|
1
|
Osipov A, Saung MT, Zheng L and Murphy AG:
Small molecule immunomodulation: The tumor microenvironment and
overcoming immune escape. J Immunother Cancer. 7:2242019.
View Article : Google Scholar : PubMed/NCBI
|
|
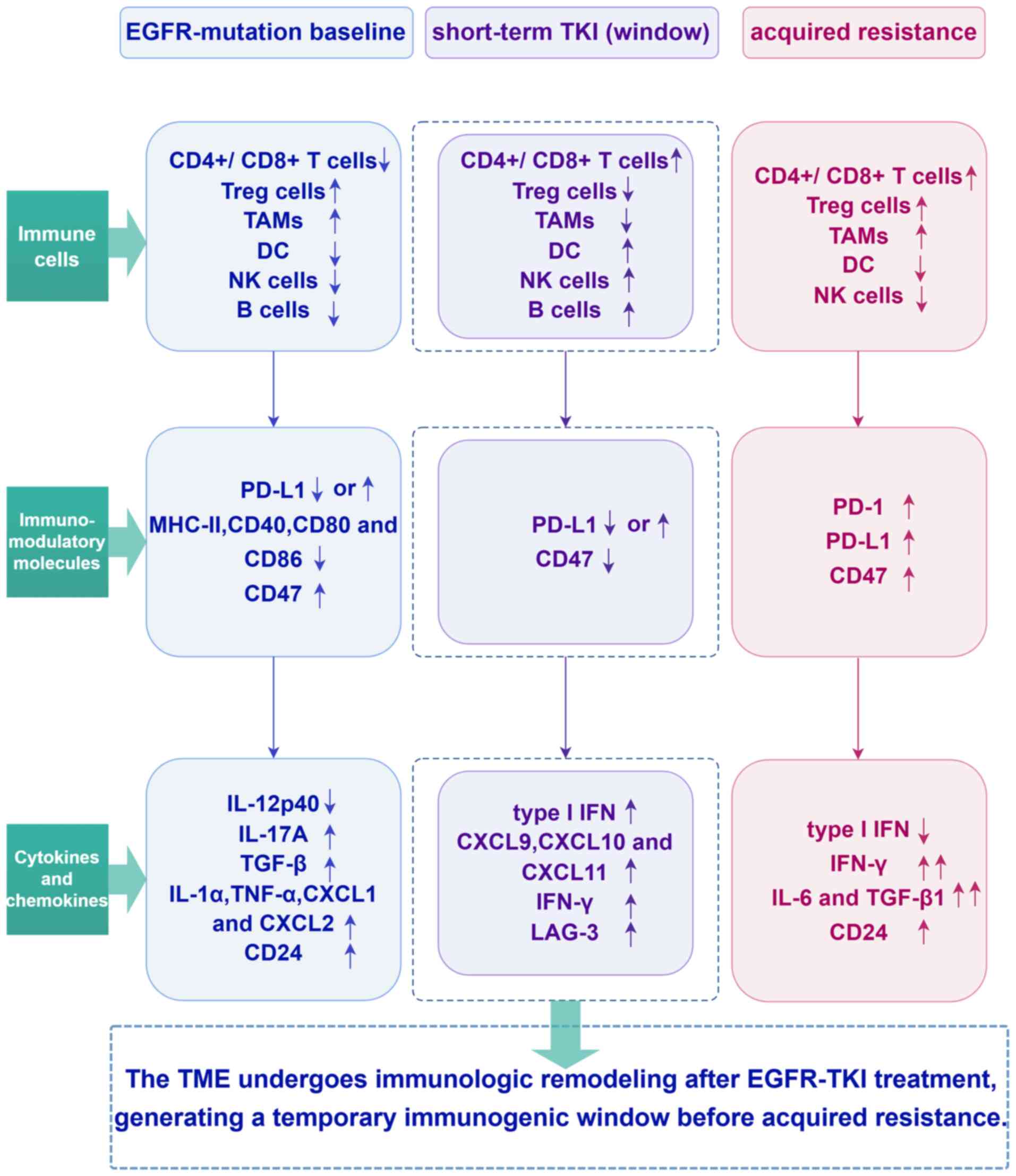
2
|
Vuletic A, Mirjacic Martinovic K and
Jurisic V: The role of tumor microenvironment in triple-negative
breast cancer and its therapeutic targeting. Cells. 14:13532025.
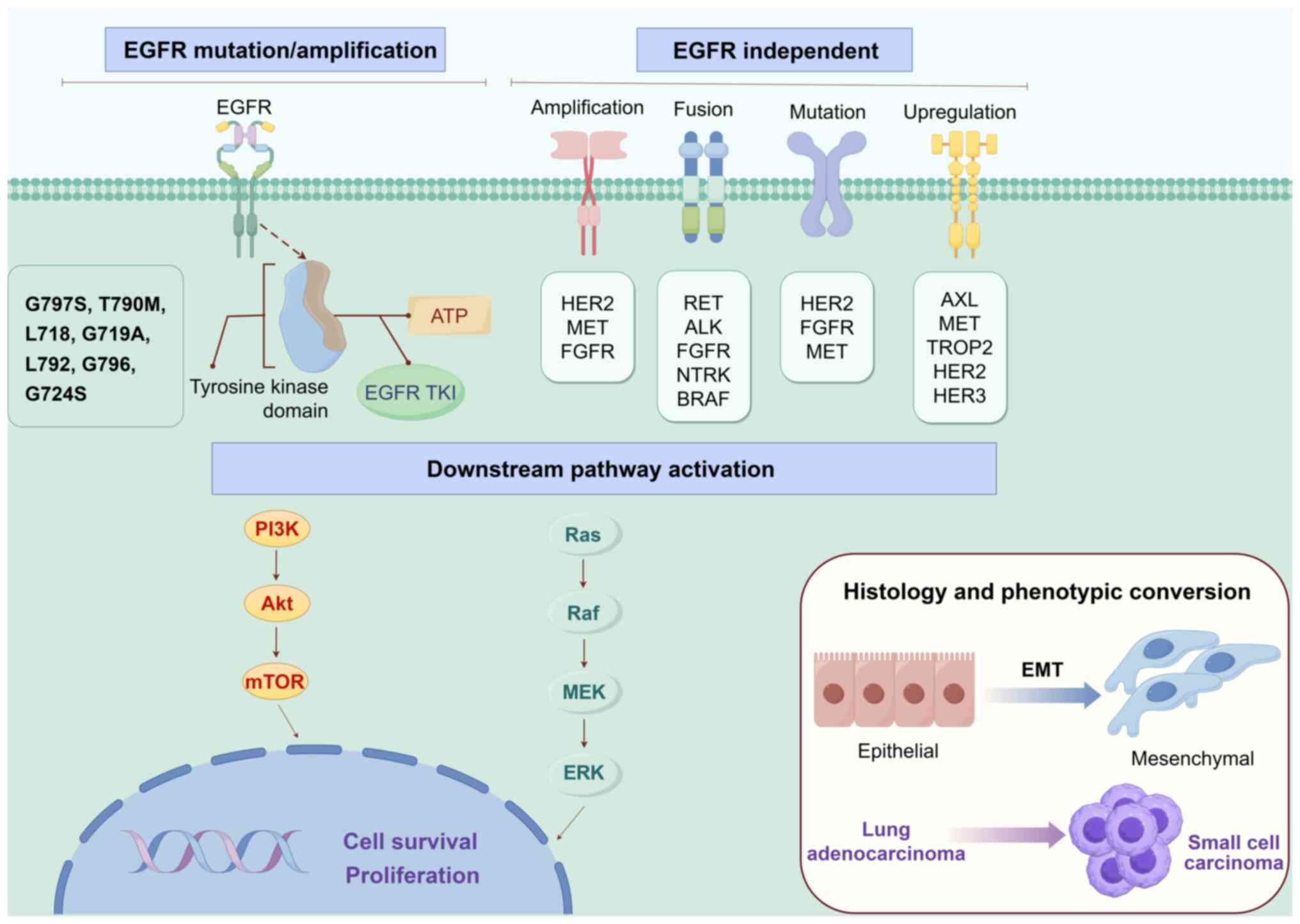
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kraja FP, Jurisic VB, Hromić-Jahjefendić
A, Rossopoulou N, Katsila T, Mirjacic Martinovic K, De Las Rivas J,
Diaconu CC and Szöőr Á: Tumor-infiltrating lymphocytes in cancer
immunotherapy: From chemotactic recruitment to translational
modeling. Front Immunol. 16:16017732025. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vryza P, Fischer T, Mistakidi E and
Zaravinos A: Tumor mutation burden in the prognosis and response of
lung cancer patients to immune-checkpoint inhibition therapies.
Transl Oncol. 38:1017882023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
To KKW, Fong W and Cho WCS: Immunotherapy
in treating EGFR-mutant lung cancer: Current challenges and new
strategies. Front Oncol. 11:6350072021. View Article : Google Scholar : PubMed/NCBI
|
|
6
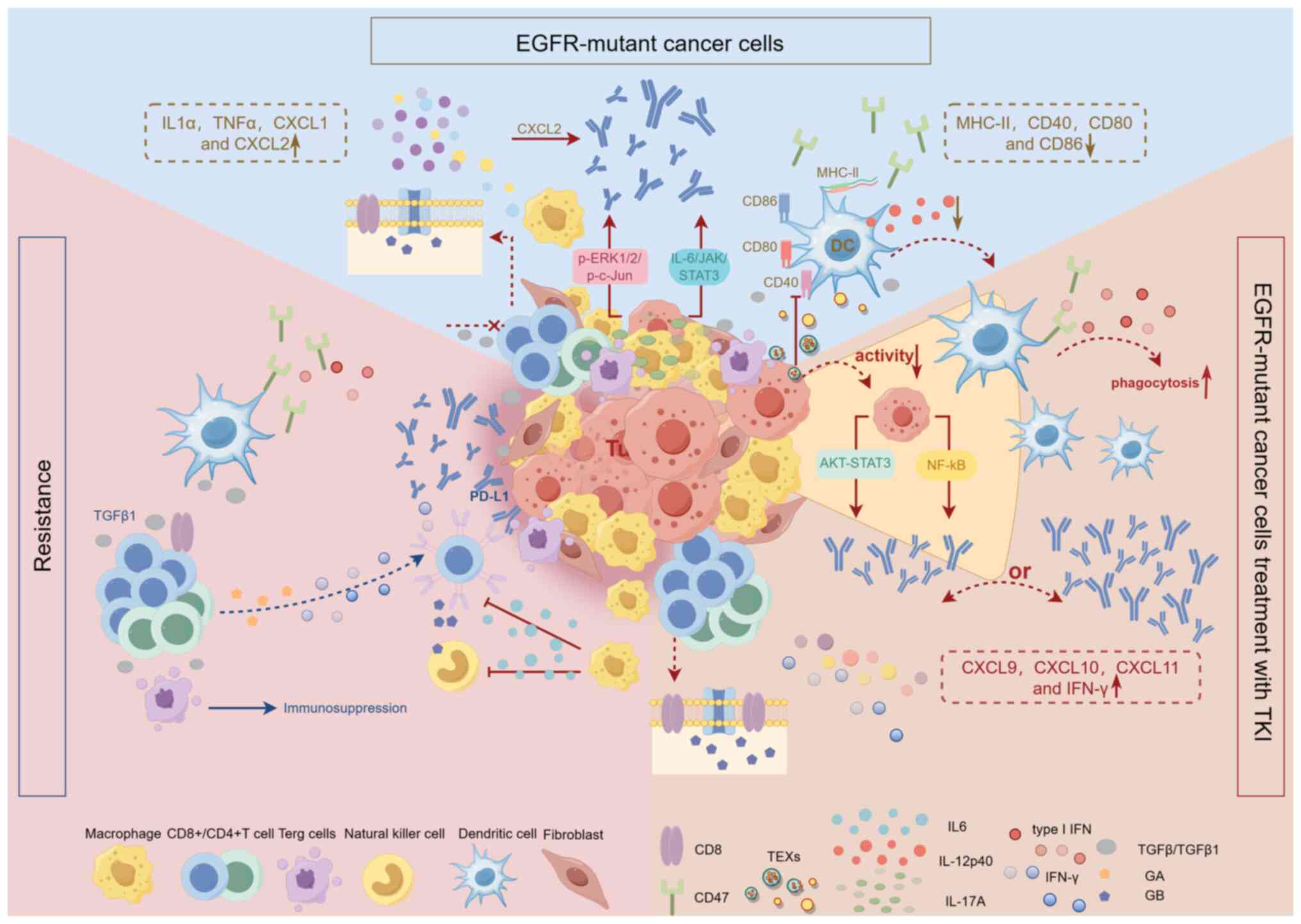
|
Jurisic V, Vukovic V, Obradovic J,
Gulyaeva LF, Kushlinskii NE and Djordjević N: EGFR polymorphism and
survival of NSCLC patients treated with TKIs: A systematic review
and meta-analysis. J Oncol. 2020:19732412020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li K, Quan L, Huang F, Li Y and Shen Z:
ADAM12 promotes the resistance of lung adenocarcinoma cells to
EGFR-TKI and regulates the immune microenvironment by activating
PI3K/Akt/mTOR and RAS signaling pathways. Int Immunopharmacol.
122:1105802023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jeong HO, Lee H, Kim H, Jang J, Kim S,
Hwang T, Choi DW, Kim HS, Lee N, Lee YM, et al: Cellular plasticity
and immune microenvironment of malignant pleural effusion are
associated with EGFR-TKI resistance in non-small-cell lung
carcinoma. iScience. 25:1053582022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu L, Wang C, Li S, Bai H and Wang J:
Tumor immune microenvironment in epidermal growth factor
receptor-mutated non-small cell lung cancer before and after
epidermal growth factor receptor tyrosine kinase inhibitor
treatment: A narrative review. Transl Lung Cancer Res.
10:3823–3839. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lu C, Gao Z, Wu D, Zheng J, Hu C, Huang D,
He C, Liu Y, Lin C, Peng T, et al: Understanding the dynamics of
TKI-induced changes in the tumor immune microenvironment for
improved therapeutic effect. J Immunother Cancer. 12:e0091652024.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Corvaja C, Passaro A, Attili I, Aliaga PT,
Spitaleri G, Signore ED and De Marinis F: Advancements in
fourth-generation EGFR TKIs in EGFR-mutant NSCLC: Bridging
biological insights and therapeutic development. Cancer Treat Rev.
130:1028242024. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Owen DH, Ismaila N, Ahluwalia A, Feldman
J, Gadgeel S, Mullane M, Naidoo J, Presley CJ, Reuss JE, Singhi EK
and Patel JD: Therapy for stage IV non-small cell lung cancer with
driver alterations: ASCO living guideline, version 2024.3. J Clin
Oncol. 43:e2–e16. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Obradović J, Niševic-Lazović J, Sekeruš V,
Milašin J, Perin B and Jurisic V: Investigating the frequencies of
EGFR mutations and EGFR single nucleotide polymorphisms genotypes
and their predictive role in NSCLC patients in Republic of Serbia.
Mol Biol Rep. 52:3502025. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamaoka T, Ohba M and Ohmori T:
Molecular-targeted therapies for epidermal growth factor receptor
and its resistance mechanisms. Int J Mol Sci. 18:24202017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yu HA, Arcila ME, Rekhtman N, Sima CS,
Zakowski MF, Pao W, Kris MG, Miller VA, Ladanyi M and Riely GJ:
Analysis of tumor specimens at the time of acquired resistance to
EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers.
Clin Cancer Res. 19:2240–2247. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wu SG and Shih JY: Management of acquired
resistance to EGFR TKI-targeted therapy in advanced non-small cell
lung cancer. Mol Cancer. 17:382018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zalaquett Z, Catherine Rita Hachem M,
Kassis Y, Hachem S, Eid R, Raphael Kourie H and Planchard D:
Acquired resistance mechanisms to osimertinib: The constant battle.
Cancer Treat Rev. 116:1025572023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Westover D, Zugazagoitia J, Cho BC, Lovly
CM and Paz-Ares L: Mechanisms of acquired resistance to first- and
second-generation EGFR tyrosine kinase inhibitors. Ann Oncol. 29
(Suppl 1):i10–i19. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ko B, Paucar D and Halmos B: EGFR T790M:
Revealing the secrets of a gatekeeper. Lung Cancer (Auckl).
8:147–159. 2017.PubMed/NCBI
|
|
20
|
Leonetti A, Sharma S, Minari R, Perego P,
Giovannetti E and Tiseo M: Resistance mechanisms to osimertinib in
EGFR-mutated non-small cell lung cancer. Br J Cancer. 121:725–737.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Thress KS, Paweletz CP, Felip E, Cho BC,
Stetson D, Dougherty B, Lai Z, Markovets A, Vivancos A, Kuang Y, et
al: Acquired EGFR C797S mutation mediates resistance to AZD9291 in
non-small cell lung cancer harboring EGFR T790M. Nat Med.
21:560–562. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Niederst MJ, Hu H, Mulvey HE, Lockerman
EL, Garcia AR, Piotrowska Z, Sequist LV and Engelman JA: The
allelic context of the C797S mutation acquired upon treatment with
third-generation EGFR inhibitors impacts sensitivity to subsequent
treatment strategies. Clin Cancer Res. 21:3924–3933. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Passaro A, Jänne PA, Mok T and Peters S:
Overcoming therapy resistance in EGFR-mutant lung cancer. Nat
Cancer. 2:377–391. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Proto C, Lo Russo G, Corrao G, Ganzinelli
M, Facchinetti F, Minari R, Tiseo M and Garassino MC: Treatment in
EGFR-mutated non-small cell lung cancer: How to block the receptor
and overcome resistance mechanisms. Tumori. 103:325–337. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Du X, Yang B, An Q, Assaraf YG, Cao X and
Xia J: Acquired resistance to third-generation EGFR-TKIs and
emerging next-generation EGFR inhibitors. Innovation (Camb).
2:1001032021.PubMed/NCBI
|
|
26
|
Roy V and Perez EA: Beyond trastuzumab:
Small molecule tyrosine kinase inhibitors in HER-2-positive breast
cancer. Oncologist. 14:1061–1069. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Engelman JA, Zejnullahu K, Mitsudomi T,
Song Y, Hyland C, Park JO, Lindeman N, Gale CM, Zhao X, Christensen
J, et al: MET amplification leads to gefitinib resistance in lung
cancer by activating ERBB3 signaling. Science. 316:1039–1043. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Punekar SR, Velcheti V, Neel BG and Wong
KK: The current state of the art and future trends in RAS-targeted
cancer therapies. Nat Rev Clin Oncol. 19:637–655. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ohashi K, Sequist LV, Arcila ME, Lovly CM,
Chen X, Rudin CM, Moran T, Camidge DR, Vnencak-Jones CL, Berry L,
et al: Characteristics of lung cancers harboring NRAS mutations.
Clin Cancer Res. 19:2584–2591. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Simanshu DK, Nissley DV and McCormick F:
RAS proteins and their regulators in human disease. Cell.
170:17–33. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Polivka J and Janku F: Molecular targets
for cancer therapy in the PI3K/AKT/mTOR pathway. Pharmacol Ther.
142:164–175. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Eng J, Woo KM, Sima CS, Plodkowski A,
Hellmann MD, Chaft JE, Kris MG, Arcila ME, Ladanyi M and Drilon A:
Impact of concurrent PIK3CA mutations on response to EGFR tyrosine
kinase inhibition in EGFR-mutant lung cancers and on prognosis in
oncogene-driven lung adenocarcinomas. J Thorac Oncol. 10:1713–1719.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Pollak M: Insulin and insulin-like growth
factor signalling in neoplasia. Nat Rev Cancer. 8:915–928. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Namba K, Shien K, Takahashi Y, Torigoe H,
Sato H, Yoshioka T, Takeda T, Kurihara E, Ogoshi Y, Yamamoto H, et
al: Activation of AXL as a preclinical acquired resistance
mechanism against osimertinib treatment in EGFR-mutant non-small
Cell Lung Cancer Cells. Mol Cancer Res. 17:499–507. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sequist LV, Waltman BA, Dias-Santagata D,
Digumarthy S, Turke AB, Fidias P, Bergethon K, Shaw AT, Gettinger
S, Cosper AK, et al: Genotypic and histological evolution of lung
cancers acquiring resistance to EGFR inhibitors. Sci Transl Med.
3:75ra262011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Oser MG, Niederst MJ, Sequist LV and
Engelman JA: Transformation from non-small-cell lung cancer to
small-cell lung cancer: Molecular drivers and cells of origin.
Lancet Oncol. 16:e165–e172. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yin X, Li Y, Wang H, Jia T, Wang E, Luo Y,
Wei Y, Qin Z and Ma X: Small cell lung cancer transformation: From
pathogenesis to treatment. Semin Cancer Biol. 86:595–606. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Li Y, Xie T, Wang S, Yang L, Hao X, Wang
Y, Hu X, Wang L, Li J, Ying J and Xing P: Mechanism exploration and
model construction for small cell transformation in EGFR-mutant
lung adenocarcinomas. Signal Transduct Target Ther. 9:2612024.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lee JK, Lee J, Kim S, Kim S, Youk J, Park
S, An Y, Keam B, Kim DW, Heo DS, et al: Clonal history and genetic
predictors of transformation into small-cell carcinomas from lung
adenocarcinomas. J Clin Oncol. 35:3065–3074. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Huang L and Fu L: Mechanisms of resistance
to EGFR tyrosine kinase inhibitors. Acta Pharm Sin B. 5:390–401.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Neel DS and Bivona TG: Secrets of drug
resistance in NSCLC exposed by new molecular definition of EMT.
Clin Cancer Res. 19:3–5. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sumimoto H, Takano A, Igarashi T, Hanaoka
J, Teramoto K and Daigo Y: Oncogenic epidermal growth factor
receptor signal-induced histone deacetylation suppresses chemokine
gene expression in human lung adenocarcinoma. Sci Rep. 13:50872023.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yu S, Sha H, Qin X, Chen Y, Li X, Shi M
and Feng J: EGFR E746-A750 deletion in lung cancer represses
antitumor immunity through the exosome-mediated inhibition of
dendritic cells. Oncogene. 39:2643–2657. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fang Y, Wang Y, Zeng D, Zhi S, Shu T,
Huang N, Zheng S, Wu J, Liu Y, Huang G, et al: Comprehensive
analyses reveal TKI-induced remodeling of the tumor immune
microenvironment in EGFR/ALK-positive non-small-cell lung cancer.
Oncoimmunology. 10:19510192021. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Lin Z, Wang Q, Jiang T, Wang W and Zhao
JJ: Targeting tumor-associated macrophages with STING agonism
improves the antitumor efficacy of osimertinib in a mouse model of
EGFR-mutant lung cancer. Front Immunol. 14:10772032023. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chen Q, Xia L, Wang J, Zhu S, Wang J, Li
X, Yu Y, Li Z, Wang Y, Zhu G and Lu S: EGFR-mutant NSCLC may
remodel TME from non-inflamed to inflamed through acquiring
resistance to EGFR-TKI treatment. Lung Cancer. 192:1078152024.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Jia Y, Li X, Jiang T, Zhao S, Zhao C,
Zhang L, Liu X, Shi J, Qiao M, Luo J, et al: EGFR-targeted therapy
alters the tumor microenvironment in EGFR-driven lung tumors:
Implications for combination therapies. Int J Cancer.
145:1432–1444. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wang DH, Lee HS, Yoon D, Berry G, Wheeler
TM, Sugarbaker DJ, Kheradmand F, Engleman E and Burt BM:
Progression of EGFR-mutant lung adenocarcinoma is driven by
alveolar macrophages. Clin Cancer Res. 23:778–788. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Valenti R, Huber V, Iero M, Filipazzi P,
Parmiani G and Rivoltini L: Tumor-released microvesicles as
vehicles of immunosuppression. Cancer Res. 67:2912–2915. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Gao L, Wang L, Dai T, Jin K, Zhang Z, Wang
S, Xie F, Fang P, Yang B, Huang H, et al: Tumor-derived exosomes
antagonize innate antiviral immunity. Nat Immunol. 19:233–245.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zhang H, Deng T, Liu R, Bai M, Zhou L,
Wang X, Li S, Wang X, Yang H, Li J, et al: Exosome-delivered EGFR
regulates liver microenvironment to promote gastric cancer liver
metastasis. Nat Commun. 8:150162017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Cho JW, Park S, Kim G, Han H, Shim HS,
Shin S, Bae YS, Park SY, Ha SJ, Lee I and Kim HR: Dysregulation of
TFH-B-TRM lymphocyte cooperation is
associated with unfavorable anti-PD-1 responses in EGFR-mutant lung
cancer. Nat Commun. 12:60682021. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Zhao J, Lu Y, Wang Z, Wang H, Zhang D, Cai
J, Zhang B, Zhang J, Huang M, Pircher A, et al: Tumor immune
microenvironment analysis of non-small cell lung cancer development
through multiplex immunofluorescence. Transl Lung Cancer Res.
13:2395–2410. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
He S, Yin T, Li D, Gao X, Wan Y, Ma X, Ye
T, Guo F, Sun J, Lin Z and Wang Y: Enhanced interaction between
natural killer cells and lung cancer cells: Involvement in
gefitinib-mediated immunoregulation. J Transl Med. 11:1862013.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Patel SA, Nilsson MB, Yang Y, Le X, Tran
HT, Elamin YY, Yu X, Zhang F, Poteete A, Ren X, et al: IL6 Mediates
suppression of T- and NK-cell function in EMT-associated
TKI-resistant EGFR-mutant NSCLC. Clin Cancer Res. 29:1292–1304.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yang L, He YT, Dong S, Wei XW, Chen ZH,
Zhang B, Chen WD, Yang XR, Wang F, Shang XM, et al: Single-cell
transcriptome analysis revealed a suppressive tumor immune
microenvironment in EGFR mutant lung adenocarcinoma. J Immunother
Cancer. 10:e0035342022. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Chen J, Jiang CC, Jin L and Zhang XD:
Regulation of PD-L1: A novel role of pro-survival signalling in
cancer. Ann Oncol. 27:409–416. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang Y, Wang L, Li Y, Pan Y, Wang R, Hu
H, Li H, Luo X, Ye T, Sun Y and Chen H: Protein expression of
programmed death 1 ligand 1 and ligand 2 independently predict poor
prognosis in surgically resected lung adenocarcinoma. Onco Targets
Ther. 7:567–573. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Azuma K, Ota K, Kawahara A, Hattori S,
Iwama E, Harada T, Matsumoto K, Takayama K, Takamori S, Kage M, et
al: Association of PD-L1 overexpression with activating EGFR
mutations in surgically resected nonsmall-cell lung cancer. Ann
Oncol. 25:1935–1940. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Yang CY, Liao WY, Ho CC, Chen KY, Tsai TH,
Hsu CL, Su KY, Chang YL, Wu CT, Hsu CC, et al: Association between
programmed death-ligand 1 expression, immune microenvironments, and
clinical outcomes in epidermal growth factor receptor mutant lung
adenocarcinoma patients treated with tyrosine kinase inhibitors.
Eur J Cancer. 124:110–122. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Akbay EA, Koyama S, Carretero J, Altabef
A, Tchaicha JH, Christensen CL, Mikse OR, Cherniack AD, Beauchamp
EM, Pugh TJ, et al: Activation of the PD-1 pathway contributes to
immune escape in EGFR-driven lung tumors. Cancer Discov.
3:1355–1363. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Lin K, Cheng J, Yang T, Li Y and Zhu B:
EGFR-TKI down-regulates PD-L1 in EGFR mutant NSCLC through
inhibiting NF-κB. Biochem Biophys Res Commun. 463:95–101. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Abdelhamed S, Ogura K, Yokoyama S, Saiki I
and Hayakawa Y: AKT-STAT3 pathway as a downstream target of EGFR
signaling to regulate PD-L1 expression on NSCLC cells. J Cancer.
7:1579–1586. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
D'Incecco A, Andreozzi M, Ludovini V,
Rossi E, Capodanno A, Landi L, Tibaldi C, Minuti G, Salvini J,
Coppi E, et al: PD-1 and PD-L1 expression in molecularly selected
non-small-cell lung cancer patients. Br J Cancer. 112:95–102. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Soo RA, Lim SM, Syn NL, Teng R, Soong R,
Mok TSK and Cho BC: Immune checkpoint inhibitors in epidermal
growth factor receptor mutant non-small cell lung cancer: Current
controversies and future directions. Lung Cancer. 115:12–20. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Chen N, Fang W, Zhan J, Hong S, Tang Y,
Kang S, Zhang Y, He X, Zhou T, Qin T, et al: Upregulation of PD-L1
by EGFR activation mediates the immune escape in EGFR-driven NSCLC:
Implication for optional immune targeted therapy for NSCLC patients
with EGFR mutation. J Thorac Oncol. 10:910–923. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhang N, Zeng Y, Du W, Zhu J, Shen D, Liu
Z and Huang JA: The EGFR pathway is involved in the regulation of
PD-L1 expression via the IL-6/JAK/STAT3 signaling pathway in
EGFR-mutated non-small cell lung cancer. Int J Oncol. 49:1360–1368.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Gainor JF, Shaw AT, Sequist LV, Fu X,
Azzoli CG, Piotrowska Z, Huynh TG, Zhao L, Fulton L, Schultz KR, et
al: EGFR mutations and ALK rearrangements are associated with low
response rates to PD-1 pathway blockade in non-small cell lung
cancer: A retrospective analysis. Clin Cancer Res. 22:4585–4593.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Li D, Zou S, Cheng S, Song S, Wang P and
Zhu X: Monitoring the response of PD-L1 expression to epidermal
growth factor receptor tyrosine kinase inhibitors in nonsmall-cell
lung cancer xenografts by immuno-PET imaging. Mol Pharm.
16:3469–3476. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
He H, Qi X, Fu H, Xu J, Zheng Q, Chen L,
Zhang Y, Hua H, Xu W, Xu Z, et al: Imaging diagnosis and efficacy
monitoring by [89Zr]Zr-DFO-KN035 immunoPET in patients
with PD-L1-positive solid malignancies. Theranostics. 14:392–405.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Huang W, Zhou J, Liu Y, Yang Y, Saladin
RJ, Hsu JC, Cai W and Kang L: Advances in immunoPET/SPECT imaging:
The role of Fab and F(ab')2 fragments in theranostics.
Acta Pharm Sin B. 15:3888–3924. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Xing S, Hu K and Wang Y: Tumor immune
microenvironment and immunotherapy in non-small cell lung cancer:
Update and new challenges. Aging Dis. 13:1615–1632. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Isomoto K, Haratani K, Hayashi H, Shimizu
S, Tomida S, Niwa T, Yokoyama T, Fukuda Y, Chiba Y, Kato R, et al:
Impact of EGFR-TKI treatment on the tumor immune microenvironment
in EGFR mutation-positive non-small cell lung cancer. Clin Cancer
Res. 26:2037–2046. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wang S, Rong R, Yang DM, Fujimoto J,
Bishop JA, Yan S, Cai L, Behrens C, Berry LD, Wilhelm C, et al:
Features of tumor-microenvironment images predict targeted therapy
survival benefit in patients with EGFR-mutant lung cancer. J Clin
Invest. 133:e1603302023. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Haratani K, Hayashi H, Tanaka T, Kaneda H,
Togashi Y, Sakai K, Hayashi K, Tomida S, Chiba Y, Yonesaka K, et
al: Tumor immune microenvironment and nivolumab efficacy in EGFR
mutation-positive non-small-cell lung cancer based on T790M status
after disease progression during EGFR-TKI treatment. Ann Oncol.
28:1532–1539. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Nigro A, Ricciardi L, Salvato I, Sabbatino
F, Vitale M, Crescenzi MA, Montico B, Triggiani M, Pepe S, Stellato
C, et al: Enhanced expression of CD47 is associated with off-target
resistance to tyrosine kinase inhibitor gefitinib in NSCLC. Front
Immunol. 10:31352020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Jurisic V: Multiomic analysis of cytokines
in immuno-oncology. Expert Rev Proteomics. 17:663–674. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Jurisić V, Bogdanovic G, Srdic T, Jakimov
D, Mrdjanovic J, Baltic M and Baltic VV: Modulation of TNF-alpha
activity in tumor PC cells using anti-CD45 and anti-CD95 monoclonal
antibodies. Cancer Lett. 214:55–61. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Jurisic V, Srdic-Rajic T, Konjevic G,
Bogdanovic G and Colic M: TNF-α induced apoptosis is accompanied
with rapid CD30 and slower CD45 shedding from K-562 cells. J Membr
Biol. 239:115–122. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Lee KL, Lai TC, Lee WJ, Chen YC, Ho KH,
Hung WY, Yang YC, Chan MH, Hsieh FK, Chung CL, et al: Sustaining
the activation of EGFR signal by inflammatory cytokine IL17A
prompts cell proliferation and EGFR-TKI resistance in lung cancer.
Cancers (Basel). 15:32882023. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Huang H, Zhu X, Yu Y, Li Z, Yang Y, Xia L
and Lu S: EGFR mutations induce the suppression of CD8+
T cell and anti-PD-1 resistance via ERK1/2-p90RSK-TGF-β axis in
non-small cell lung cancer. J Transl Med. 22:6532024. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Hong SH, Kang N, Kim O, Hong SA, Park J,
Kim J, Lee MA and Kang J: EGFR-tyrosine kinase inhibitors induced
activation of the autocrine CXCL10/CXCR3 pathway through crosstalk
between the tumor and the microenvironment in EGFR-mutant lung
cancer. Cancers (Basel). 15:1242022. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Mirjačić Martinović K, Vuletić A, Tišma
Miletić N, Besu Žižak I, Milovanović J, Matković S and Jurišić V:
Circulating cytokine dynamics as potential biomarker of response to
anti-PD-1 immunotherapy in BRAFwt MM patients. Transl Oncol.
38:1017992023. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Inoue C, Miki Y, Saito R, Hata S, Abe J,
Sato I, Okada Y and Sasano H: PD-L1 induction by cancer-associated
fibroblast-derived factors in lung adenocarcinoma cells. Cancers
(Basel). 11:12572019. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Shiiya A, Noguchi T, Tomaru U, Ariga S,
Takashima Y, Ohhara Y, Taguchi J, Takeuchi S, Shimizu Y, Kinoshita
I, et al: EGFR inhibition in EGFR-mutant lung cancer cells perturbs
innate immune signaling pathways in the tumor microenvironment.
Cancer Sci. 114:1270–1283. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhou J, Yu X, Hou L, Zhao J, Zhou F, Chu
X, Wu Y, Zhou C and Su C: Epidermal growth factor receptor tyrosine
kinase inhibitor remodels tumor microenvironment by upregulating
LAG-3 in advanced non-small-cell lung cancer. Lung Cancer.
153:143–149. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Lee CK, Man J, Lord S, Cooper W, Links M,
Gebski V, Herbst RS, Gralla RJ, Mok T and Yang JC: Clinical and
molecular characteristics associated with survival among patients
treated with checkpoint inhibitors for advanced non-small cell lung
carcinoma: A systematic review and meta-analysis. JAMA Oncol.
4:210–216. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Lee CK, Man J, Lord S, Links M, Gebski V,
Mok T and Yang JCH: Checkpoint inhibitors in metastatic
EGFR-mutated non-small cell lung cancer-a meta-analysis. J Thorac
Oncol. 12:403–407. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Peters S, Gettinger S, Johnson ML, Jänne
PA, Garassino MC, Christoph D, Toh CK, Rizvi NA, Chaft JE,
Carcereny Costa E, et al: Phase II trial of atezolizumab as
first-line or subsequent therapy for patients with programmed
death-ligand 1-selected advanced non-small-cell lung cancer
(BIRCH). J Clin Oncol. 35:2781–2789. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Garassino MC, Cho BC, Kim JH, Mazières J,
Vansteenkiste J, Lena H, Corral Jaime J, Gray JE, Powderly J,
Chouaid C, et al: Durvalumab as third-line or later treatment for
advanced non-small-cell lung cancer (ATLANTIC): An open-label,
single-arm, phase 2 study. Lancet Oncol. 19:521–536. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Gubens MA, Sequist LV, Stevenson JP,
Powell SF, Villaruz LC, Gadgeel SM, Langer CJ, Patnaik A, Borghaei
H, Jalal SI, et al: Pembrolizumab in combination with ipilimumab as
second-line or later therapy for advanced non-small-cell lung
cancer: KEYNOTE-021 cohorts D and H. Lung Cancer. 130:59–66. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Yang JCH, Shepherd FA, Kim DW, Lee GW, Lee
JS, Chang GC, Lee SS, Wei YF, Lee YG, Laus G, et al: Osimertinib
Plus durvalumab versus osimertinib monotherapy in EGFR
T790M-positive NSCLC following previous EGFR TKI therapy: CAURAL
brief report. J Thorac Oncol. 14:933–939. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Jiang T, Wang P, Zhang J, Zhao Y, Zhou J,
Fan Y, Shu Y, Liu X, Zhang H, He J, et al: Toripalimab plus
chemotherapy as second-line treatment in previously EGFR-TKI
treated patients with EGFR-mutant-advanced NSCLC: A multicenter
phase-II trial. Signal Transduct Target Ther. 6:3552021. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Mok T, Nakagawa K, Park K, Ohe Y, Girard
N, Kim HR, Wu YL, Gainor J, Lee SH, Chiu CH, et al: Nivolumab plus
chemotherapy in epidermal growth factor receptor-mutated metastatic
non-small-cell lung cancer after disease progression on epidermal
growth factor receptor tyrosine kinase inhibitors: Final results of
CheckMate 722. J Clin Oncol. 42:1252–1264. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Yang JCH, Lee DH, Lee JS, Fan Y, de
Marinis F, Iwama E, Inoue T, Rodríguez-Cid J, Zhang L, Yang CT, et
al: Phase III KEYNOTE-789 study of pemetrexed and platinum with or
without pembrolizumab for tyrosine kinase inhibitor-resistant,
EGFR-mutant, metastatic nonsquamous non-small cell lung cancer. J
Clin Oncol. 42:4029–4039. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Socinski MA, Jotte RM, Cappuzzo F, Orlandi
F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D,
Thomas CA, Barlesi F, et al: Atezolizumab for first-line treatment
of metastatic nonsquamous NSCLC. N Engl J Med. 378:2288–2301. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Nogami N, Barlesi F, Socinski MA, Reck M,
Thomas CA, Cappuzzo F, Mok TSK, Finley G, Aerts JG, Orlandi F, et
al: IMpower150 final exploratory analyses for atezolizumab plus
bevacizumab and chemotherapy in key NSCLC patient subgroups with
EGFR mutations or metastases in the liver or brain. J Thorac Oncol.
17:309–323. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Lu S, Wu L, Jian H, Cheng Y, Wang Q, Fang
J, Wang Z, Hu Y, Han L, Sun M, et al: Sintilimab plus chemotherapy
for patients with EGFR-mutated non-squamous non-small-cell lung
cancer with disease progression after EGFR tyrosine-kinase
inhibitor therapy (ORIENT-31): Second interim analysis from a
double-blind, randomised, placebo-controlled, phase 3 trial. Lancet
Respir Med. 11:624–636. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhou C, Dong X, Chen G, Wang Z, Wu X, Yao
Y, Zhang Y, Cheng Y, Pan H, Zhang X, et al: OA09.06 IMpower151:
Phase III Study of Atezolizumab + bevacizumab + chemotherapy in 1L
metastatic nonsquamous NSCLC. J Thorac Oncol. 18 (Suppl):S64–S65.
2023. View Article : Google Scholar
|
|
100
|
Park S, Kim TM, Han JY, Lee GW, Shim BY,
Lee YG, Kim SW, Kim IH, Lee S, Kim YJ, et al: Phase III, randomized
study of atezolizumab plus bevacizumab and chemotherapy in patients
with EGFR- or ALK-mutated non-small-cell lung cancer (ATTLAS,
KCSG-LU19-04). J Clin Oncol. 42:1241–1251. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
HARMONi-A Study Investigators, Fang W,
Zhao Y, Luo Y, Yang R, Huang Y, He Z, Zhao H, Li M, Li K, et al:
Ivonescimab plus chemotherapy in non-small cell lung cancer with
EGFR variant: A randomized clinical trial. JAMA. 332:561–570. 2024.
View Article : Google Scholar
|
|
102
|
Li Z, Fang W, Zhao Y, Luo Y, Yang R, Huang
Y, He Z, Zhao H, Li M, Li K, et al: Ivonescimab combined with
chemotherapy in patients with EGFR-mutant non-squamous non-small
cell lung cancer who progressed on EGFR tyrosine-kinase inhibitor
treatment (HARMONi-A): A randomized, double-blind, multi-center,
phase 3 trial. J Clin Oncol. 42 (16 Suppl):S85082024. View Article : Google Scholar
|
|
103
|
Wu YL, Wang Z, Cheng Y, Fang J, Meng X,
Pan Y, Zhao H, Zhao Y, Su H, Sun M, et al: 1255MO A phase II safety
and efficacy study of PM8002/BNT327 in combination with
chemotherapy in patients with EGFR-mutated non-small cell lung
cancer (NSCLC). Ann Oncol. 35 (Suppl 2):S8042024. View Article : Google Scholar
|
|
104
|
Fang WF, Yang Y, Zhao Y, Huang Y, Zhao H,
Zhou N, Zhang Y, Chen L, Zhou T, Chen G, et al: 646P Iparomlimab
and tuvonralimab (QL1706) plus chemotherapy and bevacizumab for
epidermal growth factor receptor inhibitor (EGFRi)-resistant,
EGFR-mutant, advanced non-small cell lung cancer (NSCLC): Updated
results from Cohort 5 in the DUBHE-L-201 study. Ann Oncol. 35
(Suppl 4):S16462024. View Article : Google Scholar
|
|
105
|
Brown H, Vansteenkiste J, Nakagawa K, Cobo
M, John T, Barker C, Kohlmann A, Todd A, Saggese M, Chmielecki J,
et al: Programmed cell death ligand 1 expression in untreated EGFR
mutated advanced NSCLC and response to osimertinib versus
comparator in FLAURA. J Thorac Oncol. 15:138–143. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Lin C, Chen X, Li M, Liu J, Qi X, Yang W,
Zhang H, Cai Z, Dai Y and Ouyang X: Programmed death-ligand 1
expression predicts tyrosine kinase inhibitor response and better
prognosis in a cohort of patients with epidermal growth factor
receptor mutation-positive lung adenocarcinoma. Clin Lung Cancer.
16:e25–e35. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Soo RA, Kim HR, Asuncion BR, Fazreen Z,
Omar MFM, Herrera MC, Yun Lim JS, Sia G, Soong R and Cho BC:
Significance of immune checkpoint proteins in EGFR-mutant non-small
cell lung cancer. Lung Cancer. 105:17–22. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Yoneshima Y, Ijichi K, Anai S, Ota K,
Otsubo K, Iwama E, Tanaka K, Oda Y, Nakanishi Y and Okamoto I:
PD-L1 expression in lung adenocarcinoma harboring EGFR mutations or
ALK rearrangements. Lung Cancer. 118:36–40. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Su S, Dong ZY, Xie Z, Yan LX, Li YF, Su J,
Liu SY, Yin K, Chen RL, Huang SM, et al: Strong programmed death
ligand 1 expression predicts poor response and de novo resistance
to EGFR tyrosine kinase inhibitors among NSCLC patients with EGFR
mutation. J Thorac Oncol. 13:1668–1675. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Hsu KH, Huang YH, Tseng JS, Chen KC, Ku
WH, Su KY, Chen JJW, Chen HW, Yu SL, Yang TY and Chang GC: High
PD-L1 expression correlates with primary resistance to EGFR-TKIs in
treatment naïve advanced EGFR-mutant lung adenocarcinoma patients.
Lung Cancer. 127:37–43. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Sakata Y, Sakata S, Oya Y, Tamiya M,
Suzuki H, Shibaki R, Okada A, Kobe H, Matsumoto H, Yokoi T, et al:
Osimertinib as first-line treatment for advanced epidermal growth
factor receptor mutation-positive non-small-cell lung cancer in a
real-world setting (OSI-FACT). Eur J Cancer. 159:144–153. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Alves Pinto I, de Oliveira Cavagna R,
Virginio da Silva AL, Dias JM, Santana IV, Souza LC, Ferreira da
Silva FA, Biazotto Fernandes MF, Junqueira Pinto GD, Negreiros IS,
et al: EGFR mutations and PD-L1 expression in early-stage non-small
cell lung cancer: A real-world data from a single center in Brazil.
Oncologist. 27:e899–e907. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Papazyan T, Denis MG, Sagan C, Raimbourg
J, Herbreteau G and Pons-Tostivint E: Impact of PD-L1 expression on
the overall survival of caucasian patients with advanced
EGFR-mutant NSCLC treated with frontline osimertinib. Target Oncol.
19:611–621. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Lakkunarajah S, Truong PT, Bone JN,
Hughesman C, Yip S, Alex D, Hart J, Pollock P, Egli S, Clarkson M,
et al: First-line osimertinib for patients with EGFR-mutated
advanced non-small cell lung cancer: efficacy and safety during the
COVID-19 pandemic. Transl Lung Cancer Res. 12:1454–1465. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Yoshimura A, Yamada T, Okuma Y, Fukuda A,
Watanabe S, Nishioka N, Takeda T, Chihara Y, Takemoto S, Harada T,
et al: Impact of tumor programmed death ligand-1 expression on
osimertinib efficacy in untreated EGFR-mutated advanced non-small
cell lung cancer: A prospective observational study. Transl Lung
Cancer Res. 10:3582–3593. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Hsu KH, Tseng JS, Yang TY, Chen KC, Su KY,
Yu SL, Chen JJW, Huang YH and Chang GC: PD-L1 strong expressions
affect the clinical outcomes of osimertinib in treatment naïve
advanced EGFR-mutant non-small cell lung cancer patients. Sci Rep.
12:97532022. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Hamakawa Y, Agemi Y, Shiba A, Ikeda T,
Higashi Y, Aga M, Miyazaki K, Taniguchi Y, Misumi Y, Nakamura Y, et
al: Association of PD-L1 tumor proportion score ≥20% with early
resistance to osimertinib in patients with EGFR-mutated NSCLC.
Cancer Med. 12:17788–17797. 2023. View Article : Google Scholar : PubMed/NCBI
|