|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD, Wagle NS and Jemal
A: Cancer statistics, 2023. CA Cancer J Clin. 73:17–48.
2023.PubMed/NCBI
|
|
3
|
Blackadar CB: Historical review of the
causes of cancer. World J Clin Oncol. 7:54–86. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tan PH, Ellis I, Allison K, Brogi E, Fox
SB, Lakhani S, Lazar AJ, Morris EA, Sahin A, Salgado R, et al: The
2019 World Health Organization classification of tumours of the
breast. Histopathology. 77:181–185. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marra A, Trapani D, Viale G, Criscitiello
C and Curigliano G: Practical classification of triple-negative
breast cancer: Intratumoral heterogeneity, mechanisms of drug
resistance, and novel therapies. NPJ Breast Cancer. 6:542020.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ma Y and Gamagedara S: Biomarker analysis
for oncology. Biomark Med. 9:845–850. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Aronson JK and Ferner RE: Biomarkers-A
general review. Curr Protoc Pharmacol. 76:9.23.1–9.23.17.
2017.PubMed/NCBI
|
|
8
|
Barzaman K, Karami J, Zarei Z,
Hosseinzadeh A, Kazemi MH, Moradi-Kalbolandi S, Safari E and
Farahmand L: Breast cancer: Biology, biomarkers, and treatments.
Int Immunopharmacol. 84:1065352020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tarighati E, Keivan H and Mahani H: A
review of prognostic and predictive biomarkers in breast cancer.
Clin Exp Med. 15:1–16. 2022.
|
|
10
|
Yi M, Xu L, Jiao Y, Luo S, Li A and Wu K:
The role of cancer-derived microRNAs in cancer immune escape. J
Hematol Oncol. 13:252020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mu D, Han B, Huang H, Zheng Y, Zhang J and
Shi Y: Unraveling the advances of non-coding RNAs on the tumor
microenvironment: Innovative strategies for cancer therapies. J
Transl Med. 23:6142025. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Abdul Manap AS, Wisham AA, Wong FW, Najmi
HR, Ng ZF and Diba RS: Mapping the function of MicroRNAs as a
critical regulator of tumor-immune cell communication in breast
cancer and potential treatment strategies. Front Cell Dev Biol.
12:13907042024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang Z, Yang X, Shen J, Xu J, Pan M, Liu J
and Han S: Gene expression patterns associated with
tumor-infiltrating CD4+ and CD8+ T cells in invasive breast
carcinomas. Hum Immunol. 82:279–287. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fu Y, Yang Q, Xu N and Zhang X: MiRNA
affects the advancement of breast cancer by modulating the immune
system's response. Biochim Biophys Acta Mol Basis Dis.
1871:1677592025. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Galvão-Lima LJ, Morais AHF, Valentim RAM
and Barreto EJSS: miRNAs as biomarkers for early cancer detection
and their application in the development of new diagnostic tools.
Biomed Eng Online. 20:212021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cuk K, Zucknick M, Heil J, Madhavan D,
Schott S, Turchinovich A, Arlt D, Rath M, Sohn C, Benner A, et al:
Circulating microRNAs in plasma as early detection markers for
breast cancer. Int J Cancer. 132:1602–1612. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bedard PL, Hyman DM, Davids MS and Siu LL:
Small molecules, big impact: 20 years of targeted therapy in
oncology. Lancet. 395:1078–1088. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang J, Wang Q, Guan Y, Sun Y, Wang X,
Lively K, Wang Y, Luo M, Kim JA, Murphy EA, et al: Breast cancer
cell-derived microRNA-155 suppresses tumor progression via
enhancing immune cell recruitment and antitumor function. J Clin
Invest. 132:e1572482022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu X, Chang Q, Wang H, Qian H and Jiang
Y: Discovery and function exploration of microRNA-155 as a
molecular biomarker for early detection of breast cancer. Breast
Cancer. 28:806–821. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu Y, Hong Q, Lu F, Zhang Z, Li J, Nie Z
and He B: The diagnostic and prognostic value of miR-155 in
cancers: An updated meta-analysis. Mol Diagn Ther. 27:283–301.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Trivers KF, Lund MJ, Porter PL, Liff JM,
Flagg EW, Coates RJ and Eley JW: The epidemiology of
triple-negative breast cancer, including race. Cancer Causes
Control. 20:1071–1082. 2009.PubMed/NCBI
|
|
22
|
Lucena C, Paulinelli R and Pedrini JL:
Oncoplastia e reconstrução mamária. (1st ed.). Vol. 1. Rio de
Janeiro: MEDBOOK. 2017.3–16
|
|
23
|
Radu I, Scripcariu V, Panuța A, Rusu A,
Afrăsânie VA, Cojocaru E, Aniței MG, Alexa-Stratulat T, Terinte C,
Șerban CF and Gafton B: Breast sarcomas-how different are they from
breast carcinomas? Clinical, pathological, imaging and treatment
insights. Diagnostics (Basel). 13:13702023. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Orvieto E, Maiorano E, Bottiglieri L,
Maisonneuve P, Rotmensz N, Galimberti V, Luini A, Brenelli F, Gatti
G and Viale G: Clinicopathologic characteristics of invasive
lobular carcinoma of the breast: Results of an analysis of 530
cases from a single institution. Cancer. 113:1511–1520. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
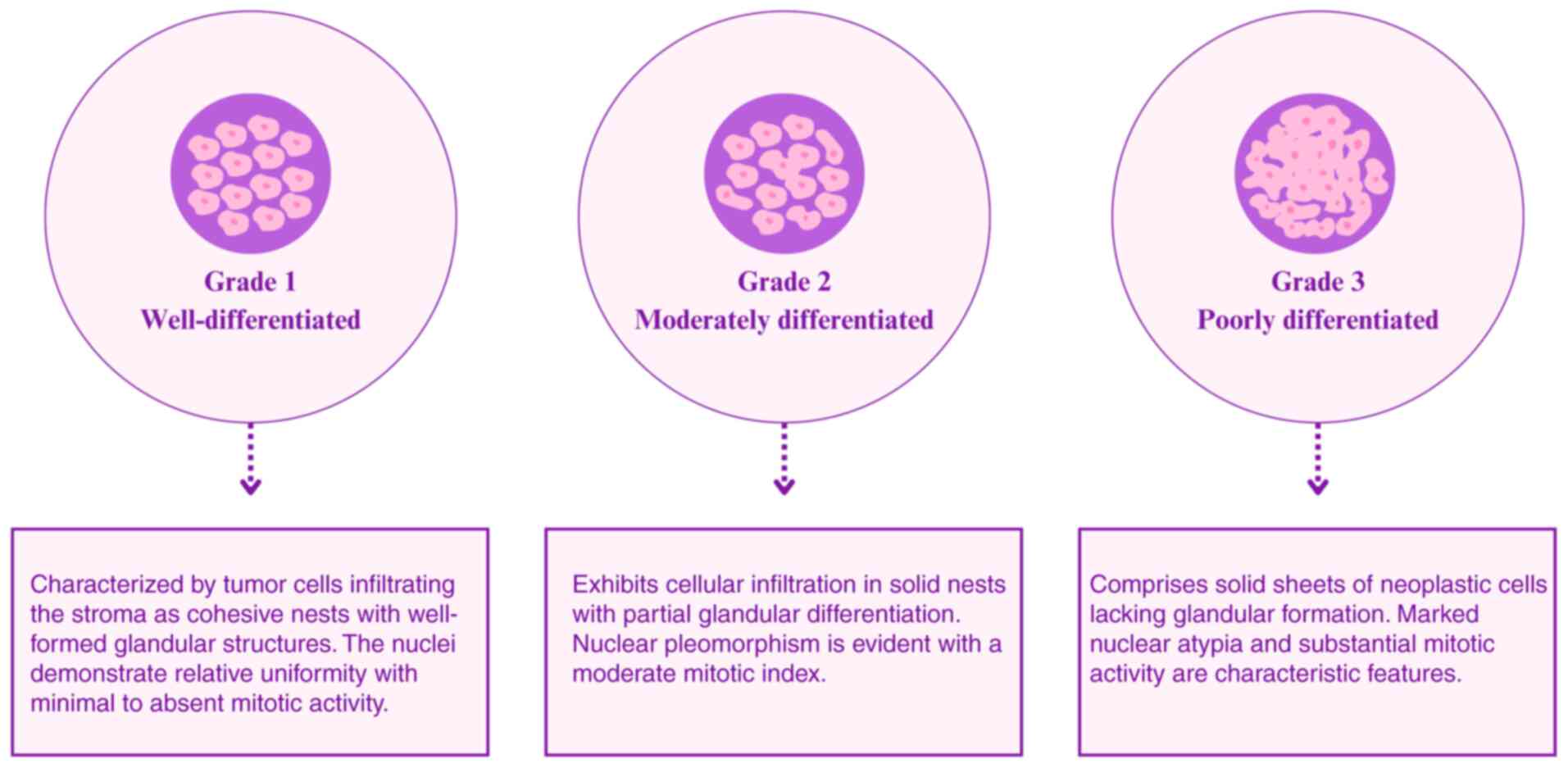
Elston CW and Ellis IO: pathological
prognostic factors in breast cancer. I. The value of histological
grade in breast cancer: Experience from a large study with
long-term follow-up. Histopathology. 19:403–410. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Moran MS, Yang Q and Haffty BG: The yale
university experience of early-stage invasive lobular carcinoma
(ILC) and invasive ductal carcinoma (IDC) treated with breast
conservation treatment (BCT): Analysis of clinical-pathologic
features, long-term outcomes, and molecular expression of COX-2,
Bcl-2, and p53 as a function of histology. Breast J. 15:571–578.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jenkins S, Kachur ME, Rechache K, Wells JM
and Lipkowitz S: Rare breast cancer subtypes. Curr Oncol Rep.
23:542021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Perou CM, Sùrlie T, Eisen MB, van de Rijn
M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA,
et al: Molecular portraits of human breast tumours. Nature.
406:747–752. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Waks AG and Winer EP: Breast cancer
treatment: A review. JAMA. 321:288–300. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wolff AC, Hammond MEH, Hicks DG, Dowsett
M, McShane LM, Allison KH, Allred DC, Bartlett JMS, Bilous M,
Fitzgibbons P, et al: Recommendations for human epidermal growth
factor receptor 2 testing in breast. J Clin Oncol. 31:118–145.
2013. View Article : Google Scholar
|
|
31
|
Parise CA, Bauer KR, Brown MM and Caggiano
V: Breast cancer subtypes as defined by the estrogen receptor (ER),
progesterone receptor (PR), and the human epidermal growth factor
receptor 2 (HER2) among women with invasive breast cancer in
California, 1999–2004. Breast J. 15:593–602. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Huang P, Chandra V and Rastinejad F:
Structural overview of the nuclear receptor superfamily: Insights
into physiology and therapeutics. Annu Rev Physiol. 72:247–272.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kim MC, Park MH, Choi JE, Kang SH and Bae
YK: Characteristics and prognosis of estrogen receptor low-positive
breast cancer. J Breast Cancer. 25:318–326. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Allison KH, Hammond MEH, Dowsett M,
Mckernin SE, Carey LA, Fitzgibbons PL, Hayes DF, Lakhani SR,
Chavez-MacGregor M, Perlmutter J, et al: Estrogen and progesterone
receptor testing in breast cancer: ASCO/CAP guideline update. J
Clin Oncol. 38:1346–1366. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Giatromanolaki A, Koukourakis MI,
Simopoulos C, Polychronidis A, Gatter KC, Harris AL and Sivridis E:
c-erbB-2 related aggressiveness in breast cancer is hypoxia
inducible factor-1 dependent. Clin Cancer Res. 10:7972–7977. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wolff AC, Hammond ME, Allison KH, Harvey
BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P,
Hanna W, et al: Human epidermal growth factor receptor 2 testing in
breast cancer: American Society of Clinical Oncology/College of
American Pathologists clinical practice guideline focused update. J
Clin Oncol. 36:2105–2122. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hammond MEH, Hayes DF, Dowsett M, Allred
DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS,
Hayes M, et al: American society of clinical oncology/college of
american pathologists guideline recommendations for
immunohistochemical testing of estrogen and progesterone receptors
in breast cancer. J Clin Oncol. 28:2784–2795. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Akshata Desai KA: Triple Negative Breast
Cancer-An Overview. Hereditary Genetics. 2012. View Article : Google Scholar
|
|
39
|
Millikan RC, Newman B, Tse CK, Moorman PG,
Conway K, Dressler LG, Smith LV, Labbok MH, Geradts J, Bensen JT,
et al: Epidemiology of basal-like breast cancer. Breast Cancer Res
Treat. 109:123–139. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Gonzalez-Angulo AM, Timms KM, Liu S, Chen
H, Litton JK, Potter J, Lanchbury JS, Stemke-Hale K, Hennessy BT,
Arun BK, et al: Incidence and outcome of BRCA mutations in
unselected patients with triple receptor-negative breast cancer.
Clin Cancer Res. 17:1082–1089. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhou Y, Tao L, Qiu J, Xu J, Yang X, Zhang
Y, Tian X, Guan X, Cen X and Zhao Y: Tumor biomarkers for
diagnosis, prognosis and targeted therapy. Signal Transduct Target
Ther. 9:1322024. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
da Silva JL, Nunes NC, Izetti P, de
Mesquita GG and de Melo AC: Triple negative breast cancer: A
thorough review of biomarkers. Crit Rev Oncol Hematol.
145:1028552020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yadav BS, Chanana P and Jhamb S:
Biomarkers in triple negative breast cancer: A review. World J Clin
Oncol. 6:252–263. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Bai X, Ni J, Beretov J, Graham P and Li Y:
Immunotherapy for triple-negative breast cancer: A molecular
insight into the microenvironment, treatment, and resistance. J
Natl Cancer Cent. 1:75–87. 2021.PubMed/NCBI
|
|
45
|
Anayyat U, Ahad F, Muluh TA, Zaidi SAA,
Usmani F, Yang H, Li M, Hassan HA and Wang X: Immunotherapy:
Constructive approach for breast cancer treatment. Breast Cancer
(Dove Med Press). 15:925–951. 2023.PubMed/NCBI
|
|
46
|
Dvir K, Giordano S and Leone JP:
Immunotherapy in breast cancer. Int J Mol Sci. 25:75172024.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
da Cunha BR, Domingos C, Stefanini AC,
Henrique T, Polachini GM, Castelo-Branco P and Tajara EH: Cellular
interactions in the tumor microenvironment: The role of secretome.
J Cancer. 10:4574–4587. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
O'Sullivan T, Saddawi-Konefka R, Vermi W,
Koebel WV, Arthur C, White JM, Uppaluri R, Andrews DM, Ngiow SF,
Teng MW, et al: Cancer immunoediting by the innate immune system in
the absence of adaptive immunity. J Exp Med. 209:1869–1882. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chiu PPL, Ivakine E, Mortin-Toth S and
Danska JS: Susceptibility to lymphoid neoplasia in immunodeficient
strains of nonobese diabetic mice. Cancer Res. 62:5828–5834.
2002.PubMed/NCBI
|
|
50
|
Dunn GP, Old LJ and Schreiber RD: The
immunobiology of cancer immunosurveillance and immunoediting.
Immunity. 21:137–148. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Muenst S, Läubli H, Soysal SD, Zippelius
A, Tzankov A and Hoeller S: The immune system and cancer evasion
strategies: Therapeutic concepts. J Intern Med. 279:541–562. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Mittal D, Gubin MM, Schreiber RD and Smyth
MJ: New insights into cancer immunoediting and its three component
phases-elimination, equilibrium and escape. Curr Opin Immunol.
27:16–25. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Palucka K and Banchereau J: Cancer
immunotherapy via dendritic cells. Nat Rev Cancer. 12:265–277.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Janssen EM, Lemmens EE, Wolfe T, Christen
U, von Herrath MG and Schoenberger SP: CD4+ T cells are required
for secondary expansion and memory in CD8+ T lymphocytes. Nature.
421:852–856. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Catalán E, Charni S, Jaime P, Aguiló JI,
Enríquez JA, Naval J, Pardo J, Villalba M and Anel A: MHC-I
modulation due to changes in tumor cell metabolism regulates tumor
sensitivity to CTL and NK cells. Oncoimmunology. 4:e9859242015.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Hori S, Nomura T and Sakaguchi S: Control
of regulatory T cell development by the transcription factor Foxp3.
Science. 299:1057–1061. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sakaguchi S, Miyara M, Costantino CM and
Hafler DA: FOXP3+ regulatory T cells in the human immune system.
Nat Rev Immunol. 10:490–500. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Mc Neil V and Lee SW: Advancing cancer
treatment: A review of immune checkpoint inhibitors and combination
strategies. Cancers (Basel). 17:14082025. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Cortes J, Cescon DW, Rugo HS, Nowecki Z,
Im SA, Yusof MM, Gallardo C, Lipatov O, Barrios CH, Holgado E, et
al: Pembrolizumab plus chemotherapy versus placebo plus
chemotherapy for previously untreated locally recurrent inoperable
or metastatic triple-negative breast cancer (KEYNOTE-355): A
randomised, placebo-controlled, double-blind, phase 3 clinical
trial. Lancet. 396:1817–1828. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hodi FS, O'Day SJ, McDermott DF, Weber RW,
Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel
JC, et al: Improved survival with ipilimumab in patients with
metastatic melanoma. N Engl J Med. 363:711–723. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Zhang Z, Huang Q, Yu L, Zhu D, Li Y, Xue
Z, Hua Z, Luo X, Song Z, Lu C, et al: The role of miRNA in tumor
immune escape and mirna-based therapeutic strategies. Front
Immunol. 12:8078952022. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Tang WW, Battistone B, Bauer KM, Weis AM,
Barba C, Fadlullah MZH, Ghazaryan A, Tran VB, Lee SH, Agir ZB, et
al: A microRNA-regulated transcriptional state defines intratumoral
CD8+ T cells that respond to immunotherapy. Cell Rep.
44:1153012025. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Sharma S, Opyrchal M and Lu X: Harnessing
tumorous flaws for immune supremacy: Is miRNA-155 the weak link in
breast cancer progression? J Clin Invest. 132:e1630102022.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wang M, Yin B, Wang HY and Wang RF:
Current advances in T-cell-based cancer immunotherapy.
Immunotherapy. 6:1265–1278. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Chen L and Flies DB: Molecular mechanisms
of T cell co-stimulation and co-inhibition. Na Rev Immunol.
13:227–242. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Naidoo J, Page DB, Li BT, Connell LC,
Schindler K, Lacouture ME, Postow MA and Wolchok JD: Toxicities of
the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann
Oncol. 26:2375–2391. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Brahmer JR, Tykodi SS, Chow LQM, Hwu WJ,
Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, et al:
Safety and activity of anti-PD-L1 antibody in patients with
advanced cancer. N Engl J Med. 366:2455–2465. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Shevach EM: Application of IL-2 therapy to
target T regulatory cell function. Trends Immunol. 33:626–632.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Wang HY and Wang RF: Regulatory T cells
and cancer. Curr Opin Immunol. 19:217–223. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Salgado R, Denkert C, Demaria S, Sirtaine
N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL,
Penault-Llorca F, et al: The evaluation of tumor-infiltrating
lymphocytes (TILS) in breast cancer: Recommendations by an
international TILS working group 2014. Ann Oncol. 26:259–271. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Mao Y, Qu Q, Chen X, Huang O, Wu J and
Shen K: The prognostic value of tumor-infiltrating lymphocytes in
breast cancer: A systematic review and meta-analysis. PLoS One.
11:e01525002016. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
van den Ende NS, Nguyen AH, Jager A, Kok
M, Debets R and van Deurzen CHM: Triple-Negative breast cancer and
predictive markers of response to neoadjuvant chemotherapy: A
systematic review. Int J Mol Sci. 24:29692023. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Leon-Ferre RA, Polley MY, Liu H, Gilbert
JA, Cafourek V, Hillman DW, Elkhanany A, Akinhanmi M, Lilyquist J,
Thomas A, et al: Impact of histopathology, tumor-infiltrating
lymphocytes, and adjuvant chemotherapy on prognosis of
triple-negative breast cancer. Breast Cancer Res Treat. 167:89–99.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Denkert C, von Minckwitz G, Darb-Esfahani
S, Lederer B, Heppner BI, Weber KE, Budczies J, Huober J, Klauschen
F, Furlanetto J, et al: Tumour-infiltrating lymphocytes and
prognosis in different subtypes of breast cancer: A pooled analysis
of 3,771 patients treated with neoadjuvant therapy. Lancet Oncol.
19:40–50. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
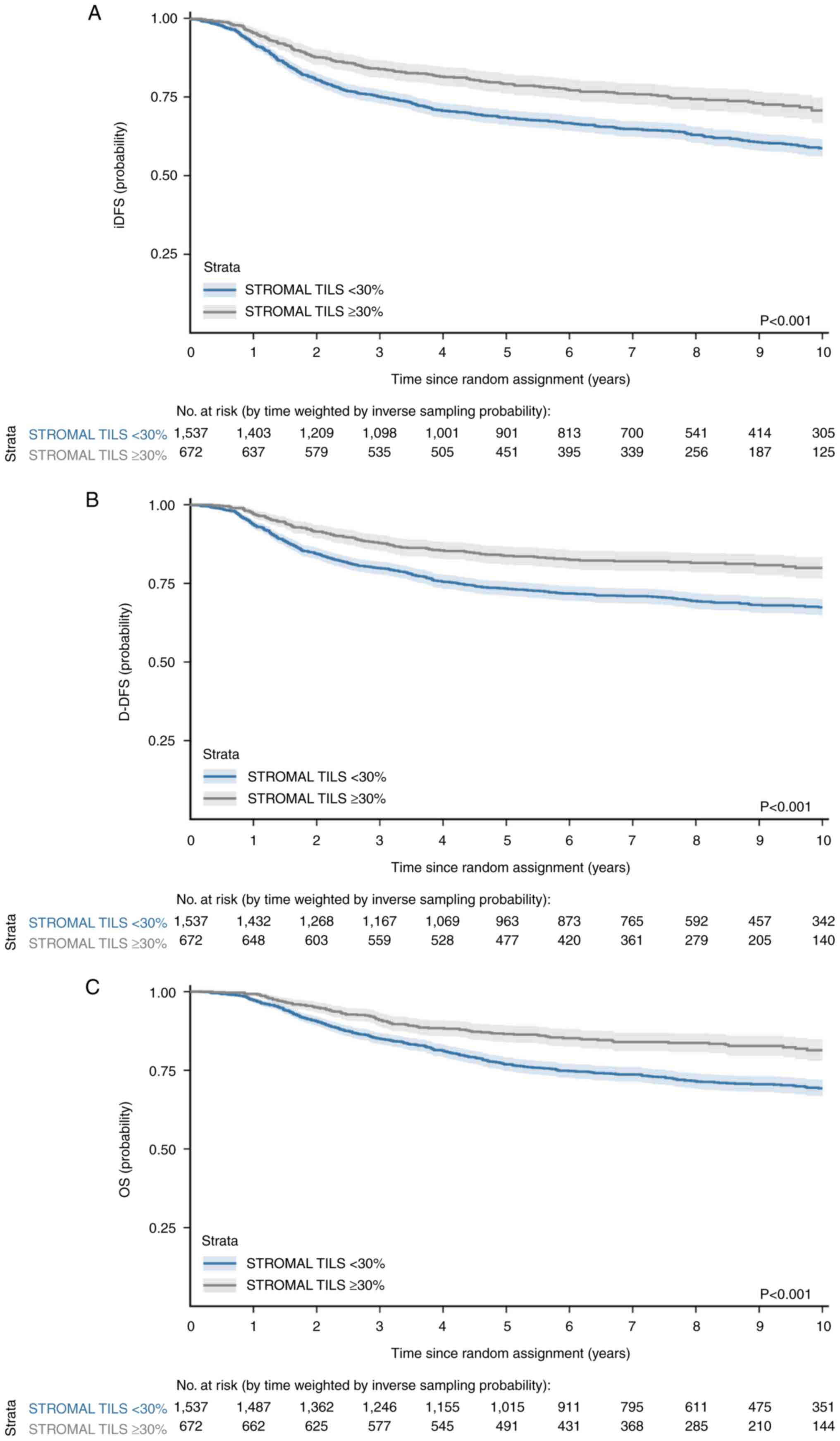
75
|
Leon-Ferre RA, Jonas SF, Salgado R, Loi S,
de Jong V, Carter JM, Nielsen TO, Leung S, Riaz N, Chia S, et al:
Tumor-Infiltrating lymphocytes in triple-negative breast cancer.
JAMA. 331:1135–1144. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Tan Q, Yin S, Zhou D, Chi Y, Man X and Li
H: Potential predictive and prognostic value of biomarkers related
to immune checkpoint inhibitor therapy of triple-negative breast
cancer. Front Oncol. 12:7797862022. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
O'Loughlin M, Andreu X, Bianchi S,
Chemielik E, Cordoba A, Cserni G, Figueiredo P, Floris G, Foschini
MP, Heikkilä P, et al: Reproducibility and predictive value of
scoring stromal tumour infiltrating lymphocytes in triple-negative
breast cancer: A multi-institutional study. Breast Cancer Res
Treat. 171:1–9. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Stanton SE and Disis ML: Clinical
significance of tumor-infiltrating lymphocytes in breast cancer. J
Immunother Cancer. 4:592016. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Li S, Zhang Y, Zhang P, Xue S, Chen Y, Sun
L and Yang R: Predictive and prognostic values of tumor
infiltrating lymphocytes in breast cancers treated with neoadjuvant
chemotherapy: A meta-analysis. Breast. 66:97–109. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Gao G, Wang Z, Qu X and Zhang Z:
Prognostic value of tumor-infiltrating lymphocytes in patients with
triple-negative breast cancer: A systematic review and
meta-analysis. BMC Cancer. 20:1792020. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Valenza C, Salimbeni BT, Santoro C,
Trapani D, Antonarelli G and Curigliano G: Tumor infiltrating
lymphocytes across breast cancer subtypes: Current issues for
biomarker assessment. Cancers (Basel). 15:7672023. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Ochi T, Bianchini G, Ando M, Nozaki F,
Kobayashi D, Criscitiello C, Curigliano G, Iwamoto T, Niikura N,
Takei H, et al: Predictive and prognostic value of stromal
tumour-infiltrating lymphocytes before and after neoadjuvant
therapy in triple negative and HER2-positive breast cancer. Eur J
Cancer. 118:41–48. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Loi S, Michiels S, Salgado R, Sirtaine N,
Jose V, Fumagalli D, Kellokumpu-Lehtinen PL, Bono P, Kataja V,
Desmedt C, et al: Tumor infiltrating lymphocytes are prognostic in
triple negative breast cancer and predictive for trastuzumab
benefit in early breast cancer: Results from the FinHER trial. Ann
Oncol. 25:1544–1550. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Stanton SE, Adams S and Disis ML:
Variation in the incidence and magnitude of tumor-infiltrating
lymphocytes in breast cancer subtypes: A systematic review. JAMA
Oncol. 2:1354–1360. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Russo L, Maltese A, Betancourt L, Romero
G, Cialoni D, De la Fuente L, Gutierrez M, Ruiz A, Agüero E and
Hernández S: Locally advanced breast cancer: Tumor-infiltrating
lymphocytes as a predictive factor of response to neoadjuvant
chemotherapy. Eur J Surg Oncol. 45:963–968. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Liu S, Duan X, Xu L, Xin L, Cheng Y, Liu
Q, Ye J, Zhang S, Zhang H, Zhu S, et al: Optimal threshold for
stromal tumor-infiltrating lymphocytes: Its predictive and
prognostic value in HER2-positive breast cancer treated with
trastuzumab-based neoadjuvant chemotherapy. Breast Cancer Res
Treat. 154:239–249. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Denkert C, Loibl S, Noske A, Roller M,
Müller BM, Komor M, Budczies J, Darb-Esfahani S, Kronenwett R,
Hanusch C, et al: Tumor-associated lymphocytes as an independent
predictor of response to neoadjuvant chemotherapy in breast cancer.
J Clin Oncol. 28:105–113. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Dieci MV, Criscitiello C, Goubar A, Viale
G, Conte P, Guarneri V, Ficarra G, Mathieu MC, Delaloge S,
Curigliano G and Andre F: Prognostic value of tumor-infiltrating
lymphocytes on residual disease after primary chemotherapy for
triple-negative breast cancer: A retrospective multicenter study.
Ann Oncol. 25:611–618. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Yuan Y, Lee JS, Yost SE, Li SM, Frankel
PH, Ruel C, Schmolze D, Robinson K, Tang A, Martinez N, et al:
Phase II trial of neoadjuvant carboplatin and nab-paclitaxel in
patients with triple-negative breast cancer. Oncologist.
26:e382–e393. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Schmidt M, Weyer-Elberich V, Hengstler JG,
Heimes AS, Almstedt K, Gerhold-Ay A, Lebrecht A, Battista MJ,
Hasenburg A, Sahin U, et al: Prognostic impact of CD4-positive T
cell subsets in early breast cancer: A study based on the FinHer
trial patient population. Breast Cancer Res. 20:152018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Cerbelli B, Pernazza A, Botticelli A,
Fortunato L, Monti M, Sciattella P, Campagna D, Mazzuca F, Mauri M,
Naso G, et al: PD-L1 expression in TNBC: A predictive biomarker of
response to neoadjuvant chemotherapy? Biomed Res Int.
2017:17509252017. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Van Bockstal MR, Noel F, Guiot Y, Duhoux
FP, Mazzeo F, Van Marcke C, Fellah L, Ledoux B, Berlière M and
Galant C: Predictive markers for pathological complete response
after neo-adjuvant chemotherapy in triple-negative breast cancer.
Ann Diagn Pathol. 49:1516342020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Floris G, Richard F, Hamy AS, Jongen L,
Wildiers H, Ardui J, Punie K, Smeets A, Berteloot P, Vergote I, et
al: Body mass index and tumor-infiltrating lymphocytes in
triple-negative breast cancer. J Natl Cancer Inst. 113:146–153.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Dieci MV, Tsvetkova V, Griguolo G,
Miglietta F, Tasca G, Giorgi CA, Cumerlato E, Massa D, Lo Mele M,
Orvieto E, et al: Integration of tumour infiltrating lymphocytes,
programmed cell-death ligand-1, CD8 and FOXP3 in prognostic models
for triple-negative breast cancer: Analysis of 244 stage I–III
patients treated with standard therapy. Eur J Cancer. 136:7–15.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Loi S, Drubay D, Adams S, Pruneri G,
Francis PA, Lacroix-Triki M, Joensuu H, Dieci MV, Badve S, Demaria
S, et al: Tumor-infiltrating lymphocytes and prognosis: A pooled
individual patient analysis of early-stage triple-negative breast
cancers. J Clin Oncol. 37:559–569. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
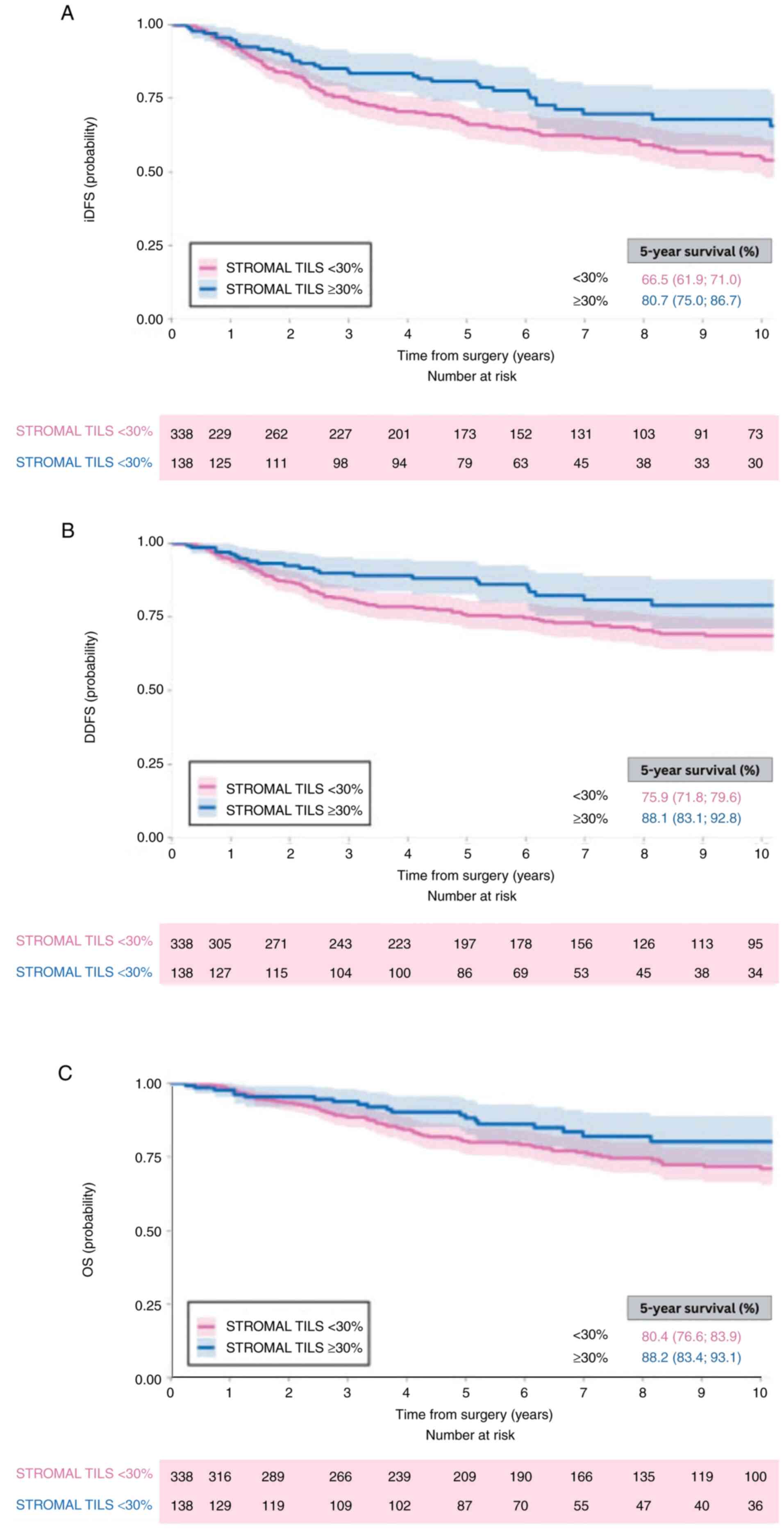
96
|
Park JH, Jonas SF, Bataillon G,
Criscitiello C, Salgado R, Loi S, Viale G, Lee HJ, Dieci MV, Kim
SB, et al: Prognostic value of tumor-infiltrating lymphocytes in
patients with early-stage triple-negative breast cancers (TNBC) who
did not receive adjuvant chemotherapy. Ann Oncol. 30:1941–1949.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
TILs in Breast Cancer. International
Immuno-Oncology Biomarker Working Group on Breast Cancer
[Internet], . [cited 2025 Jul 7]. Available from. https://www.tilsinbreastcancer.org
|
|
98
|
Laenkholm AV, Callagy G, Balancin M,
Bartlett JMS, Sotiriou C, Marchio C, Kok M, Dos Anjos CH and
Salgado R: Incorporation of TILs in daily breast cancer care: How
much evidence can we bear? Virchows Arch. 480:147–162. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Loi S, Michiels S, Adams S, Loibl S,
Budczies J, Denkert C and Salgado R: The journey of
tumor-infiltrating lymphocytes as a biomarker in breast cancer:
Clinical utility in an era of checkpoint inhibition. Ann Oncol.
32:1236–1244. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Lovat F, Valeri N and Croce CM: MicroRNAs
in the pathogenesis of cancer. Semin Oncol. 38:724–733. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Carthew RW and Sontheimer EJ: Origins and
mechanisms of miRNAs and siRNAs. Cell. 136:642–655. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Ha M and Kim VN: Regulation of microRNA
biogenesis. Nat Rev Mol Cell Biol. 15:509–524. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Titze-de-Almeida R and Titze-de-Almeida
SS: miR-7 replacement therapy in Parkinson's disease. Curr Gene
Ther. 18:143–153. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Fareh M, Yeom KH, Haagsma AC, Chauhan S,
Heo I and Joo C: TRBP ensures efficient Dicer processing of
precursor microRNA in RNA-crowded environments. Nat Commun.
7:136942016. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Mashima R: Physiological roles of miR-155.
Immunology. 145:323–333. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Bartel DP: MicroRNAs: Genomics,
biogenesis, mechanism, and function review. Cell. 116:281–297.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Shang R, Lee S, Senavirathne G and Lai EC:
microRNAs in action: Biogenesis, function and regulation. Nat Rev
Genet. 24:816–833. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Rupaimoole R, Calin GA, Lopez-Berestein G
and Sood AK: miRNA deregulation in cancer cells and the tumor
microenvironment. Cancer Discov. 6:235–246. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Roberts JT and Borchert GM: Computational
prediction of microRNA target genes, target prediction databases,
and web resources. Methods Mol Biol. 1617:109–122. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Kariuki D, Asam K, Aouizerat BE, Lewis KA,
Florez JC and Flowers E: Review of databases for experimentally
validated human microRNA-mRNA interactions. Database (Oxford).
25:baad0142023. View Article : Google Scholar
|
|
111
|
Griffiths-Jones S: The microRNA registry.
Nucleic Acids Res. 32:D109–D111. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Nair VS, Maeda LS and Ioannidis JPA:
Clinical outcome prediction by MicroRNAs in human cancer: A
systematic review. J Natl Cancer Inst. 104:528–540. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Verret B, Bottosso M, Hervais S and
Pistilli B: The molecular predictive and prognostic biomarkers in
metastatic breast cancer: The contribution of molecular profiling.
Cancers (Basel). 14:42032022. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Koncina E, Haan S, Rauh S and Letellier E:
Prognostic and predictive molecular biomarkers for colorectal
cancer: Updates and challenges. Cancers (Basel). 12:3192020.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Chang JTH, Wang F, Chapin W and Huang RS:
Identification of MicroRNAs as breast cancer prognosis markers
through the cancer genome atlas. PLoS One. 11:e01682842016.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
van Schooneveld E, Wouters MCA, Van der
Auwera I, Peeters DJ, Wildiers H, Van Dam PA, Vergote I, Vermeulen
PB, Dirix LY and Van Laere SJ: Expression profiling of cancerous
and normal breast tissues identifies microRNAs that are
differentially expressed in serum from patients with (metastatic)
breast cancer and healthy volunteers. Breast Cancer Res.
14:R342012. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Feliciano A, González L, Garcia-Mayea Y,
Mir C, Artola M, Barragán N, Martín R, Altés A, Castellvi J,
Benavente S, et al: Five microRNAs in serum are able to
differentiate breast cancer patients from healthy individuals.
Front Oncol. 10:5862682020. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Mihai AM, Ianculescu LM and Suciu N:
MiRNAs as potential biomarkers in early breast cancer detection: A
systematic review. J Med Life. 17:549–554. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Fu SW, Lee W, Coffey C, Lean A, Wu X, Tan
X, Man YG and Brem RF: miRNAs as potential biomarkers in early
breast cancer detection following mammography. Cell Biosci.
6:62016. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Hanahan D and Weinberg RA: The hallmarks
of cancer. Cell. 100:57–70. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Medarova Z, Pantazopoulos P and Yoo B:
Screening of potential miRNA therapeutics for the prevention of
multi-drug resistance in cancer cells. Sci Rep. 10:19702020.
View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Navarro A, Marrades RM, Viñolas N, Quera
A, Agustí C, Huerta A, Ramirez J, Torres A and Monzo M: MicroRNAs
expressed during lung cancer development are expressed in human
pseudoglandular lung embryogenesis. Oncology. 76:162–169. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Singh R, Ha SE, Yu TY and Ro S: Dual roles
of miR-10a-5p and miR-10b-5p as tumor suppressors and oncogenes in
diverse cancers. Int J Mol Sci. 26:4152025. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Webster RJ, Giles KM, Price KJ, Zhang PM,
Mattick JS and Leedman PJ: Regulation of epidermal growth factor
receptor signaling in human cancer cells by MicroRNA-7. J Biol
Chem. 284:5731–5741. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Castañeda CA, Agullo-Ortuño MT, Vara JA,
Cortes-Funes H, Gomez HL and Ciruelos E: Implication of miRNA in
the diagnosis and treatment of breast cancer. Expert Rev Anticancer
Ther. 11:1265–1275. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Baylie T, Kasaw M, Getinet M, Getie G,
Jemal M, Nigatu A, Ahmed H and Bogale M: The role of miRNAs as
biomarkers in breast cancer. Front Oncol. 14:13748212024.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Iorio MV, Ferracin M, Liu CG, Veronese A,
Spizzo R, Sabbioni S, Magri E, Pedriali M, Fabbri M, Campiglio M,
et al: MicroRNA gene expression deregulation in human breast
cancer. Cancer Res. 65:7065–7070. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Yan LX, Huang XF, Shao Q, Huang MY, Deng
L, Wu QL, Zeng YX and Shao JY: MicroRNA miR-21 overexpression in
human breast cancer is associated with advanced clinical stage,
lymph node metastasis and patient poor prognosis. RNA.
14:2348–2360. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Li S, Yang X, Yang J, Zhen J and Zhang D:
Serum microRNA-21 as a potential diagnostic biomarker for breast
cancer: A systematic review and meta-analysis. Clin Exp Med.
16:29–35.. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Syed RU, Banu H, Alshammrani A, Alshammari
MD, G SK, Kadimpati KK, Khalifa AAS, Aboshouk NAM, Almarir AM,
Hussain A and Alahmed FK: MicroRNA-21 (miR-21) in breast cancer:
From apoptosis dysregulation to therapeutic opportunities. Pathol
Res Pract. 262:1555722024. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Qian B, Katsaros D, Lu L, Preti M, Durando
A, Arisio R, Mu L and Yu H: High miR-21 expression in breast cancer
associated with poor disease-free survival in early stage disease
and high TGF-β1. Breast Cancer Res Treat. 117:131–140. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Wang Y, Zhang Y, Pan C, Ma F and Zhang S:
Prediction of poor prognosis in breast cancer patients based on
MicroRNA-21 expression: A meta-analysis. PLoS One. 10:e01186472015.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Bertoli G, Cava C and Castiglioni I:
Micrornas: New biomarkers for diagnosis, prognosis, therapy
prediction and therapeutic tools for breast cancer. Theranostics.
5:1122–1143. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Romero-Cordoba S, Rodriguez-Cuevas S,
Rebollar-Vega R, Bautista-Pina V, Maffuz-Aziz A, Tagliabue E, Iorio
M, D'Ippolito E, Baroni S, Plantamura I and Hidalgo-Miranda A: A
microRNA signature identifies subtypes of triple-negative breast
cancer and reveals miR-342-3p as regulator of a lactate metabolic
pathway through silencing monocarboxylate transporter 1. Cancer
Res. 76:A472016. View Article : Google Scholar
|
|
135
|
Tariq M, Richard V and Kerin MJ: MicroRNAs
as molecular biomarkers for the characterization of basal-like
breast tumor subtype. Biomedicines. 11:30072023. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Blenkiron C, Goldstein LD, Thorne NP,
Spiteri I, Chin SF, Dunning MJ, Barbosa-Morais NL, Teschendorff AE,
Green AR, Ellis IO, et al: MicroRNA expression profiling of human
breast cancer identifies new markers of tumor subtype. Genome Biol.
8:R2142007. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Kalkusova K, Taborska P, Stakheev D and
Smrz D: The role of miR-155 in antitumor immunity. Cancers (Basel).
14:54142022. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Mahesh G and Biswas R: MicroRNA-155: A
master regulator of inflammation. J Interferon Cytokine Res.
39:321–330. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Cui B, Chen L, Zhang S, Mraz M, Fecteau
JF, Yu J, Ghia EM, Zhang L, Bao L, Rassenti LZ, et al: Micro
RNA-155 influences B-cell receptor signaling and associates with
aggressive disease in chronic lymphocytic leukemia. Blood.
124:546–554. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Rai KR, Liao Y, Cai M, Qiu H, Wen F, Peng
M, Wang S, Liu S, Guo G, Chi X, et al: MIR155HG plays a bivalent
role in regulating innate antiviral immunity by encoding long
noncoding RNA-155 and microRNA-155-5p. mBio. 13:e02510222022.
View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Dawson O and Piccinini AM: miR-155-3p:
Processing by-product or rising star in immunity and cancer? Open
Biol. 12:2200702022. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Bayraktar R and Van Roosbroeck K: miR-155
in cancer drug resistance and as target for miRNA-based
therapeutics. Cancer Metastasis Rev. 37:33–44. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Zhou H, Huang X, Cui H, Luo X, Tang Y,
Chen S, Wu L and Shen N: miR-155 and its star-form partner miR-155*
cooperatively regulate type I interferon production by human
plasmacytoid dendritic cells. Blood. 116:5885–5894. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Pasculli B, Barbano R, Fontana A, Biagini
T, Di Viesti MP, Rendina M, Valori VM, Morritti M, Bravaccini S,
Ravaioli S, et al: Hsa-miR-155-5p up-regulation in breast cancer
and its relevance for treatment with poly[ADP-Ribose] polymerase 1
(PARP-1) inhibitors. Front Oncol. 10:14152020. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Kang Y, Cao X, Fan Y, Li Y, Xu T, Zhou Q
and He B: Exosome biomarkers in breast cancer: Systematic review
and meta-analysis. Clin Chim Acta. 574:1203422025. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Degheidy MS, Abou-Elalla AA, Kamel MM,
Abdel-Ghany S, Arneth B and Sabit H: Regulatory roles of
miR-155-5p, miR-21-5p, miR-93-5p, and miR-140-5p in breast cancer
progression. Curr Issues Mol Biol. 47:3772025. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Grimaldi AM, Nuzzo S, Condorelli G,
Salvatore M and Incoronato M: Prognostic and clinicopathological
significance of MiR-155 in breast cancer: A systematic review. Int
J Mol Sci. 21:58342020. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Wang F, Wang J, Zhang H, Fu B, Zhang Y,
Jia Q and Wang Y: Diagnostic value of circulating miR-155 for
breast cancer: A meta-analysis. Front Oncol. 14:13746742024.
View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Tili E, Croce CM and Michaille JJ: miR-155
: On the crosstalk between inflammation and cancer. Int Rev
Immunol. 28:264–284. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Sun R, Kong X, Qiu X, Huang C and Wong PP:
the emerging roles of pericytes in modulating tumor
microenvironment. Front Cell Dev Biol. 9:6763422021. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Anwar SL, Tanjung DS, Fitria MS, Kartika
AI, Sari DNI, Rakhmina D, Wardana T, Astuti I, Haryana SM and
Aryandono T: Dynamic changes of circulating Mir-155 expression and
the potential application as a non-invasive biomarker in breast
cancer. Asian Pac J Cancer Prev. 21:491–497. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Bašová P, Pešta M, Sochor M and Stopka T:
Prediction potential of serum miR-155 and miR-24 for relapsing
early breast cancer. Int J Mol Sci. 18:21162017. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Zhang Z, Zhang L, Yu G, Sun Z, Wang T,
Tian X, Duan X and Zhang C: Exosomal miR-1246 and miR-155 as
predictive and prognostic biomarkers for trastuzumab-based therapy
resistance in HER2-positive breast cancer. Cancer Chemother
Pharmacol. 86:761–772. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Thomopoulou K, Papadaki C, Monastirioti A,
Koronakis G, Mala A, Kalapanida D, Mavroudis D and Agelaki S:
MicroRNAs regulating tumor immune response in the prediction of the
outcome in patients with breast cancer. Front Mol Biosci.
8:6685342021. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Schwarzenbach H, Hoon DSB and Pantel K:
Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev
Cancer. 11:426–437. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
kia V, Paryan M, Mortazavi Y, Biglari A
and Mohammadi-Yeganeh S: Evaluation of exosomal miR-9 and miR-155
targeting PTEN and DUSP14 in highly metastatic breast cancer and
their effect on low metastatic cells. J Cell Biochem.
120:5666–5676. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Santos JC, da Silva Lima N, Sarian LO,
Matheu A, Ribeiro ML and Derchain SFM: Exosome-mediated breast
cancer chemoresistance via miR-155 transfer. Sci Rep. 8:8292018.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Liu F, Kong X, Lv L and Gao J: TGF-β1 acts
through miR-155 to down-regulate TP53INP1 in promoting
epithelial-mesenchymal transition and cancer stem cell phenotypes.
Cancer Lett. 359:288–298. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Khalighfard S, Alizadeh AM, Irani S and
Omranipour R: Plasma miR-21, miR-155, miR-10b, and Let-7a as the
potential biomarkers for the monitoring of breast cancer patients.
Sci Rep. 8:179812018. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Huffaker TB, Lee SH, Tang WW, Wallace JA,
Alexander M, Runtsch MC, Larsen DK, Thompson J, Ramstead AG, Voth
WP, et al: Antitumor immunity is defective in T cell-specific
microRNA-155- deficient mice and is rescued by immune checkpoint
blockade. J Biol Chem. 292:18530–18541. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Volovat SR, Volovat C, Hordila I, Hordila
DA, Mirestean CC, Miron OT, Lungulescu C, Scripcariu DV,
Stolniceanu CR, Konsoulova-Kirova AA, et al: MiRNA and LncRNA as
potential biomarkers in triple-negative breast cancer: A review.
Front Oncol. 10:5268502020. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Andrade F, Nakata A, Gotoh N and Fujita A:
Large miRNA survival analysis reveals a prognostic four-biomarker
signature for triple negative breast cancer. Genet Mol Biol.
43:e201802692020. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Santana TABDS, de Oliveira Passamai L, de
Miranda FS, Borin TF, Borges GF, Luiz WB and Campos LCG: The role
of miRNAs in the prognosis of triple-negative breast cancer: A
systematic review and meta-analysis. Diagnostics (Basel).
13:1272023. View Article : Google Scholar
|
|
164
|
Ibrahim E, Diab E, Hayek R, Hoyek K and
Kourie H: Triple-negative breast cancer: Tumor immunogenicity and
beyond. Int J Breast Cancer. 4:20979202024. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Muljo SA, Ansel KM, Kanellopoulou C,
Livingston DM, Rao A and Rajewsky K: Aberrant T cell
differentiation in the absence of Dicer. J Exp Med. 202:261–269.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Mi QS, Wang J, Liu Q, Wu X and Zhou L:
microRNA dynamic expression regulates invariant NKT cells. Cell Mol
Life Sci. 78:6003–6015. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Yao R, Ma YL, Liang W, Li HH, Ma ZJ, Yu X
and Liao YH: MicroRNA-155 modulates treg and Th17 cells
differentiation and Th17 cell function by targeting SOCS1. PLoS
One. 7:e460822012. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Touchaei AZ and Vahidi S: Unraveling the
interplay of CD8 + T cells and microRNA signaling in cancer:
Implications for immune dysfunction and therapeutic approaches. J
Transl Med. 22:11312024. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Liau NPD, Laktyushin A, Lucet IS, Murphy
JM, Yao S, Whitlock E, Callaghan K, Nicola NA, Kershaw NJ and Babon
JJ: The molecular basis of JAK/STAT inhibition by SOCS1. Nat
Commun. 9:15582018. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Alexander WS, Starr R, Fenner JE, Scott
CL, Handman E, Sprigg NS, Corbin JE, Cornish AL, Darwiche R,
Owczarek CM, et al: SOCS1 is a critical inhibitor of interferon γ
signaling and prevents the potentially fatal neonatal actions of
this cytokine. Cell. 98:597–608. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Davey GM, Starr R, Cornish AL, Burghardt
JT, Alexander WS, Carbone FR, Surh CD and Heath WR: SOCS-1
regulates IL-15-driven homeostatic proliferation of antigen-naive
CD8 T cells, limiting their autoimmune potential. J Exp Med.
202:1099–1108. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Fujitake S, Hibi K, Okochi O, Kodera Y,
Ito K, Akiyama S and Nakao A: Aberrant methylation of SOCS-1 was
observed in younger colorectal cancer patients. J Gastroenterol.
39:120–124. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Fukushima N, Sato N, Sahin F, Su GH,
Hruban RH and Goggins M: Aberrant methylation of suppressor of
cytokine signalling-1 (SOCS-1) gene in pancreatic ductal neoplasms.
Br J Cancer. 89:338–343. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Vogelstein B, Papadopoulos N, Velculescu
VE, Zhou S, Diaz LA and Kinzler KW: Cancer genome landscapes.
Science. 340:1546–1558. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Zonari E, Pucci F, Saini M, Mazzieri R,
Politi LS, Gentner B and Naldini L: A role for miR-155 in enabling
tumor-infiltrating innate immune cells to mount effective antitumor
responses in mice. Blood. 122:243–252. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Yu J, Mei J, Zuo D, Zhang M, Yu S, Li F,
Wang J, Bi D, Ma S, Wang J and Yin ZJ: Inflammatory factor-mediated
miR-155/SOCS1 signaling axis leads to Treg impairment in systemic
lupus erythematosus. Int Immunopharmacol. 141:1130132024.
View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Marson A, Kretschmer K, Frampton GM,
Jacobsen ES, Polansky JK, MacIsaac KD, Levine SS, Fraenkel E, von
Boehmer H and Young RA: Foxp3 occupancy and regulation of key
target genes during T-cell stimulation. Nature. 445:931–935. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Piña-Sánchez P, Valdez-Salazar HA and
Ruiz-Tachiquín ME: Circulating microRNAs and their role in the
immune response in triple-negative breast cancer. Oncol Lett.
20:2242020. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Vaxevanis CK, Friedrich M, Tretbar SU,
Handke D, Wang Y, Blümke J, Dummer R, Massa C and Seliger B:
Identification and characterization of novel CD274 (PD-L1)
regulating microRNAs and their functional relevance in melanoma.
Clin Transl Med. 12:e9342022. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Tumeh PC, Harview CL, Yearley JH, Shintaku
IP, Taylor EJM, Robert L, Chmielowski B, Spasic M, Henry G, Ciobanu
V, et al: PD-1 blockade induces responses by inhibiting adaptive
immune resistance. Nature. 515:568–571. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Eichmüller SB, Osen W, Mandelboim O and
Seliger B: Immune modulatory microRNAs involved in tumor attack and
tumor immune escape. J Natl Cancer Inst. 109:doi:
10.1093/jnci/djx03. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Manore SG, Doheny DL, Wong GL and Lo HW:
IL-6/JAK/stat3 signaling in breast cancer metastasis: Biology and
treatment. Front Oncol. 12:8660142022. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Gyamfi J, Lee YH, Eom M and Choi J:
Interleukin-6/STAT3 signalling regulates adipocyte induced
epithelial-mesenchymal transition in breast cancer cells. Sci Rep.
8:88592018. View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Taghikhani A, Hassan ZM, Ebrahimi M and
Moazzeni SM: microRNA modified tumor-derived exosomes as novel
tools for maturation of dendritic cells. J Cell Physiol.
234:9417–9427. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Yang P, Cao X, Cai H, Chen X, Zhu Y, Yang
Y, An W and Jie J: Upregulation of microRNA-155 enhanced migration
and function of dendritic cells in three-dimensional breast cancer
microenvironment. Immunol Invest. 50:1058–1071. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Kordaß T, Chao TY, Osen W and Eichmüller
SB: Novel microRNAs modulating ecto-5′-nucleotidase expression.
Front Immunol. 14:11993742023. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Hering C and Conover GM: Advancing
ischemic stroke prognosis: Key role of MIR-155 non-coding RNA. Int
J Mol Sci. 26:39472025. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Qattan A: Genomic alterations affecting
competitive endogenous RNAs (ceRNAs) and regulatory networks
(ceRNETs) with clinical implications in triple-negative breast
cancer (TNBC). Int J Mol Sci. 25:26242024. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Wilson TR, Udyavar AR, Chang CW, Spoerke
JM, Aimi J, Savage HM, Daemen A, O'Shaughnessy JA, Bourgon R and
Lackner MR: Genomic alterations associated with recurrence and TNBC
subtype in high-risk early breast cancers. Mol Cancer Res.
17:97–108. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Skourti E, Volpe A, Lang C, Johnson P,
Panagaki F and Fruhwirth GO: Spatiotemporal quantitative
microRNA-155 imaging reports immune-mediated changes in a
triple-negative breast cancer model. Front Immunol. 14:11802332023.
View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Duan Q, Zhang H, Zheng J and Zhang L:
Turning cold into hot: Firing up the tumor microenvironment. Trends
Cancer. 6:605–618. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Galon J and Bruni D: Approaches to treat
immune hot, altered and cold tumours with combination
immunotherapies. Nat Rev Drug Discov. 18:197–218. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Chen Y, Gao DY and Huang L: In vivo
delivery of miRNAs for cancer therapy: Challenges and strategies.
Adv Drug Deliv Rev. 81:128–141. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Haussecker D: Current issues of RNAi
therapeutics delivery and development. J Control Release.
195:49–54. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Whitehead KA, Langer R and Anderson DG:
Knocking down barriers: Advances in siRNA delivery. Nat Rev Drug
Discov. 8:129–138. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Zhao J and Feng SS: Nanocarriers for
delivery of siRNA and co-delivery of siRNA and other therapeutic
agents. Nanomedicine (Lond). 10:2199–2228. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Pagoni M, Cava C, Sideris DC, Avgeris M,
Zoumpourlis V, Michalopoulos I and Drakoulis N: miRNA-Based
technologies in cancer therapy. J Pers Med. 13:15862023. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
El Sayed SR, Cristante J, Guyon L, Denis
J, Chabre O and Cherradi N: Microrna therapeutics in cancer:
Current advances and challenges. Cancers (Basel). 29:26802021.
View Article : Google Scholar
|
|
199
|
Dasgupta I and Chatterjee A: Recent
advances in miRNA delivery systems. Methods Protoc. 4:102021.
View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Serpico D, Molino L and Di Cosimo S:
MicroRNAs in breast cancer development and treatment. Cancer Treat
Rev. 40:595–604. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
De Planell-Saguer M and Rodicio MC:
Analytical aspects of microRNA in diagnostics: A review. Anal Chim
Acta. 699:134–152. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Reid G, Kirschner MB and van Zandwijk N:
Circulating microRNAs: Association with disease and potential use
as biomarkers. Crit Rev Oncol Hematol. 80:193–208. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Zou R, Loke SY, Tang YC, Too HP, Zhou L,
Lee ASG and Hartman M: Development and validation of a circulating
microRNA panel for the early detection of breast cancer. Br J
Cancer. 126:472–481. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Ho PTB, Clark IM and Le LTT:
MicroRNA-based diagnosis and therapy. Int J Mol Sci. 23:71672022.
View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Kim T and Croce CM: MicroRNA: Trends in
clinical trials of cancer diagnosis and therapy strategies. Exp Mol
Med. 55:1314–132. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Calin GA and Croce CM: MicroRNA signatures
in human cancers. Nat Rev Cancer. 6:857–866. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Mitchell PS, Parkin RK, Kroh EM, Fritz BR,
Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O'Briant
KC, Allen A, et al: Circulating microRNAs as stable blood-based
markers for cancer detection. Proc Natl Acad Sci USA.
105:10513–10518. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Pruneri G, Gray KP, Vingiani A, Viale G,
Curigliano G, Criscitiello C, Láng I, Ruhstaller T, Gianni L,
Goldhirsch A, et al: Tumor-infiltrating lymphocytes (TILs) are a
powerful prognostic marker in patients with triple-negative breast
cancer enrolled in the IBCSG phase III randomized clinical trial
22–00. Breast Cancer Res Treat. 158:323–331. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Hendry S, Salgado R, Gevaert T, Russell
PA, John T, Thapa B, Christie M, van de Vijver K, Estrada MV,
Gonzalez-Ericsson PI, et al: Assessing tumor-infiltrating
lymphocytes in solid tumors: A practical review for pathologists
and proposal for a standardized method from the international
immunooncology biomarkers working group: Part 1: Assessing the host
immune response, TILs in invasive breast carcinoma and ductal
carcinoma in situ, metastatic tumor deposits and areas for further
research. Adv Anat Pathol. 24:235–251. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Ly A, Garcia V, Blenman KRM, Ehinger A,
Elfer K, Hanna MG, Li X, Peeters DJE, Birmingham R, Dudgeon S, et
al: Training pathologists to assess stromal tumour-infiltrating
lymphocytes in breast cancer synergises efforts in clinical care
and scientific research. Histopathology. 84:915–923. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Koboldt D, Fulton RS, Mclellan MD, Schmidt
H, Kalicki-Veizer J, McMichael JF, Fulton L, Dooling DJ, Ding L,
Mardis E, et al: Comprehensive molecular portraits of human breast
tumours. Nature. 490:61–70. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Kalecky K, Modisette R, Pena S, Cho YR and
Taube J: Integrative analysis of breast cancer profiles in TCGA by
TNBC subgrouping reveals novel microRNA-specific clusters,
including miR-17-92a, distinguishing basal-like 1 and basal-like 2
TNBC subtypes. BMC Cancer. 20:1412020. View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Chakraborty C, Sharma AR, Sharma G and Lee
SS: The Interplay among miRNAs, major cytokines, and cancer-related
inflammation. Mol Ther Nucleic Acids. 20:606–620. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
214
|
Hill M and Tran N: miRNA interplay:
Mechanisms and consequences in cancer. Dis Model Mech.
14:dmm0476622021. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Jimenez JE, Abdelhafez A, Mittendorf EA,
Elshafeey N, Yung JP, Litton JK, Adrada BE, Candelaria RP, White J,
Thompson AM, et al: A model combining pretreatment MRI radiomic
features and tumor-infiltrating lymphocytes to predict response to
neoadjuvant systemic therapy in triple-negative breast cancer. Eur
J Radiol. 149:1102202022. View Article : Google Scholar : PubMed/NCBI
|
|
216
|
Asano Y, Kashiwagi S, Goto W, Takada K,
Takahashi K, Hatano T, Takashima T, Tomita S, Motomura H, Ohsawa M,
et al: Prediction of treatment response to neoadjuvant chemotherapy
in breast cancer by subtype using tumor-infiltrating lymphocytes.
Anticancer Res. 38:2311–2321. 2018.PubMed/NCBI
|
|
217
|
Song IH, Heo SH, Bang WS, Park HS, Park
IA, Kim YA, Park SY, Roh J, Gong G and Lee HJ: Predictive value of
tertiary lymphoid structures assessed by high endothelial venule
counts in the neoadjuvant setting of triple-negative breast cancer.
Cancer Res Treat. 49:399–407. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
218
|
Khoury T, Nagrale V, Opyrchal M, Peng X,
Wang D and Yao S: Prognostic significance of stromal versus
intratumoral infiltrating lymphocytes in different subtypes of
breast cancer treated with cytotoxic neoadjuvant chemotherapy. Appl
Immunohistochem Mol Morphol. 26:523–532. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Ruan M, Tian T, Rao J, Xu X, Yu B, Yang W
and Shui R: Predictive value of tumor-infiltrating lymphocytes to
pathological complete response in neoadjuvant treated
triple-negative breast cancers. Diagn Pathol. 13:662018. View Article : Google Scholar : PubMed/NCBI
|