes TQ's pharmacokinetic
barriers while activating a novel NF-κB-ferroptosis axis. The
present study validated cyclodextrin complexation for amplifying
natural compounds' therapeutic potential and positions ferroptosis
induction as a compelling anticancer strategy.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Guangdong Basic and
Applied Basic Research Foundation (grant no. 2022A1515111167).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
WWZ, JXD, YXL and LY conceived the present study and
took responsibility for the quality of the data. WWZ and LY
designed the study, completed the experiment, and supervised the
data collection. JXD and YXL analyzed and interpreted the data. LY
wrote the manuscript. All authors read and approved the final
version of the manuscript. WWZ, JXD, YXL and LY confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved (approval no.
20240215001) by the ethics committee of Ma'anshan People's Hospital
(Ma'anshan, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mithoowani H and Febbraro M:
Non-small-cell lung cancer in 2022: A review for general
practitioners in oncology. Curr Oncol. 29:1828–1839. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Meyer ML, Fitzgerald BG, Paz-Ares L,
Cappuzzo F, Jänne PA, Peters S and Hirsch FR: New promises and
challenges in the treatment of advanced non-small-cell lung cancer.
Lancet. 404:803–822. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Banna GL, Hassan MA, Signori A, Giunta EF,
Maniam A, Anpalakhan S, Acharige S, Ghose A and Addeo A:
Neoadjuvant chemo-immunotherapy for early-stage non-small cell lung
cancer: A systematic review and meta-analysis. JAMA Netw Open.
7:e2468372024. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen YL, Xiong LA, Ma LF, Fang L and Zhan
ZJ: Natural product-derived ferroptosis mediators. Phytochemistry.
219:1140022024. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang X, Izzo AA, Papapetropoulos A,
Alexander SPH, Cortese-Krott M, Kendall DA, Martemyanov KA, Mauro
C, Panettieri RA Jr, Patel HH, et al: Natural product pharmacology:
The British Journal of pharmacology perspective. Br J Pharmacol.
181:3547–3555. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang L, Liu P, Jiang Y, Fan D, He X,
Zhang J, Luo B, Sui J, Luo Y, Fu X and Yang T: Exploration of novel
isoxazole-fused quinone derivatives as anti-colorectal cancer
agents through inhibiting STAT3 and elevating ROS level. Eur J Med
Chem. 272:1164482024. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muramoto J and Sakamoto T: Tripodal
quinone-cyanine G-quadruplex ligands as novel photosensitizers on
photoinduced cancer cell death. Molecules. 29:50942024. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dey A, Kumar EKP, Kim CH, Li Y and Park
JH: Dual stimuli-responsive nanoprecursor of ascorbic acid and
quinone methide disrupting redox homeostasis for cancer treatment.
ACS Omega. 9:32124–32132. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Modarresi Chahardehi A, Ojaghi HR,
Motedayyen H and Arefnezhad R: Nano-based formulations of
thymoquinone are new approaches for psoriasis treatment: A
literature review. Front Immunol. 15:14168422024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abutayeh RF, Altah M, Mehdawi A, Al-Ataby
I and Ardakani A: Chemopreventive agents from nature: A review of
apigenin, rosmarinic acid, and thymoquinone. Curr Issues Mol Biol.
46:6600–6619. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao ZX, Li S and Liu LX: Thymoquinone
affects hypoxia-inducible factor-1α expression in pancreatic cancer
cells via HSP90 and PI3K/AKT/mTOR pathways. World J Gastroenterol.
30:2793–2816. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Taiyab A, Choudhury A, Haidar S, Yousuf M,
Rathi A, Koul P, Chakrabarty A, Islam A, Shamsi A and Hassan MI:
Exploring MTH1 inhibitory potential of thymoquinone and baicalin
for therapeutic targeting of breast cancer. Biomed Pharmacother.
173:1163322024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shakeel I, Haider S, Khan S, Ahmed S,
Hussain A, Alajmi MF, Chakrabarty A, Afzal M and Imtaiyaz Hassan M:
Thymoquinone, artemisinin, and thymol attenuate proliferation of
lung cancer cells as Sphingosine kinase 1 inhibitors. Biomed
Pharmacother. 177:1171232024. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Burdușel AC and Andronescu E: Lipid
nanoparticles and liposomes for bone diseases treatment.
Biomedicines. 10:31582022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xie B, Liu Y, Li X, Yang P and He W:
Solubilization techniques used for poorly water-soluble drugs. Acta
Pharm Sin B. 14:4683–4716. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kowalska A and Szeleszczuk Ł: Cyclodextrin
inclusion complexes with hydrocortisone-type corticosteroids.
Pharmaceutics. 16:15442024. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sarabia-Vallejo Á, Caja MDM, Olives AI,
Martín MA and Menéndez JC: Cyclodextrin inclusion complexes for
improved drug bioavailability and activity: Synthetic and
analytical aspects. Pharmaceutics. 15:23452023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Alqahtani MS, Kazi M, Alsenaidy MA and
Ahmad MZ: Advances in oral drug delivery. Front Pharmacol.
12:6184112021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wu HH, Garidel P and Michaela B: HP-β-CD
for the formulation of IgG and Ig-based biotherapeutics. Int J
Pharm. 601:1205312021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shen Q, Shen Y, Jin F, Du YZ and Ying XY:
Paclitaxel/hydroxypropyl-β-cyclodextrin complex-loaded liposomes
for overcoming multidrug resistance in cancer chemotherapy. J
Liposome Res. 30:12–20. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saha ST, Abdulla N, Zininga T, Shonhai A,
Wadee R and Kaur M: 2-Hydroxypropyl-β-cyclodextrin (HPβCD) as a
potential therapeutic agent for breast cancer. Cancers (Basel).
15:28282023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Al-Qubaisi MS, Rasedee A, Flaifel MH, Eid
EEM, Hussein-Al-Ali S, Alhassan FH, Salih AM, Hussein MZ, Zainal Z,
Sani D, et al: Characterization of
thymoquinone/hydroxypropyl-β-cyclodextrin inclusion complex:
Application to anti-allergy properties. Eur J Pharm Sci.
133:167–182. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Swingler S, Gupta A, Gibson H, Kowalczuk
M, Adamus G, Heaselgrave W and Radecka I: Thymoquinone:
Hydroxypropyl-β-cyclodextrin loaded bacterial cellulose for the
management of wounds. Pharmaceutics. 14:28162022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Eid EEM, Alshehade SA, Almaiman AA, Kamran
S, Lee VS and Alshawsh MA: Enhancing the anti-leukemic potential of
thymoquinone/sulfobutylether-β-cyclodextrin (SBE-β-CD) inclusion
complexes. Biomedicines. 11:18912023. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Luo K and Hu W: A dual thermo/pH-sensitive
hydrogel as 5-fluorouracil carrier for breast cancer treatment.
Anti-cancer Drugs. 36:220–231. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Peng L, Liu A, Shen Y, Xu HZ, Yang SZ,
Ying XZ, Liao W, Liu HX, Lin ZQ, Chen QY, et al: Antitumor and
anti-angiogenesis effects of thymoquinone on osteosarcoma through
the NF-κB pathway. Oncol Rep. 29:571–578. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Eid EEM, Almaiman AA, Alshehade SA,
Alsalemi W, Kamran S, Suliman FO and Alshawsh MA: Characterization
of thymoquinone-sulfobutylether-β-cyclodextrin inclusion complex
for anti-cancer applications. Molecules. 28:40962023. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen K, Yang R, Shen FQ and Zhu HL:
Advances in pharmacological activities and mechanisms of
glycyrrhizic acid. Curr Med Chem. 27:6219–6243. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ma Y, Su Q, Yue C, Zou H, Zhu J, Zhao H,
Song R and Liu Z: The effect of oxidative stress-induced autophagy
by cadmium exposure in kidney, liver, and bone damage, and
neurotoxicity. Int J Mol Sci. 23:134912022. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wu J, Wang Q, Dong X, Xu M, Yang J, Yi X,
Chen B, Dong X, Wang Y, Lou X, et al: Biocompatible
AIEgen/p-glycoprotein simplesiRNA@reduction-sensitive
paclitaxel polymeric prodrug nanoparticles for overcoming
chemotherapy resistance in ovarian cancer. Theranostics.
11:3710–3724. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li Y, Cai Z, Ma W, Bai L, Luo E and Lin Y:
A DNA tetrahedron-based ferroptosis-suppressing nanoparticle:
Superior delivery of curcumin and alleviation of diabetic
osteoporosis. Bone Res. 12:142024. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang Z, Zhao Y, Wang Y, Zhao Y and Guo J:
Autophagy/ferroptosis in colorectal cancer: Carcinogenic view and
nanoparticle-mediated cell death regulation. Environ Res.
238:1170062023. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhu X, Chen X, Qiu L, Zhu J and Wang J:
Norcantharidin induces ferroptosis via the suppression of NRF2/HO-1
signaling in ovarian cancer cells. Oncol Lett. 24:3592022.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Karki N, Aggarwal S, Laine RA, Greenway F
and Losso JN: Cytotoxicity of juglone and thymoquinone against
pancreatic cancer cells. Chem Biol Interact. 327:1091422020.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yu H, Lin L, Zhang Z, Zhang H and Hu H:
Targeting NF-κB pathway for the therapy of diseases: Mechanism and
clinical study. Signal Transduct Target Ther. 5:2092020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chen Y, Fang ZM, Yi X, Wei X and Jiang DS:
The interaction between ferroptosis and inflammatory signaling
pathways. Cell Death Dis. 14:2052023. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen B, Dong X, Zhang JL, Sun X, Zhou L,
Zhao K, Deng H and Sun Z: Natural compounds target programmed cell
death (PCD) signaling mechanism to treat ulcerative colitis: A
review. Front Pharmacol. 15:13336572024. View Article : Google Scholar : PubMed/NCBI
|