Introduction
The incidence of colorectal cancer (CRC) throughout
Japan has been increasing, rendering colonoscopy a useful tool for
the diagnosis, treatment and screening of CRC. Although the annual
2-day fecal immunochemical test (FIT) is commonly used in
population-based CRC screening programs in Japan, total colonoscopy
(TCS) has recently been applied in situations, such as CRC
screening during medical check-up examinations. Furthermore,
colonoscopy and polypectomy have effectively reduced the incidence
of CRC (1-3).
The rate of TCS and insertion time are important
markers for progress being made in colonoscope training. However,
the TCS technique is difficult, and mastering this technique
requires considerable time, effort and practice (that is, a large
number of cases are required) (4-7).
Delayed or failed cecal intubation can have unfavorable results,
such as patient discomfort, complications and consecutive cecal
re-insertion failure. Various factors have been implicated in the
performance of trainees and success in performing colonoscopy. One
of the issues is that trainees tend to experience difficulty in
detecting the next lumen. Experts in colonoscopy can be judged by
the manner in which they insert the colonoscope into the oral side
without any complications by experience.
Cap-assisted colonoscopy (CAC) is a useful modality
for detecting lesions. In fact, CAC was developed to improve polyp
and adenoma detection (8-16).
CAC is particularly useful as the cap can depress the semilunar
folds, allowing the endoscopist to inspect the blind mucosal area.
The wavy cap is shorter than the conventional cap, and this
characteristic provides the wavy cap with the advantage of not
causing an eclipse on the endoscopy screen during magnified
observation. In addition, the wavy cap is designed to be
advantageous for flipping folds at the tip of the endoscope during
insertion. It is considered that a wavy cap (MAJ-Y0024-2; Olympus
Corporation) may help trainees to rapidly and promptly acquire the
TCS technique. The aim of the present study was to compare the
efficacy of colonoscopy using a wavy cap compared with colonoscopy
without a cap based on the TCS rate and insertion time achieved by
the trainee.
Materials and methods
Study population
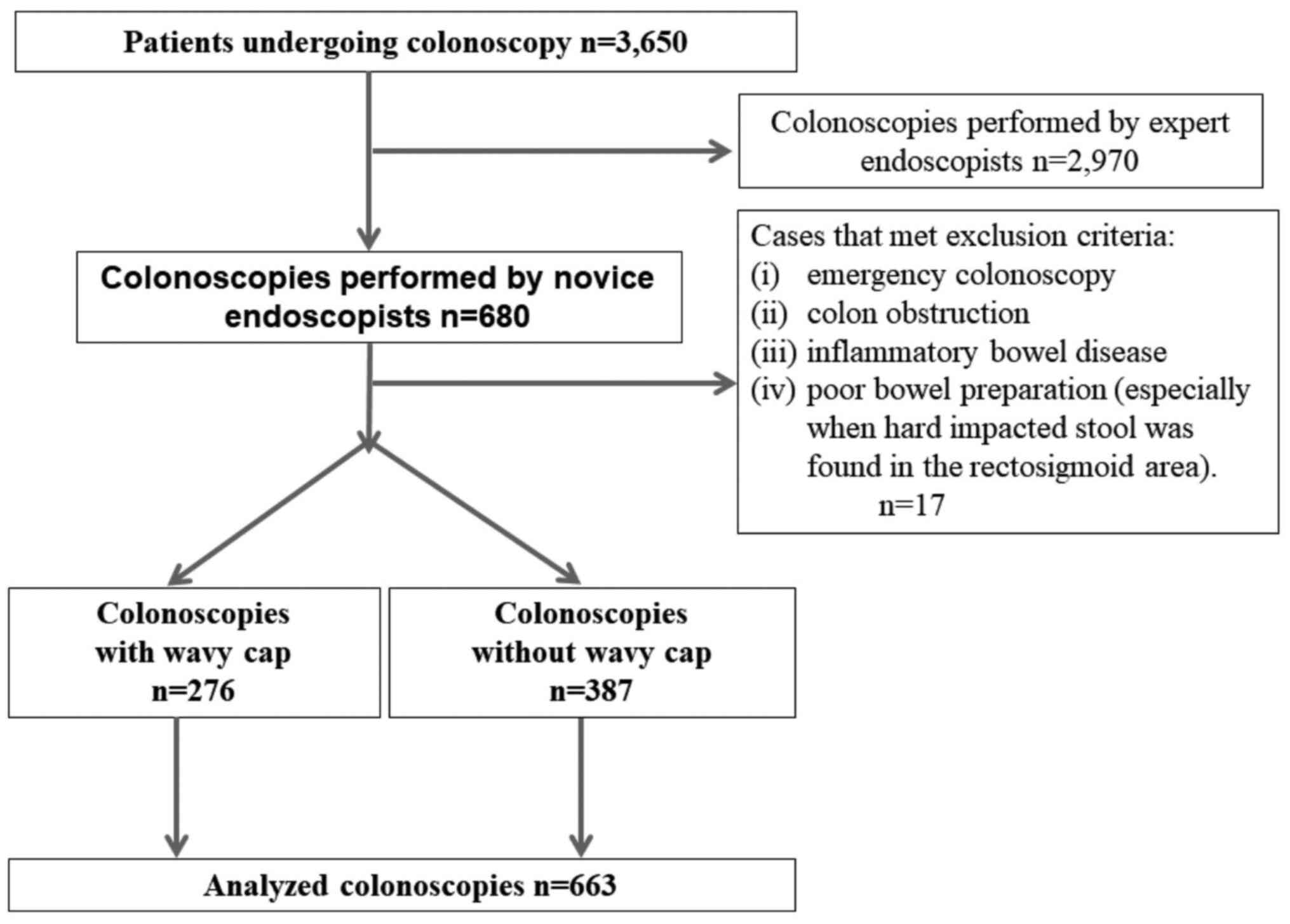
This comparative prospective trial was conducted
between May and October, 2011. When the 5 novice endoscopists (who
had each performed <10 colonoscopies) began working in routine
clinical practice at Showa University Northern Yokohama Hospital in
May, 2011, they were randomly allocated to either the cap group (Dr
Yui Jennyfer Oka, Dr Tatsuya Sakurai and Dr Tetsuya Yoshizaki) or
the non-cap groups (Dr Yu-ta Koyama and Dr Shinichi Kataoka). The
study flowchart is presented in Fig.
1. A total of 3,650 patients underwent colonoscopy at Showa
University Northern Yokohama Hospital between May and October,
2011. The 5 novice endoscopists performed 680 of these
colonoscopies (without any arbitrary patient selection). Among
these 680 patients, those with the following criteria were
excluded: i) emergency colonoscopy; ii) colon obstruction; iii)
inflammatory bowel disease; and iv) poor bowel preparation
(particularly when hard impacted stool was found in the
rectosigmoid area). Hence, 667 colonoscopies were eligible for
inclusion as follows: A total of 276 colonoscopies performed by the
cap group, and 387 performed by the non-cap group. The study
protocol was approved by the Ethics Committee at Showa University
Northern Yokohama Hospital (no. 1105-03). The study was registered
at ClinicalTrials.gov under the identifier
NCT01400087, and it was conducted in accordance with the
Declaration of Helsinki. All patients provided written informed
consent prior to participation in the study. Part of the present
study was presented at the Digestive Disease Week 2016, San Diego,
CA, USA, May 1, 2016 (poster presentation).
Training program and study design
This colonoscopy training program was conducted only
with the condition that patients did not suffer any discomfort.
Initially, the trainees practiced the endoscopic techniques for
upper endoscopy and colonoscopy using the ‘Colonoscopy training
model’ (KY11361-000, Olympus Corporation), with the goal of
performing cecal intubation within 15 min. Once the trainees had
achieved this goal, they spent 2 weeks observing experienced
endoscopists perform colonoscopies. The experienced endoscopists
instructed the trainees on the use of a colonoscope insertion
method named the ‘3S technique’: Straight insertion, slide
laterally, shortening. First, the colonoscope is straightened.
Second, the endoscopist then slides the colonoscope to pass the
fold. Third, the colon is shortened by pulling back the
colonoscope. The senior endoscopists allowed the trainees to
perform the colonoscopy procedure after ensuring that the
procedures could be performed under safe and comfortable conditions
for the patients. However, the senior endoscopists intervened
during the procedure in the following cases: i) if the trainee
could not reach the cecum within 15 min; ii) if the patients asked
for the procedure to be performed by senior endoscopists; or iii)
the trainee felt uncomfortable about performing the procedure.
Cecal intubation was documented by photographing the identified
cecal landmarks, such as the appendiceal orifice and the ileocecal
valve. Patient age, sex, body mass index (BMI) and surgical history
were recorded prior to the procedure. The trainee began the
insertion after bowel preparation was completed, and the cecal
intubation time was recorded. Following cecal intubation, the
trainee and the senior endoscopists carefully examined the colon
during the withdrawal of the colonoscope; biopsies and/or treatment
were performed as needed.
All patients underwent initial TCS using a
magnifying video colonoscope (CF-H260AZI; Olympus Corporation). The
cap group used a wavy cap (MAJ-Y0024-2; Olympus Corporation;
Fig. 2) on the tip of the
colonoscopes during every colonoscopy. Moderate sedation was
induced with a combination of intravenous diazepam or midazolam and
meperidine in almost all the patients, apart from those who refused
sedation. The quality of the colonoscopies was monitored during the
6-month training period. The TCS rate by novice endoscopists,
insertion time and learning curve were evaluated for each group.
The trainee learning curves were calculated in consecutive blocks
of 20 procedures. The primary endpoint was the comparison of the
cecum arrival rate between the cap and non-cap groups after 6
months of colonoscopic training.
Sample size calculation
The sample size was calculated using the Chi-squared
test based on previous results indicating that after 3 months, the
cecal arrival rate was significantly higher in the cap group than
that in the non-cap group. At Showa University Northern Yokohama
Hospital the cecal arrival rate in the non-cap group (trainees
without TCS experience who received TCS training for 3 years) in a
3-month period was approximately 13.5%. In a previous study, the
insertion rate increased by 1.6% when comparing the non-cap group
with the cap group (9). In the
present study, it was estimated that the insertion rate would be
10%, considering that the trainees had performed under 100 cases of
TCS. Assuming an insertion rate of 23.5% for the cap group and
13.5% for the non-cap group, the sample size was calculated. All
tests were two-sided with an alpha level of 0.05 and a power of
0.80. Subsequently, 235 patients were enrolled in each group,
considering a potential dropout of cases of approximately 10%,
yielding a target sample size of 500 patients in total.
Statistical analyses
All statistical analyses were performed using SPSS
version 19.0 software (SPSS, Inc.) and BellCurve for Excel (Social
Survey Research Information Co., Ltd.). All continuous variables
are expressed as the means ± standard deviation (SD). Continuous
variables of clinical features of enrolled patients and cecal
intubation time were analyzed using the Student's t-test.
Categorical data of clinical features of enrolled patients and rate
in total cases were assessed with the Chi-squared test. In
analyzing the intubation time and the success rate in the
consecutive blocks of 20 procedures, a two-way repeated measures
analysis of variance (ANOVA) was used followed by the Bonferroni
multiple comparison test. A P-value <0.05 was considered to
indicate a statistically significant difference.
Results
Baseline demographic and clinical data
of patients
Between May and October, 2011, 680 consecutive
patients were prospectively enrolled who were scheduled to undergo
colonoscopy at Showa University Northern Yokohama Hospital. A total
of 5 trainee doctors were randomly allocated to 2 groups as
follows: the cap group (2 doctors) and the non-cap group (3
doctors). In total, 276 colonoscopy cases were performed with cap
and 387 cases without cap. A total of 17 cases were excluded due to
the following reasons: Bowel stenosis with colon cancer (n=2),
ischemic colitis (n=3) and change to another scope (thin scope or
long scope) (n=12). The mean (SD) age of the patients was 62.5
(13.7) years, and the mean BMI was 22.7 (3.3) kg/m2. Of the
included subjects, 420 were males (63.3%) and 243 were women
(36.7%). There were 318 patients (48.0%) without a history of
surgery, and 18.1% had a history of colorectal surgery.
Additionally, 18.6% of the patients suffered from constipation.
There were no significant differences in background demographic and
clinical characteristics of the patients between the cap and
non-cap groups. The demographic data are summarized in Table I.
 | Table IDemographics and clinical features of
the enrolled patients. |
Table I
Demographics and clinical features of
the enrolled patients.
| | | | | |
|---|
| Characteristics | Total no. of
patients, n=663 | Cap group, n=276 | Non-cap group,
n=387 | P-value |
| Sex (male), n
(%) | 420 (63.3) | 166 (60.1) | 254 (65.6) | >0.05a |
| Age, years, mean
(SD) | 62.5 (13.7) | 63.1 (13.5) | 62.1 (13.9) | >0.05b |
| BMI,
kg/m2, mean (SD) | 22.7 (3.3) | 22.7 (3.3) | 22.6 (3.4) | >0.05a |
| Previous surgery, n
(%) | 345 (52.0) | 146 (52.9) | 199 (51.4) | >0.05a |
| Colorectal surgery, n
(%) | 120 (18.1) | 47 (17.0) | 73 (18.9) | >0.05a |
| Others, n (%) | 225 (33.9) | 99 (35.9) | 126 (32.6) | >0.05a |
| Constipation, n
(%) | 123 (18.6) | 53 (19.2) | 70 (18.1) | >0.05a |
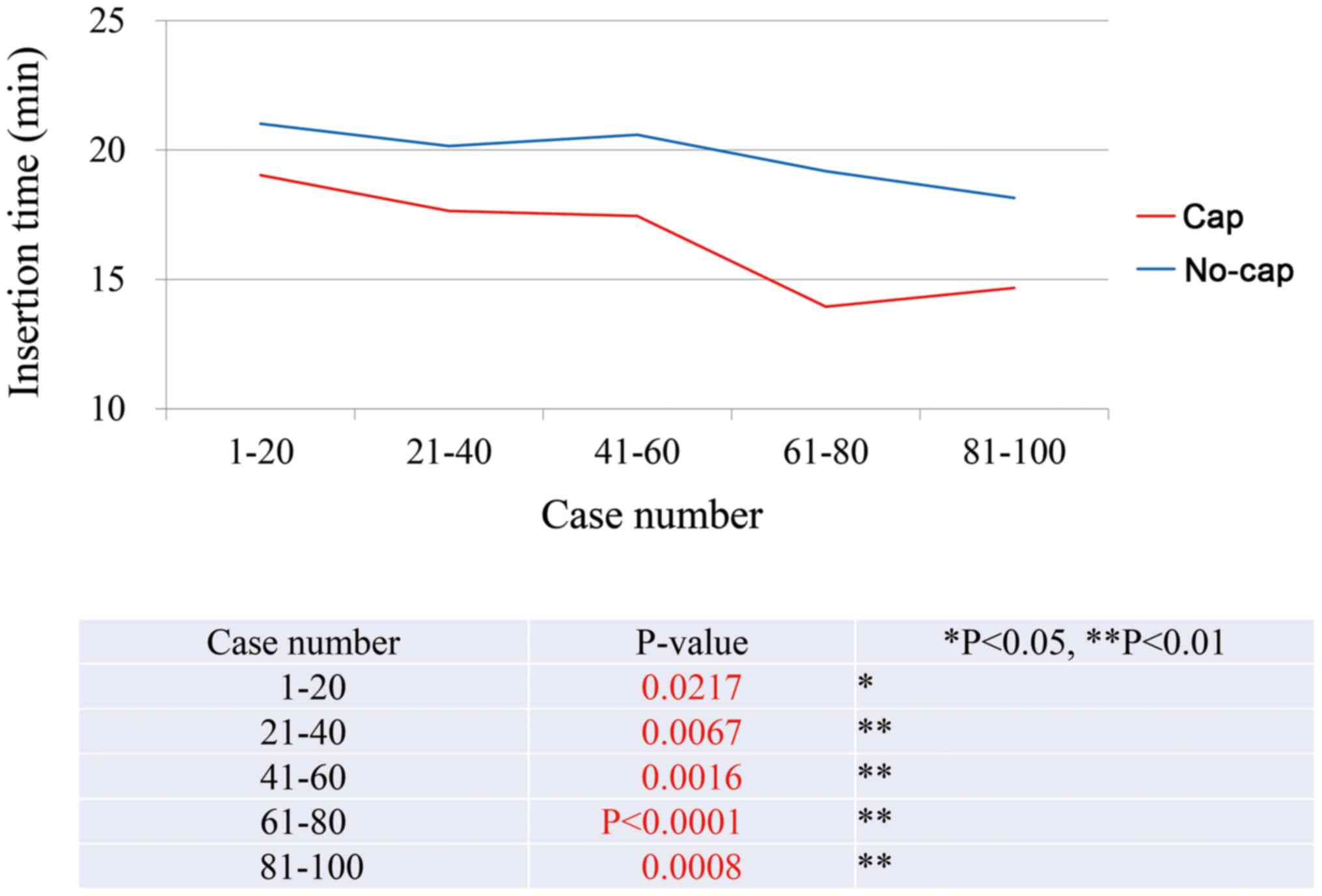
Cecal intubation time
The mean (SD) cecal intubation time (time to reach
the cecum with the colonoscope) was 15.7 (6.8) min in the cap group
and 19.11 (7.6) min in the non-cap group (P<0.001) (Table II). The expert endoscopist
assisted in all cases in which the novice endoscopists could not
perform TCS within 15 min. The skill of the trainee in performing
cecal intubation in <15 min improved rapidly and significantly
within all blocks. Based on the learning curve of the cecal
intubation time, the cap group exhibited a significantly faster
than the non-cap group in all blocks (Table III and Fig. 3).
 | Table IICecal intubation time and rate in
total cases. |
Table II
Cecal intubation time and rate in
total cases.
| Time or rate | Cap | Non-cap | P-value |
|---|
| Insertion time,
min | 15.7 (6.8) | 19.11 (7.6) |
<0.001a |
| Cecal insertion rate
(%) | 41.7 | 33.8 | 0.036b |
 | Table IIICecal intubation time in each 20
cases. |
Table III
Cecal intubation time in each 20
cases.
| Case number (groups
of 20 procedures) | Cap
(min)a | Non-cap
(min)a | P-valueb |
|---|
| 1-20 | 19.0±1.0 | 21.0±0.8 | 0.02 |
| 21-40 | 17.7±0.1 | 20.2±0.4 | <0.01 |
| 41-60 | 17.5±1.4 | 20.6±2.5 | <0.01 |
| 61-80 | 14.0±1.6 | 19.2±3.7 | <0.01 |
| 81-100 | 14.7±0.7 | 18.2±1.0 | <0.01 |
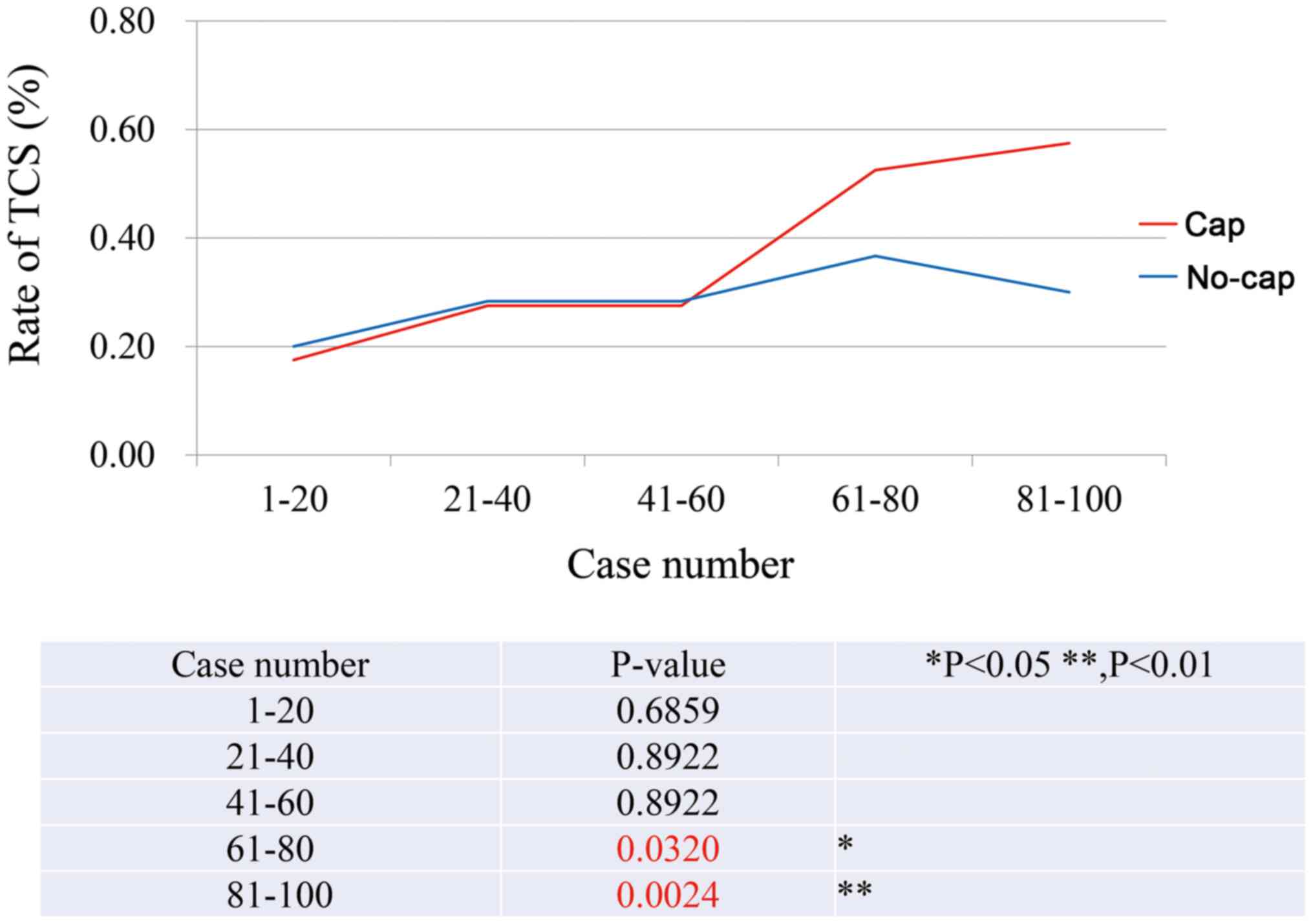
Cecal insertion rate
Cecal intubation was achieved in all cases by the
trainee and senior endoscopists. The success rate of cecal
intubation by the trainees was 115/276 (41.7%) in the cap group and
131/387 (33.8%) in the non-cap group (P=0.036) (Table II). After 60 procedures, the cap
group exhibited a significantly steeper learning curve than the
non-cap group (Table IV and
Fig. 4). During this program, no
complications were encountered in either treatment group.
 | Table IVCecal intubation rate in each 20
cases. |
Table IV
Cecal intubation rate in each 20
cases.
| Case number (groups
of 20 procedures) | Cap (%) | Non-cap (%) |
P-valuea |
|---|
| 1-20 | 17.5 | 20.0 | 0.69 |
| 21-40 | 27.5 | 28.3 | 0.89 |
| 41-60 | 27.5 | 28.3 | 0.89 |
| 61-80 | 52.5 | 36.7 | 0.03 |
| 81-100 | 57.5 | 30.0 | <0.01 |
Discussion
The incidence of CRC worldwide has been increasing,
rendering colonoscopy a useful tool for the diagnosis, treatment,
and screening of CRC. Additionally, colonoscopy with polypectomy is
one of the most effective procedures for preventing CRC.
Reportedly, colonoscopy with polypectomy has effectively reduced
the incidence of CRC (2,3). However, the technique of TCS is
difficult and doctors need to perform numerous procedures to
acquire expertise and proficiency in this technique. Even for
experts, it is not always possible to reach the cecum (17). The TCS technique is evaluated by 2
important parameters: insertion time and TCS rate.
A short cecal intubation time is important for
several reasons: Less anesthetic medication is required, colonic
inflation tends to result in less discomfort, and it allows
sufficient withdrawal time for accurate colon examination. TCS
requires extremely low air insufflations. Experts can advance a
colonoscope by pushing and pulling using meticulous lever
manipulation without air insufflation, especially in the rectum and
sigmoid colon. This ability can prevent the mucosa from touching
the lens directly and enables continuous lumen observation with low
air. One potentially promising technique is CAC. A transparent cap
(or hood), a simple plastic device, can be attached to the tip of a
colonoscope before performing the colonoscopy. Several randomized
trials (8-12)
conducted in Japan have reported mixed results regarding improved
cecal intubation times and polyp detection rates when using the
cap. Transparent caps attached to the distal tip of the colonoscope
were first designed to assist during endoscopic mucosal resection.
However, it has also been suggested that such caps are helpful for
depressing colonic folds, and thus, improve the visualization of
their proximal aspects. CAC can be easily implemented by simply
attaching a transparent rubber cap to the tip of the colonoscope,
and its use has been associated with a decrease in the cecal
intubation time, without increasing the cost of the procedure
(9,12-17).
Additionally, the cap allows for an appropriate
distance between the colonic mucosa and the lens of the
colonoscope. Additionally, the cap can be used to stretch or splay
the colonic mucosa, further contributing to improved detection
rates (9,18,19).
Previous studies have demonstrated that CAC is more effective than
non-CAC for the detection of colorectal polyps and adenomas,
particularly in difficult cases, those in which the procedure is
performed by trainees, and cases in which the lesions are located
in the right-side colon (17,18).
The endoscopic cap also reportedly improves the adenoma detection
rate, visualization of the ampulla of Vater and sclerotherapy for
hemorrhoids (22,23). A previous study demonstrated that
CAC may be of benefit in terms of cecal intubation time and
insertion rate. In the present study, the learning curve revealed
that the insertion rate increased significantly at approximately 60
procedures. It is considered that these number of cases were
necessary, as the endoscopists in the present study had minimal
previous experience in performing endoscopies. The rate of cecal
intubation did not differ significantly between the 2 groups during
the first 60 cases, whereas the usefulness of the wavy cap for
cecal intubation appeared when the number exceeded 60 cases.
Although there may be other causes, it was considered that this was
probably as the novice endoscopists were not accustomed to
endoscopic manipulation itself in the first 60 cases. Additionally,
at Showa University Northern Yokohama Hospital., it is a rule that
the endoscope should never be pushed until entering the descending
colon. As the endoscopic insertion technique itself is an advanced
technique, doctors are obligated to receive technical lectures and
practice on colon models prior to performing the procedures on
patients.
In the present study, other factors were considered
to increase the difficulty of some procedures. Several studies have
described the progress of trainees and have indicated that factors,
such as abdominal surgery history, BMI, sex and age of patients can
increase the difficulty of insertion (24-27).
In fact, it is not easy to examine and select patients for this
procedure. In the present study, patients with characteristics that
could lead to a technically difficult colonoscopy were enrolled;
thus, it was considered that this is the reason for the fact that
the learning curve of the present study was lower than that in a
previous study that had excluded such patients (6,21).
The wavy cap is shorter than the conventional cap;
however, its shape does not cause the loss of the endoscopic image.
Therefore, the wavy cap does not present an obstacle during
observation, which enables observation with a magnifying endoscopy
as clearly as when without the cap. In the present study, the cap
proved to be useful when trainees were in the process of mastering
the technique of magnified endoscopy. The present study did not
compare the performance of TCS with a wavy cap vs. conventional
caps. However, a previous study reported no differences in
insertion rate and time between CAC and cuff-assisted colonoscopy
(28).
The present study has several limitations. First, it
was a single-center study. Second, only 5 of the trainees underwent
colonoscopy training, and there were only approximately 100 cases
assigned to each trainee. Third, this was not a randomized case
study. Fourth, the present study could not compare the performance
of the wavy cap in polyp detection and cecal intubation compared
with the conventional cap, as Showa University Northern Yokohama
Hospital. does not use the conventional cap. Finally, 18.1% of the
patients had a history of colorectal surgery. The degree of
difficulty of the colonoscopy may vary depending on the location of
the previous surgery. However, it was considered that the patients
included in the present study were examined by trainees in a manner
that resembled actual clinical practice.
In conclusion, the results of the current
prospective trial suggest that a wavy cap on the tip of the
colonoscope is useful for increasing the cecal intubation rate,
decreases the insertion time, and allows for a steep learning curve
for novice endoscopists.
Acknowledgements
The authors would like to thank Dr Chiaki Nishimura
from CN Medical Research for providing advice regarding the
statistical analysis, and Dr Nobunao Ikehara for providing
beneficial suggestions. Part of the present study was presented at
the Digestive Disease Week 2016, San Diego, CA, USA, May 1, 2016
(poster presentation).
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article or are available from the
corresponding author on reasonable request.
Authors' contributions
NT was involved in the study conception and design,
acquisition of data, analysis and interpretation of data,
statistical analysis, and in the drafting of the manuscript. SEK
was involved in study supervision, the conception and design of the
study, provided critical revision and gave the final approval of
the manuscript. YM was involved in the study conception and design,
acquisition of data, and in the analysis and interpretation of
data. MK was involved in the study conception and design and
acquisition of data. TS and YK collected data, and provided and
cared for patients in the study. MM was involved in the analysis
and interpretation of the data, and in the critical revision of the
article for important intellectual content. TK, TH and KW collected
data, and provided and cared for patients in the study. HM was
involved in study supervision, auditing, collection of data, and
provided and cared for the patients in the study. TB and FI were
involved in study supervision, data collection and auditing. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee at Showa University Northern Yokohama Hospital (no.
1105-03). The study was registered at ClinicalTrials.gov under the identifier NCT01400087,
and it was conducted in accordance with the Declaration of
Helsinki. All patients provided written informed consent prior to
participation in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Winawer SJ, Zauber AG, Ho MN, O'Brien MJ,
Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF,
et al: The National Polyp Study Workgroup: Prevention of colorectal
cancer by colonoscopic polypectomy. N Engl J Med. 329:1977–1981.
1993.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Citarda F, Tomaselli G, Capocaccia R,
Barcherini S and Crespi M: Italian Multicentre Study Group.
Efficacy in standard clinical practice of colonoscopic polypectomy
in reducing colorectal cancer incidence. Gut. 48:812–815.
2001.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zauber AG, Winawer SJ, O'Brien MJ,
Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH,
Schapiro M, Panish JF, et al: Colonoscopic polypectomy and
long-term prevention of colorectal-cancer deaths. N Engl J Med.
366:687–696. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Dafnis G, Granath F, Påhlman L, Hannuksela
H, Ekbom A and Blomqvist P: The impact of endoscopists' experience
and learning curves and interendoscopist variation on colonoscopy
completion rates. Endoscopy. 33:511–517. 2001.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lee SH, Chung IK, Kim SJ, Kim JO, Ko BM,
Hwangbo Y, Kim WH, Park DH, Lee SK, Park CH, et al: An adequate
level of training for technical competence in screening and
diagnostic colonoscopy: A prospective multicenter evaluation of the
learning curve. Gastrointest Endosc. 67:683–689. 2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Chung JI, Kim N, Um MS, Kang KP, Lee D, Na
JC, Lee ES, Chung YM, Won JY, Lee KH, et al: Learning curves for
colonoscopy: A prospective evaluation of gastroenterology fellows
at a single center. Gut Liver. 4:31–35. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Spier BJ, Benson M, Pfau PR, Nelligan G,
Lucey MR and Gaumnitz EA: Colonoscopy training in gastroenterology
fellowships: Determining competence. Gastrointest Endosc.
71:319–324. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Matsushita M, Hajiro K, Okazaki K,
Takakuwa H and Tominaga M: Efficacy of total colonoscopy with a
transparent cap in comparison with colonoscopy without the cap.
Endoscopy. 30:444–447. 1998.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kondo S, Yamaji Y, Watabe H, Yamada A,
Sugimoto T, Ohta M, Ogura K, Okamoto M, Yoshida H, Kawabe T, et al:
A randomized controlled trial evaluating the usefulness of a
transparent hood attached to the tip of the colonoscope. Am J
Gastroenterol. 102:75–81. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Horiuchi A and Nakayama Y: Improved
colorectal adenoma detection with a transparent retractable
extension device. Am J Gastroenterol. 103:341–345. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Shida T, Katsuura Y, Teramoto O, Kaiho M,
Takano S, Yoshidome H and Miyazaki M: Transparent hood attached to
the colonoscope: Does it really work for all types of colonoscopes?
Surg Endosc. 22:2654–2658. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Harada Y, Hirasawa D, Fujita N, Noda Y,
Kobayashi G, Ishida K, Yonechi M, Ito K, Suzuki T, Sugawara T, et
al: Impact of a transparent hood on the performance of total
colonoscopy: A randomized controlled trial. Gastrointest Endosc.
69:637–644. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lee YT, Lai LH, Hui AJ, Wong VW, Ching JY,
Wong GL, Wu JC, Chan HL, Leung WK, Lau JY, et al: Efficacy of
cap-assisted colonoscopy in comparison with regular colonoscopy: A
randomized controlled trial. Am J Gastroenterol. 104:41–46.
2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rastogi A, Bansal A, Rao DS, Gupta N, Wani
SB, Shipe T, Gaddam S, Singh V and Sharma P: Higher adenoma
detection rates with cap-assisted colonoscopy: A randomised
controlled trial. Gut. 61:402–408. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Desai M, Sanchez-Yague A, Choudhary A,
Pervez A, Gupta N, Vennalaganti P, Vennelaganti S, Fugazza A,
Repici A, Hassan C and Sharma P: Impact of cap-assisted colonoscopy
on detection of proximal colon adenomas: systematic review and
meta-analysis. Gastrointest Endosc. 86:274–281. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kim SY, Park HJ, Kim H-S, Park DI, Cha JM,
Park SJ, Choi H, Shin JE, Eun CS, Kim JO, et al: Cap-assisted
chromoendoscopy using a mounted cap versus standard colonoscopy for
adenoma detection. Am J Gastroenterol. 115:465–472. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
de Wijkerslooth TR, Stoop EM, Bossuyt PM,
Mathus-Vliegen EM, Dees J, Tytgat KM, van Leerdam ME, Fockens P,
Kuipers EJ and Dekker E: Adenoma detection with cap-assisted
colonoscopy versus regular colonoscopy: A randomised controlled
trial. Gut. 61:1426–1434. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hewett DG and Rex DK: Cap-fitted
colonoscopy: A randomized, tandem colonoscopy study of adenoma miss
rates. Gastrointest Endosc. 72:775–781. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ng SC, Tsoi KK, Hirai HW, Lee YT, Wu JC,
Sung JJ, Chan FK and Lau JY: The efficacy of cap-assisted
colonoscopy in polyp detection and cecal intubation: A
meta-analysis of randomized controlled trials. Am J Gastroenterol.
107:1165–1173. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim HH, Park SJ, Park MI, Moon W and Kim
SE: Transparent-cap-fitted colonoscopy shows higher performance
with cecal intubation time in difficult cases. World J
Gastroenterol. 18:1953–1958. 2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kim DJ, Kim HW, Park SB, Kang DH, Choi CW,
Hong JB, Ji BH and Lee CS: Efficacy of cap-assisted colonoscopy
according to lesion location and endoscopist training level. World
J Gastroenterol. 21:6261–6270. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhang T, Xu LJ, Xiang J, He Z, Peng ZY,
Huang GM, Ji GZ and Zhang FM: Cap-assisted endoscopic sclerotherapy
for hemorrhoids: Methods, feasibility and efficacy. World J
Gastrointest Endosc. 7:1334–1340. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Silva LC, Arruda RM, Botelho PFR, Taveira
LN, Giardina KM, de Oliveira MA, Dias J, Oliveira CZ, Fava G and
Guimarães DP: Cap-assisted endoscopy increases ampulla of Vater
visualization in high-risk patients. BMC Gastroenterol.
20(214)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Oh SY, Sohn CI, Sung IK, Park DI, Kang MS,
Yoo TW, Park JH, Kim HJ, Cho YK, Jeon WK, et al: Factors affecting
the technical difficulty of colonoscopy. Hepatogastroenterology.
54:1403–1406. 2007.PubMed/NCBI
|
|
25
|
Shah HA, Paszat LF, Saskin R, Stukel TA
and Rabeneck L: Factors associated with incomplete colonoscopy: A
population-based study. Gastroenterology. 132:2297–2303.
2007.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bernstein C, Thorn M, Monsees K, Spell R
and O'Connor JB: A prospective study of factors that determine
cecal intubation time at colonoscopy. Gastrointest Endosc.
61:72–75. 2005.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Anderson JC, Messina CR, Cohn W, Gottfried
E, Ingber S, Bernstein G, Coman E and Polito J: Factors predictive
of difficult colonoscopy. Gastrointest Endosc. 54:558–562.
2001.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Sola-Vera J, Catalá L, Uceda F, Picó MD,
Pérez Rabasco E, Sáez J, Jiménez N, Arjona MD, Fernández M, Girona
E, et al: Cuff-assisted versus cap-assisted colonoscopy for adenoma
detection: Results of a randomized study. Endoscopy. 51:742–749.
2019.PubMed/NCBI View Article : Google Scholar
|