Introduction
The morbidity and mortality associated with gastric cancer ranks second among the types of cancer in China (1). Surgical resection remains the gold standard treatment for gastric cancer. In order to prolong the survival of patients with gastric cancer as much as possible, an increasing number of researchers emphasize the importance of radical surgery. However, post-operative complications always occur due to dissection and tract reconstruction. The rate of post-operative complications remains unsatisfactory, varying from 18.3 to 36% (2). Although the majority of complications can are treatable, it remains unknown whether the long-term survival of patients is affected and what type of complications affect prognosis. These are important issues that surgeons need to understand and take into consideration.
The Clavien-Dindo classification system is a widely used clinical approach (3-5). The grading of complications facilitates a more objective evaluation of the severity of the complications. The advantages of the Clavien-Dindo classification system include simplicity, an understandable format, acceptability and reproducibility. However, this standard is only suitable for the classification of general adverse events. Surgical-related complications often lack a clear definition and a set of diagnostic principles.
In 2015, the Japan Clinical Oncology Group (JCOG) established a special committee to revise the Clavien-Dindo standard and to provide a more precise evaluation of surgery-related complications known as the modified version of the Clavien-Dindo classification system (6). The classification of the surgical complications was clearly defined, allowing for a more unified standard suitable for the evaluation of early post-operative complications. For example, the placement of a gastric tube and a small intestinal decompression tube following intestinal obstruction post-surgery are considered grade II and III complications, respectively, and the replacement of the drainage tube following leakage or an abscess is listed as a grade III complication (6).
In fact, the difference between the modified Clavien-Dindo classification and the general Clavien-Dindo Classification is mainly reflected in the definition of complications. The surgical common adverse event terms and gradings according to the modified Clavien-Dindo classification are presented in Table I (including post-operative hemorrhage, intestinal fistula and intestinal obstruction). It should be noted that only the most common events are listed due to space limitations (6).
 |
Table I
List of surgical common adverse event terms and gradings according to the modified Clavien-Dindo classification.
|
Table I
List of surgical common adverse event terms and gradings according to the modified Clavien-Dindo classification.
| |
Principle of grading |
|
| Adverse explanation |
I |
II |
IIIa |
IIIb |
IVa |
IVb |
V |
Supplemental event of suffix ‘d’a |
| Post- operative hemorrhage |
Controllable with compression only |
Blood transfusion or medical management agreement indicated |
Surgical hemostasis under local anesthesia or endoscopic and radiological intervention hemostasis indicated |
Intervention under general anesthesia indicated (hemostasis) |
Single organ failure; stepdown ICU/ICU care indicated |
Multiple organ failure; IC/ICU management indicated |
Mortality |
Persistent anemia |
| Intestinal fistula |
Clinical observation or diagnostic evaluation only; intervention not indicated (drainage only through existing drain age tube) |
Medical management indicated (e.g., antibiotics) |
Image-guided drain placement/paracentesis, including drain replacement indicated |
Intervention under general anesthesia indicated (colostomy) |
At least one organ failure |
Sepsis or multiple organ failure |
Mortality |
Persistent enterocutaneous fistula |
| Intestinal obstruction |
Clinical observation or diagnostic evaluation only; medical management not indicated except for laxatives and intravenous nutrition |
Medical management beyond laxatives, NG tube placement, or intravenous nutrition management indicated |
Nasoenteric tube placement |
Treatment for ileus under general anesthesia (with or without intestinal resection) |
Extensive intestinal necrosis, at least one organ failure |
Sepsis or multiple organ failure |
Mortality |
Home intravenous nutrition |
The present study used the modified Clavien-Dindo classification system to identify the incidence of early complications and analyze risk factors for early complications following RG in patients with gastric cancer. To further benefit patients with gastric cancer, the association between complications and prognosis was further evaluated.
Patients and methods
Patients
The present study was a retrospective investigation of 525 consecutive patients who underwent RG for gastric cancer between October, 2010 and September, 2015 at the Anqing Municipal Hospital (Anqing, China). The present study was approved by the Medical Ethics Committee of Anqing Municipal Hospital (ref. no. 2020. 086). All patients provided signed informed consent prior to the surgery.
Case inclusion and exclusion criteria
The inclusion criteria were as follows: i) Gastric cancer diagnosed by gastroscopy and pathological examination prior to surgery; ii) patients show underwent either laparoscopic operation or open surgery, and the type of resection included radical/total, distal or proximal gastrectomy; iii) R0 resection and lymph nodes that reached D1+ or D2 dissection; iv) post-operative early complications occurred 30 days post-surgery; and v) the clinical pathology, complications and follow-up data of the patients were complete and correct, and each surgery was performed by the same group of surgeons.
The exclusion criteria were as follows: i) Pre-operative examination and intraoperative exploration of distant tumor metastasis, which could not be achieved by radical resection; ii) patients who had received neoadjuvant or conversion therapy prior to surgery; iii) patients who had received intraoperative therapy, such as hyperthermic intraperitoneal chemotherapy; iv) abdominal aortic lymph node dissection; v) pylorus-preserving gastrectomy; vi) the presence of other simultaneous malignant tumors; vii) remnant gastric carcinoma; and viii) emergency surgery.
Classification standards
The modified Clavien-Dindo grading system was used to classify post-operative complications (grade ≥I was defined as post-operative complications and grade ≥IIIa was defined as severe post-operative complications) (6). The present study also utilized the nutritional risk screening 2002 (NRS2002) screening tool (7), the American Society of Anesthesiologists (ASA) scoring system (8) and the Charlson comorbidity index (CCI) (9). Tumors were staged in accordance with the Union for International Cancer Control Classification System (8th edition) (10).
Patient follow-up
All patients who agreed to undergo RG were followed-up from the date of surgery. The final follow-up date was September, 2020, and the median follow-up was 62 months. Overall survival (OS) was calculated from the date of surgery to the date of death, regardless of the cause or date of censoring.
Statistical analysis
SPSS 26.0 software (SPSS, Inc.) was used for statistical analysis. Continuous variables are presented as the mean ± standard deviation. The post-operative hospital stay of the patients in the different groups was compared using the Mann-Whitney U-test. The association between the presence of complications and clinical features, including sex, age, body mass index (BMI), history of surgery, NRS2002, CCI, ASA score, pre-operative comorbidity, blood loss, operation time, type of surgery, resection type, multiple organ resection and tumor size was examined using Fisher's exact test and the Chi-squared test (univariate analysis). Valuables with P-values <0.05 in the univariate analysis were included in the multivariate regression analysis to identify the risk factors for post-operative complications and severe complications. The post-operative survival rate was analyzed by plotting the Kaplan-Meier graph, with differences in survival rates assessed using the log-rank test. A Cox proportional-hazards regression model was used for univariate and multivariate analyses. P<0.05 was considered to indicate a statistically significant difference.
Results
Patient characteristics
The present study included 387 males and 138 females, and the mean age was 62.5±10.7 years (range, 16-89 years). The most frequent complication was hypertension (16.8%), and the incidences of early-stage (T stage 1a and 1b) and advanced-stage (T stage 2, 3, 4a and 4b) and gastric cancer were 17.7% (93/525) and 82.3% (432/525), respectively. In total, 12 patients underwent combined organ resection, and no patient died from post-operative complications. The proportions of total gastrectomy and laparoscopy were 62.9% (330/525) and 23.0% (121/525), respectively. The patient characteristics are depicted in Table II.
 |
Table II
Characteristics of the 525 patients undergoing gastrectomy.
|
Table II
Characteristics of the 525 patients undergoing gastrectomy.
| Patient characteristics |
Total (n=525) |
| Age (years) |
62.5±10.7 |
| Sex (male/female) |
387/138 |
| Body mass index |
21.3±3.1 |
| History of previous abdominal surgery (%) |
51 (9.7) |
| Pre-operative comorbidities (%) |
123 (23.4) |
| Hypertension |
88 (16.8) |
| Diabetes |
19 (3.6) |
| Heart disease |
12 (2.2) |
| Cerebrovascular disease |
10 (1.9) |
| COPD |
8 (1.5) |
| Immune system diseases |
6 (1.1) |
| Cirrhosis |
6 (1.1) |
| History of malignant tumor |
4 (0.8) |
| Combination of ≥2 |
29 (5.5) |
| Multiple organ resection (%) |
39 (7.4) |
| Combined organectomy |
12 (2.2) |
| Cholecystectomy |
18 (3.4) |
| Abdominal benign tumor resection |
9 (1.7) |
| ASA score (1/2/3/4/5) |
365/124/36/0/0 |
| Histological differentiation (high/middle/low) |
35/97/393 |
| Modified Clavien-Dindo classification (1/2/3a/3b/4a/4b/5) |
25/69/15/4/1/0/0 |
| T stage (T1a/T1b/T2/T3/T4a/T4b) |
56/37/60/2/350/20 |
| N stage (N0/N1/N2/N3a/N3b) |
204/94/97/96/34 |
| TNM stage (1a/1b/2a/2b/3a/3b/3c) |
83/41/16/91/161/94/39 |
| Tumor distribution (upper/middle/lower/two sites and above) |
187/156/166/16 |
| Resection type (total/proximal/distal) |
330/9/186 |
| Type of surgery (open/laparoscopy) |
404/121 |
| Extent of lymph node dissection (D1+/D2) |
103/422 |
| Number of retrieved lymph node (pieces) |
22.9±9.8 |
| Post-operative hospital stay (days) |
11.9±5.3 |
| Duration of surgery (min) |
238.6±51.9 |
| Blood loss (ml) |
187.3±141.2 |
| Time of first flatus (days) |
4.4±1.4 |
Modified Clavien-Dindo classification and postoperative hospital stay for early post-operative complications
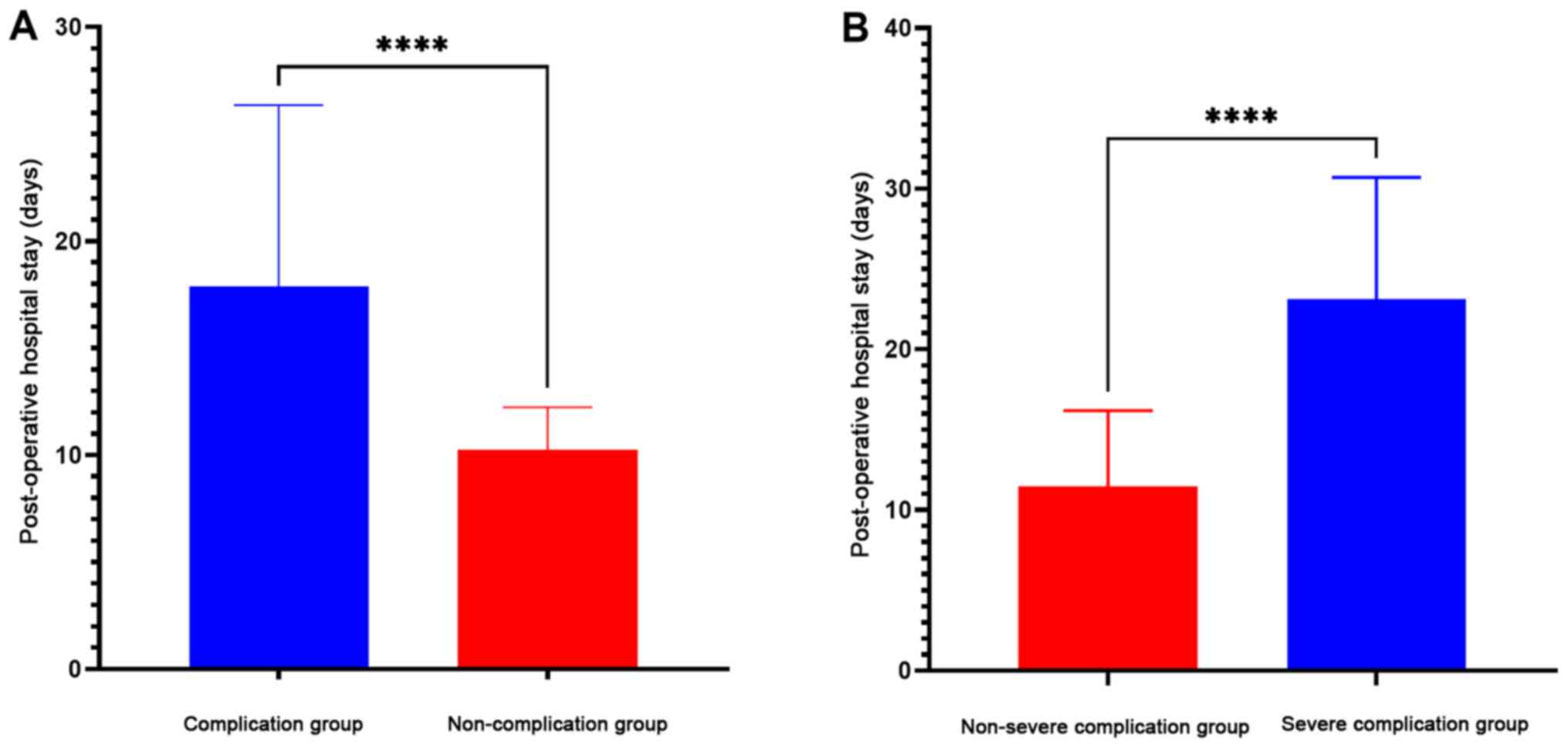
A total of 114 cases were graded as Clavien-Dindo ≥I (complications), accounting for 21.7% (114/525) of the total number of cases, and 20 cases were graded as Clavien-Dindo ≥IIIa (severe complications), accounting for 17.5% (20/114) of postoperative complications and 3.8% (20/525) of the total number of cases (Table III). The most common complication was pneumonia (42 cases), occurring at a rate of 8% (42/525), and the most severe post-operative complication was duodenal stump leakage (10 cases), accounting for 8.8% (10/114) of the complications and 50% (10/20) of the severe complications (Table III). A total of 4 patients needed to undergo reoperation in the severe complication group under general anesthesia (2 patients with abdominal bleeding, 1 patient with intestinal obstruction and 1 patient with drainage tube incarceration). The post-operative hospital stay in the complication group was 17.88±8.472 days, and that in the severe complication group was 23.10±7.594 days, which was significantly longer than that in the non-complication group (10.26±1.973 days) and non-severe complication group (11.47±4.712 days), respectively (P=0.001; Fig. 1).
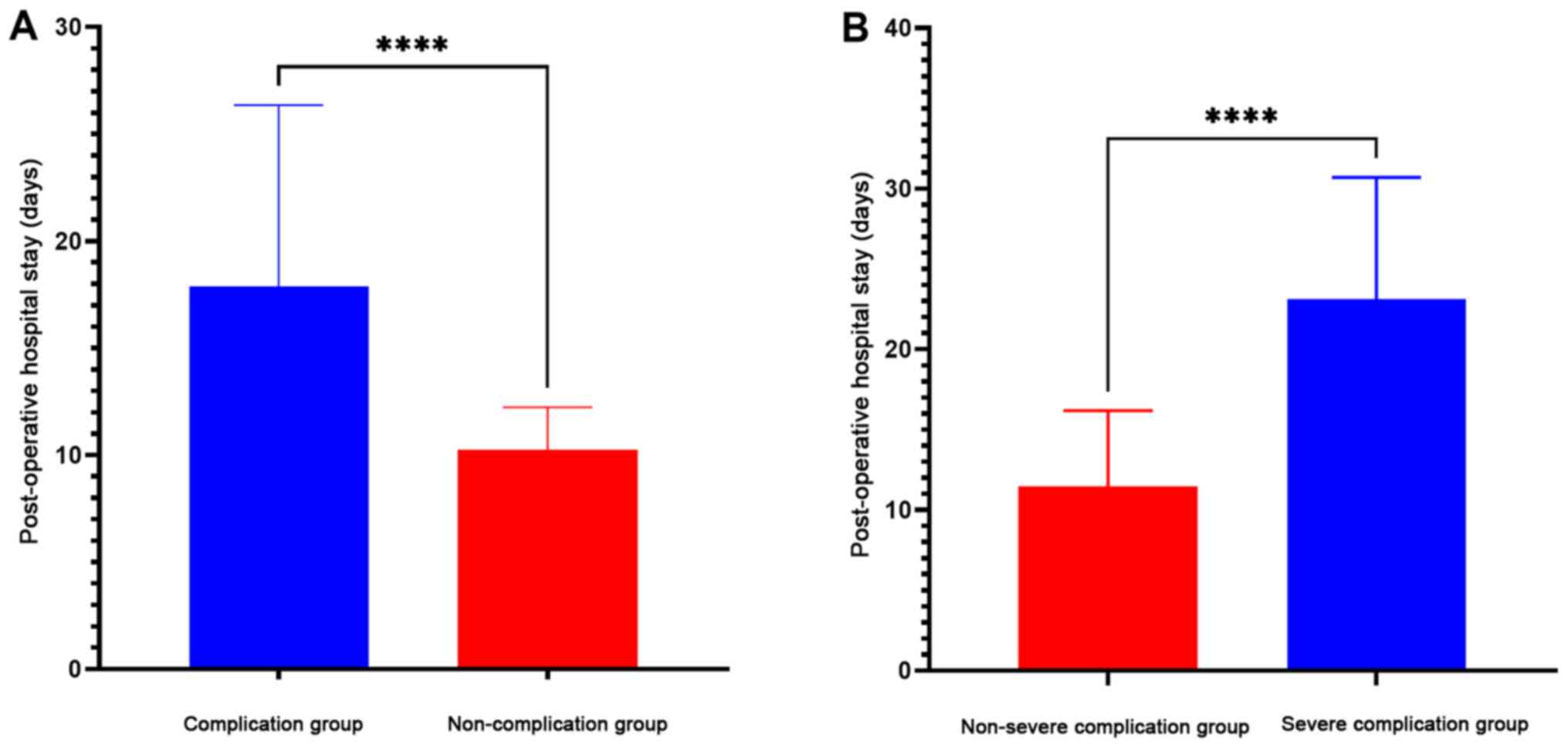 |
Figure 1
(A) Comparison of the length of post-operative hospital stay between the complication group (17.88±8.47 days) and the non-complication group (10.26±1.97 days). (B) Comparison of the length of post-operative hospital stay between the severe complication group (23.10±7.59 days) and the non-severe complication group (10.26±1.97 days). ****P<0.0001.
|
 |
Table III
Modified Clavien-Dindo classification of post-operative complications.
|
Table III
Modified Clavien-Dindo classification of post-operative complications.
| |
Modified Clavien-Dindo classification |
| Complication |
No. of cases |
I |
II |
IIIa |
IIIb |
Ⅳa |
Ⅳb |
Ⅴ |
| Pneumonia |
42 |
6 |
36 |
|
|
|
|
|
| Bloating and reflux |
12 |
11 |
1 |
|
|
|
|
|
| Duodenal stump leakage |
10 |
|
|
10 |
|
|
|
|
| Abdominal bleeding |
5 |
|
3 |
|
2 |
|
|
|
| Gastroparesis |
4 |
|
4 |
|
|
|
|
|
| Chylous leakage |
4 |
2 |
2 |
|
|
|
|
|
| Anastomotic stenosis |
4 |
2 |
2 |
|
|
|
|
|
| Ascites |
4 |
2 |
2 |
|
|
|
|
|
| Cholecystitis |
3 |
|
3 |
|
|
|
|
|
| Fever |
3 |
|
3 |
|
|
|
|
|
| Abdominal infection |
3 |
|
2 |
1 |
|
|
|
|
| Abnormal liver function |
3 |
|
3 |
|
|
|
|
|
| Intestinal obstruction |
2 |
|
1 |
|
1 |
|
|
|
| Anastomotic bleeding |
2 |
|
2 |
|
|
|
|
|
| Arrhythmia |
2 |
|
2 |
|
|
|
|
|
| Pleural effusion |
2 |
|
|
2 |
|
|
|
|
| Liver abscess |
1 |
|
1 |
|
|
|
|
|
| Urinary retention |
1 |
1 |
|
|
|
|
|
|
| Pneumothorax |
1 |
|
|
1 |
|
|
|
|
| Anastomotic leakage |
1 |
|
|
1 |
|
|
|
|
| Heart failure |
1 |
|
|
|
|
1 |
|
|
| Thrombus |
1 |
|
1 |
|
|
|
|
|
| Pancreatic leakage |
1 |
|
1 |
|
|
|
|
|
| Drainage tube incarceration |
1 |
|
|
|
1 |
|
|
|
| Fat liquefaction |
1 |
1 |
|
|
|
|
|
|
| Total |
114 |
25 |
69 |
15 |
4 |
1 |
0 |
0 |
Risk factors for postoperative complications
Univariate analysis was used to determine the risk factors for post-operative complications. Age, the ASA score, CCI, pre-operative comorbidity, blood loss and type of surgery type were associated with complications. Sex, blood loss, the duration of the surgery time and resection type were associated with severe complications (Table IV). In the multivariate analysis that included these factors, age (OR, 1.781; P=0.013), pre-operative comorbidity (OR, 1.765; P=0.020), blood loss (OR, 2.153; P=0.001) and type of surgery (OR, 3.137; P=0.000) were independent risk factors for the development of early post-operative complications. Blood loss (OR, 13.053; P=0.013) and resection type (OR, 7.936; P=0.047) were identified as independent risk factors for the development of early post-operative severe complications (Table IV).
 |
Table IV
Univariate and multivariate analysis for early post-operative complications and severe complications.
|
Table IV
Univariate and multivariate analysis for early post-operative complications and severe complications.
| |
Complications |
Severe complications |
| |
Univariate analysis |
Multivariate analysis |
Univariate analysis |
Multivariate analysis |
| |
Complications (%) |
P-value |
OR |
95% CI |
P-value |
Severe complications (%) |
P-value |
OR |
95% CI |
P-value |
| Sex (male/female) |
21.7 (84/387)/21.7 (30/138) |
0.993 |
1.781 |
1.132-2.802 |
0.013 |
4.9 (19/387)/0.7 (1/138) |
0.027 |
|
|
|
| Age (≥70 vs. <70 years) |
30.5 (46/151)/18.2 (68/374) |
0.002 |
|
|
|
6.0 (9/151)/2.9 (11/374) |
0.102 |
|
|
|
| BMI (≥24 vs. <24 kg/m2) |
27.7 (23/83)/20.6 (91/442) |
0.149 |
|
|
|
3.6 (3/83)/3.8 (17/442) |
1.000 |
|
|
|
| History of surgery (yes vs. no) abdominal surgery |
23.5 (12/51)/21.5 (102/474) |
0.741 |
|
|
|
3.9 (2/51)/3.8 (18/474) |
1.000 |
|
|
|
| NRS2002 score (≥4 vs. <4) |
23.3 (62/266)/20.1 (52/259) |
0.369 |
|
|
|
4.5 (12/266)/3.1 (8/259) |
0.395 |
|
|
|
| CCI (≥2 vs. <2) |
24.4 (87/357)/16.1 (27/168) |
0.031 |
|
|
|
4.8 (17/357)/1.8 (3/168) |
0.097 |
|
|
|
| ASA score (≥3 vs. <3) |
41.7 (15/36)/20.2 (99/489) |
0.003 |
|
|
|
5.6 (2/36)/3.7 (18/489) |
0.908 |
|
|
|
| Pre-operative comorbidity (yes vs. no) |
30.9 (38/123)/18.9 (76/402) |
0.005 |
1.765 |
1.094-2.846 |
0.020 |
6.5 (8/123)/3.0 (12/402) |
0.130 |
|
|
|
| Blood loss (≥150 vs. <150 ml) |
26.1 (81/310)/15.3 (33/215) |
0.003 |
2.153 |
1.354-3.423 |
0.001 |
6.1 (19/310)/0.5 (1/215) |
0.001 |
13.053 |
1.712-99.497 |
0.013 |
| Duration of surgery (≥235 vs. <235 min) |
24.6 (66/268)/18.7 (48/257) |
0.098 |
|
|
|
5.6 (15/268)/1.9 (5/257) |
0.029 |
|
|
|
| Surgery type (open vs. laparoscopy) |
25.0 (101/404)/10.7 (13/121) |
0.001 |
3.137 |
1.665-5.911 |
<0.001 |
3.7 (15/404)/4.1 (5/121) |
1.000 |
|
|
|
| Resection type (total vs. subtotal) |
22.4 (74/330)/20.5 (40/195) |
0.608 |
|
|
|
5.8 (19/330)/0.5(1/195) |
0.002 |
7.936 |
1.032-61.044 |
0.047 |
| Multiple organ resection (yes vs. no) |
30.8 (12/39)/21.0 (102/486 |
0.154 |
|
|
|
5.1 (2/39)/3.7 (18/486) |
0.990 |
|
|
|
| Tumor size (≥4 cm vs. <4 cm |
21.8 (62/284)/21.6 (52/241) |
0.944 |
|
|
|
4.9 (14/284)/2.5 (6/241) |
0.146 |
|
|
|
Survival analysis based on the modified Clavien-Dindo classification
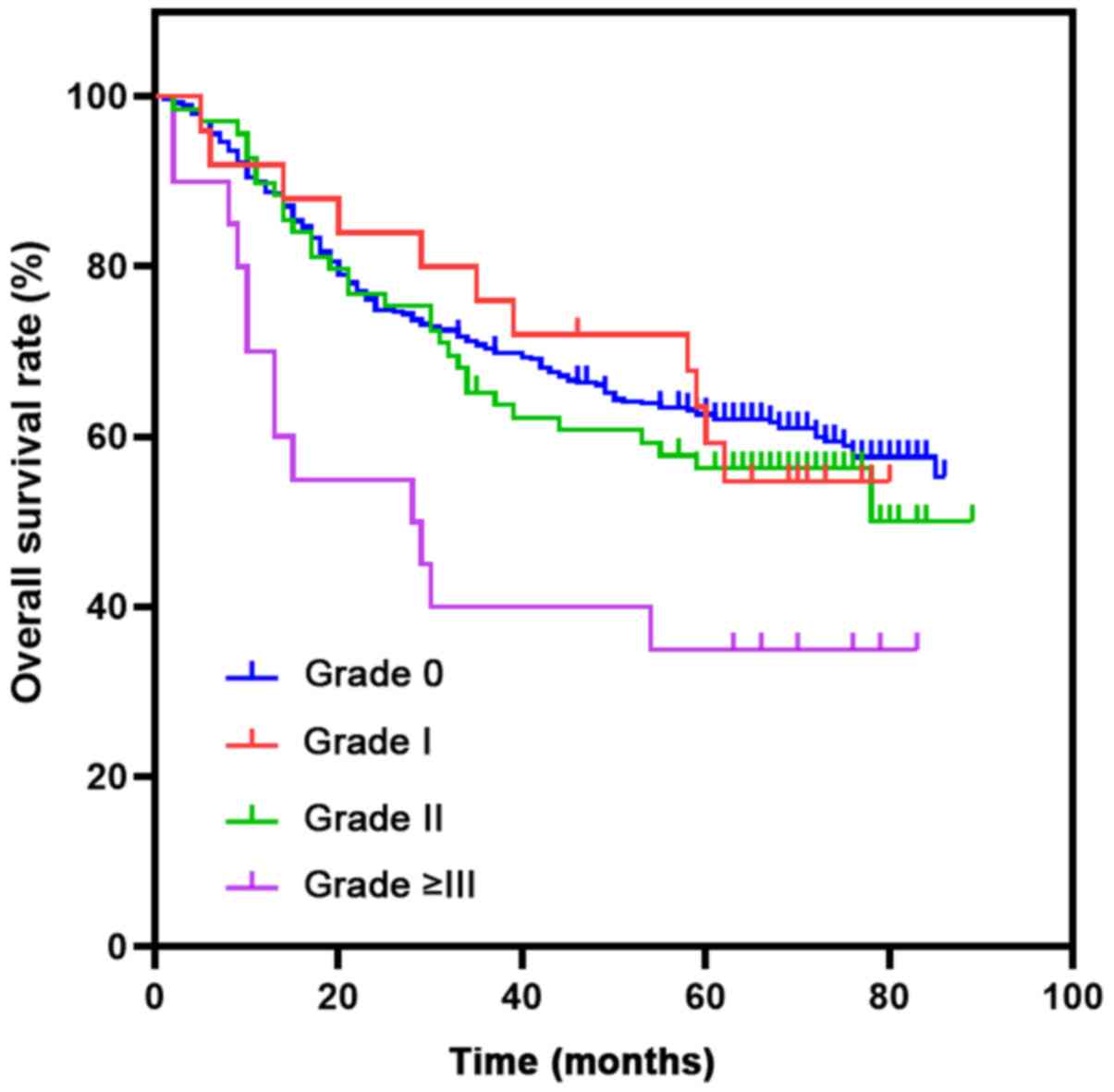
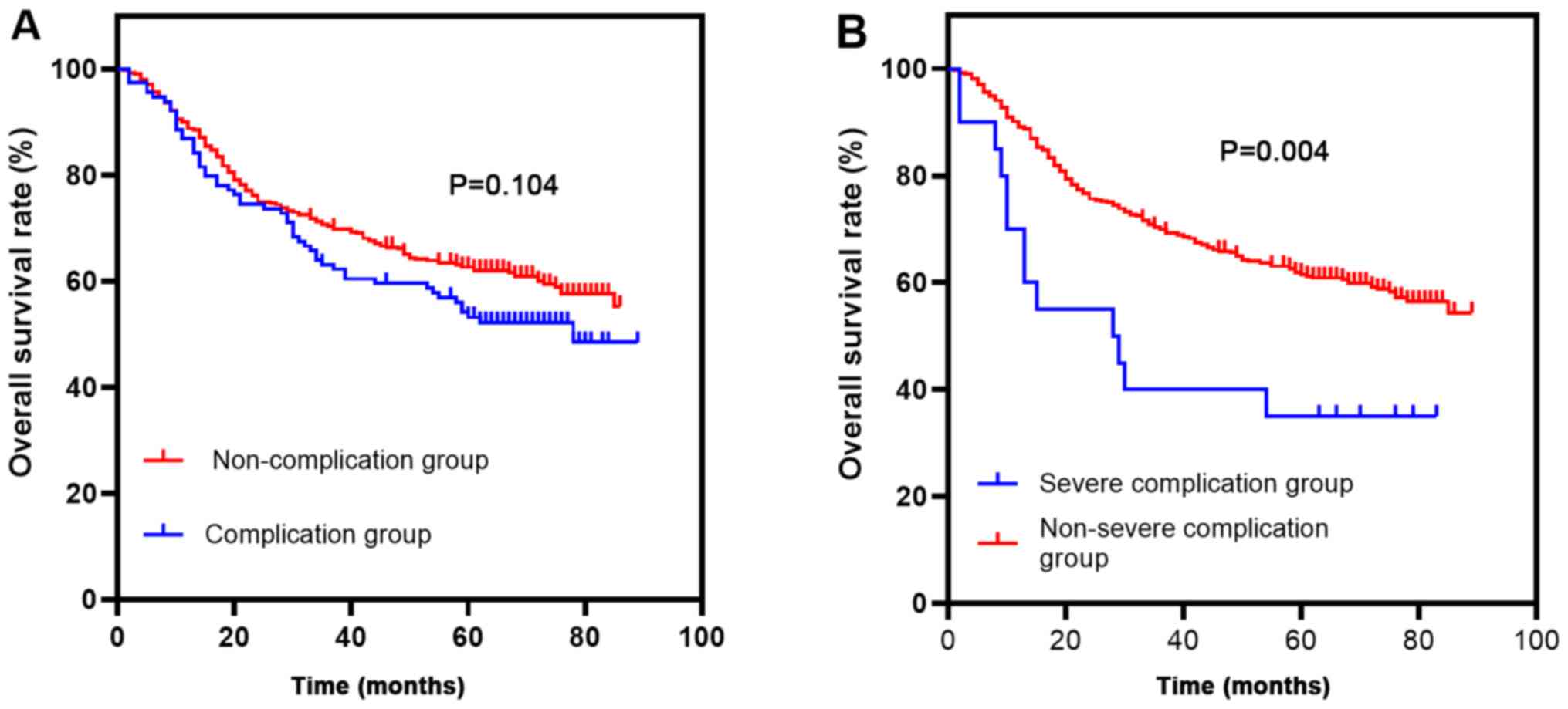
As shown in Fig. 2, the 5-year OS rates of patients with grade I, II and ≥III complications were 59.3, 56.3 and 35%, respectively. As shown in Fig. 3, the 5-year OS rates of patients in the complication group and the non-complication group were 53.2 and 62.6%, respectively (P=0.104). The 5-year OS rates of patients in the post-operative severe complication group and non-severe complication group were 35 and 61.8%, respectively (P=0.004). As shown in Table V, TNM stage [hazard ratio (HR), 2.917; P<0.001] and pre-operative comorbidities (HR, 1.448; P=0.016) were independent risk factors that affected the 5-year OS. Severe post-operative complications (HR, 1.595; P=0.107) were not identified as independent risk factors affecting the 5-year OS.
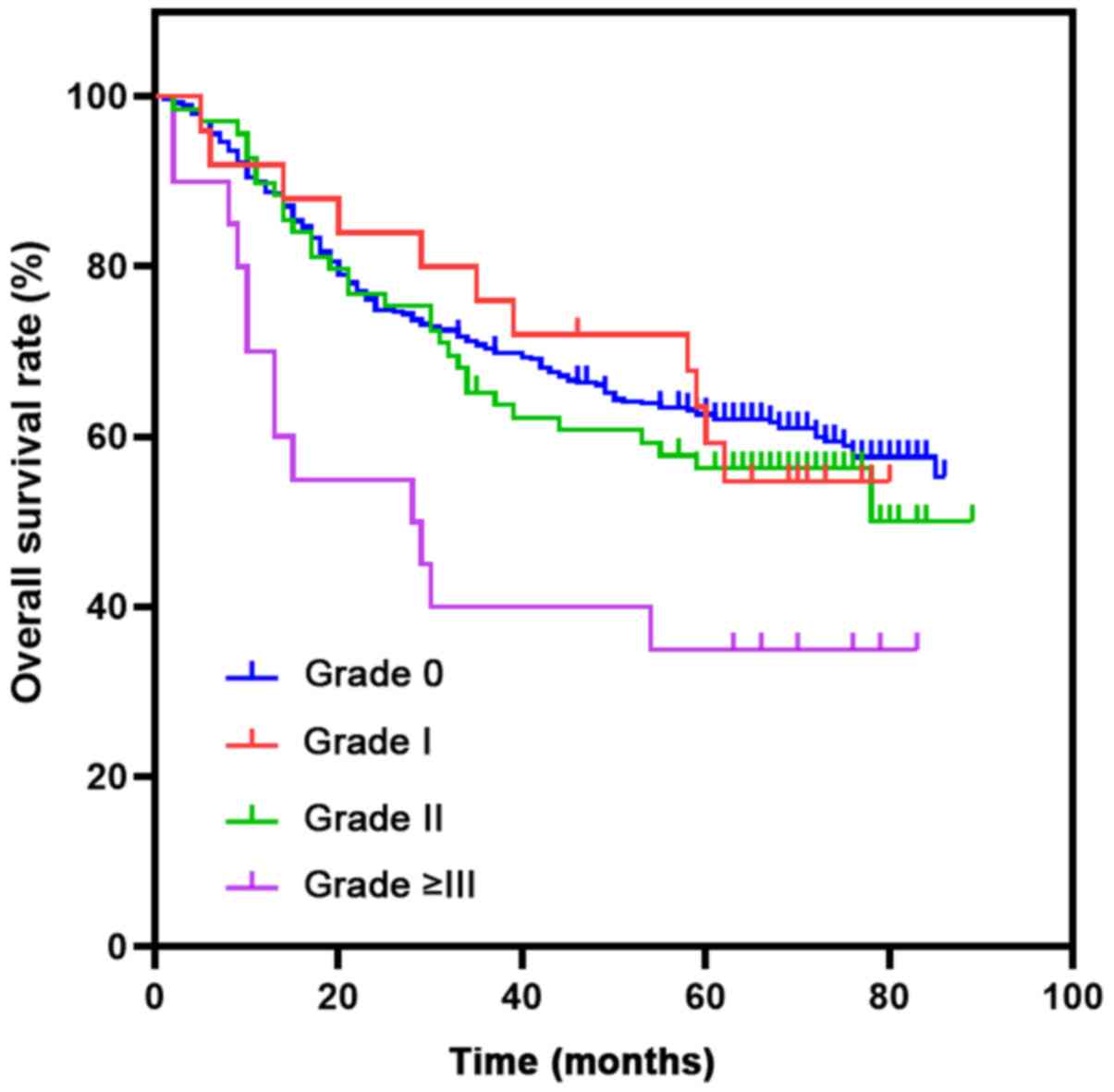 |
Figure 2
Kaplan-Meier curves were plotted to estimate the patient overall 5-year survival according to the Clavien-Dindo classification.
|
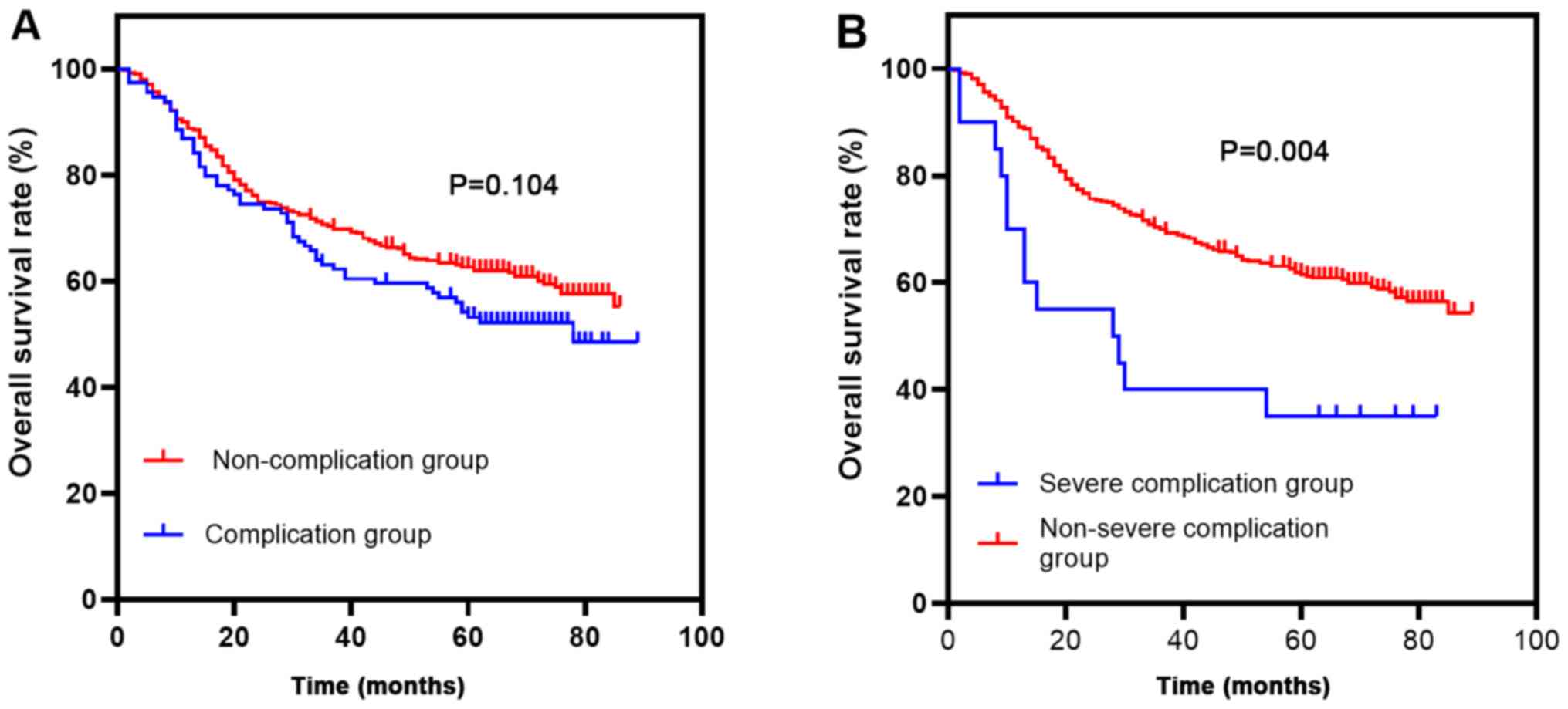 |
Figure 3
(A) Overall survival curves for 525 patients who underwent curative gastrectomy for gastric cancer. The 5-year overall survival rates of patients in the complication group and the non-complication group were 53.2 and 62.6%, respectively (P=0.104; P>0.05). (B) The 5-year OS was significantly higher in the group of patients without severe complications than in the group with severe complications (P=0.004; P<0.05).
|
 |
Table V
Univariate and multivariate analysis for independent prognostic factors for overall survival (severe complications).
|
Table V
Univariate and multivariate analysis for independent prognostic factors for overall survival (severe complications).
| |
Univariate analysis |
Multivariate analysis |
| |
P-value |
HR |
95% CI |
P-value |
HR |
95% CI |
| TNM stage |
0.001 |
3.242 |
2.373-4.430 |
<0.001 |
2.917 |
2.122-4.011 |
| Pre-operative comorbidity |
0.004 |
1.536 |
1.149-2.053 |
0.016 |
1.448 |
1.073-1.956 |
| Severe complications |
0.005 |
2.246 |
1.282-3.936 |
0.107 |
1.595 |
0.904-2.815 |
| Histological type |
0.006 |
1.602 |
1.144-2.243 |
0.363 |
1.174 |
0.831-1.660 |
| Age |
0.030 |
1.364 |
1.030-1.804 |
0.177 |
1.217 |
0.915-1.620 |
| Sex |
0.423 |
1.135 |
0.833-1.546 |
0.659 |
1.073 |
0.785-1.468 |
Discussion
The present study demonstrated that 114 patients experienced early complications following RG, 20 patients experienced severe complications, and no post-operative deaths occurred. Pneumonia, gastrointestinal symptoms (abdominal distension and reflux), duodenal stump leakage, abdominal hemorrhage, gastroparesis, chylous leakage and ascites were common early complications. The most common complication was pneumonia, which was in line with the findings of previous research (11). The following reasons may explain why pneumonia was the most common complication: i) The average age of the patients was 62.5±10.7 years, the proportion of patients ≥70 years of age was 28.8%, the lung elasticity and chest wall compliance of elderly patients were naturally reduced, the amount of residual alveolar gas was increased, and elderly patients tended to be more prone to respiratory muscle fatigue and upper respiratory tract obstruction (12); ii) the proportion of males was 73.7% (387/525), which was consistent with the data of the geographical Cancer Registry in China (13) and a greater proportion of male patients smoked (117/387), increasing their risk of developing post-operative pneumonia (14); and iii) the proportion of total gastrectomy, which has been suggested as a notable post-operative risk associated with total gastrectomy (15) in the present study was high, accounting for 62.9% (330/525).
In the present study, the most severe post-operative complication was duodenal stump leakage, which was consistent with the findings of a previous study (16). Previous studies have demonstrated that age and pre-operative comorbidity are associated with the occurrence of duodenal stump leakage (17,18). In the Anqing Municipal Hospital, the duodenal stump was reinforced, but not embedded in the past. Following technical improvement, the stump is now embedded, allowing for a marked reduction in leakage from the duodenal stump (19,20).
It is worth noting that intra-abdominal hemorrhage should alert the surgeon, as 2 of the 5 patients who presented with intra-abdominal hemorrhage required a second surgery; thus, 2 patients with anastomotic hemorrhage were successfully cured with conservative treatment, suggesting that the prognosis of anastomotic hemorrhage was superior to that of intra-abdominal hemorrhage.
A multivariate logistic regression model identified that blood loss was a 2-fold independent risk factor for post-operative complications and severe post-operative complications, which was in line with the findings of other studies (21,22). Excessive bleeding during surgery not only affects the stability of intraoperative hemodynamics, but may also affect the disposition of the surgeon, which is not conducive for the high-quality completion of the operative procedure. Patients with post-operative anemia often display a poor general condition and a lower threshold for stress, which hinders the healing of the anastomosis or stump (23). Anemia may lead to insufficient tissue oxygenation and low protein levels, ultimately increasing the risk of infection (24).
The present study demonstrated that age was an independent risk factor for post-operative complications. First, elderly patients usually exhibit insufficient lung function prior to surgery and poor sputum excretion post-surgery. Through a retrospective analysis of 750 cases of gastric cancer surgery, Miki et al (12) reported age as an independent risk factor for post-operative lung infection. Second, elderly patients with gastric cancer often present with hypoproteinemia and are more likely to develop anastomosis and stump leakage (17). Finally, compared with younger individuals, elderly patients had higher ASA scores (25). Through a gastric cancer cohort study, Nelen et al (25) found that the ASA score of elderly patients was significantly higher than that of the younger group. In addition, an age >70 years was a risk factor for post-operative complications (25).
Herein, pre-operative comorbidity was an independent risk factor for post-operative complications. Filip et al (17) found that hypertension was a dual independent risk factor for post-operative and surgical complications. Choudhuri et al (23) demonstrated that hypertension was also an independent risk factor for gastrointestinal leakage. In addition, chronic obstructive pulmonary disease (COPD) and coronary heart disease contribute to an increased probability of post-operative complications. Coimbra et al (26) demonstrated that COPD and coronary heart disease were independent risk factors for post-operative complications. Finally, diabetes may easily lead to complications, such as incision infection, poor healing and anastomotic leakage. Wang et al (27) retrospectively analyzed 1,657 cases of laparoscopic-assisted total gastrectomy, and they reported that diabetes was closely related to the incidence rate of post-operative anastomotic leakage, abdominal bleeding and lung infection.
In the present study, open surgery was found to be an independent risk factor for post-operative complications, which is in agreement with the findings of previous research (28). First, in comparison to open surgery, patients who underwent laparoscopic surgery felt less pain and had a greater ability to use lung capacity, thereby reducing the probability of lung infection. Second, minimally invasive surgery may result in a more rapid return of enteric function, and patients may be able to eat and arise earlier, thereby reducing the incidence of ascites due to hypoproteinemia and diminishing the probability of venous thrombosis and atelectasis.
In addition, total gastrectomy was found to be an independent risk factor for severe post-operative complications. Compared with subtotal gastrectomy, there is a larger range of dissections and more anastomoses in total gastrectomy (25). According to the Japanese Gastric Cancer Treatment Guidelines (29), the splenic hilar lymph nodes, as part of D2 dissection, are routinely cleaned at the Anqing Municipal Hospital. This operation may increase the incidence of vascular injury and splenic bleeding. For several special cases, such as males or 'barrel chest', esophageal-jejunum anastomoses were too difficult to perform. The incidence of pleural effusion and pneumothorax was increased when the surgeon dissected the splenic hilar and mediastinal lymph nodes (the severe complication group had 1 case with pneumothorax and 2 cases with pleural effusion who underwent pleural drainage following total gastrectomy).
The 5-year OS of the patients in the severe complication group was only 35%, which was significantly worse than that of the non-severe complication group (61.8%); however, Cox analysis revealed that severe complications were not an independent risk factor affecting prognosis, which was inconsistent with the findings of other studies (30,31). Potential explanations for the controversial data are as follows: i) Cox regression multivariate analysis revealed severe post-operative complications (HR, 1.595, P=0.107), although these complications were not significant (P>0.05), which may be related to the small sample size of the severe complication group (n=20); and ii) gastrointestinal complications (such as nausea, gastrointestinal reflux, anastomotic stenosis) in the non-severe complications group may lead to a poor post-operative nutritional status, which potentially affects long-term prognosis.
The present study had the following limitations: i) The aim of the present study was to investigate the occurrence of early post-operative complications and to minimize confounding factors via inclusion and exclusion criteria; the limitation was its retrospective nature, and the conclusions drawn need to be further confirmed by a multicenter, large-sample prospective cohort study; and ii) certain post-operative complications may occur a month later, and these later complications were not counted as data in the present study.
In addition, considering that previous literature on post-operative complications mainly included retrospective studies (30,31), the authors aim to adopt a prospective nest-case-control study to observe the association between complications and long-term prognosis following the radical resection of gastric cancer; this analysis has already been registered in the Chinese Clinic Trial Registry (ChiCTR2100043385).
In conclusion, the present study demonstrated that age, preoperative comorbidity, blood loss, and open surgery represent independent risk factors associated with early complications following RG. Total gastrectomy and blood loss were independent risk factors for early post-operative severe complications. The 5-year OS of patients in the severe complication group was significantly worse than that of patients in the non-severe complication group. Although early post-operative complications are not an independent risk factor for poor prognosis, they may significantly prolong the post-operative hospital stay. It is thus recommended that surgeons aim to minimize the occurrence of early post-operative complications, particularly severe complications, which may help shorten the length of hospital stay, increase the bed turnover rate, reduce the economic burden of patients and may ultimately improve the quality of life of patients.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National Natural Science Foundation of China (grant no. 81873730).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
JM and YW conceived and designed the study. SY, CZ and DW analyzed the data. DT and GJ interpreted the results of the analyses. JM, YW and SY drafted the manuscript. YZ and GJ edited and revised the manuscript. YZ reviewed the manuscript. JM and DT confirmed the authenticity of all the raw data All authors have read and approved the final version of the manuscript.
Ethics approval and consent to participate
The present study was approved by the Medical Ethics Committee of Anqing Municipal Hospital (ref. no. 2020. 86). Written informed consent was obtained from each patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
1
|
Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, Xia C, Sun K, Yang Z, Li H, et al: Changing cancer survival in China during 2003-15: A pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 6:e555–e567. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kurita N, Miyata H, Gotoh M, Shimada M, Imura S, Kimura W, Tomita N, Baba H, Kitagawa Y, Sugihara K, et al: Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a nationwide web-based data entry system. Ann Surg. 262:295–303. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Clavien PA, Sanabria JR and Strasberg SM: Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 111:518–526. 1992.PubMed/NCBI
|
|
4
|
Dindo D, Demartines N and Clavien PA: Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. 2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, et al: The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg. 250:187–196. 2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, Tsubosa Y, Satoh T, Yokomizo A, Fukuda H, et al: Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 46:668–685. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kondrup J, Allison SP, Elia M, Vellas B and Plauth M: Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr. 22:415–421. 2003.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mupparapu M and Singer SR: Editorial: The American Society of Anesthesiologists (ASA) physical status classification system and its utilization for dental patient evaluation. Quintessence Int. 49:255–256. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Charlson M, Szatrowski TP, Peterson J and Gold J: Validation of a combined comorbidity index. J Clin Epidemiol. 47:1245–1251. 1994.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al: The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more ‘personalized’ approach to cancer staging. CA Cancer J Clin. 67:93–99. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Gertsen EC, Brenkman HJ, Seesing MF, Goense L, Ruurda JP and van Hillegersberg R: Dutch Upper Gastrointestinal Cancer Audit (DUCA) group. Introduction of minimally invasive surgery for distal and total gastrectomy: A population-based study. Eur J Surg Oncol. 45:403–409. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Miki Y, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Kawamura T and Terashima M: Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg Today. 46:552–556. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chen W, Zheng R, Zeng H and Zhang S: The incidence and mortality of major cancers in China, 2012. Chin J Cancer. 35(73)2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rei J, Lareiro S, Fernandes P, Guerra M, Miranda J and Vouga L: Uniportal video-assisted thoracic surgery anatomical resections - does previous tobacco exposure adversely influence post-operative outcomes? Rev Port Cir Cardiotorac Vasc. 26:121–125. 2019.PubMed/NCBI
|
|
15
|
Ntutumu R, Liu H, Zhen L, Hu YF, Mou TY, Lin T, i BA, Yu J and Li GX: Risk factors for pulmonary complications following laparoscopic gastrectomy: A single-center study. Medicine (Baltimore). 95(e4567)2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ramos MFKP, Pereira MA, Barchi LC, Yagi OK, Dias AR, Szor DJ, Zilberstein B, Ribeiro-Júnior U and Cecconello I: Duodenal fistula: The most lethal surgical complication in a case series of radical gastrectomy. Int J Surg. 53:366–370. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Filip B, Toma C, Buna-Arvinte M, Scripcariu DV and Scripcariu V: Impact of surgery and early postoperative outcomes after radical gastrectomy for cancer. Chirurgia (Bucur). 113:478–485. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Paik HJ, Lee SH, Choi CI, Kim DH, Jeon TY, Kim DH, Jeon UB, Choi CW and Hwang SH: Duodenal stump fistula after gastrectomy for gastric cancer: Risk factors, prevention, and management. Ann Surg Treat Res. 90:157–163. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Orsenigo E, Bissolati M, Socci C, Chiari D, Muffatti F, Nifosi J and Staudacher C: Duodenal stump fistula after gastric surgery for malignancies: A retrospective analysis of risk factors in a single centre experience. Gastric Cancer. 17:733–744. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim MC, Kim SY and Kim KW: Laparoscopic Reinforcement Suture (LARS) on Staple Line of Duodenal Stump Using Barbed Suture in Laparoscopic Gastrectomy for Gastric Cancer: A Prospective Single Arm Phase II Study. J Gastric Cancer. 17:354–362. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wakahara T, Ueno N, Maeda T, Kanemitsu K, Yoshikawa T, Tsuchida S and Toyokawa A: Postoperative morbidity in elderly patients after gastric cancer surgery. Ann Gastroenterol. 31:621–627. 2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ishino Y, Saigusa S, Ohi M, Yasuda H, Tanaka K, Toiyama Y, Mohri Y and Kusunoki M: Preoperative C-reactive protein and operative blood loss predict poor prognosis in patients with gastric cancer after laparoscopy-assisted gastrectomy. Asian J Endosc Surg. 7:287–294. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Choudhuri AH, Uppal R and Kumar M: Influence of non-surgical risk factors on anastomotic leakage after major gastrointestinal surgery: Audit from a tertiary care teaching institute. Int J Crit Illn Inj Sci. 3:246–249. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Lv H, Yin P, Long A, Gao Y, Zhao Z, Li J, Zhang L, Zhang L and Tang P: Clinical characteristics and risk factors of postoperative pneumonia after hip fracture surgery: A prospective cohort study. Osteoporos Int. 27:3001–3009. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Nelen SD, Bosscha K, Lemmens VE, Hartgrink HH, Verhoeven RH and de Wilt JH: Dutch Upper Gastrointestinal Cancer Audit group. Morbidity and mortality according to age following gastrectomy for gastric cancer. Br J Surg. 105:1163–1170. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Coimbra FJ, de Jesus VH, Franco CP, Calsavara VF, Ribeiro HS, Diniz AL, de Godoy AL, de Farias IC, Riechelmann RP, Begnami MD, et al: Predicting overall and major postoperative morbidity in gastric cancer patients. J Surg Oncol. 120:1371–1378. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang JB, Zheng CH, Li P, Xie JW, Lin JX, Lu J, Chen QY, Cao LL, Lin M and Huang CM: Effect of comorbidities on postoperative complications in patients with gastric cancer after laparoscopy-assisted total gastrectomy: Results from an 8-year experience at a large-scale single center. Surg Endosc. 31:2651–2660. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yang SY, Roh KH, Kim YN, Cho M, Lim SH, Son T, Hyung WJ and Kim HI: Surgical outcomes after open, laparoscopic, and robotic gastrectomy for gastric cancer. Ann Surg Oncol. 24:1770–1777. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 14:101–112. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Li Z, Bai B, Ji G, Li J and Zhao Q: Relationship between Clavien-Dindo classification and long-term survival outcomes after curative resection for gastric cancer: A propensity score-matched analysis. Int J Surg. 60:67–73. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Powell A, Coxon AH, Patel N, Chan D, Christian A and Lewis W: Prognostic significance of post-operative morbidity severity score after potentially curative D2 gastrectomy for carcinoma. J Gastrointest Surg. 22:1516–1527. 2018.PubMed/NCBI View Article : Google Scholar
|